The norm is considered to be homogeneous echogenicity of the uterine tissue. In terms of its structure, this organ, which is one of the most important in the female reproductive system, has smooth muscles covered with endometrial tissue (uterine myometrium). The described structure is a reference and if deviations from the norm are detected in the density of the walls (increased echogenicity), they are recognized as a pathology.
It is important to know that a detected violation of the echo density of the uterus requires mandatory treatment, as it can be a harbinger of serious diseases of the reproductive system, including the development of infertility.
In the event that a woman feels periodic nagging pain after the process of ovulation, during menstruation, or after sexual intercourse, also if there is discomfort in the lower abdomen, it is necessary to consult a doctor for a comprehensive examination to diagnose the disease that provokes such negative phenomena in organism.
Procedures for diagnosing the disease
The echogenicity of the walls of the uterus is an indicator characterizing the structure of the tissues being studied in a woman’s body. Diagnosis of the structure and structure of the uterus is made on the basis of a comprehensive ultrasound examination of the pelvic organs.
The doctor justifies the examination result based on the information he received about the established tissue density, based on the results of analyzing the resulting tissue image using ultrasound technology:
- isoechoicity, distinguished by gray shades, and characterizes moderate (within normal limits) echogenicity of tissues;
- hypoechogenicity, distinguished by shades of black, and characterizes the echogenicity of tissues below the normative value;
- hyperechogenicity, stands out in white and characterizes the pathologically high echogenicity of the tissues and cavity being examined.
Thus, a doctor can detect increased echogenicity based on ultrasound, i.e. heterogeneity of the structure of the tissues of the uterine cavity, or neoplasms are detected in its walls.
Moderate echo density of the uterine walls is considered healthy, which is stable and not subject to any changes over time (with repeated examination).
When performing an ultrasound, it is important to provide the doctor with reliable information about the timing of the menstrual cycle, because in the second phase, thickening of the uterine tissue can be considered normal. Women also need to be careful during menopause, because... During this period, natural changes due to physiology may be observed. Increased echo density is not always a pathology. Therefore, it is so important to regularly consult a gynecologist to monitor your health.
If, based on the results of an ultrasound examination, a high level of echogenicity of the tissues and cavity is established, the doctor will prescribe additional diagnostic procedures and the necessary tests to determine the cause of the pathological changes, and, of course, select a treatment appropriate to the severity of the disease.
Myometrium during pregnancy
Heterogeneous myometrium is often detected in pregnant women during routine ultrasound and often indicates the presence of pathology. At the same time, the doctor constantly monitors the condition of the muscle layer. This is due to the fact that local thickening causes serious problems. Hyperechogenicity (the presence of abnormal seals) can lead to rupture of the uterine lining.
In this case, the doctor registers the pregnant woman and systematically examines her. Diseases that provoke such changes in the uterine layer can cause serious complications during childbirth. If fibroids grow, the course of pregnancy will be difficult.
During labor, insufficient contraction of the organ, as well as the onset of bleeding, is possible. In the absence of therapy, fibrosis often develops and scars form, leading to rupture of the birth canal.
In the first trimester, changes in the structure of the muscle tissue of the uterus can cause its excessive tone. At the same time, the risk of spontaneous miscarriage increases significantly. At a later stage, childbirth ahead of schedule cannot be ruled out.
Causes
Any deviations in echo density, be it disturbances in the cervix and walls of the uterus, its cavity, where a higher tissue density is found, is a reason for a careful study of the causes of these pathologies. The most common factors that have a negative impact on the structure of the uterus, creating heterogeneity of its density and high echogenicity, are:
- an innate genetic feature of the female body that predetermines the development of pathology;
- any surgical operation affecting the integrity of the uterus (including abortion, caesarean section);
- hormonal disorders;
- gynecological diseases of the female reproductive system.
Consequences of the development of pathology and its treatment
Pathological changes, expressed in high echogenicity of tissues and the uterine cavity, most often accompany the development of the following diseases:
- Neoplasms in the walls of the uterus (polyps, fibroids, or tumors, including malignant ones) are clearly visible during ultrasound as foci of high echogenicity. The disease requires treatment based on the danger to life and health. In the case of benign neoplasms, it is subject to observation by a doctor and surgical removal if necessary. In a situation where a malignant tumor is diagnosed, the patient undergoes treatment under the supervision of a doctor, in accordance with the necessary therapy.
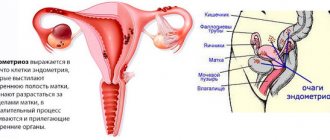
- Endometriosis also provokes the development of a heterogeneous tissue structure, and manifests itself in the high echogenicity of the uterus, its walls and cavity, which is clearly visible during diagnostics using ultrasound. Endometriosis is a disorder of the growth of endometrial tissue, which, contrary to its purpose, begins to grow into the walls of the uterus.
Treatment of myometrial changes
The treatment regimen for diffuse changes in muscle tissue largely depends on the severity of the disease, the woman’s age and the presence of concomitant pathologies. Both surgical and medical methods can be used.
The main goals of therapy include the following:
- preventing the development of complications;
- suppression of the process of estrogen production in order to prevent further development of pathology;
- preservation of reproductive function;
- preventing cells from degenerating into cancer;
- elimination of accompanying symptoms.
Drugs in various forms are used in the treatment process. These can be topical agents that are inserted into the vagina, or tablets. They should be used only as prescribed by a doctor.
Hormonal therapy of myometrium of heterogeneous structure is carried out in courses. Taking the drugs begins after menstruation and continues for three weeks, then take a break for seven days and continue treatment. The following groups of medications are used:
- estrogen-progestogen contraceptives (Diane-35, Non-Ovlon, Demoulen, Yarina or Jess). With their help, the process of ovulation and the production of estrogen are suppressed. The drugs are effective in the initial stages of the disease;
- progestin agents (Norkolut, Visanne or Utrozhestan). Medicines in this group are prescribed for varying degrees of tissue damage;
- gonadotropin releasing hormone agonists (Danogen, Danol or Nemestran).
Hormonal therapy has a pronounced effect. When combined with surgery, the risk of relapse is minimized.
Surgical treatment involves removal of lesions. The following methods can be used:
- laparoscopy;
- laser vaporization;
- cryodestruction.
After surgery, the body needs time to recover. After a few months, successful fertilization is possible.
The concept of echogenicity
Ultrasound diagnostics is based on the ability of ultrasound to be reflected from internal organs. The sensor picks up the reflected waves and transmits them to the computer. The doctor sees on the screen an image of the internal organs in the form of black, dark gray and white spots.
The procedure is absolutely safe for the human body. Diagnosis is carried out on newborn children and pregnant women without restrictions.
To obtain reliable results, the examination must be carried out correctly. Before an abdominal ultrasound, it is recommended to follow a special diet for three days. For severe constipation or flatulence, laxatives and carminatives are prescribed.
No special training is required to examine other organs. To perform an ultrasound, a sound-conducting gel is applied to the skin. This reduces the likelihood of errors.
To decipher the examination results, there are echographic signs:
- size;
- contours;
- structure;
- pathological inclusions.
Differences between normal and altered organ structure are determined using echogenicity. This concept refers to the degree of reflection of ultrasound from organs of different densities.
Main criteria
There are three main types of echostructure of organs.
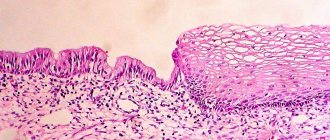
- Isoechoic. This type is the standard norm. Healthy organs have an isoechoic structure. In the photo they are presented in gray with a distinct graininess.
- Hypoechoic. Such tissues have low density and do not reflect ultrasound well; it almost does not return back to the sensor. A dark gray spot appears on the screen, with almost no grain.
- Hyperechoic. The tissues are very dense, ultrasound is reflected quickly from them. Light, almost white spots are visible on the screen. Their graininess is enhanced.
Anechoic structures also exist. They absorb ultrasound completely. Only a black spot is visible in the photo. Sometimes mixed echogenicity occurs - it is represented by hypoechoic and hyperechoic structures.
Each echogenic formation has parameters to determine its nature.
- Form. Formations can be round or irregular in shape.
- Contours. There are clear and vague.
- Structure. It can be homogeneous or heterogeneous.
The formations may be dense or have a cavity. In the latter case, they are called cysts. The cavity contains air or liquid. Cysts are unilocular when they contain one cavity. If there are several of them, the formation is called multi-chamber.
Heterogeneous myometrium
The female reproductive organ consists of several layers. The middle muscle layer - the myometrium - is penetrated by many nerve fibers and vessels. It is responsible for proper contraction of the uterus and plays an important role in the process of labor and menstruation.
Homogeneous and heterogeneous myometrium
In a healthy patient, an ultrasound examination reveals a homogeneous myometrium with an echogenic structure. The layers that make up this area do not have clear demarcation and diffuse inclusions. Closer to the isthmus and fundus of the uterus, the myometrium is thicker than in other zones.
Heterogeneous myometrium found in a woman indicates serious health problems. An accurate diagnosis can be made after a detailed examination. Ultrasound may show hyperechoic inclusions in the muscle layer, its unevenness, neoplasms or diffuse changes. With such a picture, a woman requires a mandatory consultation with a gynecologist.
One of the serious symptoms and consequences of changes in the structure of the myometrium is infertility, therefore it is important in the initial stages of the disease to prevent further pathological transformation of the muscle layer.
Reasons for the heterogeneous structure
Heterogeneous myometrium often appears due to adenomyosis and fibroids. Such diseases are of hormonal origin, and are also associated with heredity and disorders of intrauterine development.
Abortions and curettage, both for diagnostic and therapeutic purposes, lead to diffuse transformations in the structure of the myometrium due to a sharp hormonal surge or injury. Changes also occur during pregnancy and subsequent childbirth due to overextension, compression, and the appearance of hypertonicity.
Myometrial heterogeneity is diagnosed in a woman with frequent inflammatory diseases and chronic pathologies acquired through sexual contact. This means that there is an infectious cause for the appearance of diffuse changes in the layers of the uterus. Hormonal disorders and endocrine factors also affect the condition of the myometrium.
Causes of pathological formations
Average echogenicity, or isoechoicity, is considered normal. Bones and cartilage have increased echogenicity. Reduced echogenicity is characteristic of follicles in the ovary. The remaining cases are pathological.
Hyperechoic
An echo-positive formation, that is, with increased echogenicity, has a density close to bones. Tumors and scar tissue growths meet these criteria.
- Increased echogenicity occurs in the liver with cirrhosis. Normally, it has an isoechoic structure, but cirrhosis is the replacement of healthy tissue with scar tissue, which reflects ultrasound more strongly.
- High echogenicity is characteristic of some malignant tumors. They affect the liver and kidneys, less often the pancreas.
- Hyperechoic round formations in the gallbladder or kidneys are stones. They are formed due to the accumulation of bile or salts.
- If the echogenicity is moderately increased in the uterine wall, this is a sign of fibroids. A benign tumor formed by muscles grows slowly.
Hyperechoic neoplasms have clear contours and are usually oval in shape. The color in the photo depends on the density. The denser the tumor, the lighter it looks.
The concept of echogenicity of the uterus
The echogenicity of an organ, in particular the uterus, is the main criterion by which the structure is judged and various deviations from the norm are identified. This is not difficult to understand: echo refers to the reflection of sound, and echogenicity refers to the ability to reflect it.
When scanning, ultra-high-frequency sound waves - ultrasound - are sent to the organ, then the sensor captures the returned waves reflected from the organ. They are transmitted to the device’s analyzer, processed by special programs, and transformed into an image on the screen.
The degree of wave reflection depends on the density of the tissue. The denser the organ, the less it absorbs waves and the more it reflects. More waves are received by the device, the organ on the screen has a light color, even white, the image is called echo-positive. And vice versa, hollow organs containing liquid almost completely conduct (absorb) ultrasound, without reflecting waves, little of them enters the sensor, and a dark, even black, image appears on the screen - echo-negative.
The uterus is an echo-positive organ; its ability to reflect normally has a certain level. When increased echogenicity is detected, this is due to the formation of a compaction in the uterine tissue. It can be diffuse or focal for one reason or another.
Prevention
In order to prevent diffuse changes in the myometrium and the development of pathologies that provoke this process, you need to systematically undergo an examination by a gynecologist and conduct an ultrasound examination every six months. This is especially true for teenage girls and women who have undergone surgery on the genitourinary system. In addition, you need to follow the rules of hygiene and wash your intimate areas twice a day.
If suspicious symptoms appear, you should immediately contact a gynecologist. Diseases detected in a timely manner are much easier to treat.
The diffusely heterogeneous structure of the muscular layer of the uterus indicates the onset of a pathological process that needs to be eliminated as quickly as possible. Such changes can only be detected during ultrasound examination. Immediately after this, a course of therapy is prescribed.
The myometrium of the uterus is its muscular middle layer, lined from the inside with endometrium.
The structure of the uterine myometrium is a complex plexus of myocyte bundles, within which spasmodic contractions occur. Normally, the structure of the myometrium is homogeneous, the state is almost relaxed. However, for a number of different reasons, sometimes there is a multiple increase in spasms in the middle layer - hypertonicity of the uterus.
Changes in the myometrium directly depend on the current day in the women's menstrual calendar. On bleeding days, the highest frequency of spasms of the inner layer of the uterus is observed, which then sharply subsides and slowly increases until the onset of a new menstruation.
On the 7-8th day of the monthly female cycle, the approximate thickness of the myometrial layer is 1.5 mm, and before the onset of menstruation it reaches 1.5 cm.
What does the myometrium consist of?
- The longitudinal layer consists of circular and longitudinal muscles and is associated with perimetry;
- The middle one includes the vascular network;
- The submucosal layer of the uterine myometrium includes fragile and thin longitudinal tissues.
What is increased echogenicity of the endometrium?
The wall of the uterus consists of 3 layers:
- external - perimetry , covering the body and consisting of connective tissue;
- middle - myometrium , consisting of several layers of smooth muscle;
- internal - endometrium , lining the inside of the uterine cavity.
It is the endometrium that is an indicator of the state of the female hormonal and reproductive system. It consists of 2 layers: superficial epithelial, containing many glands, and deep basal, consisting of connective tissue bordering muscles. The epithelial glandular layer is also called functional; it constantly changes its thickness and density depending on the level of hormones, and is also influenced by the inflammatory process and tumors.
Normally, in women of reproductive age, the endometrium undergoes the following cyclic changes according to the results of M-echo (determining the thickness of the uterine wall):
- immediately after menstruation, its thickness is 2-5 mm, echogenicity is reduced;
- by the middle of the cycle, by the period of ovulation, it reaches 9-13 mm, echogenic properties increase, approaching the average level;
- in the 2nd half of the cycle after ovulation, the endometrium thickens to 12-20 mm, echogenicity is increased, reaching a maximum at 19-23 days (with a 28-day cycle);
- on the eve of menstruation, the thickness of the layer begins to decrease to 12-16 mm, and the density of the echostructure decreases.
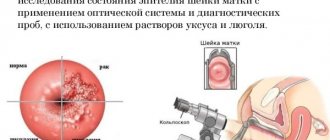
Therefore, in order to give an objective assessment of the endometrium and identify pathology, ultrasound is prescribed in the first phase of the cycle immediately after the end of menstruation, but no later than 7 days from its beginning, when the process of its thickening and compaction has not yet begun. Increased echogenicity during this period may indicate the presence of endometritis - inflammation, endometriosis - proliferation of glandular epithelium, neoplasms - polyps, cysts, adenomas, fibroids, cancer.
Also, the mucous layer of the uterus thickens to 20-22 mm and becomes denser during pregnancy, and only 6 weeks after birth returns to its original level. With the loss of a woman’s reproductive abilities, it thins to 2-5 mm, becomes denser due to atrophy of the mucous layer and its replacement with connective tissue, and after 5 years from the onset of menopause it may not be visualized at all.
Echogenicity of individual organs on ultrasound
When performing the procedure, the ultrasound diagnostician evaluates the size of the organ, its contours, homogeneity and, necessarily, the degree of echogenicity, which can indicate the presence of various pathological processes in the object under study.
Changes in the structure of the pancreas
Normally, the pancreas is located in the projection of the epigastric region and has the following echo signs.
- The echogenicity of the pancreatic parenchyma is comparable to that of the liver and is designated as average. With age, the gland undergoes changes, and the parenchyma becomes more dense.
- Usually the organ is presented in a “dumbbell-shaped” or “sausage-shaped” shape (due to the fact that the gland consists of a head, body and tail).
- The contours are clear and even, well demarcated from surrounding tissues and structures.
- The echostructure is homogeneous and fine-grained (other options are possible: homogeneous or coarse-grained).
- The Wirsung duct looks like an elongated anechoic cord, the diameter of which normally ranges from 1.6 to 2.6 mm.
We can say that the echogenicity of the pancreas is increased when its color on the device screen has a whiter tint and is in brighter ranges than the color of the liver tissue.
Common causes of hyperechogenicity are listed below.
- Interstitial edema of glandular tissue as a result of acute reactive pancreatitis. In addition to changes in density, an increase in the size of the organ is also observed.
- Increased echogenicity of the pancreas will occur with pancreatic necrosis. In this case, against the background of heterogeneous hyperechoic changes, hypo- and anechoic areas are visualized, indicating necrosis.
- Diffuse fibrosis as a result of chronic (autoimmune, alcoholic, infectious, drug) pancreatitis. The changes are based on the replacement of normal organ tissue with connective tissue.
- The echogenicity of the pancreas will be significantly increased with lipomatosis (fatty infiltration of the organ). The gland has blurred contours and a fairly light or even white tint compared to other formations.
- Diabetes mellitus, in which more than 90% of the organ tissue is destroyed.
A gastroenterologist makes a diagnosis not only based on ultrasound data, but also during a subjective examination; an ultrasound scan of the stomach is also indicated.
Echostructure of the uterus and its changes
Normally, the uterus undergoes monthly cyclic changes under the influence of pituitary and ovarian hormones. As a result of this, she has different indicators on ultrasound, correlating with the phase of the menstrual cycle.
The organ is pear-shaped, and in women who have given birth it tends to be round. Normal myometrium is characterized by average echogenicity, which is comparable to that of a healthy liver and pancreas.
The endometrium undergoes pronounced functional changes.
- On the 5-7th day of the cycle it has a lower echogenicity and a homogeneous structure. In the center of the uterus, a thin line with a hyperechoic signal is visualized, which represents the junction of the posterior and anterior layers of the inner membrane.
- By the 8-10th day, the echostructure of the endometrium practically does not change, only some thickening is noted.
- On days 11-14, its density increases, which corresponds to average echogenicity.
- Until the 15th-18th day, the density of the shell increases slowly.
- On days 19-23, the endometrium can be characterized as hyperechoic, making the central line almost invisible.
- By the end of the period, the internal lining of the uterus has a hyperechoic and heterogeneous structure.
The most common causes of increased echogenicity of the uterus are: inflammation, fibroids, polyps, endometriosis and malignant neoplastic process. The endometrium becomes hyperechoic on certain days of the cycle, as well as as a result of inflammation, the appearance of a malignant neoplasm or adenomyosis in it, or during pregnancy (hypertrophy of the functional layer and glands occurs).
Changes in the ovaries
This paired organ is located in the pelvic cavity and communicates with the uterus through the fallopian tubes. Similar to the endometrium, the ovaries also undergo a large number of changes associated with the menstrual cycle.
Normally, they have an ovoid shape, a tuberous outline due to growing follicles, and a hypoechoic structure with anechoic round inclusions along the periphery.
The echogenicity of the ovaries often increases with diffuse sclerosis (as in Stein-Leventhal syndrome), prolonged and sluggish inflammation, as well as with their malignant degeneration.
Useful video
One of the reasons when the echostructure of the uterus changes is voiced by specialists in this video.
The structure of the uterus may have the following deviations from the norm:
- heterogeneity, when areas of varying density are identified, the cause may be an inflammatory process, the presence of myomatous nodes, endometriosis, or tumors;
- hypoechogenicity - a decrease in density, characteristic of fibroids, adenomyosis, in which completely anechoic cavities-bubbles of black color can be detected;
- hyperechogenicity - an increase in echo density when the image of the uterus is colored from light gray to white.
Both a decrease and an increase in the density of an organ can be either focal in nature in the form of one or several individual light areas, or diffuse, when there are multiple light inclusions throughout the entire wall of the organ.
Concept of myometrium
The myometrium is the muscular layer of the uterus. Its structure is studied mainly during reproductive age. During menopause, less attention is paid to the myometrium, but its condition is necessarily indicated in the ultrasound examination protocol.
The uterus is a muscular organ that includes several layers. The myometrium is located between two: the endometrium and the perimeter.
The muscular layer of the uterus has a complex structure. It includes several structures:
- longitudinal outer layer, which is also called subserosal (tightly connected to the perimeter, represents circular and longitudinal muscle fibers);
- a circular middle layer called the vascular layer (represents a circular framework of muscles with numerous inclusions of blood vessels);
- longitudinal inner layer, called submucosal (looks like a thin layer with longitudinal fibers).
The vascular or middle layer of the uterine myometrium is the most powerful. The condition of the reproductive organ is mostly regulated by this area. Thanks to the unique structure of the layers of the uterus, the possibility of contractile function is created, which is important for performing reproductive tasks.
Causes of increased echogenicity of the uterus
If the M-echo shows increased echogenicity of the endometrium in the middle and in the 2nd half of the menstrual cycle, as well as during pregnancy, then there is no need to worry, this is its normal state in response to an increase in the production of sex hormones. Compaction also occurs at the beginning of menopause against the background of a decrease in hormonal function, when the endometrium atrophies and is replaced by fibrous tissue.
In all other cases, compaction of the uterus can be caused by the following diseases:
- inflammation (endometritis, myometritis, parametritis);
- adhesions, scar changes after operations;
- hormonal disorders;
- ovarian tumors with increased hormone production;
- adenomyosis (endometriosis);
- neoplasms - polyps, myomatous and fibromatous nodes, uterine cancer;
- intrauterine foreign bodies (spirals);
- frequent curettage of the uterine cavity (abortion);
- complications after childbirth - retained placenta in the uterine cavity, postpartum endometritis;
- the presence of calcifications (deposits of calcium salts) in the uterus after inflammation or surgery.
Changes in the uterus with adenomyosis
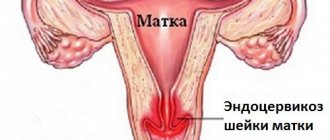
Adenomyosis or endometriosis is a common disease that occurs in women of all ages and is characterized by damage to the muscular and serous lining of the uterine walls. Endometrial cells grow into the thickness of the uterus and form peculiar passages, which is determined by ultrasound as a cellular structure.
There are diffuse and local forms of the disease. In the diffuse form, the uterus acquires a spherical shape and has the same size as at 5-9 weeks of pregnancy. Moreover, during and before menstruation, the uterus enlarges. The structure of the myometrium may look normal on ultrasound, but this does not mean that there are no changes, just small inclusions characteristic of endometriosis are not visible. In the presence of linear or point inclusions, an inhomogeneous heterogeneous structure is observed.
An important parameter in the ultrasound diagnosis of uterine diseases is echogenicity. Normally it is low. Its increase indicates the presence of pathological foci. With endometriosis, hyperechoic inclusions are determined in the myometrium, which range in size from 1 to 5 mm and are located diffusely in the thickness of the uterus.
The border between the endometrium and myometrium is tortuous, and the thickness of the myometrium of the posterior wall of the uterus is greater than the anterior one. A decrease in echogenicity occurs before menstruation due to vasodilation or tissue swelling. If an inflammatory process occurs, the average echogenicity is determined during diagnosis. Main symptoms of the disease:
- Long and heavy menstruation
- Bloody discharge of varying intensity, not associated with menstruation
- Painful pulling and aching sensations in the lower abdomen
- Menstrual irregularities.
The causes of adenomyosis can be frequent stress, complicated abortions and childbirth, constant sun exposure (occurs in women who visit solariums). Adenomyosis is dangerous for the development of infertility, especially for severe cases of the disease. The fact is that with endometriosis, adhesions often form, which interferes with the implantation of a fertilized egg. Many women who have suffered from this disease are forced to resort to in vitro fertilization (IVF).
If an ultrasound reveals heterogeneous variegated myometrium, this means that the woman suffered an inflammatory disease of the uterus and developed endometriosis. There are two types of treatment for this disease: hormone therapy and surgery. Hormonal drugs are toxic and somewhat dangerous, and they are not highly effective for endometriosis. The operation is justified only in the event of external endometriosis - extragenital. Endometriotic tissue is cauterized using special devices. Herbal preparations are used to restore hormonal levels and improve the body's immune defense, as well as prevent inflammatory diseases.
How does the myometrium change with uterine fibroids and inflammatory diseases?
More information about uterine fibroids is described in this video:
Fibroids are a benign tumor that is found in 20% of women over the age of 35. This disease is characterized by an enlarged uterus. Most often, the nodes are located in the body of the uterus. The main localizations of myomatous nodes: submucosal (submucosal), interstitial, subserous. There may also be intermediate types: interstitiosubmucous and interstitiosubserosal. The echostructure of the myometrium changes; the myomatous node itself is detected on ultrasound as an oval or round formation with clear boundaries. If there are many vessels in the node and muscle tissue predominates, it will be hypoechoic.
Also, with fibroids, calcification of the myometrium, or rather myomatous nodes, can occur. A more accurate diagnosis of uterine fibroids is possible using intrauterine ultrasound; now this method has not yet become widespread. Diagnosis is carried out with special sensors on the expanded uterine cavity. This method provides objective information about the size of the intramural part of the submucous node even before surgery. At the moment, three-dimensional echography is used in gynecology, which is more informative than conventional ultrasound.
Endometrial hyperplasia is a benign growth of the uterine lining. In this case, the endometrium has a thickness of more than 16 mm, and it itself is homogeneous or heterogeneous.
Myometritis is an inflammation of the myometrium, often developing as a result of an infectious lesion of the uterine mucosa. Clinical manifestations are very similar to those of endometriosis, so ultrasound is used for accurate diagnosis. In the uterus, signs of inflammation are detected, an increase in the thickness of the endometrium and the size of the uterus; fluid can be detected in the cavity.
If an ultrasound shows adhesions in the uterine cavity, a diagnosis of chronic myometritis is made. Myometritis and endomyometritis are often asymptomatic, so early diagnosis can be difficult. Very often, this disease is detected accidentally during a general examination, pregnancy or infertility. Untreated endometritis is dangerous for the development of complications and the formation of adhesions. If you have been diagnosed with this, do not refuse treatment. According to statistics, it is known that this disease is one of the main causes of infertility.
Diffuse changes in the myometrium are not a separate disease, but only a symptom of a primary pathology. Symptoms, in turn, will differ depending on the underlying cause.