Panaritium is an infectious inflammation of the soft tissues of the fingers and toes. This is a very common and dangerous disease. It occurs as a result of a purulent process that can occur even after a minor injury if an infection gets into the wound.
Panaritium is a complex pathology. Depending on the severity of the process, its treatment lasts from two weeks to several months.
This disease cannot be properly cured at home. In the absence of qualified medical care, the inflammation will continue to progress rapidly and affect the tissues of the hand. And this is fraught with the development of gangrene, phlegmon of the forearm, osteomyelitis and severe deformities of the fingers. Abscesses that are not treated in time often recur.
How does panaritium occur?
To start the pathological process, a tiny wound on the finger is enough - for example, from an injection or splinter.
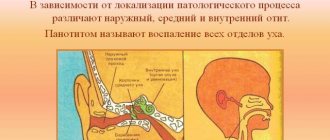
Small wounds heal quickly, but the infection remains inside and continues to multiply. In this case, the human body recognizes the danger and begins to produce phagocytes (leukocytes). The structure of the connective tissue of the hands is specific - it forms vertical fascial partitions. They go from the periosteum to the skin, dividing into vertical cells. This keeps the infection from spreading to other areas, but creates ideal conditions for an abscess to form.
When swelling occurs in such partitions and pressure in the tissues increases, debilitating pain appears. If panaritium is not treated, the infection breaks into neighboring cells, spreading to the joints and tendons.
Complications
Subungual panaritium requires surgical treatment and concomitant medicinal and supportive local therapy. The absence of necessary therapeutic measures can lead to the development of the following forms of complications:
- paronychia - purulent inflammation of the skin tissue of the nail fold;
- the spread of pus into the deep tissues causes other forms of the disease - subcutaneous, bone, articular panaritium;
- pandactylitis is a purulent inflammation of all tissues of the fingers, which, if left untreated, can spread to other fingers and further, to the wrist, palm, hand and forearm;
- transition from the acute stage of the disease to the chronic stage.
Types of felon
Panaritium on the fingers is more common than on the feet. It can develop in a person of any age, both men and women. However, most often the disease affects patients 20-50 years old. In children, severe forms of panaritium are rarely diagnosed; in them, only the periungual fold (paronychia) is usually inflamed.
Classification of panaritiums:
- Periungual form or paronychia. The painful process engulfs the edge of the nail plate and moves to the periungual fold. The reason for the occurrence of such panaritium is microtrauma of the tissues adjacent to the nail, almost imperceptible cuts - for example, as a result of an unprofessional manicure.
- Subcutaneous panaritium. Suppuration forms on the reverse side of the injury; exudate accumulates in the subcutaneous purulent bladder, often with bloody impurities. It is noteworthy that such an abscess does not hurt; a person may only be bothered by a slight burning sensation. The skin around the felon turns red. If the subcutaneous bladder increases in volume, this means that the disease is progressing. It is this form of the disease that is easier to treat than others. But due to the structure of soft tissues, inflammation quickly spreads to the joints and tendons.
- Subungual panaritium. The source of inflammation is located under the nail plate, in the soft tissues. The infection can be caused by a nail injury or splinter.
- Bone panaritium. In this case, the bone tissue of the finger becomes inflamed. Such inflammation can occur after deep injuries and fractures.
- Articular form or purulent arthritis. The joint between the phalanges is affected, the fingers acquire a spindle-shaped shape and any movement becomes painful.
- Combined articular-osseous form. Inflammation affects not only the joint, but also the bone.
- Tendon form. The most difficult and painful type of panaritium. In addition to the bone and joint, the inflammation spreads to the tendons, the affected area swells and, due to severe pain, it becomes almost impossible to move the fingers and limbs.
Attention! Identifying subcutaneous panaritium is especially difficult in people with thick, insensitive skin. The first signs of inflammation begin to appear 5-7 days after the injury, when a person hardly pays attention to the first unpleasant sensations. Without treatment, inflammation affects the tendons, joints and phalanges, leading to a complicated form of the disease.
Classification
Surgeons use several classifications of felon species. Classification of felon according to localization and depth of damage identifies the following types of felon:
- Superficial (uncomplicated) forms:
- cutaneous (or intradermal) panaritium;
- subcutaneous panaritium;
- nail felon, which is divided into subungual and periungual (or paronychia);
- Deep (complicated) forms:
- bone panaritium;
- articular panaritium;
- tendon panaritium (or tenosynovitis);
- pandactylitis (damage to all types of tissues and structures of the finger).
Classification of panaritium according to the flow distinguishes 2 stages of the process: serous and purulent-necrotic. Any type of panaritium can develop on the fingers of both the upper and lower extremities.
Symptoms of felon
How the disease will progress depends on the pathogen, the type of inflammation and the nature of tissue damage. However, different types of panaritium still have common features. These include:
- swelling of the fingers on the back of the hand;
- redness and feeling of skin tension;
- limited movement, awkwardness, stiffness;
- discomfort or pain: from tingling to sharp pulsations (depending on the depth of the lesion).
In severe cases of panaritium, the patient will suffer from high fever, intoxication, and weakness.
If the causative agent of inflammation is staphylococcus, there may not be a clear clinical picture with pain and fever. This is the danger of such felon: in the presence of staphylococcus, decay processes develop very quickly and a necrotic focus develops. Therefore, be careful - severe swelling of the hand, accompanied by weakness, drowsiness and lack of appetite, may indicate the destructive activity of staphylococcus. See a doctor immediately!
If anaerobic flora is working inside the panaritium, the hand will not only be swollen, but also purple or even cyanotic. With this type of lesion, tissue necrosis also develops very quickly.
Symptoms
Photo of felon on a child’s finger
The development of any type of felon most often begins in an acute form.
The following symptoms appear:
- In the place where the inflammatory process is localized, throbbing pain and twitching are felt.
- The skin at the site of inflammation turns red, swelling and swelling appear.
- The temperature of the skin increases at the site of the abscess.
- Pus is visible through the outer skin (with superficial panaritium).
- The patient may have an increase in body temperature, a feeling of aching, chills and weakness, and a headache.
- Restrictions appear in the motor ability of the finger, its sensitivity may become dull.
- The pain syndrome when deep panaritium occurs manifests itself in an increasing form. After a day, the pain can become unbearable, preventing you from falling asleep or even resting for a short time. The patient's ability to work is lost.
Diagnostic measures for identifying panaritium are not complicated. Surface forms are determined by external examination. If deep panaritium develops, an x-ray is performed. The presence of inflammation is confirmed by a general blood test.
With any form of development of the disease, severe consequences for the body are possible. Pyogenic microbes can travel from the inflammatory focus to distant organs.
Moreover, their defeat is accompanied by general blood poisoning. In this regard, consulting a doctor is the most correct decision in case of felon formation.
In case of refusal of treatment (they say, the abscess will break out on its own) or improper implementation, in addition to blood poisoning, the following consequences are possible:
- The inflammatory process can spread not only to soft tissues, but also to lymphatic (lymphadenitis is diagnosed) and blood vessels.
- Loss of finger functionality due to necrosis of both ligaments and tendons.
- Inflammation of bone tissue may result in bone destruction (osteomyelitis).
- Inflammation can affect all tissues of one or more phalanges of the finger (pandactylitis). In this case, amputation is often used to avoid the spread of the process to neighboring tissues.
Stages of the disease
The initial stage of the disease is called serous-infiltrative. 2-3 days after the onset of the lesion, it passes into the purulent-necrotic stage.
The serous-infiltrative stage is characterized by:
- moderate pain;
- exacerbation of unpleasant sensations when the hand is lowered down;
- redness on the back of the hand;
- swelling of fingers and hands;
- the affected finger is difficult to bend;
- body temperature fluctuates between 37-37.5 degrees;
- satisfactory health.
When the disease enters the purulent-necrotic stage, the symptoms are pronounced:
- throbbing or jerking pain in the affected finger;
- the patient is forced to keep the hand raised upward;
- paler spots are visible in the center of the reddened areas of the skin;
- the veins of the hand are dilated;
- fever, general intoxication;
- The blood test shows a high ESR and an increased number of leukocytes.
Principles of treating a disease on the big toe or hand at home
If the first signs of purulent exudate appear on a swollen finger, you need to consult a surgeon.
The initial stage of felon under the nail is treated with the following methods:
- Medication.
- People's
- Physiotherapeutic.
Provided that conservative treatment did not affect the inflammatory process or stop it, then they resort to surgical treatment in a hospital.
What not to do
This infection is unpredictable.
Any error in treatment can lead to a worsening of the condition. Therefore you cannot:
- self-medicate;
- allow unsanitary conditions;
- open the suppuration yourself;
- take thermal procedures in the presence of pus.
In case of severe pain, when pus appears, you can apply cold. This will ease the pain a little. Next, it is imperative to seek help from a surgeon.
Risk factors
The inflammatory process occurs when pathogenic microorganisms enter the wound. They may be:
- Staphylococcus aureus;
- beta-hemolytic streptococcus;
- enterococcus;
- Escherichia coli or Pseudomonas aeruginosa;
- fungal infection.
Often the cause of inflammation is a combination of several types of aerobic and anaerobic microorganisms.
People can open the gates of infection due to carelessness or bad habits. For example, microtrauma can be caused by the habit of biting nails or picking off hangnails, or getting a manicure done by an insufficiently conscientious specialist.
Factors in which you need to be extremely careful and protect your fingers from microtraumas:
- fungal infection:
- dermatosis complicated by bacterial and fungal microflora;
- nail damage due to psoriasis or eczema;
- diabetes mellitus (especially its decompensated form);
- damage to arteries and veins - it leads to disruption of blood microcirculation and disruption of tissue trophism;
- taking immunosuppressants or glucocorticoids;
- old age, vitamin deficiencies, exhaustion. hypoproteinemia;
- frequent contact with caustic chemicals;
- frequent exposure to high humidity conditions;
- work involves exposure to vibration;
- Raynaud's syndrome.
How long to treat
Any remedy for treating felon at home acts at a certain speed. For some, a few days are enough to suppress inflammation; for others, weeks are enough. The main thing in this matter is regularity.
If symptoms worsen within two days, treatment with the chosen remedy must be stopped and contact the surgical department.
There is protection from panaritium, even at home. The main thing is to be vigilant and not let everything take its course.
Diagnosis of felon
A traumatologist, orthopedist and infectious disease specialist can make a diagnosis. After examination and history collection, the doctor will prescribe:
- clinical urine analysis;
- clinical blood test;
- bacteriological culture from the affected area:
- radiography.
To clarify the shape and location of the inflammation, the doctor will carefully palpate the sore spot with a button probe.
Since articular panaritium is more difficult to identify, it may be necessary to take comparative radiographs of the finger of the same name on the right and left hands. Based on the results of the examination, the doctor will decide how to treat panaritium.
Causes of development and pathogenesis of the disease
Bone felon In the vast majority of cases, the causative agent of bone felon is staphylococcus, more rarely some other pathogen.
The infection enters the tissue through small areas of damage, such as scratches, cuts, microcracks, etc. All sorts of foreign objects contribute to the development of the inflammatory process and the spread of infection, these include glass fragments, splinters, metal filings, etc. In the area of their penetration into the tissue, infiltration (edema) and inflammation develop. Subsequently, a purulent infiltrate forms. Since the subcutaneous fatty tissue has a lobular structure and strands of connective tissue are located vertically, pus, when it melts, spreads either outward and breaks through the epithelium, or goes deeper, affecting the tendon, bone and its articular surface, thereby causing the development of one or another type of panaritium.
Inflammation in the tendon and joint can be primary and develop as a result of damage and infection. The spread of infection in this case goes through the usual stages, characteristic of the anatomical features of the structure of the hand. The most severe type of inflammation in the finger is pandactylitis; it affects all tissues of the finger. As a result of tissue compression, dry necrosis occurs, characteristic of felons.
Treatment of felon
If the patient seeks medical help in a timely manner, felon can be successfully treated using conservative treatment methods: local and systemic use of antibiotics, analgesics, UHF therapy, electrophoresis. The main thing is to ensure resorption of the infiltrate.
At this stage of treatment, additional procedures are effective: baths with saline solution or compresses on the site of inflammation, the use of ichthyol ointment or Vishnevsky ointment. Depending on the area of the lesion, you can use ointments and lotions with antibiotics, antiseptics, and applications with dimexide.
To relieve pain, you will be offered non-steroidal anti-inflammatory drugs.
If the inflammation has developed into purulent-necrotic, the painful cavity must be promptly opened, drained and washed with antiseptic solutions. During intensive treatment, a bandage and splint will be applied to the finger. Most likely, the doctor will prescribe a course of antibacterial drugs, depending on the results of a sensitivity test to one or another type of antibiotic.
Medicines for treatment
During the first few days, whitlow that appears in a superficial form on the finger can be treated conservatively at home.
In this case, ointments with antiseptics and antibiotics, as well as folk remedies, can be used.
It should be borne in mind that every day lost for treatment reduces the chances of quickly getting rid of the purulent process. This increases the likelihood of needing surgical intervention.
In many cases, when panaritium is detected, people immediately begin to use antibiotics.
However, this approach is incorrect, since antibacterial drugs are potent drugs that have certain contraindications and a number of side effects. In addition, very often panaritium occurs due to staphylococci getting under the skin.
Prevention
It is not difficult to prevent the appearance of panaritium. To do this, it is important to follow the following rules:
- wear protective gloves when working;
- observe safety precautions at work and at home;
- immediately treat any skin damage with antiseptics, including splinter injections and hangnails;
- cover injured areas with a protective plaster.
- ensure that manicure tools are sterile;
- Avoid prolonged exposure to water - it weakens the protective qualities of the skin.
Reasons for appearance
This disease usually affects people of active age, but it is also diagnosed in children (who can already walk; panaritium is a rather rare disease in an infant). The child’s immune system does not function at full capacity, so there is a risk of inflammation spreading more quickly.
The causes of panaritium are the penetration of bacteria deep into the soft tissues when the integrity of the skin is violated. This occurs as a result of wounds, cuts, bites, hypothermia and burns. This also occurs when a foreign body gets under the skin.
Purulent inflammation develops as a result of exposure to bacteria from the groups of staphylococci and streptococci. Enterococci and Pseudomonas aeruginosa may be involved in the pathogenesis. Less commonly, herpetic panaritium develops. As the name suggests, the cause is the herpes virus.
The presence of certain concomitant diseases that increase predisposition to this pathology is important. They are as follows:
- endocrine disorders (diabetes mellitus);
- atherosclerosis and obliterating endarteritis of the vessels of the lower extremities;
- various immunodeficiencies;
- frequent hypothermia;
- prolonged exposure to certain physical factors (for example, vibration).
Diagnostics
The diagnosis of bony panaritium of the thumb is made on the basis of the patient’s complaints, anamnestic details, examination data, and, if necessary, the results of additional examination methods. In the secondary form, the medical history often reveals that the patient suffered from another form of panaritium for 10-14 days.
On physical examination the following is noted:
- upon examination, with fairly rapid progression of the pathology, the finger is in a half-bent position, deformed, if the terminal phalanx is affected, it looks like a club, the skin covering the affected phalanx is bluish, smooth and shiny. When pus breaks through, a hole with pus flowing from there is visualized;
- upon palpation (palpation) - tension in the tissues of the finger, swelling, and sharp pain are noted.
Instrumental examination methods that can be used in the diagnosis of bone panaritium of the thumb are as follows:
- probing - a probe is carefully inserted into the purulent tract formed when the abscess breaks through, and with its help, the corroded surface of the bone is “groped”;
- X-ray of the finger – the X-ray image shows destruction of bone tissue. If a joint is involved in the pathological process, this appears on the image as unevenness of the articular surfaces.
Laboratory examination methods that are informative in the diagnosis of the disease described are:
general blood test - there is a pronounced increasing increase in the number of leukocytes (leukocytosis) and ESR;
- bacterioscopic examination - purulent discharge is examined under a microscope and the pathogen is identified;
- bacteriological examination - the purulent discharge is inoculated onto nutrient media, and the pathogen that provoked the development of bone panaritium is determined from the colonies. The method is also used to determine the sensitivity of pathogens to antibiotics.
Use of medicinal plants
Medicinal plants - aloe, calendula, celandine - will help to successfully combat hand felon. They have long been used to treat many diseases, including purulent formations.
Every person probably has agave in their home, but not everyone knows and uses its healing properties. For treatment, you need to take a 3-year-old plant and select the fleshiest leaf. Cut a piece, remove the peel, apply the pulp to the sore spot and attach with a bandage. To speed up the anti-inflammatory effect of agave, the pulp must be slightly crushed until juice is formed.
Celandine is used to prepare a medicinal bath. Need 1 tsp. dry herbs, pour 500 ml of water, bring to a boil and keep on low heat for 10-15 minutes. As soon as the broth has cooled to a temperature of 70˚C, you can dip your sore finger into it and hold it for about 15 minutes. Exceeding the recommended temperature may result in burns. The bath should be done at least 2 times a day.
Calendula has a good anti-inflammatory effect. It is used in the form of an alcohol solution to be added to the bath. When steaming your finger, it penetrates perfectly deep into the skin and under the nail plate. It has a healing effect not only in cases of subcutaneous panaritium of the hands, but also in its subungual form.
What clinical signs are characterized by bone panaritium?
Bone panaritium of the terminal phalanx. There are two stages of inflammation:
- Serous-infiltrative (initial);
- Purulent-necrotic (purulent).
The clinic of purulent-inflammatory processes in the hand, like any other inflammation, is characterized by the presence of symptoms such as redness (hyperemia), local increase in tissue temperature, pain in the affected area, swelling and dysfunction of the hand. However, this inflammation also has individual symptoms.
When the process is localized in the forearm or shoulder, lower leg or thigh, signs of an inflammatory process in the subcutaneous fat are localized directly at the site of the greatest damage. Symptoms of pain in the hand are determined only by palpation and, due to the prevalence of edema, it is difficult to establish the exact localization of the purulent-inflammatory process, which complicates the process of diagnosis and treatment.
Bone panaritium is a secondary process that developed when a purulent-inflammatory process spreads to the bone. Most often it develops against the background of previous subcutaneous panaritium. After the subcutaneous abscess is opened, a moment of imaginary well-being sets in, the pain subsides, the swelling goes away and it seems that the inflammatory process is subsiding. In fact, recovery does not occur. The pain only dulls and becomes constant. Purulent contents are constantly separated from the wound surface, possibly with small bone sequesters. Gradually, the phalanx swells and takes on a club-shaped shape, touching it causes severe pain.
An X-ray examination at 2-3 weeks reveals signs of bone tissue destruction in the affected area. Surgical treatment should be started based on clinical symptoms, without waiting for signs of bone destruction on the image.
An equally common complication of the subcutaneous form of felon is articular felon. Most often they are affected in the area of the interphalangeal and metacarpophalangeal surfaces. The most important symptom is pain. The patient is restless, exhausted, cannot do his usual activities, the quality of his life and the ability to fully care for himself are reduced. The affected joint thickens and becomes fusiform, and when you try to bend the pain increases sharply. The skin over the affected area is hyperemic, the swelling is predominantly localized on the dorsal articular surface.
Causes
What are the reasons for the development of felon? Only two components play an important role here:
- An open wound, better when it is punctured. If a person gets burned, gets a splinter, injures the hand, an open wound forms, cracks in the skin, then an infection can easily get inside - the second reason for the development of panaritium. This often happens during physical work, when preparing food, manicure, pedicure, etc.
- Infection. Staphylococci are common, less often - streptococci, Pseudomonas aeruginosa, Proteus and other microorganisms. They penetrate into an open wound located on the hands or feet. The deeper it is, the greater the risk of developing the disease.
The most interesting thing is that not only the reasons described above become factors in the development of panaritium. There are other situations:
- Skin contamination.
- Frequent hypothermia.
- Exposure of finger skin to various metals and chemicals.
- Ingrown nail.
- Vibration.
- Diabetes.
- Foot fungus.
Blood circulation, tissue nutrition and local immunity should be disrupted in the area. When there is no immunity, then it is easier for microorganisms to penetrate the wound and begin the inflammatory process.
On the feet, panaritium develops due to uncomfortable shoes, constant friction, punctures, etc.
go to top
Pathanatomy
On the palmar surface of the fingers there are many important anatomical formations: tendons and tendon sheaths, nerves, blood vessels, joint capsules, etc. The subcutaneous tissue in this area has a special structure. Numerous elastic and strong fibers run from the skin to the palmar aponeurosis. In addition, longitudinal bundles of connective tissue are located in the thickness of the fiber. As a result, the fiber is divided into small cells, reminiscent of a honeycomb.
This structure, on the one hand, prevents the spread of inflammation “along”, on the other hand, it creates favorable conditions for the penetration of the purulent process deep into the tissues. That is why with panaritium, rapid progression is possible, involving tendons, bones and joints, or even all tissues of the finger.
Paronychia
Paronychia is the most common hand infection that begins as an inflammation of the subcutaneous tissue but can quickly develop into an abscess. This disease occurs three times more often in women than in men. Patients with HIV infection and people taking glucocorticoids for a long time are predisposed to its development.
Some diseases damage the nail plate, periungual fold, cuticles and provoke the development of paronychia. These include:
- psoriasis,
- side effects of retinoids,
- drugs for the treatment of HIV infection.
There are two types of paronychia:
- Acute - a painful condition accompanied by the formation of pus caused by staphylococcus.
- Chronic – it is caused by a fungal infection.
Acute paronychia
Acute paronychia usually develops as a result of a minor injury that separates the periungual fold from the nail. Such damage includes:
- burrs,
- cuts when cutting nails,
- manicure,
- nail extensions.
Acute paronychia is characterized by the following symptoms:
- swelling and redness of the fingertip,
- accumulation of pus under the skin,
- inflammation of the skin fold at the base of the nail.
The area of inflammation and accumulation of pus may spread to the opposite nail fold through the skin at the base of the nail plate. Paronychia can develop into panaritium. As the infection progresses, damage to deep structures, tendons, bones and joints is possible.
Chronic paronychia
The cause of chronic paronychia is a fungal infection. If this disease does not respond to treatment for a long time, then it may be a manifestation of some kind of neoplasm.
This disease develops in people who work in a damp environment or come into contact with weak alkalis or acids. This category includes:
- cleaners,
- dishwashers,
- bartenders,
- florists,
- bakers,
- professional swimmers.
Chronic paronychia manifests itself:
- swelling, redness and tenderness of the periungual folds without signs of liquid pus,
- thickening and change in color of the nail plate, the appearance of pronounced transverse grooves on it,
- separation of the cuticle and ridges from the nail plate, which may predispose to infection.
Symptoms of panaritium
acute inflammatory process is always accompanied by an increase in body temperature
All types of panaritium have their own characteristics. However, they are united by common symptoms that characterize panaritium as an acute purulent inflammation.
Constant pain in the area of the finger or toe, which has a pulsating character. The skin around the painful area becomes very red. The finger itself swells or even swells. There is a limitation in the mobility of the toes or hands. A person cannot bend or straighten them due to severe pain. An acute inflammatory process is always accompanied by an increase in body temperature.
It often happens that you need to independently identify panaritium - the symptoms should be similar to those listed. But purulent inflammation is no joke. Therefore, you should not guess and self-medicate. You need to urgently go for a consultation with a doctor. A specialist will identify panaritium: the prerequisites for its occurrence, signs of manifestation and type of disease.
Causes of panaritium
- Consequences of hand skin contact with chemicals.
- Injections, cuts.
- Hangnails.
- Introduction of bacteria from the use of untreated manicure instruments.
- Impaired metabolism.
- Diseases of the endocrine system.
- Lack of vitamins.
- Decrease in the body's defenses.
- Regular hypothermia and excessive moisturizing of the skin of the hands.
- Systematic exposure to vibration.
- Maceration.
- Burns.
- Insufficient hygiene.
- Calluses.
Panaritium on the toes is possible, but in very rare cases.
Forecast
The prognosis for bone panaritium of the thumb is different - it depends on how quickly the bone tissue is drawn into the pathological process and how aggressive the pathogenic microflora is that provoked the development of this disease.
With timely removal of purulent contents and adequate antibiotic therapy, it is possible to preserve the tissue and functionality of the finger. In advanced cases, the process can be stopped, but shortening of the finger and disruption of its functions is possible.
The prognosis worsens sharply under such circumstances as:
- late visit to the clinic;
- self-medication - especially the “warming” method.
Kovtonyuk Oksana Vladimirovna, medical observer, surgeon, consultant doctor
4, total, today
( 56 votes, average: 4.45 out of 5)
Exostosis: causes, symptoms and treatment
Fibrous dysplasia: symptoms and treatment