Developed by the Soviet scientist M.I. Pevzner, the therapeutic diet table 4 helps to cope with acute intestinal diseases accompanied by diarrhea, in particular, colitis, enterocolitis, dysentery, intestinal tuberculosis, typhoid fever, food poisoning. Table 4 diet menu is prescribed by gastroenterologists during periods of exacerbation of gastrointestinal pathologies.
Varieties of diet No. 4:
- table 4a - therapeutic nutrition is intended to restore the functionality of the intestines in case of colitis with pronounced processes of putrefaction, increased gas formation and fermentation;
- Table 4b – a diet that helps the body cope with chronic colitis in the subsiding stage of exacerbation (prescribed after table No. 4a).
The 4-table diet for intestinal diseases relieves inflammation, reduces fermentation and putrefactive processes, restores the functioning of the entire gastrointestinal tract, and reduces the load on the digestive system through a gentle diet.
The essence of the diet
Diet number is aimed at eliminating chemical, thermal and mechanical irritants of the gastrointestinal tract. In addition, nutrition creates conditions for eliminating inflammatory processes during gastritis and restoring impaired functions after intestinal surgery.
The fourth table in terms of energy value hardly fits into the lower threshold of the physiological norm of calories - 1700-2000. Calorie intake is reduced by reducing carbohydrates and fats from the diet. This amount of calories is sufficient for the normal functioning of the body while the patient is in bed.
Chemical composition of the diet:
- 230-250 grams of carbohydrates (30-40 grams of sugar);
- 65-70 grams of protein (30-40% plant origin);
- 50-60 grams of fat (50 grams of butter).
The table also requires you to reduce the amount of table salt you consume to 8 grams.
With diarrhea and constipation, which are “bonuses” of intestinal diseases, the absorption function of the small intestine is reduced, so the intake of vitamins must be increased.
The recommended amount of free liquid is 1.5-2 liters.
Diet No. 4B
This type of fourth table is prescribed for the following conditions:
- chronic gastroenterocolitis in the stage of moderate exacerbation
- chronic enterocolitis in the stage of moderate exacerbation
- intestinal diseases during the period of subsidence of acute processes
The diet contains a moderate restriction of mechanical and chemical irritants of the digestive tract.
Chemical components:
- proteins - 100-120 grams
- fats - 100 grams
- carbohydrates - 400-420 grams
- sodium chloride (table salt) - from 8 to 10 grams
- free liquid volume - 1500 ml
Daily caloric intake: from 3000 to 3200 kcal
Frequency of meals: 5-6 times a day.
Read also: Diet 0: gentle gradual restoration of the body
The diet provides adequate nutrition during the period of moderate exacerbation or subsidence of exacerbation of the disease associated with digestive disorders, helps reduce inflammation and normalize the functions of the digestive organs.
What is possible, what is not
Allowed for use:
- Stale white bread and rye crackers made from wheat flour;
- Black and green tea, cocoa, herbal infusions and lightly concentrated coffee;
- Low-fat cottage cheese and milk, provided it is well tolerated;
- Slimy pureed soups made with water, possibly with the addition of meatballs, dumplings, pureed meat;
- Lean and lean meat, poultry without skin;
- Lean varieties of fish (hake, carp, pollock, perch, pike perch) steamed or boiled in water, jellied fish and lightly salted granular caviar;
- You can have 1 soft-boiled egg per day, in the form of a steam omelet, or as an ingredient in dishes, if recipes require it;
- Heat-treated vegetables;
- Fruits and berries in the form of mousses and soufflés, jellies and jelly, once a week you can have a fresh apple and then in grated form.
Table number 4 excludes all foods and dishes that contribute to diarrhea (fermentation and clay processes in the gastrointestinal tract) and disrupt the normal functioning of the intestines.
The following are prohibited:
- Rye bread and hot baked goods; pancakes, dumplings and pies are also prohibited;
- Coffee with milk, compotes, sweet carbonated drinks and alcohol;
- Soups with fatty meat and fish broths, milk and cheese soups;
- Barley, pearl barley, corn and millet cereals, all legumes;
- Fatty meats and poultry, fried in whole pieces, processed meat products in the form of sausages and semi-finished products;
- Fatty fish;
- Eggs fried in fat or lard, hard-boiled or eaten raw;
- Various dressings, spices and sauces;
- Chocolate, ice cream, sweets, jam;
- Fresh vegetables, fruits and berries.
Reviews about the therapeutic diet table 4
The use of therapeutic nutrition diet table No. 4 from Pevzner left behind very positive and positive results. Over the course of a week, there is a clear decrease in the inflammatory process on the walls of the gastrointestinal tract, and all rotting and fermentation is significantly inhibited. Depending on how a person recovers, on average, such a healthy diet lasts about 7-10 days. You need to leave this diet with extreme caution, gradually, so as not to provoke a recurrence of the disease.
Patients who adhered to the 4-table diet had positive impressions and reviews. They confirm that this therapeutic diet method significantly reduces painful symptoms, starting from the first days of use, and actually promotes a speedy recovery.
Varieties of table
Diet No. 4 for intestinal diseases, in addition to the main therapeutic nutrition, includes 3 more branches:
- Table No. 4a is observed for any intestinal diseases with pronounced fermentation processes, as well as after surgery on the gastrointestinal tract;
- Table No. 4b is used after diet No. 4. Indications for compliance are chronic colitis and enterocolitis in the phase of mild exacerbation, acute enterocolitis in remission;
- Table No. 4c is indicated after diet No. 4b for acute intestinal diseases (colitis, enterocolitis) during the improvement of health, as an intermediate diet and leading the patient to a balanced diet.
- We recommend reading: fasting day for gastritis
Basic Rules
Diet 4 for intestinal diseases is prescribed to patients during exacerbations; it is for this reason that the diet should be strictly followed.
Dishes that can be prepared from permitted products must be pureed and have a paste-like consistency. They help restore the inflamed area of the gastrointestinal tract, while not irritating the mucous membrane either mechanically, thermally, or biochemically.
In the daily diet of table No. 4, the total protein indicator does not change and does not exceed 90 grams/day; the amount of fats and carbohydrates, unlike proteins, is sharply reduced, the figure reaches 75-250 grams/day.
The norm of table salt has also been established, which should not exceed 9 grams/day, the amount of drinking water should be approximately one and a half to two liters per day. Based on this, the total calorie content of the daily diet is approximately 1955-2000 kcal.
The temperature of food consumed is recommended from 16 to 60°C. It should not be cold or very hot, but slightly warmer than room temperature. Fatty and smoked foods, as well as foods with a hard and thick consistency are strictly contraindicated for various diseases or inflammations of the gastrointestinal tract.
Menu for every day
For any intestinal diseases and after gastrointestinal surgery, nutrition is the main component of complex treatment. The diet menu is prescribed by the attending physician, but if you follow his recommendations, you can create a therapeutic diet for the week yourself.
Possible menu option for 3 days:
1 day:
- Breakfast: steamed protein omelette, natural coffee;
- Lunch: buckwheat with a piece of homemade chicken sausage;
- Lunch: pureed carrot soup with crumbled oatmeal;
- Afternoon snack: 1 soft-boiled egg, blueberry jelly;
- Dinner: fish cutlets with wheat breadcrumbs.
Day 2:
- Breakfast: manna with yogurt, herbal tea;
- Lunch: pureed cottage cheese, decoction of bird cherry fruits;
- Lunch: vegetable soup with rice;
- Afternoon snack: oatmeal broth with biscuits;
- Dinner: boiled beef with baked zucchini.
Day 3:
- Breakfast: pureed milk oatmeal;
- Lunch: baked apple;
- Lunch: vegetarian puree soup with semolina dumplings;
- Afternoon snack: cocoa with rice water;
- Dinner: curd pudding, chamomile tea.
The exact number of calories and chemical composition of the menu is allowed to be planned and adjusted only by a gastroenterologist. He is the one who knows how chronic enterocolitis will manifest itself, when to expect remission from gastritis, or what degree of health the patient has after surgery. All these facts allow the treating specialist to create a healthy diet strictly aimed at recovery and advise patients on appropriate recipes.
Specialized diet options number 4
Fermentative dyspepsia occurs against the background of digestive disorders caused by a lack of enzymes, diet failures, excess coarse fiber and simple carbohydrates, and problems with peristalsis. 4a diet helps solve the problems of bloating, heaviness in the abdomen, and a “lazy stomach .
Its goal: to limit the intake of substances into the body that irritate the intestines and provoke fermentation. The calorie content of the “calming” diet is 1600 kcal due to the predominance of protein and a reduced amount of carbohydrates, which have basic requirements. You need to stick to the table for no more than five days due to the monotony and scarcity of the food set.
A modified version of table 4a is recommended for intestinal diseases during exacerbations. Low-calorie menu for one day includes:
- Steamed omelette, semolina porridge with water and tea.
- Calcined cottage cheese.
- Meat puree soup, steamed meatballs and jelly.
- A glass of rose hip decoction.
- Fish aspic, boiled vermicelli and tea.
- A glass of kefir.
- White bread crackers, about 10 g of butter in porridge and no more than 30 g of sugar are acceptable during the day.
Chronic moderate inflammatory processes make adjustments to food recipes for every day. Diet 4b does not irritate the gastrointestinal tract, namely it prevents fermentation, increased secretion of bile and gastric juice. The menu recommended for complex diseases of the intestines, pancreas, liver and stomach consists of an expanded list of products:
- about 200 g of day-old or dry bread;
- soups with light (second) meat or fish broths with ground cereals, meatballs and finely chopped vegetables;
- boiled lean fish and meat or in steamed cutlets;
- boiled and grated starchy vegetables: cauliflower, potatoes and carrots;
- sweet berries and ripe fruits;
- fresh tomatoes with a good reaction to them;
- dairy products in dishes, fresh cottage cheese and kefir;
- within 15 g of butter without salt per meal;
- no more than two eggs per day, soft-boiled or in omelets, casseroles;
- cinnamon, fruit sauces, cheeses, pates and jellied dishes in small quantities, homemade sauces with broths and parsley;
- up to 100 g of fresh berries per day, baked apples, jelly and fruit jelly, except melons, plums, apricots and watermelons;
- green and black tea, coffee and cocoa with milk, fruit juices diluted with water up to 150 ml;
- less than 50 g of sugar per day, including in prepared foods.
Diet 4b recipes exclude fatty meat, poultry, fish, fresh fruit, baked goods, fatty broths and heavy cereals (millet, pearl barley), soda and chilled drinks, sweets and cappuccino:
- For breakfast, mashed potatoes with boiled fish and rice pudding.
- Fresh cottage cheese for a snack.
- For lunch, rice soup with mashed carrots, meat and buckwheat casserole, apple or quince jelly.
- For an afternoon snack, an egg white omelette and rosehip infusion.
- For dinner, carrot puree with lean beef cutlets.
- Before bed, cottage cheese or kefir.
Diet 4 for intestinal diseases in remission
The expanded menu for the week involves a transition to a nutritious diet based on boiled, steamed or baked dishes. Restrictions apply to foods that increase fermentation and flatulence:
- fried and fatty meat;
- rich broths;
- fresh vegetables and fruits;
- cereals with a high fiber content;
- legumes;
- soda;
- fresh bread and pastry.
You can treat yourself to marshmallows, marshmallows or Turkish delight.
Gluten-free menu (diet No. 4ag)
Celiac disease, or the absence of a certain protein in the intestinal mucosa, prohibits grains containing vegetable protein - gluten. Nutrition is developed with a predominance of animal protein and dairy foods, and the requirements depend on the stage of treatment. In case of complete exhaustion, intravenous administration of glucose and fructose is indicated. After vomiting and diarrhea stop, a strict diet is introduced for 8-10 months , and then gluten-containing foods are gradually included in the diet.
For children up to 3-4 months only breast milk is recommended, and for older children - gentle food in small portions and fractionally. Basic Rules:
- stew, boil and grind;
- peel the skins of vegetables and fruits;
- completely give up grapes;
- exclude coarse fibers (apples, legumes, raw cabbage);
- do not give mushrooms;
- exclude store-bought milk;
- You can use homemade dairy products if you are not lactose intolerant;
- sweets to increase calorie intake.
List of available products on the 4ag diet:
- rice, corn, soybeans, tree nuts;
- vegetables, including potatoes;
- fruits other than dates and bananas;
- corn and rice flour;
- meat and fish, caviar;
- buckwheat in small quantities;
- vegetable oils;
- homemade sour cream, cream and butter, cottage cheese and cheeses;
- sugar, honey, homemade jam;
- tea and ground coffee;
- homemade pates, store-bought seaweed, canned corn.
Wheat, oats and barley, as well as products containing them, are dangerous for people with celiac disease:
- flour, bakery products;
- canned food and sauces;
- beer and vodka;
- carbonated and packaged drinks;
- instant coffee 3 in 1;
- chewing gum, chips;
- industrial dairy products.
Intestinal diseases almost always disrupt the functioning of adjacent organs of the digestive system.
Following the principles of proper nutrition, as a rule, helps to keep symptoms under control and not lead to complications. February 6, 2019
The fourth table for gastritis in children
Therapeutic nutrition for a child with gastritis, other gastrointestinal diseases (colitis, enterocolitis) and their painful manifestations (constipation and diarrhea) begins with a fasting day. During the first 24 hours, children should not be fed; they are only allowed to consume an unlimited amount of free liquid in the form of clean still water, various decoctions and unsweetened compotes.
On the second day of the disease, the young patient can already be switched to dietary nutrition. Diet No. 4 for children has identical features and recommendations with diet No. 4 for adults. The only exception is that the energy value of foods, the daily caloric intake and the size of a child’s consumed portions are significantly less than those of an adult.
The diet is easy and relaxed for children if they have previously adhered to the principles of proper nutrition. True, limiting the consumption of sweets always upsets kids.
Key diet rules
Like any food restrictions, the 4 “B” diet contains a number of rules, compliance with which forms the basis of proper dietary nutrition:
- The required amount of water is 1.5 liters per day. Precisely pure water, not tea, milk or juices;
- The amount of salt is reduced to a minimum, that is, no more than 8 grams per day;
- Meals are divided into small parts. You need to eat six times during the day;
- Fried foods should be excluded. Food only boiled or steamed.
Also, in case of intestinal diseases, it is necessary to exclude any foods that cause fermentation or putrefactive processes in the body.
Dish recipes
Table No. 4 imposes restrictions not only on products, but also on methods of their preparation. It is allowed to boil, stew and bake, and serve food in liquid, mushy and pureed form. It is strictly forbidden to include fried foods in the menu for gastritis and after gastrointestinal surgery. But for all its severity, table 4 can be tasty and varied; for this you just need to use dietary recipes, of which there are many options.
To prepare tasty and healthy dishes, you need a table of calorie content and a list of allowed foods, the recommendations of which cannot be deviated even one step. For people who monitor their diet, a calorie table will be needed even after completing a therapeutic course of nutrition for intestinal diseases.
First course recipes
Every day in the lunch menu, especially after gastrointestinal surgery, it is necessary to include warm liquid dishes that activate the intestines and help to quickly reach a state of remission. First there will be lean puree soups, and then main courses with rich broths, dumplings and pieces of lean meat.
Meatball soup
Ingredients:
- 200 grams of minced chicken;
- 1 egg;
- 2 potatoes;
- 1 carrot;
- A pinch of salt.
Preparation:
Throw the potatoes and carrots cut into large cubes into boiling water. When the vegetables are ready, the broth must be ground until smooth and put back on the fire. Form the minced meat into meatballs, add them to the boiling soup, add salt and cook for another 10 minutes.
Protein recipes
Fish quenelles
Ingredients:
- 400 grams of hake fillet;
- 100 grams of rice cereal;
- 1 egg;
- 4 tbsp. l. sour cream;
- A pinch of salt.
Preparation:
Pre-cook the rice, drain in a colander, and after cooling, pass through a meat grinder twice along with the fish fillet. Add egg, salt to the resulting minced meat and mix thoroughly. Put water on the fire and when it boils, quickly add a teaspoonful of all the minced meat. After 10-15 minutes, the fish dumplings can be removed from the broth, seasoned with sour cream and served.
Dessert Recipes
Curd steam soufflé
Ingredients:
- 250 grams of low-fat cottage cheese;
- 2 eggs;
- 2 tbsp. l. sour cream;
- 2 tbsp. l. semolina;
- 1 tbsp. l. stevia.
Preparation:
Separate the egg yolk from the white and use a blender to mix it with all the other ingredients. Turn the whites into a thick foam (to make them beat better, you can add a pinch of salt to them). Carefully add the whites into the homogeneous curd mass, put the future soufflé in the mold and send it to the multicooker for half an hour, set to the “Steam” mode.
Diet No. 4 for gastritis, acute and chronic diseases of the digestive tract (colitis, enterocolitis) and its painful manifestations (constipation and diarrhea) directs the patient on the right path of remission. After just a week, table 4 can be changed to 4a or 4b, followed by a fairly light diet 4c and complete recovery.
THESE ARTICLES WILL HELP YOU LOSE WEIGHT
Your feedback on the article:
( 1,090 ratings, average: 4.51 out of 5)
Features of diet No. 4
The “Table 4” diet includes rules common to all tables:
- Fatty and fried foods are absolutely unacceptable;
- strict restrictions, and sometimes a complete ban on sweets;
- fractional diet - 4-5 times a day;
- using predominantly natural products.
However, the specificity of gastrointestinal diseases requires special restrictions:
- To reduce the load on the digestive system, caloric intake is limited to 2000 kcal/day. At the same time, the proportion of proteins remains within the normal range - 90 g, the emphasis is on animal proteins, which are digested faster and easier than plant proteins. The share of fats is reduced to 70 g, and the share of carbohydrates is reduced to 250 g.
- To reduce chemical irritation of the gastrointestinal mucosa, a restriction on salt is introduced - up to 10 g / day, as well as a strict ban on canned food, marinades, and smoked products. The volume of liquid increases - you need to drink up to 1.5-2 liters per day.
- Dietary table 4 allows dishes only in liquid form, ground, or pureed in order to reduce mechanical irritation of the gastrointestinal tract and facilitate the movement of the food coma in the stomach and intestines. Eating crumbly cereals is not allowed, especially during the acute period of illness.
- to avoid thermal irritation, it is recommended to eat only warm food at room temperature; very hot and very cold foods and drinks are strictly prohibited.
Video
For what diseases is it indicated?
Therapeutic diet 4 is prescribed for intestinal diseases that are accompanied by diarrhea - enteritis and colitis of various natures.
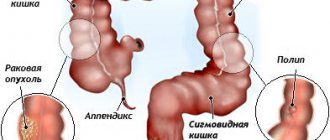
Photo: therapeutic diet 4 is prescribed for intestinal diseases
Its main characteristics are a low content of carbohydrates and fats with a normal amount of proteins, vitamins and water. The overall energy value is reduced.
The diet is prescribed taking into account the fact that with diarrhea there is a violation of the absorption of nutrients and a significant loss of fluid and electrolytes, so the food should be easily digestible, not cause fermentation and putrefactive processes, not stimulate the secretion of the digestive glands and not irritate the intestines, while compensating for water disturbances. electrolyte balance.
When is it prescribed?
Table No. 4 is shown to people:
- Having an intestinal disorder accompanied by diarrhea.
- For stomach diseases (gastritis).
- For intestinal disorders caused by infectious diseases.
- Those with diseases of the gastrointestinal tract (colitis, enteritis, duodenitis, etc.).
- With constipation due to previous intestinal diseases, after eliminating the pathology with medication.
- After treatment of intestinal diseases of any etiology.
- During the period of exacerbation of chronic gastrointestinal diseases. A therapeutic diet is also indicated for pain in the intestines due to chronic diseases, even if this is not an exacerbation, such nutrition simply helps to support the body.
- When treating the intestines surgically in the postoperative period.
Intestinal obstruction, inflammation of the large or small intestine, inflammation of the stomach wall, disruption of the pancreas - for all these pathologies, following a diet is indicated. If you have problems with the intestines and stomach, it is very important to choose the right nutrition option and table number 4 will be optimal. It is used to alleviate the patient’s condition and normalize regular bowel movements with a diseased intestine.
Dietary table 4B
This diet is prescribed for intestinal colitis and other acute diseases of this organ during the period of improvement, chronic intestinal diseases with mild exacerbations or when the condition improves after sharp exacerbations, as well as when the above diseases are combined with lesions of other digestive organs.
This diet is built on the same principle as diet number 4, but is still somewhat different from it. During the period of observance, food can be consumed not only in pureed form, but also in crushed form. Stewing and baking are allowed, but the rough crust must be removed from food prepared in this way. In addition, the list of foods that can be consumed is expanding. In addition to those allowed by Diet 4, you can also add the following products to your menu:
- Dry biscuits, savory pies and buns with apples, eggs, boiled meat, cottage cheese.
- Black and chum caviar.
- A couple of eggs a day, but only as part of other dishes, baked, cooked in the form of an omelet and soft-boiled.
- Mild cheese.
- Boiled noodles and vermicelli.
- Pumpkin, carrots, zucchini, cauliflower, potatoes in small quantities, but only heat-treated and pureed. Ripe tomatoes in small quantities. At the same time, eating mushrooms, onions, spinach, sorrel, cucumbers, rutabaga, turnips, beets, cabbage, radishes, radishes is prohibited.
- Soups with the addition of vermicelli or noodles.
- Cinnamon, vanilla, parsley, bay leaf, dill.
- Sweet types of fruits and berries, but only ripe ones, for example, tangerines, pears, apples, strawberries. At the same time, berries with coarse grains, watermelons, melons, plums, apricots, grapes and peaches must be discarded.
- Coffee.
- Pastille, marshmallows, marmalade, meringues, jams from sweet fruits and berries.
All other prohibited foods should be avoided.
Table No. 4g
Indications: - exacerbation of long-term intestinal disease (chronic form); - addition to chronic intestinal disease of pancreatitis in the acute stage.
Target:
- reducing the calorie content of food consumed; - healing of inflammatory foci. My tips
-Calorie content - 1800 kcal per day. -In the diet, carbohydrates make up up to 200 g, and proteins and fats must be reduced to a minimum, almost to 0. -Food must be warm, boiled or “steamed”. “Vegetarian” soups made from cauliflower, zucchini, and pumpkin are allowed, without adding onions or seasonings. -Do not abuse porridge. -We recommend fish or meat soufflé, minced meat or puffed cutlets (use pureed rice instead of flour). -You can use light cottage cheese up to 4-5% fat. -Instead of fruit, it is better to use jelly. "Stop" - products:
- everything is fatty; - fried food; - salinity; - smoked meats; - goose and duck meat; - fatty dairy and fermented milk products; - avocado; - nuts; - mayonnaise; - barley porridge; - millet; - bran; - mushrooms; - sauces; - legumes; - all soy products. Sample meal plan for the day
Breakfast: 2 – 3 crackers, light chicken or fish broth, still mineral water. Snack: steamed omelette and cutlet, 1 - 2 slices of bread, 200 ml of low-fat milk. Lunch: boiled fish 100 g; boiled zucchini 100 g; 1 - 2 slices of bread; raisins 30 g, tomato juice 200-250 ml. Snack: jelly, fruit jelly, still mineral water. Dinner: 150 g of oatmeal, puffed cutlet, carrot puree, 1 - 2 slices of bread, tea with milk.
Now you know what table 4 (diet 4) according to Pevzner is for diarrhea. A diet for diarrhea in an adult, and even more so in a child, should, of course, be prescribed by a doctor.
I wanted to convey to you the general principles of proper nutrition for this disease. Read my blog, eat right and don't get sick!
Allowed drinks
If a person’s gastrointestinal tract is disrupted and he suffers from diarrhea, then he should be sure to replenish the lost fluid. All drinks taken during this condition should be warm.
A diet for intestinal disorders in children and adults involves drinking non-carbonated mineral water, which will not only quench thirst, but also replenish the loss of essential microelements. It is also acceptable to take black or green tea, natural coffee and cocoa, but only without adding milk.
If you have an upset stomach and intestines, drinks made from quince, currants or rose hips have a beneficial effect on these organs. It is also acceptable to use jelly made from blueberries. To prepare it, you need to take 3 large spoons of blueberries, then grind them through a sieve, add 2 cups of water and boil for 20 minutes. Next, pour 1 large spoon of starch into the same bowl and keep the drink on the fire for about 5 minutes, stirring it regularly.
Recipes for the table No. 4
Many people believe that it is very difficult for people with a diseased intestine to prepare a dish according to the specified diet, but this is not so.
There are several simple recipes that will be useful for diet No. 4:
- Barley soup. 40 g of pearl barley, previously well washed, should be thrown into 600 ml of low-fat meat broth. On the stove, simmer the soup over low heat, stirring all the time, until the pearl barley is well boiled. The soup is cooled to just above room temperature and given to the patient.
- Meatballs made from meat and fish. The meat is thoroughly ground in a meat grinder and mixed with boiled rice cereal. To prepare meatballs, you need to take minced meat, which consists of five parts meat and 1 part rice. Meatballs are molded and steamed.
- Semolina. For 50 grams of semolina take 5 grams of sugar and cow butter. Add semolina to boiling water (one glass) with salt and sugar and stir it. The fire is turned on and the porridge cooks for 25 minutes. Then add a piece of butter.
- Blueberry compote. Only dried berries are suitable. 20 grams of blueberries are poured with boiling water (1 cup) and sugar is added as desired. Place on the fire for 25 minutes and boil all this time. Remove the compote from the stove and let it brew for three hours.
These dishes are prepared very quickly, and you don't need a lot of ingredients. But such dishes are very useful for people with sick intestines; they help not only make food easier to eat, but also nourish the body, allowing the intestines to independently establish the digestion process.
Video
Treatment tables according to Pevzner
The concept of therapeutic diets or tables was introduced for the convenience of their administration and the organization of hospital nutrition.
If the patient has several diseases, then the tables are combined with each other so as to provide the most suitable diet.
There are 16 tables in total, each of them is prescribed for the corresponding diseases:
- Diet 0 (surgical). Sometimes it is not allocated to a separate table. It is prescribed immediately before abdominal operations and within 1-2 days after them. Includes tube feeding. Diet option 0a - therapeutic fasting, is prescribed on the first day after surgery.
- Diet 1. Prescribed for gastritis with high acidity and peptic ulcers. There are two versions - for the treatment of exacerbations and for their prevention. Involves limiting products that chemically, mechanically or thermally irritate the mucous membrane. The main goal is to provide the most gentle conditions for the damaged mucosa.
- Diet 2. Prescribed for gastritis with low acidity. It assumes the presence of products that stimulate the secretion of gastric juice - seasonings, sauces, salt, coffee and others. The main goal is to stimulate digestion. Not compatible with diet 1.
- Diet 3. For intestinal atony and associated constipation. Involves the consumption of foods rich in cellulose and vegetable oils, which stimulate intestinal motility. At the same time, limiting food that can cause fermentation and putrefactive processes in the intestines - with atony, the products of these processes enter the blood in large quantities.
- Diet 4. For acute intestinal diseases and exacerbation of chronic ones. The main goal is gentle conditions for the intestinal mucosa and easy absorption of food. It involves the use of easily digestible products that do not cause fermentation, rotting, etc.
- Diet 5. For diseases of the liver, biliary tract, pancreas. The main goal is to reduce the load on these organs. Products are easily digestible. Can be combined with other gastroenterological diets.
- Diet 6. Diseases caused by uraturia (high levels of uric acid salts) - gout and urolithiasis with urate stones. The main goal is to reduce the amount of uric acid in the blood, and as a result, stop the deposition of its salts.
- Diet 7. Prescribed for various kidney diseases without symptoms of acute or chronic liver failure. Combines with other urological diets. The main goal is to reduce the load on the kidneys. Involves limiting salt and strictly monitoring fluid intake.
- Diet 8. Prescribed for obesity. Can be combined with other diets. The main goal is weight loss. It involves limiting high-calorie foods and eating various dishes containing large amounts of fiber, reducing the energy value of food.
- Diet 9. For diabetes. It involves strict recording of the amount of carbohydrates consumed and its relationship with energy expenditure. The main goal is to maintain stable normal blood glucose levels. Can be combined with table 8 and others if necessary.
- Diet 10. For diseases of the cardiovascular system. It assumes a sufficient intake of microelements from food necessary for the normal functioning of the heart, limitation or complete exclusion of foods that stimulate cardiac activity, increase cholesterol levels, and limiting salt.
- Diet 11. For tuberculosis, as well as exhaustion after various diseases, injuries, and some medical procedures. The main goal is to restore the vital functions of the body. Involves increased energy value of food and consumption of easily digestible foods.
- Diet 12. For functional diseases of the nervous system. Products that excite the nervous system are limited or completely excluded. The main goal is to provide conditions for the most effective drug therapy. Must be combined with a treatment regimen.
- Diet 13. For acute infectious diseases. The main goal is to support the immune system, providing the body with sufficient nutrients and energy, subject to bed rest. It is necessary to consume easily digestible foods that do not create putrefactive processes in the intestines. The energy value of food depends on the severity of the patient's condition.
- Diet 14. Prescribed for urolithiasis with phosphaturia (excretion of phosphoric acid salts). Limit foods containing phosphates, as well as table salt, and be sure to drink plenty of fluids. The main goal is to normalize the urine reaction and prevent the appearance of stones.
- Diet 15 (common table). The amount of incoming nutrients and energy value correspond to physiological standards. There are no special restrictions on the type of products consumed. The main goal is balanced nutrition in a hospital or sanatorium setting.
Table No. 4b
Indications:
— the final stage of intestinal disease (recovery); - chronic intestinal diseases without exacerbation; - a combination of chronic intestinal disease with other gastrointestinal diseases. Target:
- adjust the body to its usual diet; — adequate processing of products; - absorption of vitamins.
My tips
-Food: boiled or steamed, no frying. -All soups are included in the diet, except pea and bean soup. You can have a light broth with vegetables: carrots, cauliflower, zucchini. -Fish and meat as in table 4b. If necessary, you can include dairy sausages in your diet. -All porridges are allowed, except barley and millet. -You can have bread, but not fresh, rye bread. Biscuits with light cream, hard cookies, and various cheesecakes. -A little vermicelli is added to the food. -You can't have too acidic dairy products. -1-2 eggs per day are allowed, both in a dish and in a steamed omelet. -The diet contains about 50-70 g of sugar per day. -Includes beets, green boiled peas and cabbage. - From liquids - tea, weak coffee and cocoa - drinks.
“Stop” - products: - fried food; - spicy sauce; - okroshka; - ice cream; - goose, duck meat, pork; - smoked meats;
- sour milk; - hard boiled eggs"; - sweet pastries with rich cream; - butter dough, but cheesecakes are fine; - chocolate products.
Approximate menu for the day:
Breakfast: oatmeal (it is recommended to cook it with milk), egg, tea. Second breakfast: apple. Lunch: vegetable soup, pilaf and boiled meat, jelly. Afternoon snack: rosehip compote. Dinner: mashed potatoes, fish, curd pudding, tea. An hour before bedtime: fresh kefir.
Dietary table 4B
This diet is prescribed after the 4B diet as a transition to normal nutrition, for chronic enterocolitis during remission, acute intestinal diseases in the recovery stage and when combined with diseases of other digestive organs.
While following the 4B diet, foods no longer need to be washed or chopped. Eating fried foods is still not recommended, but is sometimes acceptable. In addition to previously permitted products, you can also enter the following into the menu:
- Cheesecakes with cottage cheese.
- Diet sausage, milk sausage, doctor's sausage and frankfurters.
- In limited quantities, chopped soaked herring.
- Non-acidic sour cream, but only as part of other dishes, fermented baked milk, kefir.
- Refined vegetable oils.
- All types of pasta and cereals, only legumes are excluded.
- Beetroot.
- All ripe fruits and berries, mousses, compotes, fudge, toffee, marshmallows.
- Tomato juice.
Fresh bread and baked goods, fatty poultry, strong broths, fatty fish, raw eggs, fatty meats, smoked meats, pickles, canned food, snacks, fast food, animal fats and other foods that were previously prohibited and not allowed by diet number 4B, you need must be excluded from the diet.
polzavred.ru
Varieties
Therapeutic diet number 4 has subtypes that are prescribed for various characteristics of diseases - these are 4a, 4b, 4c. Let's look at each one separately.
Therapeutic diet according to Pevzner 4a
It is prescribed when fermentation predominates in the intestines. It differs from No. 4 in that carbohydrates are excluded from the diet. This includes crackers, cereals, and sugar. Satiety is achieved by increasing protein foods. More lean meat and cottage cheese are introduced into the diet. Usually a week is enough to put the gastrointestinal tract in order, then they move on to table 4.
Diet 4b according to Pevzner
A gastroenterologist prescribes a similar diet for chronic colitis, but only when the exacerbation has already passed. You can eat up to 6 times a day. The menu for the week with diet 4b according to Pevzner is selected based on the following products:
- Stale white bread.
- Broth with meatballs.
- Mild cheese.
- Grind porridge, you can even add a third glass of milk.
- Dry biscuit.
- Curdled milk.
- Boiled vegetables.
- Compote.
- Tea coffee.
- B vitamins are prescribed.
With good results, they switch from this diet to either 4B or table No. 4.
Table number 4b according to Pevzner
It is a transitional diet. It is prescribed before transferring the patient to a balanced diet. If the patient has an exacerbation, then table 4 will not be prescribed. The products are the same as diet 4, only they are no longer crushed, and the number of servings is increased. The only thing they do is reduce the amount of salt they consume. The diet has a fairly high calorie content - 2800-3000 kcal. Therefore, it is advisable for the patient to move a lot, otherwise there is a high risk of gaining excess weight.
Medical nutrition No. 4 can be prescribed to anesthesiologists after surgery. It does not burden the intestines, thereby facilitating its work. And if the patient recovers quickly, then he needs to return to a normal balanced diet, and this is easier to do after table No. 4. Then this will happen painlessly for the gastrointestinal tract.
Dietary recommendations
During the period of following the 4-a-day diet, it is recommended to eat at least five times, and the portion size should be small. It is advisable to eat food at the same time, this will improve its absorption and normalize the functions of the gastrointestinal tract. All food and drinks consumed should be at a comfortable temperature, since food that is too cold or, conversely, very hot can trigger an attack.
When preparing food, frying should be avoided; the recommended methods of processing foods are boiling and steaming. Any food should be consumed only in liquid, pureed or mashed form.
The diet for colitis and other intestinal diseases does not allow the consumption of smoked, fatty and spicy foods, as well as solid foods containing insoluble fiber or too dry foods. Salt and sugar should be significantly limited in the diet. To make it clearer what food you should avoid first, we present a list of prohibited foods:
- Smoked products, canned food, semi-finished products, pickles, sauces, marinades, snacks, fast food.
- Fatty types of meat and poultry, strong meat broths, sausages, sausages.
- Fatty fish, caviar, dried and salted fish.
- Hard-boiled, fried and raw eggs.
- Any fresh baked goods, whole grain and rye bread, bran, pancakes, pancakes, baked goods, pasta.
- Animal and vegetable fats.
- Hard cheese, whole milk, kefir, cream, sour cream.
- Raw berries, fruits, and dried fruits.
- Vegetables.
- Barley and pearl barley, legumes, millet, buckwheat kernels.
- Spices, spices.
- Jam, honey, sweets, cakes and other sweets.
- Carbonated drinks, coffee, grape juice, kvass, fruit juices.
Despite the rather impressive list of foods that diet number 4 prohibits from consuming, you won’t have to eat sparingly, much less starve, while sticking to it, since the list of foods recommended for consumption is also quite large.
Products recommended for consumption:
- Lean poultry and meat. It can be beef, turkey, rabbit, chicken, veal. But keep in mind that after cooking, all meat dishes must be ground in a blender or pureed.
- Lean fish, such as perch or pike perch.
- Eggs, but no more than one per day. It can be added to other dishes or prepared as a steam omelette.
- Small quantities of stale wheat bread and unhealthy cookies. Occasionally, you can use a little wheat flour for cooking.
- Low-fat cottage cheese. Yogurt or milk is acceptable, but can only be used in certain dishes, such as pudding or porridge. These products cannot be consumed in their pure form.
- Butter is only allowed to be added to prepared dishes.
- Vegetable decoctions.
- Soups prepared in a second (weak) broth from fish, poultry or meat, with the addition of permitted cereals, as well as grated or chopped meat, meatballs.
- Applesauce, non-acidic jelly and jelly.
- Oatmeal, buckwheat (made from buckwheat), rice and semolina porridge, but only semi-viscous and pureed.
- Various teas, decoction of dried rosehip, black currant and quince, non-acidic juices diluted with water.
List of prohibited ingredients
One of the key rules of dietary table No. 4 is the complete exclusion of foods that have a stimulating effect on the secretion of the gastrointestinal tract. Those food ingredients that cause the development of putrefactive and fermentative processes in the intestinal lumen are strictly prohibited. Such products include sour cream, white and cauliflower, all types of cheeses, plums, grapes and grape juice, apricots, drinks with carbon dioxide, as well as dried fruits.
In order to get the desired result from following a dietary regimen, it is recommended to completely exclude the following food ingredients from the daily menu:
- first courses cooked in concentrated meat, mushroom, fish and vegetable broth, various soups containing unpureed cereals;
- fish and meat ingredients containing large amounts of fat, as well as smoked animal products, fish oil, fish caviar, all types of canned food, offal, sausages and sausages, fast food and store-bought semi-finished products;
- vermicelli, any types of pasta, barley, millet and pearl barley;
- chocolates and caramels, cakes, a drink made from cocoa powder with milk, cakes and pastry rolls, honey, fruit and berry compotes, homemade and store-bought jam;
- white cabbage, all types of legumes, lettuce, onions, garlic, tomatoes, bell and hot peppers, all types of mushrooms;
- energy and carbonated drinks, alcohol, chilled sweet drinks;
- all types of cheeses, fermented baked milk, sour cream, milk cream and kefir;
- fried chicken or quail eggs;
- lard, margarine, cooking, lamb and beef fat;
- spices and herbs, all types of sauces, including mayonnaise and ketchup, fresh and dried herbs;
- all varieties of freshly squeezed fruit and vegetable juices;
- products made from puff pastry or butter dough, pancakes, pancakes, bakery products made from wheat and rye flour.
The daily menu for children forced to follow table No. 4 includes a similar list of food products from the mentioned list.
What you can eat: table
| Product | Description |
| Soups | The first courses of every person's diet are soups; they can be cooked in low-fat broth. It is necessary to bring the dishes to a paste-like state, so you can add rice, meatballs, vegetables or pureed meat to the soup. |
| Meat | The main source of proteins and vitality is meat. You need only low-fat varieties, these include dietary rabbit meat, lean veal, and beef. Poultry meat - turkey and chicken, from which the skin must first be removed. |
| Fish | Low-fat fish, because it contains at least 14% protein, is the best source of phosphorus, iodine and calcium. You can cook the fish whole or as minced meat using steam and water. Low-fat varieties include cod, pike perch, flounder and many others. |
| Chicken eggs | It is very important to eat chicken eggs, but not more than one or two per day. A steamed omelet will be a wonderful breakfast. |
| Dairy | Homemade low-fat cottage cheese. |
| Porridge on the water | The basis of your diet, because they are easy and quick to prepare - buckwheat, rice, oatmeal, semolina. |
| Vegetables and fruits | Zucchini, potatoes, carrots, beets. But it is better to use fruits in the form of compotes and jellies. You can eat baked apples or pears. |
| Flour products | Only wheat crackers. |
General rules
Diet for diseases of the gastrointestinal tract is the most important factor in complex treatment, and in some cases it is the main component of treatment of the stomach and intestines.
Since the gastrointestinal tract is represented by a number of organs and various sections of the intestine, there are many diseases of the gastrointestinal tract, occurring in acute/chronic form, manifested by various clinical symptoms. Accordingly, therapeutic nutrition also differs. Thus, for gastroenterological diseases (gastritis with high/low acidity, peptic ulcer, gastroduodenitis), therapeutic Tables No. 1, 2 and their varieties are prescribed. For diseases of the hepabiliary system (liver, gallbladder, bile ducts) and pancreas, various options for dietary Table No. 5 are prescribed.
The main diets for intestinal diseases are therapeutic Tables No. 3 and 4, which are presented in several options (A, B, C). Among intestinal diseases, enteritis (acute/chronic diseases of the small intestine) and colitis (large intestine) are distinguished, occurring both independently and in combination (enterocolitis) with various functional disorders of the gastrointestinal tract. It is the type of disease, the form of the disease and functional disorders that determine what diet will be prescribed for intestinal disease.
This type of treatment table allows you to individualize therapeutic nutrition through correction (adding/removing a number of food products, changing the chemical composition and energy value of the diet, type of culinary processing, consistency of ready-made dishes, diet).
It is especially important for inflammation of the intestines and gastrointestinal tract that therapeutic nutrition ensures maximum sparing of the mucous membrane, since in the inflamed intestine/organ any inadequate mechanical/physical or chemical effect of food on the mucous membrane contributes to an exacerbation of the process. The basic principles of dietary nutrition for a diseased gastrointestinal tract/intestines are:
- providing patients with a complete and balanced set of nutritional macro/micronutrients in accordance with physiological norms and characteristics of the course of the disease;
- protecting the gastrointestinal mucosa from the effects of various types of negative factors (mechanical, chemical, physical);
- adherence to diet;
- reduction of the inflammatory process, restoration of function and natural intestinal biocenosis.
The prevailing functional disorders of the intestines are of great importance in choosing a diet. Thus, when putrefactive and fermentative processes predominate, in which diarrhea of varying intensity, bloating, and flatulence occur, Diet No. 4 according to Pevzner or its variations are prescribed, depending on the stage of the disease and the severity of clinical symptoms.
For example, for pain and cramps in the abdomen caused by increased gas content and intestinal distension, dietary Table 4A is prescribed to stimulate peristalsis, the distinctive feature of which is to limit the consumption of simple carbohydrates, which enhance fermentation processes. At the same time, the diet contains an increased amount of protein component (120 g) and a low content of fat (50 g) and carbohydrates (150-140 g), the total calorie content of the daily diet is 1600-1700 kcal/day.
Dishes are prepared boiled or steamed and pureed. No later than 2 weeks later, the patient is transferred to higher-calorie treatment Tables 4B and then 4B, which are less gentle and more varied in the range of permitted products.
For colitis and problems with bowel movements (constipation), treatment Table No. 3 is prescribed, which allows you to normalize impaired intestinal functions. The diet is physiologically complete, contains an increased amount of dietary fiber and macroelements, which are found in large quantities in vegetables, cereals, fresh fruits, dried fruits, and dairy products. Therapeutic nutrition involves the consumption of cold first courses, sweets and sweet dishes, and carbonated drinks.
At the same time, products that promote fermentation/rotting processes, stimulate the secretion of the digestive organs and irritate the intestinal mucosa (horseradish, mustard, hot spices) are excluded from the diet. When planning your diet, it is important to include foods that enhance intestinal motility and relieve constipation.
These are products containing simple carbohydrates (honey, jam, sugar, syrups), salt and organic acids (salted, pickled and pickled vegetables, salted fish, fermented milk drinks, canned snack foods, fruit drinks), dietary fiber (whole bread, bran, dried fruits , legumes, nuts, cereals, raw vegetables), prone to swelling (bran, fiber, seaweed), cold dishes (beetroot soup, okroshka, cold jellied dishes, jellied meat, carbonated drinks and ice cream).
For stomach ulcers and constipation, Table No. 1 will be the main one, but with an increase in the diet of boiled vegetables (zucchini, carrots, beets), prepared in the form of puree, well-cooked dried fruits, and refined vegetable oil. For liver diseases with constipation, treatment Table No. 5 is prescribed, but the content of dietary fiber and magnesium in the diet is increased (cereal/bran bread, oatmeal, buckwheat, pearl barley, vegetable/fruit juices, fruits, honey, natural vegetables).
In case of constipation against the background of exacerbation of chronic intestinal diseases, the gentle Table No. 4B is prescribed first, and then No. 4B; gentle peristalsis stimulants are included in the patients’ diet (vegetable juices, cold fruit drinks on an empty stomach, baked apples, pureed plums, carrots, beets , cabbage with the addition of vegetable oil).
Intestinal bleeding from the higher/lower parts of the intestine (rectum, sigmoid colon) requires special attention. The causes may be intestinal diverticulosis, ischemic intestinal lesions, colon tumors/polyps, infectious colitis, hemorrhoids/anal fissures, intestinal tuberculosis, ulcerative colitis and others.
A gentle way of eating may vary among different cultures and peoples and may exclude or include certain foods. Eating preferences and dietary choices directly affect a person's health and physical condition.
Diet is extremely important for stomach and intestinal upsets. A properly selected method of nutrition in such conditions will significantly alleviate a person’s serious condition and contribute to his speedy recovery. It must be remembered that with diarrhea, the patient’s body loses a huge amount of nutrients, water, minerals and salts. They must be replenished, otherwise the operation of all internal systems may be disrupted. To do this, you need to follow a special diet.
If you have an upset stomach or intestines, you should drink more water and eliminate many foods.
A diet for indigestion is organized according to the following rules:
- The patient should eat food frequently (about 5-6 times a day). At the same time, he needs to reduce the calorie content of his meals. The patient is allowed to consume no more than 2000 kcal per day. You should also reduce the amount of salt to a minimum.
- With severe diarrhea, the patient needs to drink a lot (about 1.5-2 liters of water per day). Products for such patients are boiled or steamed. During seasonal exacerbations, the patient is allowed to eat only liquid or semi-liquid food.
- A strict diet for functional disorders of the intestines and stomach must necessarily last throughout the entire period of exacerbation. After all the main symptoms have been removed and the patient’s condition has noticeably improved, a return to a varied menu is permissible. However, we should not forget that if there is a tendency to disorders of the gastrointestinal tract, a person’s food should be as gentle as possible. The foods consumed should not irritate the walls of the intestines and stomach, and therefore it is undesirable for the patient to include hard (poorly chewed), as well as sour and spicy foods in the diet.
Features of table 4A and 4B
Dietary table No. 4 is conventionally divided into subtypes such as 4A and 4B.
Therapeutic diet. Table No. 4A according to Pevzner
Option 4A is prescribed to patients to restore the functional state of the large intestine in case of colitis, accompanied by intense fermentation, gas formation and putrefaction.
Therapeutic diet. Table 4B
Table No. 4B is recommended to be prescribed during the period of subsidence of acute manifestations of the inflammatory process.
Prohibited Products
Table No. 4 completely excludes the consumption of foods containing fiber.
The list of prohibited products includes:
- Vegetables. They can be added to soups in small quantities and pureed.
- Bread. Whole grain, rye, bran, cereal. It is difficult to digest and can injure the mucous membrane.
- Fresh pastries, pancakes/pancakes. They provoke the processes of fermentation and rotting.
- Jam, honey, jam, dried fruits, sweets. During the day you are allowed to use 50 grams of granulated sugar.
- Porridge – millet, barley, barley, legumes.
- Pasta.
- Fatty broths. They contribute to increased intestinal motility and worsening of the condition.
- Fatty meats and fish.
- Canned food, pickles and fish in particular.
- Whole milk, cream, sour cream, cheese. May cause increased diarrhea. Milk must be diluted with water. It is used only for cooking porridges and puddings.
- Cocoa, coffee with milk, sweet soda, kvass.
- Sauces, marinades.
- Smoked meats, ham, sausages.