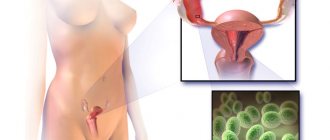
Intestinal dysbiosis is a fairly common pathology characterized by digestive disorders. He causes a lot of trouble. Symptoms of intestinal dysbiosis in women are many-sided: broken stools, periodic abdominal pain, poor digestion of food and many other signs. The disease is associated with a violation of the normal composition of the microflora, in which the body is “populated” by pathogenic bacteria. What caused this condition? And what methods can be used to combat it?
What is dysbiosis
Treatment and prevention of dysbacteriosis is impossible without knowing the definitions. This type of disease is caused by an imbalance between the bacteria living in the intestines. Dysbacteriosis is sometimes treated with antibiotics. Sometimes the cause that gave rise to the disease is used to get rid of it. An analogy is appropriate: poison becomes medicine in small quantities.
Normal microflora provides intestinal protection, helps produce and absorb vitamins and microelements. An imbalance is called dysbiosis.
Prevention of dysbacteriosis
Doctors insist that dysbiosis is always a secondary condition and goes away on its own some time after the gastrointestinal tract normalizes. Dysbacteriosis after antibiotic therapy is considered normal. If you follow the rules of personal hygiene and a balanced diet, the microflora returns to normal within a week. The exception is severe immunodeficiency due to systemic viral diseases, chemotherapy and long-term hormone therapy. In this case, all the body’s defense mechanisms suffer and without outside help the microflora is unlikely to normalize.
Prevention of intestinal microflora disorders consists of proper nutrition, normalization of work and rest schedules, and timely treatment of viral diseases and intestinal infections. Despite the fact that bacteria in fermented milk products die in the environment of the stomach, doctors and scientists insist on the need for them in the daily diet. With regular consumption of high-quality yoghurts (with a high content of bacterial cultures), a sufficient number of bacteria enter the intestines to prevent microflora disorders.
Treatment of dysbiosis
We will learn how dysbacteriosis is treated and get an idea of ways of prevention.
Prebiotics
Flora is restored by prebiotics included in food products:
- Raffinose is found in beans and peas and serves as a leading factor in the formation of the population of bifidobacteria.
- Garlic, chicory, artichoke, onions, and bananas are filled with inulin. Increases the absorption of calcium, acts as food for bifidobacteria and lactobacilli.
- Fructooligosaccharides are found in onions, bread, corn, and cereals. They provide a nutrient medium for bifidobacteria.
- Galacto-oligosaccharides are found in milk in small quantities, and in large doses in human milk and special nutritional formulas for feeding babies.
- Pectin is found in blueberries, carrots, apricots, and apples. Absorbs toxins, stimulating the production of gastric juice, and forms the natural pH factor of the environment.
- Other dietary fibers are rich in bran, fruits, vegetables, and mushrooms. In bulk, they improve digestion, slow down the absorption of nutrients, eliminating obesity, and serve as a breeding ground for bacteria.
Probiotics
Due to skillful selection of diet, a favorable background is created. Fermented milk products are not on the list; we were talking about prebiotics. Fermented milk products are known as sources of live cultures, representing probiotics. Freshness of products is an important criterion for suitability. One-day kefir is beneficial. After five days, it is not recommended to drink the drink; the necessary bacteria die.
Much healthier food is in the form of biokefirs and yoghurts. But the strains contained in drinks die from gastric juice. Being part of a drink, they are more resistant than as part of a medicine. If we talk about specialized drugs, like Hilak Forte, the strains used are characterized by increased resistance to hydrochloric acid, reaching the intestines with minimal losses.
Sorbents
Sometimes it is not possible to defeat the raging strain, and it is “washed away”. The patient swallows a sorbent, like Lactofiltrum, which absorbs the harmful strain and removes it out with the passage of chyme. The body gets rid of bacteria and excretes it in feces. Lactofiltrum does not pollute the body, like antibiotics and antiseptics.
Enzymes
A wounded intestine does not cope well with digestion. At the slightest sign of indigestion, use Creon. The drug does not treat dysbacteriosis, but relieves the gastrointestinal tract and gathers strength to fight the infection. In combination with a thoughtful diet, Creon is the optimal remedy for getting rid of imbalance. Take medicine for dysbiosis, improving food digestion.
What is dysbacteriosis
For the human stomach to function properly, it must have a balance of bacteria.
If the amount of pathogenic flora exceeds the number of vital microbes, an imbalance occurs.
If there is an excess of pathogenic microorganisms on the intestinal walls due to dysbacteriosis, the functioning of the gastrointestinal tract occurs.
Effective food processing is impossible with this disease. Moreover, it is complicated by the difficult absorption of beneficial nutrients from food by the stomach.
There is no bacterial content in the gastric cavity and small intestine.
But directly on the intestinal walls there is a huge number of microorganisms, each of which performs a specific function.
Interesting fact! The total weight of all bacteria living in and on the body of an adult is 2-3 kilograms.
The so-called “beneficial” flora is vital for human health. Without it, his body would not be able to function properly.
Thanks to the intestinal microflora, the body undergoes the process of fat, cholesterol, carbohydrate and protein metabolism.
Therefore, to maintain an adequate immune system, microflora is very important. With dysbacteriosis, it is disrupted.
The intestinal “population” provokes the body’s active production of immune reactions. It has been scientifically proven that people with strong immune defenses are less likely to get sick.
ARVI and influenza ailments affect those who cannot boast of a strong immune system. In other words, if the protective function fails, the person becomes vulnerable to many ailments.
There are bacteria in the human body whose main mission is to export toxic and other pathogenic microbes. If their number decreases, health problems arise.
With dysbacteriosis, something like a “rampant” pathogenic flora occurs in the human body. Sticks, microbes and fungi attack the tissue surface of internal organs and provoke various diseases.
Therefore, to maintain health, it is important to control the balance of pathogenic and beneficial microorganisms.
When the first signs of dysbacteriosis appear, therapeutic measures should be taken. But before that, you need to familiarize yourself with the symptoms of this pathology.
Prevention
Sad figures say that 0.6% of newborns today do not have pathologies. The rest are weakened. Microflora begins to form already in the prenatal period. While passing through the mother's birth canal, the baby continues to gain the necessary flora. The process depends on the maternal environment.
Pathologies of the parental microflora are highly likely to be transmitted to the child’s intestines. The changes are initially temporary, then chronic. The baby and parents should be treated, which indicates the importance of preventing dysbiosis for young people.
Before planning the birth of offspring, dysbiosis should be cured. Check the intestinal flora, get rid of parasites. Future mothers and fathers must pass tests to make sure that the offspring will be healthy. Give up bad habits, medications, alcohol and antibiotics.
Provide nutritious food with sufficient amounts of microelements and vitamins. Introduce milk into your diet if the product does not cause flatulence. Eat less food that falls under the definition of “animal”. Have less contact with people who have had a sore throat or flu, or suffer from intestinal disorders.
Signs of dysbiosis
In medicine, there are 4 stages of this pathology, each of which is characterized by the manifestation of specific symptoms.
Let's take a closer look at each stage of dysbiosis.
First stage
For many patients it is “not noticeable”. We are talking about an asymptomatic course of the disease.
As for the imbalance of normal and pathogenic microflora, it is insignificant. That is, the patient does not experience diarrhea and severe pain in the stomach area.
This milder form of bacterial pathology is caused by long-term use of medications (antibiotics) or poor diet.
For example, dysbiosis can be triggered by eating vegetables and fruits that have not been subjected to heat treatment.
However, at this stage of development of the pathology, the patient may experience increased gas formation and rumbling in the abdomen.
If you take therapeutic measures in time, you will be able to normalize the bacterial balance in a short time.
Second stage
Now the person will definitely feel sick. This phase of the development of the disease is characterized by the appearance of an unpleasant taste and odor in the mouth, mild stomach discomfort, decreased appetite, nausea and flatulence.
The patient's abdomen is slightly distended. However, a person who is faced with dysbiosis feels unwell at this stage. He experiences attacks of nausea more often.
The disease is also characterized by a malfunction of the gastrointestinal tract. In most cases, the patient experiences diarrhea.
It is not always possible to relieve the manifestation of this symptom by taking medications.
At this phase, dysbiosis is difficult to diagnose, because the symptoms that characterize it can be confused with signs of other diseases of the gastrointestinal tract.
Third stage
A disease that develops rapidly requires the attention of medical specialists. It will no longer be possible to get rid of it at home.
The third phase of the progression of the pathology is characterized by the presence of a large amount of pathogenic microflora on the intestinal walls, which leads to dysfunction of the internal organ systems.
Bloating is a constant companion of a patient suffering from dysbiosis. He will also experience nausea, which occurs mainly in the morning, vomiting, dizziness and other unpleasant symptoms.
This picture leads to a person’s loss of ability to work. His stomach can no longer function properly. The digestion process needs to be normalized.
Only a qualified specialist can help a person facing this problem.
At this stage, dysbiosis is easily diagnosed. The patient submits stool for analysis, studying which, medical specialists in the laboratory can see pieces of undigested food in it.
This indicates that the disease is progressing. You should not ignore the manifestation of its symptoms, otherwise it will not be possible to avoid complications.
Fourth stage
The most severe degree of dysbacteriosis. The disease in this phase is characterized by an excessive amount of pathogenic microflora, which completely displaces beneficial microorganisms.
If the patient is not provided with timely medical care, the disease will provoke a disruption in the body’s absorption of nutrients.
The most difficult to tolerate symptom of dysbacteriosis, which manifests itself at stage 4, is pain.
Severe colic that occurs in the gastric zone can rarely be stopped even by taking potent painkillers.
A patient whose body is subject to such pathology often gets sick. His body may be affected by intestinal infections.
General signs of dysbiosis, manifested at all 4 stages:
- Belching.
- Failure in the functioning of the gastrointestinal tract (diarrhea).
- Severe pain in the abdominal area.
- Flatulence (bloating).
- Increased gas formation.
The manifestation of these symptoms leads to a deterioration not only in the patient’s health, but also in his well-being.
Remember that the presence of a microflora disorder is a serious pathology that requires therapeutic measures.
Additional Products
Doctors say that 90% of people suffer from the disease. It is completely difficult to cure dysbacteriosis. Be careful with antibiotics and pharmaceutical products. Try to suppress intestinal foci of chronic infections by eating natural foods, foods rich in beneficial bacteria. A couple of times a year, take a treatment course with Normoflorin, Zosterin-Ultra and other drugs of a similar nature.
Bacterial medicines suppress pathogenic strains and restore normal microflora. Without causing damage, they increase immunity, help the intake and absorption of necessary components: proteins, fats and vitamins.
Enrich your diet with fermented milk foods rich in microflora, use dietary supplements, vitamin complexes, and antifungal agents. Periodically monitor the intestinal population by getting tested. The pharmacological market accommodates a large number of antibiotics. If a person often takes medications without prescription, such behavior leads to dysbiosis.
Correcting nutritional errors
Treatment should always begin with establishing a diet. In many cases, the intestinal microflora is able to recover on its own over time, but it needs help. Whatever option for getting rid of dysbiosis is chosen, without following the rules of a healthy diet, treatment will be ineffective.
To begin with, you should exclude fasting and strict restrictive diets, because during dysbacteriosis the body already suffers from a lack of vitamins.
Stages of treatment of dysbiosis
In this case, you should remove from your daily diet:
- fatty meat and fish;
- fried and spicy;
- smoked meats and canned food;
- baked goods, sweets, white bread;
- eggs in the form of fried omelettes and scrambled eggs, as well as hard-boiled ones;
- vegetables that have an aggressive effect on the gastrointestinal tract (radish, raw onions and garlic (except for swallowing a whole clove), sorrel);
- mayonnaise and sour sauces (ketchup);
- alcohol, carbonated drinks.
The above products have an irritating effect on the already damaged intestinal mucosa, and also feed the pathogenic microflora that has colonized the intestines.
Basic principles of proper nutrition for dysbiosis:
- eating regularly at the same time;
- eating warm food (within 25-40 degrees) and avoiding too cold or hot food;
- avoiding aggressive and spicy foods;
- chewing food thoroughly;
- eating food frequently (every two and a half hours) and in small portions;
- drink plenty of fluids, but not during meals (so as not to interfere with the digestion of food).
Diet for dysbiosis
Compliance with these simple rules is the key to quickly and completely getting rid of dysbacteriosis, as well as preventing its relapses.
The most important!
Remember: many patients harm their health with their own hands. Inspirational advertising encourages self-medication. At the same time, it is forgotten that not everything shown on TV can be trusted.
The main preventive measure is a rational, thoughtful lifestyle. Let your doctor choose the medications and dosage.
Drugs for the treatment of intestinal dysbiosis in adults include probiotics and prebiotics.
The products of the first group contain a large number of beneficial bacteria, while the second group promotes the appearance and growth of organisms necessary for the intestinal microflora.
Both probiotics and prebiotics are further classified into several types of drugs.
This is interesting! Latest research!
Testing of probiotics at the Center for Scientific Expertise has proven the various therapeutic value of these drugs. When using probiotics, it is important to ensure that as many beneficial bacteria as possible reach the intestines, but this is difficult given the acidity of the stomach.
The experiment tested more than 10 probiotics, including such popular ones as Linex, Bio-Gaya, Bifi-form. The preparations were immersed in gastric juice (purchased at a pharmacy) for some time, and then the safety of the bacteria was studied after exposure to an acidic environment. Bifi-forms, Enterozermina and Lactovit forte showed satisfactory results . In the Bifi-form capsule, the number of bacteria remained unchanged. The composition of other agents was partially destroyed, but the amount of remaining bacteria was considered sufficient to achieve a therapeutic effect. Other drugs were completely or almost completely destroyed by gastric juice.
The result of the experiment indicates the need to evaluate the acid resistance of probiotics and use only those drugs whose safety after exposure to an acidic environment has been confirmed in the laboratory. For treatment to really bring results, you need to have probiotics prescribed by a doctor.
Products with lactobacilli and bifidobacteria
Among the probiotics containing lactobacilli, there are products in both tablet and powder form.
If you prefer drugs that need to be dissolved in water, then you can use Acylact or Biobacton to restore normal microflora in the intestines of adults.
Preferring to take tablets, it is best to eliminate pathogenic microbes in the digestive system with the help of Lactobacterin.
To eliminate intestinal dysbiosis, you can use suppositories administered rectally.
In terms of their action, they cannot be compared with “Acylact” in powder form, since they do not destroy the beneficial microorganisms already present in the digestive organ.
Both suppositories and all other probiotics are allowed to be used together with antibiotics.
But since probiotics for the treatment of dysbiosis include only one component, these drugs are powerless in protecting the intestinal microflora, which is affected by a huge number of harmful bacteria.
The most diverse category of drugs are probiotics, the main ingredient of which is bifidobacteria. The most famous probiotic is Bifidumbacterin Forte.
However, when taking tablets of this remedy, it is forbidden to be treated with antibiotics. “Bifidumbacterin” is also available in the form of suppositories, used rectally, and a suspension dissolved in water.
A popular powdered probiotic is Probifor.
Anti-dysbacteriosis products containing bifidobacteria and produced in the form of tablets and suppositories cannot be used to treat children under 3 years of age. You should talk to your doctor about using the suspension.
Treatment of intestinal dysbiosis can be carried out using probiotics created on the basis of both lacto- and bifidobacteria.
To restore the balance of microorganisms, the powdered preparation “Florin Forte” is well suited. This product can improve the microflora of both children and adults.
To eliminate dysbiosis in infants, you need to combine the dose of Florina Forte prescribed by the doctor with formula milk. Adults should take this drug with food.
The Linex probiotic contains bifidobacteria and lactobacilli.
Thanks to the beneficial microorganism Enterococcus faecium, also contained in the preparation, the intestinal microflora has a multidirectional beneficial effect.
The drug "Linex" against dysbiosis can be used together with antibiotics and stored outside the refrigerator.
Doctors do not prohibit pregnant women and mothers who are breastfeeding from taking it. “Linex” is recommended to treat even newborn children for microbial imbalance in the intestines.
Symptoms of dysbiosis
The main problem in diagnosing intestinal dysbiosis is the subjective attitude of patients to symptoms and differences in their characteristics. This makes it difficult to compile a medical list of manifestations characteristic of microflora disorders. Most doctors agree that there cannot be intense signs, except in cases of critical imbalance of the flora. In the latter case, we are already talking about infectious diseases (described in international classifications of diseases). The severity of symptoms largely depends on the character and suspiciousness of the patient himself. However, the doctor may suspect intestinal dysbiosis if the patient complains of:
- Discomfort in the abdomen. Some patients are bothered by a feeling of heaviness, rumbling and seething. Unpleasant phenomena do not depend on food intake. However, they intensify after a meal. The patient may report painful sensations that indicate more serious disturbances in the intestines than changes in the composition of the microflora.
- Stool disorders. More often, dysbacteriosis is suspected when a patient has prolonged diarrhea. However, an imbalance of the intestinal flora can be indicated by periodic or regular constipation, alternation of liquid and formed stools, and the presence of impurities in the feces (mucus, greenish streaks). The green color of stool indicates increased proliferation of harmful bacteria.
- Excessive gas formation. Every second patient with dysbacteriosis complains of flatulence, frequent and violent discharge of foul gases, and psycho-emotional discomfort against this background. However, one should take into account the dependence of gas formation in the intestines on the consumption of specific foods (baked goods, vegetables, soda, sweets). Patients often overlook errors in nutrition, attributing disorders to dysbiosis.
- General symptoms. Patients are often concerned about decreased appetite, a feeling of fatigue, lethargy, drowsiness, and muscle weakness. Some patients experience an increase in body temperature, which accompanies inflammatory changes in the intestines due to microflora disorders. Some patients complain of an unpleasant taste in the mouth, dizziness, and mild nausea. Such symptoms may be due to intoxication of the body due to excessive activity of harmful bacteria.
Symptoms of intestinal dysbiosis can appear after consuming specific foods (meat, milk, spices, offal) or bother the patient regularly, regardless of what he eats. The key characteristic of the dysbacteriosis symptom complex is the prolonged and regular manifestation of discomfort (daily, longer than 1 week).
Stages of dysbiosis
Doctors classify dysbiosis into stages based on laboratory indicators. You can also assess at what stage of development dysbiosis is based on specific symptoms. So, the stages of qualitative and quantitative disorders in the composition of the intestinal microflora:
- Initial or compensated stage. Symptoms are absent or appear periodically with bloating, stool disorders, and uneven coloring of stool. The patient's general condition is not impaired, there are no extraintestinal symptoms. The disorders are provoked by a decrease in the number of lacto- and bifidobacteria with an increase in the mass of E. coli.
- The second stage, subcompensated. Disturbances in the functioning of the intestines are manifested by regular flatulence, diarrhea, decreased appetite, inclusions are visible in the feces. The general condition of the patient also changes; periodically he suffers from loss of strength and drowsiness. The condition is caused by a moderate increase in the level of opportunistic bacteria.
- The third stage, decompensated. It manifests itself as pronounced disturbances in the functioning of the intestines, such as enterocolitis. The temperature may rise, chills, nausea, and weakness may occur. The patient is worried about constant diarrhea, flatulence, and lack of appetite. The changes are caused by a significant increase in the level of one or more opportunistic or pathogenic microorganisms.
If the microflora does not return to normal, other signs of the disease appear. For example, symptoms of vitamin deficiency occur (hair loss, brittle nails, peeling skin), anemia, the patient loses weight, and suffers from frequent viral or fungal diseases.
Preparations containing a complex of beneficial bacteria
Most often, intestinal dysbiosis is treated with probiotics, which include not only bifidobacteria, but also other beneficial microorganisms.
A drug with such a wide spectrum of action is powdered “Bifikol”, rich in Escherichia coli bacteria.
Bifiform contains even more microorganisms necessary for the intestines.
This medicine is made in the form of capsules with a protective coating, which allows it to reach the intestines and remain in an acidic environment. "Bifiform", unlike "Bifikol", can be taken together with antibiotics.
In addition, doctors do not recommend using the second drug to treat children under 2 years of age.
Prebiotics rich in lactulose can be used to restore intestinal microflora.
Their main task is to break down the fructose-galactose disaccharide found in the intestinal microflora into simple acids from organic substances.
As a result of this process, blood pressure returns to normal and the activity of harmful microorganisms in the intestines is suppressed.
Medicines that act according to the scheme described above are Duphalac in the form of powder or syrup, Romphalac and Portalac.
They are suitable for treating small children, pregnant women and mothers breastfeeding. But they are contraindicated for anyone who is allergic to fructose and galactose.
Also, the listed medications are not taken against dysbiosis in case of bleeding from the rectum and intestinal obstruction.
If you suffer from diabetes, you can use Duphalac or another prebiotic only after consulting a doctor.
Treatment of the intestines with prebiotic preparations will be effective. These products maintain the balance of microorganisms in the space of the small and large intestines.
These include the drug "Hilak Forte", saturated with the bacteria Lactobacillus acidophilus and helveticus.
In addition to them, this medicine for restoring normal intestinal microflora is rich in lactic acid, which leads to an acceptable level of acidity in the gastrointestinal tract.
The drug "Hilak Forte" is unique in that it contains short-chain fatty acids, the task of which is to put the intestinal microflora in order.
The fact is that these substances have a positive effect on tissue repair processes on the walls of the digestive organ and regulate water and electrolyte balance.
The drug "Hilak Forte" is used to treat illnesses associated with microbial imbalance in the intestinal microflora in both adults and children.
There is no need to stop using this remedy if you are taking antibiotics.
Causes of imbalance between beneficial and harmful microbes
The main manifestation of intestinal dysbiosis or dysbiosis is a violation of the composition of the microflora, with an increase in the number of opportunistic and pathogenic microorganisms with a parallel decrease in the number of beneficial bacteria. There are many prerequisites for shifting the balance. Almost any of the somatic diseases entails disturbances in the functioning of the digestive system, dysfunctional disorders, which necessarily leads to a change in the composition of the microflora as a secondary condition.
Dysbacteriosis develops against the background of:
- Chronic and acute pathologies of the gastrointestinal tract. Disturbances in the functioning of the stomach and duodenum lead to changes in acidity in the intestines, which already negatively affects the flora. Pancreatic insufficiency leads to the ingestion of incompletely broken down products into the large intestine, which provoke the processes of rotting and fermentation, with subsequent displacement of the microflora. Disturbances in the functioning of the gallbladder lead to insufficient flow of bile into the intestinal lumen or disruption of its properties; in such conditions, the main factor eliminating pathogenic microorganisms from the intestine is missing.
- Severe systemic diseases. Immunodeficiency states, bone marrow disorders, viral pathologies and cancer lead to suppressed immunity and many other dysfunctions, causing the intestinal microflora to suffer.
- Taking medications. The main provocateurs of dysbiosis are considered to be antibiotics, which destroy not only harmful, but also beneficial microorganisms in the intestines. However, changes in microflora may accompany the use of any other medications that affect the functioning of internal organs, the immune system, and the gastrointestinal tract in particular. Anticoagulants, NSAIDs, and hormonal drugs can provoke dysbacteriosis.
- Infectious diseases. Pathogenic microbes that enter the body in large quantities can provoke inflammatory changes in the gastrointestinal tract. Infectious gastroenterocolitis is accompanied by dysfunction of the entire intestine. In conditions of severe diarrhea and massive fluid loss, as well as general weakening of the body, favorable conditions arise for the proliferation of bad microbes.
- Poor nutrition. For the normal functioning of the intestinal microflora, it is important to receive certain types of nutrients in balanced quantities. When healthy eating rules are violated and carbohydrate or protein foods predominate in the diet, those microbes for which more nutrients are available multiply intensively. Dysbacteriosis can be caused by regular consumption of alcohol, spicy foods, fatty foods, and some spices.
It is characteristic that in some people even the influence of one factor leads to intestinal dysbiosis, while in others the confluence of several provocateurs does not immediately cause negative consequences in the composition of the microflora. This is due to the individuality of the human body. Compensatory and protective mechanisms are different for everyone, and provocateurs act with different intensities, which determines the variability of reactions.
The best medications against intestinal dysbiosis
The tablets, syrups and powders mentioned before are not all the means that can be used to treat small children and adults.
The products included in the following list will also help cope with dysbiosis:
- "Acipol";
- "Bacteriophage";
- "Bifidum-Multi-1,2,3";
- "Kipferon";
- “Normospectrum” (separately for adults and children);
- "Polysorb";
- "Festal";
- "Enterosgel".
The active ingredients of these drugs are directed against intestinal dysbiosis or perform preventive tasks.
But, of course, not all of them can be taken together with antibiotics and given to children. Therefore, the question arises: which drug copes best with microbial imbalance?
Tablets or powder for treating the intestines are evaluated according to the parameters presented in the list below:
- coating with a special coating that does not allow the drug to break down before it enters the intestines;
- the ability to treat even infants with it;
- existing contraindications for use;
- side effects caused by the drug;
- compatibility with antibiotics;
- possibility of use during the period of bearing or feeding a child;
- storage requirements.
A drug such as Lactobacterin, produced in the form of tablets and powder, does not have a special protective shell, is not used for hypersensitivity and candidiasis and can cause allergies.
But it is allowed to be used together with antibiotics and given to children, pregnant and nursing mothers. Lactobacterin should be stored in a dry place at a temperature of 2 to 8 degrees Celsius.
Video:
The popular product "Acilact", which has 2 forms - tablets and suspension, also lacks a capsule coating and is prohibited for those who suffer from hypersensitivity and candidiasis.
Unfortunately, it can trigger allergic reactions. "Acilact" can be taken in combination with antibiotics.
But pregnant women and nursing mothers should use this remedy with caution, after consulting with a doctor.
The well-known “Bifidumbacterin”, which does not have a capsule shell and is not approved for use in candidiasis and hypersensitivity, is recommended for use only when prescribed by a doctor.
This drug may cause allergies and is not intended for use in children under 3 years of age. "Bifidumbacterin" should be stored at a temperature of 2 to 10 degrees.
“Hilak Forte” differs from the listed drugs against intestinal dysbiosis.
Although this remedy is devoid of a protective shell, it does not lead to allergies and is well tolerated by those who suffer from candidiasis and hypersensitivity.
It can be used together with antibiotics and given to children and pregnant women.
Video:
But the best in this regard is Linex, since it has a special shell, is used together with antibiotics and is suitable for children.
So, there are a variety of remedies against microbial imbalance in the intestines. The list given in the article indicates the most effective ones.
But they should be used only after consultation with a doctor and strictly according to the instructions, because each drug has its own characteristics.
When treating intestinal dysbiosis in adults, the drugs and regimens that are used for this have characteristic differences and are designed to restore the microflora. In the human intestine, the microbiocenosis consists of 2500 species of different bacteria, which are in dynamic equilibrium and are included in the vital activity of the body. Disturbance of this balance is dysbacteriosis. When the balance is disturbed, not only the processes of transformation and absorption of food undergo changes, but also the effectiveness of immune processes decreases. There are physiological development-related differences between the composition of the intestinal microflora in adults and children.
Diagnostics
If you have signs of bowel dysfunction, you should consult a general practitioner or gastroenterologist. The specialist will listen to all the patient’s complaints, ask questions to collect anamnesis and clarify symptoms, and then conduct an examination. Often, palpation and percussion examination of the abdomen is enough to identify foci of inflammation in the intestines or suspect other pathologies.
To collect information about the patient’s health status, the following is prescribed:
- general and biochemical blood test (reflect the presence of inflammatory reactions, the ratio of vitamins and minerals in the body);
- coprogram (study of the physicochemical properties of feces);
- bacterioscopic examination of feces.
The latter analysis provides only approximate information about the composition of the intestinal microflora and is considered insufficiently accurate. The fact is that the composition of bacteria in the intestinal lumen (and in feces, respectively) is radically different from the composition of the mucoid microflora, therefore the results of bacterioscopy in 90% of cases reflect dysbacteriosis.
If, during the collection of anamnesis, the doctor did not see the prerequisites for a shift in the balance of microflora, and the symptoms of intestinal disorders persist for a long time and do not respond to classical therapy, further instrumental examination will be required to determine the reasons. They may prescribe irrigoscopy, colonoscopy, gastroduodenoscopy. Examinations make it possible to study the condition of the mucous membranes of the gastrointestinal tract, identify organic changes in them, and take material for histological or bacterioscopic examination, which provides more accurate diagnostic results. However, all procedures are quite unpleasant, and therefore are used only as a last resort, when there are suspicions of more significant pathologies.
This is interesting! Modern microbita analysis
Useful information: Intestinal colitis: more than 5 symptoms, treatment (25 drugs) in adults, diet.
A new drug for intestinal pain The microflora of the small intestine, which includes not only bacteria, but also viruses and fungi, plays a special role in shaping human health. Recent studies have shown that they form a special film on the surface of the gastrointestinal tract, and do not float in the intestinal lumen, as was previously believed. It is thanks to this microbiota that food is digested, vitamins and minerals are absorbed, and human immunity is formed due to this.
Scientists have taken up the question of how to determine the composition of such a film. After all, the usual analysis for dysbacteriosis shows only those bacteria that are in the lumen. As a result, a method was developed to identify markers of microbes that shape the intestinal biota. A blood sample is taken, in which fatty acids specific to each microbe are determined. Then, using a special catalog, the exact composition of the intestinal microflora is determined.
The results display 5 variants of dysbiosis:
- Simply a deficiency of normal intestinal flora. In this case, taking pre-, meta- and probiotics is sufficient for treatment.
- 2. SIBO (bacterial overgrowth syndrome) is an overgrowth of both opportunistic and friendly flora. Suppressive therapy is needed here.
- 3. CIGR (fungal overgrowth syndrome) is the overgrowth of fungi, followed by viruses. An antifungal protocol is needed.
- 4. Mixed (SIBO + CIGR).
- 5. Imbalance of opportunistic flora against the background of reduced normal flora.
These are the latest studies and recommendations, on the basis of which the most advanced gastroenterologists provide treatment.
Treatment regimen for the disease
Treatment of intestinal dysbiosis in adults is carried out in stages and begins with eliminating the causes that caused the imbalance. Normalization of nutrition, lifestyle correction, review of methods for treating systemic diseases is the initial stage of preparation for the treatment of dysbiosis. The treatment regimen for dysbacteriosis itself consists of several stages:
- the use of medications aimed at destroying pathogenic microorganisms;
- colonization of the intestine by microorganisms included in the normal microbiocenosis;
- achieving and maintaining the balance of natural microflora;
- restoration of intestinal functions;
- strengthening the immune status of the body.
In each case, an individual approach to the choice of medication is assumed, which depends on the composition of the pathogenic and the amount of endogenous microflora.
The YouTube ID of Ojpdh—dQn4 is invalid.
Natural analogues of drugs
To cure dysbiosis, avoiding taking a large number of pharmaceutical medications, you can resort to consuming natural sources of beneficial bacteria - familiar foods.
Food products related to prebiotics
Foods rich in prebiotics :
- fermented milk products (ryazhenka, kefir, cottage cheese);
- chicory (raw root);
- cereals, wheat bran;
- raw asparagus;
- dried apricots, prunes;
- fruits (apples, citruses, bananas);
- berries (strawberries, black and red currants, plums).
Products containing sufficient amounts of probiotics and synbiotics :
- flax seeds;
- corn;
- figs;
- grape;
- sauerkraut;
- bulb onions;
- soft cheese, cottage cheese, fermented baked milk.
Antiseptic products :
- onion and garlic;
- cardamom;
- ginger root;
- dill and fennel (seeds and herbs);
- walnuts, hazelnuts and almonds;
- rowan, blueberry and other berries with a tart taste
Nutrition for dysbiosis
Antibiotics and bacteriophages
In order to cleanse the intestines of pathogenic microorganisms, antimicrobial and antimycotic drugs are used.
Antimicrobial agents include antibiotics of various groups:
- tetracycline series - Tetracycline, Minocycline, Doxycycline, Vibramycin, Doxal, Tetradox, etc.;
- penicillin - Amoxicillin, Flemoxin Solutab, etc.;
- cephalosporins - Cefoperazone, Cefpirome, Ceftobiprole, Cefotaxime, etc.;
- quinolone group - Gemifloxacin, Sitafloxacin, Moxifloxacin, Ciprofloxacin, Lomefloxacin, etc.;
- aminoglycosides - Amikacin, Farcycline, Neomycin, Garamycin, etc.;
- Metronidazole;
- Rifaximin;
- Alpha Normix et al.
Antimicrobial drugs can aggravate dysbiosis, reducing the amount of not only pathogenic, but also endogenous microflora. Therefore, antibiotics are prescribed either selectively, purposefully destroying certain types of pathogens, or when the absorption and motor function of the intestine is impaired, characterized by the growth of pathogenic microbes in the cavity of the small intestine. For dysbiosis of the large intestine, the following drugs are used: Intetrix, Nitroxoline, Ersefuril, etc. These drugs effectively destroy staphylococci, yeasts and Proteus, without having a significant effect on the natural biocenosis.
For staphylococcal infections that cause dysbacteriosis, they are treated with: Oxacillin, Nevigramon, Co-Trimoxazole, Tarivid, Palin, etc.
The drugs mainly prescribed are III and IV generation cephalosporins, which have fewer side effects than their predecessors. The course of antibiotic use should not exceed 5-7 days. The dosage is calculated individually.
To remove decay products of pathogenic microorganisms, their toxins and other waste products from the body, sorbents are prescribed along with antibiotics: Polysorb, Enterosgel, White Coal, Filtrum-STI, etc.
Currently, preparations of live bacteriophages are becoming increasingly popular in the treatment of intestinal dysbiosis. They are represented by several types of bacteria that parasitize inside bacterial cells, which leads to the death of pathogenic microbes. In nature, bacteriophages are natural regulators of the number of pathogenic microorganisms.
Bacteriophages are produced in different pharmacological forms. The name of the drug corresponds to the pathogenic organism in which the bacteriophage parasitizes. Thus, pseudomonas, staphylococcal, dysentery and streptococcal phages already exist. Preparations can contain only one of the strains of bacteriophages: Salmonella, Coli-bacteriophage, Proteus bacteriophage, Pseudomonas bacteriophage, etc. Complexes containing several types of bacteriophages are also produced: Intesti, Piobacteriophage polyvalent, Sextaphage, etc. Preparations are an effective and safe alternative to antibiotics.
The role of intestinal microflora
Normal intestinal biocenosis consists of anaerobic (lacto- and bifidobacteria, bacteroides, fusobacteria, cocci, clostridia, veillonella) and aerobic bacteria (staphylococci, streptococci, E. coli, Klebsiella, Proteus, yeast-like fungi, etc.). In total, about 500 species of bacteria live in the intestines. The ratio of anaerobes to aerobes is 10:1. In total, in the thickness and on the walls of the intestine there are from 1 to 2.5 kg of microorganisms, which consume about 10% of the energy produced by the body and about 20% of the nutrients that enter it.
Normal intestinal microflora is represented by three groups of microorganisms, the number of which must be balanced and constant:
- the main microflora (or obligate) makes up 90-95% of the total mass of microbes, represented mainly by anaerobes (bifidobacteria and bacteroides);
- accompanying flora makes up 5% of the total number of microorganisms, represented by lactobacilli, cocci, E. coli;
- facultative or residual microflora (or opportunistic), the mass does not exceed 1% of the total biocenosis, represented by Pseudomonas aeruginosa, Candida, staphylococci, Proteus, campylobacteria.
Representatives of intestinal normobiocenosis are divided according to the time of presence in its lumen. Thus, obligate microflora refers to permanent microflora, opportunistic microbes are considered non-permanent microflora, and pathogenic microflora are considered transient or random. Microflora is also divided into mucoid (closely associated with the epithelial cells of the intestine and living on the surface of its walls) and cavitary - found in liquid and viscous masses in the intestinal lumen.
Each type of bacteria performs its own tasks in the intestines. Thus, Proteus, bacteroides and clostridia are involved in the digestion of proteins and belong to the proteolytic group of bacteria. Enterococci, lacto- and bifidobacteria are involved in the processing of sugars, and therefore are called saccharolytic bacteria. The most important functions of normal intestinal microflora:
- Digestion. Microbes participate in the breakdown of carbohydrate and nitrogen-containing substances, provide deconjugation of fatty acids, neutralize chemicals entering the body, and produce some essential amino acids.
- Synthesis of vitamins. Only beneficial bacteria can synthesize vitamin K and B vitamins. They are necessary for normal metabolism and the full course of biochemical reactions.
- Protection of the body. Mucoid bacteria tightly cover the intestinal mucosa, preventing the penetration of dangerous microbes through them; they compete with potentially dangerous bacteria for nutrients, thereby reducing their numbers in the intestinal lumen. In addition, beneficial microflora produces antibacterial substances and provides nonspecific protection for the body, and also takes part in the synthesis of some immunoglobulins.
Beneficial bacteria stimulate the regeneration process of the intestinal mucosa. They also neutralize endo- and exogenous metabolites.
Prebiotics with probiotics and symbiotics
The next step in the fight against dysbiosis is the colonization of the intestines with strains of microorganisms of natural microflora. For this we use:
- prebiotics;
- probiotics;
- symbiotics.
Probiotic preparations consist of living organisms that have a stabilizing and function-optimizing effect on the natural intestinal microflora. They are divided into:
- Multicomponent (Linex, Bifikol, Bifiform), which includes a complex of beneficial microorganisms - colibacteria + bifidobacteria + lactobacilli.
- One-component (Bifidumbacterin, Lactobacterin, Colibacterin). From the name of the medicine it becomes clear which strain is included in the composition.
- Combined (Rioflora immuno, Bificol, Florin Forte, etc.) - a complex of bacteria that are not susceptible to antibiotics, stimulates the growth of natural microflora.
Probiotics contain high doses of microorganisms, so people with severe forms of immunodeficiency or prone to allergic reactions should consult a doctor before consuming eubiotics. Some types of probiotics cannot be combined with antibiotics, as they reduce the effectiveness of eubiotics.
Prebiotics are preparations in which certain substances undergo fermentation in the large intestine and the fermentation products stimulate the growth of beneficial microflora of the large intestine. Stimulation occurs selectively, mainly prebiotics stimulate the vital activity of bifidobacteria and lactobacilli.
Preparations with prebiotic action include: Normaze, Goodluck, Duphalac, Lactusan, Exportal, Bifiliz, etc. Dietary supplements with the same effect are produced: Prelax, Lactusan, Maxilak, etc. Since prebiotics are part of a food product that is not absorbed by the body, then they do not cause side effects and can be used not only for treatment, but also for preventive purposes.
Symbiotics are drugs that rationally combine probiotics and prebiotics. Prebiotics help probiotics pass through areas of the intestine with an aggressive environment, and then, as a nutrient substrate, allow them to populate the distal parts of the digestive system with beneficial microflora. The group of symbiotics includes: Bifidobac, Laminolact, Maltidophilus, etc.
The course of drugs ranges from 14 days for pro- and prebiotics and 21 days for symbiotics. Despite the safety and naturalness of the drugs, they must be used as prescribed by a doctor and in the dosage prescribed by him.
Is it possible to get rid of dysbiosis?
Therapy for dysbiosis is aimed at eliminating excess pathogenic microbes in the intestines, colonizing beneficial microorganisms, and creating favorable conditions for their reproduction. In addition, treatment should restore the digestion process, normalize the protective and absorption functions of the intestine, optimize the supply of nutrients, and restore immunity. This will require an integrated approach, which includes the use of antibacterial drugs, products based on beneficial bacteria, normalization of the patient’s diet and lifestyle.
Medicines for harmful bacteria
They are prescribed by a doctor taking into account the results of bacterioscopy and the sensitivity of bacteria to certain antibiotics. Most often, broad-spectrum drugs from the group of antibiotics or antimicrobial agents are prescribed. The course of treatment lasts 7-10 days and precedes the use of other drugs for the treatment of dysbiosis. Most commonly prescribed medications:
- Alpha-Normix (1 tablet 3 times a day for 7 days);
- Furadonin (1 tablet 2 times a day for 5-7 days);
- Nifuroxazide (1 tablet 3 times a day for up to 10 days).
This is interesting!
To selectively suppress pathogenic microorganisms, it is possible to use special bacterial preparations (only after obtaining the results of bacterioscopy). These include bacteriophages. These products contain a sterile filtrate of phagolysate of certain bacteria, which can accumulate and stimulate the lysis of a specific microorganism or several species at once. Most often, Intesti-Bacteriophage, staphylococcal, pseudomonas, etc. are prescribed. The course of treatment lasts 7-20 days, during which the drug is taken 20-30 ml 3 times a day (the dose must be adjusted by the doctor).
Medicines with beneficial bacteria
To restore normal intestinal biocenosis, agents from the groups of probiotics and prebiotics are prescribed. Combinations of these drugs are most effective.
Probiotics include medications that contain one or more types of living beneficial bacteria protected by an acid-sensitive membrane. They are important both for populating beneficial microflora in the intestines and for suppressing the proliferation of opportunistic microorganisms. Lacto- and bifidobacteria increase the acidity in the intestinal environment, which adversely affects the activity of potentially dangerous microorganisms, but has a positive effect on the rate of reproduction of beneficial bacteria. Probiotics can be mono- or polycomponent (contain 1 type of bacteria or several).
Most often prescribed:
- Linex (2 capsules 3 times a day, 7-14 days);
- Acidolac (2 sachets 3 times a day, 7-14 days);
- Biosporin (2 sachets 3 times a day, 2-3 weeks).
Prebiotics are drugs of non-bacterial origin. They contain substances that change the acidity in the intestines, or can be used by beneficial bacteria as a substrate for growth and reproduction. The most popular of them:
- Hilak-Forte (30-50 drops mixed with water 3 times a day, 2-3 weeks);
- Duphalac (5-15 ml 1 time per day on an empty stomach, 500 ml per course);
- Normaze (5-15 ml 1 time per day on an empty stomach or 5 ml 2 times per day).
Other drugs
In the complex therapy of dysbiosis, agents that are not related to bacteria can also be used. For example, as symptomatic therapy for severe discomfort in the intestines or to eliminate the consequences of its improper functioning.
To eliminate pain or stinging due to bloating, antispasmodics and drugs against increased gas formation are prescribed. The first include Duspatalin, Mebeverine, No-shpu, Buscopan. To eliminate excess gas, simethicone-based products are prescribed (Espumizan, Espusin, Meteospasmil). Drugs of this kind are taken in a short course until the disturbing symptom disappears.
Against the background of antibiotic therapy for advanced dysbiosis, the use of sorbents may be required. These products eliminate waste products of pathogenic bacteria, alleviate the toxic load on the body, and relieve signs of general intoxication. For this purpose, Enterosgel, Sorbex, Atoxil are prescribed. Sorbents are also taken in the shortest possible courses, up to 5 days.
For severe digestive disorders, enzyme and choleretic drugs are prescribed. The first include Creon, Pangrol, Pancreatin. They optimize food processing and eliminate favorable conditions for rotting and fermentation in the intestines. Choleretic drugs (Karsil, Allochol) promote normal bile production, improve its antiseptic properties, and normalize the permeability of the intestinal wall.
Symptomatic therapy
To normalize intestinal functions, medications are used that are prescribed by a gastroenterologist. The use of vitamin complexes and microelements is mandatory. A number of medications are also used to reduce the symptoms of the disease:
- for diarrhea, antidiarrheal agents are used - Attapulgite, Baktisubtil, Bifikol, Gastrolit, Diosmectite, Intetrix, etc.;
- for the treatment of constipation - Lavacol, Fortrans, Tranzipeg, Senalex, Guttalax, Glycelax, etc.;
- antispasmodics to relax the bile ducts - No-shpa, Duspatalin, etc.;
- choleretic drugs - Hofitol, Allohol, Peridol, Holagol, Tanacehol, etc.;
- enzymatic - Creon, Mezim, Festal, etc.
All medications must be taken according to the instructions, individual recommendations and in compliance with the regimen.
Most often, medications for dysbiosis are probiotics and prebiotics. Other types of drugs are prescribed in case of serious damage to the body as a result of dysbacteriosis and its severe forms.
If you have intestinal dysbiosis, it is important to follow a diet, as some foods complicate the effect of drugs or impede intestinal function.
Treatment of dysbiosis should begin when the first symptoms of the disease appear. If the condition cannot be corrected with nutrition, then you need to contact a gastroenterologist and begin the recommended treatment. In the initial stage, the body’s biocenosis system is quickly restored. In an advanced state, dysbiosis takes much longer and is more difficult to treat.
Many modern doctors believe that intestinal dysbiosis is not an independent disease at all, but its presence in many children and adults cannot be denied.
Symptoms of this disease occur in people of different genders and ages.
Despite this prevalence of pathology, many doctors experience serious difficulties in making an accurate diagnosis and choosing a treatment regimen.
Causes
There are many causes of dysbiosis, among which a number of provoking factors are noted:
- Diseases of the gastrointestinal tract;
- Therapy with antibacterial drugs;
- Treatment with medications, including hormonal and anti-inflammatory non-steroidal drugs;
- Conducting radiation and chemotherapy;
- Dietary disorders;
- Unstable psycho-emotional state, stress, depression;
- Changes in the body due to age and physiology;
- Impact of viral and respiratory diseases;
- Eating low-quality food, poorly purified water, poor environmental conditions;
- Infections in the intestines;
- Overstrain of a mental and physical nature.
This condition must be treated comprehensively. To do this, it is important to consult a doctor in time and establish the cause of dysbiosis.
The doctor will conduct a number of diagnostic measures and refer you for laboratory tests. Based on the results, he will prescribe the right treatment.
What symptoms accompany the disease?
The most noticeable symptoms of intestinal dysbiosis include manifestations of various intestinal disorders.
As a rule, people do not attach importance to these signs, and therefore the disease often becomes chronic.
Also, the treatment regimen for intestinal dysbiosis in adults must necessarily include the use of bacterial preparations that contain live cultures.
Treatment of symptoms of intestinal dysbiosis in adults should be carried out within 2 months. In addition, it is imperative to prescribe medications that help restore normal motor skills.
Symptoms and treatment of dysbiosis require careful attention. It is impossible to effectively treat this disease without following a special diet.
There is also a need to stimulate the body's reactivity.
Treatment of dysbiosis in women is practically no different from the treatment method in men. However, the presence of concomitant ailments must be taken into account.
If a violation of the microflora in the intestines is accompanied by vaginal dysbiosis, the use of additional drugs is indicated - usually special suppositories, gels or ointments are used.
Understanding the concept
Intestinal dysbiosis is a clinical and laboratory syndrome that accompanies qualitative and quantitative disturbances in the composition of the intestinal biocenosis. The term has been in use since 1916. Initially introduced into medical terminology to refer to symptoms of intestinal dyspepsia (rotting and fermentation processes) by the German physician Nissle.
Disruption of microflora provokes disturbances in the functioning of the adaptive, compensatory and protective mechanisms of the intestine. This is expressed in a decrease in the number of beneficial microbes in favor of opportunistic (potentially dangerous) and pathogenic (disease-causing) ones.
According to statistics, 90% of the population experience symptoms of dysbiosis in the gastrointestinal tract at least once in their lives. Microflora disorders can occur in women and men with the same frequency. Due to the natural imperfections of the gastrointestinal tract, dysbiosis most often manifests itself in children in the first year of life.
Drug treatment
Treatment of dysbiosis with drugs must necessarily be comprehensive. In this case, the following medications for intestinal dysbiosis are usually used:
- Prebiotics. These substances are not digested, but create a favorable habitat for obligate flora. These include lactulose, inulin, galactose and other oligosaccharides. The listed substances are found in fairly large quantities in dairy and cereal products. Drugs for intestinal dysbiosis such as Duphalac, Normaze, Lactusan are available in pharmacies;
- Probiotics. These tablets contain live cultures of bacteria. There are monocomponent products that contain one representative of obligate microflora - bifidumbacterin, colibacterin, lactobacterin. Treatment of dysbiosis with such drugs usually lasts for a month to a month and a half. You can also treat with inexpensive drugs for intestinal dysbiosis - multicomponent drugs or symbiotics. They contain several representative obligate flora. These products include Linex, Bifiform, Bificol. Treatment lasts about 2 weeks;
- Antagonists. These drugs for the treatment of intestinal dysbiosis include bacteria that do not belong to the obligate flora, but can suppress the proliferation of opportunistic microorganisms. These include enterol, bactisporin, bactisubtil. Their treatment lasts for a week;
- Combined drugs. This remedy for intestinal dysbiosis, in addition to obligate flora, contains substances that have an immunomodulatory effect. These include acipol and bifiliz. Treatment takes 10-14 days;
- Synbiotics. This is an effective remedy for intestinal dysbiosis, which contains obligate flora and a prebiotic. These include maltidophilus, laminolact, bifido-bak. Treatment should last at least three weeks;
- Intestinal antiseptics. These drugs are almost not absorbed, but at the same time they suppress the proliferation of pathogenic microorganisms without affecting the main flora. The best remedy for intestinal dysbiosis in this category is Intetrix. Prescribed course for 3-5 days;
- Antibacterial drugs. Antibiotics for intestinal dysbiosis are prescribed exclusively for established forms of the disease. At the same time, it is very important to take into account the sensitivity spectrum of the microorganism to antibiotics;
- Bacteriophages. To eliminate the symptoms of dysbiosis, you can take medications containing viruses that attack a specific type of bacteria. They are combined with antibacterial treatment or used as an alternative therapy.
An effective topical remedy is suppositories against dysbacteriosis. They are administered rectally and act directly on the rectum.
Treatment
How to treat adults with medications
When trying to cure dysbiosis, only complex therapy, a regimen developed by a gastroenterologist, gives a stable result. The main task is to eliminate the root cause - that is, the primary treatment of the underlying disease that caused a pathological imbalance of the bacterial flora.
Basic goals of therapy:
- suppress the reproduction and activity of harmful microbes;
- remove from the body toxins released by pathogenic microflora, poisons formed during putrefactive processes;
- normalize the contractile and absorption function of the intestine (in case of periodic diarrhea and constipation);
- eliminate favorable environments and opportunities for the development of pathogenic microorganisms;
- restore populations of natural intestinal bacteria and maintain stimulating conditions for their growth;
- increase the body's immune defense;
- bring to normal the ratio between macro- and microelements, preventing the development of dysbacteriosis;
- carry out anthelmintic treatment in case of intestinal colonization by parasites.
Beneficial and harmful bacteria living in the intestinal lumen
Main groups of drugs
Antibacterial
Suppress abnormal growth and activity of microbes when the cause of dysbiosis is enterococcal infection, candidomycosis, Escherichia coli, staphylococci, streptococci.
Depending on the identified pathogen, the following are prescribed: Levomycetin, cephalosporins (do not act on enterococci and listeria), Nystatin, Pimafucin, Enteroseptol, Azithromycin.
But antibiotics very often disrupt eumicrobiosis - the natural microflora in the large intestine, so they are used for a course of 7 - 10 - 14 days only for pathologies accompanied by active growth of microbes in the small intestine.
Important!
Antibiotics should be prescribed only after a bacterial culture test has been carried out, when the pathogen is identified and its sensitivity to various agents is determined, choosing the most optimal one.
Treatment with antibiotics of the underlying disease - the cause of intestinal dysbiosis - should be accompanied by simultaneous intake of probiotics (approved for use together with antibacterial agents), as well as Wobenzym, Phlogenzyme with highly active bioenzymes, which minimize the likelihood of developing “side effects” and drug-induced dysbiosis.
Antimicrobials
If dysbacteriosis is confirmed, antiseptic medications are prescribed that have minimal effect on the natural intestinal flora, promoting the breakdown and absorption of substances necessary for the body and at the same time suppressing the activity of aggressive microbes, proteas, and yeast fungi. These include: Furazolidone, Ersefuril, Tiberal, Intetrix.
For severe staphylococcal dysbiosis, Tarivid, Palin, Metronidazole, Biseptol, Nevigramon are prescribed.
Rectal antibacterial, antimicrobial, antimycotic suppositories act locally, maximally preventing side effects, while maintaining effectiveness in dysbacteriosis of any complexity. In addition, some suppositories contain corticosteroids that relieve inflammation and swelling of the intestinal walls.
Of these, they include: Metronidazole, Canesten, Genferon, Levomycetin.
But antibacterial suppositories are not allowed to be used by women carrying a child.
Probiotics (eubiotics)
Available in ampoules, bottles, powder, suppositories, tablets, they contain a large volume of living natural bacteria that suppress pathological microbes and actively colonize the intestines.
| Type of probiotics | Probiotic Base | Name | Peculiarities |
| Single drugs. In case of severe dysbacteriosis, they are used only in combination with others, since they contain the same type of active substance | lactobacilli | Trilact, Acylact, Acidobak, Biobakton, Gastrofarm, Primadophilus, Lactobacterin, Regulin Narine; Biobakton, Rela Life Euflorin-L | Compatible with antibiotics |
| bifidobacteria | Bifidumbacterin forte, Biovestin, Probifor, Bifidobacterin-Multi, Bifidum-BAG, Bifilong | Not compatible with antibacterial agents | |
| Polycomponent symbiotics, combining several types of beneficial and non-pathogenic species of bacteria | combination of bifidobacteria and lactobacilli | Florin Forte, Normobakt, Bacteriobalance, Biovestin-Lacto, Bifidin, Bonolact Pro+Biotik, Polybacterin, Symbiolact | Not recommended for people with increased allergic sensitivity or severe immunodeficiency (dosage calculation required) |
| lacto- and bifidobacteria, natural enterococci | Linex | Used together with antibiotics, approved for lactating and pregnant women | |
| bifidobacteria in combination with non-pathogenic Escherichia coli | Bificol | Not compatible with antibiotics | |
| bifidobacteria, non-pathogenic enterococci | Bifiform | Combined with antibiotics; allowed for pregnant and lactating women |
In addition to them, multicomponent probiotics Enterol, Bifidoback, Acipol, and Yogulact are actively used.
Combined probiotics, in addition to normal flora bacteria, often contain:
- substances that maintain a favorable environment for their growth: soybean and propolis extract in Bioflora, immunoglobulins in Kipacid, lysozyme in Bifiliz;
- enterosorbents such as activated carbon, SUMS-1: Ecoflor, Probiofor, Bifidobacterin-forte, Bificol forte (so-called probiotic complexes);
- bacteria that do not live in the intestines, but suppress the vital activity of pathogens (the so-called self-excreting antagonists), which are found in Sporobacterin, Baktisubtil, Enterol.
Probiotics can be used not only in the form of capsules, powder, tablet form, but also in suppositories. The advantages of suppositories Bifidumbacterin, Bifinorm, Lactonorm, Lactobacterin, used rectally, lie in their local effect, which makes it possible to regulate the balance of microflora locally - in the intestines, without affecting the body as a whole. In addition, bifidobacteria and lactobacilli immediately enter favorable conditions for them, without moving through the gastrointestinal tract for a long time and without being destroyed.
Video. How to treat dysbiosis
Prebiotics
Unlike probiotics, prebiotics do not contain natural bacteria, but create an environment for the active reproduction of beneficial microorganisms and are used at any stage of the treatment of dysbiosis.
They are produced in the form of medicines and biologically active additives (dietary supplements). Most contain lactulose, which activates the growth of natural bifidobacteria and stimulates the immune system.
Lactulose-containing prebiotics Duphalac, Normaze, Romphalac, Portalac, Goodluck, Lactusan, Lactofiltrum are allowed for pregnant women and infants. Contraindicated for those with fructose or galactose intolerance, those suffering from diabetes mellitus, intestinal obstruction, or intestinal bleeding.
Other effective prebiotics include Hilak forte, Baktistatin, Ortho Prebio.
Hilak forte is a universal prebiotic for any age, indicated during pregnancy and lactation. Restores the natural intestinal flora, epithelial cells of the intestinal mucosa, normalizes acidity.
Bactistatin contains active antibacterial substances (bacteriocins, lysozyme) that suppress intestinal pathogens; digestive enzymes. Stimulates the synthesis of interferon, increasing protective functions, absorbs and removes poisons and allergens, reducing intoxication; normalizes intestinal motility, provides conditions for the restoration of healthy microflora.
The new prebiotic Ortho Prebio (Raftilose Synergy1) contains acacia gum, natural inulin, enriched with oligofructose. Actively “grows” the natural healthy intestinal microflora, increasing up to 10 times in 10 days. Works much more effectively than many similar drugs.
Synbiotics
Representatives of medicinal synbiotics contain a complex of pro- and prebiotic components.
Among them we can highlight:
- Bifainol (bifidobacteria in combination with vitamins and eicosapentaenoic and docosahexaenoic acids);
- Bifidumbacterin 1000 (lactulose with bifidobacteria);
- Evitalia (lacto- and propionobacteria with lactic acid streptococcus);
- Normoflorin-D (lactobacteria with bifidobacteria and lactitol);
- Normoflorin-D (bifidobacteria and lactobacilli with lactitol);
- Bion - 3 (lacto- and bifidobacteria with a vitamin-microelement complex);
- Maxilac (fructooligosaccharides with bifidobacteria and lactobacilli);
- Algibif (bifidobacteria with sodium alginate).
Photo gallery. Basic pro- and prebiotic medications
Linex Bactistatin Acylact Bifiform Lactofiltrum Bificol Lactobacterin
How to choose the best
Since certain strains of bacteria and complexes of active organic substances, taking into account their properties, are purposefully used for specific manifestations of the disease, the specialist selects the optimal probiotic or prebiotic drug for the treatment of a specific form of dysbiosis.
To relieve diarrhea, probiotics with saccharomycetes (Enterol), or beneficial bacilli, which are found in Bactisubtil and Biosporin, are optimal.
The doctor chooses a medicine after reviewing the results of a stool test. And usually the best option is a probiotic containing those organisms that are deficient in the intestines.
When treating dysbacteriosis, a drug with lactobacilli is first taken, then a drug containing bifidobacteria is taken, and sometimes after this drugs with colibacteria (Colibacterin) are also prescribed. It is often advisable to take symbiotics containing a combination of bacteria necessary for the intestines.
General rules for use and duration of treatment
Prebiotics are drunk 3-4 times a day with food until the condition is stable and negative manifestations subside. It is allowed to drink them for quite a long time - months.
Probiotics are usually taken half an hour to an hour before meals with the same frequency as prebiotics, but the duration of administration is approximately 2 - 4 weeks. However, in case of acute intestinal infection with severe diarrhea, their intake for 3–4 days is increased to 6 times a day until the diarrhea stops.
Important!
In case of increased gastric acidity, 10–15 minutes before taking the prescribed probiotic, it is advisable to drink half a glass of alkaline mineral water or take acid-reducing agents (Phosphalugel, Almagel, Maalox, Gastal).
Bacteriophages
Like antibiotics, these drugs are aimed at eliminating bacteria, but unlike antibacterial agents, they are not toxic and selectively suppress only certain microbes, without affecting the healthy intestinal flora. An analysis of stool for dysbacteriosis will allow you to accurately select the desired bacteriophage, taking into account the susceptibility of specific pathogens to it.
Some bacteriophages acting on specific microorganisms that provoke dysbacteriosis:
- staphylococcus: Piopolyphage (tablets), Staphylococcal bacteriophage (liquid);
- enterococcus: liquid Intesti-bacteriophage;
- Pseudomonas aeruginosa: liquid Bacteriophage pseudomonas aeruginosis;
- Protea: Coliproteophage (tablets);
- Escherichia coli: liquid purified polyvalent Pyobacteriophage.
Sorbents
They bind and absorb toxins and allergens, preventing putrefactive processes from developing. Used at an early stage of therapy. Polysorb, Smecta, Pepidol, Enterosgel, Polypefan.
Enzymes
They help active digestion and stimulate the motor and absorption functions of the intestines. Festal, Digestal, Panzinorm, Mezim, Creon.
Antispasmodics
Relieves intestinal and stomach cramps. The most effective are Dicetel, No-shpa, Duspalitin, Meteospasmil.
Regulators of peristalsis
Restores normal movement of the food bolus from the stomach to the intestines and peristalsis. Helps with nausea, vomiting, bloating, diarrhea. The most common are Smecta, Trimedat, Motilium, Loperamide, Trimebutin.
Absorption stimulants
Essentiale, Karsil, Legalon stimulate the functions of cell membranes in the intestinal tissue, promoting the normal absorption of nutrients, and relieve colic.
Immune defense modulators
Restore local immunity in the intestines, increase the protective functions of the weakened body. For this purpose, Taktivin, Levomisol, Timalin, Immudon, Timogen, Immunofan are prescribed. Used for a month at the last stage of treatment to stabilize the result simultaneously with vitamins.
Diet
Therapy of dysbacteriosis requires the mandatory inclusion of dietary nutrition in the treatment regimen. It may be less or more “restrained” in diet, which is associated with the severity of the disease, but the basic principles remain unchanged:
- exclude products with chemical dyes, preservatives, flavors and flavor enhancers;
- take into account the nutritional characteristics necessary in the treatment of a disease that provokes dysbacteriosis;
- use products that do not cause diarrhea, constipation, compensate for anemia, vitamin deficiencies;
- consume foods taking into account the likelihood of developing food allergies, which often accompany dysbacteriosis;
- do not drink alcohol, but if this principle is violated, choose strong drinks, since beer, wine, champagne are more likely to cause aggravation;
- Despite the variety of diets for dysbiosis, one should not fanatically concentrate on the time of food intake and its quantity (excluding overeating). There is no need to languish from hunger and eat when you feel that it is necessary. The best option is to eat small meals frequently.
Prohibited Products
Products that require limitation or exclusion:
- starchy foods, spicy foods, fatty meats, offal, mushrooms;
- canned food, spices (except cinnamon, cloves, pepper, bay leaf, coriander);
- alcohol, strong and surrogate coffee;
- sweet fatty foods, dark chocolate, buttercream cakes, fried donuts, ice cream
- fried, fatty, heavy dishes, sauces such as mayonnaise, pickles, marinades;
- raw vegetables for dysbacteriosis with frequent diarrhea (cabbage, including sauerkraut, carrots, beets, green salad, spinach, radish, radish), containing coarse plant fiber. It irritates the intestinal mucosa, easily causing diarrhea.
Photo gallery. Foods and dishes that need to be removed from the diet or limited
Fried, salted, pickled mushrooms Mayonnaise and sauces with a similar composition Beer and other alcohol with a yeast component (wine, champagne) Fatty sweets, including cakes with butter cream Fried meat, potatoes Pancakes, especially those with yeast Pickles and marinades
Features of nutrition for various types of dysbiosis
Not all products allowed for dysbiosis can be consumed in certain forms of it.
During fermentation processes in the intestines, limit sweets, sugar, honey, jam, milk, and raw fiber. If there is no increased acidity, it is undesirable to wash down food with water, since diluted gastric juice worsens the digestion of food, exacerbating the fermentation processes. Boiled vegetables, cereals, fermented milk products, and spices are allowed: bay leaves, cloves, pepper, which suppress fermentation. Recommended products are boiled, baked, low-fat broths, eggs in a bag, steam omelettes.
During putrefactive processes, the intake of meat and fats is limited, the diet increases vegetable and fruit dishes (especially apples), preferably baked kefir, and yogurt. Boiled vegetables, porridge, kefir, dried apricot compotes, apricot puree, and cranberry jelly are allowed. Herbs: wormwood, sage, lemon balm.
For fungal dysbiosis, limit foods with yeast: cheese, grapes, champagne, beer, kvass, pancakes, pancakes, fresh bread, warm pies, sauerkraut, kefir with fungal starter.
Allowed foods and dishes
In case of dysbacteriosis, the following is introduced into the diet:
- protein products: dishes from lean boiled, stewed without oil meat, fish, poultry, cottage cheese, cheese;
- stale bread, dry cookies without margarine, durum pasta;
- vegetables and fruits in large quantities, but if they have coarse fiber - always boiled and baked;
- eggs in any form, except fried;
- fermented milk products (excluding fungal dysbiosis), low-fat sour cream;
- sweets: natural marmalade, marshmallows - in small quantities;
- any porridge, during fermentation processes - it is better with diluted milk.
Photo gallery. What to eat if you have dysbiosis
Boiled potatoes Fermented milk products without preservatives, kefir Well-cooked porridge - a source of protein, vitamins and processed fiber Baked vegetables for less intestinal irritation during diarrhea Apricots and dried apricots destroy putrefactive microbes Steam omelets baked in the oven Carrot juice is a healing drink Low-fat cottage cheese, like source of complete protein Boiled and stewed lean meats Fruits, preferably baked
Sample menu for the week
On any day of the week, in the absence of diarrhea, a vegetable salad with vegetable oil (150 - 200 g) and stale bread (30 g) are added to the main menu.
| Monday | Not strong tea, Dry biscuits (30 g), cheese (20 g), Cottage cheese casserole (150 g) from low-fat unleavened cottage cheese Natural cherry jelly, Low-fat chicken broth with vermicelli (200 g) Boiled meatballs (100 g) with potatoes boiled in milk and carrots, Oatmeal porridge (200 g) with butter (5 g) Compote of lingonberries and raspberries Fruit puree of pear and peach (150 – 200 g) |
| Tuesday | Natural coffee with milk, brewed gingerbread (40 g) Omelette baked with tomatoes (150 g) Bean soup with potatoes and beef (200 g) Stewed vegetable stew with veal (200 g) Cheesecake with semolina and cottage cheese (100 g) Kefir , natural blackcurrant jelly Marmalade (30 g), apples baked with cinnamon |
| Wednesday | Chicory in milk, dry salted crackers (30 g), cheese (20 g) Fish baked in Polish in milk sauce (without butter) (200 g), mashed potatoes (150 g) Buckwheat porridge boiled in milk (200 g ) Mashed pea soup (200 g) low-fat curd cheese (100 g) Banana puree (150 g) Apple juice, diluted Marshmallow (30 g), fresh blueberry jelly or decoction of dried blueberries, strawberries, currants |
| Thursday | Light herbal tea, marmalade (30 g) Carrots stewed in milk sauce (150 g) Steamed chicken cutlets (100 g) with stewed zucchini and tomatoes (200 g) cherry strudel with cottage cheese and custard (150 g) Macaroni and cheese ( 150 g) Eggs “in a bag” with spinach Lingonberry jelly, kefir Apricot puree (200 g) with cream (20 g) |
| Friday | Natural coffee with milk, cheese (20 g), croutons Stewed fish with carrots (150 g), boiled potatoes (150 g) Wheat porridge (200 g) boiled with butter (5 g) Light meatball soup Chicken, boiled turkey (150 d) with rice and egg Carrot juice with cream (20 g), weak tea, herbal decoction Dry salted crackers (without margarine) – 40 g Decoction of rose hips and chokeberry |
| Saturday | Mild cocoa with milk, marshmallows (30 g) Semolina porridge (150 g) with butter (5 g) Meat soufflé in an omelet (200 g), zucchini pancakes (150 g) Low-fat fish soup (250 g) with potatoes Curd casserole with dried apricots (150 g), natural strawberry jelly, dried fruit compote, weak tea Kefir |
| Sunday | Chicory with milk, cheesecakes (100 g) with pectin confiture (20 g) Potato casserole with beef (200 g) and low-fat sour cream (25 g) Light cabbage soup (250 g) Boiled fish (150 g) with rice (100 g), cheese (20 g) Boiled eggs Benedictine Compote of fresh black currants and apples (or dried fruits) Kefir, tea from dried raspberries and strawberries, charlotte with apples (50 g) |
Folk remedies
Traditional recipes used in isolation for dysbiosis are not able to cure the pathology, so they cannot become a separate method of treatment. Homemade medicinal recipes can help relieve acute symptoms of the disease, improve general condition, and saturate the body with useful substances, but they cannot eliminate the cause of dysbiosis and represent only part of complex therapy.
It is optimal to use herbal mixtures that have a combined and mutually reinforcing effect in restoring flora, relieving inflammation and spasms, activating the intestines during constipation and strengthening during diarrhea.
Certain foods and plants recommended for dysbiosis
| Product, plant | Pathogens that are suppressed |
| Apples | Protea, Klebsiella, Shigella |
| Cowberry | fungi of the species Candida |
| Apricot | Enterococcus, Proteus, Staphylococcus, Klebsiella, Pseudomonas aeruginosa, inhibits fermentation |
| Cranberry | Protea, Salmonella, Klebsiella, Shigella |
| Strawberries | Enterococcus, shigella, staphylococcus, streptococcus |
| Raspberries | |
| blueberry | Staphylococcus, Klebsiella, Enterococcus, Proteus |
| Cloves and cinnamon | Escherichia, Pseudomonas aeruginosa, Proteus, Klebsiella, Candida |
| Garlic | Protea, Klebsiella, strong bactericidal properties |
| Black currant | staphylococcus, Proteus, enterococcus, general bactericidal effect |
| Rowan chokeberry | General antibacterial effect |
| Horseradish | Protea, Klebsiella, Pseudomonas aeruginosa |
| Carrot | salmonella, protozoa, clostridia, Candida |
Herbs have excellent anti-inflammatory and antimicrobial properties: wormwood, sage, chamomile, cinquefoil, St. John's wort, thyme, birch leaf, calamus root, calendula, oregano, yarrow, bird knotweed. For decoctions, it is advisable to take several types of herbs.
Photo gallery. Healing plants, herbs and berries that suppress the development of intestinal pathogens
Chamomile will help with many manifestations of dysbiosis Wild strawberry St. John's wort Calendula flowers Garlic is a powerful bactericidal product Cinquefoil anserina, erecta Lingonberry Thyme Black currant
Medicinal herbal teas:
- In equal proportions, take lingonberry and birch leaves, thyme, rose hips, calendula flowers, chamomile, cinquefoil and yarrow.
- A tablespoon of the mixture is poured into 0.5 liters of boiling water, leaving to steep for an hour. Drink half a glass up to 4 times a day for 7 to 10 days.
- In equal parts, take currant leaves, blueberries, raspberries and strawberries, rose hips, and calamus root. Two tablespoons of raw materials are brewed with 0.5 liters of boiling water. Infuse the decoction for 12 hours in a warm place (in a thermos). Drink a third of a glass before meals.
- Decoction of Potentilla erecta. Particularly good for diarrhea. For the decoction, take 1 tablespoon of raw material, pour in 250 ml of boiling water and boil slowly for 15 - 20 minutes. The decoction must be infused overnight. Drink 60–80 ml three times a day.
Home Recipes:
- Garlic. If there are no contraindications (kidney disease, erosions and ulcers in the stomach, esophagus and intestines, high acidity), it is advisable to eat up to 3 cloves of garlic per day.
- Mash with honey. If fungal dysbiosis has not been diagnosed and there are no fermentation processes in the intestines and stomach, prepare yeast brew with honey. Half a liter of boiled warm water, honey - 2 tablespoons, 2 grams of yeast. Mix and place in a warm place for 1 hour (no more). In the morning, drink half a glass before breakfast.
- Jerusalem artichoke puree. Peel 300 g of Jerusalem artichoke, cut, pour boiling milk (1 glass) and water (half a glass) and cook until soft. Drain the milk broth, bring to a boil and add a tablespoon of flour and salt into it, boiling until thick. There is no need to sauté flour in oil. The resulting sauce is seasoned with Jerusalem artichoke. Eaten with dill.
Important.
If you have dysbacteriosis, it is not recommended to use decoctions and infusions of medicinal herbs for enemas without the advice of a doctor. Enemas flush out not only pathogenic bacteria from the intestines, but also those necessary for digestion, so active use of this method can worsen the condition of bacterial imbalance.
Traditional methods of treatment
Treatment of dysbiosis with folk remedies can be used as an auxiliary method of therapy. Quite often, when intestinal microflora is disturbed, it is recommended to use garlic.
To do this, it is enough to eat 1-3 cloves at dinner and wash it down with yogurt.
Dysbacteriosis can also be treated by swallowing a clove of garlic in the morning on an empty stomach. The duration of such therapy with folk remedies should be 1-2 weeks. This will restore normal microflora and strengthen the immune system.
Folk remedies for intestinal dysbiosis also include flax seed. It can be added to porridge - 1 dessert spoon. This remedy not only helps to treat and restore microflora, but also copes with gastritis with high acidity.
Also, for this disease, it is useful to drink freshly squeezed celery root juice. To cope with pathology, it is enough to take 1-2 teaspoons half an hour before meals.
Herbs for intestinal dysbiosis are no less effective. You can use decoctions and infusions made from calendula, St. John's wort, chamomile, nettle, and horsetail.
Is it possible to cure dysbiosis?
Timely diagnosis of pathology is a guarantee of effective disposal of it. Therefore, to avoid complications, seek medical help at the first signs of illness.
Dysbacteriosis can be cured, especially if it appears against the background of toxic damage to the body.
If a person has taken antibiotics or other medications for a long time, his microflora will be disrupted. This is a logical consequence.
Important! If the work of the intestinal microflora has been disrupted due to the development of duonitis, gastritis or other diseases of the gastrointestinal tract, then you should not count on complete treatment. It is likely that in this case it will not be possible to completely stop the symptoms of dysbiosis.
As medical practice shows, with timely initiation of treatment, the prognosis is favorable.
However, in order not to harm your health, do not try to normalize the functioning of microflora by using dietary supplements.
Also, you should not count on a positive effect from kefir therapy. Its effectiveness has not been proven.
Thus, it is possible to determine 2 main prognoses in the treatment of dysbiosis:
- Favorable prognosis - the pathology was provoked by long-term use of medications or intestinal infection.
- Unfavorable prognosis - the pathology was provoked by ulcerative colitis, gastritis, duodenitis (chronic form).
Efficiency of dysbacteriosis therapy
After the course of treatment, clinical therapy, the effectiveness is visible, after it is possible to cure dysbiosis:
- The condition of the body changes after two weeks of treatment in advanced stages.
- Flatulence disappears.
- Pain in the stomach area decreases or disappears.
- The stool returns to normal.
Bacteriological treatment entails changes. After culture studies, improvement occurs after a month of intensive treatment.
Scatological and biochemical effectiveness:
- Iodophilic flora and extracellular starch disappear.
- Alkaline phosphatase is not detected in the stool and the level of enterokinase decreases to normal.
Efficiency of drug use
The use of these drugs for the treatment of dysbiosis is indicated if the cause of the problem is pathogenic bacteria, and the pathology is accompanied by an inflammatory process of an infectious nature.
If the clinical picture is severe, the following is prescribed:
- tetracyclines;
- penicillins;
- fluoroquinolones;
- cephalosporins.
For mild cases, they are limited to antimicrobial agents, for example Furazolidone.
Therapy lasts 1-1.5 weeks. Immediately after treatment, it is necessary to drink sorbents - drugs for the treatment of dysbiosis, which will remove dead pathogens and their waste products from the body.
It is worth considering a small nuance - the simultaneous use of antibiotics and probiotics or prebiotics is prohibited; it is necessary to maintain an interval of 1.5-2 hours between doses of the drugs. Otherwise, the treatment will be ineffective.
In the first case, antibacterial agents will destroy beneficial microorganisms, in the second, the components of the prebiotic medicine will bind and remove the antibiotic ingredients.
These drugs are prescribed only for a certain form of the disease and strictly taking into account the sensitivity of the identified microorganism.
- For staphylococcus - macrolite, Clarithromycin, Oleandomycin, as well as semi-synthetic penicillins such as Oxacillin and Amoxicillin and Lincomycin are prescribed.
- For Proteus and deformation of the shape of E. coli, effective drugs nitrofurans are prescribed, which belong to the group of special intestinal antiseptic substances. These can be sulfonamide drugs (Sulgin, Fthalazol), as well as derivatives of nalidixic acid (Nevigramon peraprate).
- When enterococci are detected, semisynthetic penicillin (Apicillin) and macrolides (Erythromycin and Levomecitin) are prescribed.
- For Pseudomonas aeruginosa, aminoglycosides (antibiotics Gentamicin and Kanamycin), as well as drugs such as carbenicillin and polymyxin, are prescribed.
- For candidiasis dysbacteriosis, amphotericin B, Diflucan and Lamisil are prescribed.
Bacteriophages are viruses that infect a specific type of microorganism. They can be combined with antibacterial medical therapy or used as a substitute alternative treatment. Bacteriophage probiotics can be taken either orally or as enemas.
Since dysbacteriosis leads to hypovitaminosis, for its treatment the doctor prescribes various multivitamins such as: Decamevit, Multitabs, etc.
Immunomodulators and biostimulants are prescribed to restore microbial balance, restore immunity and reduce the number of colds. These are drugs such as: Echinacea tincture, Schisandra, Eleutherococcus alcohol tincture, propolis extract, and Dibazol.
For diarrhea - sorbents and astringents, antidiarrheal drugs and antispasmodics.
For constipation - osmotic laxatives (Forlax), Sorbitol, Xylitol, as well as herbal laxatives, Lactulose and various choleretic drugs.
Some experts are inclined to believe that dysbiosis is not an independent disease, but a set of symptoms that accompany many problems in the functioning of the digestive system. The cause of the syndrome is a violation of the quantitative norm of certain groups of bacteria inhabiting the intestines. The symptom complex is distinguished by the following manifestations:
- problems with bowel movements (diarrhea or constipation);
- belching;
- bloating;
- colic;
- flatulence;
- unpleasant foreign taste in the mouth;
- rumbling in the intestinal area;
- skin allergies to certain products;
- intestinal allergy symptoms (diarrhea with foam, nausea, vomiting);
- manifestations of intoxication (headache, general weakness, low-grade fever);
- decrease in the body's defense response (immunity).
Various factors can contribute to the development of a symptomatic complex. All lead to the same result - a violation of the microbial composition of the lower gastrointestinal tract: increased contamination of the small intestine or a change in the composition of bacteria in the large intestine.
When treating dysbiosis, it is important to follow a diet, but the treatment of such a pathological process of the digestive system cannot be done without the use of drug therapy.
Drugs for the treatment of dysbiosis have various therapeutic effects on the condition of the intestine itself and on its microbial composition. Some medications affect the normalization of the function of the walls of the large or small intestine, others contribute to the population of the necessary groups of bacteria, others play the role of an intestinal antiseptic to destroy pathogenic microflora, and others increase the protective function of the body.
Based on the characteristics of the cause of dysbiosis, for the effectiveness of therapy, patients are prescribed:
- probiotics (preparations containing natural cultures of microorganisms, the presence of which is necessary for the normal functioning of the gastrointestinal tract);
- prebiotics (food additives, dietary supplements, preparations containing natural fibers that are not digested by the stomach. Coarse fiber enters the lower digestive tract and serves as “food” for microorganisms inhabiting the intestines);
- antiseptics (antibacterial drugs, the action of which is aimed at reducing the quantitative composition of bacteria with increased colonization of the intestines);
- synbiotics (combined drugs that include both probiotics and prebiotics).
To cure dysbiosis at home and not cause harm to health, you must adhere to the exact dosage of the product in stages.
The use of sorbents is a mandatory part of the treatment of intestinal microbial imbalance. They are necessary to prevent intoxication of the body and eliminate its manifestations. Drugs in this group can increase the effectiveness of therapy.
Enterosgel. For the treatment of grade I or II dysbiosis in adults and children aged 5-14 years, a sufficient daily dose of 45 g of the drug is sufficient. The dosage regimen is as follows: 15 g of gel (1 tablespoon filled to the brim) is mixed well with 30 ml of water until smooth and diluted with another 100-150 ml of water. The product must be taken 1.5 hours before meals.
For children aged 1-5 years, the daily norm is 22-25 ml of gel (1/2 tbsp. 3 times a day). Infants 1/2 tsp. The gel should be diluted in breast milk, the volume of which is 3 times the amount of the drug.
Polysorb MP. Enterosorbent, which binds, neutralizes and removes toxins of various natures. The polysorbic function is performed by the only active ingredient of the drug: colloidal silicon dioxide.
Treatment with this remedy can only be done by diluting the powder with water. The amount of substance and water to prepare the suspension depends on how much the patient weighs:
- up to 10 kg – daily dose – 1 tsp. powder per 50 ml of water;
- 10-30 kg – dose for 1 dose – 1 tsp. for 50 ml of water;
- 30-60 kg – dose for 1 dose – 1 tbsp. l. per 100 ml of water;
- more than 60 kg – dose for 1 dose – 1.5-2 tbsp. l. for 150 ml of water.
It is necessary to take a suspension from Polysorb 2-4 times a day 1-1.5 hours before meals. The course of treatment is 3-14 days.
The treatment complex for dysbiosis may include antidiarrheal drugs. One of the popular ones is Enterol.
The product is available in powder 100 mg and 250 mg and capsules 250 mg.
- children from 1 to 3 years old are prescribed 1 capsule 2 times a day, 1-3 sachets (100 mg) per day or 1 sachet (250 mg) per day;
- children over 3 years of age and adults 2 capsules 2 times a day, 2-4 sachets (100 mg) per day or 2 sachets (250 mg) per day.
Loading …
Regime and diet
The diet of a woman suffering from dysbiosis should:
- Be rationed and constant (without stress in the form of a hunger strike, but in small portions in parts).
- Contain foods rich in dietary fiber and vitamins.
- Be built with a predominance of fermented milk products containing beneficial lactobacilli in them.
- Avoid all heavy meals while your intestines are recovering.
Such a diet will help eliminate the symptoms of dysbiosis and begin to nourish the body with the missing elements. Proper nutrition in any illness is the key to a quick recovery.
Features of treatment of intestinal dysbiosis in adults with medications
Therapy for dysbiosis is a whole range of measures, including taking medications for various purposes.
So, first of all, it is important to eliminate the causes, and only then begin to restore the functioning of the digestive organs.
Be careful! The duration of treatment and dosage of any drug should be determined only by a specialist.
Exceeding the permissible dose for a particular patient may lead to unwanted side effects, as well as negative consequences for the body.
Antibacterial therapy
This group of drugs is prescribed by a doctor if dysbiosis leads to pronounced inflammatory changes in the mucous membrane of the digestive tract or the processes of digestion and absorption of food are affected.
The course of therapy can last from a week to 10 days. Sometimes treatment can last up to two weeks. The most justified is the prescription of drugs that do not have a systemic effect . They are poorly absorbed and work primarily in the intestinal lumen.
This list contains:
- Alpha Normix (rifamixin) is the best remedy for dysbacteriosis. Available in tablets containing 200 mg of active substance, as well as in granules for preparing a suspension. Has a wide spectrum of antibacterial activity. The treatment is well tolerated and side effects are rare. Pregnant and lactating women should only use if absolutely necessary. The urine may turn red.
- Nifuroxazide (Stopdiar, Enterofuril, Ersefuril) – capsules or tablets for oral administration. Contraindicated for children under 6 years of age. A suspension is available for children. The spectrum of action is wide. Does not affect obligate flora. Stimulates the activity of the immune system. Contraindicated for pregnant women, but during breastfeeding treatment is possible in a short course. Allergic reactions are possible.
- Phthalazole is a sulfonamide. Available in tablets. The spectrum of antimicrobial action is small, but the drug additionally reduces the activity of the inflammatory process in the intestines. There are many contraindications and side effects, which limits the possibilities of use.
- Sulgin is a sulfonamide. Release form: tablets. Contraindicated for pregnant and lactating women. There are many other contraindications and numerous side effects. Sufficiently large doses of medication are used for treatment.
In severe cases, they resort to prescribing drugs that have a systemic effect:
- Furazolidone is a nitrofuran derivative, tablets. Acts on the bulk of gram-negative and gram-positive bacteria, causing the death of protozoa. Drug resistance develops slowly. High doses of medication are used for treatment. Since there is a systemic effect, side effects often occur in the form of nausea, vomiting, and loss of appetite. Allergic reactions and drug interactions are possible.
- Metronidazole (Trichopol, Flagyl) – tablets. The spectrum of antibacterial action is wide. It also affects protozoa. Use during pregnancy is possible, but during lactation it is strictly prohibited.
- Biseptol is a combination remedy. Contains sulfonamide (sulfamethoxazole) and an antimicrobial agent - trimethoprim. Due to this, the spectrum of antibacterial action is significantly expanded. There are many contraindications and serious side effects are possible.
- Nevigramon is a derivative of nalidixic acid. A drug from the quinolone group. Available in capsules. Contraindicated for children, pregnant and lactating women. An analogue is Negram - tablets.
Characteristic symptoms
When the intestinal microflora is disturbed, the first signs go unnoticed for a long time, everything is attributed to fatigue, stress, lack of sleep and other everyday excuses.
And dysbiosis continues to actively develop, and over time the number of symptoms will increase.
The main ones:
- Stool disorder - diarrhea begins, or diarrhea gives way to constipation. There may be mucus or pus in the stool.
- Abdominal pain appears ; as dysbiosis progresses, it can increase in severity and frequency of manifestation.
- Failure to pass gas creates additional discomfort, bloating and discomfort. After going to the toilet, the condition temporarily improves.
- Loss of appetite , as every meal is accompanied by nausea, and in severe cases, vomiting.
- Allergic manifestations in the form of skin rash, hives, sneezing. Itching due to dysbacteriosis is also not uncommon. Especially if it is caused by parasites in the intestines.
- A characteristic sign of intoxication is temperature with increasing weakness - with dysbacteriosis, it often stays around 37˚C-38˚C.
- Dry skin , brittle and split hair, thin nails - all these are indirect signs of vitamin deficiency caused by intestinal dysbiosis.
When a person develops these symptoms in turn, he does not immediately understand what it is, and only an increase in the severity of the disease gives reason to think about dysbiosis.
The more this or that symptom manifests itself, the more advanced the disease is, and it will be more difficult for a woman to treat intestinal dysbiosis.
The right approach to treatment
In most cases, dysbiosis does not require any treatment. If you follow a diet and maintain a healthy lifestyle, the beneficial microflora in the intestines will restore on its own. The number of lacto- and bifidobacteria will increase, which will gradually displace harmful microorganisms.
A gastroenterologist can only prescribe the patient to take probiotics and (or) prebiotics, as well as multivitamin complexes to speed up recovery and improve well-being. Doctors begin complex and rather long-term treatment when the following symptoms appear:
- dyspeptic disorders - attacks of nausea and vomiting, chronic diarrhea or constipation, lack of appetite, pain in the epigastric region;
- signs of general intoxication of the body - weakness, apathy, fatigue;
- clinical manifestations of vitamin deficiency - hair loss, delamination of nail plates, dry skin, neurological disorders.
Such symptoms indicate a disruption in the metabolic processes of proteins, fats, carbohydrates, biologically active substances and their incomplete absorption. Pathology therapy begins with identifying the cause of dysbiosis and eliminating it. Diseases of the liver, stomach, intestines and pancreas are treated, often causing the death of beneficial microflora in the intestines.
Features of dysbiosis in pregnant women
Due to the fact that the fetus is in close connection with the mother, any dysfunction of the body is transmitted to it, which negatively affects its development. Therefore, before pregnancy, you should pay attention to the prevention of dysbiosis and undergo the necessary examinations. Otherwise, if there is dysbacteriosis during pregnancy, problems may arise - delayed fetal development, since due to the disease the supply of nutrients to the blood will decrease.
Therapy consists of diet and taking special medications prescribed by a doctor. Breastfeeding a child gives him the opportunity to avoid dysbiosis in infancy and reduce the likelihood of its occurrence in adulthood.
Factors in the development of the disease
Dysbacteriosis does not develop in absolutely healthy people. This condition is a signal that indicates that not everything is in order in the body.
The following factors can lead to the development of dysbiosis:
- Surgeries that were performed on the stomach or intestines;
- Poor diet (large amounts of flour, spicy, fatty foods and fermented milk products);
- Decreased immunity;
- Various sexually transmitted bacteria.
Features of the examination
To obtain reliable research results, it is not enough to have a qualified doctor and modern equipment nearby. Much depends on the patients themselves, or rather, their awareness in terms of preparation. What does it mean?
Three days before taking a stool test, you must exclude from your diet foods that cause fermentation, namely: meat and fish dishes, alcoholic beverages, and beets. You should also stop taking antibacterial and laxatives. This even applies to rectal suppositories and Vaseline oil.
To obtain biological material, you must wait for spontaneous bowel movements, but do not resort to laxatives. Feces should be placed in a special sterile container, which is purchased in advance at the pharmacy. If you haven’t found such a container, then use a container you have at home, but it must be sterilized before use.
Approximately ten grams of sample is sufficient for analysis. Try to deliver the biomaterial to the laboratory as soon as possible. If there is a delay, the death of anaerobic microorganisms will occur, which will distort the results.
To diagnose dysbacteriosis, coproscopy is performed
Probiotics
The products contain dried but live bacteria that have a positive effect on intestinal function. The healing powder is in capsules that completely dissolve, bypassing the stomach, the secretion of which can destroy microorganisms.
Medicines in this category are divided into several groups:
- Monocomponent. Contains one strain - bifidobacteria, colibacteria, lactobacilli. Popular drugs are Bifidumbacterin, Colibacterin, Lactobacterin.
- Multicomponent. There are several types. Representatives of this type are Bifiform, Linex, Bifikol.
- Combined. The composition is supplemented with a complex of immunoglobulins and a nutrient medium. A drug for dysbacteriosis such as Bificol or Rioflora Immuno is often prescribed.
- Synbiotics. Medicines combine the qualities of a probiotic and a prebiotic - Laminolact, Bifidobac, Maltodophilus. This group of drugs also includes conditionally antagonists, since they suppress the vital activity of pathogens - Enterol, Bactisubtil, Bactisporin.
Stages of dysbiosis
There are the following stages of the disease, during which a gradual disruption of the functioning of the gastrointestinal tract occurs:
| Disease stage | Symptoms of the disease |
| 1 | With degree 1, the protective endogenous flora decreases; bifido- and lactoflora are not affected; there are no clinical signs of the disease. This stage is common for the latent phase of the disease. |
| 2 | During the second stage, the number of beneficial microorganisms decreases to a critical extent. The development of pathogenic microflora is rapid. The first signs of dysbacteriosis appear, indicating malfunctions in the intestines. |
| 3 | In the third degree of microbiological disorders, the inflammatory process destroys the intestinal walls, aggravating chronic indigestion. This stage of the disease requires serious treatment not only with diet, but also with medications. |
| 4 | At this stage, harmful microorganisms almost crowd out beneficial ones, this leads to the appearance of intestinal diseases that are dangerous not only to the health, but also to the life of the patient. |
We can distinguish forms of dysbacteriosis according to the type of disease:
- Latent (compensated) - a hidden course, it does not lead to changes in a person’s condition;
- Subcompensated - the first symptoms of intestinal malfunction appear due to local inflammatory phenomena.
- Decompensated - there is a drop in the body's resistance, pathological processes cover the large and small intestines.
Nutrition during and after treatment
Intestinal dysbiosis requires dietary restrictions to regulate natural processes:
- You can drink coffee and tea half an hour after meals;
- Fatty and spicy foods with a lot of seasonings should be excluded from the diet;
- Those who like to drink water with their food should give up this habit - most often the gastric juice is diluted in this way, the processing of food in the stomach is delayed and complicated
- High concentration of proteins, which gradually increases. Only the meat should be lean, so as not to aggravate the situation;
- Bread, especially wheat varieties, is quite difficult to digest; it is better to avoid baking. Or switch to homemade crackers, they are less harmful;
- Nicotine and alcohol are excluded during treatment for dysbiosis. Liqueur, vodka or cognac in small quantities is less harmful to the stomach than “fizzy” alcohol: champagne, beer. Mineral water with gas is also not recommended;
- Raw vegetables are better absorbed and have a richer vitamin bouquet than boiled ones;
- The functionality of the body increases if you introduce sprouted wheat sprouts into your diet at least once a day. You can use the peeled wheat, but do not add milk or water when pouring, just moisten it so that the wheat is not so hard;
- Lactobacilli are found in natural fermented milk products. Especially in kefir and whey. There may be side effects in the form of loose stools, but the intestines simply start working better.
There is no special diet for each person, you just need to follow some rules, avoid unwashed fruits, low-quality foods and eat food every three hours in small portions. It is important to eat hot liquid food every day: soup, broth.
Methods for diagnosing dysbiosis
When a patient approaches with the complaints described above, the doctor collects information from the patient’s words, palpates the intestines, and prescribes a stool test. The analysis involves diluting one gram of feces in a special solution, after which it is sown on a nutrient medium. If the laboratory technician sees a decrease in the number of bifidobacteria, and at the same time an increase in the number of staphylococci or fungi, it means that intestinal dysbiosis is occurring.
Other diagnostic methods include:
- Clinical blood test - shows the presence of inflammation and possible bleeding in the intestines. With severe dysbacteriosis, anemia is observed - a decrease in the level of hemoglobin in the blood.
- Colonoscopy. Allows you to assess the condition of a section of intestine up to one meter long. It involves inserting a probe into the anus, so the procedure is very unpleasant for most patients. In some cases, it can be replaced by sigmoidoscopy.
- Irrigoscopy. A contrast agent is injected into the intestine, after which an X-ray examination is performed. The picture shows the condition of the colon, changes in its tissues and mucous membranes. This diagnostic method is more accurate than colonoscopy.
- Gastroscopy. Required when determining the causes of dysbacteriosis. If, based on certain signs, one can suspect that the imbalance is associated with digestive disorders in the stomach and duodenum, then gastroscopy will prove or disprove this.
Drug therapy
The use of medications is designed to eliminate symptoms, restore the concentration of beneficial bacteria, and increase immunity:
- To relieve symptoms of dysbiosis, it is recommended to use drugs with antispasmodic effects - Drotaverine, No-shpa, Papaverine.
- Laxatives and antidiarrheals are used - Forlax, Lactulose, Loperamide.
- If necessary, choleretic drugs (Legalon) and agents that improve the production of enzymes are prescribed - Mezim, Festal, Pancreatin.
The following groups of medications are indicated for complex treatment:
- Antibiotics. Their job is to destroy pathogens. You cannot use it on your own, as you need to determine the sensitivity of bacteria to the drugs.
- Bacteriophages. Viral agents that can penetrate a foreign microorganism and destroy it from the inside.
- Intestinal antiseptics. Used to reduce the infectious process.
- Probiotics. Contains live bacteria necessary for the normal functioning of the gastrointestinal tract.
- Prebiotics. The composition contains components that stimulate the development of beneficial microflora.
- Immunomodulators. Designed to simulate natural protection.
- Multivitamins. Replenishes the deficiency of substances A, D, E, group B, etc.
The main direction is to eliminate the cause of dysbiosis. Otherwise, the restoration of balance will not last long, and soon the patient will again experience the symptoms of the pathology.
For any disease, pregnancy is a risk factor for the use of many medications.
Medicines and herbs that are completely harmless at first glance can provoke an increase in the tone of the uterus, relaxation of the cervix, and cause spasms of the muscle tissue of the uterus, which is dangerous for spontaneous abortion and early labor.
Some medications can lead to delayed development of the embryo and fetus and have teratogenic properties, leading to intrauterine deformities.
In addition, any medications can provoke acute allergic reactions, including laryngeal edema and rapidly developing anaphylactic shock.
Since many pharmacological agents are used to treat dysbacteriosis, when expecting the birth of a baby, special attention is required to the contraindications set out in the instructions, which even the doctor is not always aware of.
Dangerous during pregnancy:
- Sumamed, Zitrolide (Azithromycin), Furadonin, Metronidazole, Trichopolum. Ciprofloxacin, Ciprolet, Nolitsin, Levomycetin, Biseptol, Ersefuril are prohibited;
- antispasmodics that contain bromine (Decitel) can cause neurological disorders in the fetus.
- laxatives for constipation Loperamide (Imodium), Senna;
- Among medicinal herbs and plants, the following are especially undesirable and even dangerous: tansy, wormwood, aralia, barberry, oregano, juniper, buckthorn, nutmeg, pennyroyal, celandine, lovage;
- products - garlic, rhubarb, radish, parsley.
The list of drugs that can be used to treat intestinal dysbiosis is quite wide. They differ in action, cost, manufacturers, and release form.
| Release form | Description |
| Pills |
|
| Powders |
|
| Suspensions |
|
| Drops | Antidiarrheal agent. Hilak forte. |
Herbal medicine for dysbiosis
Traditional medicine offers many natural remedies that can cure most known diseases, including dysbiosis. However, the treatment process usually requires patience and regularity, since natural remedies act very gently.
Herbal medicine is the basis of traditional medicine. There are healing herbs for dysbiosis that affect certain manifestations of the disease.
IMPORTANT! Treatment exclusively with herbs is possible only in cases of mild dysbacteriosis. In other cases, traditional methods are only an addition to the main treatment prescribed by a specialist.
Video - How to treat intestinal dysbiosis
Healing herbs for dysbiosis
| Effect | Grass |
| Antiseptic and antibacterial | Alpine Cladonia, Bearded Usnea, moss moss, rose hips |
| Anti-inflammatory | Chamomile, calamus root, burdock seeds |
| Against flatulence and bloating | Peppermint, eucalyptus leaves, dill seeds |
| Enveloping (regenerate the mucous membrane) | Flax seeds, spotted orchis, marshmallow root |
| Painkillers | Chamomile, St. John's wort, lemon balm |
| Astringents (used for diarrhea) | Oak bark, cinquefoil erecta, St. John's wort, bird cherry |
| Laxatives (used for constipation) | Flax seeds, dandelion, plantain seeds, buckthorn bark, oregano, aloe |
Herbs are used both separately and in collections in the form of infusions and decoctions.
IMPORTANT! Herbs are highly allergenic, so treatment should begin with minimal dosages. If you are prone to allergic reactions, it is better to completely abandon herbal medicine.
Video - How to treat dysbiosis with folk remedies
Effective phytotherapeutic recipes for dysbiosis
| Purpose | Dosages | Cooking method | How to use | Duration of treatment |
| Infusion against dysbacteriosis No. 1 | A teaspoon of chamomile, sage and St. John's wort herbs, 200 ml boiling water | Brew the herb with boiling water in a thermos, leave for an hour, then strain | Dilute half a glass of infusion with half a glass of warm water, drink twice a day an hour after meals | Two weeks |
| Infusion against dysbacteriosis No. 2 | A tablespoon of rose hips and lemon balm, a liter of boiling water | Pour boiling water over the herbs in a thermos, leave for 11-13 hours, strain | Consume warm three to four times a day about an hour before meals | Two weeks |
| Infusion against dysbacteriosis No. 3 | A tablespoon of flaxseeds and St. John's wort, half a liter of boiling water | Grind the seeds, put them together with lemon balm in a thermos, and brew with boiling water. After two hours, strain | Drink a warm infusion half a glass up to four times a day about an hour before meals | Month |
| Anti-flatulence infusion | A teaspoon of dill and flaxseed, a glass of boiling water | Grind the seeds in a coffee grinder, place in a clay or enamel bowl, pour boiling water over them, and close with a lid. Strain after an hour | Drink two tablespoons of infusion 25-35 minutes before each meal | Up to one month |
| Flatulence remedy | A teaspoon of dill seed, a teaspoon of olive oil | Grind dill seeds in a coffee grinder and mix with oil | Take a spoonful of the tea mixture 20 minutes before each meal. | Up to two weeks |
| Decoction for dysbacteriosis (with diarrhea) | Half a tablespoon of oak bark and a tablespoon of St. John's wort herb, a liter of water | Place the herb in an enamel pan and add water. After bringing to a boil, immediately remove from heat, wrap in a towel, leave for an hour, then strain | Take one glass of decoction at room temperature twice a day an hour and a half before meals. | Three to five days |
| Decoction for dysbacteriosis (with constipation) | Half a tablespoon of chamomile and a tablespoon of dandelion, a liter of water | Place the raw materials in a saucepan, add water, and let simmer over low heat for five minutes. Then leave it to brew for half an hour, strain | Take a glass of warm decoction three times a day one and a half hours before meals. | A week |
Composition of vaginal microflora
The microflora of the vaginal cavity is formed as follows:
- lactobacilli. They are called Dederlein sticks. The number of lactobacilli reaches 90%;
- bifidobacteria. They are part of the microflora of the female genital organs in an amount of 9-10%;
- key cells. Includes Candida, Leptothrix, Gardnerella, and others. Their number is insignificant (1%).
The ratio of microorganisms on the mucous membranes of a woman’s genital organs is stable. The immune system plays a key role in this process. It controls the number of pathogenic microorganisms. The body is able to independently normalize microflora without additional measures. In case of significant violations, local immunity cannot cope with the problem, which causes violations.
Diet
Rational nutrition is used as an independent method of therapy for latent disease or is used in complex treatment to compensate for the deficiency of microelements and vitamins. It is prohibited to consume during this time:
- confectionery;
- smoked meats, pickles and marinades;
- alcoholic drinks;
- fat meat;
- concentrated broths;
- pasta;
- mushrooms;
- potato;
- refined sugar.
In case of increased flatulence, the following are excluded from the menu:
- semolina and rice;
- whole milk;
- baked goods;
- sweet apples, bananas, grapes;
- turnip;
- carbonated drinks.
Fried foods are prohibited; steamed or boiled foods are recommended. Fermented milk products such as kefir and yogurt are beneficial. In the absence of severe irritation of the intestinal mucosa, fresh vegetables and fruits with a high fiber content are allowed.
It is advisable to discuss a diet for dysbacteriosis with your attending physician, who will take into account the severity of the process, concomitant diseases, causes of pathology and the patient’s condition.
More about dysbiosis
With intestinal dysbiosis, otherwise known as dysbiosis, the balance (eubiosis, eubacteriosis) of beneficial and opportunistic (bad) microorganisms (microbes) in the intestine is disturbed. Dysbacteriosis (microbiocenosis) can be either an independent disease or accompany chronic gastritis, ulcers and other diseases of the gastrointestinal tract.
Normally, about 500 species of different microorganisms (2-3 kg) are present in the adult body. About 60% of all these microorganisms live in the gastrointestinal tract. These microorganisms are involved in the digestion of food, help synthesize vitamins, and remove toxins from the body. The main bacteria present in the intestinal flora are lactobacteria and bifidobacteria.
Three types of bacteria are involved in the digestion of food:
- beneficial - lactobacilli, bifidobacteria. They help maintain the balance of other bacteria (including harmful ones), prevent the development of allergic reactions, weakened immunity and other negative effects on the body;
- neutral. They are located in a certain place and do neither harm nor benefit;
- harmful - streptococcus, staphylococcus, candida fungus. These bacteria are provocateurs of various diseases and disruptions in the gastrointestinal tract.
You should know that there is no such disease officially, and what we call dysbiosis is actually a functional disorder. As a rule, dysbiosis is a sign of another disease of the digestive tract.
Diagnostic features
Diagnosis is based on data from laboratory and instrumental studies, and patient complaints. The main range of research consists of the following activities :
- palpation of the abdomen and abdominal organs;
- stool examination (occult blood, microbiological examination for helminths, bacterial culture);
- blood and urine tests;
- Ultrasound of the abdominal organs.
If the diagnosis is doubtful, endoscopic examination of the intestinal tract through probing (colonoscopy, sigmoidoscopy) may be required. It is especially important to carry it out if tumors, intestinal bleeding and other complications are suspected.
Diagnosis of the disease
In order to accurately make a diagnosis and determine treatment methods, it is necessary to rely not only on the external manifestations of the disease. To make a diagnosis, the doctor collects an anamnesis and finds out the possible causes of microflora dysfunction. After this, a more detailed examination of the gastrointestinal tract is prescribed (in case of chronic dysbacteriosis, an examination of the immune system is also prescribed).
The following instrumental and laboratory methods are used for research:
- microscopic examination of stool;
- a scraping is made from the intestinal wall (colonoscopy) for further examination;
- stool culture (including for dysbacteriosis);
- a blood test (to detect inflammation and hidden bleeding in the intestines), this test also shows anemia during an exacerbation;
- Ultrasound of the abdominal cavity;
- radiography of the intestine using a contrast agent to detect pathologies - irrigoscopy;
- fibroesophagogastroduodenoscopy. This method consists of examining the mucous membrane of the stomach, esophagus, and duodenum using an endoscope;
- coprogram.
Since dysbacteriosis causes symptoms that look like signs of diseases such as colitis, enterocolitis, gastritis, inflammation of the small or large intestine, rectum, the doctor’s task is to carry out a differentiated diagnosis of these diseases.
What are the consequences of dysbiosis?
With dysbacteriosis, in some cases, pseudomembranous colitis appears as a complication. However, often the influence of dysbiosis is more subtle.
It is now recognized that intestinal flora plays an important role in the regulation of the immune system and inflammatory processes. Bacteria influence which organisms and food components will be classified as known and harmless, and which the immune system will have to act on.
With dysbiosis, the immune system may not recognize the infection or react too aggressively, which can result in food allergies and autoimmune diseases.
In addition, it is believed that the natural “bacterial layer” in the intestines protects the mucous membrane and limits its permeability. When there is an imbalance, the intestinal wall becomes more permeable, allowing more toxins from food to enter the bloodstream.
If the intestinal barrier is weakened due to dysbiosis, more surface bacteria can enter the bloodstream. This activates the immune system and puts the body into a kind of “chronic inflammatory state.”
Elevated levels of inflammation are known to be a risk factor for metabolic syndrome, which may be associated with obesity, elevated blood lipids, and decreased glucose tolerance.
https://www.youtube.com/watch?v=9LoYxiRw1ek
The consequences of metabolic syndrome include arteriosclerosis, increased risk of heart attack, and type 2 diabetes.
An autoimmune disease, type 1 diabetes mellitus, which often occurs in childhood, can also occur; this is apparently related to nutrition and the microbiome.
Dysbiosis is associated with many other diseases, but to date it has not been possible to establish clear cause-and-effect relationships.
Scientists hope that with a more thorough study of the intestinal flora, it will be possible to better explain diseases such as depression, chronic fatigue, rheumatism, etc. diseases.
Why is dysbacteriosis dangerous?
In addition to constant discomfort and deterioration in quality of life, long-term dysbiosis can cause serious pathologies. Due to impaired absorption of nutrients, patients develop vitamin deficiency, iron deficiency anemia, fungal and viral diseases with all associated complications. Decreased immunity leads to frequent colds, acute respiratory infections and acute respiratory viral infections, and in some cases can provoke the appearance of tumors in the body.
The danger of dysbacteriosis for women
Main symptoms
In women, symptoms of vaginal dysbiosis manifest themselves as follows:
- change in the nature of discharge. They become abundant, acquire an uncharacteristic color (white, yellowish, greenish), smell (fishy, putrid), consistency (excessively viscous);
- the appearance of itching, burning, discomfort in intimate places;
- discomfort during sexual intercourse and urination.
The nature of the changes and the number of unpleasant symptoms depend on the degree of disruption of the microflora of the mucous membranes. Emerging problems may indicate the development of completely different diseases. If characteristic signs of imbalance are identified, it is imperative to consult a doctor.
Main stages of the disease
- There is a slight increase in the concentration of pathogenic flora and a decrease in the number of obligate bacteria. There are usually no symptoms.
- A critical decrease in the concentration of beneficial microflora, rapid growth of pathogenic flora. This stage often manifests itself with symptoms such as diarrhea, constipation and flatulence.
- Active reproduction of pathogens, inflammation of the intestinal mucous walls.
- General exhaustion of the body, vitamin deficiency, obligate microflora is almost completely replaced by pathogenic and conditionally pathogenic fungi/bacteria.
Prebiotics
The main purpose of prescribing such drugs is to create favorable conditions for the normal functioning of the obligate intestinal microflora. These are dietary fibers that are not digested in the intestines. They serve as a nutrient substrate for beneficial microflora.
Prebiotics include:
- Lactulose is a disaccharide consisting of lactose and fructose. Stimulates the growth of bifidobacteria and lactobacilli. Suppresses the activity of pathogenic microorganisms (clostridium, E. coli). There are many lactulose-based drugs on the pharmaceutical market: Duphalac, Portolac, Normaze, Lactusan. Such medicines are available in the form of syrup. Additionally, they have a laxative effect and help eliminate toxins.
- Inulin is a polysaccharide found in many plants. One of these drugs is Ortho Prebio. It is an oral powder that can be added to drinks or food.