Bilirubin is known to most patients in clinics only by ear.
Yes, we heard. And this is practically the limit of knowledge. However, this is a very important and apparently the most common indicator in a general blood test. It is by the concentration of bilirubin that one can judge the state of metabolic processes and possible diseases of certain organs. A blood test for bilirubin is prescribed in almost all unclear situations. It is carried out during regular preventive examinations, during pregnancy, to diagnose certain diseases.
What is bilirubin?
Bilirubin is a type of chemical pigment compound. It is this element that gives bile and feces their characteristic color, since in its pure form bilirubin is a brownish crystal.
Bilirubin has a toxic effect on nerve cells, becoming a factor in the development of characteristic encephalopathy, kernicterus. Conjugation or the process of chemical binding of free bilirubin occurs in the liver tissues. The breakdown of red blood cells, which occurs predominantly in the tissues of the spleen, ensures the release of a large amount of free bilirubin, which enters the liver through the portal veins with the bloodstream. The biochemical processes of “binding” and transformation of bilirubin in liver cells cause a decrease in its toxic effect on tissues and organs.
Different types of bilirubin
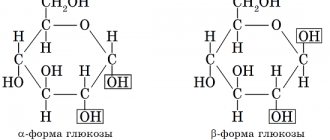
In the human body, bilirubin is present in two varieties, bile fractions: conjugated, bound or direct bilirubin, and indirect or free bilirubin. In a biochemical study of blood components, the amount of bilirubin can be calculated in a general form for both fractions (total bilirubin); if the norm is exceeded or there are indications, a study of the indicators of each fraction separately is prescribed.
Indirect bilirubin is produced constantly: every day, the breakdown of red blood cells releases almost 300 milligrams of bilirubin. Entering the liver tissue through the bloodstream, indirect bilirubin is transformed through biochemical processes that culminate in conjugation with glucuronic acid and the formation of conjugated bilirubin. Indirect bilirubin is toxic to tissues and organs. Easily penetrating cells, it conjugates with fats and contributes to disruption of cellular respiration and metabolism, protein formation, and transport of potassium ions. An increased concentration of indirect bilirubin is especially dangerous for the brain tissues that are most sensitive to it.
The importance of normalizing bilirubin and methods for achieving it
Every woman wants to be healthy, and to achieve this you need not only treatment, but a timely visit to the doctor if unpleasant symptoms appear. If a study of blood from a vein reveals an imbalance of bilirubin, then both medications and a certain diet are recommended to normalize it.
How to reduce
Having identified the reasons that increase pigment, determine ways to help reduce its level:
- intravenous administration of glucose, which allows destruction products to leave the body as a result of biochemical processes;
- the use of therapeutic plasmapheresis, albumin.
- phototherapeutic effect - irradiation with lamps that converts indirect bilirubin into direct bilirubin, which is excreted from the body.
It is imperative to follow nutritional rules . It is recommended to exclude fatty, spicy and too salty foods from the menu, and reduce the consumption of butter, margarine, baked goods, garlic, and onions to a minimum.
How to increase
With reduced pigment, nutrition plays a certain role. It is necessary to exclude alcoholic beverages, coffee, smoked, salty, fried, and spicy foods.
Strong physical activity is recommended. Activity should not be excessive, but you should not lead a sedentary lifestyle. As a medical treatment, choleretic drugs are prescribed.
Visiting a doctor, undergoing the prescribed examination and passing all the necessary tests (with proper preparation for them) will help avoid health problems.
It is always important to monitor your condition, but you should especially pay attention to it after 50 years, since age-related changes occur in the body, and there is a risk of developing various diseases.
Laboratory tests make it possible to diagnose many diseases, which may be indicated by deviations from the norm of certain indicators. An important indicator is bilirubin, the norm of which differs in women, men and children. Let's look at what this component is, what its functions are, and how to interpret the results of the analysis.
Total bilirubin is increased
What is considered an increased amount of bilirubin? The norms vary depending on the person’s age: the highest levels of bilirubin, which do not accompany diseases and dysfunctions, are observed in infants, which is due to the process of accelerated breakdown of fetal red blood cells, which are found in large quantities in the blood of the fetus and newborn. The yellowish color of the skin and sclera of children in the first weeks after birth is a consequence of a temporary high concentration of bilirubin.
Photo: Happypix/Shutterstock.com
The process of increased production of bilirubin normally ends by the age of one month, after which the normative indicators almost correspond to the norms for the adult body. What is the norm of bilirubin determined for different age periods?
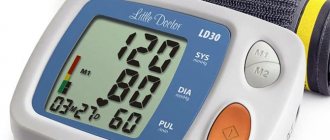
| Indicator name/patient age | From birth to 3 days | 3-6 days | 1 month and older, children | Adults |
| Total bilirubin | 24-190 | 28-210 | 3.5-20.4 | 8-20.5 |
| Direct bilirubin | 0.5-10.2 | 1-12.4 | 0-5.1 | 0-5.1 |
| Indirect bilirubin | 23.5-180 | 27-198 | Until 16.5 | Until 16.5 |
Analysis transcript
It is important to control the content of indirect bilirubin fraction. If its level is elevated, this indicates that there is a rapid, increased breakdown of red blood cells with the release of hemoglobin, which the liver does not have time to process. Another cause of hyperbilirubinemia is impaired motility of the gallbladder, which prevents bile from flowing normally into the duodenum.
With increased hemolysis, the concentration of hemoglobin increases, and at the same time the amount of indirect bilirubin fraction increases. Similar changes occur with hemolytic disease (incompatibility between the blood of mother and fetus).
Hepatocytes (liver cells) are not able to quickly process excess indirect toxic bilirubin when liver functionality is impaired. Its content in the blood increases when there is a deficiency of cyanocobalamin (vitamin B12). Metabolism is also disrupted in some genetic diseases (Gilbert's syndrome).
Normal values
First, during the study, doctors calculate the level of total and direct bilirubin, and the resulting difference in these indicators is the content of the indirect form.
In healthy men and women, pigment indicators are almost the same, since the level of the indirect fraction is not affected by gender or hormones. A variant of the norm is a decrease in the substance with age. The younger the person, the more bilirubin of this fraction is in the blood. In newborn children, the level of the substance is higher than in adults.
The norm of indirect bilirubin in children in µmol/l:
- in children younger than 2 days after birth – from 57 to 198;
- from 2 to 6 days – from 25 to 176;
- in infants from 6 days - from 5 to 21.
The norm in women reaches 17.2 µmol/l. In expectant mothers, this indicator does not change if they are healthy.
Indirect bilirubin in men is normally about 20 µmol/l. This value may increase with Gilbert's syndrome (pigmentary hepatosis), which is often diagnosed in men. The pathology is accompanied by a slight increase in pigment content. Often the disease is discovered by chance during a preventative medical examination.
Promoted
Elevated unconjugated bilirubin almost always indicates severe pathologies. Doctors identify the following reasons for increased indirect bilirubin:
- Anemia. With a lack of hemoglobin, oxygen starvation of organs and tissues occurs. As a result, red blood cells are destroyed to provide the body with additional iron-containing protein. Then the content of indirect bile pigment increases.
- Hepatitis of any origin. With an inflammatory disease, the liver is not able to process the toxic substance.
- Cirrhosis. This pathology is accompanied by the destruction of hepatocytes and scarring of the liver tissue. Because of this, the functions of the liver are disrupted, and then it does not have time to transform the pigment into a non-toxic form.
- Pigmentary cirrhosis. This is a hereditary pathology associated with insufficient activity of the enzyme UDPGT, which is involved in the neutralization of the bile component.
- Lucy-Driscoll syndrome. This is congenital hyperbilirubinemia in newborns. It develops as a result of the penetration into the child’s body of substances that prevent the transformation of indirect bilirubin into direct bilirubin.
- Hemolytic disease. This is a serious childhood disease that occurs due to incompatibility of the blood of mother and fetus for different antigens (for example, Rh factor).
- Diseases of the gallbladder, in which the flow of bile slows down. Then the level of the bile component increases.
- Liver tumors.
- Deficiency of nutrients.
- Infectious diseases.
- Excessive blood loss, etc.
The likelihood of hyperbilirubinemia increases after taking medications containing toxic substances.
Drinking alcohol in large doses can also cause an increase in the indirect fraction of bile pigment.
Demoted
Deviations from the norm to a lesser extent were not previously taken into account. But according to recent medical research, the concentration of the bile component may decrease in diseases associated with insufficient blood supply to the myocardium. According to cardiologists, cardiac ischemia is accompanied by a decrease in the level of unconjugated bilirubin.
Decreased test results may indicate the following diseases:
- functional kidney failure;
- tuberculosis;
- blood cancer;
- exhaustion of the body.
The amount of pigment may decrease if a person abuses strong coffee, tea or suffers from frequent stress.
Low study values are sometimes misleading. To ensure reliable results, the analysis is carried out in the morning before meals.
A blood test will help determine changes in the norm of this component.
- Before blood is drawn, the patient is warned about the purpose of the test.
- Blood is taken from a vein in the arm of an adult, and from a child’s heel or veins on the head. This blood test for bilirubin will show the amount of the component contained in the blood.
- Before the study, the patient should limit himself to fatty foods, drinking alcoholic beverages, and smoking.
- A blood test for bilirubin is taken in the morning because it is forbidden to eat 8 hours before the test.
- Otherwise, the result may be distorted. Infants are not fasted before donating blood.
- Drinking caffeine or coffee.
- Taking medications such as heparin, warfarin, etc.
- Unbalanced diet and prolonged fasting.
- The use of medications to treat diseases of the liver and biliary tract.
- Carrying a child.
- The patient sits or lies down. The nurse applies a tourniquet to the arm, a syringe is inserted into a vein, and blood is taken for analysis.
- The procedure causes almost no pain, and after collection the blood is sent directly to the laboratory.
- If deviations from the norm are detected, the doctor must diagnose the reason for the change in this indicator.
- To do this, it is necessary to undergo a repeat blood test to confirm or refute deviations in the concentration of the substance.
- You may have to undergo additional examination to identify the causes of the disease that provoked the changes.
When deciphering the analysis, the doctor considers several factors: the patient’s age group, his gender.
It compares the indicators with generally accepted standards and analyzes whether the concentration of the substance in the blood is normal, elevated, or whether its level has decreased.
In cases where bilirubin is detected within normal limits, then additional examinations are not required.
If an increase or decrease in concentration is detected, the doctor takes steps to identify the cause of the pathological abnormalities.
For this purpose, additional tests may be carried out and taken.
Causes of increased bilirubin in the blood
The main diagnostic value for dysfunctions and diseases is excess of bilirubin standards in both fractions. The pathological threshold for hyperbilirubinemia is 34 microns per 1 liter of blood; at this concentration, jaundice develops as a syndrome. The accumulation of bile pigment in the subcutaneous tissues, sclera, and mucous surfaces leads to the appearance of an icteric tint. Contrary to popular belief, jaundice is not synonymous with hepatitis B, although it can occur as part of the symptom complex of this disease. In various diseases and pathologies, the manifestations of jaundice have features characteristic of each individual case. Elevated bilirubin, especially when significantly higher than normal, is a sign of a health- and, in some cases, life-threatening condition. The reasons for the increase in free and bound fractions are divided.
If direct bilirubin is elevated, this can cause diseases such as:
- acute viral hepatitis A, B, secondary hepatitis due to infectious diseases such as mononucleosis;
- chronic form of hepatitis C, hepatitis of autoimmune etiology;
- hepatitis of bacterial etiology due to brucellosis, leptospirosis;
- consequences of food poisoning, medications (non-steroidal anti-inflammatory drugs, hormonal contraceptives, etc.);
- gestational jaundice in women during pregnancy;
- tumor formations in liver tissue;
- some genetic abnormalities and syndromes that are factors in the development of hereditary jaundice.
In most cases, direct bilirubin exceeds standards in diseases and conditions associated with damage to liver tissue. Diseases accompanied by an increase in the concentration of indirect bilirubin:
- some types of congenital hemolytic anemias;
- mismatch of blood type, Rh factor when donating blood and its components;
- autoimmune, resulting from the development of an autoimmune disease (systemic lupus erythematosus, rheumatoid arthritis) hemolytic anemia;
- diseases of infectious etiology (general sepsis, malarial fever, typhoid fever);
- hemolytic anemia, provoked by uncontrolled use of medications (acetylsalicylic acid, insulin, a group of cephalosporins, penicillins, non-steroidal anti-inflammatory drugs);
- hemolytic anemia of toxic etiology (poisoning from snake bites, consumption of mushrooms, contact with arsenic, copper sulfate, poisons, etc.);
- hereditary diseases
Photo: Africa Studio/Shutterstock.com
Symptoms and causes of pigment deficiency
Reduced bilirubin is less than 3 µmol/l. This happens infrequently, and sometimes it is associated with the presence of severe pathologies. There are practically no symptoms.
The main reasons provoking deviations from the norm:
- treatment with certain medications;
- excess vitamin C in the body;
- abuse of coffee (its individual components affect the concentration of this substance).
A decrease in bilirubin in the female body occurs in the following cases:
- chronic kidney pathologies, both hereditary and as a result of frequent inflammation;
- acute leukemia, which occurs in the bone marrow and impedes the formation of red blood cells;
- aplastic anemia is a rare blood disease that requires urgent medical intervention and complex treatment, resulting from radioactive radiation, poisoning with poisons or medications, and autoimmune pathologies.
Coronary artery disease negatively affects the level of bilirubin, significantly reducing it.
Causes of increased bilirubin in the blood
If liver function is impaired, preventing conjugation, excessive production of bile pigment in the body, or difficulty in the outflow of bile, the content of bilirubin in the serum begins to increase. The reasons for high bilirubin detected during the analysis of blood components are different, but always have a direct correlation with its excess production or dysfunction in the hepato-biliary system.
The accumulation of bilirubin as its concentration increases manifests itself in several stages. First of all, a yellowish tint appears on the sclera of the eyes, then yellowness of the oral mucosa occurs, at the next stage the yellowness spreads to the face, the surface of the palms, soles and covers the rest of the body. A common symptom accompanying jaundice with hyperbilirubinemia is itching.
Yellow skin may not necessarily be a sign of increased bilirubin. This pigmentation feature can occur with excessive accumulation of carotene, for example, with excessive consumption of carrots and tomatoes. Yellowness of the skin is included in the symptom complexes of diabetes mellitus and hypothyroidism. A distinctive feature is the invariability of the color of the sclera.
Manifestations of the disease
Symptoms may vary depending on the degree of pathology, the reasons for the increase in the indicator, and the amount of pigment.
- With anemia and anemia, weakness, increased fatigue, pale skin, enlarged spleen and dizziness with migraine begin.
- In case of liver diseases, the color of urine changes, there is discomfort in the hypochondrium area on the right, hepatic colic, bitterness in the mouth, and lack of appetite may be disturbing.
- If there is a problem with the gallbladder and its pathways, a person feels bloating, decreased appetite, flatulence, aversion to food, and nausea.
In addition, all patients with elevated bilirubin have yellow skin. Nausea, vomiting, fever, and upset bowel movements may occur.
Types of jaundice depending on the cause of high bilirubin
Increased free and direct bilirubin are detected as a consequence of one or more factors that provoke hyperbilirubinemia:
- increasing the number of red blood cells, accelerating the process of destruction of red blood cells;
- non-free excretion of bile;
- pathology of the process of processing and/or excretion of bile pigment.
Increasing the number or accelerating the process of destruction of red blood cells
Increased breakdown of blood cells - red blood cells - causes the development of hemolytic jaundice, accompanied by an excess of standards for indirect bilirubin. This condition occurs with hereditary defects of red blood cells, as well as with significant hemorrhages (extensive hematomas, infarctions of lung tissue), some infectious diseases, malignant tumors, poisoning, as well as with a mismatch of blood type and Rh factor in the donor and recipient or in the mother and fruit. Hemolytic jaundice is manifested by the following symptoms:
- lemon-yellow tint of the sclera, mucous membranes, and skin;
- pale skin as a result of anemia;
- increased volume of the spleen, accompanied by pain in the left hypochondrium;
- dark color of urine and feces due to high concentration of urobilin;
- general deterioration of health due to insufficient oxygenation (headache, increased heart rate, increased fatigue), a possible increase in temperature to low-grade levels.
Bile flow disorders
With various disturbances in the removal of this biological fluid from the liver, conjugated bilirubin, instead of being excreted from the body, enters the bloodstream, which contributes to the development of so-called subhepatic jaundice. The most common causes of disruption of bile outflow include:
- the occurrence of obstacles in the bile ducts (gallstones, tumor formations, tissue pathologies, parasites);
- injuries, tumors compressing the bile ducts;
- diseases of the tissues of the biliary tract of an inflammatory nature, provoking hardening of the ducts;
- congenital pathologies of the biliary tract.
Subhepatic jaundice is manifested by the following symptom complex:
- pronounced yellowness of the sclera, skin, mucous membranes;
- sensation of skin itching of varying severity, from mild to unbearable;
- signs of disruption of the gastrointestinal tract - increased gas formation, nausea, dyspepsia, lack of appetite, reflux of food mass from the stomach into the esophagus, etc.;
- The color of stool with this type of jaundice is light, almost white, which is associated with a reduced amount of stercobilin, urine is dark;
- pain in the area of the right hypochondrium.
With this type of jaundice, blood tests reveal an excess of conjugated bilirubin.
For any reason, it is worth remembering that the severity of external manifestations of hyperbilirubinemia depends not only on the stage of the disease or pathology, but also on the characteristics of the skin, physique, and accompanying symptoms. Thus, with increased deposition of fatty tissue or swelling, jaundice of the skin is much less noticeable than with a thin build.
Treatment of pathology
Normalization of the amount of bilirubin in the blood begins with a complete examination of the body. The action is performed to identify the root cause of the deviation of the indicator from the norm and develop adequate treatment to get rid of the pathology.
If the level of bilirubin in a woman’s blood is elevated, the main treatment method is infusion therapy. During it, an intravenous infusion of glucose, detoxification drugs and special solutions is administered to help remove excess bilirubin from the human body. However, the above method is resorted to only in the most extreme cases.
An easier way to treat pathology is the so-called phototherapy. During its implementation, the patient is irradiated with special lamps. They do not harm the human body. This effect contributes to the destruction of indirect bilirubin, which is highly toxic. Such an impact leads to the fact that the substance is converted into a direct form. It is less toxic and is easily excreted by the body.
Phototherapy is the safest way possible. This makes it possible to use it even in the treatment of pathology in infants under one year of age.
If phototherapy does not help, medications that stimulate the flow of bile may be prescribed. Additionally, a woman must adhere to a diet. Diet is a concomitant condition for any method of therapy prescribed to combat elevated levels of bilirubin in the blood. To bring the indicator value back to normal, you must stop using:
- strong tea;
- flour;
- alcohol;
- coffee;
- canned;
- fried;
- chocolate;
- smoked
A limit on the quantity of consumption is introduced. In particular, you should not eat the yolk. While on a diet, your doctor may prescribe activated charcoal or its analogues. This will speed up the cleansing of the body from toxic substances. Decoctions of rose hips, mint with St. John's wort and motherwort, as well as a number of other natural infusions, can help in the fight against normalizing the level of bilirubin in the blood.
Additionally, treatment of the underlying pathology is carried out. Therapy is selected depending on the results of the studies. Not only the level of bilirubin in a woman’s blood is taken into account, but also other indicators indicating the general condition of the human body. In some cases, hospitalization may be necessary.
If the level of bilirubin in the blood is too low, therapy will be aimed at combating the underlying disease or condition that provokes this phenomenon. There is no artificial increase in the amount of the substance in the blood.
So how to treat?
First of all, it is necessary to accurately determine the cause. For this purpose, an extensive examination is prescribed using laboratory and instrumental diagnostic techniques. Based on all the results obtained and the medical history, the doctor makes a final diagnosis.
Further treatment tactics depend on the pathology. Hepatoprotective drugs, as a rule, are an obligatory component of complex therapy. Their activity is aimed at improving the normal functioning of hepatocytes.
In case of bile stagnation, choleretic drugs are selected (ursodeoxycholic acid is highly effective).
If a patient is diagnosed with a hereditary disease (Gilbert's jaundice), then treatment is considered successful if it allows to achieve the longest possible remission. In this case, the main therapeutic measures are aimed at alleviating specific symptoms. For Gilbert's syndrome, Barboval® can be prescribed (phenobarbital, which is part of it, binds bilirubin and accelerates its utilization), B vitamins, probiotics and ursodeoxycholic acid®.
To eliminate viral hepatitis, direct-acting antiviral drugs are indicated along with immunostimulants. Critical situations with terminal liver cirrhosis require surgical intervention - organ transplantation. Treatment of intoxication necessitates the selection of sorbents and antioxidants.
In addition, the patient is prescribed a special diet that completely prohibits alcohol, fried and fatty foods, as well as coffee and carbonated drinks.
After completing the full course of treatment, a repeat analysis is performed. To eliminate instrument errors, it is advisable to submit biomaterial in the same laboratory. The results obtained indicate that the level of direct bilirubin in women indicates effective therapy and complete recovery. The absence of a positive trend determines the need to correct the chosen treatment tactics.
Bilirubin is a product of pigment metabolism, which is formed from hemoglobin contained in destroyed red blood cells. It has a red-brown color. This process occurs in the liver. Bilirubin is excreted in bile, feces and urine.
The products of its processing include stercobilin and urobilin, which give feces and urine their characteristic color. Based on the level of bilirubin in the blood, one can judge the functioning of the liver and metabolic processes in general. The level of bilirubin in the blood of women ranges from 5.1 to 17.3 µmol/l.
In the male half of humanity, the upper limit of total bilirubin can reach 20.5 µmol/l.
Education
Erythrocytes or red blood cells contain hemoglobin, which carries oxygen to all organs and tissues of our body. Over time, these cells become damaged.
The destruction of red blood cells occurs mainly in the liver, and a small part of them is destroyed in special cells of the spleen and bone marrow.
In this case, hemoglobin is released and, through certain biochemical reactions, is converted into bilirubin.
Factions
There are total, direct and indirect bilirubin.
- Total bilirubin is the entire pigment volume contained in the blood plasma. It includes direct and indirect bilirubin.
- Conjugated (or direct) bilirubin is soluble in water. It is one of the components of bile and is excreted from the body along with feces.
- Indirect (or unconjugated) bilirubin is insoluble in water. It's toxic. During certain reactions in liver cells, it binds and turns into direct bilirubin.
The insoluble fraction, i.e. indirect bilirubin, is toxic. In order to neutralize it, it is converted into a soluble form in the liver, i.e. into direct bilirubin.
In laboratory studies, total bilirubin readings are key. The bilirubin level in women is slightly lower than in men. If the bilirubin content exceeds the permissible values, then pay attention to which of the fractions is increased. An increase in the indirect fraction of bilirubin is a cause for concern, because it is toxic.
Measuring bilirubin levels is important in diagnosis. The level of bilirubin in the blood of women is somewhat different from that of men. In newborns it depends on age. Indicators of total, direct and indirect bilirubin allow us to judge the condition of the liver and its functioning. What is the normal level of bilirubin in the blood of women and men? This is clearly seen from the table below.
| Thrace bilirubin | Women | Men |
| General | 5,1-17,3 | 5,5-20,5 |
| Straight | 1,5-4,7 | 1,7-5,1 |
| Indirect | 3,2-12,0 | 3,5-12,5 |
Normally, approximately 75% of the total bilirubin level should be direct bilirubin. The norm for women and men for this indicator does not differ significantly. The level of bilirubin in the blood of women is slightly lower than that of men. This is due to the fact that representatives of the fair sex have slightly fewer red blood cells in their blood.
Bilirubin in newborns requires special discussion. Here the norms will be completely different and they will depend on the age of the newborn. Thus, in children aged 3-4 days, so-called physiological jaundice may appear, which disappears after a few days. This process is absolutely normal, so there is no need to be alarmed.
| Age | Norm of bilirubin |
| At birth | 49-64 |
| 3-6 days | 150-200 |
| 12-21 days | 8,5-20,5 |
In premature babies in the first two to three weeks, the norm of this indicator is slightly lower and is 172 µmol/l. If the bilirubin value is higher than indicated, then we can talk about pathological jaundice, and this condition requires hospitalization - examination and treatment in a hospital.
The level of bilirubin in the blood in women should not exceed 17.3, in men this figure should not be higher than 20.5 µmol/l. If this value is higher than the specified value, then this may indicate a pathological process occurring in the body. It could be:
- Hepatitis (A, B or C).
- Cholecystitis.
- Hereditary disorders of bilirubin metabolism.
- Cirrhosis of the liver.
- Mononucleosis.
- Tumor processes in the liver, including cancer.
- Hemolytic anemia.
- Pancreatic tumors, including cancer.
- Transfusion of donor blood incompatible with the recipient's blood.
- Reaction to drugs.
- Drug overdose.
- Alcohol poisoning.
A decrease in bilirubin levels can be observed while taking certain medications, for example, Phenobarbital, Theophylline or vitamin C.
A special biochemical analysis allows you to determine blood bilirubin. We found out what the normal level of blood bilirubin is. Now let's talk about indications for determining bilirubin levels. This analysis is prescribed in the following cases:
- With a comprehensive examination of blood biochemistry.
- During a comprehensive diagnosis of patients undergoing inpatient treatment.
- If you suspect hepatitis A, B or C.
- If cirrhosis of the liver or other pathology of this organ is suspected.
- For cholecystitis, pancreatitis and cholelithiasis.
- For tumor processes of the liver.
- In case of poisoning due to medications, drugs or alcohol.
- For hemolytic anemia.
- To monitor the effectiveness of therapy.
The normal level of bilirubin in the blood of women is no higher than 17.3 µmol/l; in men this figure is slightly higher.
Where to do the analysis?
The level of bilirubin in the blood can be determined in any biochemical laboratory. Blood is donated for this study from a vein in the treatment room. This is usually done in the morning on an empty stomach. The last meal is allowed at least 4 hours before blood sampling. There are no restrictions on food intake for children before taking the test.
For newborn children, there is a non-invasive method for determining this indicator. It is determined by a special device - a transcutaneous bilirubinometer. This device is able to determine the concentration of bilirubin by the color intensity of the skin.
Several factors can distort the true values of bilirubin. Therefore, it is better to exclude them on the eve of the bilirubin test. These factors include:
- Coffee and medicines containing caffeine.
- Taking medications such as Warfarin, Aspirin, Heparin.
- Choleretic drugs.
- Strict diets and prolonged fasting.
- Pregnancy.
During pregnancy, bilirubin should remain normal. A slight increase is possible in the third trimester. This may occur due to a violation of the outflow of bile.
In any case, if an increase in bilirubin concentration is observed, this fact requires careful diagnosis and treatment.
Pathologies of the processing and excretion process as causes of high bilirubin
Disturbances in the process of metabolism and excretion of bilirubin from the body are one of the factors contributing to the constant increase in its concentration. Among the diseases and pathologies, there is a group of hereditary jaundice, caused by genetic abnormalities, and acquired, arising as complications of diseases.
Increased bilirubin in hereditary jaundice
The hepatic processing step consists of conjugation of free bilirubin, transport and removal. Disturbances in this process may be associated with genetic pathologies in the following diseases:
- Gilbert's syndrome is the most common pathology caused by an enzyme deficiency that prevents the conjugation of bilirubin in the liver cell. This form of hyperbilirubinemia is considered the most easily occurring and can be asymptomatic with episodes of exacerbation due to stressful situations, illnesses, injuries, excess load on the liver (alcohol abuse, fatty, spicy foods, etc.). The frequency of occurrence in the population depends on the region: for example, in the European population, Gilbert's syndrome is registered in 3-5 people out of 100; in the countries of the African continent this figure reaches almost 40%. The prognosis of the disease is favorable; if the rules for preventing exacerbations are observed, therapy is not required;
- Crigler-Najjar syndrome;
- Dubin-Johnson syndrome.
Acquired jaundice
Acquired jaundice is one of the most common types of icteric symptom complex. There are prehepatic jaundice, in which excess bilirubin cannot be processed by the liver, and hepatic or parenchymal jaundice.
With parenchymal jaundice, damage to the parenchyma and bile ducts leads to disturbances in the uptake, binding and excretion of bilirubin, and its return to the blood serum during bile stagnation. This pathology is accompanied by increased direct bilirubin in the blood. Why does hepatic jaundice occur?
The most common causes of hepatic jaundice are liver diseases. Among them are cirrhosis of the liver and hepatitis of various etiologies.
Liver cirrhosis can be a consequence of various diseases, as well as alcohol addiction and other toxic effects on the body. This is a condition of the liver in which a change in its tissue occurs, a violation of the histoarchitecture of the parenchyma. Normal liver tissue is replaced by connective tissue, blood supply and transportation of bile through capillaries are disrupted. These processes develop due to damage or death of liver cells.
When the liver tissue is replaced by connective tissue, the organ is not able to fully function, including the function of conjugation and excretion of bilirubin. Most often, cirrhosis develops in the last stages of hepatitis, as well as with severe alcoholism.
The clinical picture of cirrhosis includes parenchymal jaundice with characteristic additional manifestations: increased volumes of the liver, spleen, severe skin itching, abdominal ascites, varicose veins of the esophagus and intestines.
Liver failure with progressive cirrhosis is accompanied by damage to brain tissue, decreased blood coagulation, internal hemorrhages and extensive bleeding.
Hepatitis as a disease accompanied by hepatic jaundice can have a diverse etiology. The inflammatory process in the liver during hepatitis can be a consequence of a viral infection, an autoimmune disease, toxic damage or alcohol poisoning.
There are acute and chronic stages of hepatitis. Among acute hepatitis, the most common is infectious hepatitis, caused by various hepatitis viruses. Common symptoms of infectious hepatitis include:
- a picture of general intoxication of the body: nausea, headaches, fever, etc.;
- pain in muscles, joints;
- pain in the right hypochondrium during palpation or occurring spontaneously;
- yellowness of the sclera and skin of varying degrees of severity;
- changes in the color of stool and urine;
- a characteristic change in the blood picture detected during laboratory diagnostics.
The progression of the disease may be accompanied by a transition to the chronic stage, degeneration of liver tissue, damage to brain tissue (hepatic encephalopathy), a combination of liver and kidney failure, which can lead to death.
Carrying out diagnostics
If there is a suspicion of increased bilirubin levels in the blood, you should consult a physician. He will examine the patient, paying attention to the color of the sclera and skin, as well as the presence of a viscous coating on the tongue. Additionally, the size of the liver is assessed. If inflammation is present, the organ acquires fairly clear contours and can be palpated. If it turns out that the problem is in the liver, the therapist will refer the patient to an infectious disease specialist or gastroenterologist. If at the time of the patient’s treatment the presence of a tumor process is known, the oncologist will carry out treatment. In this case, a biochemical blood test is prescribed. It is carried out by collecting material from a vein. The analysis is carried out on an empty stomach. Additionally, liver tests can be performed.
The doctor may prescribe an ultrasound of the liver. It will allow you to visualize the contours of the organ, find out its exact location, and also find out the condition of the bile ducts and parenchyma.
A detailed clinical blood test is also performed. With its help, the doctor can get an idea of the general condition of the body. If leukocytosis is present, this indicates the presence of inflammation. If there is a low hemoglobin concentration, this may indicate the development of anemia.
In order to determine exactly how the indicators will change, a Harrison test may be prescribed. The essence of the method is to study the ability of bilirubin to be oxidized to biliverdin. The process is carried out under the influence of reagents. The doctor may order additional tests. They depend on the preliminary diagnosis.
Bilirubin as a cause of newborn jaundice
Jaundice of a newborn baby, which is a cause of concern for many young parents, refers to the physiological phenomena of the child’s body adapting to life outside the mother. Physiological jaundice of newborns is also a manifestation of hyperbilirubinemia. After birth, the hemoglobin present in the fetal blood breaks down, being replaced by a new form of hemoglobin. This process is accompanied by a partial breakdown of red blood cells and, as a result, an increase in the amount of bilirubin. So the most common cause of jaundice in children during infancy is bilirubin, which the liver will successfully convert into a bound form within a few days without consequences for the child’s health.
Photo: Paul Hakimata Photography/Shutterstock.com
As a rule, the highest concentration of bilirubin in infants is observed on days 3-5, after which the levels begin to decrease on their own. However, physiological jaundice in children does not always go away on its own and without consequences. If the indicators are exceeded, it is necessary to identify the cause and timely elimination of the hyperbilirubinemia factor and symptomatic therapy. With an increased content of unconjugated bilirubin, this fraction is able to penetrate the blood-brain barrier and cause the development of a condition such as kernicterus, damage to the nuclei of the brain, a condition that threatens severe health problems and death. What factor can cause the development of a pathological form of hyperbilirubinemia in a newborn? Factors that provoke the development of this condition include prematurity of the fetus, Rh conflict in mother and baby, congenital pathologies of the biliary tract, liver, etc. With insufficient nutrition in the first days of life, intestinal pathologies or spasms that make defecation difficult, anomalies of the urinary tract bilirubin can also reach critical values against the background of physiological jaundice in newborns.
Folk remedies
It is possible to normalize bilirubin levels, in accordance with the table, in a woman’s body at any age through the use of traditional medicine recipes.
An infusion prepared from corn silk stabilizes the functions of the liver, biliary tract and kidneys. Take 1 d.l. stigmas, pour 200 ml of boiling water, then keep in a steam bath for 15–17 minutes.
Then the infusion is allowed to cool for 45–50 minutes, after which it is filtered and water is added so that the volume is 200 ml. Before use, the infusion is heated and shaken. Drink it every 2–4 hours, 1–3 tbsp. for adults, and 1–2 d.l. for children for a month.
Tea made from chamomile flowers effectively reduces bilirubin. For this, 1 tbsp. the herbs are placed in a teapot and 200 ml of boiling water is poured in, left for half an hour and filtered. The liquid is then divided into three equal parts, which should be taken after each main meal.
Adding 1 tsp. mint leaves in tea help normalize digestion, improve the functioning of the liver and gall bladder. This tea can be drunk for 1.5–2 months.
A decoction of birch leaves effectively reduces the level of bilirubin in the blood. 3 tsp you need to pour 1 tbsp. boiling water and leave for 25–30 minutes. The resulting broth is divided into 8 equal parts. Drink 1 part 4 times a day. Store in the refrigerator.
For the infusion of St. John's wort, you need to take 2 tbsp. herbs and pour 200 ml of boiling water over them. Leave for 30 minutes and then filter. You need to drink the infusion in the morning and evening after meals, 100 ml. The course of treatment is usually 1 month.
The substance and its function in the female body
, has a reddish-yellow color, one of the intermediate products of the breakdown of hemoglobin that occurs in the spleen.
This is indirect bilirubin; above the norm for women, it is toxic and poisons the entire body.
From the spleen it enters the liver, where direct bilirubin is formed. It removes all toxins through the production of bile. This process occurs continuously.
Total bilirubin shows a woman’s health, the condition of her liver, and diseases associated with blood disorders.
The peculiarity of this indicator is that it is lower in women than in men.
Women produce fewer red blood cells and have lower hemoglobin. The result is a lower bilirubin value.
The importance of monitoring the indicator and the consequences of imbalance
The exception is newborns. Their pigment amount is very high, but by the end of the first month it decreases to the level of an adult.
| Age | General | Indirect | Straight |
| (µmol/l) | |||
| Newborn | 23,9 | 8,72 | 14,4 |
| 1-3 day | 54,3-90,1 | 7,87 | 45,5-82,3 |
| 5-10 day | 52,02-69,1 | 7,72-7,82 | 44,3-63,3 |
| 1 month | 9,2-14,5 | 1,2-4,5 | 6,7-10,4 |
| Over a month and adults | 3,2-17 | 6,4-16,8 | 0,9-4,3 |
Each laboratory's equipment and reagents have their own standards. Laboratory test forms must be consulted.
An increase in bilirubin during ovulation and climate change is also considered normal. This usually manifests itself in the fact that the woman will want sweets.
A slight increase in this indicator may occur in women in the last trimester of pregnancy. But this does not affect the child or the mother in any way. This is due to the greater load on the expectant mother's liver.
The norms of the indicator may also change with age due to the influence of external and internal factors on the body.
In the first phase of the menstrual cycle, a slight increase in total bilirubin is observed. However, after it ends, the indicator value returns to normal.
Immediately after birth, the level of bilirubin in the blood can vary greatly over a short period of time. The indicator stabilizes after the first month of life. If this does not happen, the child may have some kind of pathology. To identify the cause of the deviation, it is worth conducting a full examination.
In women, compared to men, the level of bilirubin is slightly lower. This occurs due to the fact that a woman has fewer red blood cells in her blood. However, the rule is not always followed. The specifics of a particular woman’s body and existing diseases may affect the value of the indicator.
For most of a woman’s life, bilirubin in a woman’s blood remains at the same level. After 50 years, no changes occur. Deviations from the average statistical norm can be observed after reaching 60 years of age. Doctors often associate this fact with the occurrence of cardiovascular diseases. This can indirectly lead to a decrease in the level of bilirubin in the blood. However, this fact has not been proven for certain.
Timely blood tests will help identify the development of diseases at an early stage. Experts advise doing this even after taking medications for a long time, since some of them do not have the best effect on the functioning of organs and systems.
The amount of bilirubin in the blood helps to identify liver diseases (hepatitis, cirrhosis), find out about the presence of stones or tumors in the pancreas, and vitamin B12 deficiency.
The greatest danger is the growth of indirect bilirubin, which, being toxic, poisons the body and can affect brain cells.
A decrease in the amount of this substance often indicates coronary heart disease.
When pigment values increase to more than 200 µmol/l, there is a risk of renal or heart failure; with a value from 300 µmol/l, life is threatened.
If a woman does not pay attention to the symptoms indicating an imbalance in the body, then the occurrence of pathology may be overlooked. As a result, the disease will progress, and further treatment will require more time and effort, and there will be a risk of complications.
How to increase
When is it necessary to consult a doctor?
When monitoring your health, you discovered:
- discomfort and feeling of heaviness in the right hypochondrium;
- bitter belching, nausea;
- weakness, fatigue;
- urine color is almost brown;
- elevated temperature;
- itching of the skin;
- severe headaches, dizziness, rapid heartbeat.
If a woman has symptoms of increased bilirubin in the blood, then she urgently needs to consult a doctor.
In order for a woman to be cheerful, healthy and look good, she needs to go to routine check-ups with doctors, take tests, and undergo examinations.
All this will be able to identify the causes of increased bilirubin in the blood of women and prevent diseases at an early stage.
What should you be afraid of when bilirubin increases?
If the disease is associated with a malfunction of the spleen, then this is fraught not only with pain and heaviness, but also with enlargement of the organ. Characteristic hemolytic anemia can lead to internal organs becoming unstable, resulting in their complete failure.
There is another danger - the appearance of hepatitis or cirrhosis, kidney failure. In some cases, if treatment is not promptly provided, cancer of the internal organs may develop.
With a high level of bilirubin, the brain and the entire body experience severe intoxication, which causes a disruption in their functionality with characteristic manifestations.
What is dangerous about high bilirubin levels?
Bilirubin is an extremely toxic substance that causes intoxication and disruption of the functioning of the body's organs. Brain tissue is the most sensitive in this regard.
The remaining systems (liver, kidneys, heart) are more resistant to the effects and are able to function for a long time with an increased bilirubin content.
The duration of such functioning is determined by hyperbilirubinemia - the severity of the increase.
Patterns and degrees of increase in bilirubin
| The degree of increase in bilirubin | Characteristics of the condition |
| Slight excess of the norm | This type of hyperbilirubinemia includes an increase in total bilirubin to a level of 50 to 70 µmol/l. This condition does not pose an immediate threat to the body, since it does not cause toxic damage to organs. A person can live a long time with a slight excess, but it is imperative to determine the cause of the increase. |
| Marked increase in bilirubin levels | In this state, the concentration of bilirubin ranges from 150 to 170 µmol/l. This condition poses a non-critical danger to the body. Prolonged existence with this level of hyperbilirubinemia causes bilirubin intoxication, which must be eliminated as soon as possible. |
| Severe hyperbilirubinemia | It means a condition when the bilirubin level is elevated to a level of 300 µmol/l. In this condition, there is an immediate threat to human life caused by severe intoxication and impaired functioning of organs. |
| Extremely severe hyperbilirubinemia | In this state, indicators exceed a concentration of 300 µmol/l and are critical for human life. If the cause of the increase is not eliminated within a few days, the patient will die. |
Indicators of normal bile pigment
Medicine has established standard norms for the hemoglobin product. The level of the substance is determined using a biochemical blood test. To obtain reliable data, there are certain requirements for taking tests: in the morning you must refrain from eating after sleep, and take the test only on an empty stomach and in the morning. For biochemical analysis, blood must be obtained from a vein.
Important! The normal bilirubin level (total) is 8.5-20.5 µmol/liter. For the indirect fraction, the indicator should be 3.4-17.1 µmol, and for the direct fraction – up to 3.4 µmol.
Even slightly elevated bilirubin is a serious disorder that cannot be ignored or allowed to remain in the body for a long time.
The difference between direct bilirubin and other types
In medical science, there are two types of bilirubin - direct and indirect.
The second of them, also called unbound, is formed in liver cells (about 80%), and the rest is in the spleen and bone marrow cells. Direct bilirubin, called bound, is formed in the liver by adding glucuronic acid to indirect bilirubin. This is required in order to convert a toxic and insoluble substance into a soluble form and successfully remove it from the body with bile.
However, non-toxic and easily soluble direct bilirubin can also have harmful effects on the body. With an increased concentration of this substance in bile, it is prone to precipitation and crystallization, which can ultimately lead to the formation of solid deposits in the structural elements of the gallbladder and its ducts.
The results of laboratory tests often mention total bilirubin, but this is a clinical name; there is no such substance in the body. This concept refers to the total amount of direct and indirect bilirubin.
Features of bilirubin, called conjugated
Direct bilirubin received its name for its ability to react directly with the reagent used in tests. The mechanism of formation of conjugated bilirubin occurs in the liver. Most of it is excreted through the intestines, a small amount is excreted through the kidneys in the urine in the form of urobinogen.
A feature of direct bilirubin is its minimal toxicity, in contrast to indirect bilirubin. A distinctive feature of direct bilirubin is the ability to be excreted from the body due to its solubility. The formation of conjugated bilirubin occurs on the basis of unconjugated bilirubin.
Indirect bilirubin is practically insoluble in water. it requires fats, for this reason accumulation occurs in adipose tissues and brain lipids. Indirect bilirubin is excreted only after conversion to conjugated bilirubin.
The liver produces bilirubin. But a distinctive feature of direct bilirubin is its formation in special cells - hepatocytes. Also, part of the indirect bilirubin is created outside the liver.
An increase in bilirubin does not always indicate a disease; sometimes an increase in levels occurs when the liver is functioning properly.
Reasons for the low value
This phenomenon is quite rare. Typically, a decrease in bilirubin occurs when there is an insufficient level of red blood cells.
Such indicators can be observed if the body contains:
- Kidney failure.
- Tuberculosis.
- Leukemia.
- Severe exhaustion.
If bilirubin is low, then before starting treatment, it is recommended to repeat the test in another clinic. It is advisable to take the material on an empty stomach, eliminating all kinds of physical and emotional stress.
To normalize the indicator, you need to cure the underlying disease.
Many people do not understand what it means when bilirubin is elevated and why it is dangerous. This is a pigment with a toxic composition, and its amount in excess of the norm is fraught with severe intoxication of the body and damage to internal organs.
Treatment of pathology includes the use of choleretic agents, enzymes, hepatoprotectors, drugs to improve liver function and eliminate intoxication, and immunomodulators. Elevated bilirubin is common, especially in newborns, while low bilirubin, on the contrary, is extremely rare at any age.
The patient becomes anxious when the doctor orders a blood test for bilirubin. When is such an analysis needed, what are the standards for its indicators? The most important thing is what do increased or decreased values indicate? This issue should be dealt with in order to begin timely treatment.