Blepharitis is a group of diseases associated with inflammation of the ciliary margin of the eyelids, predominantly of infectious or allergic origin, prone to long-term progression and frequent relapses. The disease is difficult to treat and can sometimes cause infection of the eye and weakened vision.
With blepharitis, the eye as a whole may remain unchanged, which often leads to the mistaken belief that the disease is trivial and does not require treatment. In fact, this is not the case, and with long-term blepharitis, the eyes are constantly exposed to infection, which can cause significant problems, including deterioration of vision.
Causes
The causes of the disease are:
- reduced immunity;
- allergic reactions;
- vitamin deficiency (lack of vitamins in the body);
- anemia (lack of hemoglobin in the blood);
- recent infectious eye diseases (may appear as a complication of a current disease);
- use of low-quality cosmetics (mascara, eye shadow);
- demodicosis of the eyelids (a disease caused by a skin mite);
- hereditary predisposition (if the parents had chronic blepharitis, then there is a high probability that the child will also develop this disease);
- excessive consumption of alcohol, drugs, smoking (bad habits negatively affect the immune system and destroy the body);
- diabetes mellitus, cancer, HIV;
- diseases associated with the digestive system (poisoning, ulcers, gastritis);
- working with hazardous substances;
- spending a long time in the sun, in dusty rooms, long walks in windy weather.
It can be concluded that the causes of the disease are divided into two groups. Firstly, it appears due to the entry of infectious bacteria into the visual apparatus (most often associated with reduced immunity). The second group of causes of pathology is allergic reactions.
With allergies, the patient often experiences an inflammatory process (blepharitis) in the eyelid area.
Vision can be restored without surgery
Non-surgical eye treatment in 1 month...
>
Blepharitis in children
Blepharitis in children develops if the skin of the eyelids is thin, and the deeper tissues are loose and contain little fat. The disease can go unnoticed for a long time, so treatment often begins when the pathological process is already in full swing.
The most common cause of pathology is the active reproduction of Staphylococcus aureus with a general weakening of the body.
Factors that provoke the disease in a child are:
- hypothermia;
- decreased general immunity;
- past infectious diseases;
- physical or nervous stress;
- chronic diseases of the digestive system;
- diabetes;
- helminthic infestations;
- allergic reactions;
- various metabolic disorders;
- contact with mechanical particles in the eyes;
- the presence of chronic foci of infection (sore teeth, inflamed tonsils, etc.).
If blepharitis is diagnosed, the baby, in addition to the medication prescribed by the doctor, needs to adjust the diet (in some cases, a special hypoallergenic diet is indicated). Physiotherapeutic techniques are widely used, including ultraviolet irradiation, ultra-high frequency therapy (UHF), magnetic therapy and electrophoresis with solutions of vitamins and antibacterial agents.
Antibacterial eye ointments such as Colbiotsin, Oriprim-P and Oftalmotrim have proven their effectiveness. Eye drops are also widely used - sodium sulfacyl solutions, Picloxidin and Miramistin.
Among herbal remedies for topical use, chamomile decoction and calendula tincture, which are characterized by a pronounced anti-inflammatory effect, are recommended.
Risk group
The risk group is people susceptible to blepharitis. This group includes:
- People suffering from hyperopia (farsightedness - see far, but not close) and do not wear optics.
- People whose work involves sitting at a computer for long periods of time. This group of people includes schoolchildren who need to concentrate their vision on one thing (textbook) for a long time. People in this group constantly strain their eyes. Eye moisture decreases, resulting in ophthalmological problems.
- Women using cosmetics. Often, low-quality cosmetics are purchased, which negatively affect the microflora of the eye.
- People who have recently had infectious eye diseases are most susceptible to the development of pathology.
- People with the following diseases: allergies, diabetes, diseases associated with the gastrointestinal tract (gastrointestinal tract).
The risk group is recommended to pay increased attention to the visual apparatus. Be sure to take ophthalmic vitamins 2-3 times a year.
Folk remedies
We have a huge variety of different recipes open to us. Moreover, you don’t have to go to the field and look for the right plant there, you just need to go to the pharmacy and buy the right herbal mixture. But it must be remembered that any treatment, even with folk remedies, requires the correct diagnosis of the disease or infection.
- Bird cherry infusion is used to rub the eyes in case of acute conjunctivitis, and as a mouth rinse for stomatitis. Due to the high content of amygdalin, the berries are used without seeds. 60 gr. Flowers are poured into 300 ml. Boiling water, leave for 10 hours in a steam bath, filter through gauze and apply to the eyes 2-3 times a day. Contraindications for women with signs of pregnancy, as well as those who have a contraceptive effect.
- Tea lotions: pour boiling water over tea bags and apply them to your eyelids for 20 minutes. Reduces inflammation, soothes itching.
- Apply syntomycin ointment to the edges of the eyelids 3 times a day until the condition completely improves.
- The remedy is especially effective for scaly blepharitis. Bring corn oil to a boil, wait until it cools, lubricate the edges of the eyelids 3 times a day.
- For purulent eye infection. Wash your eyes daily with a 2% aqueous solution of boric acid, and apply lotions with fresh (boiled) cottage cheese before going to bed. This method has its drawbacks. With constant use, acute poisoning of the body, vomiting, diarrhea, headaches, and convulsions occurs.
- Infusion of thyme with chamomile. This collection is a very strong anti-inflammatory agent. Apply lotions 3-4 times a day. There are no contraindications for use, with the exception of a selective allergic reaction.
- Laundry soap works well against Demodex mites. Soap foam is applied to the affected area, after 3-5 minutes it is washed with water and lubricated with Vaseline.
- Ulcerative blepharitis is well treated with an infusion of celandine herb. Pour 2 tablespoons of herbs with a glass of boiling water and let stand for 2 hours. The infusion is ready.
- Scaly blepharitis can be cured with burdock oil; the affected areas of the eyelids are generously lubricated at night.
- To heal wounds on the edges of the eyelids, you can use fresh aloe juice.
- Thyme herb in the amount of 2 teaspoons, pour 150 ml. Boiling water, leave the resulting decoction for 1.5 hours. Has an antibacterial effect. Wipe your eyes with the solution morning and evening.
- Cook 1 onion over low heat for 40 minutes in 0.5 liters of water, strain through a colander. Rinse your eyes with the resulting decoction every 2-3 hours. Healing agent.
- Boil 12 small bay leaves in 0.25 liters of water for 3 minutes. An effective remedy for allergic blepharitis.
- Herbal mixture for eye baths - take chamomile, string grass and calendula leaves in equal parts. 2 tablespoons of the resulting mixture, pour 170.0 ml of boiling water and place in a water bath for 10 minutes, preferably leave for 1-2 hours. Cool, moisten sterile cotton swabs and apply to eyelids for 25 - 35 minutes. This collection is an anti-inflammatory and antiseptic, helps with various forms of blepharitis.
- The method is not for the picky. We take our urine, moisten a cotton or gauze swab generously, and place it on the eyes. At this moment, try to blink so that the liquid gets onto the infected areas or wounds. This method does not require any special preparation. Very effective.
Classification
Depending on the characteristics of the causative agent of inflammation, the following types of blepharitis are distinguished:
- Demodectic mange - develops due to penetration of a skin mite under the skin. This mite lives on the skin of almost the entire population. Under the influence of factors (usually infection), it penetrates inside and begins to have a destructive effect on the human visual apparatus. It does not manifest itself as actively as other types of pathology. Itching, burning, and mild pain are observed. There are small scales along the edges of the eyelids.
- Scaly. Small scales form on the skin. Scales are dead tissue cells. They cling tightly to the skin, so trying to “pick” them off is not recommended. This action may cause a wound. The pus from scaly blepharitis is removed. Does not leave behind scars, ulcers, wounds with proper treatment.
- Allergic. With an allergic type of inflammation, blepharitis is considered a secondary symptom of an allergy. Often “connected” with other inflammatory diseases. People who experience allergy attacks are concerned about conjunctivitis (inflammation of the mucous membrane of the eye).
- Ulcerative blepharitis. Triggered by the penetration of infectious bacteria into the body. Ulcerative blepharitis is characterized by the appearance of small purulent ulcers. Eyelashes stick together. Ulcerative blepharitis primarily affects the eyelash cells. Therefore, after suffering from the disease, eyelashes may begin to grow incorrectly, and deformation of the eyelids occurs. In order to avoid negative consequences, it is recommended to consult a doctor immediately. After ulcerative wounds, scars often remain.
- Meibomian. Bubbles containing secretory fluid (cellular fluid) appear. Bubbles should never be burst. They disappear on their own after a certain period of time (depending on treatment). Fluid accumulates in blisters due to clogging of the glands. Meibomian blepharitis is a chronic type of disease. Concerns the patient in case of relapse (repetition).
- Rosacea-blepharitis (angular). A rash appears in the eyelid area. Often, in combination with acne of a reddish (pinkish) color.
Blepharitis is classified according to the form of the disease:
- acute, appearing in the patient for the first time (or irregular repetitions);
- chronic, blepharitis bothers a person constantly (regularly).
Depending on the location there are:
- posterior blepharitis;
- front;
- corner (angular).
All types are treatable. The main thing is to see a doctor in time. Follow the prescribed course of treatment and follow the recommendations of a specialist.
Types of blepharitis
Based on location, blepharitis is divided into anterior and posterior.
The anterior inflammatory focus is often seborrheic or infectious; small pustules appear at the location of the cilia. Posterior blepharitis involves the meibomian glands, which form the tear film, in the pathological process. These two types can occur simultaneously.
According to the classification, blepharitis is distinguished by etiology, clinical manifestations, and severity of the disease.
Infectious (ulcerative) blepharitis
The disease develops against the background of a bacterial infection (staphylococcus). The hair follicles of the eyelashes become inflamed, and pus is produced in the follicles. Over time, chronic ulcers form along the edges of the eyelids. Yellow scabs are noticeable on the eyelashes, and the hairs are stuck together. After removing the dried crusts, the ulcerated surface of the epidermis and mucous membrane opens. After healing, characteristic scars remain.
In severe chronic ulcerative blepharitis with frequent exacerbations, some eyelashes become white and fall out. The skin along the edges of the eyelid is wrinkled. After healing, scarring causes eyelashes to grow in the wrong direction.
Allergic
This form of blepharitis in 98% of cases is combined with rhinoconjunctivitis (seasonal allergic inflammation of the mucous membranes of the eyes and nose). The disease occurs suddenly and has an acute development with the following symptoms:
- itching, burning of the conjunctiva;
- redness of the eyeball, eyelid;
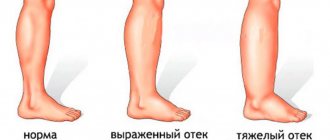
- severe swelling on the face;
- lacrimation;
- pain in the eyes in bright sunlight.
A distinctive feature is that both eyes are affected equally. If the pathology has become chronic, the patient experiences unbearable itching. Exacerbations of inflammation are diagnosed during the flowering season of plants.
Some people develop drug-induced blepharitis during long-term therapy with pharmacological drugs (eye ointments, gels, drops, less often when taking medications orally).
Scaly
This is a simple form of the inflammatory process. Patients experience redness of the eyelids, moderate swelling, and thickening around the edges. Scales form on the skin as a result of desquamation of epithelial cells of the sebaceous glands and epidermis. The scales are located at the base of the eyelashes, tightly attached, and difficult to remove.
Demodectic
Blepharitis due to a parasitic infection. When a hair (cilium) is removed, a mite is found at its root.
Inflammation differs in its clinical course. At the beginning of the development of the disease, the eye is constantly itchy, irritation intensifies in the morning, after waking up. An abundant sticky exudate appears, which is constantly released from the mucous membrane, causing the desire to wipe the eyelids. Cutting pain may occur in the eye socket.
As blepharitis progresses, the eyelash follicles become inflamed. The edges of the eyelids become bright red and thicken. A distinctive feature is the formation of a “collar” at the base of the cilia along the entire edge of the eyelids. These are dead cells and secretion secreted by the sebaceous glands. Exudate accumulates between the hairs and gradually dries out, which gives the appearance when a person does not follow the rules of personal hygiene.
Meibomian
This is blepharitis, provoked by increased secretion of the meibomian glands, the ducts of which emerge at the edges of the eyelids. These are modified glands that produce sebum.
Inflammation is caused by hypersecretion and partial or complete obstruction of the excretory ducts. Pathology is more often diagnosed in children.
Acne blepharitis (rosacea)
The origin of acne blepharitis is unknown. It is characterized by the appearance of small dense red-gray nodules on the eyelids. Around them are located pustules - an element on the skin in the form of vesicles containing purulent exudate. Rashes in the form of rosacea are often observed.
This form of blepharitis is associated with the following internal factors:
- genetic disorders of vascular regulation;
- gene expression, as a result of which the capillary endothelium grows rapidly;
- malfunctions of the immune system and digestive tract.
With ophthalmic rosacea, 50% of patients first develop eye symptoms - inflammation of the mucous membrane, hyperemia, irritation. A person is being treated for common conjunctivitis. And only after 1-2 years the first signs of the disease appear on the skin of the eyelids. In 8-16% of patients, the disease occurs in a severe form (damage to the deep layers of the skin, sclera, cornea).
Angular
If the lesion is localized only at the edges of the eyelids, in the corners of the eye, such blepharitis is called angular or angular.
At the site of inflammation, redness develops and exudate resembling foam is released. The eyelids thicken at the corners, become dense, and difficult-to-heal cracks appear on them.
The disease is more often found in adolescents and people of working age.
Symptoms
The pathology is easily recognized by a swollen eyelid. This is precisely the primary symptom. Also signs are:
- sticky eyelids;
- formation of yellow secretion in the corners of the eyes (especially in the morning);
- sensation of a foreign body in the eye (dust, sand, small particles);
- sticky eyelashes;
- the appearance of small ulcers, yellow crusts;
- redness and thickening of the eyelids;
- burning, itching (eyelids do not stop itching);
- sometimes there is an increase in temperature;
- increased lacrimation;
- acute reaction to light (especially when changing from a dark room to a bright one).
When the first symptoms appear, it is recommended to consult a doctor immediately. Then possible complications can be avoided. It is recommended not to self-medicate. This may lead to undesirable negative consequences.
Causes of blepharitis
The main causes of the disease in adults are as follows:
- weakened immune system;
- hidden chronic diseases of a person;
- allergic diseases;
- constant irritants to the eyes (dust, smoke, soap);
- infectious diseases;
- failure to comply with normal hygiene rules;
- mental disorder;
- poor nutrition;
- congenital pathologies (farsightedness, myopia);
- hypothermia;
- chronic diseases of the digestive system;
- diabetes;
- helminthic infestations;
- various metabolic disorders;
- the presence of chronic foci of infection (sore teeth, inflamed tonsils (sore throat, pharyngitis))
The main causes of the disease in children are mainly gross violations of hygiene, contact with small foreign bodies in the eyes, dust, unsanitary living conditions of the child, the use of other people's towels and handkerchiefs, weakened immunity due to vitamin deficiency, and chronic diseases of the human body.
Our body comes into contact with billions of microorganisms every day, which can cause many diseases. But not everyone is able to overcome the barrier of our immune system. A lack of vitamins and microelements in the body weakens it and allows microbes to act and multiply in the human body.
According to medical statistics, the main risk group for this disease is people from 40 years of age to the elderly, but cases of the disease in children caused by Staphylococcus epidermidis (epidermal staphylococcus) are also common.
Diagnostics
Usually, an external examination of the patient is enough for an ophthalmologist to make an appropriate diagnosis. Blepharitis of the eyelids has striking symptoms. This group of inflammations is easy to recognize after external examination.
Therefore, an experienced ophthalmologist does not require additional research.
Sometimes biomicroscopy is performed to clarify the disease and determine the type. The procedure is performed using a special slit lamp. Biomicroscopy allows you to examine the components of the eye (eyelids, mucous membrane, eyeball, cornea). The procedure is based on the contrast of the illuminated area and not. It is thanks to this that a qualitative study of the visual organs is carried out.
In the event that the pathology arose due to the appearance of infectious bacteria, a smear is taken from the person. Allows you to determine the genus and type of bacteria. This is necessary in order to identify the type of inflammation and prescribe the most effective treatment.
If blepharitis has an allergic basis, the patient needs to consult an allergist to prescribe quality treatment.
Symptoms of blepharitis
Symptoms of blepharitis
Here are the signs that can help identify blepharitis:
- purulent discharge from the corners of the eyes and the edges of the eyelids (see photo above).
- sticky eyelashes after sleep.
- burning under the eyelid.
- pain when blinking.
- fear of bright light.
- swelling of the eye bags.
- eyelash loss.
- inflamed edges of the eyelids.
The symptoms of blepharitis in children are identical to those in adults. Standard set of symptoms.
Redness of the edge of the eyelids, swelling of the eye bags, pain in bright light, purulent discharge along the edges of the palpebral fissures and eyelids.
Treatment
Treatment of pathology does not include the use of surgical methods. Can be done with medications, physiotherapy, massage and other conservative methods. This usually covers a long period during which the sick person must follow the doctor's recommendations.
Medicines
To treat inflammation, antibacterial antiseptic drops and ointments are prescribed. Such medications block the proliferation of bacteria and kill the causative agent of the disease. It is important to use medications according to the prescribed dosage. Do not deviate from the dosage prescribed by the doctor.
Physiotherapy
Physiotherapy for blepharitis includes the following activities:
- UHF – exposure of the affected area to a high-frequency electromagnetic field. Has an anti-inflammatory, analgesic effect. The electric field is distributed evenly over the eye area, including deep tissues. UHF reduces the patient's overall discomfort and reduces inflammation.
- Magnetic therapy is the effect of a weak magnetic field on the affected eye. The advantage of this procedure is that no additional contact with the eye is required for treatment. Magnetic therapy can be performed through a bandage. This helps to avoid additional injuries. The procedure is prescribed for a number of infectious and inflammatory diseases.
- Electrophoresis is the direct application of electric current to the affected area. Allows you to reduce the intensity of drug treatment. When using electrophoresis, drugs remain in the visual organ longer. They accumulate. Due to this, the greatest effectiveness of treatment is observed.
- Darsonvalization is the effect of high-frequency pulsed currents on the affected areas. The use of this procedure is possible only after appropriate prescription by a doctor. Darsonvalization is considered a dangerous procedure. If used incorrectly, injury may occur.
- UFO – ultraviolet irradiation. Based on the effect of ultraviolet spectrum on tissues and organs.
The set of physiotherapeutic measures is determined by the attending physician. Depends on the degree of the disease, type and individual characteristics of the patient.
Traditional methods
The use of traditional methods is possible provided that the treatment prescribed by the doctor is followed. Traditional methods can speed up the healing process and make a person feel better.
Diet
For pathology, it is recommended to use:
- dairy products (milk, cheese, cottage cheese);
- vegetables fruits;
- drinking plenty of fluids.
Steam or boil food. Eating fried fatty foods is not recommended. Limit consumption of sweets and salty foods. You should not eat smoked meats.
Massage
Eyelid massage is often prescribed. It accelerates the regeneration of new tissues. Thanks to massage sessions, inflammation goes away faster.
Diagnosis of the disease
An additional examination is prescribed by an ophthalmologist, taking into account the patient’s complaints.
The following methods are used to diagnose blepharitis:
| Name | Description |
| Visometry | Determination of visual acuity. |
| Biomicroscopy | A thorough examination of all ocular structures (eyeball, eyelids, conjunctiva, protective film). |
| Biopsy and tissue histology | Tests can confirm or refute the presence of malignant processes. |
Microscopic examinations help determine the presence of Demodex mites. For allergic blepharitis, allergy tests are performed.
Complications
If blepharitis is not treated sufficiently, the following complications may occur:
- simple blepharitis becomes chronic, periodically bothering the patient throughout life;
- injuries of the cornea, eyelids;
- the appearance of chronic conjunctivitis (inflammation of the mucous membrane of the eye);
- improper eyelash growth;
- the appearance of scars;
- development of abscesses, appearance of chalazions (can only be done surgically);
- chronic dry eye (moisturizing drops are prescribed on a regular basis).
Pathology refers to diseases that are easily treatable. If you consult a doctor in a timely manner, the above complications can be avoided. Complications appear with poor quality treatment and advanced stages of inflammation.
Symptoms of the disease in photographs
Blepharitis is accompanied by the following symptoms:
| White spots under the eyes | Redness | Purulent discharge |
| Discomfort in the eye area | Eyelash loss | Copious secretion of tears |
| Swelling of the eyelids | Peeling skin |
Sometimes, as a result of blepharitis, small blood vessels dilate. Because of this, nets or stars form on the skin. About 50% of cases of the disease are accompanied not by excessive production of tears, but by their lack. This manifestation is called dry eye syndrome. The disease may be accompanied by a fear of light.
It is worth noting: Symptoms of blepharitis are not always permanent. Periods of improvement (remission) may alternate with exacerbations of symptoms of the disease.
Let us consider the symptoms of the disease for some types of blepharitis separately.
Allergic
As a result of allergies, not only the eyelids become inflamed, but also the conjunctiva. The disease is accompanied by itching, pain in the eyes, swelling, flow of tears, and secretion of mucus from the eyes.
Demodectic
The first symptoms are itching and mucous discharge in the affected area. Later, inflammation, thickening of the eyelids and redness of the eyes appear. Dried mucus turns into scales.
Scaly
Sometimes accompanied by seborrheic type dermatitis in certain areas of the skin. The eyelids turn red. Their edges thicken. The skin does not bleed after removing the resulting scales. Dried sebaceous glands form yellowish crusts.
Ulcerative
Drying pus forms crusts. If they are removed, ulcers with blood and pus form. After some time, they are replaced by scars. Loss of eyelashes is observed.
Blepharitis rosacea
The eyelid becomes covered with pink blisters and pustules.
Paying attention to the symptoms, the ophthalmologist makes a diagnosis and prescribes treatment.
Prevention
The possibility of inflammation cannot be excluded. But you can reduce the risk of occurrence. It is recommended to adhere to the following tips:
- maintain immunity (eat fruits, vegetables, take appropriate vitamins 2-3 times a year, spend time outdoors, adhere to a healthy lifestyle);
- maintain personal hygiene (have your own towel, wash your face several times a day);
- take the choice of cosmetics seriously;
- do not touch your eyes with dirty hands;
- treat infectious diseases in a timely manner (blepharitis sometimes acts as a complication of various types of infectious diseases);
It is important to take care of your eyes. It is recommended to visit an ophthalmologist several times a year.
Treatment of blepharitis
Treatment of eyelid inflammation in adults is a long and complex process. To prevent the disease from progressing and relapses, it is necessary to prescribe therapy, taking into account the underlying cause of the disease.
Antibiotics
For ulcerative, meibomian blepharitis, antibiotics are used in the form of ointments for application to the eyelids - erythromycin, tetracycline, syntomycin.
The medicine is applied after removing crusts, plaque, mucus, and pus. To do this, take a swab, generously soaked in an antiseptic, disinfectant solution and carefully remove pathological contamination.
Antiseptics
Drugs with antimicrobial action for blepharitis:
- Furacilin;
- Chlorhexidine;
- Miramistin.
If the patient has a simple scaly inflammation, after washing they are lubricated with an alcohol solution of brilliant green 1%. For angular blepharitis caused by a specific pathogen (Diplobacillus Morax-Axenfeld), zinc ointment and solutions based on this chemical element are prescribed.
Anti-inflammatory drugs
Anti-inflammatory drugs relieve swelling, redness, reduce irritation of nerve endings, resulting in the elimination of itching and burning. Patients are prescribed corticosteroids for topical use.
For scaly blepharitis of the eyelids, dexamethasone and hydrocortisone ointment are prescribed 2-3 times a day. For ulcerative inflammation, Maxitrol ointment is indicated - a complex-action drug based on dexamethasone (hormone), neomycin, polymyxin (antibiotics).
Eyelid hygiene
With blepharitis, eyelid hygiene is of particular importance. In order to cure the disease quickly, it is necessary to carry out daily procedures prescribed by the doctor - washing, disinfection, cleansing, adding medications.
Regardless of the type of blepharitis, eye hygiene is carried out every morning, after a night's sleep.
If you have inflammation of the eyelids, it is strictly forbidden to wash your face with cold water. This will lead to spasm of the veins, stagnation of blood and aggravate the inflammatory process. Warm water, on the contrary, will cause a rush of blood to the affected area, speed up metabolism and tissue regeneration.
After washing, do a light massage of the eyelids, having previously dripped local anesthetics (painkillers) into the eyes - novocaine 2%, dicaine 0.25%. All movements should be carried out towards the edges of the eyelids. When the procedure is carried out correctly, pathological exudate and fatty secretion are released from under the eyelashes.
After the massage, the eyelid is carefully wiped with an alcohol solution using a cotton swab, in the direction from the inner corner to the outer. Do not allow the drug to come into contact with the cornea.
Dry and dense scales are soaked with the prepared furatsilin solution. Make warm lotions for 10-15 minutes from cotton balls or gauze napkins. This manipulation is indicated at night and in the morning when there is increased production of pus. After antiseptic treatment of the ulcers, brilliant green is applied to the cracks.
During treatment, it is prohibited to use decorative cosmetics or wear contact lenses.
Blepharitis - what is it?
Any inflammation of the outer edge of the eyelid is commonly called blepharitis.
In the eyelid, anterior and posterior ribs and intermarginal (intercostal) space are distinguished. Eyelashes grow on the front rib, in the bulbs of which the ducts of the sebaceous glands open. This feature of the outer edge is sensitive to both external stimuli and endogenous factors. It is no secret that any blockage of the sebaceous gland leads to its inflammation due to stagnation of sebaceous secretion. It’s enough to remember how skin that has similar problems behaves - dozens of teenagers suffer from so-called blackheads. Modified sweat glands are located between the eyelashes. They also produce a special secretion that protects the skin of the eyelids from drying out and peeling.
The ducts of the cartilage glands, the meibomian ones, open into the intermarginal space . They are located on the inner surface of the eyelid. Their fatty secretion lubricates the edges of the eyelids, promoting their closure and tight fit.
Blepharitis is an inflammatory process that does not have a specific infectious agent. It is believed that such inflammation is a consequence of metabolic disorders in general, primarily fat and carbohydrate. Poor nutrition, violation of the work and rest schedule, the desire to change the climate and relax in warm countries, hormonal imbalances, and beauty salon procedures can cause blepharitis.
It has been proven that in 5% of cases, the lack of correction of refractive errors contributes to changes in the properties of fatty secretions and, subsequently, the appearance of blepharitis. Often the disease is combined with dental caries, chronic tonsillitis, nasal polyps, adenoids and other pathological processes in the paranasal sinuses.
Neuroendocrine changes during puberty often cause dysfunction of the cartilage glands and sebaceous glands located in the edges of the eyelids. Such dysfunction can manifest itself as either hypersecretion or insufficient secretion. With frequent blinking, the secretion mixed with tears forms a foamy discharge. Blondes with thin and delicate skin, who have reduced resistance to external physical and radiation irritants, are predisposed to blepharitis.
Factors contributing to the occurrence and development of blepharitis are unfavorable external conditions: dust and smoke in industrial premises, prolonged exposure to chemical compounds in the air (for example, particles of car exhaust gases), allergic irritants (pollen, poplar fluff).
How to treat eye blepharitis?
vitamins. It is very important to maintain good hygiene. You can accidentally introduce germs into the affected areas of the eyelids and eyes. Because of this, the disease will be even more difficult and longer.
Medicines are selected according to the type of blepharitis. For one form or another of inflammation, antihistamines, antibacterial, antiseptic drugs, glucocorticosteroids, and sulfonamides are prescribed. Medicines are prescribed in drops, ointments and tablets. For almost any type of blepharitis, Furacilin is prescribed, from which a solution for washing the eyelids is made. A universal remedy for this disease is brilliant green.
dexamethasone-based drops, for example, Maxidex.
Treatment of ulcerative blepharitis will require gentamicin-based antibiotics. If you are intolerant to such drugs, antibacterial ointments are used. One of the complications of ulcerative blepharitis is ulceration of the cornea. For tissue healing, drops “Vitasik”, “Korneregel”, etc. are used. They accelerate regeneration.
For demodectic blepharitis, Dexa-Gentamicin ointment is prescribed, which helps destroy mites. The drug is applied to the eyelids in a thick layer. Allergic inflammation of the eyelids is treated with anti-allergic drugs: Alomide or Lekrolin. When barley occurs, antibacterial drops are instilled into the eyes: “Levomycetin”, “Floxal”. Tetracycline ointment is also used.
Surgical intervention
In severe advanced forms of the disease, surgery may be required. For example, a patient needs plastic surgery if he has inversions or eversion of the eyelids to remove chalazions. Surgery is also necessary to remove scar tissue and destroy tear ducts.
It is important to understand that treatment is quite difficult and requires time. It should continue until the symptoms of blepharitis completely disappear. In the future, it is recommended to use the recommended medications for 3-4 weeks in order to avoid relapses.
Doctors' recommendations
General recommendations from doctors:
- To achieve the best effect, use medications only on the recommendation of an ophthalmologist. Buying and using the drug on your own can end badly.
- Before using any ointment, read the instructions, even if it was prescribed by a doctor. Pay special attention to the “Contraindications” and “Side Effects” paragraphs.
- Store medications at appropriate temperatures.
- If you can’t put the medicine on your own, your hands are shaking, ask your relatives for help. If you accidentally touch the ointment to your eyes, you can cause an infection.
- When using many ointments, contact lenses are removed. They prevent the penetration of drug components.
- If the medicine is used for children, administer in a supine position. First, the ointment is applied to one eye and covered with a band-aid. After 15 minutes in the second. This will help if the child is too active and cannot sit in one place.
To obtain effectiveness from the treatment, it is necessary to use ointments correctly. They are applied to the skin using a cotton swab or hands, which should be washed first. If the inflammatory process is manifested by redness of the mucous membrane, gluing of the eyelids, medications are placed in the conjunctival cavity.
Adding medicine:
- Use 10 minutes after instillation of drops.
- If the ointment is stored in the refrigerator, warm it in your hands before use. It will be easier to squeeze out of the tube and will not irritate the mucous membrane.
- Wash your hands thoroughly before using the medicine.
- Position yourself in front of a mirror, this will allow you to control your movements.
- Unscrew the cap and take the tube with your thumb and forefinger.
- Tilt your head back slightly.
- Using the index finger of your second hand, pull the lower eyelid down so that a space is formed between the eye and the eyelid, called the conjunctival sac or “pocket.”
- Look up, squeeze 1 cm of medicine into the resulting cavity.
- Release the lower eyelid.
- Carefully lower the upper eyelid, lift it by the eyelashes and apply it over the protruding ointment from the lower eyelid.
- Don't blink. Lie down with your eyelids closed for 10–15 minutes. Then blink a little.
Prevention of blepharitis
Regardless of the cause of blepharitis, you must adhere to some rules:
- try to follow a plant-milk diet (sweet, fried, spicy, salty foods promote the production of gastric juice and increase the secretion of eyelid secretions);
- beware of colds (ARVI increases the manifestations of blepharitis);
- Carry out regular hygiene procedures (always rinse your eyelids only with warm water - cold water leads to venous stagnation);
- do not forget to use drops and ointments prescribed by your ophthalmologist;
- follow a sleep and rest schedule, during the day try to watch TV for no more than 2 hours in a row;
- In spring, try to protect your eyes with sunglasses.
The MedicCity clinic receives daily consultations from highly qualified ophthalmologists who use the most modern equipment to diagnose and treat eye diseases. Regular examination by an ophthalmologist will allow you to avoid serious eye diseases and maintain good vision!
Chronic form of blepharitis
The result of the fact that people susceptible to ordinary infection of the eyelid margins neglect preventive measures is the occurrence of chronic blepharitis, which develops into a serious pathology that requires complex treatment.
As a result, the symptoms are eliminated, and the disease continues to occur in a latent form. Most often, chronic damage to the organs of vision affects both eyes at once, in particular in the form of posterior or anterior blepharitis.
The chronic form occurs in the following cases:
- vitamin deficiency, tendency to allergies;
- anemia;
- diseases of the digestive system;
- poor eyesight.
Symptoms of chronic blepharitis include all the main signs of the disease. The only difference is that this form appears at some interval.
Causes and grounds for blepharitis
If an eye doctor or therapist diagnoses blepharitis, before prescribing treatment, he will definitely determine the cause of its appearance and development. Among the most basic reasons that cause the development of pathology are:
- Fungus;
- The appearance of subcutaneous mites;
- Penetration of various microbes and bacteria;
- Infectious pathologies;
- Allergy;
- Lack of beneficial vitamins;
- Severe forms of tuberculosis;
- Diseases in the digestive system;
- Inflammation in the nasopharynx and mouth;
- Development of anemia and diabetes;
- Adverse habits;
- Serious violation of proper care, adverse environmental influences;
- Hypothermia and penetration of foreign objects;
- Stress and load on the nervous and mental system;
- One-time overvoltage;
- Worm infestations;
- Different types of pathologies affecting the eyes.
If blepharitis is diagnosed in children, then the cause in most cases is the presence of Staphylococcus aureus.
General strengthening procedures
To prevent the disease from appearing again, it is very important to adhere to the following rules:
- Perform sanitation of foci of chronic infection;
- Use medications that normalize immunity;
- Take vitamins;
- Treat concomitant ocular pathologies.
In addition, even during long-term remission it is very important:
- Take courses of anti-relapse therapy using medications recommended by your doctor;
- Observe hygiene rules;
- Be observed with some frequency by an ophthalmologist, etc.
- Remember that ulcerative blepharitis can cause serious problems in the functioning of the visual system and significantly worsen the general condition of the body. That is why the disease should not be allowed to become severe.
How to alleviate the patient's condition
Recommendations to alleviate the patient’s condition with blepharitis:
- Compresses improve blood circulation, relieve inflammation, soften scales. The fabric is dipped in warm water or herbal decoction.
- Refusal of makeup and contact lenses. Makeup will irritate the inflamed tissue again and again. Contact lenses should be replaced with glasses. After recovery, it is necessary to change old lenses, as traces of bacteria may remain on them.
- Getting rid of dandruff. It is little known that dandruff can occur not only on the scalp, but also in the eyebrows and eyelashes. This problem can be eliminated with special shampoos or a folk remedy - honey and apple cider vinegar.
- Vitamins and microelements. During an eyelid infection, it is necessary to consume vital nutrients through food. Omega-3 is found in oily fish, liver, avocado and olive oil. Vitamins of groups A, B, C can be found in green vegetables, cabbage, pineapple, pumpkin, melon and sweet pepper. Bone broth is a nutritious meal for people suffering from blepharitis.
How does blepharitis start?
There are micro-openings on the eyelids - excretory ducts, which contain the meibomian glands and glands of the eyelashes (Zeiss and Moll). Microbes can get into these ducts: viruses, bacteria, fungi. When favorable conditions arise for them, they begin to reproduce. This happens at a time when the human body is weakened by a cold or other illness. Inflammation can begin in the meibomian glands, in the corners of the eyes, in the follicles of the eyelashes. Depending on what factor caused blepharitis and where it is localized, one or another type of disease is diagnosed. Various forms of inflammation of the eyelid margins are treated using different methods. Let's look at the causes of blepharitis.
Main symptoms of pathology
Due to the fact that blepharitis is characterized by the development of several types, the general symptoms of the pathology can be divided into main and characteristic of a particular type of disease. Among the main signs of pathology are:
- Redness of the eyelids;
- Severe swelling around the edges of the eyes;
- Constant sensation of a foreign object in the eye;
- Painful sensations;
- Sensitivity to light;
- Increased dryness and tearing of the eye;
- Unpleasant burning of the skin of the eyelids;
- Slow growth or loss of eyelashes;
- Formation of crusts on the eye;
- Eye fatigue and decreased quality of vision;
- Pronounced hyperemia of the eyelids.
Along with the main signs, other symptoms can be noted that are characteristic of each individual type of pathology.
Here are some basic examples of the development of each specific form of pathology:
- Allergic – constant, very unpleasant itching, debilitating pain, accumulation of mucus. Such symptoms develop seasonally or from close contact with allergens, individual for each patient.
- Demodectic mange - severe morning itching, irritating pain, formation of sticky mucus, which after some time dries out and turns into crusts. The skin becomes very thick and itchy.
- Ulcerative – the presence of purulent inflammations, small ulcers. In places of severe damage, loss of eyelashes is observed, and sometimes inversion of the eyelids is observed.
- Meibomian, where there is a complete blockage of the glands of the same name. Here unpleasant symptoms such as burning, itching of the skin, severe redness and a debilitating stinging sensation are noted.
Modern doctors note several common symptoms that are characteristic of all forms of blepharitis and inflammation.
These are such unpleasant symptoms as sensitivity to the sun and wind, eye fatigue, complete destruction of the hairline, heaviness of the eyelids with a relatively low load.
Blepharitis - symptoms and treatment
The clinical picture of blepharitis is determined by its form and, of course, the presence of a particular pathogen.
Considering that the first complaint of a person suffering from blepharitis will most likely be itching, this symptom should be paid attention to if it becomes obsessive and protracted. Redness of the eyelids, especially combined with their thickening, will also indicate an inflammatory process in the edge of the eyelid.
The female half of the population notes that they cannot use cosmetics because itching and hyperemia intensify, and increased lacrimation appears. Almost everyone who subsequently develops blepharitis experiences discomfort from sun exposure.
If blepharitis begins in the cold season, then lacrimation bothers the person quite strongly due to the disruption of all mechanisms of the act of blinking, and as a result, the loss of the protective function of the eyelids. With reduced secretion of the sebaceous glands, dry eyes appear and difficulty opening the eyes in the morning.
All the symptoms of blepharitis may not manifest themselves in full force for a long time, so a person is in no hurry to consult an ophthalmologist. Dealing with blepharitis, coping with its manifestations, and identifying the pathogen is available only in medical institutions.
The initial manifestations of scaly blepharitis can only be seen by a doctor using biomicroscopy. Laboratory diagnostics to determine the presence of demodex or other pathogens are available only to a doctor. A specialist should prescribe appropriate treatment based on the type of blepharitis.
Self-medication methods that people begin to use when initial symptoms appear make it difficult to diagnose and identify the pathogen, and lengthen the treatment period.
Treatment of blepharitis presents certain difficulties, because blepharitis is a polyetiological disease. A direct connection with the general condition of the human body requires treatment and examination by other specialists. Despite the fact that in clinical practice we deal with simple and demodectic blepharitis, no one is immune from the transition to a more severe form - ulcerative. Currently, the pharmaceutical market offers a variety of drugs for the treatment of this disease.
Only a specialist can figure out which drug will be used in a particular case.
The main direction in the treatment of blepharitis remains the release of the ducts from the inflamed secretion of the glands. To do this, the doctor performs several sessions of eyelid massage . The essence of the method is that the doctor uses a glass rod to compress the edges of the eyelids on both sides, thereby freeing the ducts. At the same time, a cloudy, thick, yellowish secretion is released from the glands. After each procedure, it is necessary to treat the edge of the eyelid with a 70% aseptic solution.
Against the background of such treatment, eye drops with a wide spectrum of action are used. In medical practice, Sofradex, Floxal, Signicef are used. After several massage sessions, the use of special ointments and gels is justified.
Ointments and gels should be medicinal preparations, not cosmetics!
Recently, long-term use of Blefarogel-2, which, in addition to antibacterial properties, has an anti-demodectic effect, has had a good effect. Treatment of blepharitis should be accompanied by the use of vitamins, especially group B, the use of immunomodulators, as well as treatment of diseases that contribute to the long and protracted course of blepharitis (for example, diabetes).
Some ophthalmologists recommend constant treatment of the edges of the eyelids with various alcohol tinctures - calendula, chamomile, but such treatment contributes to drying of the surface of the eye. Therefore, the use of such a therapeutic measure requires a careful approach on the part of the doctor. Treatment of blepharitis is a long and painstaking process, and requires patience from both the doctor and the patient.
List of ointments
Maxitrol
Combined product. At the same time, it eliminates the inflammatory process and fights infection.
The drug penetrates the cell membrane, causing their death. Designed for use in the eyes. May cause increased intraocular pressure, irritation and burning.
Synthomycin liniment
100 g of medicine contains 5 g of chloramphenicol. Synthomycin liniment accelerates the healing process when wounds form. Used for local and external use.
Hydrocortisone
Designed for outdoor use. It is not recommended to put the ointment into the conjunctival sac. It is a synthetic glucocorticosteroid.
Tetracycline 1%
The drug is contraindicated in case of hypersensitivity to the active substance. Allergic reactions to the components of the medicine are possible. Tetracycline ointment is a broad-spectrum antibacterial agent. Used for infections that cause blepharitis.
Ofloxacin
The active substance is ofloxacin. The medicine is antimicrobial, with high activity against most microorganisms.
Contraindicated during pregnancy, placed behind the lower eyelid.
Dancil
Used for the treatment and prevention of blepharitis. Available in the form of ointment and drops. You cannot use both types of medication at the same time; an overdose of the active ingredient is possible.
Prenatsid
It is a glucocorticoid and steroid hormonal drug. Prenacid has a pronounced anti-inflammatory effect.
After use, it burns slightly and causes a tingling sensation in the eye.
Fucidin
Treats skin infections caused by bacteria sensitive to fusidic acid. Used externally. Recommended for use as lotions.
Dexamethasone
The medicine is placed behind the lower eyelid. It has anti-inflammatory, anti-edematous and anti-allergic properties.
Cannot be used for a long time as it causes adverse reactions. Dexamethasone penetrates into the systemic circulation.
Demazol
Used to treat bacterial or parasitic blepharitis. The medicine relieves inflammation, swelling, reduces itching, and eliminates the feeling of sand in the eyes.
Apply Demazol with a cotton swab to the edges of the upper and lower eyelids.
Demalan
Refers to antiparasitic drugs. Effective in the treatment of demodicosis. Demalan is contraindicated if you are allergic to active substances. Side effects are not a reason to discontinue the drug; burning and itching pass quickly.
Mechanism of disease development
Blepharitis is usually caused by an overgrowth of bacteria that lives along the edges of the eyelids and at the base of the eyelashes. Over time, these bacteria accumulate and create a structure called a biofilm. This film is similar to plaque on the teeth; it is a constant source of bacterial toxins, and in addition, it is a nutrient substrate for mites that parasitize the sebaceous glands of the eyelashes - Demodex folliculorum. Suppression of local immunity promotes the proliferation of mites, which aggravate irritation and inflammation of the eyelids.
Bacterial exotoxins cause inflammation of the meibomian glands. They usually produce a special composition that lubricates the edge of the eyelid, thereby keeping the tear fluid within the tear lake. When the function of these glands is impaired, the eye gradually loses the necessary moisture and dryness of the cornea develops.
Given that tear fluid contains a special antibacterial component, the loss of this protective environment promotes the growth of bacteria in the biofilm. Thus, the pathological circle is closed, and blepharitis becomes chronic. When the meibomian glands become blocked, a chalazion or gordelum (hordeum) may subsequently develop.
Staphylococcal/ulcerative blepharitis: diagnosis
Having identified the symptoms in order to prescribe treatment, the ophthalmologist needs to conduct a thorough diagnosis of eye pathology. After a detailed story from the patient, the doctor proceeds to a visual examination of the eyelids and eyelashes using a slit lamp.
Often there is a need to order a laboratory study of the cellular and microbial composition obtained by scraping from the conjunctiva. This allows the ophthalmologist to detect the presence of microscopic demodex mites in the eyelash bulbs.
Also, diagnosis of ulcerative/staphylococcal blepharitis may include:
- Measuring blood sugar levels (allows you to detect the presence of diabetes mellitus, which can cause the disease);
- Fecal analysis to detect the presence of parasites in the body;
- Biomicroscopy - a complete examination of the state of the visual system (eyeball and eyelids);
- Testing visual acuity, accommodation and refraction;
- Consultation and diagnosis of other doctors - dermatologist, gastroenterologist, endocrinologist, ENT specialist (blepharitis often occurs against the background of general diseases of the body).