Staying in bed for a long time slows down the body's metabolism, disrupts normal blood circulation and causes the formation of bedsores. The disease is accompanied by tissue necrosis and can be fatal. The initial stage of bedsores is a slight hyperemia and thickening of the skin. If preventive measures are not taken in time, the disease will begin to progress, causing excruciating pain to the person.
What is a bedsore?
Bedsores (decubitus) are necrosis (death) of soft tissue, followed by ulcers in places where the skin and/or underlying tissue is damaged.
They occur as a result of lying or sitting in one position for a long time, due to pressure on an area of the body. It especially occurs in sick people who need care and are bedridden. It can only be prevented by treatment and prevention.
On average, a person unconsciously changes his position several times during sleep, so bedsores do not occur even during prolonged bed rest. However, people who are bedridden cannot move or turn around on their own. Without proper care, they are at risk of bedsores.
Which parts of the body are especially at risk?
Areas of the body at increased risk for pressure ulcers: Ulcers can form in areas, especially where the skin is in close contact with bone.
Erosions (i.e., superficial defects of the epithelium) can occur in all areas of the body where the skin passes only over the bone.
These areas are not protected by muscle or fat tissue. These include:
- elbow;
- forehead, cheekbones;
- sacrum bone (coccyx);
- bulges at the top of the femur;
- heel, ankle.
In the supine , wounds most often occur in the sacrum, heels and elbows. In the lateral position, ulcers appear on the hills of the thighs and ankles.
If the patient lies on his stomach, tissue necrosis forms on the forehead and cheekbones. Also, the areas of skin between the fingers and toes are at risk.
Causes of bedsores
As noted above, bedsores develop as a result of impaired blood circulation and nervous trophism with prolonged pressure on soft tissues. It is important to know that with qualified patient care, bedsores can be avoided in ⅔ of cases.
Here are the pathological factors contributing to the formation of bedsores:
- forced long-term stay in a horizontal position: condition after a stroke, heart attack, severe surgery, fracture; being on mechanical ventilation, late stages of dementia, Alzheimer's disease, multiple sclerosis, severe encephalopathy, etc.;
- overweight; dystrophy, cachexia;
- urinary and fecal incontinence;
- dry skin;
- anemia;
- diseases accompanied by circulatory disorders: diabetes mellitus, atherosclerosis, obliterating endarteritis, vasculitis, thrombosis, etc.;
- prolonged fever;
- unbalanced protein-poor diet;
- weakened body.
What does a bedsore look like in a person (symptoms)?
The first signs of a developing pressure ulcer: redness , which persists even in the absence of pressure. At the initial stage, patients often do not notice erosion.
Without proper treatment, the bedsore continues to spread. Subsequent stages of superficial skin damage occur with deep bleeding wounds with inflammation of muscle and bone tissue.
Other possible symptoms, e.g.
- itching;
- strong pain;
- and burning in the affected area.
However, people suffering from nerve damage due to other diseases may experience few or no symptoms even in advanced stages.
In addition, if pathogenic microorganisms (viruses, bacteria, etc.) enter the ulcer, an unpleasant odor occurs.
Folk remedies
Treatment of initial bedsores can be carried out with folk remedies. There are many recipes for improving blood supply to tissues and increasing the body's defenses. At the initial stage of the disease, you can use red rose oil. It has a bactericidal and healing effect. The reddened surface is lubricated with an oil swab.
Recipes for bedsores at the initial stage:
- Cut an aloe leaf in half and apply it to the sore spot. You can use squeezed juice. The plant has a wound-healing effect and promotes tissue regeneration.
- Grind the calendula flowers, mix a tablespoon of raw material with Vaseline. Lubricate the affected area 2 times a day.
- Make a vodka infusion. Combine calendula and vodka in a 1:2 ratio. Leave for 2 weeks and wipe the problem area. You can install gadgets. Alcohol warms the skin and helps increase blood flow.
- Steam the millet, put warm cereal in gauze and apply to the bedsore. The procedure improves blood circulation.
- Mix honey and mashed potatoes in equal quantities, apply the lotion to the reddened area.
In addition to healing ointments and lotions, it is necessary to provide the patient with proper nutrition. Protein is required to build muscle mass. They are found in eggs, meat, dairy products, and nuts. Vitamins B and C are needed for tissue regeneration. It is necessary to include cereals, citrus fruits, and sweet peppers in the menu.
The initial stage of bedsores in bedridden patients responds well to treatment. It must be remembered that the development of the pathological process begins unnoticed and can quickly turn into necrosis, causing additional suffering to the patient. Treatment of an advanced form is long and expensive; its absence can cause gangrene and sepsis. Competent care, massages and special orthopedic devices help prevent bedsores and improve the patient’s condition.
Classification of bedsores
Doctors divide bedsores into grades I-IV:
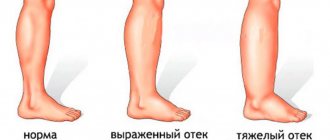
- Degree I: hyperemia (redness), swelling of damaged skin areas. If you remove pressure from the affected area, the irritation does not go away. The skin area may be warmer than usual.
- Grade II: Formation of a painful, moist ulcer. Detachment of the upper layers of skin begins, and blisters form.
- Grade III: deep wound. There is abundant fluid discharge from the injury and necrosis.
- Grade IV: The final stage of a pressure ulcer is a deep tissue injury where muscles, bones and tendons are visible (see photo above). As a result, deep erosions (ulcers) form in the bones.
Stages of development of bedsores:
- the first stage is local blanching of the skin, followed by cyanosis, swelling of the tissues, and the appearance of blisters leading to detachment of the epidermis;
- the second stage - with endogenous bedsores, the development of wet necrosis, rapid proliferation of pyogenic and putrefactive flora, the release of foul-smelling fluid from under necrotic tissues, purulent-resorptive fever, intoxication, a rise in body temperature, depression of consciousness, delirium, tachycardia, enlarged liver, etc. occur. ;
- the third stage is the healing stage, with favorable development of the process, the wound is cleansed of necrotic tissue, scarring, and epithelization.
Causes and risk factors
Bedsores occur as a result of prolonged mechanical impact and impaired blood microcirculation, especially after prolonged lying or sitting. Over time, small blood vessels become damaged:
- constant pressure on the skin compresses small blood vessels;
- as a result, the corresponding area is less well supplied with oxygen;
- eventually, the tissue dies, the skin thins and an open wound (ulcer) forms.
In addition to pressure, friction also contributes to bedsores; layers of tissue can rub against the surface, causing damage to small blood vessels.
Risk factors
Various factors contribute to the development of pressure ulcers. These include:
- decreased sensitivity to pain: in some diseases, the patient does not even notice that a part of the body is under pressure. May occur as a result of paralysis, diabetes mellitus, circulatory disorders, due to atherosclerosis, anemia, Parkinson's and Alzheimer's disease, stroke;
- diseases , skin irritations;
- Wetness: For people who spend hours in diapers, wet skin softens over time. This makes them more prone to damage. Not only feces and urine, but also heavy sweating irritate the skin;
- poor nutrition: in cases of malnutrition, the skin is often very thin and has a poor blood supply;
- Obesity: In people who are overweight, damage occurs more quickly because the bone and skin are subjected to greater pressure in bed. In addition, overweight people often sweat excessively, which also contributes to the development of bedsores;
- older people: Older people are more likely to get sick than younger people because they are at greater risk of poor circulation, decreased cardiac output and nervous system disorders. In addition, with age, the skin loses its resistance and elasticity, which can also contribute to the development of bedsores. Urinary incontinence, which is not uncommon in old age, further contributes to bedsores.
Why do bedsores form in a bedridden patient?
This disease appears during prolonged contact with a hard surface, when pressure is constantly applied to an area of the body. As a result, the tissues are compressed by the bones, the vessels are pinched, and therefore blood circulation is disrupted. Oxygen and nutrients stop flowing into this area of the skin, which causes the tissue to begin to die.
In bedridden patients, bedsores also appear on the body due to friction and sliding. Damage to the skin occurs when a person tries to change position or is pulled from place to place to change bedding or change clothes. Sliding occurs if a person is in a semi-sitting position without support.
The likelihood of developing this disease depends on the severity of the patient's condition and the quality of care.
Since bedsores are caused by compression of soft tissues by bone, the following groups of patients are at risk:
- people with limited mobility, bedridden patients (who are in a coma, paralyzed, after surgery);
- overweight patients, especially if they sweat a lot;
- patients with diabetes mellitus and other diseases that cause circulatory problems;
- severely malnourished people who eat little and drink little fluid;
- patients with cardiac and neurological diseases, brain or spinal cord injuries;
- patients who suffer from urinary or fecal incontinence;
- patients with allergies to skin care products;
- aged people.
Bedsores occur with diaper rash, so bedridden patients need careful care. A predisposing factor is dirty bed linen, folds in the bed, the presence of crumbs, grains of sand or other small objects in the bed where the person is lying.
Necrotic areas may appear after a fracture if the bandage is applied too tightly. There is a high likelihood of bedsores in people with too dry or moist skin, vitamin C deficiency and impaired consciousness (they do not adhere to doctor's recommendations).
Prevention of bedsores
Of course, bedsores can be treated, but it is better to prevent their occurrence. For necrosis, there is a set of preventive measures that, if carried out correctly and in a timely manner, will help avoid the occurrence of ulcers.
Measures to prevent the formation of necrosis in a seriously ill patient are quite simple. It is necessary to change position every 2-3 hours to redistribute the pressure to different parts of the body. An anti-decubitus mattress can perform the same function. In addition, it is imperative to regularly change underwear and bed linen, and monitor the patient’s hygiene.
An additional means of prevention is the use of anti-bedsore drugs: powders, ointments, gels, solutions, patches, aerosols.
Common means used to prevent bedsores are camphor, ammonia and talc. They dry the skin, protecting against diaper rash, which turns into erosion. Protection against diaper rash is the main thing in preventing bedsores. All these measures are mandatory when caring for a bedridden patient.
Prevention should be carried out from the first day of the disease and when the first signs of soft tissue death appear.
Means for uniform distribution of pressure on the body
If regularly changing the patient's position is not enough to prevent bedsores, additional means can be used to help evenly distribute pressure on the body. However, they do not replace regular changes of position.
Prevention
Expensive, painful and lengthy therapy may not be necessary if due attention is paid to preventing the formation of purulent wounds. It includes a mandatory change in the patient’s body position at least once every two hours.
The areas of greatest pressure should be lightly massaged, however, it should be remembered that intense massaging movements of the reddened skin should not be used.
The comfort and safety of a bedridden patient will be ensured by an anti-bedsore mattress and an adjustable bed, bedding made from natural materials with a smooth texture. It doesn't hurt to use products that treat diaper rash.
Remember, before using any products or medications, you should consult a specialist.
Treatment of bedsores
If prevention does not help and the patient still develops bedsores, they must be quickly treated to prevent further spread of the wound.
Particularly important: the affected area of the body should be exposed to as little as possible.
Depending on the severity, the ulcer should be treated with special ointments, followed by applying a bandage to the wound.
Remedies for bedsores: effective ointments and gels
Popular medicinal ointments and gels are the following drugs:
- Algofin is an ointment whose main components are chlorophyll and fatty acids. These are natural substances that have a strong anti-inflammatory effect. The drug triggers accelerated regeneration of skin cells. Price 100 rub.
- Zinc ointment is a preparation consisting of petroleum jelly and zinc oxide. Apply to the skin at least 6 times a day. Creates a thin protective film impenetrable to pathogenic microorganisms. It has an antibacterial effect and dries the wound. 20-40 rub.
- Stellanine is a strong anti-inflammatory drug. It is effective in treating the disease; when used, the damaged area of the skin is regenerated. Apply to the skin 3 times a day.
- Fukortsin is a bright pink solution with bactericidal properties. Destroys pathogenic flora.
- Multiferm - used for the treatment of bedsores of the first and second stages. Price 150-160 rub.
General information about the disease
A bedsore is a local pathomorphological change in tissue up to necrosis (death), which develops as a result of constant long-term compression of an area of the body, with subsequent disruption of blood circulation and nervous regulation.
Epidemiology
The incidence of pressure ulcers in inpatients around the world ranges from 3% to 30%, depending on the level of development of state medical care and the specifics of a particular medical department. institutions. The largest number of these complications occurs in neurological (“post-stroke”), oncology, burn, geriatric departments, hospices, intensive care units. Even with proper preventive care, the pathological incidence of bedsores here reaches from 20% to 60%.
According to American studies, from 5 to 40 thousand dollars are spent on one patient with bedsores per year. In England, the national cost of all patients with pressure ulcers is estimated at £200 million.
From the above we can conclude that bedsores are not only a medical problem, but also a socio-economic one.
Etiology
Bedsores can develop only in patients with low physical activity (or lack thereof - “bedridden patient”).
If the underlying disease is accompanied by hemodynamic and metabolic disorders (acute cerebral circulatory failure, myocardial infarction, cardiac arrhythmias, diabetes mellitus, etc.), the risk of developing bedsores increases several times. Diseases and conditions in which bedsores develop are:
- Cardiovascular pathology: myocardial infarction, cerebral infarction, severe heart rhythm disturbances (3rd degree atrioventricular block), thrombosis of the great vessels.
- Paralysis (hemiplegia, tetraplegia, for example, after spinal cord or brain injuries).
- Postoperative period - bedsores develop mainly in seriously ill patients whose postoperative period is long (after peritonitis, pancreatic necrosis, cardiac surgery, etc.)
- Comatose state (coma) - since the duration of a coma is difficult to predict, such patients most often require careful care.
- Special cases: necrosis of the gums and jaw due to improper use of dentures, forced movement in a wheelchair (bedsores on the buttocks, sacrum), incorrectly fixed plaster cast.
Factors that contribute to the formation of bedsores:
- old age - the metabolic and regenerative processes of the body are significantly slowed down;
- poor nutrition and drinking regime;
- severe metabolic disorders (diabetes mellitus, liver cirrhosis, hypothyroidism, Itsenko-Cushing's disease);
- involuntary acts of defecation and urination.
Pathogenesis
Constant compression of soft tissues (2 - 3 hours without movement of the patient) leads to disruption of microcirculation in the superficial layers (skin, subcutaneous fatty tissue); in the absence of preventive measures, deeper layers (muscles, large vessels and nerves) are also subject to compression, blood flow to local area of the body decreases, nervous regulation stops.
Nutrition and exchange of microelements in cells decreases to a critical level, local hypoxia and acidosis develop, and gradual necrosis begins (from superficial to deep layers).
First, the epidermis and dermis die, forming dense blisters with serous-hemorrhagic fluid, then subcutaneous fatty tissue, fascia, muscles, tendons and, finally, bone.
Bedsores bring not only local painful irritation, but are also a source of generalized intoxication by the decay products of dead cells - body temperature, heart rate, respiratory movements increase, and pronounced signs of inflammation are observed in blood and urine tests.
Bedsores quickly become infected, purulent foci form, and the process can involve bone tissue with the formation of osteomyelitis. Without surgical excision of necrotic tissue and antibiotic therapy, there is an almost 100% risk of developing systemic infection (sepsis).
Classification
Stages of bedsores:
- Stage 1 - local focus of hyperemia with a bluish tint, swelling, decreased sensitivity, numbness, coldness. When pressing with a finger, the redness does not disappear;
- Stage 2 - the formation of a bubble on the skin filled with liquid, the formation of a focus of inflammation with a central depression (future ulcer);
- Stage 3 - a formed ulcer from which fluid is released (hemorrhagic, purulent, serous);
- Stage 4 - deep necrosis of the skin in the form of a wide wound filled with dead tissue and pus. At the bottom of the wound you can find tendons, articular surfaces, and areas of bone.
Pathogenetic classification of Professor M.D. Dibrov
Stage of circulatory disorders - acute disruption of arterial inflow and venous outflow leads to hypoxia and tissue edema. The skin looks hyperemic, and after a while the red color gives way to bluish.
The stage of tissue necrosis and suppuration is descending tissue necrosis from the epidermis to the muscles, fascia and bones. Attachment of a bacterial infection. A deep ulcerative defect is detected on the skin. This stage is divided into 2 types depending on the presence of secondary flora and the prevalence of the process:
- Type 1 - coagulative necrosis. The ulcer is dry, without visible purulent discharge, and has clear boundaries;
- Type 2 - liquefaction necrosis. A purulent wound with a large amount of fluid discharge, uneven edges, tendency to spread.
The regeneration stage is the restoration of tissue healing processes, the formation of a dense scar.
According to the development mechanism:
1. Exogenous - prolonged pressure, humidity, friction:
- internal - develop in places where plastic drainages, urinary catheters, and colostomy bags are installed;
- external - formed in places of pressure of a hard surface on the skin above bone protrusions, with constant friction against bedding, humidity (involuntary urination).
2 . Endogenous - formed due to existing violations of local tissue trophism (hematoma after a blow with a blunt object), neurotrophic pathologies (spinal cord or brain injury), decompensation of endocrine diseases.
3 . Mixed - combine exogenous and endogenous symptoms (for example, with an advanced malignant tumor).
To size:
- Small bedsore - up to 5 cm in diameter.
- The average bedsore is from 5 cm to 10 cm in diameter.
- Large bedsore - from 10 cm to 15 cm in diameter.
- Giant bedsore - more than 15 cm in diameter.
- A bedsore with a fistula is formed when the deep layers of tissue become necrotic first. A cavity with pus is formed in the intermuscular spaces, which can communicate with the bone cavity through pathological passages and cause osteomyelitis, or open on the skin (more favorable prognosis).
The most common locations of pressure ulcers are the skin over the ankles, the lateral surfaces of the knee joints, the iliac crests, the sacrum, the coccyx, the buttocks, the lateral surfaces of the ribs, the shoulder blades, the sternum, the occipital bone, and the frontal bone.
Types of bedsores: dry and purulent
Doctors use several classifications of such injuries: according to the degree, cause of occurrence, size, types of complications, but the division into dry or wet necrosis deserves special mention:
- Dry bedsores (mummified) - the tissues dry out, like a mummy, the affected area has clear boundaries, there is no discharge, infections occur extremely rarely. The patient feels more or less normal, sometimes complains of pain,
- Purulent bedsores (bedsore gangrene) are much more dangerous: the wound is swollen, infected, with purulent discharge. The patient's health deteriorates sharply: fever, delirium and/or loss of consciousness appear. The patient suffers from vomiting, palpitations, etc. If treatment is not started, blood poisoning (sepsis) will begin, which can be fatal.
Hygiene measures
Poor care of the patient’s skin is one of the powerful factors in the development of pressure ulcers. You should definitely devote a lot of time and effort to hygiene, and perform all stages of care (cleansing, protection, moisturizing).
Under no circumstances should you wash the patient with hard washcloths or use rough towels. Detergents should be gentle, not strong-smelling and without dyes. Contact of the patient's skin with water should be minimized.
Also, keep your bed linen clean and change it promptly. There should be no crumbs or other irritating objects on the sheets.
Torrance classification
In clinical practice, it is customary to classify the degree of pressure ulcers according to Torrance’s 5-step breakdown:
Stage 1. Reactive hyperemia and redness is reversible. When pressing on the affected area, redness occurs, which immediately disappears. This suggests that the microcirculation of blood vessels occurs without changes. Bedsores initial stage (see photos).
Stage 2. After pressure, erythema (redness of the skin) persists. This means that the area of skin has microvascular injury, inflammation, or tissue swelling. Obvious signs of damage (blisters, etc.) form on the skin. It is at this stage that bedsores (see photo) begin to bring the first pain to the patient.
Stage 3. Complete damage to the skin, reaching deep to the border of the main tissue. The edges of the wounds have clear contour boundaries. Swelling and erythema are observed. The bottom of the wound is filled with granulation tissue, the red or yellow color of disintegrating tissue.
Stage 4. What do bedsores look like at this level of disease? Subcutaneous tissue is damaged. Fat necrosis is caused by inflammation and thrombosis of small vessels. The bedsore zone, as a rule, has well-demarcated outlines. The bottom of the wound may be covered with black necrosis (tissue death).
Stage 5. Extended necrosis, spreading to the fascia (dense membrane covering the muscles) and muscle tissue. Joints and bones are damaged, forming deep black fistulas.
Different stages of bedsores have specific treatment methods. At the initial stage (levels 1, 2 and 3), a conservative treatment method based on antiseptic dressings is sufficient. At levels 4 and 5, the situation can be corrected only through surgical manipulation. Proper care of bedsores will help avoid drastic measures. It is easier to prevent a disease than to treat it, especially since this is a very complex and time-consuming process.
Why are bedsores dangerous?
Bedsores primarily worsen a person’s well-being and can increase the duration of treatment for the underlying disease. Seriously ill people, in addition to the symptoms of the leading disease, experience pain from the resulting ulcers, which causes discomfort and further limits the ability to move, which can lead to the formation of new bedsores.
The greatest danger is the fact that with the appearance of wounds, an infection can enter the body. In addition, various microorganisms that can cause all sorts of diseases easily penetrate into a weakened body through open affected areas.
Infection of wounds can cause life-threatening conditions:
- Cellulitis is a purulent inflammatory process that occurs in the subcutaneous fatty tissue, quickly growing into adjacent tissues;
- Osteomyelitis – inflammation of the bones;
- Purulent arthritis - inflammatory processes in joints and ligaments;
- Destruction of vascular walls - entails bleeding and poses a danger to life due to the possible spread of infection through the blood throughout the body;
- Blood poisoning is the most dangerous condition, since pathogenic bacteria can penetrate the most important organs - the brain, heart and cause irreversible processes. In more than half of cases, this disease is fatal.
What to remember
- Before you begin treatment of a pressure wound, you should clarify the stage of its development, otherwise the medications used may be ineffective.
- Stages 1 and 2 bedsores are considered superficial, 3 and 4 - deep.
- Superficial wounds can be cured at home, deep pathological changes only with the participation of a surgeon.
- Traditional medicine can be used as an adjuvant in the treatment of pressure wounds.
- An anti-decubitus mattress reduces the likelihood of skin ulcers, but does not cure them.
Stages of pathology
So, above we discussed what such phenomena as bedsores are, causes, prevention. Treatment of pathology varies depending on the extent of the process occurring. That is why it is advisable to touch upon the main stages according to which bedsores develop.
Stage 1. Initial degree, which is characterized by the presence of the following symptoms:
- The surface of the skin is not damaged.
- There is redness. If the patient has light skin. When pressing on such an area, the color does not change.
- In dark-skinned patients, redness is not visible. However, when pressed, the epidermis does not turn white. The surface may appear irritated, cyanotic, or purple.
- Sometimes such areas are painful and especially sensitive. They may feel warmer or colder to the touch, softer than the rest of the skin.
Stage 2. Now the bedsore is an open wound. The following symptoms characterize degree 2:
- The epidermis (top layer of skin) is damaged. Sometimes it may be completely absent.
- A red-pink, swollen wound is visually observed. It reminds me of an ulcer.
- In some cases, a bedsore is a blister filled with fluid. It may be intact or already burst.
Stage 3. We are talking about a deep wound here. The symptoms are as follows:
- The bedsore reaches the fatty tissue.
- The resulting ulcer looks like a crater.
- There may be yellowish dead tissue at the bottom of the wound.
- This damage spreads further, affecting layers of healthy skin.
Stage 4. This grade is assigned to extensive tissue necrosis. The signs of stage 4 are as follows:
- Bones, tendons, and muscles may be visible in the wound.
- The bottom of the ulcer is represented by hard dead tissue, dark in color.
- The lesion is widespread far beyond the primary focus.
Categories of people especially in need of proper care
Elderly bedridden patients are most susceptible to developing bedsores
Prevention of bedsores is especially necessary if the bedridden patient:
- elderly;
- completely immobilized, for example, with damage to the brain and spinal cord;
- has a fever;
- is obese or, on the contrary, weighs too little;
- does not eat well due to various reasons, especially if he receives little protein from food;
- drinks little;
- has diabetes;
- suffers from anemia;
- notes increased sweating;
- cannot hold urine or feces;
- has dry, thin skin;
- suffers from kidney disease, due to which the tissues swell;
- sick with obliterating endarteritis, atherosclerosis, vascular thrombosis;
- suffers from diseases of the nervous system that rob him of sensitivity in the limbs or torso and limbs;
- disoriented in a place, in one’s own personality, while the person does not lie quietly, and wrinkles the bed linen under him (see symptoms of dementia).
In the last two cases, such a person will not be able to complain that something is pressing or hurting; he will need to be patient and check all the “usual” places for bedsores constantly.