Why is urination impaired during menopause?
A decrease in estrogen levels and a radical change in the hormonal levels of the female body affects the functionality of all internal organs, especially the genitourinary system. There is a decrease in immunity, impaired blood circulation in the pelvic organs, and deterioration in the morphology of the vaginal mucosa. The urethral sphincter weakens. For this reason, already at the beginning of menopause, a woman complains of a frequent urge to urinate.
Vaginal dryness
The functionality of the excretory system is related to the level of estrogen in the body. During menopause, their number noticeably decreases, which causes dryness of the vaginal mucosa. A reduction in mucus secretion is also observed in the urethra. The genitals become vulnerable to infections. The structure of the mucous membranes of the urinary system becomes thinner. Pathological processes provoke urinary incontinence.
Weak pelvic floor muscles
With age, the muscular system becomes weaker. During menopause, the process becomes more noticeable. The reason is a reduction in the amount of estrogens that produce collagen. Muscle weakness contributes to loss of control over the organs of the urinary system.
In advanced cases, prolapse of the reproductive organs occurs. If treatment is not started in a timely manner, they resort to surgical therapy.
Decreased bladder elasticity
Menopause provokes changes in hormonal levels. As a result of decreased elasticity, the walls of the bladder become rigid. This makes the organ more sensitive: it is susceptible to contraction even with small movements. The urge to urinate appears if the volume of urine is above 100 ml when the normal value is 400 ml.
Excess weight
Metabolism is directly related to hormonal levels. During menopause, most women suffer from excess weight. This has a negative impact on the condition of internal organs, which are unable to cope with the resulting load. The intestines and bladder weaken. It becomes difficult for a woman to hold urine when she urges.
Urination disorder
Experts identify several conditions associated with pathological urination.
- Stress urinary incontinence. Appears in a certain situation - physical activity, especially heavy lifting, coughing, laughter, severe emotional stress, crying. This happens due to tension in the abdominal muscles, as a result of which the sphincter of the urinary canal relaxes.
- Sudden urinary incontinence . The situation is provoked by internal changes in the body; external factors do not play a role. The process is completely uncontrollable, it is impossible to foresee or predict when this will happen.
- Frequent urination . Going to the toilet continues endlessly during the day and at night. There is a constant urge to urinate. In this case, urine is released in small quantities.
The appearance of burning, itching, and other unpleasant sensations in the genitourinary organs is grounds for contacting specialists. This is how inflammatory processes manifest themselves.
- Urinary incontinence during menopause is characterized by the following symptoms:
- Urine is poured out during any physical activity, the process is not controlled, the woman does not feel the urge before this.
- When the bladder is full and the urge appears, the woman does not have time to run to the toilet.
- Going to the toilet continues at night. Urination during menopause at night more than 2 times is considered pathological.
What to do if you have fibroids?
- You are experiencing sudden abdominal pain.
- And I’m already quite tired of long and painful periods.
- And for some reason the recommended medications are not effective in your case.
- In addition, constant weakness and ailments have already become a firm part of your life.
- Now you are ready to take advantage of any opportunity.
An effective treatment for uterine fibroids exists. Follow the link and find out what the woman who cured uterine fibroids recommends to you - after the doctors did not help her.
Symptoms of disorders
Imperative disturbances in urinary excretion during menopause are a combination of frequent urination during the day and night against the background of atrophy of the vaginal mucosa.
The problem is accompanied by the following symptoms:
- The urge to urinate bothers you at night. A woman may experience them more than twice.
- The urinary tract becomes infected.
- Urine is released involuntarily during periods of laughter, coughing or physical exertion. It is stress incontinence that causes social and hygienic problems.
Frequent urination interferes with a full life. Women suffering from a severe form of the disease are forced to stay at home.
- Dry mouth and frequent urination: causes and which doctor to consult
Lifestyle of a woman with symptoms of urinary incontinence
Some targeted changes and restrictions may help, such as:
- Refusal to consume alcohol, chocolate, vinegar, dairy products, tomatoes, citrus fruits, coffee, sweets, large amounts of liquid. These foods and drinks are bladder irritants.
- Monitoring the relationship between your height and weight, bringing them closer to normal. The accumulation of excess fat puts pressure on the organs of the genitourinary system and provokes incontinence.
- Getting rid of severe constipation, after consulting with a urologist about your diet.
- Refusal to use diuretics and laxatives in treatment.
- Training the pelvic floor muscles with Kegel exercises. This is an effective way to get rid of incontinence.
- Getting rid of the addiction to smoking, this habit is often the cause of urinary incontinence.
- Visiting the toilet every 2-4 hours during the day is mandatory.
The appearance of mucous secretions due to improper metabolism
One of the causes of mucous secretions is metabolic disorders. It is also necessary to consider various pathologies such as diabetes, blood pressure problems or obesity. The combination of all these diseases, as well as hormonal changes in the female body during menopause, can affect the properties of vaginal secretions, which can change their color and aroma.
Most women during menopause are at risk of exposure to pathological processes in the internal genital organs. This primarily applies to the formation of malignant tumors. Even if sexual secretions that smell unpleasant appeared after menopause, and they were not there before, it is necessary to carry out all examinations so as not to miss and get rid of the development of severe pathology.
Treatment of incontinence
The problem that has arisen can and should be treated; there are a sufficient number of ways to get rid of urinary incontinence during menopause.
- Balanced diet. You need to eat more healthy foods that contain fiber and help prevent constipation. You need to add vegetables and fruits to your diet, as well as whole grain bread. At the same time, it is important to maintain the consumption of clean water (not counting tea, coffee and other drinks), 40 ml of water per 1 kg of weight is required. This will prevent unnecessary problems with bowel movements and overactive bladder.
- Physical exercise. Diversify your leisure time with various active hobbies or walks in the fresh air. Stand up as often as possible when working sedentarily.
- Physiotherapy. A set of simple exercises is required to maintain the tone of the pelvic floor muscles.
- Regulate your urination time. You should visit the toilet at the first urge of the bladder, do not put it off until later, this leads to muscle strain and increased sensitivity of the organ.
If you follow these simple rules, you can avoid drug and surgical treatment of urinary incontinence.
Associated symptoms
Vaginal and genitourinary disorders are inherent in urogenital problems. Due to insufficient estrogen production during menopause, the vaginal microflora undergoes changes. The deterioration of her condition provokes the spread of pathogenic bacteria. During this period, the woman begins to worry about thrush, atrophic vaginitis, urethritis and cystitis. Poor circulation in the urethral area leads to increased urination.
Severe symptoms of urethritis include:
- feeling of discomfort in the urethra;
- itching;
- aching pain in the lower abdomen;
- burning sensation in the urethra;
- increased body temperature;
- nausea;
- asthenia;
- discharge from the genitals;
- bloody issues;
- prolapse of the posterior or anterior vaginal wall.
Symptoms at the onset of the disease may be blurred. Diagnosis of the pathology is difficult due to the lack of clear signs.
The following may act as a provocateur for exacerbation of chronic urethritis:
- hypothermia;
- drinking alcohol;
- emotional disorder;
- sexual intercourse.
Lack of therapy provokes the disease to become chronic, which further complicates therapy.
In the chronic course of the pathology, symptoms are spontaneous and worsen when exposed to negative factors.
Symptoms
Menopause in women is accompanied by severe disturbing symptoms. The main things patients complain about are headaches, frequent hot flashes, and increased sweating. Complaints about urinary incontinence are less frequent. Often a woman does not understand that she is faced with just such a problem. You can determine your urinary incontinence by the following signs:
- fluid flows out of the urethra during coughing, sudden movement, strong tension, sneezing;
- if you want to go to the toilet in a small way, you cannot restrain yourself even for a few minutes;
- urine leakage regularly occurs during night sleep;
- frequent exacerbations of chronic cystitis, accompanied by pain in the lower abdomen, burning and pain when emptying the bladder;
- Every trip to the toilet is accompanied by the release of a small amount of urine and a feeling of incomplete emptying.
The intensity of manifestations depends on the stage of the pathology. In medicine, there are three degrees of urinary incontinence.
- Easy. Accompanied by unpleasant sensations and discomfort when going to the toilet in small ways, frequent urges and night awakenings. The volumes of spontaneously leaking liquid are insignificant. It happens that the patient does not notice signs of the disease, perceiving wet underwear as natural processes in the body.
- Average. The patient experiences repeated spontaneous urine discharge throughout the day. It is already difficult to ignore such symptoms, so the woman begins to look for methods to solve an intimate problem.
- Heavy. During the day, a woman experiences more than 10 spontaneous discharges from the urethra. In this case, the patient feels the urge, but urination is weak and incomplete. Leaks occur between trips to the toilet. With severe incontinence, a woman suffers from enuresis.
Diagnostics
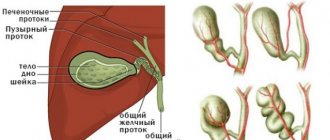
Diagnosis of urination during menopause is not difficult. You should seek help from a specialist. The gynecologist prescribes an ultrasound of the pelvic area, kidneys and urethra, as well as a number of laboratory tests.
Analyzes
Laboratory diagnosis involves a general urine test, a test for urine outflow in the bladder and culture for the presence of bacteria. If a traditional examination in a laboratory does not indicate negative results, then they resort to consulting a psychologist.
- Cystitis during pregnancy: cure and prevent recurrence
Ultrasound
A common diagnostic method for urinary incontinence during menopause is ultrasound examination. An ultrasound examination determines the functionality of the bladder ureter, urethra and uterus.
Additional measures
It is important to carry out differential diagnosis to distinguish cystitis from other pathologies of the urinary tract, which are characterized by inflammation. The specialist excludes the presence of vascular dementia, diabetes mellitus, circulatory disorders and Parkinson's disease.
Treatment
Frequent urination during menopause is not a disease as such, but there are cases when treatment for this disease is simply necessary. There are several treatment options depending on the severity of the symptom. Conservative treatment for frequent urination:
- electrical stimulation of muscles;
- exercises that strengthen the pelvic muscles;
- introduction of collagen and blood plasma into the periurethral area to fix and stabilize the functioning of the urethra.
For incontinence, patients may undergo surgery using the free loop method or a sling. A sling is a small strip made of a special material that is placed in the pelvis, where it holds the cervix, holding back fluid, preventing it from descending.
Drug therapy
Depending on the cause of this symptom during menopause, a certain group of medications is prescribed:
- uroantiseptics are prescribed for cystitis, pyelonephritis or urethritis (Canephron, Uronesan);
- antibiotics are prescribed for inflammation of the urinary system (Amoxiclav, Gentamicin);
- pribiotics are prescribed if the flora in the urinary and reproductive tract has been changed (Linex, Bifiform);
- insulin therapy is used if the patient has diabetes;
- antispasmodic therapy is prescribed if stones are also observed in the urinary tract (No-shpa, Spazmalgon).
Prevention
To prevent frequent urination in women over 60, you need to start changing your lifestyle after age 40.
- Be sure to exercise to keep your pelvic muscles toned. Daily walking will also be very beneficial.
- Eliminate alcohol from your diet, as well as strongly brewed tea and coffee.
- You should always watch your weight.
- Take various complex medications to support the body during changes, as well as vitamin and mineral supplements.
- It is important to visit a gynecologist at least twice a year so as not to lose sight of the pathological processes that gain momentum at this age.
Let's summarize. Don't be discouraged if you experience frequent urination during menopause. You already know what to do. The most important thing is to find a doctor with whom you can easily discuss any concerns!
Drug treatment
Medicines are necessary when urinary incontinence has become too severe to be treated with physical therapy alone. It can be treated with various drugs. Antispasmodics demonstrate good effectiveness, they reduce the tone of the smooth muscles of the urinary tract, thereby significantly reducing the number of urges. These drugs include Vesicare, Detrusitol and Driptan.
Medicines such as Aksamon, Neuromidin and Ubredit help to cope with excess nerve impulses. They reduce the activity of the bladder sphincter and urinary tract. Cymbalta and Duloxetine will help restore flexibility, elasticity and firmness of the pelvic floor muscles.
Since menopause, first of all, negatively affects hormonal levels, it is often recommended to take appropriate hormonal medications. They help stabilize hormone production or replace missing biologically active substances. Thanks to this, it is possible to eliminate many unpleasant symptoms of the menopause. The most common drugs in this group are Klimen, Divina and Klimonorm.
What to do with severe urinary incontinence in women, which makes it impossible to lead a normal lifestyle? Surgery will help get rid of the problem, if not forever, then for a long time. There are many similar methods that are quite effective and do not cause serious damage to women’s health:
- installation of a sling - a special elastic loop that supports the urethra in a position in which unauthorized leakage of urine becomes impossible;
- colposuspension - attachment of weakened muscles of the urethra to the inguinal ligaments;
- injection of special substances - collagen, silicone, adipose tissue, into the submucosal area of the urethra. Thanks to this solution, it is possible to achieve a normal position of the organ;
- Colporrhaphy is a modern method based on artificial tightening of the vaginal walls, as a result of which the pressure on the bladder is reduced and urination is normalized.
It is important to understand that menopause is inevitable, and it will bring with it significant changes in the body. Therefore, every woman should carefully monitor her health. If you feel that you are having problems urinating, be sure to visit your doctor.
Causes of disruption of the normal process of urination during menopause
Even if you have never experienced such discomfort and strictly monitor your health, incontinence during menopause can still occur. This is primarily due to hormonal changes. Lack of estrogen provokes a loss of tissue strength and elasticity, which disrupts the normal functioning of the bladder.
There are several reasons for frequent urination during menopause in women:
- Pain in the lower abdomen and frequent urination: reasons, why it is dangerous and what to do
- Loss of muscle tone in the pelvic floor. Due to loss of collagen, muscles are no longer able to fully control urination.
- Overweight. During menopause, a woman's body can gain weight, and every extra kilogram puts additional stress on the pelvic floor muscles, which already suffer from loss of elasticity.
- Loss of elasticity of bladder tissue. Urinary incontinence during menopause can be caused by bladder tissue that does not stretch well and becomes stiff with age. All this causes irritation, which causes the organ to contract at the slightest physical activity.
- Lack of mucous secretion. Dryness of the mucous membranes during menopause leads to thinning of the tissue, which in this state cannot effectively fight infections without allowing them into the body.
- Changes in the position of the internal genital organs. The reason for frequent urination during menopause may be prolapse of the vagina or uterus due to weakening of the walls. Therefore, the female organ changes its location, irritating the bladder.
- Presence of diseases. Disturbances in the urinary system may be associated with problems of other organs (kidney problems, diabetes, impaired digestion).
- Uterus removal. Doctors have not yet fully studied the connection between uterine loss and incontinence during menopause, but this problem may well arise after surgery.
Causes of frequent urination
Frequent urination, which can be caused by urinary incontinence and cystitis, has many causes. As a rule, in the overwhelming majority of cases, the development of cystitis and urinary incontinence in women during menopause is based on hormonal imbalance.
Weakness of the pelvic floor muscles
A decrease in the tone of the pelvic floor muscles is possible in the absence of regular intimate life. In turn, irregular sexual intercourse is caused by a decrease in libido due to hormonal imbalance.
Changes in bladder elasticity
A decrease in sex hormones significantly affects the tissues of the genital organs and the walls of the bladder. As a result, tissues lose their elasticity and tone. Thus, estrogen deficiency contributes to thinning of the bladder walls and deterioration of blood supply.
Sexual infections and vaginal dryness
In turn, changes in the walls of the bladder create favorable conditions for the proliferation of opportunistic and pathogenic microflora. It is the proliferation of pathogenic flora that causes the development of cystitis.
Dryness of the vaginal walls also occurs due to a decrease in the amount of estrogen. Gradually, a change in the vaginal microflora is observed, which can be transferred along an ascending path.
Obesity
Often, during menopause, women experience excess weight, which appears due to insufficient physical activity, metabolic disorders and poor nutrition. Excess weight negatively affects the condition of bladder tissue.
During menopause, there is a decrease in the body's defenses. As a result, non-compliance with the diet, minor hypothermia and other provoking factors can cause cystitis.
Possible consequences
For the vast majority of women, frequent urination has a negative impact on both the physical and psychological levels. Pathology changes the entire structure of life. The woman is mentally focused on the problem. Long walks and sports become impossible.
The feeling of uncleanliness aggravates the problem, since even aromatic pads are not able to cope with the pungent odor of urine and absorb the entire volume of excreted urine. The woman begins to avoid visiting public places.
Why does urine smell strong during pregnancy?
During pregnancy, a woman's kidneys produce much more urine in response to hormones and the needs of her growing unborn child. But even during this period of life, urine should not have a sharp and fetid odor, although its presence may not always indicate any diseases.
In fact, the smell of urine during pregnancy intensifies after the first days of fertilization of the egg. The problem is that not all women notice this in a timely manner, and after they discover it, they panic. If your urine is a normal, natural color, then there is most likely nothing to worry about.
Changes in urine odor during pregnancy may occur due to lack of adequate hydration. Pregnant women should drink more water because fetal fluid needs new supplies just as much as you and your baby do. The expectant mother should drink 8-10 glasses of water per day.
During pregnancy, you may experience urinary incontinence, which is characterized by involuntary leakage of fluid from the bladder when you strain, cough or sneeze. Even a small leak can significantly increase the unpleasant smell of urine.
ATTENTION! Feeling lonely? Losing hope of finding love? Do you want to improve your personal life?
You will find your love if you use one thing that helps Marilyn Kerro, a finalist in three seasons of the Battle of Psychics.
Diagnostic methods
Ultrasound is always used to identify pelvic pathology. The reproductive organs, urethra, bladder, kidneys and ureters are examined. In this way, violations of the structure of organs, changes in their position, and the presence of neoplasms are determined.
It is necessary to submit a urine test and a vaginal smear; a blood test for hormones, an ultrasound of the thyroid gland, and a consultation with an endocrinologist and other specialists may be prescribed. It is possible that complex treatment will be required.
Risk factors
Below we will discuss in more detail what provokes frequent trips to the toilet in adulthood.
- Muscle tone. Previously, the pelvic muscles were in good shape. Thanks to their elasticity, a woman could hold urine. And when possible, empty the bladder. Menopause changes this process. And control is lost.
- Obesity. If you are overweight, the organs located in the lower abdomen are overloaded with heaviness. Frequent urge to urinate occurs more often in older, overweight women, especially if they have been obese throughout their lives. But for those patients who have gained extra pounds due to menopause, problems are also possible.
- Bladder tissue. Loss of elasticity of the walls of the bladder leads to their ability to stretch. And even a minimal amount of urine provokes the urge.
- Dry mucous membranes. The infection easily penetrates the bladder if the protective barrier is broken due to drying out of the mucous membrane.
- Uterine prolapse. If the muscles completely lose their elasticity, then it will be impossible to retain the internal organs. And then they leave the correct position. This often happens with the uterus. And in those cases when it is deleted. There is no clear answer to why this happens. And yet, because of one organ, others also suffer.
What diseases can biofeedback treat?
- Stress urinary incontinence (stress urinary incontinence).
- Overactive bladder or urge urinary incontinence.
- Initial stages of prolapse of the uterus and walls of the vagina, bladder and rectum; prevention of severe prolapse in the future
- Postpartum changes in the pelvic floor.
- Female sexual disorders.
- Interstitial cystitis and a number of cases of pelvic pain syndrome.
- Incontinence of gas and/or stool
How are biofeedback treatment procedures structured?
Treatment with the biofeedback method is carried out in the form of exercises on the Urostym device , manufactured by Laborie , Canada.
This unique system allows the patient to coordinate the work of the pelvic floor muscles with specific visual images that are displayed on the computer screen. It's like an exciting computer game. For example, by tensing your pelvic floor muscles, you can virtually control a combat helicopter through the Urostym system and shoot at targets or perform other virtual actions. This makes the treatment process more effective, and, of course, interesting and easy.
Together with biofeedback therapy, ELECTRIC STIMULATION OF THE PELVIC FLOOR MUSCLES can be effectively used.
The method is based on the use of a natural phenomenon given to us from birth - nerve endings approach muscle fibers and cause them to contract when necessary.
Electrical muscle stimulation
promotes restoration of nervous and muscle tissue, improvement of neuromuscular impulse transmission.
In combination with the biofeedback
, electrical stimulation allows you to achieve muscle strengthening and proper functioning with the possibility of using these skills in everyday life.
Treatment of urogenital disorders in menopause
The goals of therapy are to reduce the symptoms of vaginal and cystourethral atrophy in order to improve the quality of life of menopausal women.
Indications for hospitalization
Hospitalization is indicated for patients with stress urinary incontinence for surgical treatment.
Non-drug treatment
Using biofeedback and electrical stimulation of the pelvic floor muscles.
Drug therapy
For urogenital disorders, pathogenetic systemic and/or local hormone replacement therapy is carried out. Systemic HRT regimens are described in detail above.
Local therapy is carried out if the patient does not want to receive systemic therapy or there are contraindications to systemic therapy.
Combined (systemic and local) therapy is indicated when systemic therapy is insufficiently effective.
In the presence of imperative urinary disorder syndrome, drugs are additionally used that have an antispasmodic effect on the detrusor, thus normalizing the tone of the bladder and urethra.
- M-anticholinergics: oxybutynin 5 mg 1–3 times a day orally before meals, or
- tolterodine 2 mg 2 times a day, or
- trospium chloride 5–15 mg in 2–3 doses.
- tamsulosin 0.4 mg 1 time per day orally after breakfast, or
- midodrine 2.5 mg 2 times a day orally, course 1–2 months.
- distigmine bromide 5–10 mg 1 time per day in the morning orally 30 minutes before meals. The duration of therapy is determined individually.
[37], [38], [39], [40], [41]
Surgery
For stress urinary incontinence, surgical treatment is indicated. The most rational and minimally invasive is the TVT or TVT-O operation (application of a free synthetic loop under the middle third of the urethra using vaginal access) or the introduction of DAM(+) gel into the paraurethral space.
Sources used:
- https://doktora.guru/simptomy/obschie-simptomy/nederzhanie-mochi.html
- https://stopzaraza.com/pochki/chastoe-mocheispuskanie-u-zhenshhin-pri-klimakse.html
- https://stopzaraza.com/pochki/nederzhanie-mochi-u-zhenshhin-pri-klimakse-raznovidnosti-prichiny-diagnostika-lechenie-i-preparaty.html
- https://uran.help/diseases/chastoe-mocheispuskanie-pri-klimakse.html
- https://ilive.com.ua/health/urogenitalnye-rasstroystva-v-klimakse_77365i15953.html
Diagnosis and treatment
Certain women are convinced that enuresis in women during menopause cannot be cured. And you can only hide the smell using scented pads. In fact, if such a difficulty is left without treatment, it will become more complicated and turn into some other, more serious disease that can no longer be treated. Such a problem needs to be cured, and for this purpose there are a large number of methods that depend on the main reason for its occurrence.
Conservative treatment
To eliminate urinary incontinence during menopause, therapy can be complex. Essential importance in this method of treatment relates to Kegel exercises - gymnastics to restore muscle tone of the pelvic floor. These exercises are performed while sitting. The bottom line is this: you need to alternately tense and relax your muscles. You can imagine that you want to go to the toilet, but you need to restrain the urge to urinate. Such exercises should be performed 3-4 times a day. Start with a short period of muscle contraction and gradually reach the point of holding in one position for 3 minutes. Then you can change the exercises a little, performing them during coughing, laughter, and other provoking conditions. Such incontinence can also be cured with the help of medications. However, it can only help with mild variants of the disease. What is prescribed for this disease:
- Driptan;
- Vesicare;
- Detrusitol.
These drugs affect the activity of the urethra and bladder sphincter;
- Ubretid;
- Aksamon;
- Neuromidin.
These drugs also have the ability to restore flexibility of the pelvic floor muscles:
- Duloxetine;
- Cymbalta.
These drugs relieve tension in the nervous system, helping to normalize other processes in the body. To eliminate this difficulty, certain women resort to hormonal drugs, which are used to relieve a number of menopausal symptoms:
- Klimonorm;
- Divina;
- Klymen.
Homeopathic substances can also correct this condition:
- Remens;
- Klimadinon;
- Climaxan.
Surgical operations against incontinence
To eliminate this problem 100%, which usually appears during menopause, therapy can also be surgical. It is more traumatic, but provides an excellent effect. You should not use surgery if you have a serious form of diabetes mellitus, inflammation and tumor diseases, or pathologies in blood clotting. There are several types of operations:
Using a sling
A sling is an elastic device in the form of a loop that helps maintain the urethra in the desired position. As a result, urine will not be able to flow out on its own. A similar procedure is performed under local anesthesia, and this is the most common action for this problem. However, return of urinary incontinence is likely and this procedure may be repeated;
Use of medications
There are substances (collagen, adipose tissue, silicone) that, when introduced into the submucosal area of the urethra, secure it. This forms the anatomically correct position of the urethra. They are hypoallergenic, and the procedure itself is practically non-traumatic. Effectiveness is achieved by replenishing the lack of soft tissue in this area. Injections are performed on an outpatient basis, local anesthesia is used, however, this method is not a panacea. After this is done, the problem may reappear.
Colposuspension
The tissues that have lost their tone near the urethra are secured to the inguinal ligaments. This is done during laparoscopic surgery using general anesthesia. From the point of view of effectiveness, this method is in the first position. However, in most situations it is used as a last resort, since it has a significant list of contraindications and difficulties in performing the operation;
Colporrhaphy
Using this method, the vaginal walls are tightened. When their position normalizes, the factors of urinary incontinence disappear, as the pressure on the organs decreases.
What else can be done to normalize urination?
For urinary incontinence during menopause, therapy does not have to consist solely of the efforts of the attending physician. It is necessary to change your lifestyle, which will help eliminate or prevent the problem from forming:
- Take 30-minute walks;
- Beware of foods and drinks that irritate the bladder (pepper, alcohol, coffee, chocolate);
- Strive to go to the toilet “little by little” according to the schedule;
- Monitor your body weight, try to lose weight if you have excess fat. Urinary incontinence is not at all an end to a normal life. This is only a prerequisite for visiting a doctor. In modern medicine, this problem is treated without consequences.
How to correct your own lifestyle Therapy for a disease such as urinary incontinence during menopause can take a certain period. During this period of time, a woman needs to follow the following principles of a healthy lifestyle:
- get rid of bad habits (smoking and drinking alcohol);
- eliminate overly peppery foods, herbs and spices from the menu;
- try to stick to the diet, table No. 8 in order to control body weight;
- use gaskets;
- Carry out personal hygiene after each urination and bowel movement.
Particular attention should be paid to the daily routine. A woman must go to the bathroom every 2-3 hours to completely empty her bladder, without allowing urine to accumulate and stagnate. If you have urinary incontinence, which is accompanied by a strong unpleasant odor, even despite hygiene procedures, you should drink more water per day. Water will rinse the urinary tract well, and the unpleasant odor will be eliminated. If the smell of urine is very strong, we can conclude that there is an inflammatory process in the bladder. In this case, you should immediately consult a doctor.