One of the most serious diseases known to mankind is cerebral hemorrhage (CB).
Half of the patients who have suffered it die, the rest become disabled.
A favorable prognosis directly depends on how promptly the patient contacted a specialist, and how quickly the causes were identified and treatment began.
Characteristics of the pathology
The names “cerebral hemorrhage” and “hemorrhagic stroke” mean the occurrence of the same disorders. Spontaneous cerebral hemorrhage is bleeding that occurs in the brain parenchyma (nervous tissue), often spreading to the area of the ventricular system, less often to the area of the subarachnoid space (the cavity between the membranes of the brain - soft, arachnoid), which causes the corresponding symptoms.
Hemorrhage in the brain is called a violation of cerebral blood flow, which occurs in an acute form, and is associated with damage to the integrity of the walls of blood vessels, which causes blood to enter the parenchyma. Bleeding into the substance of the spinal cord is called hematomyelia. The main reasons why hematomyelia occurs: injuries in the spinal column, excessive muscle tension in the back (heavy lifting, tiring exercises).
Brainstem stroke - what is it?
Brainstem stroke is an acute pathological condition in which blood circulation in the brain stem is disrupted. Stroke can also affect the brain and spinal cord (called spinal stroke). As a result, neurons are starved of oxygen and die, which leads to the loss of brain functions controlled by this area.
Why does a brainstem stroke occur, what is it and is recovery possible for patients who have suffered an attack?
The brain stem is an important part of the nervous system. It is located at the base of the skull, through which pass pathways connecting the spinal cord and the cerebral cortex. The brain stem includes the medulla oblongata, pons and midbrain, contains cranial nerves and their nuclei, vasomotor, respiratory nerve centers. Thus, the brain stem ensures the interaction of central nervous system structures, transmits commands from the brain, carries out reflex reactions, chewing, swallowing, regulates muscle tone, is responsible for breathing, blood circulation, autonomic reactions, thermoregulation, balance, and participates in the functioning of the organs of hearing and vision.
Alcohol abuse and smoking, poor and irregular diet, excess weight, sedentary lifestyle, stress, and overwork increase the risk of stroke.
Types of strokes
Ischemic brainstem stroke occurs due to blockage or compression of the vessels carrying blood to the brain, a detached thrombus, a blood clot, or, in rare cases, droplets of fat or air bubbles. Compression of the vessel may occur due to a tumor or scar formed after an injury. Ischemic stroke develops much more often than hemorrhagic stroke and has a more favorable prognosis.
A hemorrhagic stroke develops as a result of a rupture of a vessel, in which not only the nutrition of a certain area of the brain is disrupted, but the blood permeates and compresses the brain tissue, forming a hematoma. With a hemorrhagic brainstem stroke, life-support nerve centers are damaged in the brainstem.
Due to a lack of oxygen, the nerve cells of the stem brain cease to perform their functions, as a result of which the coordinated work of all internal organs ceases.
Causes
Among the pathologies leading to brain stem stroke, the most common are the following:
- arterial hypertension - causes irreversible changes in the arteries and arterioles of the brain, the walls of blood vessels become brittle, and sooner or later they may rupture with hemorrhage;
- atherosclerosis - observed in most older people, leads to the appearance of cholesterol plaques in the arteries supplying the brain, as a result of which the plaque clogs the vessel;
- aneurysms and vascular malformations – cause strokes in young patients without concomitant pathology or in combination with it;
- diabetes mellitus and other metabolic disorders affecting blood vessels;
- rheumatic diseases;
- heart diseases - valve pathologies and congenital defects;
- bleeding disorders, including when taking thrombolytic drugs prescribed to cardiac patients.
2/3 of cases of brain stem stroke are fatal; the most dangerous period in this regard is the first two days.
Alcohol abuse and smoking, poor and irregular diet, excess weight, sedentary lifestyle, stress, and overwork increase the risk of stroke.
Symptoms of a brainstem stroke
The deterioration of the condition occurs suddenly, the following signs are observed:
- articulation and clarity of speech are impaired (slurred speech);
- there is a lack of coordination;
- dizziness occurs, gait becomes unsteady;
- facial skin may become pale or red;
- blood pressure rises, pulse quickens;
- the temperature decreases and then increases;
- sweating develops.
In the future, these symptoms may be accompanied by respiratory and circulatory disorders. Breathing during a stroke becomes hoarse, rapid, shallow, with difficulty inhaling and exhaling. The patient may lose consciousness.
In some patients, brain stem stroke is accompanied by the development of locked-in syndrome. In this condition, as a result of disruption of the transmission of impulses from the brain to the muscles of the body, paralysis of the limbs and complete loss of motor function occurs. The patient retains consciousness and is able to understand and evaluate what is happening. For such a patient, active participation in his rehabilitation is possible.
Even minor symptoms of a stroke cannot be ignored, as a stroke can lead to irreversible consequences. When the first signs appear, you must immediately seek emergency medical help, and until doctors arrive, provide the patient with rest in a lying position and an influx of fresh air.
Treatment tactics
The prognosis for stroke directly depends on the time of initiation of treatment. A patient with acute cerebrovascular accident must be taken to the neurosurgical department of the hospital as quickly as possible. How long does the treatment take, what kind of therapy is carried out in the hospital, and what is the likelihood that the patient will recover from a stroke?
The possibility of successful rehabilitation depends on which functional centers of the brain stem were affected and which functions were affected.
In the first few hours after a hemorrhagic stroke, surgery may be necessary to stop the bleeding.
If necessary, platelet mass is infused into the affected area. This method is especially effective in the first few hours after the onset of the disease. Studies show that patients who received such therapy had a faster improvement in the trophism of ischemic tissue, a faster recovery of motor functions and a lower risk of death. Among other things, platelet infusion reduces the risk of late complications.
In the first 1–3 days after a stroke, treatment is carried out in a hospital setting. After stabilization of the patient’s condition, diagnostics are carried out to determine the extent of damage to the stem structures. In accordance with the test results, treatment is prescribed, which has the following goals:
- restore and maintain vital functions of the body;
- restore physiological blood supply to areas of the brain affected by stroke;
- relieve swelling and inflammation of damaged brain tissue;
- maintain the rheological properties of blood and normal coagulation;
- support the functioning of the cardiovascular system.
Specific treatment is also prescribed, which depends on the location and size of the lesion.
After discharge from the hospital, treatment at home continues for several weeks, including drug therapy, massage and exercise. This is followed by a rehabilitation period that may take several months.
Prognosis for recovery from brainstem stroke
2/3 of cases of brain stem stroke are fatal; the most dangerous period in this regard is the first two days. This is due to a violation of basic life functions.
Even minor symptoms of a stroke cannot be ignored, as a stroke can lead to irreversible consequences.
The prognosis largely depends on the timeliness of medical care provided; treatment is most effective in the first three hours after the attack. The prognosis depends on the patient’s age: in old people, the body’s regenerative abilities are reduced.
The possibility of successful rehabilitation depends on which functional centers of the brain stem were affected and which functions were affected:
- breathing - a disorder occurs when the respiratory center of the brain stem is damaged. The patient cannot breathe on his own and in most cases becomes dependent on a ventilator. However, if the respiratory brain center is not completely destroyed, recovery is possible;
- swallowing – one of the main signs of brainstem infarction is dysphagia, or swallowing disorder. This disorder occurs in most people who have had a brainstem stroke. Dysphagia threatens with life-threatening consequences: aspiration pneumonia, exhaustion and dehydration. The prognosis for recovery of patients with dysphagia is uncertain; constant drug therapy is required;
- coordination of movements - an early sign of a stroke is dizziness, an unsteady gait and loss of balance. Usually these signs disappear during treatment and rehabilitation. The prognosis for restoration of this function is generally favorable;
- motor skills of the limbs - with a stroke, control of the movements of the arms and legs is impaired, often on one side. A favorable prognosis for such a disorder can be made only in the first 2–3 months after a stroke, then the dynamics of recovery of motor functions decreases. After 6 months, complete or partial restoration of motor control is extremely rare;
- thermoregulation – a stroke may be accompanied by a violation of thermoregulation, which indicates a serious condition of the patient. A persistent increase in temperature above threshold values indicates damage to the thermoregulation center and aggravates ischemic damage to brain tissue. A decrease in body temperature for every degree doubles the likelihood of a favorable outcome;
- vision – when the oculomotor center, which is located in the brain stem, is damaged, eye movements are impaired. The chances of restoring visual functions with proper therapy are quite high.
Video
We offer you to watch a video on the topic of the article.
Types of hemorrhage
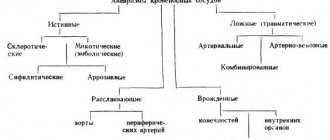
Considering what causes hemorrhage in the brain, primary and secondary forms of pathology are distinguished. Primary forms occur with a frequency of about 88% of cases; they arise as a result of rupture of medium- and small-caliber arteries, most often damaged in the process of chronic arterial hypertension or amyloid angiopathy.
Secondary forms are associated with tumors formed in the brain tissue, blood clotting disorders and abnormal development of elements of the circulatory system. In this case, the cause of intracerebral bleeding is ruptured aneurysms and arteriovenous dysplasia (improper development, absence of areas, underdevelopment of blood vessels).
There are forms of stroke (hemorrhagic stroke) taking into account the nature of the course - acute, acute, subacute. In the first case, there is a rapid transition to a coma with severe depression of respiratory and cardiac activity. The most acute form develops with extensive, large-scale hemorrhage in the area of the cerebellum, pons, and cerebral hemispheres, the consequence of which is death a few hours later.
In the acute form, symptoms develop over a period of several hours. Early diagnosis and correct therapy increase the patient's chances of a favorable outcome. Typically, the acute form occurs with bleeding in the lateral (side) parts of the hemispheres.
There are types of cerebral hemorrhages, taking into account the location and size of the hemorrhage. In 90% of cases, foci of hemorrhage form in the supratentorial (upper, above the tentorium of the cerebellum) areas of the brain. Taking into account localization, the following forms are distinguished:
- Subdural (between the meninges - dura, arachnoid). Associated with TBI. The acute course often leads to death; chronic forms, in the case of correct therapy, have a relatively favorable prognosis.
- Lobar (blood does not get beyond the cortex and white matter).
- Lateral (bleeding in the area of the subcortical nuclei, towards the outside of the internal capsule - a plate of white matter bounded by the caudate and lenticular nuclei).
- Medial (bleeding in the thalamus, towards the inner side of the internal capsule).
- Intraventricular (within the ventricular system).
- Mixed (distribution of blood in different anatomical zones).
Foci of hemorrhage in the posterior fossa of the skull (cerebellum, trunk) occur with a frequency of 10% of cases. Depending on the stage of completion, developing (progression of neurological symptoms is observed) and completed (regression of neurological symptoms is observed) hemorrhagic stroke is distinguished.
Treatment
Non-surgical (conservative treatment) is based on basic and specific reparative and neuroprotective therapy using medications of different spectrum of action.
Basic treatment
- Control of the respiratory system. Depending on the situation, intubation or artificial ventilation may be necessary.
- Normalization of blood pressure : lowering with medications for hypertensive patients and increasing for those suffering from hypotension. The heart rate is controlled (arrhythmia and tachycardia are avoided).
- Infusion therapy (to balance the water-salt balance and biochemical composition of the blood). Use of diuretics.
- Fighting hyperthermia.
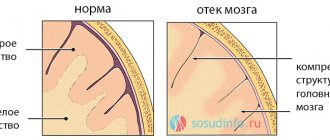
- Drugs that prevent and relieve swelling of the brain.
- Treatment of symptoms : in the presence of seizures - antispasmodics, in case of psychomotor agitation - sedatives.
Prevention of possible complications of an inflammatory-infectious nature (use of antibiotics and uroseptics).
Specific treatment is aimed at improving the repair of nerve tissue:
- antioxidants: Emoxipin, Mildronate, Vitamin E;
- neuroprotectors: Cerebrolysin, Actovegin, Piracetam.
Neurosurgical treatment
Surgery is indicated in almost all cases of hemorrhagic stroke, because pathology occurs at the site of hemorrhage.
Main indications for surgical intervention:
- The hemorrhage is located in a place that can be operated on without high risks;
- Rupture of aneurysm of a vessel;
- Increased intracranial pressure;
- Breakthrough of leaked blood into the ventricles of the brain;
If the decision is made to undergo surgery, it must be carried out as soon as possible. Surgically removing blood from the resulting hematoma will help relieve compression and thereby save lives.
Rehabilitation therapy
The recovery period is very long and varies depending on the complexity and extent of the hemorrhage.
Rehabilitation methods:
- physiotherapy;
- massage;
- physiotherapy.
Recovery is carried out under the supervision of a specialist. In case of speech dysfunction, sessions with a speech therapist are necessary.
Causes
Taking into account the causes of cerebral hemorrhage and accompanying symptoms, the doctor prescribes treatment. Bleeding in the brain occurs due to diseases that cause damage to the wall of the elements of the circulatory system, which causes its rupture or increased permeability. Main provoking diseases:
- Arterial hypertension (sustained increase in blood pressure).
- Vascular aneurysms (protrusion of the wall, pathological expansion of the artery), arteriovenous malformations (anomaly of vascular development, is an interweaving of arteries and veins without capillaries).
- Amyloid angiopathy (a disease of small cerebral vessels associated with the deposition of protein plaques on the walls - amyloid), vasculitis (inflammatory damage to the vascular walls), arteritis (inflammation of the vascular walls associated with infection or an autoimmune reaction).
- Hemophilia (blood clotting disorder caused by genetic factors), thrombocytopenia (decreased platelet concentration in the blood).
- Connective tissue dysplasia caused by genetic factors. It is characterized by defects in the fibrous structures of connective tissue, which leads to disruption of the formation of organs, including blood vessels (idiopathic increase in wall thickness, pathological tortuosity).
- Chronic alcoholism, accompanied by liver failure and hypocoagulation (deterioration of blood clotting).
- Angiomas (cavernous, venous). Tumors formed by abnormal blood vessels.
- Arterial dissection. A tear in the arterial wall, which allows blood to enter the space between the linings of the artery.
A common complication of cancer localized in the brain is hemorrhage into the tumor site. Other provoking factors: long-term use of anticoagulants, antiplatelet agents, fibrinolytic drugs (Acetylsalicylic acid, Heparin), drug use (cocaine, amphetamine).
Treatment of hemorrhagic stroke
When providing first aid to a patient with a hemorrhagic stroke, it is necessary to:
- call an ambulance;
- put the patient on the bed so that the head is 30 degrees above the body level;
- free the chest from clothing;
- provide access to fresh air.
If a cerebral hemorrhage is confirmed, the patient requires immediate hospitalization in a specialized intensive care unit or intensive care unit.
Therapeutic measures in the first days are aimed at supporting and restoring the vital functions of the body. It is necessary to provide a supply of humidified oxygen or transfer the patient to artificial ventilation, normalize blood pressure, and take measures that will help reduce cerebral edema and the level of intracranial pressure.
In the future, special attention is paid to preventing the occurrence of infectious complications and their treatment. The patient must be under the supervision of medical personnel throughout the entire rehabilitation period, because his condition may suddenly worsen.
Diagnostic methods
If the patient is conscious and able to communicate normally, it is necessary to collect an anamnesis from him or (if this is not possible) from close people and find out complaints. Changes will be noticeable when examining the patient; neurological defects will appear if you ask the patient to smile or stick out his tongue.
Computed tomography is considered the main method for diagnosing cerebral hemorrhage in a hospital setting; it allows one to diagnose the affected area, its location and size. It is also possible to use magnetic resonance imaging (especially if the lesions are small in size or vascular malforations are present). However, this diagnostic method is expensive and not always available.
In the presence of subarachnoid hemorrhages, lumbar puncture and examination of cerebrospinal fluid are considered an informative method. Red blood cells will be present in the cerebrospinal fluid. Another diagnostic method that will help detect hemorrhoidal stroke can be angiography; it allows you to determine the nature of blood flow in the affected vessels, as well as disturbances in vascular development due to the introduction of radiopaque substances.
Drug treatment
The therapeutic course of treatment of hemorrhagic stroke in the acute period using medications is aimed at:
Elimination of pain and normalization of body temperature. The best option is to prescribe drugs such as Paracetamol, Efferalgan, Diclofenac sodium, Propafol, Aspizol, Dantrolene, and intravenous drip of Magnesium sulfate.
Decreased blood pressure levels. This allows you to reduce the intensity and then stop the bleeding. First of all, the administration of Labetalol, Nicardipine, Esmolol, Hydralazine is used. Subsequently, the patient is transferred to tableted antihypertensive drugs - Captopril, Enalapril, Capoten.
If the pressure remains at a high level, the prescription of diuretics (Chlorothiazide, Andapamide, Lasix) and calcium antagonists (Nimotop, Nifedipine) is considered justified. Note! In the first days of illness, it is forbidden to sharply reduce blood pressure. In case of a sharp drop in blood pressure, intravenous drip administration of vasopressors is used - Norepinephrine, Mezatone, Dopamine.
Reducing cerebral edema. For this purpose, Dexamethasone is administered for three days. As the edematous process progresses, Manit, Albumin, and Refortan are added.
Correction of neurological symptoms. They use sedatives - Diazepam and muscle relaxants - Vecuronium).
Fighting bedsores. For this purpose, the skin is treated with camphor alcohol and talc.
Symptomatic treatment is also carried out. When fighting convulsions, Lorazepam, Thiopental or anesthesia is administered for 1-2 hours, vomiting is eliminated with Metoclopramide or Torekan, and through the use of Haloperidol, it is possible to eliminate manifestations of psychomotor agitation. If a secondary infection occurs, a course of antibacterial therapy is prescribed.
If large hematomas are detected, surgical intervention is considered justified. Intracerebral hemorrhage can be removed if it is localized in an accessible part of the brain, and also provided that the patient is not in a coma.
Surgical intervention
Surgical treatment is carried out in the neurosurgical department, the indications for its implementation are:
- diagnosing large hemispheric hematomas;
- breakthrough of blood into the cerebral ventricles;
- aneurysm rupture.
By removing blood, it is possible to reduce intracranial pressure, which not only improves the general condition, but also saves the patient’s life. Three types of operations are carried out:
Trephination. A part of the skull bone above the site of hemorrhage is removed. Thanks to the formation of a channel, it is possible to remove the blood that has accumulated. Thanks to this operation, it is possible not only to remove hemorrhage, but also to reduce pressure in the cranial cavity. It is considered justified to carry out such surgical intervention when diagnosing superficial hemorrhages in the hemispheres.
Puncture. The skull is pierced with a needle, the process is controlled by special equipment. Through it, blood is suctioned from the area of the hemorrhage. Surgery is considered most effective for hemorrhages that are localized in the deep parts of the brain.
Symptoms
Symptoms accompanying cerebral hemorrhage in adults indicate the development of neurological deficits. General cerebral symptoms (nausea accompanied by vomiting, psychomotor agitation, epileptic seizures) prevail in comparison with focal manifestations. Often a coma develops in a short period of time.
Focal manifestations are due to influencing factors and reasons:
- Localization of the outbreak.
- Functional disorders of the area of the brain subjected to compression by the hematoma.
- Increased intracranial pressure, impaired cerebrospinal fluid circulation (cerebrospinal fluid circulation), development of hydrocephalic syndrome.
- Dislocation (displacement) of brain structures under the influence of a hematoma.
- Brain swelling.
- Blood enters the ventricular system and the subarachnoid space (the cavity between the meninges - soft, arachnoid).
Extensive hemorrhage in the area where the basal ganglia is located usually occurs during the daytime and is more often detected in patients with a history of arterial hypertension. Hemorrhagic stroke often occurs against the background of psycho-emotional or physical stress.
Symptoms progress rapidly, reaching peak, pronounced manifestations in a few seconds. The patient usually falls and develops into a coma a few seconds later. Signs of hemorrhage in the area of the basal ganglia in the head in an adult include partial or complete paralysis of the muscles in the half of the body opposite to the location of the hemorrhage. Other manifestations:
- Pathological reflexes in the feet. Signs that appear against the background of damage to the pyramidal tracts. Babinski's symptom - line irritation of the plantar zone leads to involuntary extension of the big toe, sometimes accompanied by fanning of the remaining fingers. Rossolimo's symptom - short taps on the 2, 3, 4, 5 fingers lead to their reflex bending.
- Deviation of gaze towards the side of the lesion.
- Respiratory dysfunction.
- General cerebral symptoms – bradycardia (decrease in the number of heartbeats), flushing (flush of blood) of the face, vomiting.
An increase in the volume of the hematoma provokes the formation of edema around the affected area. At the same time, intracranial pressure increases, signs of herniation (protrusion of a section of the brain matter) are observed - complete paralysis, disruption of vital (vital) functions - respiratory, heart activity.
If an extensive, volumetric focus of hemorrhage breaks into the ventricular system in the direction of the lateral ventricles, the patient's condition worsens. Against the background of disturbances, the coma deepens and the tendon and foot reflexes are suppressed. The formation of foci of hemorrhage in the area of the visual thalamus usually leads to blood entering the zone of the 3rd ventricle.
Small foci of this localization are manifested by hemianopsia (bilateral loss of half the visual field), hemiparesis (muscle paresis in one half of the body), hemianesthesia (sensitivity disorder). Hyperkinesis (pathological involuntary movement caused by a reflex contraction of a muscle group) is often observed in half of the body lesion.
Brainstem stroke - features and consequences of a brain stroke
Brainstem stroke is a special case of cerebral stroke . With this pathology, problems with the blood supply to cells affect one of the most important parts of the brain - the brain stem. This structure is responsible for vital functions. And disruption of blood flow leads to their insufficiency.
A brainstem stroke is accompanied by the death of neurons in the main part of the brain—the brainstem. Tissue death occurs as a result of acute disruption of cerebral blood supply.
This type of stroke differs from others in that it poses an immediate threat to the life of the victim.
The blockage in the brain stem impairs vasomotor and respiratory function, disabling the person. In the absence of timely assistance, death is often recorded. The recovery prognosis does not exceed 3%.
Brainstem stroke - what is it?
Chemical reactions constantly occur in the brain; even with a slight decrease in blood flow, the organ begins to experience oxygen deficiency. In a healthy person, 50 ml of blood flows through 100 grams of brain matter; in a cerebral accident, 10 ml. This leads to the loss of some functions.
Interesting fact! A nerve cell can exist without oxygen for no more than 7 minutes, then it dies.
The brainstem is the main part of the brain located at the deep base of the skull. This zone contains the midbrain and medulla oblongata, nerve ducts, cranial nerve nuclei, and pons.
The medulla oblongata regulates the process of breathing, blinking, sneezing, coughing, and swallowing. Damage to this area causes cardiac arrest and blockage of breathing.
The pons is responsible for the perception of auditory information; at this point the bridge connects to the cerebellum and spinal cord. If the functioning of the bridge is impaired, deafness and facial paralysis develop. The midbrain regulates unconscious motor acts and movements of body parts. Dysfunction of this area leads to problems with movement.
The trunk is localized in a hard-to-reach place under the cerebral hemispheres.
Attention. If the area swells, it quickly moves and is compressed, which is fatal for the victim. This part of the brain is adjacent to the spinal cord and is associated with the activities of the central nervous system and internal organs.
The brain stem controls:
- heart muscle;
- respiratory tract organs;
- auditory and visual organs;
- body temperature;
- muscle tone;
- motor ability;
- vegetative functions;
- chewing and swallowing functions;
- organs of the reproductive system.
The brainstem region receives information from the sensory organs, then the data passes to the cerebral cortex, from which signals proceed to the spinal cord.
Brainstem stroke develops due to the inability of blood vessels to deliver oxygen and nutrients to the brainstem. Tissues begin to die, their functionality is lost.
Classification and causes of attack
Since brain stem stroke develops identically to blockades of other localizations, they have common causes. The causes depend on the mechanism of damage to the arteries and neurons. Based on this, hemorrhagic and ischemic brainstem stroke are distinguished.
The first occurs due to a rupture of the artery supplying the brain, which leads to hemorrhage. Its cause is hypertension or congenital pathology of blood vessels, expressed in their thinning.
Causes of ischemic type
Ischemic stroke of the brain stem is accompanied by blockage of the arteries, due to vascular obstruction or the formation of a blood clot or atherosclerotic plaque. Among the risk factors for this form of pathology are arterial hypertension, diabetes mellitus, increased concentration of cholesterol in the blood, atherosclerosis, and diseases of the cardiovascular system.
Note! Increase in blood pressure to 140-90 mm. Hg Art. increases the possibility of cerebrovascular accident.
The causes of ischemic stroke of the brain stem are differentiated into the following groups.
- Atherothrombotic. Ischemic phenomena occur as a result of a gradually enlarging blood clot inside the vascular canal. This condition is preceded by a sharp change in mood, absent-mindedness, aggressiveness, and memory impairment. This type occurs more often in the morning.
- Embolic. Occurs suddenly, the victim feels sharp pain from lightning-fast blockage of a vessel with an embolus. Such a stroke usually develops against the background of cardiac pathologies. More often detected during the day after physical or emotional stress.
- Hemodynamic. It develops with low blood pressure, when the brain does not receive the required amount of nutrients.
- Lacunarnaya. Accompanied by damage to the smallest capillaries, which are localized in the deep layers of the brain. It often happens during the day due to increased blood pressure.
- Hemorheological. Develops as a result of increased blood viscosity. Rarely diagnosed.
For reference. After blockage of the vascular canal, ischemic phenomena occur, nerve cells die, losing their functions. Brain swelling develops.
What causes hemorrhagic form
Brainstem hemorrhagic stroke is diagnosed when a vascular canal ruptures, leading to cerebral hemorrhage. Based on the location of hemorrhage, the type is differentiated into parenchymal, subarachnoid, and epidural.
Diagnostic methods
To confirm the presence of pathology, pay attention to such symptoms of hemorrhage as acute, intense pain in the head, bouts of vomiting, depression of consciousness, and focal neurological deficits. Less common signs of cerebral hemorrhage are observed: seizures, meningeal syndrome.
A physical examination allows for an accurate diagnosis. The doctor pays attention to the presence of provoking diseases in the anamnesis - arterial hypertension, atherosclerotic lesions of cerebral vessels, pathologies of the hemostatic system, diabetes mellitus. During the examination of the patient, characteristic signs are revealed:
- Crimson-red, bright coloring of the skin of the face.
- Increased sweating in the facial area.
- Noisy, stridorous (hoarse, accompanied by hissing, whistling) breathing.
- Decrease in heart rate and, accordingly, pulse.
- Increased blood pressure values.
- Hyperthermia (overheating of the body).
To determine the fact of hemorrhage in the brain, research methods such as MRI, CT, and angiography of cerebral vessels are used. During the instrumental examination, the presence of a focus of hemorrhage and its exact location, the degree of damage to surrounding brain tissue, and the presence of edema of the brain matter are determined.
Computed tomography is the main research method for the formation of an intracranial focus of hemorrhage of non-traumatic origin. A blood clot in the images is manifested by the formation of increased density with the presence of a hypodense (low density) strip around it, which represents the liquid fraction of blood.
During angiography of cerebral vessels, malformations, aneurysms and other abnormal elements of the circulatory system present in the brain are revealed. Differential diagnosis is carried out in relation to a tumor, ischemic damage to brain tissue. If a cerebral hemorrhage occurs after a blow to the head, MRI and CT scans reveal signs of traumatic damage to the brain.
Diagnostics
To confirm the diagnosis, the doctor uses different methods - emergency ones and a number of less frequently used ones. Key studies include:
- questioning if the patient is conscious;
- checking nervous reflexes - vision, sensitivity of the limbs;
- measuring pulse, pressure, ECG;
- lumbar puncture to detect blood penetration into the cerebrospinal fluid;
- magnetic resonance imaging of the brain (MRI) to detect hematoma, tumor and displacement of the brain lobes;
- angiography is a study of the vascular network that helps detect arterial aneurysms and malformations.
First aid
Correctly provided first aid often means increasing the chances of a favorable outcome. If a person falls and shows signs of a stroke, the following steps must be taken:
- Place it on a flat surface, turn it on its side, placing a small pillow under its head.
- Loosen constricting, squeezing items of clothing (tie, belt, shirt collar).
- Provide access to fresh air (open a window).
The patient's condition should be assessed. If there are no signs of breathing or heartbeat, perform artificial heart massage and simultaneously ventilate the lungs. It is necessary to call emergency doctors or arrange for the patient to be transported to the hospital.
Brain stem stroke: causes, symptoms, treatment
A brain stem stroke is an acute disorder of cerebral circulation, characterized by a sharp deterioration in the patient’s well-being. Accompanied by disruption of vital functions. Failure to promptly seek medical help can lead to the development of complications, such as disability or even death.
Brain stem stroke
Brainstem stroke is characterized by the appearance of a pathological focus in the brainstem. In this regard, it has the most unfavorable prognosis for recovery, since vital centers are concentrated in this place, which leads to dysfunction of the brain. It can be hemorrhagic, ischemic and mixed, therefore it occurs not only in older people, but also at a young age.
As a result of brain damage, the patient will have to undergo long-term treatment and a long rehabilitation process, including physical exercise and massage.
Mechanism of occurrence
There are 2 types of brainstem stroke:
- Ischemic. It is characterized by a circulatory disorder that develops as a result of blockage of a blood vessel by a detached atherosclerotic plaque. In this case, stem cells die due to a lack of oxygen and nutrients, disruption of metabolic processes, as well as the adverse effects of decay products of dead neurons.
- Hemorrhagic. Caused by the rupture of small or large blood vessels, which leads to the occurrence of a hemorrhage.
Symptoms
Clinical manifestations of stroke are characterized by great diversity.
In the ischemic form of the disease, symptoms appear gradually, over several hours or even days. The main signs are blurred vision, impaired coordination of movements, numbness of the face and other parts of the body, tingling, the appearance of paresis and even paralysis. The skin becomes pale, breathing and heart rate increase, and arrhythmia (interruptions in heart function) and hypertension may develop.
Hemorrhagic stroke occurs suddenly. Dizziness appears, speech is impaired, and body temperature rises. The man loses consciousness. There are signs of damage to the centers of human vital activity: breathing, heartbeat, sensory organs, etc. If emergency medical care is not provided in a timely manner, a coma may occur.
Diagnostics
The diagnosis of stroke can be made by examining the patient and performing neurological tests. However, in order to confirm the diagnosis, establish the location of the pathological focus and the degree of tissue damage, it is necessary to conduct additional diagnostics.
Main research methods:
- Computer or magnetic resonance imaging. Makes it possible to determine the degree of tissue damage. This is the very first diagnostic method that needs to be done as quickly as possible after a person’s health deteriorates.
- Angiography using contrast agents. Necessary for identifying disorders in the functioning of the blood vessels of the brain: atherosclerosis, thrombosis.
- Cardiography. Allows you to diagnose heart rhythm disturbances, which indicate changes in blood flow in the vessels.
Treatment
Treatment of brainstem stroke should begin immediately; the earlier appropriate therapy is carried out, the greater the chance of preventing irreversible changes from occurring. A full-fledged rehabilitation plays an important role, which will avoid the development of complications and speed up the patient’s recovery.
Treatment methods
Stroke therapy should be comprehensive, aimed at eliminating the cause that provoked the development of the pathology, as well as supporting the functioning of the respiratory and cardiovascular systems, and relieving swelling of brain tissue. In case of ischemic stroke, it is necessary to remove the source of hemorrhage. In this case, the patient’s condition and the characteristics of the course of the disease are taken into account.
In case of breathing problems, oxygen oil is applied to the patient, and if there is no positive result from its use, the trachea is intubated for artificial ventilation.
In case of hemorrhagic stroke , accompanied by hemorrhage, it is necessary to use hemostatic drugs. If the pathological focus is large, surgical intervention may be indicated.
In the ischemic form of the disease, thrombolytics (Actilyse) or anticoagulants (Heparin) must be used to dissolve the blood clot that provoked the development of ischemia of brain structures.
- Normalization of blood pressure. When indicators increase, drugs are used to reduce it - Magnesium sulfate, Metoprolol and other drugs intravenously or intramuscularly. If blood pressure drops, it is recommended to use Dexamethasone, Atropine, Dopamine, etc.
- Relieving swelling. It is carried out with the help of diuretics - Furosemide, Mannitol.
- To support nerve cells and improve their nutrition, it is recommended to use vascular drugs - nootropics. These include: Thiocetam, Piracetam, Cavinton, Cortexin, etc.
- Symptomatic therapy. In cases of severe pain, it is advisable to use analgesics and nonspecific anti-inflammatory drugs. If the patient's condition has worsened due to the addition of secondary microflora, it is necessary to use broad-spectrum antibiotics.
If bulbar syndrome occurs, when swallowing functions are impaired, tube feeding is indicated.
Prognosis for the disease
About 70-80% of patients who have suffered a stroke die within the first 3 days. The percentage of disability is extremely high and amounts to about 50-60%. Complete recovery is possible only in 2-3% of all cases. For others, dysfunction persists throughout their lives.
Signs of a poor prognosis:
- "closed person" syndrome - absence of all motor functions, only eye movements are preserved;
- disorders of the respiratory and cardiovascular systems;
- neurological changes within 1 year after the disease.
Consequences
As a result of a brainstem stroke, irreversible consequences often develop. In this case, speech, swallowing, and coordination in space are impaired. Paresis and paralysis develop. In some cases, it is impossible to independently maintain hemodynamics, thermoregulation and other vital functions.
Speech Impairment
Poor blood circulation in the brain stem leads to deterioration of speech. A similar problem persists in 30% of patients who have had an attack. The main manifestations are that speech becomes unclear, unclear, and confused. Correction is possible with the help of a speech therapist, it depends on the degree of damage to the center.
Swallowing disorder
Swallowing impairment is the main sign of stroke localization in the brainstem. Occurs in more than 60% of all cases. Full restoration of function is almost impossible. The patient needs to be fed through a tube for a long time, but even if the condition normalizes, the person will be able to eat only soft, semi-liquid and ground food.
Impaired motor function of the limbs
When the trunk is damaged, many important functions of the body are disrupted, including motor functions. A person cannot control the work of muscles; movements of the arms and legs become spontaneous.
In the first few months after a stroke, movement may be restored, but if rehabilitation is not started in a timely manner, the likelihood of a positive outcome will become much less. If the problem cannot be resolved within a year, it will be almost impossible in the future.
Loss of coordination
The degree of impairment of motor coordination depends on the severity of the damage to brain tissue. Dizziness and other symptoms persist for several months, but quickly resolve with the use of vascular medications.
Breathing problems
When the respiratory center is damaged, breathing problems develop. It manifests itself in the form of slower breathing when awake, as well as the occurrence of episodes of apnea - short-term cessation of breathing during sleep. In some cases, a person is unable to breathe on his own and must be kept on a ventilator. However, the prognosis is extremely unfavorable.
Hemodynamic instability
With a brainstem stroke, the functioning of the cardiovascular system is disrupted. The main manifestation is hemodynamic instability, which occurs in the form of surges in blood pressure and increased heart rate.
Visual impairment
If the eye movement control center is affected, spontaneous twitching of one or both organs of vision occurs. The patient is unable to concentrate on an object, and strabismus gradually develops.
Unstable thermoregulation
Violation of thermoregulation processes indicates a critical condition of the patient. The main manifestations of this condition are a sharp increase in body temperature to febrile levels in the first few days after a stroke.
A sharp decrease in body temperature is accompanied by the death of brain cells and is an important sign of an unfavorable prognosis for the patient.
Methods of treatment and rehabilitation
The patient is placed in a ward where intensive care is performed. The main drugs used for treatment: Ketoprofen (non-steroidal anti-inflammatory drug), Mannitol (diuretic), Urapidil (adrenergic blocker). If there are indications (the level of depression of consciousness is less than 8 points in accordance with the criteria of the Glasgow scale, tachypnea - rapid shallow breathing, bradypnea - rare breathing), the patient is connected to a ventilator (artificial ventilation).
If blood coagulation processes are disrupted, drugs are prescribed to replace the clotting factor. Correction of conditions is carried out - hypoglycemia (low glucose level), hyperglycemia (high glucose level), hyperthermia. If necessary, anticonvulsant therapy is carried out.
Surgery for cerebral hemorrhage is performed to reduce the amount of bleeding, prevent damage to the parenchyma and restore brain function. Surgical removal of the hematoma prevents the development of mass effect (pressure on surrounding tissues) and reduces the impact of toxic substances formed during the decomposition of the spilled blood.
Operations are of the following types: transcortical (through the cortex) removal, external drainage (removal of liquid contents) of the hematoma and ventricles, puncture or stereotactic aspiration (suction of liquid contents). Rehabilitation after an episode of cerebral hemorrhage involves the following measures:
- Bed rest for 3 weeks.
- Preventing emotional and physical stress.
- Control of life-supporting functions (breathing, cardiac activity).
- Monitoring and correction of oxygen levels in the blood (prevention of hypoxia).
Rehabilitation measures include preventing the development of bedsores, performing therapeutic exercises (passive, active) and breathing exercises, prescribing massage against the formation of bedsores. In the later stages of rehabilitation, physiotherapy, occupational therapy (work therapy), restoration of cognitive functions and speech are included.
How to recover from a brain hemorrhage
Recovering from a stroke requires a lot of time and effort. The rehabilitation program must be developed for each patient individually. It includes:
- Therapeutic exercise. Exercising helps reduce the likelihood of recurrent hemorrhage. The patient may be prescribed breathing exercises, yoga, and Pilates.
- Diet. It is necessary to exclude smoked meats, sweets, fatty meats, and, in case of diabetes, some vegetables and fruits from the diet. The optimal option in this case is table No. 10.
- Speech technique. In case of speech disorders, the patient requires sessions with a speech therapist to restore normal function of the speech apparatus.
- Psychotherapeutic technique. It involves overcoming a depressive state associated with the fact that the patient cannot lead his usual life.
Possible complications and prognosis
Depending on the causes of the brain hemorrhage and the severity of the symptoms, the consequences may vary. The prognosis for life with a cerebral hemorrhage is relatively unfavorable, depending on the location and size of the hemorrhage focus and the degree of its influence on the surrounding brain structures. Statistics show that with large-scale, voluminous hemorrhages in the brain, the chances of survival are low. The mortality rate within 30 days after the onset of hemorrhage is 35-80% of cases.
In 50% of cases, death occurs within the first 2 days. About 65% of patients who survive a hemorrhagic (associated with cerebral hemorrhage) stroke die within a year due to complications - secondary hemorrhages in the trunk area, status epilepticus, pneumonia, pulmonary edema, sepsis, thromboembolism of the pulmonary arteries. The consequences of extensive hemorrhage in the brain are expressed in the development of a stable neurological deficit that is not amenable to drug correction in surviving patients.
What are the manifestations?
Symptoms of cerebral hemorrhage depend on the location of the vascular accident. Against the background of general manifestations, signs characteristic of a specific affected area develop. Based on them, we can guess which part of the brain is affected.
The main manifestations can be divided into groups:
- General cerebral symptoms. The reasons for its occurrence are cerebral edema and increased pressure in the cranial cavity. The occurrence of the latter is possible due to a violation of the outflow of cerebrospinal fluid (a consequence of hemorrhage into the ventricles), improper functioning of the blood-brain barrier with high blood pressure, and head trauma. Brain edema also occurs when its structures are compressed by an increasing hematoma or due to dislocation.
- Meningeal symptoms (stiff neck, Kernig's sign). This clinic develops if bleeding in the cranial cavity occurs in the space between the meninges.
Meningeal syndrome is a set of symptoms caused by irritation of the meninges
- Focal symptoms. Directly related to the localization of the vascular accident. Damage to the nerve centers responsible for controlling certain functions manifests itself in different ways: paralysis, numbness, visual and speech impairment.
Extensive intracerebral hemorrhage is usually accompanied by the development of edema, displacement of brain structures, and their compression, which is usually manifested by general symptoms (vomiting, headache, convulsions, coma), as well as signs of irritation of the meninges. Focal symptoms begin to come to the fore after the swelling begins to subside, or when certain nerve centers are involved in the process and their functions are impaired.
Signs indicating increased intracranial pressure
These include a group of general cerebral symptoms, which in one way or another accompanies any pathological processes in the cranial cavity, be it bleeding, inflammation, injury or exposure to toxic substances. The reasons for increased intracranial pressure are as follows:
- inflammation, one of the characteristic manifestations of which is swelling;
- impaired circulation of cerebrospinal fluid (hemorrhage into the ventricles with the development of hemotamponade of the latter) or circulatory disorders (hypervolemia);
- change in the normal arrangement of brain structures (trauma; compression by a hematoma, resulting in swelling).
Epidural hematoma manifests itself as hypertensive-dislocation syndrome
The cranial cavity is limited in volume, therefore the appearance of additional formations (tumor, and in the context of this topic - hematoma), an increase in brain structures in size due to edema is accompanied by an increase in intracranial pressure. The signs of this condition are as follows:
- Expanding headache.
- Nausea and vomiting.
- Convulsive syndrome.
- Visual impairment due to swelling of the optic discs.
- Depression of consciousness (stupor, stupor, coma).
Brain swelling leads to compression of its structures in the natural canals of the skull. Thus, the brainstem is pinched in the foramen magnum, which is accompanied by disruption of the functioning of the vital centers of the medulla oblongata and can cause death. With dislocation and compression of brain structures, focal symptoms are added to the general symptoms, since certain nerve centers are affected. Over time, these manifestations begin to predominate, and when the swelling decreases, they come to the fore.
Signs of intracranial hemorrhage are caused by increased intracranial pressure, irritation of the membranes, as well as damage to specific nerve centers.
Features of the clinical picture of hemorrhage with damage to certain brain structures
The hemispheres of the brain have different specializations
When the left hemisphere suffers, movement and sensitivity disorders on the right, speech disorders, and memory problems become frequent manifestations. The right hemisphere is responsible for the perception of non-verbal information, imaginative thinking, and the ability to perform several tasks simultaneously. When hemorrhaging in this area, in addition to paralysis and sensitivity disorders, mental disorders (aggression, anxiety, depression) occur.
Bleeding into the ventricles is dangerous due to the possibility of hemotamponade (blockage) and disruption of the outflow of cerebrospinal fluid. This situation leads to increased intracranial pressure and serious consequences (compression of vital centers, coma, death). No less serious disorders occur when the brain stem is damaged, since this is where the respiratory and vasomotor centers are located. Cerebral hemorrhage with damage to the cerebellum is accompanied by impaired coordination of movements, the occipital lobe - visual disturbances, and the frontal lobe - convulsive syndrome.
Prevention
Your doctor will help you find out how to prevent the development of pathology. It is recommended to give up smoking, alcohol and drug abuse. Another preventive measure is monitoring blood pressure values (taking antihypertensive drugs). To avoid the occurrence of recurrent foci of hemorrhage, antihypertensive therapy is carried out in patients who have had a stroke, regardless of the presence of a history of arterial hypertension.
A cerebral hemorrhage is a life-threatening condition that requires immediate medical attention.
Classification of cerebral hemorrhages by location
The World Health Organization (WHO) currently identifies 5 types of cerebral hemorrhages:
- Intracerebral, or intracerebral hemorrhage, when burst vessels are located in the deep layers of white or gray matter, and blood pours into the thickness of the brain.
- Subarachnoid, in which ruptured vessels are affected by an aneurysm or amyloidosis, and blood enters the cavity, which is filled with cerebrospinal fluid.
- Ventricular or ventricular hemorrhage affecting the lateral ventricle of the brain.
- Epidural, in which the spilled blood enters the space between the skull and the brain.
- Subdural, in which blood spreads under the dura mater of the brain.
Tomography and other diagnostic methods can help specialists find out which part of the organ has undergone changes due to such a phenomenon as cerebral hemorrhage, the symptoms of each type of which have their own characteristics.
Is it possible to prevent hemorrhage?
There is no method that 100% guarantees the prevention of pathology, but the proposed medical recommendations will significantly reduce the risk of cerebral hemorrhage:
- Annual medical examinations. The indicator of cholesterol and blood clotting is important.
- Pressure control. Frequent hypertensive crises are the main provoking factor.
- Rejection of bad habits.
- Smart nutrition. The menu should reduce the content of animal fats, giving preference to plant foods.
- Control your weight. Obesity interferes with proper blood flow.
- Exercise in moderation. Increased physical activity is no less harmful than physical inactivity. To maintain physical activity, walking, cycling, swimming or exercise therapy are suitable.
Brain hemorrhages are dangerous and, according to medical statistics, almost always result in disability or death of the patient. Timely delivery of the patient to the doctor will help reduce the severe consequences of hemorrhage.
Violation of the integrity of the vessels of the head provokes hemorrhage in the brain. In adults, cerebral hemorrhages occupy a significant part of the pathologies of the development of the vascular system, because The lion's share is taken by hemorrhagic strokes (in older and elderly people) and injuries of various origins with hemorrhages (in young and middle-aged people). Other causes give a small percentage of hemorrhages, but they will be listed below. An interesting fact is that scientists from the Kazan Medical University have calculated that with each decade of life the risk of non-traumatic hemorrhages in people increases by 2 times, and after eighty years this figure is amazing - 25 times compared to the previous one. This indicates significant “wear and tear” of the brain vessels and an increase in associated risks (falls, infection, etc.).
What to do with the patient
If there are at least 2-3 manifestations of pathology, you must ask the person to raise their hands, smile and say a simple sentence. Stroke victims are characterized by difficulties with speech, immobility of the facial muscles on the affected side (crooked smile), and differences in the pace and height of raising the arms.
Important information: What are the prognosis for recovery after ischemic stroke of the brain stem?
If these disorders are present, it is necessary to provide the patient with first aid as quickly as possible:
- Call an ambulance, briefly describing the victim's condition.
- Lay the patient down, freeing him from tight clothing and raising the upper part of his body by 30°.
- If you lose consciousness and stop breathing, perform cardiopulmonary resuscitation until the medical team arrives.
Treatment methods for stroke are divided into conservative (medicinal) and surgical. Conservative therapy is used for the following indications:
- small size intracerebral hematoma;
- hemorrhagic impregnation of the affected parenchyma;
- rehabilitation after surgical treatment.
Drug treatment consists of the following stages:
- Relieving cerebral edema. To reduce intracranial pressure, hormonal anti-inflammatory drugs (Prednisolone) and fast-acting diuretics (Furosemide) are used.
- Prevention of parenchymal bleeding. To prevent hemorrhages, hemostatic agents (Troxerutin, Dicynon) are used. When treating with hemostatic agents, monitoring of blood clotting is necessary: with an increased risk of thrombosis, the development of ischemic stroke is possible.
- Stabilization of blood pressure. Relieving a hypertensive crisis and maintaining normal blood pressure reduces the risk of hemorrhage complications. Antihypertensive medications are selected individually.
- Reducing stress. Emotional stress and extraneous irritants can aggravate circulatory disorders, so patients are advised to stay in the intensive care unit or intensive care unit, complete rest and take tranquilizers (Phenazepam).
- Stimulation of cerebral circulation. To improve blood supply to the tissues of the central nervous system, Piracetam, Cerebrolysin, Mildronate, etc. are used.
In case of coma and impaired respiratory function, the patient is intubated and transferred to artificial ventilation.
Surgical treatment of hemorrhagic stroke is indicated for patients with large blood collections (more than 30 ml). It is carried out to remove the hematoma and drain the ventricles (in case of ventricular damage). This allows you to reduce compression of brain tissue and the area of necrosis. Surgery is also necessary for patients with vascular abnormalities and brain tumors.
Clinic: symptoms and signs
It is necessary to call an ambulance for subarachnoid hemorrhage if, against the background of normal health, a person has:
- headache that gets worse with any activity;
- nausea and vomiting;
- the appearance of psycho-emotional disorders: fear, drowsiness, increased excitability;
- convulsions;
- disturbance of consciousness: stupor, fainting or coma appears;
- the temperature increased to febrile and subfebrile values;
- photophobia.
Symptoms persist for several days.
Separately, there are signs that arise when the functioning of the cortex and nerves of the brain is disrupted . This is evidenced by:
- loss of skin sensitivity;
- speech problems;
- the appearance of strabismus.
A few hours after the effusion of blood, symptoms of meningitis appear:
- Kernig's sign (a person is unable to straighten a leg that is bent at the same time at the knee and hip joints);
- stiffness of the neck muscles (the patient does not reach his chin to his neck).
Traumatic subarachnoid hemorrhage due to traumatic brain injury requires monitoring for signs of damage to different brain regions.
Problems with the frontal lobe will be indicated by:
- speech disorder;
- cramps in the fingers;
- unsteady gait;
- speech disorders;
- behavior changes.
When the temporal lobe , hearing is lost, memory impairment, auditory hallucinations and tinnitus appear.
Impaired reading ability, loss of tactile sensations, and ability to navigate indicate problems in the parietal lobe .
Damage to the occipital lobe results in visual impairment and visual hallucinations.
With a relapse, existing symptoms intensify and new ones appear. For some, blood pressure rises, arrhythmia begins, pulmonary edema occurs and the heart stops.
Periods
Hemorrhagic stroke is characterized by the following stages:
- Acute - general symptoms predominate, associated with increased pressure in the cranial cavity due to the effusion of blood. Lasts up to 1 week, characterized by accumulation of blood with damage and necrosis of nerve cells. The most dangerous phenomenon in this period is cerebral edema with dislocation of its structures, which can cause death.
- Restorative – starts from the second week. At this time, reparative processes take place in the brain: blood is removed and the structure of the parenchyma is restored by multiplying neuronal cells. Duration: from 2 weeks to several months.
- The stage of residual effects lasts until the end of life. With competent and timely treatment and proper rehabilitation, it is sometimes possible to restore many functions of the body and body, and even restore the patient’s capacity.
Classification of hematomas
Often, hematomas on the head appear after damage to soft tissues as a result of bruises, blows, or pinching of the head during difficult childbirth. Therapy is selected taking into account the severity of the injury, location and size of the formation. A subcutaneous hematoma on the head (bruise) was noticeable already during the external examination. The damaged area will rise above the others.
Depending on the size of the hematoma in the head after the blow, it is divided into types:
- Small - contain up to 50 ml of liquid.
- Medium – filling the cavity by 50-100 ml.
- Large – blood loss is more than 100 ml.
Subdural hematoma
Depending on the location, there are several types of brain hematomas.
Subdural hematoma of the brain
Subdural - the main feature of such an injury is the rupture of blood vessels, mainly veins. It is located between the arachnoid and dura mater of the brain.
Blood leaking into the tissue forms a hematoma, which puts pressure on the brain. With its progressive increase, the patient’s consciousness fades, and this can lead to irreversible consequences.
Causes of hemorrhages in the ventricles of the brain
The reasons for the formation of hemorrhage in the ventricles of the brain are not fully understood and there are no specific clear reasons for this pathology.
Risk factors include the following:
- Arterial hypertension (in primary hemorrhages) is a chronic increase in blood pressure, especially dangerous in the absence of at least basic treatment.
- Uncontrolled use of antiplatelet agents, fibrinolytics.
- Vascular aneurysms are enlargements of an artery and can be congenital or acquired.
- Diabetes mellitus (with this disease the level of glucose in the blood constantly increases, which causes all kinds of complications).
- Mechanical damage to cerebral vessels (trauma).
- Hemorrhagic diathesis is increased fragility of the walls of blood vessels.
- Oncological diseases - benign and malignant tumors.
- Infectious and inflammatory processes in brain tissue (encephalitis).
There are many reasons that contribute to hemorrhage in the ventricles of the brain. They primarily affect nervous tissue. Primary factors provoke multiple complications, which leads to hemorrhages of this kind. One of the first such complications is an increase in the permeability of the walls of the vessels of the ventricular system.
Symptoms of hemorrhage in the ventricles of the brain
One of the very first symptoms is the rapid development of a coma. If the rush of blood into the ventricles occurs quickly, then a rapid loss of consciousness is observed. If the ventricular system is filled with blood gradually, then consciousness is not lost immediately, but after some time.
As the volume of blood in the ventricles increases and swelling occurs, the loss of consciousness becomes deeper, respiratory distress, changes in pulse, vasomotor disorders in the face, limbs and in the torso itself, and cyanosis are observed. Damage to the brain causes hemipreparalysis of gaze in the opposite direction. Jumps in body temperature may be observed - initially the temperature drops below normal, but during the day it may rise significantly (up to 40), and if blood enters the third ventricle, the temperature can reach critical levels - 42 degrees.
Laboratory tests show an increase in leukocytes in the blood, sometimes protein and sugar are present.
Early contracture can also be considered a sign of hemorrhage in the ventricles of the brain. Periodic tonic spasms are observed, occurring spontaneously or during respiratory movements. Tonic spasm is a condition during which the head is thrown back, the legs are convulsively extended, and the arms are bent and clenched in the fingers.
If hemorrhage occurs in the lateral ventricles, then the following clinical picture is observed:
- the comatose state develops rapidly;
- vomit;
- the frequency and rhythm of breathing is disrupted;
- change in heart rate - first it slows down and then increases;
- facial hyperemia;
- profuse sweating;
- severe increase in body temperature;
- pendulum-like movements of the eyeballs when the body is in a horizontal position;
- tonic convulsions during breathing;
- increased tendon reflexes and at the same time decreased skin reflexes.
Hemorrhages into the ventricle most often lead to rapid death, since the spilled blood affects vital centers.
Treatment methods
If hemorrhage is suspected, it is very important to provide the patient with first aid. To do this, first of all they call an ambulance. In this case, it is strictly forbidden to disturb a person, even if he is in his original position, but does not move either independently or with outside help.
Attention! It is very important to provide timely assistance, and then begin effective treatment, only then can you count on favorable prognoses.
What to do if an attack begins?
According to statistics, it was determined that hemorrhage occurs most often during the daytime. Therefore, if a person exhibits characteristic symptoms, emergency assistance may be required.
- A person begins to complain of a sudden unbearable headache.
- The limbs become noticeably numb.
- Cloudiness or loss of consciousness occurs.
These signs should alert others and become a good reason to urgently call an ambulance.
First aid for hemorrhagic stroke
Before the arrival of specialists, it is recommended to provide the following assistance:
- The person should be in such a position that he has free access of air and blood flow.
- In case of vomiting, turn the patient on his side so that the person does not choke on the vomit.
- Apply a cold compress to your head.
- Measure blood pressure.
- Do not disturb the patient and wait for the ambulance to arrive.
First aid nuances
It is worth paying attention that it is strictly forbidden to try to bring the patient to his senses, to move or disturb him. Special treatment for hemorrhage can only be provided by medical professionals.
Reference! The emergency doctor is obliged to carry out the following life-saving measures:
- Introduce a special drug that quickly eliminates cerebral edema.
- Stop bleeding.
- Bring blood pressure back to normal.
- Deliver to intensive care promptly.
Posture for first aid for stroke
Depending on the lesion, the patient may even be prescribed surgical treatment. In this case, the operation must be performed in the first three days after the hemorrhage. These surgical measures consist of several procedures that help get rid of accumulated blood in the aneurysm. Thus, intracranial pressure quickly decreases and the patient’s chance of recovery increases.
The subsequent stage of treatment involves the use of medications that are aimed at normalizing blood pressure and maintaining the patient’s condition in the postoperative period.
Diagnosis of the condition
If after an injury there are no external manifestations of a head hematoma, this does not mean that the vessels inside the skull were not damaged. In this case, the examination can be difficult. But experts mostly believe that unconsciousness after injury is caused by bleeding inside the skull, when there is no evidence to the contrary.
The best way to determine the location and size of the formation is visualization. It involves the following methods:
- CT scan. To obtain detailed images of brain slices, an X-ray machine is used that is connected to a computer;
- MRI. Allows you to identify the presence of a hematoma in various parts of the brain, determine its size and location.
CT and MRI are painless examination methods.
Possible prognosis after an attack
Almost half of the patients die a month after the hemorrhage. The prognosis for recovery in the following categories is bleak:
- Patients over 70 years of age.
- People with voluminous tumors (about 50 mm).
- Patients in a coma.
- Patients with hemiplegia, hyperglycemia.
- People with impaired structures of the “gray matter”.
- Patients diagnosed with ventricular hemorrhage.
Most often, a fatal attack occurs when the trunk is damaged. Some patients have persistent disorders of the central nervous system. But restorative complex therapy is sometimes effective. Relapses of the crisis are possible in 4 percent of cases (with a diagnosis of amyloid angiopathy and aneurysm above).
Intracerebral bleeding is very dangerous for humans; this disease is easier to prevent than to eliminate its consequences. A healthy lifestyle, eliminating bad habits, and nutritious nutrition is the first step on the path to success. If you have warning symptoms, you should immediately consult a doctor or call an emergency hospital.
Symptoms
Signs of cerebral hemorrhage include the following:
- confusion (the victim is unable to answer simple questions, remember information about himself, realize his location, etc.);
- Strong headache;
- uncoordinated movements, unsteadiness of gait;
- difficulty speaking;
- dilation of the pupil on the affected side;
- nausea, vomiting without relief;
- a sharp decrease in sensitivity (numbness) and mobility of the arms and legs on one side;
- pain in the eyes, photophobia, visual disturbances (spots, circles before the eyes, vision of surrounding objects in red);
- rapid and intermittent heartbeat;
- flushed face;
- dizziness;
- convulsions;
- involuntary urination and defecation;
- chills, sweating, fever (with damage to the autonomic nervous system against the background of ventricular or parenchymal-ventricular hemorrhage).
Symptoms of hemorrhagic stroke develop immediately after a hypertensive crisis, severe emotional stress or other stress. In 3 out of 4 patients, the pathology is diagnosed in the daytime. Often the first sign of an acute circulatory disorder is a severe headache, which quickly turns into loss of consciousness.
The nature of the manifestation of the pathology distinguishes intracerebral hemorrhage from ischemic stroke.
Hemorrhage is characterized by rapid development (within minutes or hours), vomiting without relief, rigidity (severe tension) of the neck muscles, migraine headache and prolonged loss of consciousness.
With ischemic damage, these signs are absent.
The loss of consciousness during a stroke occurs in several stages:
- stunning (symptoms of this stage are the victim’s poor response to surrounding people, lack of understanding of the situation and location);
- somnolence (the gaze is lost, directed into space, a state similar to sleep with open eyes);
- stupor (deep sleep, reflexes are preserved, pupillary reaction is weak, but touching the cornea provokes a reaction);
- coma (lack of response to any irritants, impaired respiratory and cardiac activity).
Diagnostics and first aid
The doctor assesses the patient's condition and prescribes a computed tomography scan. Using CT:
- the area where the bleeding occurred is identified;
- data on the liquor system is obtained;
- it is checked whether there is cerebral edema.
High-precision CT angiography allows you to find out where the source of bleeding is . Negative CT results are associated with insignificant amounts of hemorrhage. They also occur when diagnostics are carried out at a later date.
If negative results are obtained, a lumbar puncture and cerebrospinal fluid examination are prescribed. SAH is indicated by an increasing concentration of red blood cells.
If the disease occurs due to an aneurysm, then vascular angiography . A radiopaque contrast agent is injected into them and X-rays are taken. Endovascular surgery is performed on damaged areas.
First aid is aimed at stabilizing the patient's condition. He needs to be taken to the hospital when the first symptoms appear .
Treatment is carried out to stop the bleeding and eliminate its source. It is important to prevent the development of complications and relapses.