Author: A. Olesya Valerievna, candidate of medical sciences, practicing physician, teacher at a medical university
Cerebral edema (CE) is a pathological condition that is formed as a result of exposure to various factors damaging brain structures: traumatic injury, compression by a tumor, penetration of an infectious agent. The adverse effect quickly leads to excessive accumulation of fluid, increased intracranial pressure, which leads to the development of severe complications, which, in the absence of emergency therapeutic measures, can result in the most tragic consequences for the patient and his relatives.
What it is
Cerebral edema is rightfully considered one of the most dangerous complications of any intracranial disease. It was first described in the mid-19th century. With this disease, extensive impregnation of the tissues of the central organ of the nervous system with fluid from the vascular environment occurs. The cause and location of the problem does not matter, since the presence of edema in the head is spoken of only in cases where there are general symptoms indicating damage to the entire organ, and not to its individual parts.
Changes in the brain can threaten the patient’s life, so they are classified as the most severe complications.
The fundamental factor for the formation of edema is the presence of severe decompensated microcirculatory failures in the tissues of the organ, which begin to appear in areas with pathological foci. If the course of the primary disease is too severe, a violation of the mechanisms of autoregulation of the tone of the vascular walls may occur, which leads to their paretic expansion. Such lesions quickly spread throughout the brain, affecting healthy tissues of the organ, causing vasodilation in them and increasing hydrostatic pressure. When the walls of blood vessels are defective and there is increased pressure on them, naturally, the liquid components of the blood cannot always be retained inside the vascular bed and flow through the walls, soaking the brain matter.
In any other organs, tissue swelling does not cause dire consequences, but with the brain the situation is a little different, since it is limited by the volume of the skull, which means that the organ cannot grow to too large a size. If the brain swells, it is in a compressed state, provoking ischemia of nerve fibers and the progression of swelling. In addition, with this disease, the level of oxygen supplying the brain decreases, the concentration of CO2 increases, and the oncotic and osmotic pressure of the plasma decreases due to a decrease in protein and changes in the balance of blood electrolytes.
Due to the fact that each cell in the brain, when they swell, becomes oversaturated with fluid and increases in volume several times, the organ itself loses the ability to perform its functions, and the metabolism in it is also disrupted.
Brain edema, what is it and what are the consequences
Cerebral edema is not a primary disease. It is a pathological condition that develops as a result of pathological changes caused by other diseases. This is a kind of reaction of the body to negative influences.
The acid-base balance is disrupted, the total amount of fluid inside the skull increases, which leads to a pathological increase in intracranial pressure.
Consequences after treatment depend on the timing of its initiation, the correct approach and the severity of the primary injury. Full recovery is possible.
Various neurological disorders may appear: convulsions, epileptic seizures, paralysis of the limbs and other sensory disorders. Headaches, states of depression and depression, mental disorders can haunt a person for a long time due to the unfavorable outcome of the pathology.
What are the causes
The brain (hereinafter referred to as the brain) is an organ characterized by an increased blood supply, so it is very easy to provoke problems with microcirculation that turn into swelling. The larger the area of initial injury, the greater the risk that AGM may occur. Edema can be caused by various disorders and illnesses:
- ischemic stroke. In this condition, blood flow in the brain is disrupted due to blockage of blood vessels by blood clots, which prevent normal oxygen supply to cells. As a result, the cells die and the organ swells;
- cerebral hemorrhage caused by a ruptured artery, it develops with trauma and vascular aneurysm, causing increased pressure inside the head;
- hemorrhage in parts of the brain and its tissue;
- oncology in GM;
- proliferation of metastases in the brain, regardless of the location of the main tumor;
- head injuries with brain damage;
- meningoencephalitis, infectious inflammation of the meninges;
- fracture of the base of the skull;
- toxoplasmosis. This disease can cause swelling of the central nervous system in the fetus during fetal development;
- bruises inside the skull after head injuries;
- brain contusion;
- severe poisoning with alcoholic beverages, chemicals, poisons, toxins;
- rapid and sharp decline in renal and liver functions of a decompensated nature;
- swelling of the skin caused by decompensated myocardial dysfunction or allergies.
There are a number of other reasons why swelling occurs:
- increased blood pressure due to increased pressure in small blood vessels, that is, dilation of the cerebral arteries leads to the accumulation of cerebrospinal fluid in the interstitial space;
- impaired vascular permeability, which causes an increase in pressure in the interstitial space and causes destruction of cell membranes.
Normally, the pressure inside the skull in adults varies from three to fifteen mm Hg. Coughing, sneezing, increased intra-abdominal pressure and other physiological factors can increase its value to fifty to sixty mmHg, without causing any problems with the human nervous system. Why? Since the pressure value inside the head quickly returns to normal due to the internal protective features of the cerebral system.
Breast swelling can be diagnosed not only in adults, but also in newly born children. The cause of the development of the disease in infants is most often birth trauma, but it can also be triggered by other factors:
- oncological processes;
- oxygen starvation;
- infections or inflammations in the infant's breastbone;
- infections developed in the womb;
- late toxicosis during gestation;
- hematomas and bruises.
In children, paraventricular edema can be detected already in the first weeks of life.
Causes of GM swelling
Normally, intracranial pressure (ICP) in adults is between 3 and 15 mm. Hg Art. In certain situations, the pressure inside the skull begins to rise and create conditions unsuitable for the normal functioning of the central nervous system (CNS). A short-term increase in ICP, which is possible with coughing, sneezing, heavy lifting, or increased intra-abdominal pressure, as a rule, does not have time to have a detrimental effect on the brain in such a short period of time, and therefore cannot cause cerebral edema.
It’s another matter if damaging factors leave their influence on brain structures for a long time and then they become the causes of a persistent increase in intracranial pressure and the formation of such a pathology as cerebral edema. Thus, the causes of swelling and compression of the GM may be:
- Penetration of neurotropic poisons, viral and bacterial infections into the GM substance, which happens in the case of poisoning or various kinds of infectious and inflammatory diseases (encephalitis, meningitis, brain abscesses), which can become a complication of influenza and purulent processes localized in organs located in the immediate vicinity to the brain (tonsillitis, otitis media, sinusitis);
- Damage to the brain substance and other structures as a result of mechanical impact (traumatic brain injury - TBI, especially with fracture of the bones of the vault or base of the skull, hemorrhage and intracranial hematomas);
- In newborn children - birth injuries, as well as pathology of intrauterine development, the cause of which was illness suffered by the mother during pregnancy;
- Cysts, primary tumors of the brain or metastases from other organs, compressing the nervous tissue, preventing the normal flow of blood and cerebrospinal fluid, and thereby promoting the accumulation of fluid in the brain tissue and increasing ICP;
- Operations performed on brain tissue;
- Acute cerebrovascular accident (stroke) of the ischemic (cerebral infarction) and hemorrhagic (hemorrhage) type;
- Anaphylactic (allergic) reactions;
- Climbing to high altitudes (above one and a half km) - mountain edema in persons involved in mountaineering;
- Liver and kidney failure (in the stage of decompensation);
- Withdrawal syndrome in alcoholism (alcohol poisoning).
Any of the listed conditions can cause cerebral edema, the formation mechanism of which in all cases is, in principle, the same, the only difference being that the edema affects only a separate area or spreads to the entire substance of the brain.
A severe scenario for the development of AMS with transformation into swelling of the brain threatens the death of the patient and looks like this: each cell of the nervous tissue is filled with fluid and stretches to unprecedented sizes, the entire brain increases in volume. Ultimately, the brain, limited by the cranium, begins to not fit in the space intended for it (brain swelling) - it puts pressure on the bones of the skull, causing it to compress itself, since the hard cranium does not have the ability to stretch parallel to the increase in brain tissue, which is why the latter is subjected to injury (compression of the brain). In this case, intracranial pressure naturally increases, blood flow is disrupted, and metabolic processes are inhibited. Cerebral edema develops rapidly and without the urgent intervention of medications, and sometimes surgery, it can return to normal only in some (not severe) cases, for example, when climbing to a height.
Who's at risk
People from the following categories have a high risk of developing cerebral edema:
- heart patients and patients with problems of the vascular system, those who have suffered coronary artery disease, arterial hypertension, atherosclerosis. Most often, for this reason, pathology occurs in older people;
- people whose work involves the possibility of injury or a high risk of falling from a height;
- alcoholics. For those who abuse alcohol, ethanol kills nerve cells in the brain, and in their place, cerebrospinal fluid accumulates;
- newborns who are born naturally by passing through the birth canal.
Causes of swelling
A pathological increase in the volume of the brain matter can be caused by various reasons, including: trauma, infectious lesions, tumors, vascular pathologies.
Regional swelling can usually be caused by diseases and conditions that affect only a small part.
- Tumors, cancer diseases;
- Cystic formations;
- Blood tumors due to injury;
- An abscess due to an infection that has entered the brain.
The causes of a widespread increase in the volume of the brain matter include various diseases, poisoning, consequences of drowning, suffocation, and other injuries.
There are many reasons that can create both local and widespread swelling of the brain tissue.
- Skull and brain injuries, bruise after injury;
- Strokes and cerebral hemorrhages often occur in older people;
- Neonatal cerebral edema due to trauma during childbirth;
- Severe allergy attack;
- Epilepsy, heat stroke in childhood,
- Preeclampsia in the second half of pregnancy with a severe outcome;
- Severe infections: encephalitis, meningitis, mumps, toxoplasmosis;
- Many operations during which there is intervention in the cranial cavity cause edema. For example, swelling may occur after removal of a brain tumor.
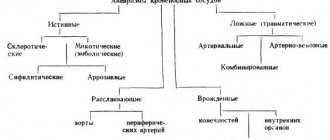
Classification
Depending on the affected area, swelling can be of two types:
- local or perifocal edema - affects a specific area of the organ;
- diffuse is extensive edema that affects the brain stem and hemispheres. In this case, the symptoms of the pathology are more pronounced.
Edema is also distinguished depending on the reasons that provoked the accumulation of cerebrospinal fluid in the cells of the organ.
Most often, traumatic edema is diagnosed, which, depending on the etymology, can be vasogenic or cytotoxic.
| Type of edema | Description |
| Vasogenic cerebral edema | Occurs due to dysfunction of the blood-brain barrier, while the white matter greatly increases in volume, and pathological symptoms appear already on the first day after injury. With this type of swelling, fluid accumulates in the nerve tissues that surround tumors, surgical areas, areas of inflammation, ischemia and injury. This type of swelling can quickly turn into compression of the GM. |
| Cytotoxic edema | Cytotoxic edema can be triggered by the following pathologies:
With this type of disease, mainly the gray matter swells. |
| Osmotic edema | It develops against the background of an increase in the osmotic concentration of nervous tissue. A similar phenomenon can develop in the following cases:
|
| Interstitial edema | It is characterized by the penetration of cerebrospinal fluid through the side walls of the ventricles into the tissues that surround them. |
Special attention to infants
The brain tissue and nervous system in newborns are in a developing stage, for this reason cerebral edema occurs differently in them than in adults. It develops in a matter of minutes and can be caused by the following factors:
- consequences of birth injuries;
- the presence of intrauterine infections;
- infection with meningitis or meningoencephalitis during childbirth or later;
- congenital pathologies of brain and nervous system development.
Suspicion of the development of edema may arise based on the following symptoms:
- the appearance of vomiting;
- inhibited state;
- restless behavior and continuous crying;
- breast refusal;
- convulsions;
- swollen large fontanel even when the child is calm.
With cerebral edema in newborns, symptoms increase quickly, and the child’s condition sharply worsens. In most cases, this condition is fatal within a very short time.
What development options are possible?
Swelling of the brain is not safe for the life of any person, because without adequate treatment it can provoke decompensated disorders in the body or consequences incompatible with life.
This disease is dangerous because it does not even always respond to treatment, so there are three main options for the consequences of brain swelling:
- The disease progresses, develops into swelling of the brain and ends in the death of the patient. This sequence of pathological conditions occurs in half of the cases. Edema is dangerous - as it progresses, a critical amount of dissolved substances accumulates in the brain. The patient will remain stable as long as there is room in the skull for the expanding brain. The more swelling becomes, the more dense brain structures will move inside the soft ones, for example, the cerebellar tonsils will be pressed into the brain stem, which will ultimately lead to respiratory arrest and cessation of heart function.
- The swelling is eliminated completely without causing any complications. This is a very rare outcome after treatment of the pathology; it is only possible if the swelling is diagnosed in young and physically healthy people, against the background of alcohol or other type of poisoning of the body. If the dose of toxins is compatible with life and the patient is taken to a medical facility in a timely manner, the swelling of the brain can be stopped without any consequences for the body.
- The swelling of the brain is eliminated, but due to serious complications the patient becomes disabled. This outcome of the disease is possible in cases where swelling is caused by meningitis, head injuries and moderate meningoencephalitis. In most cases, it is impossible to visually determine whether a person has a disability.
Why does brain swelling occur?
In the absence of timely treatment, any pathology of the central nervous system can provoke swelling. For example:
| Causes of cerebral edema | brief information |
| Severe traumatic brain injury | Occurs during accidents and any other incidents or after surgery. It is characterized by the development of a moderate to severe head contusion, a fracture of the base of the skull, a hematoma in the area of intracerebral structures, a subdural hematoma, and axonal damage. |
| Hemodynamic disorder | Extensive ischemic or hemorrhagic stroke, hemorrhage in the subarachnoid space or ventricles of the brain cause edema and swelling of brain formations. |
| Infectious pathology | Meningitis, meningoencephalitis, etc. |
| Neoplasms in GM | Benign and malignant tumors inside the skull, metastatic damage to the tissues of the nervous system. |
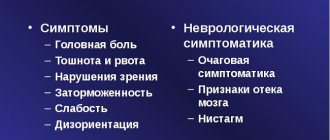
Symptoms
The clinical picture of edema is very diverse; the most characteristic, but not specific, symptom is a terrible headache that cannot be relieved by any painkillers.
The appearance of such symptoms should especially raise suspicion if there has been a recent head injury or, in addition to a headache, the victim has nausea and vomiting.
Let's list all the most basic signs of edema, which can appear gradually or lightning fast, depending on how quickly swelling progresses in adults:
- consciousness becomes darkened. The degree of his disorder can vary, from mild congestion to a deep coma. As the pathology progresses, the fainting state increases and deepens;
- symptoms indicating the presence of inflammation of the meninges of an infectious nature, their combination with a deterioration in general well-being and clouding of consciousness should be especially alarming;
- with edema at the initial stage, focal symptoms may develop - impaired motor activity of the limbs, paralysis of 1/2 of the torso, visual disturbances, speech disorders, hallucinations, and coordination of movements in general may be impaired. With classic swelling of brain tissue, these functions are completely stopped, since the patient is unconscious and his body is not capable of higher nervous activity;
- as the pathology progresses, short-term convulsive states begin, which are subsequently replaced by a complete weakening of muscle tone;
- Blood pressure drops and pulse destabilizes. This symptomatology indicates the spread of edema to the brain stem, in which the main centers for ensuring the conditions for preserving life are located;
- uneven breathing, which also indicates damage to important parts of the brain stem, in particular the respiratory center;
- floating of the eyeballs or divergent strabismus indicate that the GM cortex is disconnected from the subcortical centers.
In the initial stages, memory disorders, forgetfulness, decreased vision, and neck pain occur.
If the swelling is caused by alcohol intoxication, then pronounced cyanosis and bruising may appear on the face. In most cases, the symptoms only increase, and the disturbance of consciousness deepens, as a result of which the patient completely loses the ability to higher nervous activity and the ability to motor activity.
Signs of the disease in newborns are severe anxiety, incessant crying, enlarged pupils, refusal to breastfeed, tension or swelling of the fontanel. Also, the baby may have a very enlarged head, and convulsions may occur. The critical period for babies is the month after birth. If such symptoms appear, you should immediately seek help from a doctor, since delay can result in the rapid development of the disease and death.
Clinical manifestations of pathology
The main clinical sign by which cerebral edema is judged is a disorder of consciousness. With the gradual progression of the pathology, consciousness changes from stupor to coma, and after some time convulsions, muscle atony and other manifestations develop. In the case when the patient’s consciousness changes slowly, he complains of intense headache and nausea, movement disorders, visual disturbances, hallucinations, and then symptoms of cerebral edema are added.
Dangerous symptoms of brain swelling in adults include coma, respiratory distress, a sharp decrease in blood pressure, instability of heart contractions, an increase in body temperature above 40 ° C, divergent strabismus and the symptom of “floating” eyeballs.
Stages of ONGM and their signs
In clinical medicine, there are three degrees of severity of pathology:
- mild degree – clinical manifestations are erased. Sometimes patients complain of prolonged headaches and a feeling of general malaise;
- pathology of moderate severity is manifested by dilation of the pupils, weakening of the corneal reflex, confusion of the patient’s consciousness and gradual immersion in a coma. At this stage, the development of convulsive syndrome is possible;
- the severe stage is characterized by coma, lack of pupillary response to light, “floating” eyeballs, hypotension and fever.
The prognosis for the patient depends on the severity of the clinical manifestations of the disease. In the absence of treatment, the pathology can progress.
Diagnostics
If there is a suspicion of swelling of the central part of the nervous system, only a doctor can tell you how to relieve the swelling. Initially, the patient should be examined by a neurologist and an ophthalmologist. Children under one year old undergo neurosonography. Older patients undergo a CT or MRI scan of the head.
Conclusions about the reasons for the formation of OBM are made on the basis of the collected anamnesis, assessment of the medical history in neurology, general and biochemical blood tests and the results of studies visualizing the structure, functions and biochemical characteristics of the brain. Since this pathology rapidly progresses, all diagnostic procedures should be carried out in a hospital setting together with therapy. Treatment measures can be carried out depending on the severity of the patient in the intensive care unit or intensive care unit.
Recovery
The processes of complications, their severity and severity, will directly depend on the quality and efficiency of medical care. Restorative measures after the operation are carried out in the hospital. If during the development of brain swelling the visual and speech centers and the area of the musculoskeletal system were affected, then the person will have to learn to walk and talk again.
The consequences after the acute stage of the disease will not always be serious, but in some cases there is a possibility of death. A pathology of this type, taking into account the individuality of clinical manifestations and the many causes of its occurrence, almost always remains unpredictable for doctors, therefore, in any case, three main paths of the disease are always considered:
- Subsequent development of pathology, compression of brain structures by edema, death of a person.
- Elimination of swelling, patient disability.
- Elimination of edema without any serious consequences.
According to world statistics, five out of ten patients who have been diagnosed with cerebral edema die within a few days after the onset of the pathological process.
Treatment methods
If the brain matter swells in climbers due to a rapid increase in altitude or cerebrospinal fluid accumulates locally for another reason, then treatment in a medical facility may not be necessary. The symptoms will go away on their own within two to three days. All this time, a person may feel a headache, nausea and dizziness, so diuretics, analgesics and antiemetic medications may be additionally prescribed. More severe conditions may require extensive medication or even surgery.
The complex of therapeutic procedures should include several areas:
- combating existing swelling and preventing its progression;
- determination of the causes of development of pathologies and their relief;
- elimination of additional symptoms that aggravate the patient’s well-being.
Conservative methods
Treatment with medications must be comprehensive. Initially, medications are prescribed that remove excess cerebrospinal fluid from organ tissues:
- osmotic diuretics. An example is Manit. After its infusions, loop diuretics are administered to provide maximum dehydration effect;
- loop diuretics (Furosemide, Lasix, Trifas) in a very high dosage. This is necessary to quickly achieve the required concentration of active ingredients and achieve a diuretic effect;
- L-lysine escinate. Taking such drugs is necessary to remove fluid from tissues and reduce signs of swelling;
- hyperosmolar solutions (glucose 40%, magnesium sulfate 25%). These drugs short-term increase plasma osmotic pressure and enhance the effect of diuretics. Additionally, brain cells are provided with nutrients.
Dehydration therapy must be supplemented with adequate oxygenation and means to improve metabolic processes in the brain. To this end, the following activities are carried out:
- a machine for artificial ventilation of the lungs is installed or humidified oxygen is introduced by drip;
- measures are taken for local cooling - the patient’s head is covered on all sides with ice packs;
- medications are administered that normalize brain metabolism (Actovegin, Ceraxol, Kotexin);
- To prevent the expansion of swelling, corticosteroids are prescribed, but they are effective only for local lesions. These drugs strengthen the walls of blood vessels in the brain.
It is necessary to treat not only the swelling itself, but also the causes that provoked it, as well as the consequences caused by the disease. Depending on the situation, it is necessary to pay attention to any manifestations of the disease and, if necessary, correct the condition of the heart, eliminate the signs and consequences of poisoning of the body, and combat increased body temperature, which can aggravate swelling.
After establishing the exact cause of the formation of edema, the following drugs and measures can be prescribed:
- antibiotics that have high penetrating ability against the blood-brain barrier - Cefuroxime, Cefepime;
- means for removing toxins from the body;
- drugs to combat seizures - barbiturates;
- drugs to suppress excitability, sedatives and muscle relaxants (Diazepam, Relanium);
- drugs that normalize blood circulation and brain nutrition - Trental, Curantil, etc.
Swelling of the brain tissue can be treated only in a hospital setting under the supervision of specialists; any delay can cause death.
Surgical
If drug treatment for swelling is not enough, surgery may be prescribed:
- craniotomy (Fig. a) – excision of operable intracranial tumors, but only when the patient is in a stable condition;
- endoscopic removal of bruises in the brain;
- ventriculostomy (Fig. b) - installation of drainage in the form of a hollow needle and catheter to ensure the outflow of cerebellar fluid from the cerebellum, reduce pressure inside the skull and reduce swelling in general.
Rice. A
Rice. B
Etiology
There can be many reasons for the development of cerebral edema in children and adults. The most common of them are:
- Infections (toxins damage nerve tissue, which leads to the occurrence of an inflammatory process).
- Trauma to the brain and spine (for example, swelling of the brain after an accident, surgery, a strong blow to the head, a fall, etc.). The site of injury on the head after an injury in an accident may become very swollen, which usually occurs with a TBI.
- Tumor processes (cancer), in particular glioblastoma and cysts, localized in various parts of the brain, which lead to problems with the outflow of cerebrospinal fluid or displacement of brain structures.
- Hemorrhagic stroke, penetration of blood into the subarachnoid space.
- Embolism of the head vessels with the simultaneous occurrence of ischemic stroke.
- Heavy exposure to radiation.
- Poisoning with drugs, poisons, toxins (extremely dangerous during pregnancy).
- Encephalitis tick bite (the likelihood of dying from such a pathological process is high).
- The presence of metastases in the brain due to cancer.
- Metabolic encephalopathy (observed in severe renal or liver failure, in the last stages of alcohol dependence, in diabetes).
- Eclampsia.
- Water intoxication.
- Some types of vaccinations (controversial issue).
It happens that the brain often begins to swell in newborns who were born prematurely, or during a pathological course of labor. In this case, swelling in infants is traumatic.
The brain may begin to swell due to exposure to a number of toxins: gasoline, ethyl alcohol (and other types of alcohols), phenol, cyanide, etc. A huge number of medications that are used to treat various diseases and have a pronounced neurotoxic effect, in cases of overdose, can also lead to toxic cerebral edema. This category of medications includes: tranquilizers, antipsychotic drugs, tricyclic antidepressants, antihistamines.
Patient prognosis
How long do people live with this pathology? As practice shows, in the initial stages this can still be a reversible process, but as the disease progresses, the chances of a complete recovery are minimal, since severe swelling provokes the development of irreversible changes in the brain structures, namely, it causes the death of nerve fibers and destruction of fibers with myelin.
Complete recovery from edema is possible only if it is of toxic origin and only when the patient is young, healthy and delivered to a medical facility on time. Spontaneous disappearance of signs of pathology is possible in the case of mountain edema, if the patient was quickly removed from the high-mountainous area where he developed the pathology. The duration of regression of symptoms in this case is no more than 2-3 days.
Most often, it is impossible to recover completely; the patient may experience residual effects that are invisible to others, but cause some discomfort to the patient:
- headache;
- increased intracranial pressure;
- absent-mindedness;
- memory problems;
- sleep problems;
- depressive states;
- convulsions;
- impaired coordination of movements;
- violation of physical development;
- problems with communication skills;
- epileptic seizures;
- paralysis;
- breathing problems;
- coma;
- the patient is in a vegetative state due to loss of functions of the cerebral cortex.
In the case of severe swelling of the brain and its compression, the prognosis for life is disappointing, since displacement of the brain structures provokes respiratory arrest and cessation of the heart muscle, that is, leads to the death of the patient.
Why is OGM dangerous?
The consequences of cerebral edema can be early and long-term. Early complications include coma, death from cerebral edema, infectious or traumatic tissue damage during surgery, and loss of motor or mental function.
Edema of the central nervous system structures is a dangerous and difficult to treat complication of diseases of the central nervous system. This condition develops in various pathologies in people of any age. Without timely emergency care, swelling can lead to compression of the stem structures and death of a person. In this regard, if there are pathologies of the central nervous system, you should promptly consult a doctor and undergo the necessary treatment.
Long-term or residual consequences are manifested by paresis, paralysis, increased intracranial pressure, atrophy of the cerebral cortex, memory loss, absent-mindedness and forgetfulness, depression, euphoria and loss of criticism of one’s own condition, violation of the moral norms of society, headaches and other complications. The prognosis after undergoing AGM is unfavorable; patients are assigned disability group II or III.
Doctors know that cerebral edema is a serious condition and how long patients live. With timely provision of medical care and relief of pathological changes, life expectancy is not reduced. If therapy is not provided in full or late, then neurological deficit, coma and dysfunction of internal organs can cause the death of the patient.
Swelling and headache during pregnancy
Swelling of the limbs is one of the common symptoms during pregnancy. The main signs of swelling:
- rapid weight gain - more than 1 kilogram per week;
- change in the shape of the face, enlargement of the lips and nose;
- swelling of the eyelids, bags under the eyes;
- the foot does not fit into worn-out shoes;
- numbness and tingling of the limbs;
- It’s hard to bend your hand into a fist, it’s hard to move your toes.
If swelling is accompanied by a headache, you should immediately consult a doctor. This condition indicates gestosis, which is especially dangerous in the last trimester of pregnancy.
During pregnancy, the list of drugs that can be used to relieve pain is very limited. Of the approved drugs, you can take Ibuprofen or Nurofen (only in the first and second trimester), Papaverine and Paracetamol.
Limiting daily fluid intake and taking diuretic medications will help relieve swelling: Canephron, Phytolysin, Eufillin. You can also take infusions and decoctions of cranberries, lingonberry leaves, lovage, bearberry leaves and birch.
Before taking any medications, you should consult a supervising obstetrician-gynecologist.
Prevention
Illness can be avoided if you follow safety rules. These include:
- fastening seat belts;
- wearing a helmet when riding a bicycle, rollerblading, or working on a construction site;
- undergoing acclimatization during mountaineering;
- to give up smoking;
- constant monitoring of blood pressure.
What is the main danger of edema?
Swelling of any tissue in the human body is a fairly common and completely natural phenomenon, which, as a rule, passes without any special consequences. But the brain is in a limited space, in a dense cranium, which cannot increase its volume under the pressure of its tissues.
Whatever the causes of cerebral edema, they ultimately lead to compression of its substance in a narrow space. And this circumstance entails the greatest danger: neuronal ischemia worsens, the progression of edema intensifies, and at some point brain functions are lost.
Diagnostic methods
If you suspect a pathology, it is recommended to consult a neurologist or neurosurgeon. Research methods used to make a diagnosis:
- CT scan of the brain. Computed tomography is performed using x-rays, which are used in minimal quantities. In this case, the doctor determines the characteristic cerebral edema using a series of images, which he receives from different projections. The method helps to identify provoking factors: tumors, abscesses, etc.
- MRI. Magnetic resonance imaging is considered a more reliable research method than CT. In addition, the specialist obtains images using nuclear magnetic resonance. This method is safe and reliable. On a computer monitor you can get a 3D image of the organ being examined. With cerebral edema, swollen tissues and compressed centers are visible.
- General blood analysis. Used as an auxiliary method to determine the condition of the body as a whole. At the same time, deviations from the norm of leukocytes, erythrocyte sedimentation rate, and platelet count are assessed. However, in the initial stages of cerebral edema, general indicators may remain unchanged.
- Encephalography. Used as an auxiliary method to identify the degree of neurological disorders. In this case, a special device with many wires is put on the patient’s head. The electrodes transmit impulses from the brain, which are recorded on a special diagram, with the help of which the doctor can detect the presence of disturbances in the functioning of the organ.
MRI of the brain is the most reliable method for determining cerebral edema
Additionally, in rare cases, a lumbar puncture may be used, in which a small amount of fluid is removed from the spinal cord for examination. The procedure is carried out using a thin and long needle, which is placed between the 3rd and 4th or 4th and 5th vertebrae. Puncture is performed only in extreme cases, as it has a number of contraindications and side effects.
Diagnosis criteria
Cerebral edema is confirmed if there is:
- characteristic neurological symptoms;
- high rate of increase in intracranial pressure;
- papilledema;
- increased tendon reflexes;
- decreased reaction of the pupils to a light stimulus;
- divergence of eyeballs;
- pronounced swelling of the conjunctiva.
The diagnosis is confirmed only through a brain scan using computed tomography or magnetic resonance imaging.
The mechanism of edema formation
The occurrence of edema can be a cause of death, and it occurs by the following mechanism:
- Each cell of the brain organs is filled with biological brain fluid. Swelling may be localized to the focal point of organ damage in the brain, and may also occupy all cells of the brain tissue;
- The cells stretch and the brain becomes larger;
- It presses on the inside of the skull because it does not fit into its volume;
- When the brain edema, the cells are compressed, which is why they are injured.
Brain cells are subject to injury due to the hard shell of the skull. The pressure in the cerebral arteries inside the skull increases, and a disturbance in the microcirculation of blood flow in the brain occurs. Edema leads to inhibition of all brain functions.
The development of edema occurs quite quickly and urgent medical treatment is necessary. Sometimes emergency brain surgery is required to save a person's life.
Kinds
According to the extent of its course, the disease is divided into three types - local, diffuse and generalized cerebral edema.
In the first case, there is a non-extensive formation, which, as a rule, covers the part of the brain affected by a hematoma, tumor or abscess. Generalized edema spreads over the entire brain area. It occurs in cases of traumatic brain injury, prolonged lack of oxygen access (suffocation, drowning), intoxication and significant loss of body protein. Diffuse cerebral edema usually extends to only one hemisphere
Based on their origin, 4 types of edema can be distinguished:
- vasogenic (associated with a violation of the blood-brain barrier, which means the entry of plasma proteins);
- cytotoxic (change in osmotic regulation of cell membranes);
- ischemic (hemorrhage);
- interstitial (excessive amount of cerebrospinal fluid in the brain tissue).
Based on location, 3 types of pathology can be distinguished:
- swelling of cerebral vessels;
- swelling of the brain;
- swelling of the brain stem (the most dangerous type, as it blocks the vital functions of the body).
Depending on the factor in the appearance of edema, the following types of pathology differ:
- postoperative;
- post-traumatic (arising as a result of traumatic exposure);
- toxic (for any severe poisoning);
- tumor (in the presence of neoplasms);
- inflammatory;
- epileptic (occurring with epilepsy);
- ischemic (appearing after hemorrhages);
- neuroendocrine.
Symptoms
Clinically, signs of swelling can be divided into cerebral and focal. Symptoms of cerebral edema, their alternation and combination with each other depend on the root cause of the disease. In this regard, gradual and lightning-fast forms of swelling are distinguished. In the first case, there is time to prevent the progression of edema, and in the second, all that remains is the fight for life and slowing down the progression of the pathology for some time.
In adults
For this disease, the following groups of symptoms are distinguished:
- focal symptoms;
- clinic on the background of intracranial hypertension;
- stem symptoms.
Symptoms in adults:
- Blurred consciousness. It manifests itself in all types of the disease and varies in severity: from stupor to deep coma. With further increase in edema, the depth of the fainting state increases.
- Balance is disturbed when walking.
- Headache. It happens due to chronic and increasing acute brain diseases.
- Decreased vision.
- Drop in blood pressure, drowsiness, weakness.
- Nausea accompanied by vomiting.
- Convulsions, up to loss of consciousness (the patient bites his tongue).
- Breathing disorders.
In children
Young mothers are advised to monitor their children very closely in order to promptly notice any deviations in the baby’s behavior. The presence of a pathological condition in a child is indicated by increased intracranial pressure, neurological changes, and dislocation syndrome of brain structures. The main symptoms of cerebral edema in children are complemented by lethargy, weakness, and headache. Paresis and paralysis may appear or intensify, and the optic nerve swells.
As the pathology progresses, convulsions occur, the functions of the cardiovascular system are disrupted, and symptoms increase. The clinical picture is as follows:
- intractable hyperthermia;
- headache;
- excited state;
- "brain" scream;
- bulging fontanel;
- stiff neck;
- coma;
- sopor;
- acute renal failure;
- symptoms of occipital and temporoparietal herniation of the brain: strabismus, anisocoria, disturbance of vital functions (dislocation syndrome of brain structures);
- oculomotor crisis with gaze fixation and dilated pupils, tachycardia, increased muscle tone, hyperthermia, pressure instability (midbrain compression syndrome);
- mydriasis, vomiting, anisocoria, loss of consciousness (trunk compression syndrome);
- bradypnea, bradycardia, dysphagia, vomiting, paresthesia (impaired sensitivity) in the shoulder girdle, stiff neck, respiratory arrest (cerebellar entrapment syndrome).
Prognosis and complications
If you managed to get rid of cerebral edema in the initial stages, then the prognosis is favorable. In advanced cases, irreversible processes and death of neurons occur with the further appearance of pathologies. To prevent complications, you need to follow all the doctor’s recommendations during the rehabilitation period: eat right, take medications and get plenty of rest.
Early consequences:
- frequent headache;
- memory and attention disorders;
- dizziness;
- coordination problems;
- fainting.
Frequent dizziness may occur after cerebral edema.
Long-term consequences that may occur 6–12 months after rehabilitation:
- epileptic seizures;
- decreased visual acuity;
- mental disorders;
- feeling of spasms in the head;
- convulsions.
To eliminate the consequences, medications are prescribed that improve brain function and the conduction of nerve impulses, as well as antioxidant drugs.
First aid for suspected swelling
Emergency care for cerebral edema is a set of measures aimed at eliminating the threat to the patient’s life, which allows him to be transported to a medical facility for further therapy and examination.
The immediate range of actions is as follows:
- Elimination of poor activity of vital brain functions.
- Implementation of forced diuresis.
- Correction of acid-base balance and electrolyte levels.
- Elimination of excessive permeability of the brain's BBB.
- Normalization of blood pressure.
- Correction of psychomotor agitation.
- Relief of elevated temperature.
- Improving metabolic functions and blood circulation.
- Carrying out oxygen therapy, etc.
Any symptom that is life-threatening must first be eliminated in order to be able to diagnose and transport the patient to the right place.
Therapeutic effects
Treatment and diagnostic procedures (tomography, neurological examination, clinical and biochemical tests) are carried out simultaneously, since cerebral edema is a life-threatening condition.
The main measures to eliminate pathology include several points.
- Dehydration treatment is a priority - it rids the cerebral tissue of fluid. It is carried out using intravenous administration of diuretics with drugs that potentiate their effect.
- Symptomatic treatment consists of correcting cardiovascular activity, lowering body temperature, removing toxic compounds from the body, and administering antibiotics. Elimination of the cause of the pathology, which is carried out through surgery or drainage, is carried out after stabilization of the condition.
- Improving brain metabolism is achieved through oxygenation, artificial ventilation, administration of glucocorticoids and drugs that correct metabolic brain processes.
Sometimes swelling is eliminated through surgery: decompression craniotomy is performed in the fronto-parietal-temporal region on one or both sides. With its help, a “window” is created (by removing a bone fragment), the dura mater is dissected, and then plastic surgery is performed using a graft. This method is used only in extreme cases, when cerebral edema is not relieved by medications, since complications are possible after surgery: damage to the brain and its blood vessels when the dura mater is opened, and swelling of the brain with entrapment in the trepanation “window.”
How to help a patient at home
Can brain swelling go away without complications? Yes, if the disease was treated in a hospital and the patient was provided with timely assistance at home.
If you suspect that a patient has this pathology, relatives should immediately call an ambulance, and before the doctors arrive, they must do the following:
- Lay the patient on a horizontal surface, open all windows to allow oxygen to flow.
- During attacks of vomiting, carefully monitor the patient so that the airways are not clogged with vomit. In this case, you can lay the patient on his side.
- Cover the patient's head with ice packs or wrap a cloth soaked in cold water.
- If there is an oxygen mask in the house, put it on the patient.
The sooner the patient is taken to the hospital, the greater the chance that the serious consequences of the disease will be minimized. When independently transporting a patient to a medical facility, the following rules must be observed:
- lay the patient horizontally, without placing anything under the head;
- place a rolled blanket or pillow under your feet;
- turn your head to the side to prevent vomit from entering your respiratory tract.
First aid
Trying to relieve swelling on your own without the help of a doctor can be fatal.
First aid for the occurrence of cerebral edema includes several actions. First, to reduce tension, a person's head is covered with ice packs. In addition, about 30 ml of glucose and 15 ml of piracetam are injected, glucorticoids and Lasix saline solution are administered. An oxygen mask is put on the patient to provide the brain with sufficient access to the substance.
After the measures are taken, the person is admitted to the hospital: if the cerebral edema is of a traumatic nature, then to the neurosurgical department of the neuralgic hospital; in case of toxic swelling, the patient is hospitalized in the intensive care or toxicology department.
Briefly about cerebral edema in children
The principles of the occurrence of cerebral edema in children over 2 years of age do not differ from those in adults. The development of pathology in infants has a number of features:
- their edema increases at lightning speed due to imperfect mechanisms for maintaining vascular tone and normal cerebrospinal fluid pressure, as well as unstable cerebrospinal fluid dynamics;
- in children under 1.5 years of age, the bones of the skull can still diverge due to the compliance of the sutures and fontanelles, thus increasing the capacity of the subarachnoid space.
Therefore, despite the rapid increase in edema, dislocation of brain structures rarely occurs with timely initiation of therapy.
Children aged 6 months to 2 years who have been diagnosed with any pathology of the central nervous system are at risk for developing cerebral edema. Those who have had allergic reactions are also predisposed to this pathological condition. Among the causes of edema in children are the following:
- intrauterine asphyxia or hypoxia;
- prolonged labor;
- birth injury;
- congenital defects and developmental abnormalities of the nervous system;
- intrauterine infections.
The first signs of cerebral edema in young children are:
- irritability, anxiety, brain “cry” or drowsiness, apathy;
- the child refuses breast or formula;
- bulging of a large fontanel;
- vomiting or repeated regurgitation;
- epileptic seizure
In children under 1.5-2 years of age, in addition to meningeal symptoms, convulsions, increased reflexes and oculomotor disorders, head circumference increases, and the bones of the skull become mobile during palpation as a result of suture dehiscence. And in infants, an already closed fontanel may open.
Reliable methods for diagnosing edema in children are CT, MRI and neurosonography (possible up to the age of one year with an open large fontanel).
Unlike adults, in children, craniography reveals an increased pattern of digital impressions, and the bones of the cranial vault become thinner, which is a sign of cerebrospinal fluid hypertension.
Despite the fact that the child’s brain has greater neuroplasticity, its swelling has the following consequences:
- delayed psychomotor development;
- symptomatic epilepsy;
- posthypoxic encephalopathy;
- frequent fainting.
Approaches to the treatment of cerebral edema in children are the same as in adults. Only the dosage of drugs is calculated taking into account the age and weight of the child.
Classification of cerebral edema
Cerebral edema is classified according to its prevalence, as well as the predominant mechanism of development.
Types of edema depending on the prevalence of the process
There is local (local, limited) cerebral edema, an example of which is perifocal edema around a tumor, cyst, ischemic focus, etc. A diffuse (generalized) type is also distinguished, in which the pathological process affects the cerebral hemispheres and stem structures. It is characterized by pronounced cerebral and focal symptoms.
Osmotic cerebral edema
Osmotic cerebral edema is prognostically unfavorable and the most dangerous, since clear criteria for the treatment of this condition have not yet been developed. It develops as a consequence of a violation of the normal osmotic difference between brain tissue (which has a higher osmolarity) and plasma.
Water intoxication of the central nervous system progresses due to an increase in the concentration of metabolic products in neurons and an artificial decrease in plasma osmolarity during intravenous infusion (introduction) of low-osmolar solutions. Most often observed in encephalopathies of a metabolic nature (renal or liver failure, hyperglycemia).
Relieving this type of edema is difficult. The fluid is not retained in the bloodstream and is directed into the cells and intercellular space of the brain tissue. The search for a drug that would retain water in the plasma is one of the primary research tasks of practicing neurologists.
Vasogenic type of edema
Vasogenic edema is caused by impaired permeability of the blood-brain barrier and capillary basement membrane. Disruption of the normal structure of the vascular wall occurs due to direct trauma (primary mechanism) and when it is exposed to free radicals, histamine, bradykinin (secondary mechanism).
As a result, active migration of blood plasma containing electrolytes and proteins occurs from the vascular bed into the brain tissue. The oncotic pressure of the latter increases and promotes the accumulation of fluid in the intercellular space. Most often, the vasogenic type of edema is observed in the perifocal zone of a tumor, stroke, contusion lesion, as well as in infectious and allergic pathologies.
Hydrostatic type of cerebral edema
The hydrostatic mechanism for the development of cerebral edema occurs during liquor hypertension and usually manifests from the periventricular (periventricular) space. At this point, the transition of water from the interstitial space to the cerebrospinal fluid deteriorates.
This also includes the occurrence of edema against the background of increased pressure in the capillaries and deterioration of venous outflow. Hydrostatic edema appears when there are volumetric formations of the brain (cyst, tumor, aneurysm), which compress large veins, sinuses, and also impede the circulation of cerebrospinal fluid.
Cytotoxic cerebral edema
Cytotoxic edema is formed as a result of exogenous (poisoning with alcohol, chemicals) or endogenous poisoning of the body. Among the causes of this condition are renal and liver failure, paraneoplastic syndrome, hemorrhagic and ischemic stroke.
The cytotoxic form of cerebral edema in 90% of cases is diffuse, spreading with lightning speed (within 1-2 hours) to the cerebral hemispheres and brain stem, accompanied by signs of herniation.
Possible causes of facial swelling
Below are the most common causes of facial puffiness.
Actinomycosis
Actinomycosis is a rare and potentially dangerous chronic bacterial infection that causes swelling and abscesses in the soft tissues of the body. This condition usually affects the mouth, nose, throat, stomach and intestines.
Other symptoms of actinomycosis include the following:
- chest pain;
- cough;
- fever;
- bumps on the face;
- skin inflammation;
- weight loss.
When treating people with actinomycosis, doctors usually prescribe large doses of the antibiotic penicillin. If the patient is allergic to this drug, he will be offered remedies with a similar effect. Sometimes people have to undergo treatment for several months to completely get rid of the infection, but it should be understood that actinomycosis is a non-contagious, that is, non-contagious disease.
Allergic conjunctivitis
Allergic conjunctivitis is an inflammation of the eye that develops as a result of an allergic reaction. Allergens include the following:
- dust;
- mold spores;
- pet hair;
- pollen.
The main symptom of this condition is reddened and moist eyes, in which there is a burning sensation and itching. The skin around the eyes may become swollen, especially after waking up.
For any form of conjunctivitis, it is important not to rub your eyes, as doing so can make symptoms worse.
People can prevent allergic conjunctivitis by avoiding allergens. Treatment for this condition involves applying cold compresses to the inflamed areas and taking medications such as antihistamines and anti-inflammatory or steroid eye drops.
Anaphylactic shock
Anaphylactic shock is an acute allergic reaction. This is a medical condition that can be fatal and therefore requires immediate medical attention. Symptoms tend to appear soon after the body interacts with allergens, and their severity quickly worsens. Symptoms of anaphylactic shock include the following:
- labored breathing;
- diarrhea;
- swelling of the face;
- urticaria (red, raised, itchy rash);
- itching;
- loss of consciousness;
- nausea and vomiting;
- cardiopalmus;
- sudden drop in blood pressure.
If a person experiences symptoms of anaphylactic shock, they should seek emergency medical attention immediately.
People who experience symptoms of anaphylactic shock for the first time are at risk of developing future reactions. They should avoid exposure to allergens and carry an epinephrine auto-injector with them at all times.
Angioedema
Angioedema is swelling that occurs as a result of an allergic reaction to food, medications, or other allergens such as insect bites. In addition to facial swelling, symptoms of angioedema include the following:
- hives;
- itching;
- rash;
- abdominal cramps.
Mild angioedema does not always require treatment, although in such cases exposure to allergens should be avoided. For moderate to severe symptoms, the use of epinephrine, antihistamines, or other medications may be necessary.
Home care methods include using cold compresses and wearing loose clothing.
Nose fracture
Various traumatic episodes can cause a nasal fracture. Such damage can also lead to facial swelling and other symptoms, such as:
- crooked nose;
- bruising;
- nosebleeds;
- pain.
A nasal fracture does not always require medical attention, but people should see a doctor after any facial injuries. Treatment usually involves taking painkillers, splinting, and applying cold compresses. Some patients in such situations require surgery.
Cellulite
Cellulite is a bacterial skin infection that causes redness, swelling and local fever in the affected areas. Cellulite can also cause pain. Without treatment, this condition can be life-threatening.
Signs of an acute infection include the following:
- fever;
- chills;
- red streaks extending from the rash.
To treat cellulite, doctors usually prescribe antibiotics, which patients take for at least five days. Painkillers and complete rest for the body also help reduce discomfort.
Cushing's syndrome
Cushing's syndrome is a disorder that occurs when the body begins to produce too much of the hormone cortisol. People with Cushing's syndrome often have a swollen and round face. Their skin can be easily bruised, and their hair becomes thicker.
A common cause of Cushing's syndrome is the intake of large amounts of glucocorticoids.
Some types of tumors can also lead to excess cortisol production. However, this medical condition is rarely endogenous, that is, caused by internal pathological processes in the body.
According to the US National Institute of Diabetes and Digestive and Kidney Diseases, the endogenous form of Cushing's syndrome affects 40 to 70 patients per million of the world's population.
Treatment depends on the cause of the problem. Treatment options include cortisol-lowering drugs, surgery, radiation therapy, and chemotherapy.
Allergy to medications
An allergic reaction to specific medications may require emergency medical attention. In addition to facial swelling, it can cause the following:
- labored breathing;
- fever;
- hives;
- itchy red rash;
- cardiopalmus;
- stomach upset.
It is important for people to tell their doctors, dentists, and pharmacists if they are allergic to certain medications and to avoid using those medications. Professional medical workers will be able to select alternative and safe pharmacological products.
Common causes of drug allergies include the following:
- certain antibiotics, such as penicillin;
- anticonvulsants;
- nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin and ibuprofen;
- drugs for chemotherapy.
People with allergies may need to wear medical bracelets at all times to help prepare those around them for emergency situations.
Hypothyroidism
Hypothyroidism, or an underactive thyroid, is a medical condition in which the thyroid gland produces too low amounts of hormones. Thyroid hormones help the body regulate its use of energy.
Swollen skin on the face is one of the symptoms of hypothyroidism. Other symptoms include the following:
- constipation;
- depression;
- dry skin;
- fatigue;
- high cholesterol;
- muscle weakness;
- painful or stiff joints;
- decreased heart rate;
- gaining excess weight.
People who experience symptoms of an underactive thyroid gland should meet with a doctor for evaluation. According to the American Thyroid Association, about 60% of people with thyroid disease do not know they have the condition.
Hypothyroidism cannot be cured, but by taking medications and making positive lifestyle changes, its symptoms can be managed.
Preeclampsia
Preeclampsia is a medical condition that develops in women while pregnant and requires emergency treatment. Early signs include increased blood pressure and increased levels of protein in the urine. Preeclampsia can cause dangerous complications - high blood pressure, kidney and liver damage, and epileptic seizures.
Symptoms of preeclampsia include the following:
- abdominal pain;
- constant headache;
- sudden weight gain;
- swelling of the face and hands;
- visual disturbances.
To treat preeclampsia, doctors may recommend early birth. However, the choice of treatment depends on the duration of pregnancy and the severity of the disease.
If this condition develops before the 37th week of pregnancy, the doctor may recommend monitoring the patient's condition by medical personnel and taking medications to lower blood pressure and prevent epileptic seizures.
Sinusitis
Sinusitis is a common medical condition that occurs as a result of inflammation of the sinuses and sinuses.
Sinusitis can cause swelling and tenderness of the face around the nose and eyes, as well as the following symptoms:
- cough;
- fatigue;
- fever;
- headache;
- nasal congestion;
- rhinorrhea;
- sore throat.
Home care methods include maintaining fluid balance, applying warm compresses and steam treatment. Over-the-counter decongestants can reduce nasal congestion, and pain relievers can ease headaches.
If symptoms do not subside after a few weeks, this may indicate that the person has a bacterial infection that requires treatment with antibiotics.
Dental infections
Dental or gum infections can cause swelling in the chin area. They also cause pain in the area.
Dentists usually prescribe antibiotics to treat such infections. They may also perform a procedure to remove the nerve or damaged pulp from the affected tooth. People can use salt water rinses or over-the-counter medications to reduce discomfort.
Superior vena cava syndrome
Superior vena cava syndrome is a serious medical condition that causes swelling and discoloration of the face and neck.
The superior vena cava is a large vein that carries blood from the head, neck and upper chest to the heart. Superior vena cava syndrome occurs when an obstruction develops in this vein.
Obstruction often results from tumor pressure on the vein due to lung or breast cancer. However, there may be other causes, such as tuberculosis or swelling of the thyroid gland.
Symptoms of superior vena cava syndrome usually develop gradually. These may include the following:
- dyspnea;
- cough;
- difficulty swallowing;
- headache;
- dizziness.
In this condition, people need to urgently seek help from a doctor.
Prevent so you don't die
To prevent swelling of the brain, the following safety measures should be observed:
- give up bad habits: smoking and alcohol abuse;
- avoid head injuries (fasten a seat belt in a car, wear a helmet when riding a bicycle or rollerblading, etc.);
- monitor blood pressure indicators;
- take measures to prevent infectious diseases of the brain;
- normalize weight and eat right;
- promptly treat diseases associated with disorders of the circulatory system.
Following these simple rules will help reduce the risk of a dangerous pathology.
Cardiovascular diseases
In cardiovascular diseases, blood pressure increases due to increased cardiac output or increased total peripheral vascular resistance. Features of arterial hypertension in cardiovascular diseases:
- The headache is paroxysmal, the pain occurs when the pressure increases, and its intensity decreases when it decreases;
- With heart failure, swelling of the legs periodically occurs, most often in the evenings; in the morning the swelling goes away. The face with cardiac edema usually does not swell;
- Blood pressure is increased due to systolic (upper) pressure;
- Pain in the heart, feeling of constriction, palpitations;
- The swelling does not hurt, it is elastic to the touch, a hole remains at the place of finger pressure, which disappears within a few seconds;
- Minor subcutaneous hemorrhages may occur;
- There is no change in the amount or composition of urine;
- A severe complication of cardiovascular disease is pulmonary edema, which is accompanied by shortness of breath, palpitations, chest pain and fear of death. In case of pulmonary edema, you should immediately call an ambulance, give the patient a comfortable sitting position (orthopnea with legs down), while tourniquets can (and even should) be applied to the leg area to reduce the flow of blood into the upper torso.
The patient's condition is changeable - the state of health can change dramatically during the day under the influence of emotional or physical stress, drinking coffee, alcohol, or smoking.
For the treatment of cardiovascular diseases, beta blockers, calcium channel blockers, antiarrhythmic drugs, and diuretics are prescribed.
Treatment
With minor concussions, there are cases where the symptoms went away spontaneously without medical intervention. Treatment for the condition is determined by the doctor based on the causes of the swelling and its symptoms.
Most often, treatment is aimed at normalizing oxygen access to the affected parts of the brain. Typically, preparative and surgical treatments are used for this. The following treatment methods are commonly used:
- Oxygen therapy is aimed at improving brain oxygen supply;
- hypothermia is associated with a decrease in body temperature to relieve edema;
- medications are selected depending on the causes of edema;
- Intracranial pressure is reduced by a ventriculostomy procedure, which involves draining excess fluid through a catheter.
During surgery, the cause of the swelling can be identified and eliminated. So, if the manifestation was caused by a tumor, it is removed surgically. If the pathology was caused by damage to a blood vessel, it is restored.
Sometimes, with the permission of a doctor, traditional methods of treating edema are used. For example, a decoction of white mistletoe helps with the development of tumors. To prepare the solution, take about 3 grams of plant flowers per glass of milk.
Propolis tincture is effective in treating the disease - there are 10 grams of alcohol per gram of substance. Propolis is dissolved, and then the mixture is filtered. Use the solution three times a day before meals.
Causes
The most common manifestations of edema include:
- bruises, injuries, suffocation;
- injuries that form under the dura mater of the brain without breaking the shell of the skull;
- tumors;
- hemorrhages after a stroke;
- infectious diseases;
- allergies;
- poisoning;
- in newborns – umbilical cord strangulation, birth injuries.
Almost always, cerebral edema occurs after head surgery and operations with spinal anesthesia. Significant blood loss with a decrease in pressure can also affect the condition.
Forecast and consequences
Even if timely therapy was carried out. Doctors do not guarantee a favorable outcome for the patient.
Depending on the severity of the lesion, various subsequent symptoms may appear after treatment. These include:
- pathologies of sleep and wakefulness;
- headache;
- absent-mindedness;
- neuralgic abnormalities;
- depression;
- deviations in the physical condition of the body;
- communication disorders.
After surgery, the patient may also experience asymmetrical distortion of the face, strabismus, motor impairment and manifestations of epilepsy.
Possible residual factors after the disease are influenced by the timeliness and correctness of the therapy initiated - due to edematous pressure on the brain centers, many body systems may be affected. In addition, in the case of hypoxia, neuronal cell death occurs. This can cause failure of analytical centers and even paralysis of the entire body. In critical cases, a coma is noted.
In the absence of adequate treatment, cerebral edema can cause irreversible consequences that adversely affect the functioning of the entire body, including death. That is why, if any symptoms of the disease occur, it is important to immediately seek medical help to avoid problems.
Source: RusMeds.com
One of the causes of secondary brain damage that develops after TBI is edema. Morphological manifestations of impaired circulation of tissue fluid in various pathologies have long been known to pathologists.
Since 1967, after the first publication by J. Klatzo, it has been customary to distinguish between vasogenic and cytotoxic types of cerebral edema. According to V. Wahl et al. For the development of vasogenic cerebral edema, three conditions are necessary: 1) increased capillary permeability; 2) prolonged increased intravascular pressure, which promotes the release of plasma beyond the capillary; 3) distribution of fluid throughout the intercellular spaces. All these conditions are created during the destruction of blood vessels at the site of contusion.
Vasogenic cerebral edema is always more pronounced in the white matter than in the gray matter. An explanation for this was given in 1936. A morphological study conducted by L. Jaburek showed that the white matter consists of parallel bundles of nerve fibers with wide intercellular spaces, which favors extracellular fluid accumulation. Whereas in the gray matter, with a high density of cells and many intercellular contacts, the intercellular spaces are narrow.
The cytotoxic type of cerebral edema is characterized by swelling of all cellular elements of endothelial cells, glia and neurons, i.e. intracellular accumulation of excess fluid. The intercellular space in these cases is reduced. The famous pathophysiologist R. Fishman proposed replacing the term “cytotoxic” edema with “cellular” edema, because Changes in brain tissue detected by electron microscopy are not always the result of toxic effects, but may reflect different phases of normal metabolic processes. However, due to a certain conservatism in medicine known and justified by life itself, this proposal did not find wide support.
Currently, after the introduction of modern methods of intravital brain imaging into clinical practice, in the English-language literature the term brain swelling often refers to an increase in brain volume, regardless of the reason that led to this.
In terms of prevalence, post-traumatic cerebral edema can be: a) local, usually around the site of injury (contusion, crush injury, hematoma, etc.); b) diffuse, involving the entire one hemisphere of the brain; c) diffuse, spreading to both hemispheres.
Focal brain damage is usually accompanied by perifocal cerebral edema. According to CT and MRI of the brain, the first signs of perifocal cerebral edema are detected 24-48 hours after injury and reach a maximum in the time interval from the fourth to the eighth day after TBI. The presence of perifocal edema around an intracerebral hematoma is a poor prognostic factor. Thus, according to L. Marshall, death was noted in 32% of victims with intracerebral hematoma. In all these cases, severe perifocal cerebral edema was detected on CT.
Perifocal edema is a consequence of physical destruction of brain tissue, which disrupts the integrity of the blood-brain barrier
Disruption of the blood-brain barrier is one of the most common consequences of severe brain injury. The degree of disruption of the permeability of the blood-brain barrier correlates with the severity of TBI and indicates the possibility of developing secondary brain damage, such as increased intracranial pressure, interstitial cerebral edema, and the entry into the brain of substances that have a toxic effect on neurons.
Various mechanisms of damage to the blood-brain barrier have been described, for example, physical destruction of the vessel walls and direct leakage of fluid from the capillary lumen into the pericapillary space.
Increased capillary permeability has also been described in cases where the integrity of the vessel wall is preserved. For example, vasogenic edema, as pathophysiologists believe, can develop when the anatomical integrity of the vessel walls. Thus, increased capillary permeability that continues for at least 24 hours contributes to the development of vasogenic edema. In these cases, widening of interendothelial gaps, increased pinocytosis in the cytoplasm of endothelial cells, and changes in the properties of the cell membrane were observed.
Increased osmotic pressure also contributes to the release of fluid from the vascular bed. At the site of brain contusion, the concentration of sodium ions increases by more than 100% compared to normal, while the concentration of potassium ions drops by 70% or more. An increase in sodium concentration in necrotic tissue, accompanied by an increase in chloride ions, attracts water to this area.
A number of studies have shown a correlation between the severity of perifocal edema and the presence of leukocyte infiltrate in this area.
As R. Vaz et al. showed, cytotoxic edema can also develop in the perifocal zone. Based on an electron microscopic examination of the vessels of the pericontus zone, surgically removed during neurosurgical operations in 11 patients with severe brain contusions, the authors came to the conclusion that primary edema of endothelial cells is the leading link in the pathophysiology of post-traumatic cerebral edema. The cause of intracellular edema of endothelial cells is their increased permeability to ions and water. In turn, the reason for the increase in the permeability of cell membranes is their deformation that occurs during brain injury. At least in an experiment on cell culture, mechanical tension of endothelial cells of brain vessels, cardiomyocyte cell cultures, leads to an increase in the permeability of the membranes of these cells for calcium ions.
Focal cerebral edema that occurs after acute arterial occlusion initially develops according to the cytotoxic type. In these cases, with intact capillary walls, perifocal ischemia and anoxia lead to insufficiency of the ATP-dependent sodium pump of the cells. As a consequence of this, there is an active entry of sodium ions into the cytoplasm of the cell along with chlorine ions. Following sodium chloride, water is also attracted into the cell. Continued arterial occlusion leads to cerebral infarction, disruption of the blood-brain barrier, and secondary vasogenic edema, which may appear hours to days after the onset of cytotoxic edema.
Diffuse enlargement of one cerebral hemisphere is often observed after removal of an ipsilateral acute subdural hematoma. There is no clear explanation for this fact. It is believed, based on experimental data, that this almost instantaneous process is not a consequence of cerebral edema (the development of which requires considerable time, on average, at least 24 hours). Primary vasodilation with subsequent disruption of the integrity of the blood-brain barrier and secondary development of cerebral edema seems most likely.
Diffuse increases in the volume of both hemispheres of the brain are found primarily in children and adolescents and are believed to result from vasodilation resulting from loss or reduction of vasomotor tone. It has been shown that acute hyperemia alone can lead to an initial increase in brain volume in children and adolescents with subsequent development of edema. In adult patients, post-traumatic cerebral hyperemia is often secondary, developing after a temporary decrease in cerebral blood flow and, as D. Lang et al. believes, has more severe consequences than in children.
As CT studies by A. Marmarou have shown, with focal brain lesions, an increase in brain volume is primarily the result of overhydration, intra- and extracellular edema. At the same time, in the first hours after injury, the blood supply to the brain is significantly reduced. In some cases, perifocal cerebral edema can spread to the entire hemisphere, and possibly to both hemispheres.
Intravital visualization of the dynamics of brain volume increase has become possible using CT and MRI of the brain. Whereas the changes detected at autopsy reflect only the final phase of this complex process.
S.Yu.Kasumova
Source: medbe.ru
How can you suspect cerebral edema: main symptoms
Suspecting the onset of cerebral edema is a very difficult clinical task. After all, it is almost impossible to differentiate its first signs and manifestations of the underlying disease.
The onset of edema can only be assumed if the absence of progression of the primary pathology in the patient is precisely proven. The complication manifests itself as an increase in neurological deficit and the appearance of seizures against the background of a dynamic deterioration of consciousness up to a coma.
Subjective sensations of a person, or Complaints during the development of cerebral edema
As cerebral edema increases, the patient’s first complaints will be:
- bursting headache;
- constant nausea and repeated vomiting, which does not bring relief and is not associated with food intake;
- drowsiness (the most unfavorable prognostic sign);
- seizures that have not previously been observed. At first they are clonic or tonic-clonic in nature and end quite favorably. But as the edema further develops, the frequency of seizures increases, intracranial pressure increases and depression of consciousness progresses;
- photophobia.
All these symptoms are caused by increasing cerebrospinal fluid hypertension and relate to cerebral manifestations of neurological pathology, which are not strictly specific to cerebral edema.
Signs of cerebral edema detected during an objective examination
The clinical picture of cerebral edema manifests itself as an increase in the severity of local symptoms and an increase in general cerebral symptoms due to its spread to functionally significant parts of the brain (thalamus, hypothalamus, stem structures, etc.) or its generalization. When examining a patient, a neurologist will identify three groups of signs of the formation of cerebral edema:
- symptoms indicating increased cerebrospinal fluid pressure in the cranial cavity;
- worsening of focal and widespread rostrocaudal increase in neurological symptoms;
- signs of brain stem dislocation.
With increasing cerebrospinal fluid hypertension, meningeal symptoms first appear (stiff neck, hyperesthesia, Kernig and Brudzinski's symptoms), then tendon reflexes increase and their reflexogenic zone expands.
Oculomotor disorders are added: limited movement of the eyeballs, weakened convergence, diplopia, body temperature rises. Convulsive syndrome progresses.
The second group of symptoms is characterized by an increase in focal neurological deficit (paresis, speech disorders, etc.), as well as the emergence of signs of the spread of the pathological process from the cerebral cortex to the subcortical, and then stem structures.
Edema of the cerebral hemispheres is characterized by depression of higher nervous activity and consciousness. Generalized convulsions develop. When the subcortex is involved (basal ganglia, hypothalamus, limbic system, etc.), hyperkinesis, psychomotor agitation, grasping and protective reflexes occur, and the time of the tonic phase of epileptic seizures is prolonged.
Signs of herniation of brain structures that appear against the background of their dislocation are divided into upper (when the midbrain is displaced into the notch of the tentorium of the cerebellum) and lower (when the brain stem is pinched in the foramen magnum).
Symptoms of midbrain damage are:
- depression of consciousness to a comatose state;
- anisocoria (pupils of different sizes);
- mydriasis (dilated pupils);
- strabismus, or squint;
- spastic unilateral paralysis;
- partial cramps in the limbs.
Bulbar syndrome (dysarthria, dysphagia, dysphonia), which is considered the first sign of displacement of the medulla oblongata and indicates a critical increase in pressure inside the skull, is accompanied by the following symptoms:
- a sharp drop in blood pressure,
- bradycardia,
- decreased muscle tone and body temperature,
- lack of tendon reflexes,
- maximum dilation of the pupils on both sides in the absence of photoreaction,
- immobility of the eyeballs,
- the appearance of pathological breathing, which turns into apnea (lack of breathing).
Manifestation mechanism
Cerebral edema is the body’s reaction to severe damage that affects blood microcirculation in the organ. Due to metabolic insufficiency, the transport of oxygen and, accordingly, the evacuation of carbon dioxide through the arteries are disrupted. Other abnormalities that can cause the disease are:
- disturbances of electrolyte, energy and protein metabolism;
- deviations of the blood environment reaction from the norm;
- changes in plasma protein or electrolyte pressure in the brain.
Due to the disruption of transport functions, tissue swelling occurs, which provokes the release of blood cells through the membranes and the attachment of water molecules to the proteins of the nervous system. This condition can impair important brain centers such as breathing and thermoregulation.
It is often difficult to establish the presence of this condition due to its masking behind other symptomatic manifestations. Brain swelling is most likely if the clinical symptoms of the disease do not progress, but the neuralgic symptoms intensify.
Symptoms and signs
In order to make a diagnosis, as well as help a sick person in a timely manner, it is necessary to know the symptoms and various signs of cerebral edema. This disease develops slowly and gradually due to any complications of a particular disease or injury.
At the first stage, when the disease is just beginning to manifest itself, you can note the following symptoms:
- Significant headaches that may be accompanied by vomiting;
- Constant nausea;
- Restless state, the ability to navigate in time and space is impaired. This is due to the fact that swelling affects the nervous system;
- Constant drowsiness that does not go away even after a good rest;
- High blood pressure, regular breathing failure, arrhythmia;
- Constricted pupils.
As the disease progresses, the patient notices more serious signs. Depending on how long the swelling progresses, its symptoms can be divided into three groups.
The first is neurological symptoms that arise due to swelling of the cerebral cortex (the subarachnoid lobes may also be affected). This includes signs such as convulsions, a general agitated state of the body, increased blood pressure and muscle tone.
If there is a sudden increase in the level of intracranial pressure, then the patient will have the following symptoms: vomiting and constant nausea, significant headaches, the movement of the headballs is disrupted, the general condition of the person changes from depressed to highly agitated, and severe convulsions appear. Cramps, by the way, can occur both in the limbs and in the facial muscles, and these are the most important symptoms of such a disorder. They can be of different durations.
With the so-called progressive edema, due to which pinching and severe displacement of brain structures occurs in the head. Also, a person develops a high temperature (40 degrees or more), which cannot be brought down, the pupils do not react to light, very strong convulsions and unilateral paralysis (paresis) occur. The heart rhythm is disturbed, pain reflexes, as well as tendon reflexes, are completely absent. The patient is in a comatose state.