In a stage 4 coma, the chances of survival are negligible. If within 20-30 minutes during resuscitation measures it was possible to achieve restoration of spontaneous breathing, spinal or brainstem reflexes, electrical impulses of the brain, then stabilization of such a patient is possible.
The severe unstable condition of a patient with a 3rd degree coma can progress until a 4th degree coma develops. This is a transcendental state, which is characterized by deep depression of all body functions. Life support is possible with the help of artificial respiration devices, parenteral nutrition and medications
Causes
Brain depression with profound loss of consciousness can occur in a person due to various provoking factors - both external and internal. Main causes of coma:
- metabolic - various poisonings by metabolic products or chemical compounds;
- organic - due to the destruction of areas of the cortex due to diseases of the heart, pulmonary system, urinary structures, as well as due to brain injuries.
Internal negative factors can be:
- hypoxia – low concentration of oxygen molecules in human brain tissue;
- a large number of acetone molecules in the bloodstream - for diabetes, or ammonia for liver damage;
- addiction;
- alcoholism;
- tumors.
It is not always possible to immediately understand against the background of what severe disorder the coma arose. This makes it difficult to select the optimal treatment regimen. Modern diagnostic tests come to the rescue. If the cause of the coma cannot be determined, then the treatment strategy for a person is symptomatic.
What is an induced coma?
From a medical point of view, this is a temporary immersion of the patient in an unconscious state. The activity of the cerebral cortex and subcortex is inhibited and all reflex functions are completely disabled.
Artificial coma is used only in the most extreme cases. That is, when there is no other way to protect the patient’s body from irreversible brain changes that threaten his life. This happens with swelling of brain tissue and compression effects on them, as well as with hemorrhage or bleeding accompanied by severe traumatic brain injuries or pathologies of cerebral vessels.
An artificial coma can be used to replace general anesthesia in cases of emergency surgery of a large volume or directly on the brain.
Symptoms
First of all, what a person feels in a coma is the absolute lack of possibility of contact with the environment and relatives/acquaintances. In fact, an unconscious state, characterized by the inability to perform mental activity, will be a consequence of damage to the cerebral cortex.
Other signs of coma directly depend on the cause of its development. Thus, hyperthermia is a prolonged increase in a person’s temperature, which is inherent in overheating. Whereas in case of poisoning with alcohol or sleeping pills, a decrease in temperature will be characteristic.
Lack of spontaneous breathing is described as coma in car accidents. Bacterial infections, as well as brain tumors or kidney filtration failure are disorders in which breathing becomes shallow and slow.
Changes in the cardiovascular system:
- a decrease in the frequency of contractions of the heart chambers directly indicates their damage;
- tachycardia – increased rhythm, especially in combination with high blood pressure numbers – intracranial hypertension;
- if the pressure decreases, it is necessary to exclude diabetic coma and drug poisoning, as well as internal bleeding.
The color of the skin can also tell specialists a lot - cherry-red develops due to carbon monoxide poisoning, and cyanosis - due to suffocation. Bright pallor of the skin indicates previous massive blood loss.
However, against the background of pathological inhibition of processes in brain cells, the reaction of the pupils to light in humans is different - in case of metabolic disorders it remains intact, but in case of strokes or tumor wedging into the brain stem, it is absent.
Information about whether a person in a coma can hear or not is contradictory. However, the presence of various sounds from the patient is usually considered a favorable symptom.
Brain death
Based on data indicating the cessation of functioning of the brain and its stem, brain death is confirmed by a council of doctors. This concept is legally enshrined and defines the death of a person, despite the presence of cardiac activity and breathing supported artificially.
Subscribe to our Yandex Zen channel!
Life support systems have a high cost, so at a certain stage the question is raised about disconnecting the patient from life support devices. This creates the possibility of obtaining donor organs for transplantation.
The following criteria for brain death have been defined:
- Damage to the brain structure. There must be a history of trauma, after which it is impossible to definitely restore its structure. Diagnosis is carried out using CT.
- A full examination confirms that the depressed state is not caused by intoxication.
- Body temperature 32°C or more. A hypothermic state can lead to a decrease in electrical activity on the EEG, but when the temperature rises, the indicators are restored.
- The observation period for injuries ranges from 6 to 24 hours; after drug intoxication and in children, the observation time is increased.
- Does not react with movement to severe pain, there are no reflex reactions to pain in the form of rapid breathing or heartbeat.
- Apnea is confirmed by a special test. Ventilation of the lungs is carried out with pure humidified oxygen or mixed with carbon dioxide for 10 minutes. After this, its feed is reduced. Spontaneous breathing should return within 10 minutes. If this does not happen, brain death is diagnosed.
- Absence of corneal reflexes: no eye movement during cold testing, fixed pupils, corneal, pharyngeal, gag reflexes, blinking, swallowing disappear.
- EEG in the form of an isoelectric line.
- According to angiography, there is no blood flow. During ophthalmoscopy, glued red blood cells are found in the retina - a sign of stopping blood flow.
Types and classification
In medical practice, doctors distinguish up to 15 degrees of damage - from complete consciousness to its absolute absence. Meanwhile, cerebral coma is most often considered to be of the following types:
- severe - the bangs do not open their eyes and do not respond to external stimuli;
- medium - there is no consciousness, but a person can spontaneously open his eyes slightly or utter individual sounds, twitch his limbs;
- mild - a comatose state in which a person opens his eyes in response to a loudly spoken command, can answer questions briefly, but his speech is incoherent and confused.
If a person is put into an artificial coma by doctors, the degree of its severity varies depending on the goals of the treatment tactics.
Doctors consider other types of suppression of mental activity based on why people in a coma are unable to have contact with the outside world:
- traumatic - with cranial lesions;
- apoplectic - the result of a hemorrhagic stroke, hemorrhage into the brain structure;
- meningeal – the result of meningitis;
- epileptic – a complication of severe status epilepticus;
- tumor – pathological pressure on intracranial structures;
- endocrine – for dysfunction of the thyroid/pancreas;
- toxic – decompensation of hepatocytes, renal glomeruli.
In general, 3 parameters are assessed in a person in a coma - speech, movement and the ability to open the eyes. Directly depending on the assessment of the level of consciousness, therapeutic measures are selected.
How and why coma occurs
Going into deep sleep is a consequence of partial brain dysfunction after an apoplexy.
The main symptoms are the absence of consciousness, reflexes and any reaction to the external environment. There are many factors that seriously disrupt the functioning of brain cells and lead a person to incapacity with loss of consciousness. These include:
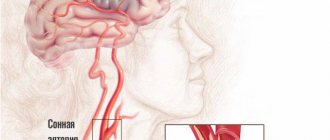
- cerebral hemorrhage;
- ischemia – lack of blood supply to neurons and, as a result, the death of some of them;
- swelling of brain cells due to hypoxia or mechanical effects on the cerebral cortex;
- depletion of the walls of blood vessels in the head;
- severe poisoning of the body;
- blood diseases and angiopathy;
- acute lack of vitamins.
Compared with ischemic stroke, hemorrhagic cerebral stroke causes coma in the majority of all cases. Moreover, the severity of symptoms in the second variant is the greatest, since a fairly impressive part of the neurons responsible for innate reflexes and body systems are affected.
In this case, the following gradually advancing symptoms can be observed:
- Dizziness.
- Decreased visual acuity
- Increasing drowsiness.
- Dullness of consciousness, slowing of thought processes.
- Numbness of the limbs.
- Loss of coordination.
Unlike ischemic damage to brain cells, with cerebral hemorrhage, coma after a stroke develops rapidly. In this case, the person has less chance of recovery than in the first case, and the prognosis is extremely disappointing. The result of brain cell necrosis is a separate topic for discussion.
Diagnostics
The task of a specialist when a person is suspected of having a coma is to find out its cause, as well as differentiate it from other pathological conditions with a similar clinical picture. Of great importance is the collection of information from relatives - what preceded the depression of brain activity, what measures were taken, a list of chronic diseases.
Thus, cerebral coma in young people is a common result of poisoning with sleeping pills, narcotic drugs or alcoholic beverages. Whereas in old age it is the result of diabetes, hyperthyroidism or stroke.
The next stage of diagnosis is examination of a person in a coma:
- reflex assessment;
- reaction of the pupils to light directed into the eyes;
- speech assessment;
- following the doctor's commands - conscious actions during a coma are, as a rule, impossible.
Laboratory and instrumental activities:
- CT;
- MRI;
- electroencephalography;
- radiography;
- biochemical and general blood tests;
- urine tests;
- Ultrasound of internal organs.
Only after a thorough analysis of all diagnostic information will a specialist be able to answer the question of how long a person can be in a coma, as well as what actions should be taken first in a coma.
Neurological comas
They are directly related to damage to the central nervous system. These include:
- coma that occurs during strokes;
- apoplectiform coma;
- epileptic coma;
- coma caused by trauma, such as traumatic brain injury;
- a comatose state caused by inflammatory processes, as well as benign and malignant neoplasms in the brain and its membranes.
Treatment tactics
When a person is in a coma, specialists carry out therapeutic measures in two directions - maintaining the maximum possible vital functions, as well as eliminating the main cause of such a pathological condition.
Of course, when a person is in a coma, he is not able to tell the doctor what he feels, where it hurts. Therefore, all activities will be carried out taking into account known information and inspection results:
- maintaining respiratory activity - preventing tongue retraction, applying an oxygen mask if necessary;
- correction of blood circulation - administration of cardiovascular medications;
- in the intensive care unit, according to individual indications, a person is connected to artificial life support devices;
- for seizures - administration of anticonvulsant drugs;
- for hyperthermia - measures to reduce temperature;
- in case of poisoning – removal of toxins and poisons.
In the future, treatment tactics will consist of feeding a person in a coma, preventing the appearance of bedsores, and correcting pressure parameters, including intracranial pressure, until consciousness returns. If necessary, brain tumors, bone fragments, and areas of aneurysm rupture are removed using surgical methods.
Coming out of a coma
No doctor can give an exact answer to how long the patient will remain in a coma and whether he will come out of this state. At the same time, the chances of emerging from a mild and moderate coma are relatively high, but this process is very long and gradual. Coming out of a coma stage often includes the following:
- opening the eyes under the influence of stimuli;
- fixation of gaze;
- recognition of loved ones;
- understanding spoken speech, following oral commands;
- speech restoration;
- restoration of formally clear consciousness.
Consequences of coma
Since the brain is affected, even after emerging from a coma, many vital functions may not be restored. The vegetative state after a coma, the prognosis of the consequences of which in many cases is disappointing, can drag on for many years. In this state, a person only regains wakefulness, his heart and lungs function normally, but all cognitive functions are lost, there is no movement, speech or reaction to verbal stimuli. The result is often death from infections and bedsores.
Forecast
Bringing a person out of a coma is, of course, not an easy task and can only be done by highly qualified specialists who work in specialized neurological centers. The prognosis depends entirely on the severity of the vegetative state - with mild precoma due to a rise in glucose, recovery occurs in full. Whereas in a coma due to a massive hemorrhagic stroke or a car accident, the person is unlikely to recover. However, doctors in intensive care perform all the required actions.
In addition, relatives are told how to bring the patient out of a coma - talk, read aloud their favorite books, tell important news about the family. This often contributes to the return of consciousness to the person. After a coma, he does not always sensibly assess his well-being and the disorder that happened to him. Therefore, he is under the supervision of doctors.
Avoiding coma allows timely treatment of chronic diseases, as well as compliance with all doctor’s recommendations.
Signs of coma during stroke
Symptoms increase gradually, and the signs of coma during a stroke will depend on the stage of the pathological process. To diagnose the problems that have arisen, neurologists and resuscitators recommend performing a simple test, during which the degree of stroke complications is assessed by checking the patient:
- presence of paralysis;
- speech disorders;
- lack of ability to assess what is happening;
- memory impairment (complete or partial);
- confusion.
If during an ischemic stroke the symptoms progress gradually, then hemorrhagic coma occurs within a few minutes. With a hemorrhagic lesion, the victim almost immediately loses consciousness and suppresses protective reflexes.
Traditional methods of treating alcoholic coma
Alcoholic coma is a serious problem that is very difficult to cope with at home, so you should not neglect medical help. Despite this, some manage, using folk methods passed down from generation to generation since ancient times, to avoid a serious condition. They are most suitable for restoring the body after a severe illness. For first aid, medicinal herbs are used:
- rosehip, which helps cleanse liver cells and blood vessels;
- juice from cabbage leaves will help reduce pain in the liver area, and the vitamins contained inside will replenish those lost by the victim’s body;
- Lingonberries and currants are used by healers in all cases associated with intoxication, because a huge amount of vitamins inside will start the liver and restore lost cells;
- cranberry, which equally has a healing effect, helps liver cells recover, for which you should grind one teaspoon of cranberries with honey and consume before eating;
- black radish helps cleanse liver cells, like previous herbal products, for which you should mix it with honey and take two tablespoons twice a day;
- benefits of citrus fruits. Their benefits in restoring liver cells are invaluable and remove harmful substances.
First aid for alcoholic coma
At the slightest suspicion of alcoholic coma, it is recommended to seek emergency care to avoid the patient’s transition from the state of the first degree of alcoholic coma to the second. Of course, the first degree of alcoholic coma sometimes passes without dangerous consequences, but it’s not worth taking risks with this. If the victim does not respond to stimuli for more than 7 hours, calling an ambulance is mandatory. The slightest delay can cost the patient his life.
If emergency assistance for an alcoholic coma has already been called, do not relax, because first aid can save a life. You can independently begin the procedure of cleansing the patient’s body. The biggest danger facing a drinker is respiratory arrest, which is why you should follow the following algorithm of actions:
- To begin with, you should put the victim on his left side, adjust his left upper limb, stretching it, and bend his lower limb at the knee.
- The next step is to clear the vomit from your mouth with your finger, on which you can first wrap a piece of cloth.
- If you have a syringe in the house, you can use it to suction out secretions that have accumulated in the oral cavity. If it is not there, then you should leave it to the doctors.
- The danger of coma is that the victim's tongue may stick into the throat, blocking breathing. Due to the fact that the jaw muscles are cramped, it is extremely difficult to open them, but by pressing on the base, you can open your mouth slightly and extend your jaw.
- If the drinker is having convulsions, then for his safety it is recommended to hold his limbs and body.
Possible complications and consequences
Hypoglycemic coma is often accompanied by the development of complications - both current and long-term. Current complications arise parallel to the hypoglycemic state and accompany it. These may be myocardial infarction, stroke, aphasia.
Long-term complications of hypoglycemic coma appear several days or even weeks after the acute condition. The most common complications are encephalopathy, parkinsonism, epilepsy.
One of the complications of hypoglycemic coma is myocardial infarction
Therapy
After transporting the patient to a medical facility, doctors from the intensive care unit will take charge of his health. The first actions will be aimed at ensuring breathing and blood circulation using hospital devices. After this, the patient awaits an urgent examination in order to make an accurate diagnosis and confirm the coma.
Diagnosis is made by taking an anamnesis. If the victim remains unconscious, his relatives may be called in to help. Doctors will also conduct a physical and neurological examination to assess the condition of the body. If anyone is suspected, their stage will be assessed using the Glasgow scale or another relevant one at that time. In addition, you will need to conduct laboratory tests with the study of blood and urine, neuroimaging and measure intracranial pressure. If the diagnosis remains unclear, an EEG or lumbar puncture may be prescribed.
The basis of treatment is various medications aimed at eliminating the root cause of coma. Doctors have to be very careful in their choice, since a coma makes it impossible to use some drugs. The patient’s survival will depend only on correctly selected medications.
Types of medications:
- anticonvulsants;
- sedatives;
- antiemetics;
- antipyretics;
- antibiotics;
- vitamin B;
- glucose.
If there is a suspicion of poisoning by low-quality food or medications, the patient may also be prescribed gastric lavage. If there are tumors or some other damage to the brain, surgery is often required.
The sooner the doctor begins treatment, the higher the chances of a positive outcome.
Rehabilitation
Recovery procedures after a stroke begin when a person emerges from a comatose state with the involvement of psychologists, neurospeech therapists, and physiotherapists. The main goals of the process are considered to be the normalization of movements, sensitivity, memory, speech, intelligence, and emotional background.
Patients are prescribed massage, exercise therapy, physiotherapy, articulation exercises, and drug therapy. Providing quality care is a must.
Compliance with the recommended measures allows you to achieve an hourly restoration of lost functions.
Caring for a patient in a coma
It is never known in advance how long it will take to care for a patient who has fallen into a comatose state. Therefore, it is very important to take care of him. A special role is given to the nutrition that the patient receives through a tube. An excellent option is baby food in liquid form or products processed using a blender. In addition, in order to avoid the appearance of wounds, bedsores, the patient must be treated every day with a special solution or soap, comb his hair, clean the oral cavity with wet wipes, it is also important to change the patient’s position and turn him over. All these functions are performed by specially trained medical personnel. If necessary, the patient can be connected to artificial ventilation, a special monitor that will display the body’s main vital signs - pulse, blood pressure. A patient in a coma is usually prescribed antibiotics to protect him from infections. It is also very important that the patient’s body receives all the vitamins and microelements necessary for the body’s functioning.
The first symptoms of an alcoholic coma
If a person who has taken a certain dose of alcohol exhibits the following symptoms, then we can safely say that the person is developing an alcoholic coma:
- dizziness;
- disorientation;
- inability to distinguish familiar objects;
- pale complexion;
- muscle cramps;
- narrow pupils.
In this case, it is important to provide assistance in a timely manner and, most importantly, appropriate and correct. It is worth starting by clearing the stomach by inducing vomiting, giving the victim to drink about seven tablets of activated charcoal and laying him on his side. These manipulations will reduce the risk of alcoholic coma. You shouldn’t wake him up, because healthy sleep is another important step towards recovery. A hangover, of course, cannot be avoided, as can a severe headache.
Diarrhea, gagging and heartburn may occur. If nothing alarming happens, then there is no reason to worry, and the victim can recover at home. To speed up recovery, it is recommended to ensure silence and dim light around the patient. It is worth drinking water or other liquid products more often. If the victim is in pain, then taking painkillers is not prohibited.
Prevention
To prevent hypoglycemia, you should carefully adhere to the prescribed dosage of insulin or hypoglycemic drugs. Patients should be informed about the need to eat after an insulin injection. Patients following a daily routine and diet help reduce the risk of a drop in blood glucose concentration.
Patients suffering from diabetes and their loved ones should know the signs of a hypoglycemic state. When these appear, the patient urgently needs to drink warm sweet tea, eat a piece of sugar, candy or a piece of white bread.
Video from YouTube on the topic of the article: