Updated: March 4, 2020, at 16:15
Diarrhea with cholecystitis is a common occurrence. Mostly people over 40 years old experience this pathology.
Also at risk are patients who are overweight. Feces during cholecystitis are one of the main indicators of the course of the disease.
Some doctors believe that diarrhea due to cholecystitis is not a completely correct interpretation of a disorder of the gastrointestinal tract.
It is believed that inflammation of the gallbladder is more often accompanied by constipation than diarrhea. Despite the disagreement among gastroenterologists, loose stools due to cholecystitis cannot be ignored.
What do changes in stool characteristics indicate?
You can judge health problems or nutritional costs by the following characteristics of stool:
- frequency of visiting the toilet. Norm: regularly, 1-2 times a day, but at least 1 time in 24-48 hours, without prolonged strong straining, painless. After defecation, the urge disappears, a feeling of comfort and complete bowel movement occurs. External circumstances can increase or inhibit the frequency of the urge to defecate. This is a change in the usual environment, a forced position in bed, the need to use a bedpan, being in the company of other people, etc. Changes: Lack of bowel movements for several days (constipation) or too frequent bowel movements - up to 5 times or more (diarrhea).
- daily amount of feces. Norm: With a mixed diet, the daily amount of feces fluctuates within a fairly wide range and averages 150-400 g. Thus, when eating predominantly plant foods, the amount of feces increases, while in an animal that is poor in “ballast” substances, it decreases. Changes: Significant increase (more than 600 g) or decrease in the amount of feces. Reasons for increasing the amount of feces (polyfecal):
- Consuming large amounts of plant fiber.
- Increased intestinal peristalsis, in which food is poorly absorbed due to its too rapid movement through the intestinal tract.
- Disruption of digestive processes (digestion or absorption of food and water) in the small intestine (malabsorption, enteritis).
- Decreased exocrine function of the pancreas in chronic pancreatitis (insufficient digestion of fats and proteins).
- Insufficient amount of bile entering the intestines (cholecystitis, cholelithiasis).
Reasons for reducing the amount of feces:
- Constipation, in which due to prolonged retention of feces in the large intestine and maximum absorption of water, the volume of feces decreases.
- Reducing the amount of food eaten or predominantly digestible foods in the diet.
- Passing feces and floating in water. Normal: feces should be released easily, and in water it should sink gently to the bottom. Changes: If there is insufficient amount of dietary fiber in food (less than 30 grams per day), feces are released quickly and splash into the water of the toilet.
- If the stool floats, this indicates that it has an increased amount of gas or contains too much undigested fat (malabsorption). Also, stool may float if you eat a lot of fiber.
- If the stool is difficult to wash off with cold water from the walls of the toilet, it means it contains a large amount of undigested fat, which happens with pancreatitis.
- Stool color. Normal: With a mixed diet, the stool is brown. Breastfed babies have golden-yellow or yellow stools. Change in stool color: Dark brown - with a meat diet, constipation, impaired digestion in the stomach, colitis, putrefactive dyspepsia.
- Light brown - with a dairy-vegetable diet, increased intestinal motility.
- Light yellow - indicates too rapid passage of feces through the intestines, which do not have time to change color (diarrhea) or impaired bile secretion (cholecystitis).
- Reddish - when eating beets, when bleeding from the lower intestines, for example. for hemorrhoids, anal fissures, ulcerative colitis.
- Orange – when consuming the vitamin beta-carotene, as well as foods high in beta-carotene (carrots, pumpkin, etc.).
- Green - with a large amount of spinach, lettuce, sorrel in food, with dysbacteriosis, increased intestinal motility.
- Tarry or black - when eating currants, blueberries, as well as bismuth preparations (Vikalin, Vikair, De-Nol); with bleeding from the upper gastrointestinal tract (peptic ulcer, cirrhosis, colon cancer), with ingestion of blood during nosebleeds or pulmonary bleeding.
- Greenish-black - when taking iron supplements.
- Grayish-white stool means that bile is not entering the intestines (bile duct blockage, acute pancreatitis, hepatitis, cirrhosis of the liver).
- Consistency (density) of stool. Normal: shaped and soft. Normally, stool consists of 70% water, 30% from the remains of processed food, dead bacteria and desquamated intestinal cells. Pathology: mushy, dense, liquid, semi-liquid, putty-like. Change in stool consistency. Very dense feces (sheep) - for constipation, spasms and stenosis of the colon.
- Mushy feces - with increased intestinal motility, increased secretion in the intestines during inflammation.
- Ointment-like - for diseases of the pancreas (chronic pancreatitis), a sharp decrease in the flow of bile into the intestines (cholelithiasis, cholecystitis).
- Clay or putty-like feces are gray in color - with a significant amount of undigested fat, which is observed when there is difficulty in the outflow of bile from the liver and gallbladder (hepatitis, blockage of the bile duct).
- Liquid – in case of impaired digestion of food in the small intestine, impaired absorption and accelerated passage of feces.
- Foamy - with fermentative dyspepsia, when fermentation processes in the intestines prevail over all others.
- Loose stools like pea puree - with typhoid fever.
- Liquid, colorless stools like rice water - with cholera.
- When the stool has a liquid consistency and frequent bowel movements, one speaks of diarrhea.
- Liquid-mushy or watery stools can occur with high water consumption.
- Yeasty stool - indicates the presence of yeast and may have the following characteristics: curdled, foamy stools like rising sourdough, may have strings like melted cheese, or have a yeasty odor.
- Shape of feces. Standard: cylindrical, sausage-shaped. The stool should come out continuously, like toothpaste, and be about the length of a banana. Changes: ribbon-shaped or in the form of dense balls (sheep feces) is observed with insufficient daily water intake, as well as spasms or narrowing of the large intestine.
- Smell of feces. Normal: fecal, unpleasant, but not harsh. It is due to the presence of substances in it that are formed as a result of bacterial breakdown of proteins and volatile fatty acids. Depends on the composition of the food and the severity of the processes of fermentation and decay. Meat foods give off a pungent odor, while dairy foods give off a sour odor. If digestion is poor, undigested food simply rots in the intestines or becomes food for pathogenic bacteria. Some bacteria produce hydrogen sulfide, which has a characteristic rotten odor. Changes in stool odor. Sour – for fermentative dyspepsia, which occurs with excessive consumption of carbohydrates (sugar, flour products, fruits, peas, etc.) and fermented drinks, such as kvass.
- Fetid - with impaired pancreatic function (pancreatitis), decreased flow of bile into the intestines (cholecystitis), hypersecretion of the large intestine. Very foul-smelling stool may be due to bacterial overgrowth
- Putrefactive – in case of indigestion in the stomach, putrefactive dyspepsia associated with excessive consumption of protein products that are slowly digested in the intestines, colitis, constipation.
- The smell of rancid oil is due to bacterial decomposition of fats in the intestines.
- Faint odor - with constipation or accelerated evacuation from the small intestine.
- Intestinal gases. Normal: Gases are a natural by-product of the digestion and fermentation of food as it moves through the gastrointestinal tract. During and outside of bowel movements, 0.2-0.5 liters of gas are removed from the intestines of an adult per day. The formation of gas in the intestines occurs as a result of the vital activity of microorganisms inhabiting the intestines. They decompose various nutrients, releasing methane, hydrogen sulfide, hydrogen, and carbon dioxide. The more undigested food enters the colon, the more active the bacteria are and the more gases are produced.
An increase in the amount of gases is normal.
- when eating large amounts of carbohydrates (sugar, baked goods);
- when eating foods that contain a lot of fiber (cabbage, apples, legumes, etc.);
- when consuming foods that stimulate fermentation processes (brown bread, kvass, beer);
- when consuming dairy products if you are lactose intolerant;
- when swallowing large amounts of air while eating and drinking;
- when drinking large amounts of carbonated drinks
An increase in the amount of gases in pathology.
- Enzyme deficiency of the pancreas, in which food digestion is impaired (chronic pancreatitis).
- Intestinal dysbiosis.
- Irritable bowel syndrome.
- Gastritis, peptic ulcer of the stomach and duodenum.
- Chronic liver diseases: cholecystitis, hepatitis, cirrhosis.
- Chronic intestinal diseases – enteritis, colitis
- Malabsorption.
- Celiac disease.
Difficulty in passing gases.
- intestinal obstruction;
- intestinal atony with peritonitis;
- some acute inflammatory processes in the intestines.
- Stool acidity. Normal: with a mixed diet, acidity is 6.8–7.6 pH and is due to the vital activity of the colon microflora. Changes in stool acidity:
- sharply acidic (pH less than 5.5) – with fermentative dyspepsia.
- acidic (pH 5.5 - 6.7) - if the absorption of fatty acids in the small intestine is impaired.
- alkaline (pH 8.0 - 8.5) - with rotting of undigested food proteins and activation of putrefactive microflora with the formation of ammonia and other alkaline substances in the colon, with impaired pancreatic secretion, colitis.
- sharply alkaline (pH more than 8.5) - for putrefactive dyspepsia.
Normally, feces should not contain blood, mucus, pus, or undigested food residues.
Stool becomes discolored due to the disruption of the process of excretion of bilirubin. It is produced by the liver and enters the intestines. There, bilirubin undergoes biochemical changes and turns into stercobilin. It is a pigment substance that makes stool brown. If there is insufficient flow of bile into the gastrointestinal tract, too little stercobilin is formed to color the stool.
Discoloration of feces occurs for three reasons:
- food;
- medications;
- gastrointestinal pathologies.
Very light coloring of the stool can result from eating a significant amount of fatty foods (lard, sour cream, butter, etc.). When the diet is normalized, the stool turns brown again.
Some medications discolor stool:
- antibacterial and anthelmintic agents;
- anti-tuberculosis drugs;
- non-steroidal anti-inflammatory drugs;
- antiepileptic drugs;
- products based on acetylsalicylic acid;
- gout medications;
- oral contraceptives.
If these two reasons are absent, we can say that the stool has lost its natural color due to pathology.
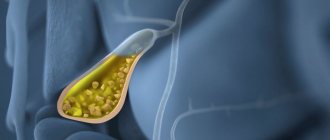
Another reason why stool may become discolored is cholecystitis. This is the name for inflammation of the gallbladder, an organ in which bile produced in the liver accumulates before being released into the intestines. With cholecystitis, a large amount of fat and nitrogenous products are found in the stool, leading to a change in its color to light, sometimes whitish.
Symptoms of gallbladder inflammation: stool discoloration; pain in the right hypochondrium that occurs after eating spicy or fatty foods or drinking alcohol; constant nausea; bitter or metallic taste in the mouth; irritability, insomnia; white coating on the tongue, dry mouth. Cholecystitis can occur in acute and chronic forms - the color of stool changes in both cases. In case of acute cholecystitis, the patient needs urgent surgery. The chronic form is treated conservatively: with medications and diet.
Laboratory diagnostics
To determine the diagnosis, a study of the composition of feces is carried out - a coprogram. Feces contain a large amount of bile acids, which should be excreted no more than 100 mg/g per day. In patients, this figure increases several times.
If the patient is worried about diarrhea with bile, pain in the iliac region of the abdomen, a biochemical blood test is prescribed. Based on its results, an increase in the concentration of liver enzymes ALT, AST, alkaline phosphatase, and bilirubin can be detected. The blood contains high levels of low-density cholesterol, DPA (diphenylamine - an indicator of inflammation), and acute phase proteins. In general clinical analysis, an increased ESR is noted. When the pancreas is involved in the inflammatory process, an increased level of β-amylase, leukocytes, and protein is diagnosed in the urine.
For a comprehensive diagnosis, stool is analyzed for the presence of parasites. The worm can cause blockage of the bile ducts with further inflammation (cholecystitis).
According to individual indications, intestinal colonoscopy is performed to assess the condition of the mucous membranes.
A gastroenterologist also prescribes an ultrasound of the abdominal cavity, during which he examines the gallbladder, liver, and pancreas. Patients are shown duodenal intubation with bile sampling for further biochemical, microscopic and bacteriological examination.
Additional symptoms for cholecystitis
This disease is characterized not only by the appearance of white diarrhea, but also by intense pain in the right hypochondrium.
If the disease has entered an acute stage, then immediate hospitalization is necessary.
Symptoms of the disease: severe pain in the right side, the patient’s temperature rises.
The pulse becomes more frequent.
With the disease in the chronic stage, there is almost no pain, but the color of the skin and whites of the eyes change. The patient experiences bloating and stool changes color to white.
Acholic stool - how dangerous is it?
The color of stool is considered one of the main indicators of the health and normal functioning of the digestive system. Normally, stool is colored brown by bile, which is produced by the liver. Bile in a certain amount is stored in the gallbladder and is released into the duodenum when food passes through it. If for some reason it is not produced or a person’s bile ducts are blocked, acholic stool appears.
IMPORTANT! The natural remedy Nutricomplex restores proper metabolism in 1 month. Read the article{amp}gt;{amp}gt;…
Stool color indicates a person's health status
The feces of a healthy person mainly consist of the remains of food that he consumed in the last two days. Normally, feces are light or dark brown in color, dense in consistency, without a specific odor or foreign impurities. The appearance of feces of an unusual light color is not yet a reason for hasty conclusions and panic. First you need to find out what reasons could have caused this.
The color change could be caused by:
- various physiological processes occurring in the body;
- medications;
- diseases affecting the digestive system.
The most common cause of discolored stool in adults is the abuse of fatty foods. For example, butter or sour cream. Such changes, as a rule, do not bring any discomfort to a person and spontaneously disappear after changing the diet.
ADVICE! Get rid of dark circles around your eyes in 2 weeks. Read the article{amp}gt;{amp}gt;…
https://www.youtube.com/watch?v=https:W5x7nv1ek4Q
Certain medications can also cause stool to lighten. These include antibiotics, antifungals and oral contraceptives. If, in addition to this symptom, the patient experiences an increase in general body temperature and abdominal pain, it is necessary to immediately stop taking the pills and contact your doctor to prescribe therapeutic measures.
Why does diarrhea occur when the gallbladder is inflamed?
This question is asked by all gastroenterologist patients who are faced with this annoying problem.
When the outflow of bile slows down as a result of the inflammatory process, stagnation occurs in the patient's body.
What provokes the appearance of cholecystitis? Let's look at the main reasons:
- Worm infestation. Colonization of the intestines by pathogenic worm parasites is always accompanied by unpleasant consequences. Such inhabitants have a bad effect on the functioning of internal organs, including the gallbladder.
- Pregnancy. We have already said above that the female half of the population is more susceptible to this disease than the male half. The chances of contracting cholecystitis increase significantly during pregnancy. Why does the expectant mother develop diarrhea? It’s all about 2 factors: firstly, the restructuring of hormonal levels, and secondly, the increase in the size of the uterus, which puts pressure on the reservoir organ.
- Infectious process. Usually, when a pathogenic microorganism settles in the gastrointestinal tract, the reservoir organ also suffers. An infection always has a pathological etymology, therefore, its presence in the human body does not pass without leaving a trace.
- Poor nutrition. This is the leading reason explaining the appearance of the inflammatory process of the reservoir organ. When a person eats unbalancedly, that is, consumes insufficient amounts of proteins, carbohydrates, fats and other important and necessary substances, pathological changes occur in his body. Cholecystitis is one of them.
- Changes in intestinal microflora. Some pathogenic microorganisms negatively affect the functioning of the gallbladder. They not only increase the inflammatory process, but also contribute to a more pronounced manifestation of other symptoms of cholecystitis, such as nausea. To eliminate congestion caused by intestinal infection, it is necessary to “even out” the bacterial balance. In this case. the patient will probably be prescribed probiotics.
- Genetic factor. A wise man once said that we are all hostages of our genes. Yes, if there was a person in your family who had problems with the gallbladder, then the chance that you will encounter a similar problem is high.
To reduce the risk of cholecystitis, you need to eat right and lead a healthy lifestyle.
This recommendation may seem difficult to many people, however, it is worth remembering, especially for those who have previously had difficulties with the gallbladder.
First of all, we recommend avoiding fried foods. All dishes that a gastroenterologist's patient should give preference to should be steamed.
Products can also be boiled before use. The patient needs to exclude semi-finished products, fried meat/fish, smoked meats, canned food, and mushrooms from the menu.
Also, the diet is adjusted so that the patient’s menu does not include foods that have a choleretic effect.
It is important that, regardless of the cause of diarrhea in this pathology, its treatment is started in a timely manner.
Why does a person need bile?
This is a very important fluid, without which the human body would not be able to function.
We list its main properties:
- Launching enzymes necessary for the stomach. Stimulation of intestinal peristalsis.
- Neutralization of bilirubin, cholesterol and other dangerous substances in the body.
- Ensuring the digestion process.
- Production of mucus necessary to protect the intestinal walls.
- Softening food.
Without bile it would be impossible to imagine digestion. The mechanism of its entry into the stomach is as follows: first it is produced by the liver, then the bile enters its reservoir organ, from where it enters the stomach, and finally into the intestines.
The opinion that it is impossible to live without a reservoir organ is erroneous.
Many patients suffering from cholecystitis have it removed because treatment with conservative methods does not bring the desired relief.
Without the reservoir organ, the liver cells will not stop synthesizing the yellow liquid, but it will enter the stomach differently.
So, we found out that cholecystitis is characterized by an inflammatory process on the body of the gallbladder.
It can be chronic and acute. Let's consider each pathology separately.
Chronic form
This disease is less dangerous, because the symptoms in the absence of exacerbation of this disease manifest themselves less clearly.
Diarrhea with cholecystitis may be present if the disease has become chronic.
Hepatic colic, in the absence of exacerbation of the disease, rarely occurs if a person eats properly.
It is important to remember that for a gastroenterologist patient, diet should be a key factor in recovery.
If you do not adhere to its rules, you can provoke the growth of an inflammatory focus on the body of the reservoir organ, thereby provoking a complication.
Also, the storage of this pathology contributes to long-term consumption of alcoholic beverages and vitamin deficiency.
Women are more likely to experience such an unpleasant phenomenon as diarrhea due to cholecystitis than men.
The reasons for this phenomenon are as follows:
- Imbalance of diet. When a person does not have a culture of eating, he often encounters such an unpleasant phenomenon as disruption of the digestive system and gastrointestinal tract. This applies primarily to girls who prefer to lose weight through diets. Typically, any significant dietary restrictions lead to insufficient amounts of microelements and vitamins.
- In pregnant women, the gallbladder is compressed, which leads to disruption of its functionality. As a result of this, the organ may become inflamed. The consequences of this are unpleasant.
- Diarrhea due to cholecystitis in reproductively healthy women appears as a result of hormonal changes. Some hormones, including progesterone, have a negative effect on the muscle fibers of the gallbladder, which can cause inflammation.
If you ignore the chronic course of this disease, it may worsen.
Aggravated form
And in most cases, diarrhea due to cholecystitis (exacerbated) occurs in people over 50 years of age.
Sometimes loose stools are the only sign of pathology. Therefore, if it does not disappear on day 3, you should seriously think about your health.
Typically, the pathology is aggravated by the presence of calculi in the reservoir organ - small cholesterol plaques, the movement of which can provoke the appearance of severe colic in the right hypochondrium.
Acute cholecystitis is a phenomenon encountered after eating. When an organ is severely inflamed, a person must intelligently approach the organization of his diet.
It is forbidden to eat spicy, smoked, salty, fatty foods, etc. Otherwise, severe hepatic colic occurs.
What dangerous consequences can an exacerbation of cholecystitis lead to?
- Rupture of the reservoir organ.
- Obstructive jaundice is a yellowing of the whites of the eyes, sclera and epithelium.
- Acute pancreatitis. This pathology is accompanied by inflammation of the tissue surface of the pancreas.
- Peritonitis.
A person whose cholecystitis has worsened will exhibit symptoms such as fever, chills, diarrhea and severe hepatic colic.
It is important that the treatment strategy chosen by the gastroenterologist is aimed not only at relieving the symptoms of cholecystitis, but also at eliminating its root cause.
We will talk about provoking factors below.
Treatment
If, after stopping the medications and changing the diet, white diarrhea does not go away, then the doctor recommends diagnosing it to identify the cause of the pathology.
Usually, if white feces are associated with the use of medications that provoke discoloration of stool, then the color is restored on the second or third day after the drug is discontinued. But it is necessary to assess the risks when treating a patient after discontinuation of the drug.
For cholecystitis, it is recommended to take antispasmodics or use choleretic drugs. Developing dysbiosis stabilizes the intake of enzymes. This could be Linex, Hilak Forte, etc.
Maintaining the amount of fluid lost is important. This patient should drink more water, mineral water, and solutions to prevent water loss (Regidron, Ringer). You should not drink fruit drinks, sweet soda, or compotes.
If severe dehydration occurs due to diarrhea, solutions may be administered through an IV.
The food should be gentle: jelly, stale bread or crackers, rice porridge.
You can use folk recipes, including decoctions of oak bark and blueberries.
Diet
The nutrition of patients in the acute phase of the process must certainly be gentle and fractional. In particularly serious cases, sometimes they even resort to a couple of “hungry” days, during which only liquids are allowed (weak warm tea, rosehip decoction, diluted berry or fruit juices, etc.).
Next, all products are boiled or cooked using a double boiler, and then pureed. Stewing and baking before remission occurs are prohibited. All fatty dishes and products are removed from the diet (dairy, pork, goose, lamb, duck, red fish, lard, pastry creams, etc.), smoked foods, canned food, spicy seasonings, sweets, cocoa- and caffeine-containing drinks, chocolate, egg yolks , baked goods.
Slimy soups, pureed porridges, vegetable, fish, meat or cereal soufflés, puddings, dumplings, steamed cutlets, jelly, mousses, and protein omelettes are welcome. Butter (as a source of mucous membrane protector - vitamin A) and vegetable oils (soybean, corn, vegetable, cottonseed, olive, etc.) are allowed. All drinks and meals should be served warm to the patient, as cold can cause a painful attack of pain.
After the long-awaited remission occurs, baking and stewing are allowed, food is no longer pureed, and fresh berries, herbs, vegetables, and fruits are included in the diet. To improve the composition of bile and reduce its ability to form stones, dietary fiber is indicated. It is rich in grains (buckwheat, oats, barley, etc.), kelp, bran, vegetables, algae, and fruits.
ethnoscience
- Tincture of wormwood with vodka. To drink this medicine you need to drink 20 drops every 3 hours. You can make a decoction based on this raw material: half a teaspoon of herb per 250 grams of water, boil for 10–15 minutes and drink in small doses throughout the day. The decoction and tincture are not sweetened with honey or sugar.
- If diarrhea is long-lasting, you can brew and boil a sliver of oak bark. It is added to 0.5 liters of water, the broth is boiled until it boils down to the volume of a glass. The medication is taken in the following dosage: 2 teaspoons 3 times a day.
- Another recipe for diarrhea is also based on a decoction of oak bark: a teaspoon of plant material is taken in a glass of boiling water. Then boil the broth for half an hour and drink 4 teaspoons 3 times a day until the symptoms completely stop.
- We infuse blueberries by pouring 250 grams of boiling water over them, leave for half an hour and drink little by little throughout the day. You can make jelly from berries and starch. It is also an effective remedy for treating diarrhea.
- You can infuse bird cherry berries or boil them in boiling water at the rate of 2 teaspoons of plant material per 250 or 500 grams of water. The medicine is taken 1⁄4–1/2 cup 3 times a day.
- We cut the blackberry branches into twigs 5 cm long. Take 2 teaspoons of plant material and pour a glass of boiling water. We insist on them for 60 minutes and drink them instead of tea. In 2–3 days, the functioning of the gastrointestinal tract is restored.
Why is stool light in color: causes
Food significantly influences the color of excrement. Sudden light color of stool can be caused by heavy consumption of fatty foods (butter, sour cream). Potatoes and white rice can have the same properties if you eat a lot of them the day before and without adding other foods.
If the diet consisted more of meat foods, and you suddenly ate a large amount of plant foods, then the feces will become much lighter. When changing shade, first of all, remember your diet in previous days. It was probably nutrition that caused this phenomenon.
There are a number of medications that can cause lightening of excrement. These include:
- antibiotics;
- anti-inflammatory drugs;
- antipyretics (aspirin, ibuprofen, paracetamol);
- antifungal agents;
- drugs for the treatment of tuberculosis;
- gout medications;
- drugs for the treatment of epilepsy.
If you have undergone an examination such as an x-ray of the gastrointestinal tract or other procedures in which it is necessary to take barium sulfate, then 2-3 days after the stool will very sharply lighten. When the barium is completely removed from the body, the excrement will return to its normal color.
Forecast and prevention of the disease
Preventing cholecystitis is not difficult at all. To do this, it is enough to observe certain restrictions in food: reduce the consumption of salted, smoked, fried foods, include more raw and boiled vegetables in the diet, avoid too fatty meat. In addition, sufficient physical activity will also help avoid inflammation of the bile duct and diarrhea. Diarrhea with cholecystitis does not always occur - it is a nonspecific sign of the disease. However, diarrhea due to inflammation of the gallbladder significantly worsens the patient’s condition and requires treatment.
Sources
https://lechigemor.ru/holetsistit/simptomy/10457-tsvete-kala-pri-holetsistite-1.html https://goodyhealth.ru/obescvechennyj-kal.html https://holecistit.gastrit-i-yazva. ru/meteorizm/belyj-kal-pri-holetsistite/ https://www.belinfomed.com/zhelchnyj-puzyr/kal-pri-holecistite.html https://jeludokbolit.ru/xolecistit/ponos-pri-xolecistite.html https://bezboleznej.ru/holecistit
Development mechanism
Hologenic diarrhea develops after excessive intake of bile acids (BAs) into the large intestine.
It is here that more water and electrolytes are absorbed from the food mass - feces are formed. The effect of FA on the intestinal walls leads to the production of the enzyme adenylate cyclase, which activates the hormonal messenger cAMP. It interferes with the absorption of water and sodium, which enter the lumen of the colon. After this, secretory diarrhea develops.
FA is formed in liver cells - hepatocytes. Normally, they are deposited in the gallbladder and flow into the duodenum only during meals.
After several transformations, the acids enter the ileum, are broken down by enzymes of anaerobic bacteria, are absorbed into the blood and transported back to the liver. Only 5% of FA is excreted in feces.
A functional change in this circuit results in excess FA in the large intestine. This occurs when the absorption of acids is impaired (malabsorption), the evacuation of food mass is accelerated, and bile acids are poured into the empty intestine.
Symptoms
If, in addition to lightening the stool, you feel unwell and a deterioration in your general condition, you should seek medical advice. Especially if you eat, the malaise does not go away within a day. Symptoms to watch out for:
- persistent increase in temperature;
- stool disorder;
- nausea, vomiting;
- pain in the abdomen, left hypochondrium, girdle pain;
- yellowed sclera of the eyes and skin;
- lack of appetite;
- sudden weight loss;
- dark urine;
- flatulence, abdominal enlargement;
- stool with mucus.
If there are at least two additional signs with light-colored stool, it is necessary to undergo a medical examination to determine the diagnosis. With some problems, for example, with advanced pancreatitis, the count is not days, but hours. Be attentive to symptoms and do not ignore serious ailments.