What it is?
Peritonitis is inflammation of the peritoneum. The victim has a stomach ache, stool and gas retention, vomiting and tension in the abdominal muscles. He is in a serious physiological condition, suffering from an excess of heat in the body, which leads to a rapid increase in temperature.
Peritonitis of the abdominal cavity is treated only surgically.
The peritoneum is a serous covering that protects the gastrointestinal tract. The peritoneum is parietal and visceral.
The first type of membrane protects the inner wall of the abdomen. Visceral covers the surface of the organs located inside the parietal layer.
Causes of peritonitis
Infectious peritonitis is caused by bacteria and germs. The following microorganisms provoke the disease:
- fusobacterium;
- enterobacter;
- Proteus;
- streptococcus;
- eubacteria;
- peptococcus;
- Pseudomonas aeruginosa;
- staphylococcus
In most cases, viral peritonitis is caused by Escherichia coli and staphylococci.
In addition to microbes, there are other causes of the disease:
- inflammation processes occurring in the peritoneum (cholecystitis , appendicitis);
- defect of the digestive system;
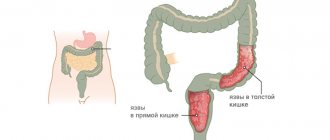
- the appearance of through holes in the abdominal organs (duodenum or stomach during an ulcer, appendix, colon);
- surgical interventions in the abdominal organs;
- inflammation of the phlegmon of the abdominal covering of the abdomen, processes of decay in the retroperitoneal tissue.
Causes
There are extremely many causes of inflammation of the peritoneum in adults and children, but they are all associated with the spread of infection into the abdominal cavity. Primary infection is rare. It is associated with infection entering the peritoneum with blood.
Secondary infection occurs as a result of a violation of the integrity of the organs of the abdominal cavity and pelvis. The causes of the development of microbial peritonitis are such pathologies.
- Appendicitis is an inflammation of the appendix. It is the cause of peritonitis in about half of the cases. This complication develops if the patient does not have the appendix removed. Due to inflammation, it ruptures and infects the peritoneum with microbes. Appendicitis and peritonitis are related: the disease is a complication of acute phlegmonous or gangrenous inflammation of the appendix.
- Perforation of a stomach or duodenal ulcer. This cause leads to peritonitis in approximately 15% of all cases. Perforation of the ulcer leads to the contents of the affected organs leaking into the abdominal cavity. Chemical, physical and bacterial damage to the peritoneum occurs, and the higher the acidity of the stomach juice, the stronger the burn.
- Gynecological and obstetric pathologies - salpingitis, salpingoophoritis, accumulation of pus in the fallopian tubes, rupture of cysts in the ovary or damage to the fallopian tube. The progression of peritonitis in women in such cases can be very severe. The disease can occur in approximately 10% of cases.
- Intestinal and biliary pathologies. In about 10% of cases, inflammation of the peritoneum can be a complication of intestinal obstruction, intestinal diverticulosis, Crohn's syndrome, inflammation of the gallbladder, or the accumulation of stones in this organ. In extremely rare cases, peritonitis can be caused by tooth infections.
- Open or closed abdominal lesions. With penetrating wounds, direct infection occurs due to the presence of microbes in the environment. With closed injuries, the disease develops due to a violation of the integrity of the abdominal organs, as well as the urinary organs.
- Factors in the development of aseptic peritonitis are fluids that are aggressive to the peritoneum - blood, urine, gastric or pancreatic juice, feces. Sometimes the disease is caused by enzymatic fluids.
Symptoms
There are 3 stages of the disease. Therefore, everyone has their own symptoms. The main signs of peritonitis:
- increased temperature and blood pressure;
- nausea with vomiting;
- dry mouth;
- cardiopalmus.
Peritonitis in children has the same symptoms as symptoms in adults
Symptoms of the first stage of the disease
This is long-term abdominal pain that gets worse with changes in body position. The patient lies and tries not to make movements. The Shchetkin-Blumberg symptom allows you to detect this disease.
It is necessary to slowly press on the abdominal wall, hold your hand for 3-6 seconds and sharply remove it. The occurrence of sharp pain indicates that the person is suffering from peritonitis.
The disease can also be identified using Mendel's symptom. You need to tap over the entire abdominal area. If the pain intensifies, the person is sick. This method determines the location of the pathology.
Symptoms of the second stage of peritonitis
The pain in her stomach and the tension in her muscles are subsiding. Stool retention, bloating, and frequent vomiting with an unpleasant odor begin to appear.
The heartbeat also accelerates (more than 115 beats per minute), blood pressure decreases, and body temperature increases. Intoxication symptoms occur.
Symptoms of the third stage of the disease
Due to lack of water, the patient’s skin becomes pale and facial features become sharp. There is a rapid heartbeat, low blood pressure, incomplete breathing, and bloating.
There is no peristalsis - wave-like contractions of the walls of the gastrointestinal tract, leading to the movement of food.
The patient's psychological state changes dramatically due to intoxication (poisoning): from adynamia (loss of strength) to euphoria (state of bliss). In rare cases, delirium and confusion of consciousness appear.
Primary diagnosis
If intestinal peritonitis is suspected, diagnostic measures must be carried out simultaneously with the provision of emergency medical care. To avoid life-threatening complications, an accurate diagnosis of the patient should be made no later than 2 hours from the onset of the disease.
When diagnosing intestinal peritonitis, the following information must be taken into account:
- presence of peritoneal symptoms;
- abdominal x-ray and ultrasound data;
- peritoneal puncture data;
- result of diagnostic laparoscopy;
- laboratory test indicators.
The initial diagnosis can be made based on the general clinical picture of the disease. Specialists pay special attention to pain during the initial examination of the patient. For this, a number of modern methods are used (for example, the Shchetkin-Blumberg technique), which can confirm the development of intestinal peritonitis in a patient. When self-relieving pain with the help of various painkillers, a reliable clinical picture can be greatly distorted.
Types and stages of peritonitis
Acute peritonitis is classified into three stages:
- Intestinal peritonitis of the first stage (reactive, duration – half a day). The body begins to fight the infection that has entered the peritoneum. This leads to localized inflammation in the form of edema, hyperemia (overflow of blood vessels in the body area), and accumulation of exudate.
Types of peritonitis
Depending on the prevalence of the inflammatory process, the following forms of peritonitis are distinguished:
- Local (occupies one anatomical section of the abdominal cavity);
- Widespread (2-5 anatomical sections of the abdominal cavity are involved);
- Total (six or more anatomical parts of the abdominal cavity are involved).
It is also important to consider the type of exudate. So, depending on the nature of the exudate, the following forms of peritonitis are distinguished:
- Serous;
- Fibrinous;
- Purulent;
- Hemorrhagic;
- Gall;
- Fecal;
- Mixed.
Peritonitis can also be acute or chronic. The chronic form of the disease is more common with systemic infections of the body (syphilis, tuberculosis). Acute peritonitis occurs in three phases: reactive, toxic, terminal.
The first stage (reactive) is recorded in the first 12-24 hours of the disease. During this period, swelling of the peritoneum occurs, exudation with fibrin loss. In the clinical picture, local symptoms of the disease are especially pronounced.
The second stage (toxic) develops after 24-72 hours. During this period, toxicosis increases, as a result of which general intoxication symptoms prevail over local ones.
The third stage (terminal) develops after 72 hours. This period is characterized by severe intoxication.
Diagnostics
The initial stage includes examining the patient and identifying symptoms:
- Medel;
- Bernstein;
- Voskresensky;
- Shchetkin-Blumberg.
The patient undergoes research:
- Radiography. A “sickle” symptom is established under the diaphragm. In case of intestinal obstruction, a Kloiber cup is determined.
- Blood analysis. An increase in the erythrocyte sedimentation rate and an increase in the number of leukocytes are detected;
- Ultrasound of the peritoneum.
In rare cases, laparoscopy is prescribed.
Diagnosis of peritonitis
In addition to the data obtained during the examination, to diagnose peritonitis, doctors prescribe laboratory and instrumental studies:
- Clinical blood test: shows nonspecific signs of inflammation - increased number of leukocytes, accelerated ESR. The leukocyte index of intoxication is above 4 (in the terminal stage it can reach 12).
- An ultrasound of the abdominal cavity shows the presence of liquid and gas in it.
- X-ray of the abdominal cavity: in addition to fluid and gas, you can see signs of intestinal paresis (horizontal levels of fluid in the intestinal loops with accumulations of gas above them - the so-called Kloiber Cups).
- Blood biochemistry shows changes characteristic of multiple organ failure. If possible, a blood procalcitonin test is prescribed, an elevated level of which is characteristic of peritonitis and sepsis.
- If technically possible, a computed tomography scan is prescribed, which allows you to clearly visualize the condition of the abdominal cavity.
In unclear cases, doctors may go for diagnostic laparoscopy - an endoscopic examination of the abdominal cavity - or laparotomy - an open operation.
X-ray for peritonitis: dilated intestinal loops
Treatment
Once peritonitis is identified, the patient is scheduled for surgery. It is aimed at eliminating the root cause. The disease cannot be cured in any other way.
Surgery
The patient is hospitalized and preoperative measures aimed at treating peritonitis are carried out:
- relieve pain shock - anesthesia is administered;
- bring the pressure back to normal by introducing food, fluids, and medications.
It also helps normalize the amount of water in the human body and destroy infections.
During surgery, a laparotomy is performed, treating all the contents with a special antibacterial agent. The abdominal wall is cut to identify through holes in the stomach or intestines. The perforations are sutured, the pus along with part of the hollow organs is cut off and removed.
During an emergency operation, when peritonitis progresses in the final stages, the surgeon eliminates exclusively the cause of the disease. The remaining measures are scheduled for the next term, because purulent inflammation prevents their implementation.
Decompression of the small intestine is carried out by nasointestinal intubation. This is the insertion of a hose through the mouth or nostril cavity. It is also used for the purpose of evacuation of intestinal contents and artificial supply of nutrients.
Drainage - removal of fluid using rubber tubes - of the large intestine is carried out to eliminate peritonitis through the anus. The event includes the removal of exudate and the introduction of antimicrobial solutions to destroy harmful microorganisms.
Peritonitis in a child
It is peritonitis that can become a serious cause for concern for parents if it appears in a child. This disease is quite rare, but if it does appear, it brings many problems. In 70% of cases it leads to death, so you should act immediately and seek medical help. Fortunately, modern medicine can reduce the mortality rate by up to 20%. The most common type is tuberculous peritonitis.
Since children often get sick with various bacterial diseases, the risk of inflammation of the peritoneum is high. The infection penetrates through the blood into weak areas of the body and begins to multiply. Therefore, here parents should not wait for the child to recover on his own, but start treating him in the early stages so that sepsis does not develop.
go to top
Treatment after surgery
Peritonitis after surgery requires special treatment. It involves taking medications that destroy pathogenic microflora, restore the activity of the gastrointestinal tract and normalize the immune system.
The patient is also prescribed a diet that he must adhere to for a week. Peritonitis in children is treated in the same way as in adults.
Drug treatment
The following types of medications are prescribed:
- antibiotics. Penicillin-Teva, benzylpenicillin, ceftriaxone, gentamicin and others;
- diuretics, the active ingredients of which are Indapamide (trade name - "Arifon"), Spironolactone ("Veroshpiron"), Torasemide ("Trigrim");
- means aimed at removing toxic substances from the body. These include “Calcium gluconate”, “Splenin”, “Unitiol”, etc.;
- infusion solutions (“Hemodez”, “Gelatinol”, “Reopoliglyukin”);
- blood products – “Albumin” (5% and 20% solutions), “protein”, “fibrinogen”;
- non-steroidal anti-inflammatory drugs - Ketoprofen, Arcoxia, Indomethacin;
- anti-vomiting agents. Contains ondansetron (Emeset), domperidone (Motilium);
- drugs aimed at preventing the development of intestinal paresis. These are "Neostigmine", "Physostigmine".
Peritonitis: treatment
Peritonitis must be treated as quickly as possible, immediately after confirming the diagnosis of inflammation of the peritoneum. Delay at all stages of diagnosis increases the risk of death.
The surgeon’s tasks during treatment are: eliminating the cause of peritonitis and sanitation of the abdominal cavity, as well as etiopathogenetic and symptomatic treatment after surgery.
Surgical treatment
Despite the fact that laparoscopy is a modern method of surgical intervention, treatment of acute abdomen most often occurs through laparotomy. The advantages of an incision in the anterior abdominal wall include: a wide surgical field and speed of access.
During surgery, the surgeon eliminates the cause - sanitizes the source of inflammation, sutures the perforation of the internal organ or removes the damaged organ. After which the abdominal cavity is washed with antiseptic solutions. The edges of the wound are sutured, leaving space for drainage - a tube through which inflammatory exudate will be released in the postoperative period.
Surgical treatment is an integral component of eliminating the cause of peritonitis and the patient’s recovery.
Conservative treatment
Conservative therapy for peritonitis complements surgical treatment. The goal is to eradicate the infectious agent, restore the function of organs and body systems, that is, complete recovery.
- Antibiotic therapy
Antibacterial therapy is carried out with broad-spectrum antibiotics, which act on several types of infectious agents at once. The greatest bioavailability is achieved with intravenous administration of drugs.
- Correction of metabolic disorders
In the postoperative period, the patient is administered infusion solutions that reduce the severity of symptoms of intoxication and restore water and electrolyte balance.
- Diuretics
In the absence of signs of renal dysfunction, urination is stimulated by certain groups of diuretics. Thus, toxins are eliminated from the body and their concentration in the blood decreases. The patient's general well-being improves.
- Anticoagulants
Every surgical intervention poses a risk of thrombosis. Anticoagulant therapy prevents a reactive increase in blood clotting.
Depending on the stage of the disease and the presence of complications, therapeutic treatment can be supplemented with the introduction of blood components, non-steroidal anti-inflammatory drugs, antipyretic and antiemetic drugs.
Sanitary procedures
The medical staff takes care of post-operative sutures once a day. The nurse examines the wound surface and treats the sutures with disinfectant solutions. After performing sanitary and hygienic procedures, apply a clean bandage.
Prevention
Purulent peritonitis can be avoided by observing the following rules:
- do not delay the treatment of diseases that can lead to serious complications (appendicitis, stomach ulcers, pancreatitis, etc.);
- get 50%-60% of all energy per day from fruits, vegetables and other foods rich in vitamins and chemical elements;
- give up unhealthy foods (fast food, sweet carbonated drinks, etc.);
- avoid body hypothermia;
- avoid stress;
- do not take medications without consulting a doctor;
- get enough sleep, don’t forget to rest after work;
- Wash fruits, vegetables, berries and hands thoroughly before eating.
Postoperative care
After surgery, it is important to continue drug treatment to prevent complications.
On the second day after surgery, parenteral nutrition is started. The volume of infusion therapy is approximately 50-60 ml per kilogram of body weight per day. When intestinal motility is restored, they switch to enteral nutrition: administration of nutritional mixtures using a probe through the mouth and nose. The composition of the mixtures and the duration of such feeding are determined by the doctor.
With positive dynamics and restoration of normal intestinal function, they switch to natural nutrition. This usually occurs no earlier than the fifth day after surgery. It is necessary to adhere to a low-calorie diet. During this period, it is recommended to eat low-fat meat broths, vegetable purees, jelly and compotes. Gradually increase the calorie content of the diet by adding meat, eggs, and dairy products. You should not eat rich meat broths, smoked meats, spices, confectionery, chocolate, coffee, carbonated drinks, or legumes.
Several times a day it is necessary to inspect the postoperative wound, pay attention to the cleanliness of the dressing and the degree of wetting. The bandage needs to be changed regularly. When changing the dressing, you must follow the antiseptic rules and avoid dislodging the drainage tube.
Grigorova Valeria, medical observer
49, total, today
( 201 votes, average: 4.55 out of 5)
Rectal bleeding: causes, symptoms, treatment
Biliary peritonitis: causes, symptoms, treatment, prevention, risks
Related Posts
Post-op period
The recovery stage (after surgery) includes the following activities:
- Infusion of solutions capable of restoring the acid-base, water, electrolyte balance in the patient’s body.
- Restoring the functions of the liver, kidneys, pancreas, supporting their vital functions.
- Drug therapy - administration of antibiotics. Medicines to which the identified pathogenic microorganism is sensitive are used.
Experts advise a patient who has suffered diffuse peritonitis to strictly adhere to the following recommendations:
- Prevention of dysbiosis - taking probiotics and eubiotics.
- Proper nutrition - avoiding foods high in sugar and baked goods.
- The predominance of foods high in fiber, dairy and fermented milk products in the menu.
End-stage symptoms
The terminal phase is the phase that begins 72 hours after the onset of the disease. It is characterized by an extremely serious condition of the patient. The main features are as follows:
- The man is immobilized.
- Depressed consciousness (to the point of coma).
- Intoxication of the body is visible by the worsening signs of the previous stage.
- Symptoms of multiple organ failure.
- Thready pulse.
- The skin is bluish, grayish, very pale.
- Weak breathing (sometimes it is necessary to maintain the patient’s vital activity using a mechanical ventilation device).
- Renal failure is expressed in a sharp decrease in the volume of urine excreted or in the complete absence of urine.
- Vomiting of intestinal contents (excreted by fecal odor).
- Progressive intestinal paresis.
- One of the dangerous manifestations is septic shock.
- The abdominal muscles noticeably weaken (in contrast to the extremely tense state in the previous stage).
The fatal outcome at this stage of the disease is 50% of cases.
Stages of acute peritonitis
The development of peritonitis is divided into the following stages:
- early – lasts 12 hours;
- late – 3-5 days;
- final – 6-21 days.
Depending on the severity of inflammation, the following stages are distinguished:
- reactive - a hyperergic reaction that occurs in response to irritation of the peritoneal tissue and is manifested to a greater extent by local rather than general symptoms;
- toxic – expressed in an increase in signs of intoxication of the body in response to inflammation;
- terminal – manifested by signs of exhaustion of the body and is accompanied by dysfunction of vital systems and organs.
Features of the disease
To put it briefly and precisely, peritonitis is an inflammatory process occurring in the peritoneum.
The abdominal cavity is the volume located below the chest. It contains certain organs, such as the small and large intestines. And the peritoneum is the inner lining of the abdominal cavity.
When fecal peritonitis occurs, the activity of many organs is disrupted.
If appropriate measures are not taken in a timely manner, the pathology can cause serious damage to human health and even lead to the death of the patient.
Medical statistics show that the mortality rate from this pathology is high.
The peritoneum is a semi-permeable film, one might say - a membrane. In the body, this membrane performs many different and very important functions.
Among the main ones the following stand out:
- barrier;
- resorptive;
- exudative.
The peritoneum protects the internal organs of the abdominal cavity from the penetration of microbes. When diffuse peritonitis occurs, this protection is significantly weakened.
The resorptive function is reduced to absorbing exudate and lysis products, and the exudative function is to secrete serous fluid.
In the presence of fecal pathology, all these processes slow down or stop.
The pathogenesis of fecal peritonitis is determined by a large number of components. The rate of development of the disease depends on the volume of toxins that are absorbed by the peritoneum.
The larger the inflamed surface area, the faster toxins enter the blood. An aggravating factor in the development of fecal peritonitis is intense dehydration.
When fluid loss per day exceeds the five-liter mark, it can cause an attack of heart failure. Symptoms of this kind are associated not only with fecal peritonitis, but also with other types of peritonitis.
Depending on the type of pathology, a course of treatment and postoperative rehabilitation is prescribed.
Successful experience in the treatment of peritonitis shows that the symptoms of the pathology are ambiguous, so it is very important to pay attention to them in a timely manner.
Most often, the first signs of the disease indicate acute poisoning or stomach upset. With the fecal variety of pathology, the clinical picture looks standard.
Only an experienced doctor is able to determine the level of danger of existing signs. To distinguish between certain stages of disease development, a classification system has been created.
According to this system, peritonitis is divided into primary and secondary.
In the first case, infection of the peritoneum occurs in the absence of an inflammatory focus in the abdominal cavity.
In this case, infection occurs through the hematogenous or lymphatic routes, and the fecal variant of peritonitis is impossible.
Secondary peritonitis spreads from purulent foci that have formed in the abdominal cavity.
For a more accurate description, experts distinguish the following types of peritonitis:
- local;
- common;
- spilled.
Local pathology affects one area of the abdominal cavity. In the second option, the lesion spreads to several anatomical sites.
Diffuse peritonitis can affect the entire abdominal cavity.
Classification
By etiology
- Bacterial peritonitis. The bacterial form of the disease is associated with the activity of pathogenic microorganisms in the abdominal cavity.
- Aseptic peritonitis. The aseptic form develops against the background of other peritoneal lesions not associated with bacterial infection.
By the nature of the fluid that accumulates in the peritoneum
Based on the nature of the fluid that accumulates in the abdominal cavity, the following forms of the disease are distinguished:
- serous;
- hemorrhagic;
- fibrinous;
- feces;
- purulent;
- fibrinous;
- putrid.
According to the course of symptoms
- Acute peritonitis. An acute disease occurs abruptly, progresses quickly and often leads to complications. Typically, this form is characteristic of a common process in the abdominal cavity.
- Chronic peritonitis. If peritonitis is limited in nature, then its course is usually chronic. The disease develops gradually, symptoms progress slowly. Against the background of a chronic course, conditions that threaten the patient’s life are less likely to occur, but in most cases this form is more difficult to treat.
By location
Based on location, the following forms of the disease are distinguished:
- subphrenic;
- appendicular;
- subhepatic;
- pelvic;
- interintestinal.
Complications and consequences
In the postoperative period, constant monitoring of the patient is required. The likelihood of complications depends on when medical care was provided. Of no small importance is the nature of the pathological process and the initial state of human health.
The catarrhal stage of peritonitis is characterized by pronounced pain, which can cause loss of consciousness. If the operation is performed at this stage, the purulent masses will not have time to spread to other organs. If assistance is not provided in a timely manner, there is a risk of the following complications:
- uremic encephalopathy;
- adhesions in the peritoneum;
- necrosis of the intestinal walls;
- purulent inflammation of soft tissues;
- disruption of the process of oxygen delivery to tissues;
- sepsis;
- death.
The most important danger of peritonitis is the high risk of death. According to statistics, the mortality rate is 20%. Early diagnosis of the disease significantly increases the likelihood of favorable developments.
What kind of disease is this?
Diffuse peritonitis is an inflammatory process that affects the parietal and visceral layers of the peritoneum. It can be of both aseptic and bacterial origin. Primarily associated with the severe general condition of the patient. This is caused by multiple organ failure.
Let's turn to anatomy to better understand what diffuse peritonitis is. The layers of the peritoneum are serous membranes consisting of mesothelium, a single-layer type of epithelium. They are divided into two categories:
- Visceral epithelium - covers the internal organs of the peritoneum.
- Parietal (or parietal) - lines the walls of the abdominal region itself.
As soon as inflammation occurs in the peritoneum, the serous membrane immediately tries to protect healthy neighboring tissues from the inflammatory focus by creating so-called adhesions. This is local peritonitis. In the case when such a barrier is unsuccessful (inflammation spreads to neighboring areas), the process already takes on an extensive, diffuse character. Diffuse peritonitis develops.
Statistics say that 15-20% of patients admitted to hospitals with a diagnosis of peritonitis require immediate surgical intervention. Mortality among patients is high - 40-50% of cases.
Doctors classify diffuse peritonitis of the abdominal cavity as a group of pathologies under the general name “acute abdomen.” That is, to acute forms that require immediate surgical intervention.
Symptoms of the toxic stage
The phase begins 24-72 hours after the onset of the disease. First of all, it is characterized by a sharp deterioration in the patient’s condition. The following symptoms are noted:
- Increase in body temperature.
- Loss of consciousness.
- Change in breathing rate. It itself becomes noisy.
- Weak pulse. Sometimes almost thread-like.
- A person is constantly tormented by thirst.
External manifestations:
- The patient’s face resembles the so-called “Hippocratic mask” - haggard, sunken cheeks, sunken eyes.
- Dry lips.
- The tongue is also dry, coated with a grayish coating.
- The patient is not breathing from the stomach.
- The abdomen on palpation is board-shaped (due to muscle tension).
The following symptoms may also occur:
- Reducing the amount of urine excreted by the body.
- Bloating.
- Loss of consciousness.
- Lack of peristalsis of the intestinal tract due to its paresis.
Ultrasound examination shows the presence of free fluid in the abdominal cavity. Its character can be purulent-hemorrhagic or purulent-fibrous.
Possible complications
Against the background of diffuse peritonitis, the following pathologies often develop:
- Acute renal failure.
- Dehydration of the body.
- Toxic shock.
- Pneumonia of congestive type.
Diffuse peritonitis is a dangerous, rapidly developing disease with a high probability of death. However, there are no specific preventive measures that can protect against this disease. Doctors advise adhering to a healthy lifestyle, promptly dealing with even seemingly minor illnesses, not self-medicating, and if alarming symptoms are detected, immediately seek qualified medical help.