Stomatitis – inflammation, damage to the mucous membrane of the mouth, tongue, palate of the gums. It is characterized by an inflammatory process in the oral cavity, specific plaque and ulcers. This disease may go away on its own within a week, but will definitely return as soon as an irritating or provoking factor appears again.
This lesion most often occurs in children under 5 years of age. Breasts are additionally protected by antibodies from mother's milk, but are also at risk, especially after a cold, vaccination, or any process that was accompanied by an increase in temperature, especially a prolonged one.
What is stomatitis
Stomatitis is a disease characterized by inflammation of the oral mucosa. May have different etiologies.
Depending on the form and stage of the disease, stomatitis can cause various symptoms. The disease can be successfully treated if diagnosed and treated in time.
Stomatitis can develop in both a newborn and a one-year-old child and older. This pathology is very common among children, as it can be transmitted through contact. The little ones are most susceptible, since the immune system is still immature and unable to fully resist infections.
Note! Local symptoms of stomatitis always occur, but general symptoms occur only in severe cases.
Stomatitis comes in different varieties. Depending on age, one can determine the tendency of children’s predisposition to one or another type of pathology:
- in infants and under 3 years of age - stomatitis due to candida fungi;
- from 1 year to 3 years – a tendency to the herpetic type;
- from 7-15 years – aphthous stomatitis.
Other forms of the disease are diagnosed regardless of age.
Medicines for bacterial stomatitis
The main component of therapy for bacterial inflammation of the oral mucosa is rinsing with antiseptic solutions. If pathology is diagnosed in an infant, rinsing can be replaced with irrigation . Many manufacturers produce drugs with special spray nozzles, as in the photo, which are designed for comfortable treatment of stomatitis in children.
Antibiotics and local antiseptics are indicated for primary therapy. And to prevent the disease and prevent complications - immunomodulators.
Most often, doctors prescribe the following drugs:
Spray "Lugol". Contains potassium iodide and glycerol. Indicated for the treatment of stomatitis in children over 5 years of age. Frequency of use: 5–6 times a day.
- Semi-synthetic antibiotic "Augmentin". Belongs to the group of penicillins and is prescribed for severe disease. The main active ingredients are amoxicillin and clavulanate. Release forms: powder for injection, tablets, syrup, suspension. The dosage is determined by the attending physician and depends on the age of the baby, the severity of stomatitis and individual factors. The drug is contraindicated in children under 2 months of age.
- Gel "Metrogil Denta". Contains an antibiotic and an antiseptic, due to which it has a double effect. The product can be used to treat stomatitis in children over 6 years of age.
Classification of stomatitis
The classification includes several types of stomatitis. Depending on the cause of the disease, there are:
- viral stomatitis;
- fungal;
- bacterial;
- allergic;
- traumatic;
- herpetic stomatitis;
- medicinal.
Important! Among all forms of stomatitis, viral and bacterial are the most contagious - they can easily become infected.
Based on the depth of damage to the mucous membrane, we can distinguish:
- catarrhal;
- vesicular;
- aphthous;
- erosive.
Stomatitis can be mild, but sometimes the disease is accompanied by signs of general intoxication. In children, the disease can occur in acute, recurrent and chronic forms.
Each form of childhood stomatitis has its own specific symptoms. Depending on what caused the disease, the principles of therapy differ. The diagnosis must be made by a doctor, since only after a medical examination can an effective remedy be selected.
Prevention of stomatitis
After the child recovers, you need to replace his toothbrush, pacifier, and bottle to avoid secondary infection of the mucous membrane . If your baby has carious lesions, you need to visit the dentist to heal them and prevent a relapse.
Oral hygiene plays a huge role in preventing outbreaks of any type of stomatitis. Other rules that promote prevention include:
- Washing your hands before eating, after walking, playing with other people's toys.
- Systematic intake of vitamins and balanced nutrition.
- Keeping the house clean. Especially if there is a patient in it.
- Exclusion from the diet of very spicy, salty, sour, cold, hot foods. Limited sugar intake.
- Healthy lifestyle. Spending time outdoors and playing sports is good for strengthening the immune system.
If you detect the slightest signs of inflammation of the child’s oral mucosa, you should consult a dentist. Determining the diagnosis from a photo and treating children for stomatitis with self-selected medications is not only useless, but also dangerous. Moreover, both for the health and for the life of the baby.
Causes of stomatitis
In order to competently get rid of the problem, it is always important to take into account the factors that provoked the development of the pathology. Stomatitis can develop for the following reasons:
- penetration of viruses, fungi and bacteria into the oral mucosa;
- activation of viruses that are already in the body against the background of a decrease in the body’s immune defense;
- mouth burns from hot food;
- mechanical damage to the integrity of the mucous membrane;
- dental problems;
- unsuitable oral care products;
- wearing braces or other corrective structures;
- improper oral hygiene.
All these factors can lead to inflammation of the oral cavity. In addition to the main reasons, stomatitis in a child can occur due to the following factors:
- lack of vitamins and general weakening of the body;
- diabetes mellitus or other systemic pathologies;
- long-term use of antibiotics, which disrupts the constant microflora and the ability to protect against infections;
- dehydration due to food poisoning and intoxication;
- allergic reaction;
- anemia;
- hormonal disorders.
Some forms of stomatitis, for example, the candidal type of disease, can appear in a baby as a result of infection during passage through the birth canal from a mother who suffered from thrush.
Poor nutrition, parents’ failure to comply with the baby’s thermal regime, and genetic predisposition can also affect the likelihood of stomatitis in the child’s mouth.
Recommendations for parents
Before the baby gets to the doctor, ease her condition - let's rinse her mouth more often with decoctions of medicinal herbs. Do not give rough and hot food, or better not force him to eat at all. More warm drinks and rest. You can numb the pain with a weak anesthetic solution.
Always make sure that your child eats well, or better yet, regularly takes a complex of vitamins for children, like Doromarin, which has shown itself to be effective for the prevention and treatment of thrush (in combination with medicinal drugs). The recovery process goes very quickly, the baby becomes more active and copes with many diseases more easily, including stomatitis.
The natural composition of children's vitamin DoroMarine (Far Eastern kelp, also known as angustata, sea cucumber extract and sea calcium plus fruit juice for taste) allows it to be taken by children from 3 months to 16 years. Pleasant to the taste, healthy, it will strengthen the general condition of the child’s body, including a guaranteed effect against stomatitis.
Thanks to the strong immunocorrective ability of the components of Doromarin a, it is effective against most childhood diseases. These vitamins do not cure, they give the body strength to defeat pathogenic cells on its own. Doromarin not only strengthens the immune system, it provides relief from symptoms plus comprehensive recovery from stomatitis.
For stomatitis (treatment or prevention), the following properties of Doromarin vitamins are important:
- reduce the aggressiveness of microflora;
- protect the mucous membrane by covering it with a thin layer of jelly-like substance;
- absorb harmful substances from the oral cavity;
- reduce dysbacteriosis, microflora thrush;
- heal wounds, burns, ulcers, cracks;
- suppress the activity of harmful bacteria, especially Candida;
- slight antimicrobial effect;
- immunostimulating effect;
- effective against gum disease.
Most of the properties of the DoroMarine complex are due to the effectiveness of alginic acid and its derivatives, the content of which in DoroMarine is up to 55% (of the dry residue). This natural therapeutic and prophylactic product for children is ideal for children who are very physically active, whose environment has changed, who have contact with sick children (kindergarten, school, sanatorium), who suffer from allergies, various infections and viruses more often than twice a day. year.
These vitamins are indispensable for immunity for weakened children who eat poorly or have metabolic problems (specific diseases, hormonal, including diabetes, hypothyroidism, etc.). It is definitely recommended for children who constantly watch TV or sit in front of the computer. This will allow them to improve their vision and have a beneficial effect on the condition of the whole body. There are many positive reviews from satisfied parents who recommend taking the vitamin complex for children Doromarin.
Remember, stomatitis is not scary for healthy kids!
Symptoms of stomatitis
Stomatitis can be identified by characteristic signs. Some of them are characteristic of any form of pathology. But there are also those that are characteristic only of a specific form of the disease.
The incubation period for stomatitis ranges from 4-8 days, depending on the child’s health, age and form of pathology.
The first signs of any stomatitis are as follows:
- temperature increase;
- fever;
- general weakness;
- Nausea and vomiting are possible;
- enlarged and painful lymph nodes;
- signs of respiratory disease.
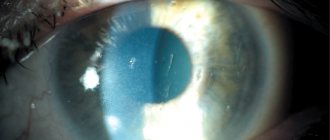
Note! In rare cases, stomatitis is accompanied by conjunctivitis.
The main symptom of stomatitis is the formation of wounds in the mouth that cause pain and discomfort. Their character may differ depending on the causative agent of the disease; it is important to pay attention to the photo.
Features of viral stomatitis
Viral stomatitis is one that develops under the influence of viral pathogens. The disease can be provoked by herpes, adenovirus, or enterovirus pathogens. Sometimes the cause of the sore is recent flu, measles, rubella and other infections.
In the viral form of the disease, the symptoms are:
- the mucous membrane becomes covered with bubbles;
- after their rupture, ulcers form in the mouth;
- lesions tend to merge;
- the affected parts are covered with a yellowish coating.
Usually the bubbles are localized on the tongue, gum, and palate. Less commonly, lesions form in the child’s throat or on the face.
Note! With a herpetic lesion, an abscess may appear on the lip, around the mouth and even on the wings of the nose.
Features of fungal stomatitis
Infectious stomatitis of fungal etiology occurs when a large number of pathogenic microorganisms enter the baby’s oral cavity or active reproduction of existing ones begins. In children, candidal stomatitis is characterized by the following manifestations:
- temperature rise up to 40 degrees;
- enlargement and hardening of lymph nodes;
- the formation of a white coating with a cheesy consistency;
- smell from the mouth;
- pain of ulcers.
Babies become capricious, may cry and refuse to eat. The fact is that almost any product upon contact with the mucous membrane of the mouth causes even more severe pain. If the formed plaque is removed, the opened lesions may bleed.
Some children complain of dry mouth and itching. The mucous membrane burns and causes a lot of anxiety for the child. That is why sometimes first aid is to relieve pain and reduce symptoms.
Features of bacterial stomatitis
Bacterial stomatitis is a common diagnosis among young children. They are exploring the world and, striving for this goal, it is impossible to keep track of them. It is difficult to prevent a child from putting dirty hands in his mouth and picking up things from the floor. That is why, if there is even minor damage to the oral mucosa, the risk of bacterial penetration is extremely high.
Symptoms of the bacterial form of pathology are as follows:
- severe hyperemia of the mucous membrane;
- multiple erosions;
- yellow crusts on sponges;
- profuse drooling;
- putrid odor from the mouth.
A yellowish coating may form in areas of outbreaks. This form of the disease can become purulent. The blisters are filled with purulent or bloody contents.
It is important to start treating the pathology as soon as possible. Otherwise, unpleasant complications may develop. It is important to rinse your mouth many times throughout the day to release any bacteria buildup.
Features of aphthous stomatitis
Aphthous stomatitis is a type of chronic disease. Aphthae, painful necrotic areas, form in the mouth.
Aphthae are usually round in shape and white in color. The disease is accompanied by high fever. Inflated values persist for 10 days.
Features of angular stomatitis
Angular stomatitis is popularly called “jams”. Most often it is associated with a lack of iron in the child’s body. It can occur in a newborn, at 2 years of age, and during school years.
It is important to clearly identify why the problem occurred. After this, the doctor prescribes therapy. The disease is characterized by the formation of painful areas in the corners of the lips.
Therapy for aphthous stomatitis
Since the disease often manifests itself against the background of an allergic reaction to foods, you need to exclude nuts, honey, strawberries, and citrus fruits from the diet . If your baby is taking medications, you should consult your doctor about replacing the prescribed drug with a safer analogue.
Treatment of childhood aphthous stomatitis should include:
- Taking antiallergic medications. Antihistamines include Suprastin, Tavegil, Claritin and many others.
Local treatment of aft. In the early stages of the disease, antiseptic rinses with Miramistin solution and lubrication of the rash with an anti-inflammatory gel with an analgesic effect are indicated. One of these is “Cholisal”. After the acute symptoms have been eliminated, the stage of treating the mucous membrane with epithelizing agents, for example, Solcoseryl gel, begins.
- The use of local immunomodulators. You can use toothpastes based on lysozyme, lactoferrin, glucose oxidase - enzymes that help improve local immunity. It is recommended that adolescent children be given the drug “Imudon”, produced in the form of lozenges. You need to take it five tablets a day for two weeks.
- Sanitation of the oral cavity. One of the causative agents of aphthous stomatitis is staphylococcus, which is abundant in carious lesions and plaque. Therefore, dental diseases are treated before starting drug therapy.
Physiotherapy - irradiation of aphthae with UV rays - has a good effect on the treatment of stomatitis in young children. A pediatric dentist or pediatrician can prescribe a referral to a treatment room.
If the disease manifests itself frequently, an immunological examination should be performed. If this is not enough, then specialists such as an endocrinologist, gastroenterologist, and otolaryngologist help identify the pathology that led to the development of chronic recurrent aphthous stomatitis.
Complications after stomatitis
Although stomatitis may seem like a relatively harmless disease, if you do not provide qualified assistance to your baby, the following consequences are possible:
- decreased general immunity;
- vulnerability to infectious diseases;
- dental exacerbations;
- weight loss and developmental delay due to refusal to eat due to pain.
To prevent all possible unpleasant phenomena caused by this disease, it is important to get rid of stomatitis in the mouth as soon as possible. First you need to contact your pediatrician and undergo an examination.
General signs of stomatitis in children
Symptoms of stomatitis in children are divided into two main groups:
- Local (local). These include swelling, hyperemia (redness), rashes on the tongue and mucous membranes.
- Are common. This is a rise in temperature, weakness, rapid fatigue, chills.
How to understand that a child has stomatitis?
Signs of the manifestation of the described disease in children are redness and rashes on the mucous membrane, the appearance of plaque on the lips, tongue, cheeks, pain in the mouth that appears during conversation and eating.
Stomatitis in an infant is manifested by complete refusal of food. The baby is worried and constantly cries.
The famous pediatrician Komarovsky E.O. puts forward the theory that the fundamental cause of stomatitis of all forms in children is changes in the bactericidal composition of saliva.
Diagnosis of the disease
To choose the right treatment methods, the doctor needs to receive the results of the examination. It is not always easy to determine the causative agent of a disease by eye and choose the best medicine.
The following tests may be recommended:
- examining a smear under a microscope;
- cytology;
- PCR analysis;
- enzyme immunoassay.
For research, the child’s blood, a scraping from the oral mucosa, or even a smear can be taken.
Note! If stomatitis develops frequently, it is necessary to determine the blood sugar level, since fungal infections often occur at high levels.
If a child's stomatitis is chronic, a more complete examination may be required. Perhaps the reason is in the internal organs or in the presence of a parasitic disease. An ultrasound examination, stool and blood analysis for the presence of worms are performed.
After the diagnosis, the doctor will be able to issue a prescription that will take into account all the individual characteristics and needs of the little patient.
Types of disease
Taking into account the cause of the disease, the following types of stomatitis are noted:
- allergic - appears during exposure to an external agent on the body. A common phenomenon in children, difficult to treat;
- catarrhal - characterized by a tendency to chronicity and a blurred clinical picture;
aphthous - is the result of advanced stomatitis of herpes origin;
- herpetic - appears as a result of infection with the human papillomavirus. Often observed in children at one year of age;
- traumatic - appears after injuries to the mucous membrane and is dangerous due to infection;
- infectious (viral) - caused by parainfluenza virus, influenza, measles, chickenpox, adenovirus;
- ulcerative - can be both a complication of catarrhal stomatitis and an independent form;
- bacterial - the causative agents are streptococci and staphylococci. This type includes diphtheria and gonorrheal stomatitis;
- candidiasis - appears due to the proliferation of fungi of the Candida group in the oral cavity. As a rule, it is observed in one-year-old infants and in children aged two years.
Principles of treatment
Stomatitis is treated at home. The general principles of therapy are as follows:
- diet;
- anesthesia;
- Regular treatment of the oral cavity with prescribed medications.
It is very important to treat teeth with stomatitis. Bacteria can often accumulate in carious teeth, which complicates treatment and increases the rehabilitation period.
Mouth rinses
Regardless of what type of stomatitis you encounter, rinsing your mouth with antiseptics is extremely important. Some people use plain water.
Although this has some effect, it will be more beneficial if special medications are used:
- "Chlorophyllipt";
- "Chlorhexidine";
- "Furacilin";
- "Lugol";
- "Malavit."
The herbal antiseptic “Tonsilgon” has proven itself well. This drug contains practically no substances that could have contraindications or cause a negative reaction in a small organism.
Simpler methods are also suitable, for example, a solution of hydrogen peroxide or iodine. Folk methods of cleansing the oral cavity include rinsing with a decoction of chamomile, oak bark, burdock, yarrow or elecampane. You can use one substance or combine herbs.
During the healing stage, you can add cosmetic oils of peach, olive or flax to rinsing solutions.
How to relieve pain
At the very beginning of treatment for stomatitis, it is extremely important to anesthetize all erosions and ulcers. Such medicines are available in the form of gels, aerosols and sprays.
The following medications effectively relieve pain in the mouth:
- "Tantum Verde";
- "Kamistad";
- "Holisal";
- "Hexoral";
- "Kalgel".
These are only general recommendations for the treatment of stomatitis of various etiologies. However, when prescribing a course of treatment, the doctor will definitely take into account the cause of the disease.
Treatment of the bacterial form
Ointment for stomatitis, the cause of which is the penetration of bacteria, can be based on antibiotics. The oral cavity must be treated with Miramistin solution. In severe cases, therapy with medications in tablets may be prescribed.
Doctors often prescribe the drug Augmentin. This broad-spectrum antibiotic effectively fights many bacteria. The medicine is based on Amoxicillin and clavulanate. This medication is not prescribed to patients under 2 years of age.
Note! Children at an early age are rarely prescribed tablets or injections for stomatitis; these forms of the drug are replaced with suspensions.
The drug "Metrogil Denta" is a gel used for bacterial infections. The composition contains an antibiotic and an antiseptic. Used in patients over 6 years of age. Apply the product directly to the lesions in the mouth using a cotton swab or finger.
Other antibacterial agents, for example, Grammidin, may also be prescribed. Levomekol ointment can be used topically.
Treatment of the viral form
Rinsing and treating the oral cavity with antiseptic agents is mandatory. Miramistin is recommended. The product is applied using a cotton swab or gauze. At an older age, you can use aerosols.
It is important to use drugs that have antiviral and immunomodulatory effects:
- "Viferon";
- "Acyclovir";
- "Oxolin."
Before applying medicinal products, the skin in the affected areas should be dried using cotton swabs. Typically the duration of use is about a week.
Note! Oxolinic ointment is used mainly externally, as it is weakly attached to the mucous membranes.
Treatment of fungal form
It is important to regularly rinse fungal stomatitis with antiseptics or soda solution. Soda perfectly neutralizes the environment nutritious for fungi. After the procedure, relief comes quickly. It is important to rinse at least 4 times a day.
The following antifungal agents can be used:
- "Nystatin";
- "Fukortsin";
- "Fluconazole".
It is important to agree on the dosage and treatment regimen with your doctor. Much depends on the child’s age and body weight. Some drugs are not prescribed to infants.
Restoration of the mucosa
Even after the main lesions are eliminated and the pain is not so severe, it is important to help the skin fully recover. For this purpose, the following regenerating drugs are used:
- "Solcoseryl";
- "Aekol";
- "Methyluracil".
You can use oil solutions and drops containing sea buckthorn, rose hips, propolis and vitamins.
What to be careful with
When treating stomatitis, it is not recommended to use products that irritate the oral mucosa, for example, boric acid, alcohol and similar substances.
You should also avoid using brilliant green, methylene blue solution (or blue). Some doctors are of the opinion that it is not advisable to use Fukortsin when treating children, but the drug can be used as prescribed by a doctor.
Treatment with folk remedies can be combined with the main therapy, but it is important to talk about this with a specialist. Parents must provide the child with food that does not injure the mucous membrane of the mouth or burn it. The temperature of the food should be warm. It is important to exclude everything salty, spicy or sour.
It is necessary to provide the baby with plenty of fluids. Using this method, you can prevent drying out of the oral mucosa, and thereby speed up recovery.
You can bathe a child with stomatitis, but it is better to avoid the procedure if the baby has a high fever or the disease occurs with complications.
Treatment of childhood stomatitis
How to treat stomatitis in children depends on the form of the disease.
It is important to make a correct diagnosis so that relief occurs as soon as possible. How to treat stomatitis in children with its different forms? Herpetic stomatitis in children is treated with antiviral drugs containing acyclovir (Zovirax, Acyclovir, Valtrex). These drugs are prescribed locally and for oral administration.
Immunomodulators are also used locally - Viferon gel and Imudon (lozenges).
For local treatment, antiseptic solutions (Miramistin, Chlorhexidine) are used.
- Treatment of aphthous stomatitis in children includes the use of Cholisal gel, which has an anti-inflammatory and analgesic effect. When stomatitis occurs in an infant, gels used during teething (Dentinox) are usually prescribed;
- Treatment of candidal stomatitis in children consists of treating the mucous membrane and taking oral antifungal drugs. If stomatitis is caused by taking antibiotics, you should, if possible, stop taking them and give the child means to restore the microflora.
When the temperature rises and intoxication, drugs based on ibuprofen (Nurofen, Panadol) are used.
Stomatitis in children under one year old at elevated temperatures can be accompanied by intoxication and dehydration, so it is very important to follow the drinking regime (warm, fractional drinks with the exception of acidic drinks and juices).
Treatment of stomatitis in children usually takes place at home. Inpatient treatment is prescribed for persistent relapses and prolonged course of the disease.
Do not use sprays containing 10% lidocaine when treating stomatitis in children. They provide excellent pain relief, but can cause burns on the thin mucous membrane. It is necessary to exclude dyes (potassium permanganate, brilliant green), since they do not help speed up healing, but at the same time stain the mucous membrane and can hide the true course of the disease.
Treatment of stomatitis in children with folk remedies involves the use of plant substances that have immunomodulatory properties (aloe, rose hips, honey, propolis, cranberry).
Stomatitis in infants should in no case be accompanied by cessation of breastfeeding. Even if the baby refuses to suckle due to pain. In this case, you should pump.
It is impossible to answer exactly how long stomatitis lasts in children. Usually, from the first manifestations to complete recovery, it takes from 7 to 14 days. The severity and duration of stomatitis depend on the condition of the child’s body, his immunity and the form of the disease.
In the treatment of stomatitis, it is important to start a comprehensive approach from the first manifestations of the disease. Delaying an appointment with a specialist and self-medicating is extremely undesirable. Therefore, the question of how to quickly cure stomatitis in a child has only one answer: it must be treated under the supervision of a specialist.
Causes of the disease
They are determined by imperfect immunity, anatomical features of the child’s oral mucosa and failure to comply with basic hygiene rules. Young children have a weak immune system and are therefore more susceptible to the influence of pathogens. If the baby has a thin and delicate mucous membrane, it is easily injured, wounds are formed, into which pathogenic agents quickly penetrate. For example, when a child, when teething, pulls various objects into his mouth to scratch his gums, the same applies to eating unwashed fruits. In addition, the saliva of an adult has antiseptic properties, that is, the adult body successfully fights the penetration of pathogenic microorganisms, which is why children are more susceptible to stomatitis.
The disease develops from the introduction and active reproduction of bacteria, viruses, fungi, under the influence of allergens, traumatic factors, and the presence of an autoimmune disease. Stomatitis can also occur due to hypovitaminosis, diabetes mellitus, iron deficiency or due to taking antibiotics, with hormonal changes in the body during puberty.
There are also factors that increase the likelihood of developing the disease:
- lack of hygiene;
- state of constant stress;
- poor quality, unbalanced nutrition;
- severe hypothermia or overheating;
- hereditary predisposition.
Therapy for aphthous type
When the first aphthae are detected, it is important to immediately exclude allergenic, coarse, and spicy foods from the diet. Treatment consists of the following medications:
Antihistamines
- " Suprastin ": children under one year old, 1/4 tablet. 2-3 times a day, from 1 to 6 years, 1/4 tablet. 3-4 times or 1/2 tablet. 2 times, from 6 to 14 years 1/2 3 times;
- " Tavegil ": recommended from 6 years, 1/2 tablet. in the morning and at night.
Antiseptic rinses
- " Miramistin ": used for rinsing, wiping (spraying) the mucous membrane 3-4 times a day. Once the acute signs of the disease have disappeared, you can rinse your mouth 5-7 times a day with solutions of baking soda (1 tsp of soda for 1 cup of water) or 2% boric acid (diluted like soda).
Means for treating mucous membranes
- " Bonafton ": applied 3-4 times/day for 5-10 minutes. during the week;
- " Lugol ": treatment is performed after eating (after 30-40 minutes).
The solution is applied to the affected area every 5 hours, and its application is repeated after 3 minutes. In 1 session you need to do 3 treatments. If a gag reflex appears, you can carry out the procedure with the drug in the form of a spray: the mucous membrane is irrigated 4-6 times at the same time interval (for a child, 1 press is enough). "Lugol" is used for 3 days, a second course is allowed after 3 days. - " Gexoral ": used to irrigate the mouth after eating. Children from 6 years of age are treated with 1 spray twice a day (treatment of children from 3 to 6 years of age is discussed with the doctor individually).
- “ Vinilin ”: problem areas are treated with a tampon soaked in balm twice a day before meals.
Physiotherapy
Ultraviolet irradiation gives good results.
A referral for the procedure is given by a pediatrician or dentist. Since the main “culprit” of the disease is staphylococcus (a microorganism present in plaque and carious cavities), it is necessary to sanitize the oral cavity.
Prevention
Preventing stomatitis is a very important and not so difficult task:
- Monitor your child’s diet: regular and only healthy. It is important to drink plenty of fluids.
- Strengthen the baby's immunity.
- Protect from crowds of people during periods of influenza and ARVI epidemics.
- Keep your home clean and ventilate the room regularly.
- Do not treat the child yourself without a doctor’s prescription, especially with antibiotics, which kill all beneficial flora.
It is better to prevent stomatitis by making some efforts than by spending a lot of nerves, money and time on treatment. In addition, infectious diseases can lead to serious pathologies in the functioning of the heart and other internal organs, especially in fragile children.
Useful article? Add to your bookmarks!
Causes of disease development in the mouth
The health of the oral mucosa depends on saliva . It has disinfecting properties and blocks the development of pathogenic bacteria in the microflora. But if the composition of saliva changes , it no longer copes with its functions. This happens due to dehydration. Dry or indoor air a small amount of fluid intake, lead to dehydration
Reference! The main signs of dehydration: dry mouth, thirst, infrequent bladder emptying, dark urine, pale face, dark circles under the eyes.
Common causes of stomatitis:
- weak immunity (usually a consequence of long-term or frequent illnesses);
- avitaminosis;
- poor living conditions;
- poor oral hygiene
- untimely treatment of dental diseases;
- taking antibiotics , which lead to disruption of the microflora.
The main cause of infection is infection entering the body . The infection gets to the mucous membrane due to non-compliance with hygiene rules.
It is especially dangerous if the child has injuries in the oral cavity.
Symptoms of stomatitis
In the early stages of the disease, redness, slight swelling, and burning appear (see photo above). Later, round or oval ulcers, covered with a thin film of gray or white color, form on the tongue, inside the cheeks and lips. The ulcers are surrounded by a reddish border, the surrounding tissues appear to be quite healthy. When eating food, discomfort and pain are felt, it becomes difficult to move the tongue and lips.
Multiple appearances of ulcers located at a distance from each other are possible. If the ulcers are close together, they merge . The manifestation of the disease is possible several times a year (relapses), in which case the disease can be defined as chronic.
There is a more severe form of the disease with the formation of large and deep ulcers (aphthous). Accompanied by the disease:
- bad breath
- increased salivation,
- increased sensitivity of the tongue.
Getting to the heart of the disease
First, let's figure out what stomatitis is. This is inflammation in the mucous tissues on the surface of the oral cavity. It may be infectious, viral, fungal or allergic in origin.
Pathology appears due to the body’s defensive reaction to foreign molecules. Their invasion activates immune cells. As a result, inflammatory foci form on the oral mucosa, which are called stomatitis.
The disease occurs in people of any age. Today we will look at childhood stomatitis according to the following points:
- causes;
- types of stomatitis;
- symptoms;
- how pathology is treated.
Diagnosis of stomatitis
To determine the nature of the disease, a scraping or smear is taken from the oral mucosa from a sick child. Using PCR , ELISA they determine what caused the disease: viruses or bacteria .
They also take a blood test , which determines the state of immunity. If the disease is chronic or constantly relapses , the patient donates blood for sugar. If necessary, the patient is prescribed a consultation with an endocrinologist, dentist and gastroenterologist.