Antibiotic treatment of pneumonia in adults: scheme and course.
Treatment of pneumonia is carried out mainly in a hospital setting.
In some situations (for example, with the development of respiratory failure), resuscitation measures may be required, so staying at home after establishing and confirming the diagnosis is unacceptable, especially if we are talking about severe forms of pneumonia: bilateral, congestive, streptococcal or klebsiella.
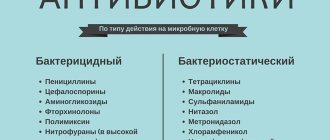
Antibiotics for pneumonia are the basic basis for treatment tactics for patients of any age and with any form of diagnosis.
Selecting an effective drug for a pulmonary infection is a very difficult task, since all drugs have varying degrees of activity against harmful organisms (infectious agents).
In some cases, you have to wait more than 10 days for the results of a special sensitivity test.
Such a period can cost the patient his life, so it is important to know the basics of antibacterial therapy in order to provide the patient with the necessary assistance and begin treatment at the initial stage.
- When is hospitalization necessary?
- Antibacterial therapy of pneumonia in adults
- Antibiotic treatment regimen for pneumonia in adults
- Antibiotic treatment of pneumonia in adults according to the type of pathogen
- Errors in prescribing antibiotics for pneumonia
- Nosocomial and community-acquired pneumonia
- If antibiotics don't help with pneumonia
The main reasons for the development of the disease
Which antibiotics to take for pneumonia in adults in each specific case can only be determined by a doctor based on a thorough examination of patients and clinical tests. It is known that the disease can be caused by the activation of pathogenic microorganisms. But the causes of the development of pathology can be a variety of bacteria:
- Pneumococci. In more than half of the cases, these microorganisms are diagnosed.
- Staphylococci. Found in 5% of cases.
- Haemophilus influenzae. Laboratory tests reveal it in 6-7% of cases.
- Enterobacteria and mycoplasma. Detected in 6% of cases.
Other causes include streptococci, legionella and E. coli. Such microorganisms are found in 2-4% of cases.
In this regard, only a specialist will be able to tell you which antibiotics for pneumonia in adults will be effective, because each of them has a different active composition.
Modern macrolides in the treatment of community-acquired pneumonia
Pneumonia is a group of acute infectious (mainly bacterial) diseases of different etiology, pathogenesis and morphology, characterized by focal damage to the respiratory parts of the lungs with intra-alveolar exudation, detected during physical and x-ray examinations, as well as feverish reaction and intoxication expressed to varying degrees (Russian Respiratory Society, 2010). According to the Central Research Institute for Organization and Informatization of Healthcare of the Ministry of Health of the Russian Federation, 424,457 people suffered from pneumonia in 2008, and in 2009 - 449,673 patients [1, 2]. The incidence rate of pneumonia is significantly higher in elderly patients and ranges from 25 to 114 per 1000 people per year [3].
Pneumonia ranks first among the causes of mortality from infectious diseases and sixth among all causes of mortality [4]. The most common deaths are observed in cases of severe pneumonia, especially in socially disadvantaged individuals or in patients with severe comorbidities [5, 6].
The following types of pneumonia are distinguished:
- community-acquired pneumonia (home, outpatient) is an acute disease that arose in a community setting, i.e., outside the hospital, diagnosed in the first 48 hours from hospitalization [7];
- nosocomial pneumonia (hospital, nosocomial) - a disease characterized by the appearance on an x-ray of “fresh” focally infiltrative changes in the lungs and clinical data confirming their infectious nature (a new wave of fever, purulent sputum or purulent discharge of the tracheobronchial tree, leukocytosis, etc.) later 48 hours or more after hospitalization [8];
- aspiration pneumonia (with epilepsy, swallowing disorders, vomiting) - pulmonary lesions resulting from aspiration (microaspiration) of a larger or smaller amount of contaminated contents of the nasopharynx, oral cavity or stomach and the subsequent development of an infectious process [9];
- pneumonia in persons with severe immune defects (congenital immunodeficiency, HIV infection, drug addiction, chronic alcohol intoxication, malignant neoplasms, agranulocytosis, use of immunosuppressive therapy).
Community-acquired pneumonia is the largest group, characterized by a severe course and a high risk of complications, including pleurisy, abscesses and other purulent-destructive processes [10].
All community-acquired pneumonia are divided into the following groups:
- pneumonia that does not require hospitalization;
- pneumonia requiring hospitalization;
- pneumonia requiring hospitalization in intensive care units [11].
Risk factors for the unfavorable course of community-acquired pneumonia are:
1. Age over 60 years.
2. Concomitant diseases:
- chronic obstructive pulmonary disease (COPD);
- bronchiectasis;
- malignant neoplasms;
- diabetes mellitus (DM);
- chronic renal failure;
- congestive heart failure;
- chronic alcohol intoxication (CAI);
- addiction;
- severe body weight deficiency;
- past cerebrovascular diseases.
3. Ineffectiveness of initial antibiotic therapy.
Urgent hospitalization in intensive care units is required in cases where the patient has signs of severe community-acquired pneumonia, which include:
- respiratory rate more than 30 per minute;
- systolic blood pressure (SBP) below 90 mm Hg. Art.;
- the presence of bilateral or multilobar pneumonic infiltration;
- rapid progression of focal infiltrative changes in the lungs;
- septic shock;
- the need to administer vasopressors;
- acute renal failure.
It is known that in community-acquired pneumonia, the main pathogen is pneumococcus (Streptococcus pneumoniae) [12], the second most important pathogen is Haemophilus influenzae [13].
In addition to mandatory laboratory and instrumental studies, various PSI and CURB-65/CRB-65 scales are currently used in the diagnosis of community-acquired pneumonia [14].
In order to determine the risk factors, prevalence, structure and frequency of deaths due to pneumonia in a multidisciplinary emergency hospital, the authors conducted a retrospective study, during which 180,727 inpatient records were analyzed. Of these, 172,420 patients (95.5%) were treated and discharged, 1677 (0.9%) patients were transferred to other health care facilities, and 6630 patients (3.6%) died.
Of the deaths, the study included 1497 cases of community-acquired pneumonia confirmed at the section, which were divided by the authors into two subgroups: “Community-acquired pneumonia as the main disease” (I) included 97 patients (6.4%) and “Community-acquired pneumonia as a complication of the main disease "(II) included 1400 (93.6%) patients (Fig. 1).
Among the 1497 deceased patients with community-acquired pneumonia, there were 768 men (51.4%) and 729 women (48.6%) (Fig. 2).
The age structure of 1497 patients with community-acquired pneumonia is presented in Fig. 3. As can be seen from this illustration, the majority of patients (43%) were over 75 years of age.
Of the 1497 cases of community-acquired pneumonia that resulted in death, in 136 observations (9%) there was a discrepancy between the clinical and pathological diagnoses (Fig. 4).
According to the nature of the lesion, pleuropneumonia occurred in 49.4% of cases, focal confluent pneumonia - in 22.6%, abscess pneumonia - in 19.5%, and focal pneumonia - in 8.5% of cases.
By localization, bilateral community-acquired pneumonia was more common - 41 (42.2%). A summary table of the locations of pulmonary tissue damage in community-acquired pneumonia is presented below (Table 1).
Community-acquired pneumonia was combined with CAI in 71.1% of cases, with previous stroke in 56% of cases, with COPD in 24.7% of cases, with multifocal atherosclerosis in 32% of cases, with ischemic disease in 25.7% of cases heart disease (CHD), in 20.6% of events - with type 2 diabetes (Fig. 5).
Thus, in the vast majority of observations, community-acquired pneumonia is secondary, i.e., it is a complication of the main or background disease, aggravates its course and worsens the prognosis of patients. The data obtained by the authors in case of suspected pneumonia dictate the need for a diagnostic search aimed at identifying the substrate for the development of the inflammatory process in the lung tissue. In this regard, diagnosis, and often treatment of community-acquired pneumonia remains one of the pressing problems of modern therapy. The choice of antibiotic for the treatment of pneumonia is usually done empirically. In this case, the guidelines for its choice are the epidemiological situation, the expected sensitivity of the flora (Table 2) and some other aggravating factors [15].
The semisynthetic macrolide clarithromycin, along with aminopenicillins and respiratory fluoroquinolones, occupies one of the leading positions in the treatment of community-acquired pneumonia and other infectious diseases of the lower respiratory tract. The multifaceted etiopathogenetic effect of clarithromycin on the process of bacterial inflammation ensures its high effectiveness, confirmed in a number of comparative studies. The antimicrobial spectrum of clarithromycin, including S. pneumonia, H. influenza, as well as new prolonged forms of the drug, determines its demand in the treatment of this category of patients. In the presence of atypical mycobacteria and Pseudomonas aeruginosa, clarithromycin is used in combination with other antimicrobial drugs, significantly increasing the effectiveness of the therapy.
The mechanism of the antimicrobial action of clarithromycin is due to a violation of protein synthesis in the microbial cell. As a result of reversible binding to the 50 S-subunit of ribosomes and inhibition of translocation and transpeptidation reactions, the formation and growth of the peptide chain is inhibited [16]. The main effect of clarithromycin is bacteriostatic, but at high concentrations and low microbial density the drug has a bactericidal effect against S. pyogenes and S. pneumoniae. Moreover, the antimicrobial activity against these pathogens and methicillin-sensitive strains of Staphylococcus aureus is 2–4 times higher than that of erythromycin [17].
Many clinical studies and as a result of many years of experience in use have revealed the high effectiveness of clarithromycin in the treatment of lower respiratory tract infections. According to the results of a study that included 252 patients with community-acquired pneumonia, a 7-day course of treatment with extended-release clarithromycin (1000 mg once daily) was as clinically effective as a similar duration of treatment with levofloxacin (500 mg once daily). The overall rates of pathogen eradication (87% and 88%, respectively) and radiographic improvement (95% and 88%, respectively) also did not differ. Both drugs turned out to be equally effective against both typical and atypical pathogens [18].
In severe cases of community-acquired pneumonia in a hospital setting, combination therapy is more effective. This has been confirmed by many clinical observations. A cohort study involving 1391 patients with community-acquired pneumonia found that mortality during treatment with a combination of a third-generation cephalosporin with a macrolide was 2 times lower than with beta-lactam monotherapy [19]. Another study showed that the combination of a beta-lactam with a macrolide is more effective than that of a beta-lactam with a fluoroquinolone (mortality rate - 4.9% and 15.0%, respectively) [20].
Regardless of the antimicrobial effect, clarithromycin, like a number of other macrolides, exhibits anti-inflammatory, immunomodulatory and mucoregulatory effects at the level of the respiratory system. Clarithromycin has a modulating effect on phagocytosis, chemotaxis, killing and apoptosis of neutrophils. The oxidative “explosion” is inhibited, resulting in a decrease in the formation of highly active compounds that can damage one’s own tissues. The synthesis and/or secretion of pro-inflammatory cytokines (interleukins-1, 6, 8, tumor necrosis factor alpha) is inhibited and the secretion of anti-inflammatory cytokines (interleukins-2, 4, 10) is enhanced [21].
Thus, the presence of additional properties, along with high antibacterial activity, ensures rapid regression of symptoms and improvement in the condition of patients when treated with clarithromycin for respiratory tract infections.
Clarithromycin has rightfully occupied its niche in the treatment of acute and chronic respiratory tract infections. It retains one of the leading positions in outpatient practice and in the pharmaceutical market of the Russian Federation, which is due to its wide spectrum of activity, rapid achievement of high peak concentrations at the site of infection and a favorable safety profile. A dosage form with a delayed release of the active substance due to a special surface layer and matrix base (Klacid SR) is identical in effectiveness to the standard one, is better tolerated, improves compliance and can be recommended for active use. The evidence available today on non-antibacterial action, combined with the favorable clinical and pharmacological characteristics of clarithromycin, allows us to consider it as an adjuvant drug in the treatment of many respiratory diseases.
Literature
- Morbidity rate of the Russian population in 2007. Statistical materials of the Ministry of Health and Social Development of Russia, 2008, 527–572.
- Community-acquired pneumonia in adults. Clinical recommendations (edited by A. G. Chuchalin, A. I. Sinopalnikov). M.: Atmosphere, 2005.
- Zilber A.P. Sketches of respiratory medicine. M.: Medpress-inform, 2007.
- Ewig S. Community-acquired pneumonia. Epidemiology, risk, and prognosis // Eur Respir Mon. 1997; 3: 13–35.
- Mira JP., Max A., Burgel P.-R. The role of biomarkers in community-acquired pneumonia: predicting mortality and response to adjunctive therapy // Critical Care. 2008; 12(Suppl. 6):S5 1–7.
- Rodriguez R., Fancher M., Phelps M. An emergency department based randomized trial of nonbronchoscopic bronchoalveolar lavage for early pathogen identification in severe community-acquired pneumonia // Ann Emerg Med. 2001; 38: 357–363.
- Vardakas KZ, Siempo II, Grammatikos A. Respiratory fluoroquinolones for the treatment of community-acquired pneumonia: a meta-analysis of randomized controlled trials // CMAJ. 2008; 179(12):1269–1277.
- Drummond MF, Becker DL, Hux M. An economic evaluation of sequential iv/po moxifloxacin therapy compared to iv/po coamoxiclav with or without clarithromycin in the treatment of community-acquired pneumonia // Chest. 2003; 124:526–535.
- Landen H., Moller M., Tillotson GS Clinical experience in Germany of treating community-acquired respiratory infections with the new 8-methoxyfluoroquinolone, moxifloxacin // J Int Med Res. 2001; 29:51–60.
- Li X., Zhao X., Drlica K. Selection of Streptococcus pneumoniae having reduced susceptibility to levofloxacin and moxifloxacin // Antimicrob Agents Chemoter. 2002; 46:522–524.
- Marrie TJ, Peeling RW, Fine MJ Ambulatory patients with community-acquired pneumoniae: the frequency of atypical agents and clinical course // Am J Med. 1996; 101:508–515.
- Sethi S. The role of antibiotics in acute exacerbation of COPD // Curr Infect Dis Rep. 2003; (5): 9–15.
- Torres A., Muir J.-F., Corris P. Effectiveness of oral moxifloxacin in standard first-line therapy in community-acquired pneumonia // Eur Respir J. 2003; 21: 135–143.
- Wilson W. Short-term and long-term outcomes of moxifloxacin compared to standard antimicrobic treatment in acute exacerbation of chronic bronchitis // Chest. 2004; 125:(3):953–964.
- Bartlett JG, Dowell SF, Mandell LA Practice guidelines for the management of community-acquired pneumonia in adults. Infectious Diseases Society of America // Clin Infect Dis. 2000; 31: 347–382.
- Wozniak DJ, Keyser R. Effects of subinhibitory concentrations of macrolide antibiotics on Pseudomonas aeruginosa // Chest. 2004; 125: 62 S-9 S.
- Sivapalasingam S., Steigbigel NH Macrolides, clindamycin, and ketolides. Pronciples & Practice of Infectious Diseases // Churchill Livingstone, 6th edition. 2004: 396–417.
- Kozlov RS, Sivaja OV, Stratchounski LS 7-year monitoring of resistance of clinical S. pneumoniae in Russia: results of prospective multicenter study (PEHASus) // Proc 45th ICAAC, 2005, Washington DC.
- Stahl JE, Barza M., DesJaidin J. Effect of macrolides as part of initial empiric therapy on length of stay in patients hospitalized with community-acquired pneumonia // Arch Intern Med. 1999; 159:2576–2580.
- Martinez JA, Horcajada JP, Almela M. Addition of a macrolide to a beta-lactam-based empirical antibiotic regimen is associated with lower in-hospital mortality for patients with bacteremic pneumococcal pneumonia // Clin Infect Dis. 2003; 36:389–395.
- Martinot JB, Carr WD, Cullen S. Clarithromycin Once-a-Day Study Group. A comparative study of clarithromycin modified release and amoxicillin/clavulanic acid in the treatment of acute exacerbation of chronic bronchitis // Adv Ther. 2001; 18:1–11.
A. L. Vertkin, Doctor of Medical Sciences, Professor Zh. M. Oralbekova A. S. Skotnikov, Candidate of Medical Sciences
GBOU VPO MGMSU Ministry of Health and Social Development of Russia , Moscow
Contact information for authors for correspondence
Buy an issue with this article in pdf
Risk factors
Pneumonia in an adult does not occur just like that. The most common risk factors are:
- Weakened immunity.
- Poor nutrition, when the diet does not contain enough quality meat, fresh fish, vegetables and fruits.
- Frequent stress.
Often, persistent colds provoke the occurrence of pathology. The result is a chronic infectious focus that promotes the proliferation of microorganisms. Alcoholism and smoking are also considered risk factors.
Nosocomial and community-acquired pneumonia
There are some differences in the prescription of treatment regimens for nosocomial infections and diseases that occur outside the hospital.
In any case, the mainstay of treatment for any inflammation caused by bacteria is antibiotics.
In the first few days of treatment, an infusion (droppers) or injection (injections) form of drug administration is used, as this promotes the rapid accumulation of active substances in the blood plasma and their transportation to organs and tissues.
On days 3-4 the patient is transferred to oral administration.
Folk remedies for pneumonia in adults: recipes
Folk remedies for treating pneumonia at home. Some people try not to use medicinal... “Read more”
Variety of pathologies
Which antibiotics for pneumonia in adults can contribute to recovery depends on the etiology of the disease. According to medical terminology, the types of pneumonia are as follows:
- viral;
- bacterial;
- fungal;
- mycoplasma;
- mixed.
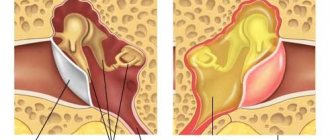
Depending on the identification of the species, the doctor prescribes a suitable antibiotic. The most common pathology is hospital-acquired pneumonia. The disease can develop in a patient within three days after being admitted to the hospital. Microorganisms settle in the lower respiratory tract, entering through the nasopharynx and gastrointestinal tract.
Depending on the course, experts distinguish pneumonia:
- spicy;
- atypical;
- chronic.
In addition, pneumonia is divided into right-sided, left-sided and bilateral. The disease can be mild or severe in severity.
Treatment of pneumonia at home in adults and children
Treatment of pneumonia at home can be carried out only after examination by a doctor and the appointment of appropriate therapy, if there are no indications for hospital treatment.
It should be noted that about 80% of patients (including older children) with community-acquired pneumonia can be treated at home, as well as in a day hospital.
Indications for treatment in a hospital are:
- the patient’s age is less than six months or older than 65 years (this category of patients has too high a risk of developing DN and other complications, so treatment should be carried out only in a hospital setting);
- severe pneumonia;
- presence of pregnancy;
- suspicion of atypical pneumonia;
- the patient has underlying diseases that can aggravate the course of pneumonia and cause complications. Patients with congenital heart defects, cystic fibrosis, bronchopulmonary dysplasia, bronchiectasis, immunodeficiency conditions, diabetes mellitus, etc. are subject to hospitalization;
- patients who have recently completed or are currently receiving immunosuppressive therapy;
- pneumonia is treated with antibiotics within 48 hours to no avail, with clinical symptoms progressing. Those. in an adult patient, fever persists, respiratory failure increases, etc.;
- lack of conditions for treatment at home (children from disadvantaged families, boarding schools, patients living in hostels, etc.) are hospitalized.
Read more: How to take antibiotics correctly and how often you can take them
Antibiotic for pneumonia in adults: names, list
Antibiotics should be the basis of treatment for pneumonia. But the choice of specific tablets depends entirely on the identified pathogenic microorganism that caused the development of the pathology. Pulmonologists use the following types of drugs in their practice:
- Penicillins. They can be either synthetically produced or natural. Used for pneumococcal and staphylococcal infections.
- Tetracyclines. Capable of killing many pathogens.
- Cephalosporins. Effective against gram-negative bacteria and E. coli.
- Fluoroquinolones. Doctors prescribe them for diagnosed bacterial pneumonia.
- Macrolides. If pneumonia is caused by mycoplasma, then with the help of this type of pills you can quickly stop the inflammatory process.
Antibiotic tablets for pneumonia in adults can be prescribed by a pulmonologist based on clinical tests. But it is important to remember that such drugs should be taken at regular intervals, strictly following the recommended dosage, and not interrupt the prescribed course.
Regardless of the severity of the disease, in the first days of the development of the pathology, the patient is prescribed bed rest. Next, we will consider the most famous and effective antibiotics in the form of tablets from the types described above.
Causes of pneumonia
Pneumonia usually develops against a background of weakened immunity and can be caused by viruses, fungi or bacteria. The choice of pneumonia medications for adults depends on the severity of the disease and the type of bacteria that causes it.
Typically inflammation is caused by the following microbes:
- Staphylococci.
- Pneumococci.
- Chlamydia.
- Candida.
- Streptococci.
- Haemophilus influenzae.
- Pseudomonas aeruginosa and some other types of bacteria.
Conventionally, the types of disease can be divided into 3 categories, based on which tablets for pneumonia are selected: hospital-acquired, community-acquired and first aid-induced pneumonia. Community-acquired pneumonia can be typical or atypical and is caused by a certain type of bacteria and viruses. Hospital illness develops in patients staying in hospitals, as well as with artificial ventilation or excessively weakened immunity.
Doctors also divide pneumonia into 3 groups according to the form of its course: mild, moderate and severe. The severity is determined by the doctor after a full medical examination. The first two stages of the disease can be cured by taking tablets orally, while in the third stage injections or droppers are usually prescribed for a faster effect of the drug on the body.
Penicillin series
The most commonly recommended antibiotics are penicillin for pneumonia in adults. The list of known ones is:
- "Amoxicillin";
- "Ampicillin";
- "Amoxiclav".
Amoxicillin in tablet form is prescribed three times a day. The dosage for adult patients is usually 500 mg. However, depending on the severity of the pathology, the doctor may increase it to 1 g. “Ampicillin” has similar instructions for use.
"Amoxiclav" is produced on the basis of two active components and contains semi-synthetic produced penicillin amoxicillin, as well as clavulanic acid. The dosage is prescribed depending on the severity of the disease. Doctors usually recommend taking 250 mg orally two or three times a day.
What injections can be prescribed to treat both forms of pneumonia?
Nosocomial infection:
- penicillin in combination with clavulanic acid;
- fluoroquinolones (“Tsiprobay”, “Taravid”, “Peflacin”);
- third generation cephalosporins (Klaforan, Fortum);
- carbapenems (“Tienam”);
- aminoglycosides (“Gentamicin”).
Community-acquired infection:
- macrolides (“Rulid”, “Rovamycin”);
- first generation cephalosporins (Cefazolin, Kefzon);
- penicillin with clavulanic acid (Amoxiclav).
In addition to antibiotics, treatment of pneumonia includes taking the following groups of drugs:
- immunomodulators;
- vitamin or vitamin-mineral complexes and supplements;
- absorbents;
- antitussives;
- antiviral (not in all cases).
Depending on the degree of damage, the patient may be prescribed an infusion (intravenously) of blood plasma, interferon, immunoglobulins, etc.
Line of cephalosporins
If the disease is caused by E. coli or gram-negative bacteria, then cephalosporin antibiotics are prescribed for pneumonia in adults. The names of specific drugs are as follows:
- "Cephalexin";
- "Cefepime."
Cephalexin is available in standard pills and capsules. The drug is prescribed 30 minutes before the main meal, 0.25-0.5 g every 6 hours. It is important to take the medicine at least four times a day. "Cefepime" is indicated for pneumonia of mild or moderate severity. To cure, doctors prescribe up to 1 g of antibiotic per dose. There should be 12 hours between taking pills. However, the dosage can be increased by the pulmonologist to 2 g if the patient's condition is severe.
Additional drugs for treatment
Drug treatment of pneumonia is always complex. It also includes taking anti-inflammatory drugs, expectorants and cough medicines.
In most cases, pneumonia is accompanied by a severe cough with the production of viscous sputum, so taking cough medicine is a mandatory part of therapy. When inflammation occurs in the lungs, a secretion begins to be actively produced in the respiratory system - viscous sputum, which not only provides a favorable environment for the proliferation of pathogenic bacteria, but also interferes with normal ventilation of the lungs.
Therefore, taking expectorants is also very important; they dilute mucus and restore natural ventilation of the lungs. As such drugs for pneumonia, mucolytic or secretolytic drugs are prescribed, which have a restorative effect on the ciliary layer of the membrane. Under the influence of mucolytic tablets or syrups, sputum leaves faster and easier.
In order to induce coughing, secretomotor agents are prescribed. However, they are dangerous if blood comes out of the throat during attacks of pneumonic cough. For hemoptysis, secretomotor drugs are prescribed with caution.
Most often, doctors prescribe the following cough tablets for pneumonia in adults:
- Expectorants such as Mucoltin or Thermopsis.
- Tablets for thinning sputum: Bromhexine, Ascoril.
- Carbocisteine or Erdosteine tablets, which prevent excessive phlegm production.
- Effervescent tablets such as Acetylsteine are also prescribed to thin the mucus. They are effective against viscous sputum and have a pronounced expectorant effect.
The doctor will prescribe one type of drug or another; the choice depends on the intensity of the cough and the type of sputum, as well as the presence of other pathologies and the general condition of the patient. If the cough is minor and the sputum does not cause any particular problems, Ambroxol tablets may be prescribed.
If the discharged sputum contains pus, stronger remedies will be required. Patients often take Acetylcysteine.
Macrolide and tetracycline tablets
Antibiotics for the treatment of pneumonia in adults (tablets) should be selected based on the type of microorganism that caused the pathology. Tetracyclines are prescribed quite rarely. This is justified by the fact that this type of antibiotic accumulates in tissues and organs. This causes a large number of side effects. Among the pills, the most popular are:
- "Doxycycline";
- "Tetracycline".
Doctors prescribe Tetracycline 0.5 g four times a day. Treatment should be carried out for at least a week.
Doxycycline is also used to treat pneumonia. The maximum dosage is 600 mg. The duration of therapy can only be determined by a doctor based on the development of the inflammatory process.
However, macrolide antibiotics in tablets for pneumonia in adults are considered the most effective and safe. Among them, doctors highlight:
- "Sumamed";
- "Erythromycin";
- "Clarithromycin."
“Sumamed” is easy to use because you only need to take one pill per day containing 500 mg of the active ingredient. Moreover, the therapy is also short-lived. If the pathology proceeds without complications, then the course of treatment is usually 3-5 days.
"Erythromycin" in tablet form is prescribed four times a day at a dosage of 250 mg.
Antibiotics for the treatment of pneumonia in adults are varied. Many people prefer to prescribe drugs that should be used for a short period of time. So, Clarithromycin should be taken only twice a day. This scheme suits many patients. However, pulmonologists can prescribe the drug to the patient in the form of an intravenous solution.
The best antibiotics for pneumonia in adults should be safe and not cause serious side effects. The names given above are already familiar to many, because they are effective, but act gently and quickly.
What antibiotics are used for pneumonia?
Today, simple penicillins and other similar drugs are not used to treat pneumonia, since there are more effective and safe drugs of the latest generation. They have a wide spectrum of action, a small number of contraindications, can be used in small doses and have virtually no toxic effect on the liver, kidneys and other organs.
Symptoms of pneumonia
| Group | Drugs | Example image | Peculiarities |
| Cephalosporins | "Ceftriaxone", "Cefotaxime" | Prescribed for uncomplicated pneumonia caused by pneumococci, streptococci, enterobacteria. The substance has no effect on Klebsiella and Escherichia coli. Prescribed in case of proven sensitivity of microorganisms to the drug, as well as contraindications to macrolides | |
| Macrolides | "Azithromycin", "Midecamycin", "Clarithromycin", "Erythromycin" | Prescribed as a first-line drug in the presence of contraindications to drugs of the penicillin group. Effective for atypical pneumonia, pneumonia due to acute respiratory infections. It has a good effect on chlamydia, mycoplasma, legionella, and hemophilus influenzae. Worse effect on staphylococci and streptococci | |
| Semi-synthetic penicillins | "Amoxiclav", "Flemoclav", "Ampicillin", "Oxacillin" | It is prescribed experimentally or with proven sensitivity of microorganisms. Used for diseases caused by Haemophilus influenzae, pneumococci, as well as mild pneumonia of viral-bacterial etiology | |
| Carbapenems | "Imipenem", "Meropenem" | They affect bacteria that are resistant to the cephalosporin series. They have a wide spectrum of action and are prescribed for complex forms of the disease and sepsis. | |
| Fluoroquinolones | "Sparfloxacin", "Moxifloxacin", "Levofloxacin" | The drugs have a good effect on pneumococci | |
| Monobactams | "Aztreonam" | Drugs that are similar in action to penicillins and cephalosporins. Good effect on gram-negative microorganisms |
When prescribing antibiotics for the treatment of pneumonia, it is very important to pay attention to the compatibility of specific drugs. It is not recommended to take drugs from the same group at the same time, or to combine certain drugs (“Neomycin” with “Monomycin” and “Streptomycin”, etc.).
Prevalence of pneumonia
Video: Antibiotics for pneumonia
Use of fluoroquinolones
Which antibiotics for pneumonia in adults (tablets) will help cope with the infectious process completely depends on the microorganism that caused the pathology. If the disease is caused by legionella or E. coli, then fluoroquinolones are prescribed. This type of antibiotic drugs has its advantages. They penetrate deep into damaged tissues without causing pathogens to develop resistance to them.
What antibiotics are prescribed for pneumonia in adults? The names of drugs from the category of fluoroquinolones are as follows:
- "Ofloxacin." Prescribed twice a day from 200 to 800 mg.
- "Ciprofloxacin." It is recommended to take 250 to 500 mg twice daily.
The course of therapy is determined by the pulmonologist individually in each specific case. On average, treatment for moderate pneumonia lasts from one to two weeks.
What is pneumonia and why is it dangerous?
Many patients believe that pneumonia and pneumonia are different diseases, however, this is not the case. Pneumonia is inflammation of the lungs. The term pneumonia always implies inflammation of the lung tissue, as well as the presence of exudation in the alveoli, small-caliber bronchi, bronchioles, as well as damage to interstitial tissue.
It should be noted that pneumonia can only be an acute process. Chronic pneumonia does not exist.
The main cause of pneumonia is bacteria, but it also occurs:
- viral pneumonia (one of the complications of influenza, adenovirus, respiratory syncytial infection, etc.);
- fungal pneumonia (usually found in patients with immunodeficiency conditions);
- mixed inflammation (bacterial-viral);
- parasitic pneumonia (also typical for immunodeficient patients);
- aspiration (such pneumonia develops during aspiration of vomit, gastric juice, etc. into the lungs). As a rule, passive flow of stomach contents into the lungs can occur due to shock conditions, resuscitation measures, myasthenia gravis with impaired swallowing, impaired consciousness, etc.
Antibiotics for pneumonia are the mainstay of treatment. Antiviral therapy is advisable only for proven viral (in the vast majority of cases influenza) pneumonia.
Read further: When are antibiotics used for influenza in adults and children?
Antibiotics for pneumonia are prescribed taking into account the spectrum of the main pathogens. If the antibiotic therapy is ineffective within 48 hours, it is recommended to change the antibiotic or add a second drug.
For severe pneumonia, two antibacterial drugs are immediately prescribed.
It should be noted that severe pneumonia is considered a special form of the disease. This is due to the fact that severe pneumonia is accompanied by severe intoxication, hemodynamic disturbances and the development of severe respiratory failure. Sepsis and septic shock are also possible. The prognosis for severe pneumonia is always unfavorable, so such patients always require mandatory intensive care.
Timely prescribed antibiotics for pneumonia significantly reduce the risk of an unfavorable outcome, as well as the development of severe complications, such as:
- pulmonary abscesses;
- gangrene of the lung;
- sepsis and septic shock;
- pleurisy;
- pleural empyema;
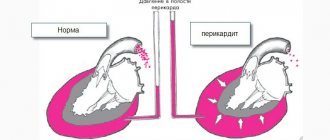
- endocarditis, pericarditis, myocarditis;
- meningitis;
- acute respiratory failure (respiratory failure) and pulmonary edema, etc.
It is necessary to understand that pneumonia is a dangerous infectious disease, which with proper treatment has a favorable outcome. However, only the attending physician should prescribe antibiotics for pneumonia. Self-medication can be dangerous to health and cause the development of severe life-threatening complications.
Side effects from antibiotic therapy
Antibiotic tablets for pneumonia in adults can cause serious side effects. Therefore, it is so important that they are prescribed by a specialist based on an accurately established diagnosis. However, the specificity of the tablets is such that even when prescribed correctly, they can cause:
- digestive disorders;
- allergic reactions.
Due to the fact that antibiotics disrupt the natural flora, vaginal candidiasis is often observed in the body of women. Patients of both sexes may develop:
- allergic reactions;
- neurotoxic symptoms;
- anaphylactic shock.
The least dangerous in terms of complications are tablets belonging to the penicillin series, as well as cephalosporins and macrolides. Therefore, pulmonologists often prescribe these medications.
Use of expectorants
In addition to the fact that the patient must take antibiotics for pneumonia, the patient is prescribed a whole range of drugs, the purpose of which is to speed up the recovery process.
The doctor will prescribe tablets for pneumonia, which will help cure the cough. The drugs may have mucolytic and expectorant effects. Mucolytics are prescribed in cases where the mucus secreted during coughing is highly thick, viscous and viscous. Such medications for pneumonia help thin the mucus and make it easier to remove. This category of drugs includes the following:
| A drug | Photo | Price |
| Ambroxol | from 47 rub. | |
| Bromhexine | from 20 rub. | |
| Acetylcysteine | from 118 rub. | |
| Lazolvan | from 173 rub. | |
| Carbocisteine | specify |
Treatment of cough is based on expectorants in cases where sputum is already produced, is transparent and has low viscosity. In this case, the attending physician will recommend taking the following medications:
| A drug | Photo | Price |
| Stoptussin | from 144 rub. | |
| Pertussin | from 25 rub. | |
| Mukaltin | from 13 rub. | |
| Alteyka | from 129 rub. |
The attending physician can more accurately recommend the type of drug to relieve cough due to pneumonia. When prescribing a medicine, he will take into account the total duration of the disease, the nature of the pathology, and the characteristics of the sputum produced.
In addition to drug treatment, for pneumonia it is important to follow general recommendations, namely:
- walk in the fresh air more often;
- Healthy food;
- to live an active lifestyle;
- Take vitamin complexes periodically.
Following these simple rules will reduce the risk of contracting pneumonia and will also speed up the recovery process.
To ensure that the medications used do not harm the body, but help cope with the infection, they must be prescribed by a doctor after conducting the necessary examinations.
Video on the topic: What to do to make your lungs breathe easily
Contraindications to antibiotic use
If a patient has an individual intolerance to any drug, this is a direct contraindication to its use. Also, many antibiotics are prohibited for use during pregnancy and lactation.
However, such patients with clearly established pneumonia also require antibacterial therapy. At the same time, the doctor selects the most gentle pills for the woman in terms of their effect on the body. According to the level of danger, they are classified as group B.
Antibiotic classes for treating pneumonia
Previously, classes and individual antibacterial drugs used to treat various forms of pneumonia were mentioned. Let's look at these drugs in more detail.
Penicillins
Penicillins are one of the oldest groups of antibiotics that have not lost their relevance. Aminopenicillins are a subclass of penicillins. Of these, amoxicillin, ampicillin, amoxicillin with clavulanic acid are used for pneumonia and bronchitis.
Amoxicillin with clavulanic acid, widely known under the trade names Augmentin, Amoxiclav, Flemoclav, is called protected aminopenicillin.
“Protection” in its formula is provided by clavulanic acid. The fact is that some microbes have learned to produce an enzyme that destroys the antibiotic. And to cure the infection caused by them, the antibiotic must be protected. The security of amoxicillin with clavulanic acid lies in the fact that they cope better with the action of microbial enzymes than simple amoxicillin.
The penicillin class is periodically replenished with new dosage forms.
Cephalosporins
Cephalosporins are a class of antibiotics related to penicillins. The list of cephalosporin drugs is quite long. These include, for example, the famous ceftriaxone - one of the best antibiotics in its class.
Within the cephalosporin group, drugs are divided into generations. It is important to note that belonging to one generation or another does not indicate modernity and better quality of the medicine. Generations of cephalosporins tend to differ in their microbial exposure profiles.
Thus, representatives of the first and second generations are more focused on the fight against respiratory tract infections, and the third and fourth are more focused on pathogens of the intestinal group of infections.
- The first generation of cephalosporins includes cephalexin, cefadroxil, and cefazolin.
- For the second - cefuroxime, cefaclor.
- Third generation - ceftriaxone, cefotaxime, ceftazidime, etc.
- Fourth - cefepime.
Macrolides
The most important feature of macrolides, which in practice largely determines their choice, is the ability to act on so-called intracellular pathogens.
Intracellular pathogens are mycoplasmas, chlamydophila, legionella. Hiding inside the cells of the human body, they escape the attack of most antibacterial drugs.
Macrolides include midecamycin, clarithromycin, azithromycin and other antimicrobial drugs. This is a dynamically developing class of antibiotics, the list of which is constantly growing.
Tetracyclines
The tetracycline series contains many outdated drugs. However, doxycycline remains relevant and is used for both pneumonia and bronchitis. It acts on intracellular pathogens and is especially good against Haemophilus influenzae.
Doxycycline is contraindicated in children under 8 years of age.
Aminoglycosides
Antibiotics of the aminoglycoside class are practically not used to treat pneumonia and bronchitis on their own. The fact is that they do not act on pneumococcus - one of the most common microbes in pneumonia.
Aminoglycosides are usually added to treatment when it is necessary to act on Pseudomonas aeruginosa and coliform bacteria. Such drugs also work well against staphylococcus.
A big disadvantage of representatives of this group is their toxicity to the kidney structures and inner ear.
Gentamicin, amikacin - these drugs are used most often.
Fluoroquinolones
Fluoroquinolones are perhaps the most dynamically developing class of antibacterial substances.
They are divided into generations. Time-tested ciprofloxacin, more modern gatifloxacin, moxifloxacin (3-4th generation) are widely used to treat pneumonia.
Modern fluoroquinolones have a wide spectrum of antibacterial activity. They are able to cure infection caused by intracellular microorganisms.
Fluoroquinolones are low-toxic, but are prohibited for use in pediatric practice due to their possible effect on the development of the musculoskeletal system.
Diagnosis of pneumonia
To decide which antibiotics to take for pneumonia in adult patients, the doctor conducts a detailed examination. To do this, the specialist uses the following methods:
- inspection;
- listening to the lungs with a stethoscope;
- measuring body temperature;
- sputum analysis;
- general and biochemical blood test;
- chest x-ray.
It is believed that radiography is the basis of diagnosis. The examination must be carried out in direct, in some cases - lateral projection. This method allows the doctor to accurately diagnose, predict possible complications, prescribe effective therapy and evaluate its effectiveness. Therefore, x-rays of the lungs for pneumonia are performed several times.
Depending on the severity of the disease, the doctor may prescribe the following measures:
- bronchoscopy;
- tomography
This is necessary to exclude tuberculosis and lung cancer. A pleural fluid test may also be ordered.
Pathogens and tablets for hospital-acquired pneumonia
Each department has its own microorganisms that can cause inflammation of the lungs. In the surgery department, gram-negative and staphylococcal flora predominate. In therapy, a person can expect E. coli, as well as Klebsiella, fungi of the genus Candida.
In a situation where a person falls ill with pneumonia in a hospital, tablets in the form of semi-synthetic penicillins are used for treatment, which are combined with clavulonic acid, second and third generation cephalosporins, and respiratory fluoroquinolones. If the cause of the disease is Pseudomonas aeruginosa, a group of combined semi-synthetic penicillins will be effective. Representatives of the latter group are the following drugs: Timentin, Tazocin.
Suspicious symptoms
Even the best antibiotics for pneumonia in adults cannot improve the condition unless an accurate diagnosis is made. Common symptoms of the disease are:
- increased body temperature;
- dry hacking cough;
- chest pain.
As inflammation increases, the patient complains of lack of air, excessive anxiety, muscle pain and fatigue. Sometimes blueness of nails and lips is observed.
Despite the commonality of symptoms, pneumonia can be caused by various types of microorganisms. Only laboratory tests will help establish their pathogenicity. Therefore, if you suspect the development of pneumonia, you should immediately consult a doctor. It is forbidden to use any pills or other drugs on your own to avoid serious complications and death.
If the doctor discovers pneumonia, then antibiotic therapy will be the only correct solution. However, complex treatment is necessary. To do this, the pulmonologist prescribes expectorants and antipyretics. To strengthen the immune system, vitamin complexes with a high content of vitamins such as C, A and group B are required.
Of course, the use of antibiotics leads to various kinds of complications. To get rid of unpleasant symptoms, probiotics and prebiotics can be prescribed. They must be taken to tidy up the intestinal microflora. Homeopathy is also becoming relevant, but only a doctor can prescribe such drugs in accordance with the patient’s condition and his individual physical characteristics.
Strong antibacterial agents
For severe pneumonia in adults, doctors prescribe strong antimicrobial agents to patients. The most popular include:
- Avelox - tablets based on moxifloxacin hydrochloride, belong to the group of fluoroquinolones, have a bactericidal effect. Contraindications: severe diarrhea. Dosage: 400 mg once a day for 10 days.
- Ospamox is a powder for preparing a suspension based on amoxicillin. It belongs to the group of penicillins and has a rapid effect. Contraindicated in infectious mononucleosis and individual lymphocytic leukemia. Dosage: 1.5-2 g/day in 3-4 doses over a course of 2-5 days.
How an antibiotic is selected
Antibiotics are the main part of treatment in the treatment of pneumonia. The choice of a group of similar drugs is made by a specialist based on an examination of the patient and the results of laboratory tests and bacterial culture of sputum.
Only after the causative agent of the disease has been identified can a test of its sensitivity to a specific class of antibiotic be carried out.
However, often the patient's condition requires immediate treatment. Therefore, before identifying the pathogen, the doctor may prescribe an antibiotic, following these principles:
- The use of broad-spectrum tablets. In this case, the dosage is calculated in such a way that there is a constant concentration of the active component in the blood.
- If atypical pneumonia is detected, then specialized medications containing clarithromycin are also needed. Sumamed is considered the most effective drug.
Urgent prescription of drug therapy
The decision on emergency or planned hospitalization is made by the doctor after examining the patient or after a diagnostic examination (x-ray, laboratory results).
If a patient is taken to a therapeutic or pulmonology department by ambulance, and his condition is assessed as critical, doctors have to prescribe drug therapy empirically, that is, based on the clinical manifestations of the disease.
Urgent hospitalization is necessary for signs of acute respiratory failure (respiratory rate above 40 per minute), confusion, and symptoms of increasing intoxication.
The degree of infiltration and destruction of lung tissue, as well as hemodynamic disorders, are detected by medical diagnostic methods in a hospital (x-ray, blood test).
Based on the nature of the symptoms and taking into account the fact that the main drugs in the treatment of pneumonia are antibacterial drugs, specialists prescribe drug therapy.
The effectiveness of the treatment course directly depends on the accuracy of identification of the causative microorganism. If the pathogen is highly sensitive to anti-inflammatory antibiotics, the patient’s condition quickly improves and the risk of complications is eliminated.
In such situations, doctors do not have time to wait for the results of microbiological analysis (laboratory reports are issued in 24-48 hours), since in severe forms of pneumonia there is a high risk of developing total sepsis or pulmonary edema, which leads to death.
Mixed pneumonia caused by typical and atypical pathogens poses particular difficulty in developing a treatment regimen.
Doctors, before prescribing what medications a patient should take, proceed from the fact that the most common pathogens of pneumonia are pneumococci, Haemophilus influenzae, mycoplasma, and moracella. In recent years, cases of pulmonary diseases caused by chlamydia and legionella have become more frequent.
Classification of antibacterial drugs used in the treatment of pneumonia
The need for the development of new antibiotics is caused by the addiction (resistance) of pathogens to the effects of drugs.
The following groups of drugs that act on the causative agents of pneumonia are used in treatment regimens:
- Semi-synthetic penicillins ( Amoxicillin , Ampicillin, Amoxiclav , Carbenicillin, Ampiox, Flemoxin Solutab). The drugs have relatively low toxicity, so they are prescribed for the treatment of children.
- Cephalosporins (4 generations of antibiotics). The most effective drugs are the IV generation group (Cefepime (Maxipim), but III generation drugs (Cefotaxime, Ceftriaxone , Ceftazidime, Cefoperazone) are also widely used in medical practice.
- Carbapenems The drugs are effective against strains of gram-negative bacteria resistant to cephalosporins of the III-IV generations (Imipenem, Tienam, Meropenem).
- Macrolides have a mechanism of action similar to that of tetracyclines, but drugs of this series are less toxic ( Azithromycin , Clarithromycin, Midecamycin).
- Fluoroquinolones – effective against pneumococcus (Levofloxacin, Moxifloxacin)
- Aminoglycosides – act against gram-negative pathogens (Amikin).
- Monobactams are similar in mechanism of action to penicillins and cephalosporins (Azactam, Aztreonam)
- Tetracyclines ( Doxycycline , Vibramycin).
The effectiveness of a treatment course with antibiotics is assessed by the general condition of the patient and the results of laboratory tests.
With the right choice of anti-inflammatory antibiotic, test results should improve within two to three days. The drug is not changed during this time, since signs of the disease persist for 2-4 days (temperature, fever), and the increased content of leukocytes in the blood lasts up to 5 days.
The exception is when the patient's condition rapidly deteriorates despite intensive therapy.
Choice of antibacterial therapy according to the recommendations of the European Respiratory Society
| Disease category | Antibacterial drug |
| Severe pneumonia. Need for hospitalization | Cefuroxime, Cefotaxime, Ceftriaxone, Amoxicillin, Benzylpenicillin, additionally macrolides (Azithromycin, Clarithromycin, Erythromycin) |
| Moderate pneumonia with a good prognosis. Treatment in intensive care wards | Cefuroxime, Cefotaxime, Ceftriaxone + fluoroquinolones (ofloxacin, ciprofloxacin); II-III generation cephalosporins + macrolides (erythromycin) |
| Patients undergoing treatment on an outpatient basis when diagnosed with primary (uncomplicated pneumonia) | Aminopenicillins. Alternative drugs: Tetracycline antibiotics, cephalosporins (oral), macrolides |
The Commission on Antibiotic Policy under the Ministry of Health of the Russian Federation and the Russian Academy of Medical Sciences recommends, when choosing an anti-inflammatory antibiotic, to take into account the patient’s age, with the exception of clinically severe cases.
For mild forms of pneumonia, patients under 60 years of age are prescribed antibiotics in tablets (aminopenicillins, macrolides); after 60 years, cephalosporins of the second generation (capsules, tablets) and additionally macrolides.
Other drugs included in complex therapy
If pneumonia is caused by a viral pathogen, antiviral drugs are prescribed in tablets ─ Arbidol , Acyclovir , Valacyclovir.
With the development of pulmonary diseases against the background of decreased immunity, Didanosine, Zidovudine, Saquinavir, and interferons are prescribed.
Bronchodilators (in the form of inhalation) are prescribed to relieve spasms in the bronchi, mucolytics are prescribed to stimulate sputum discharge (Amroxol, Lazolvan, Ambrobene, Mucosolvan, Halixol)
As anti-inflammatory drugs that relieve symptoms of intoxication, drugs such as Ibuprofen, Papacetamol, Fenspiride, Erespal (syrup, tablets) are prescribed. Ibuprofen is prescribed for bronchitis and pneumonia to relieve headaches and attacks of fever.
Expectorants are prescribed simultaneously with a course of antibiotic treatment.
This group of funds includes:
- Marshmallow root potion;
- Bronholitin;
- Doctor Mom;
- Overslept.
Important! Treatment of pneumonia is carried out comprehensively - in addition to taking prescribed medications and procedures, it is necessary to follow a diet and daily routine. Only in this case does complete recovery occur.
You cannot rely on patient reviews of medications, since the effectiveness of pharmacological agents depends on the correct identification of the causative agent of the disease.
After severe forms of pneumonia and bronchitis, physiotherapy, therapeutic exercise complexes, restoratives and vitamin complexes are prescribed.
Sanatorium-resort complexes of appropriate specialization play a major role in the rehabilitation of patients with pulmonary diseases.
Auxiliary drugs for pneumonia
In addition to antibiotics, it is recommended to treat pneumonia using auxiliary agents. Among the additional drugs often used are:
- Expectorants and bronchodilators (Gerbion, Pertussin syrups, Salbutamol spray).
- Antipyretic medications (Paracetamol, Aspirin, Ibuprofen).
- Vitamin complexes with a high content of vitamins A, C, group B (Supradin, Duovit, Complivit).
For patients who have a hard time tolerating synthetic drugs, homeopathy becomes relevant. Among such remedies, the most effective are Aconite, Bryonia, Belladonna, Sanguinaria, Arsenicum Yodatum. The patient should be treated with such drugs in accordance with his constitutional type.
Antipyretics
The course of pneumonia is usually accompanied by a high body temperature, which must be reduced, since it interferes with the normal functioning of the body's immune system and impairs the absorption of medications. You can take them in the form of powders for making drinks, capsules, tablets. At critical temperatures, intramuscular administration is possible. List of the most popular titles:
- Efferalgan,
- Tylenol,
- Calpole,
- Flukold,
- Coldrex,
- Doloren,
- Opradol,
- Solpadeine,
- Citripan,
- Fervex.
It is also possible to prescribe the following broad-spectrum anti-inflammatory drugs with antipyretic effect:
- ibuprofen;
- paracetamol;
- aspirin;
- analgin.
If there is vasospasm (the patient has cold extremities), antipyretics are taken together with no-shpa.
Important! The active ingredients of different antipyretics differ, and their interaction with other drugs may affect the effectiveness of treatment. Therefore, they should be taken only as prescribed by a doctor.
Tetracyclines
Until the causative agent of pneumonia is determined in adult patients, tetracycline antibiotics can be used in treatment, which is especially important when the infection is actively developing.
It is important to take into account that these drugs are ineffective compared to other antibiotics, which is due to the formation of immunity by many known microorganisms. However, in some cases their use is necessary. In complex therapy, at the initial stage, Vibramycin, Doxycycline, Unidox Solutab, etc. are prescribed.
Tips for choosing drugs
If a doctor prescribes antibacterial agents, then he must take into account the individual characteristics of the patient, the form of the disease, and the body’s response to a particular drug. So, for mild or moderate community-acquired pneumonia, the following is prescribed:
Macrolides and third generation fluoroquinols (Moxifloxacin, Ciprofloxacin). For patients with severe forms of the disease - a combination of cephalosporins, macrolides or fluoroquinols. Introducing drugs into the body for 2-3 days through a dropper, and then, if the patient’s condition improves, then transferring him to antibiotics in tablet form. Medicines are used to reduce their intake to one or two times a day.
The duration of taking antibiotics depends on the patient’s condition and can range from seven days to twenty-one.
Among mucolytics, Bromhexine has proven itself best. Although it is effective, it has few side effects. Also in the top three popular medicines in this group are Lazolvan and Ambroxol. Acetylcysteine and Lazolvan are best used for inhalation with a nebulizer.
Among the popular anti-inflammatory drugs that reduce swelling and relieve pain are Diclofenac and Ibuprofen.
Stages of lobar pneumonia and methods of its treatment
What symptoms of tuberculosis will this article tell you?
How to determine pneumonia in a child //drlor.online/zabolevaniya/legkix/pnevmoniya/po-kakim-priznakam-opredelyaetsya-u-rebenka.html
Pneumonia or pneumonia - definition of the disease
Pneumonia (pneumonia) is an infectious disease of the lower part of the respiratory system. The inflammatory process begins in the alveoli. Exudate may accumulate. Why is that bad? The fact is that it is in the lungs that gas exchange occurs. The blood is saturated with oxygen, and carbon dioxide is also eliminated through the lungs. Inflamed areas cannot participate in these processes to their full potential. The amount of oxygen decreases and this mainly affects the brain and cardiovascular system. Pneumonia can be an independent disease and then it is called primary, but in some cases it is a complication of other diseases (secondary). For example, against the background of chronic bronchitis.
Aminoglycosides
The group of aminoglycosides is quite often prescribed for pneumonia caused simultaneously by several types of bacteria.
There are 3 generations of aminoglycosides:
- 1st generation includes Neomycin, Kanamycin and Streptomycin;
- group 2 includes Tobramycin, Gentamicin and Netilmicin;
- The least toxic and more effective is the 3rd generation aminoglycoside – Amikacin (Amikin).
A characteristic feature of aminoglycosides is poor absorption when taken orally, therefore the parenteral route of administration (injection) is most often used.
What pathogens cause pneumonia?
Colds in children and adults often develop into obstructive bronchitis, and in the absence of proper treatment and the addition of bacterial microflora, they can develop into pneumonia.
The most common causative agent of pneumonia remains pneumococcus; less commonly, the disease is provoked by mycoplasmas, chlamydia and Haemophilus influenzae . In young people, the disease is most often caused by a single pathogen. In old people, in the presence of concomitant diseases, the disease is provoked by a mixed microflora, where both gram-positive and gram-negative bacteria are present.
Lobar pneumonia in all cases is caused by streptococcus. Staphylococcal pneumonia is less common, mainly in the elderly, in people with bad habits, as well as in patients who have been on hemodialysis for a long time or have had the flu.
Quite often it is not possible to determine the pathogen. In this case, antibacterial drugs are prescribed by trial. Recently, the number of pneumonias caused by atypical pathogens has increased.
Azithromycin gives good results for pneumonia in adults and children. It is generally well tolerated by patients of all age groups and rarely produces side effects.
Azithromycin belongs to the group of macrolides. This antibacterial drug is often prescribed for intolerance to antibiotics from the penicillin group.
Features of the treatment of pneumonia in children
When treating pneumonia in children, it is necessary to select the correct dosage form of the drug.
To treat children under 6 years of age, you should take a suspension, since it is very difficult for a child to swallow the entire capsule, and if you pour the powder out of the capsule, the baby will not want to swallow it because the taste is too bitter. For severe lower respiratory tract infections, the dosage is calculated by the attending physician, who also determines the duration of therapy . In most cases, the course of treatment lasts three days, but for severe pneumonia, a weekly course may be recommended. The child should take the medicine at the same time every day. This ensures a constantly high concentration of the antimicrobial agent in the blood.
Treatment should not be interrupted when the patient's condition improves. If you do not take the full course of antibiotics, a superinfection may develop that is difficult to treat.
Azithromycin is a broad-spectrum, long-acting antibiotic. After taking the last capsule, the therapeutic concentration of the active substance in the blood remains for three days . Thanks to this property, this macrolide becomes the drug of choice for the treatment of pneumonia.
The effectiveness of antibiotic tablets
Antibacterial drugs are prescribed to destroy bacteria and stop their reproduction. If this is not done on time, serious damage will be caused to the body, and the person may die with advanced pneumonia. The course of antibiotic treatment is calculated based on the stage and type of disease, as well as the strain of the infectious agent.
For example, it takes a week to treat the extracellular form of the pathogen, but it takes about a month and a half to get rid of a lung abscess.
As a rule, the first signs of the work of antibacterial agents are noticeable within 3 days after the start of therapy:
- the patient’s temperature decreases and the chills stop;
- shortness of breath and symptoms of respiratory failure disappear due to blood saturation with oxygen;
- the volume of sputum secreted decreases, pus disappears.
Antibiotics help reduce the area of inflammation, freeing breathing and relieving the patient of pain.
Proper nutrition
Pneumonia requires complex treatment, so painkillers, antitussives, mucolytics and antispasmodics are added to antibacterial drugs. Traditional medicine methods are also often used, but only as support for basic antibiotic therapy. In addition, the patient should put his lifestyle in order: quit bad habits, start eating right and doing physical exercise.
How to take antibiotics correctly
Antibiotics have a strong effect, so they should be used based on several important rules:
- Self-administration of antibiotics is excluded. This can cause complications and resistance (immunity) to certain groups of microorganisms with the development of a chronic process;
- Violation of the dosage prescribed by the doctor is prohibited (excess can lead to damage to the kidneys and liver, and a decrease can “drive” the infection inside, thereby promoting the development of new bacterial strains);
- the general course of antibiotic therapy should not be interrupted even if there is a significant improvement in the patient’s general condition. Otherwise, an exacerbation of pneumonia resistant to the prescribed antibiotic is possible;
- during treatment, it is recommended to take biological products (probiotics) that restore intestinal microflora (Linex, Lactofiltrum, etc.) without the presence of living bacteria, since antibiotics destroy them;
- the patient must inform the doctor about all negative reactions that occurred during previous antibiotic therapy;
- When taking antibacterial agents orally (taken by mouth), you must use only clean, still water.
Important! The use of antibiotics is justified if we are talking about a serious infection that threatens human life (pneumonia, tuberculosis, etc.). In all other cases, antibiotics should be avoided, using other, safer means.
What is pneumonia
Pneumonia is popularly called pneumonia. It is a lower respiratory tract infection with an incubation period of 2 to 10 days and involves the lung tissue. There are several types of disease:
- Atypical. Caused by chlamydia, legionella, mycoplasma, that is, atypical microflora.
- Aspiration. It occurs when water, food or foreign objects enter the respiratory tract.
- Hospital. The disease develops while the patient is in the hospital.
- Out-of-hospital. Occurs as a complication after a viral infection. It is often a cause of death due to a severe decrease in immunity.
New generation antibiotics help to avoid complications of pneumonia, which can cause lung abscess, pleural empyema, pneumothorax and other serious diseases. The most serious consequence of pneumonia is respiratory failure. This pathology develops in patients with other chronic diseases or in elderly patients who do not receive adequate antibiotic treatment. Failure often causes death.
Recovery time
The duration of treatment depends on the form of the disease, individual health characteristics and the correctness of the chosen treatment tactics in each specific case.
The average treatment time for typical community-acquired pneumonia is from 1 to three weeks (depending on the severity of the initial symptoms).
In cases with an atypical or nosocomial form of the disease, the recovery time increases on average by 2 times and amounts to 7-14 days for a mild degree of the disease, and for a severe course of the disease - 14-56 days. The duration of illness may be prolonged if patients are immunocompromised, young children, or elderly people.
To a great extent, the duration of pneumonia depends on the timeliness of treatment. There are very insidious forms of the disease that occur without fever. The absence of the main symptom of illness often leads to a delay in the start of therapy and, accordingly, an increase in recovery time.
If the following symptoms appear, you should immediately consult a doctor and undergo an examination (x-ray and blood test):
- Coughing;
- Shortness of breath, inability to take a deep breath, pale skin;
- Worsening after a cold;
- The duration of a cold is more than 7 days.
Precautions for people who have had pneumonia
The correctness of therapy from the very beginning of the disease is also of great importance. Here, a bacterial study of the microflora plays a decisive role, making it possible to determine the type of causative agent of pneumonia and select the most effective medications (in particular, antibiotics).
Evaluation of the effectiveness of antibiotic therapy
The duration of the treatment course of antibiotics directly depends on how positive the dynamics of the patient’s general condition are.
The result of the therapy can be assessed after 3 days, after which the doctor determines further treatment tactics. If there is no positive effect and hyperthermia persists, the initially used antibiotic is replaced by another or combination drugs are selected. The next assessment of the effectiveness of treatment is also carried out after 3 days.
The criteria for the success of antibiotic use are normalization of body temperature and improvement of the patient's condition. In addition, laboratory diagnostics are performed (blood, sputum and urine tests) and x-ray examination, which indicates the absence of infiltrates in the lung area.
Pneumonia is a very dangerous disease that can lead to serious consequences. Antibiotic therapy is effective only when the nature of the development of the inflammatory process is clarified. In other cases, antibiotics can cause significant harm to health, so taking them on your own is excluded.
The principle of choosing an antibiotic for lung pathologies
Specialists select antibiotics for the treatment of lower respiratory tract infections based on data on the most common causative agents of these pathologies. This approach is due to the fact that not all clinics have the opportunity to quickly culture sputum and determine which microorganism caused the disease. In some cases, pneumonia causes a nonproductive cough, making it very difficult to take sputum samples.
The choice of antibiotic is often complicated by the fact that the doctor is not able to constantly monitor the course of the disease and, if necessary, promptly adjust treatment. Different antibiotics have different pharmacological effects and penetrate differently into different tissues and fluids in the body. Thus, only a few types of antibiotics penetrate well into cells - macrolides, tetracyclines and sulfonamides.
If the pathogen is sensitive to an antibacterial drug, but the drug reaches the site of inflammation in insufficient concentration, then there will be no effect from such treatment. But you need to understand that with this method there is no improvement in the patient’s condition, but microbes become resistant to the antibiotic.
A very important aspect when choosing antibiotics is the safety of the drug. In home treatment settings, the choice is most often given to oral medications . Doctors try to select medications whose frequency of administration is minimal, but whose effectiveness is high.
In pediatric practice, when choosing antibacterial drugs, preference is given to syrups and suspensions with a broad-spectrum active substance.
Pathogenetic basis of therapy
When inflammation begins in the lungs under the influence of infectious agents, excessive production of mucous secretion occurs. The body is unable to cope with the infection, and thus rushes to remove the destroyed pathogenic microflora from the lungs. But with weak immunity, microbes multiply faster than mucus is eliminated, and pus appears in the sputum.
Antibiotics are a means of preventing the proliferation of microorganisms. However, pathogenic mucus still remains, which, if not removed in a timely manner, can become a source of relapse of the disease. And this is where modern approaches to the treatment of pneumonia come to the rescue, allowing you to regulate recovery processes without metabolic disorders.
Pathogenetic therapy includes the use of the following groups of drugs:
- Drugs used to regulate metabolism: hormones, vitamins, amino acids, plasma-substituting solutions, etc.;
- Drugs that affect the nervous system: antipsychotics, barbiturates, sedatives and general tonics, stimulants, etc.;
- Preparations for effects on the heart and blood vessels: cordigit, korglykon, digitalis, no-spa, etc.;
- Preparations for stimulating the urinary system: furosemide, bearberry or lingonberry leaf, clopamide, bear's ear grass, etc.;
- Means for normalizing the functioning of the gastrointestinal tract and liver: Liv-52, silybor, essentiale, etc.;
- Means that allow the pancreas to function: pancreatin, festal, panzinorm.
All drugs that increase the level of the body’s immune forces during illness and during the rehabilitation period can be included in pathogenetic therapy. Its methods are no less important than antibiotic therapy, and during the recovery period the body comes first.
The most commonly used drugs for treatment
| Drug name | Forms of release, one-time and daily |
| Antibacterial drugs | |
| Natural and semi-synthetic penicillins | |
| Amoxicillin | Capsules 500 mg. Single dose 0.5 g, daily dose - 1.5 g. Dry substance for preparing a suspension 250 mg/5 ml in 60 ml bottles. Up to 20 kg: single dose 125 mg, daily dose - 375 mg. More than 20 kg: single dose 250 mg, daily dose - 750 mg. In case of severe infections it can be doubled. |
| Amoxicillin/clavulanic acid Augmentin Amoxiclav | Powder for preparing a solution in bottles of 0.6 and 1.2 g. Single dose for adults and children over 12 years old - 1.2 g, daily dose - 3.6 g. IV drip (up to 4.8 g for severe infection). Powder for making syrup 70 ml (228.5 mg/5 ml) in bottles. It is prescribed to children twice a day 25/3.6 - 45/6.4 mg/kg or 45.6/6.4-70.0/10 mg/kg in case of severe infection. Tablets of 1.0 g in blisters. 1 tablet twice a day. Augmentin SR (amoxicillin 1000 mg, clavulanic acid 62.5 mg). Single dose: 2 tablets, take 2 tablets twice a day. |
| Second generation cephalosporins | |
| Cefuroxime axetil Zinnatm Zinaceftm | Tablets 0.125 g; 0.25 g; 0.5 g. Suspension 0.125 or 0.25 g in 5 ml. Daily dose 1.0 g. Dry substance for injection 0.15 g and 1.5 g. Daily dose 3-6 g. |
| Third generation cephalosporins | |
| Cefotaxime | Dry substance for injection, 0.5 and 1.0 g. Single dose 0.5-1.0 g, daily dose – 2.0-6.0 g. IV twice a day. |
| Cefoperazone | Dry substance for injection 0.5 g; 1.0 g; 2.0 g. Single dose 0.5-1.0 g, daily dose – 2.0-4.0 g, maximum daily dose – 12 g. |
| Ceftriaxone | Dry substance for injection 0.5 and 1.0 g. Single dose 1.0-2.0 g, daily dose - 2.0 g. IM, IV once a day. |
| Ceftazidime | Vials for injections of 500 mg; 1.0 g; 2.0 g. IV two to three times a day. Daily dose up to 6 g. |
| Fourth generation cephalosporins | |
| Cefepime | Vials for intravenous injections 0.5 g, 1 g, 2 g. Daily dose - 4.0 g. |
| Cephalosporins active against MRSA | |
| Ceftaroline | Dry substance for intravenous injection 600 mg in a bottle. Single dose 600 mg, daily dose - 1200 mg. |
| Macrolides | |
| Azithromycin | Tablets 125 mg, 500 mg. Syrup 100 mg/5 ml; 200 mg/5 ml |
| Spiramycin Rovamycin | Tablets 1.5 million units and 3 million units. Granules for preparing a suspension 1.5 million units; 375 thousand units; Powder for the preparation of an injection solution for intravenous administration (1.5 million units of active substance in one bottle) In severe cases, the daily dose is up to 9 million units. |
| Clarithromycin | Tablets of 0.25 g and 0.5 g. Powder for suspension 0.125 g/5 ml of 60 ml. Dry substance for injection 0.5 g in a bottle. Single dose 250-500 mg, daily dose - 500-1000 mg. Take twice a day. UNO - tablets of 0.5 g. Single dose 500-1000 mg, daily dose - 500-1000 mg. Take once a day. |
| Josamycin | Tablets 0.5 g; 1.0 g. Suspension 0.15 g/5 ml and 0.3 g/5 ml in 100 ml bottles. Single dose 5000-1000 mg, daily dose - 1000-2000 mg. |
| Roxithromycin | Tablets of 150 mg and 3000 mg. Daily dose 300 mg in one or two doses. |
| Carbapenems | |
| Imipenem/cilastatin Imipenem | Vials for intravenous and intramuscular injections of 500 mg and 750 mg. Daily dose up to 4 g. |
| Meropenem | Vials for intravenous injections of 1000 mg. Single dose 500-1000 mg three times a day, daily dose - 3000-6000 mg. |
| Doripenem | Dry substance for the preparation of solution for infusion - 500 mg. A single dose of 500 mg three times a day, a daily dose of 1500 mg. |
| Second generation fluoroquinolones | |
| Ciprofloxacin | Tablets of 0.25 g, 0.5 g, 0.75 g, 0.1 g. Solution for infusion - 0.1 and 0.2 g in 50 ml bottles. Single dose - 0.25-0.5 g, daily dose - 500-1000 mg. |
| Third generation fluoroquinolones | |
| Levofloxacin | Tablets of 0.25 g, 0.5 g. Vials for intravenous infusion of 500 mg per 100 ml. |
| Fourth generation fluoroquinolones | |
| Moxifloxacin | Tablets of 0.4 g. Bottles for intravenous infusion of 0.4 g in 250 ml. The daily dose is 0.4 g once orally or intravenously. |
| Aminoglycosides | |
| Amikacin sulfate Amikacin | Ampoules of 2 ml/100 mg, for IV and IM injections. Daily dose up to 15 mg/kg in two to three doses. |
| Tobramycin sulfate Tobramycin Nebcin Brulamycin | Vials for intravenous and intramuscular injections of 40, 50, 75 and 80 mg. Daily dose 5 mg/kg in three to four doses. |
| Other | |
| Vancomycin | Bottles of 0.5 or 1.0 g. Daily dose - 2.0 g. |
| Linezolid | Tablets 600 mg. Take twice a day. Daily dose 1200 mg. Vials for intravenous infusions of 200 and 600 mg. Single dose 400-600 mg, daily dose - 800-1200 mg. |
| II. Mucolytics | |
| Acetylcysteine ACC Fluimucil | Effervescent tablets of 100, 200, 600 mg. Daily dose 600 mg in one or three doses. Granules for preparing a solution - 100 mg, 200 mg. Solution for inhalation 200 mg/1 ml. |
| Ambroxol hydrochloride Lazolvan Ambrobene Ambrohexal Flavamed | Tablets 30 mg. Single dose 30 mg three times a day, daily dose - 90 mg. Ampoules for intravenous injections 15 mg/2 ml. The daily dose is 45 mg. Effervescent tablets 100, 200, 600 mg. Daily dose 600 mg in one or three doses. Syrup 15 mg/5 ml; 30 mg/5 ml, 60 and 100 ml. Children under 2 years old: 15 mg in two doses, 2-6 years old - 22.5 mg in three doses, 6-12 years old - 30-45 mg in two or three doses, adults - 90 mg/day. |
| Bromhexine/salbutamol/guaifenesin Ascoril | Tablets 8/2/100 mg, 1 tablet three times a day. Syrup 4/2/100 mg in 10 ml. Children under 6 years old - 5 ml three times a day, 6-12 years old - 5-10 ml three times a day. |
| Carbocisteine Fluditec Bronkatar | Capsules 0.375 g. 1 capsule three times a day. Syrup 0.05 g, 0.02 g in 1 ml (5%, 2%) 125 ml, 300 ml. Dose for adults 5% - 1 tbsp. l. three times a day. |
If after viewing the table you have questions like:
- Why is anti-inflammatory therapy not presented?
- Where are the vitamins and immunomodulators?
- But what about everyone’s favorite hemodez?
There is only one answer: today there is no evidence base for the effectiveness of these drugs to prevent complications, reduce treatment time or improve the outcome of the disease. All these procedures significantly increase the cost of treatment and the risk of developing allergic and toxic complications.
Alternative methods of treatment and traditional medicine can complement doctor's prescriptions at different stages of treatment and recovery. By relying only on them, you expose yourself or your loved ones to the risk of complications and death.
Types of drugs
Antibacterial agents for pneumonia are divided into groups depending on the main active ingredient in the composition:
- Penicillins. This type of antibiotic appeared first. There are semi-synthetic and natural types, but the effectiveness does not change. The list of side effects is limited to allergic manifestations, diarrhea and hypersensitivity. Used against staphylococci and streptococci.
- Tetracyclines. These agents are used much less frequently, since microorganisms easily develop resistance to the active substance. In addition, tetracyclines accumulate in human bones and can cause tooth decay. Such drugs are not allowed for pregnant and lactating women, small children and patients with kidney pathologies. Doxycycline and tetracycline are the most common drugs.
Cephalexin
- Cephalosporins. There are 4 generations of this type of medicine. First: Cephalexin, Cefazolin. Effective against staphylococci and pneumococci. Second: Cefuroxime, Cefurabol. They are used to treat both gram-positive and gram-negative flora. Third: Cefoperazone, Cefotaxime. Prescribed for complications in the last stages of pneumonia. Fourth: Cefepime. The most powerful drug from the group of cephalosporins.
- Macrolides. Drugs in this group are prescribed to treat pneumonia caused by legionella, cocci and chlamydia. They are taken on an empty stomach, as food inhibits the absorption process. Allergies are rare. Erythromycin, Clarithromycin and Azithromycin are mainly prescribed. Patients diagnosed with liver disease should not take such medications.
- Aminoglycosides. Antibiotics of this pharmacological group are intended to neutralize aerobic gram-negative bacteria. Moreover, they are effective in case of infection with several strains of microorganisms, when it is necessary to use combined agents. Aminoglycosides include Gentamicin and Amikacin. The dose of the drug is individual for each patient and is based on the indicators of his body (weight, age) and the severity of the disease. During the course of treatment, it is necessary to monitor the condition of the kidneys, especially glomerular filtration.
- Quinols and fluoroquinols. They are used to treat pneumonia caused by E. coli and Legionella. Active substances are excreted from the body in the urine, so impaired renal function is a contraindication. Also, the product should not be used for liver diseases, in childhood, allergies and pregnancy. Medicines called Ciprofloxacin and Levofloxacin are used.
Levofloxacin
Adverse reactions
In some cases, when taking Azithromycin to eliminate pneumonia, some side effects may develop.
May be observed:
- flatulence and abdominal pain;
- digestive and stool disorders;
- various types of colitis;
- jaundice;
- vomiting or nausea;
- nervous excitement;
- dizziness;
- skin rash and itching;
- arthralgia;
- neutropenia.
If any adverse reactions occur, you should inform your doctor. It is possible that the doctor will reduce the recommended dose of the drug for an adult or include another drug in the treatment.
Penicillins
A group of penicillin antibiotics has a bactericidal effect, destroying the affected cell.
For uncomplicated pneumonia, Penicillin is one of the most effective antibiotics, but this group also includes other drugs with similar effects:
- Oxacillin - has an anti-inflammatory effect, taken orally 1 hour before a meal or 1.5 hours after a meal;
- Dicloxacillin - has a similar effect to Oxacillin, however, with the same dosage, the concentration of the drug in the blood is 2 times higher. Taken orally up to 4 p.m. per day from 0.25 mg. Sometimes the drug is administered by injection;
- Ampicillin has a wide spectrum of action and is prescribed for respiratory diseases. Oral dosage of 250 – 500 mg is recommended. up to 4 r. per day, and by injection - according to the scheme;
- Amoxicillin (Flemoxin) is an analogue of Ampicillin, but has a much less negative effect on the intestinal microflora. Taken exclusively orally in accordance with the prescribed regimen;
- Carbenicillin (Piopen) is an antibacterial agent (in the form of IV and IM injections) prescribed for moderate severity of the development of the pathological process in the upper respiratory tract;
- Ticarcillin (Tikar) – this antibiotic is close in action to Carbenicillin, but its effectiveness is 3 to 4 times higher. The drug is used in the form of injection solutions, but not more than 3200 mg. every 4 hours;
- Amoxiclav is considered one of the best antibacterial agents taken orally in the form of tablets and suspensions. The duration of the general course of treatment is 7–10 days.
Important! Many bacteria have developed resistance to penicillin antibiotics due to the length of their use in medicine. Therefore, a sensitivity test is required.
Cephalosporins
There are IV generation cephalosporins.
- I generation (Cefalexin, Cefazolin, Solexin, Keflex, Ancef, etc.) is most effective against pneumococci, streptococci and staphylococci;
- II generation (Cefuroxime, Mefoxin, Alphacet, Anaerocef, Zinnat, Tarcefandol, etc.) are more active against gram-negative bacteria;
- The third generation (Cefixime, Cefsulodin, Ceftazidime, Pancef, Spectracef, etc.) is characterized by an active effect on gram-negative bacteria;
- IV generation cephalosporins (Cefepime, Cefpirom, Maxicef, Cefvnorm, Maxipim, etc.) have a wide spectrum of antimicrobial effects and are actively used in complex treatment.
Medicines in this category have a stronger anti-inflammatory effect compared to the penicillin group, despite the same mechanism of action.