Despite the fact that science and medicine are moving forward, the health of the population can hardly be called ideal.
Often people do not pay attention to their diet. There is poor quality food, fatty, fried. Excessive alcohol consumption also has a significant impact on health. Some medications actually relieve the symptoms of diseases, however, they negatively affect the digestive system and the stomach itself. One of the most common problems is chronic erosive gastritis. In this article we will talk about this form of the disease in more detail.
Erosive gastritis of the stomach
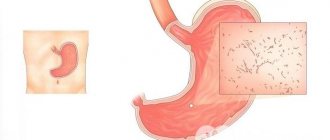
Erosive gastritis is an inflammatory pathology of the stomach, in which single or multiple defective areas in the form of erosions are formed on its walls, causing destruction of the mucous membrane.
Erosion that forms on the wall of the stomach is a minor pathological defect in its mucous membrane
Erosion that forms on the wall of the stomach is a minor pathological defect in its mucous membrane.
Typically, the size of such erosional areas varies from 0.2 to 15 mm. Often the bottom and edges of erosions have a pronounced brown color due to previous hemorrhage caused by pathological irritation of the gastric mucosa and increased permeability of its vascular network. With frequent bleeding, this pathology is defined as erosive-hemorrhagic gastritis.
Today, erosive gastritis of the stomach is still poorly understood. However, medical specialists are still inclined to believe that the origins of its development may be: poor nutrition, unstable psycho-emotional state, the bacterium H. pylori, chronic diseases and damage to the stomach, long-term use of certain medications, the presence of endocrine and oncological diseases, as well as alcohol abuse .
Experts warn that it is strictly prohibited to independently treat the symptoms of erosive gastritis; you must immediately seek qualified medical help.
Doctors say that all of the above factors can provoke the appearance of hypoxia of the tissues of the gastric mucosa, which can result in the formation of erosions in the stomach. Depending on the type of disease that has developed, the clinical picture of the pathology can vary significantly and is characterized by various symptomatic manifestations, however, in most cases, the symptoms of erosive gastritis manifest themselves in the form of acute abdominal pain, heartburn, nausea, vomiting, seething and bloating, diarrhea with blood discharge.
Chronic erosive gastritis of the stomach develops quite slowly
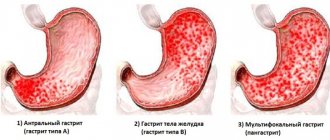
Types of erosive gastritis of the stomach
- chronic erosive gastritis of the stomach: develops quite slowly, characterized by the formation of multiple ulcerative defects affecting the deep layers of mucosal tissue;
- acute erosive gastritis of the stomach: develops rapidly and painfully, damaging mainly the superficial epithelium of the mucosa;
- erosive antral gastritis of the stomach: caused by infection with H. pylori, characterized by erosive lesions of the antral (lower) part of the stomach, in which the damaged mucosal epithelium loses its ability to regenerate. Doctors note that treatment of antral erosive gastritis should always begin with taking antibiotics that suppress the activity of the bacterial environment in the stomach;
- erosive reflux gastritis of the stomach: occurs due to the reflux of intestinal contents into the adjacent section of the stomach, characterized by deep damage to the mucous membrane in the form of the formation of extensive erosive and ulcerative defects on it, causing detachment of stomach tissue.
Description by code 25.0
A complication of the acute stage of the disease occurs as a result of arrosion (violation of the integrity of the walls during necrotic and ulcerative processes) of the vessel, with disturbances in the outflow of venous blood.
Clinic complications:
- dizziness;
- pale skin;
- weakness;
- collapse (sudden cardiovascular failure with loss of consciousness and death);
- melena (black, shapeless stool with an unpleasant odor, a mixture of blood with the contents of the intestines and stomach);
- single or repeated vomiting, including masses of the type of coffee grounds;
- hypotension (low blood pressure);
- acute pain (may be absent).
Erosive gastritis of the stomach: symptoms and treatment
https://youtu.be/lLRU0zhZVG8
Erosive gastritis is an inflammatory lesion of the gastric mucosa, in which single or multiple erosive defects form on its walls against the background of minimal activity of the inflammatory process. Erosive gastritis is often accompanied by bleeding and hemorrhagic imbibition of the affected mucous membrane.
The acute form of the disease is rare, proceeds violently and is difficult to treat, and therefore in most cases becomes chronic. Chronic erosive gastritis is diagnosed, according to various sources, in 2-18% of all patients who underwent endoscopic examination for epigastric pain.
Experts in the field of clinical gastroenterology note that this pathology is 3 times more common among men. At the same time, the acute form of the disease is characteristic of men of working age; it is less common among children and affects mainly the female sex; Chronic erosions also form more often in men, but already in old age. Acute erosive gastritis accounts for up to 5% of all gastric bleeding.
Bleeding develops in every third patient with gastric erosions, and in 3% it can be so massive that it leads to an unfavorable outcome. The most relevant study of erosive gastritis is for gastroenterologists and surgeons.
Today it is known that erosive gastritis is a manifestation of severe disorders of homeostasis, metabolism, immune reactions and microcirculation of the initial parts of the digestive tract. Today it is known that erosive gastritis is a manifestation of severe disorders of homeostasis, metabolism, immune reactions and microcirculation of the initial parts of the digestive tract.
Typically, erosive gastritis in the early stages is successfully disguised as foodborne toxic infections or an exacerbation of chronic gastrointestinal pathology
Diagnostics
Diagnostic criteria
Complaints and anamnesis: pain in the navel and pyloroduodenal area, severe dyspeptic symptoms (nausea, belching, heartburn, less often - vomiting); combination of early and late pain; loss of appetite, weakness, fatigue, headache, sleep disturbance, local hyperhidrosis.
Physical examination: signs of polyhypovitaminosis, moderate symptoms of chronic intoxication, pain in the pyloroduodenal area in the navel area.
Laboratory tests: CBC, OAM - without features, coprogram - symptoms of impaired digestion (determination of neutral fat, undigested muscle fibers), feces may be positive for occult blood. Diagnosis of H. pylori (cytological examination, ELISA - detection).
Instrumental studies: fibrogastroduodenoscopy - endoscopic changes in the mucous membrane of the stomach and duodenum (swelling, hyperemia, hemorrhage, erosion, atrophy, hypertrophy of folds, etc.).
Indications for consultation with specialists:
3. Physiotherapist.
List of main diagnostic measures:
1. General blood test (Er, Hb, L, leukoformula, ESR).
2. General urine analysis.
4. Ultrasound of the abdominal organs.
6. Diagnosis of H. pylori (breath test, HpSA in stool, determination of IgG to HP, urease test, brush cytology).
7. Consultation: dentist.
9. Consultation: neurologist.
List of additional diagnostic measures:
2. Histological examination of the biopsy specimen.
3. Daily pH-metry of the upper gastrointestinal tract - (implementation required).
4. Determination of serum Fe.
5. Determination of diastase.
7. Study of gastric juice.
8. X-ray examination of the upper gastrointestinal tract with barium.
Symptoms of erosive gastritis
Typically, erosive gastritis in the early stages is successfully disguised as foodborne toxic infections or an exacerbation of chronic gastrointestinal pathology. The patient is concerned about dyspeptic symptoms - heartburn, nausea, mild epigastric pain, flatulence and stool instability.
Therefore, the correct diagnosis is often made at the stage of manifest manifestations, when bleeding develops from the eroded mucous membrane, expressed by vomiting streaked with blood or melena (black feces containing elements of digested blood). Gastric bleeding is one of the characteristic signs of erosive gastritis. If erosive gastritis is caused by severe stress, then its first sign is most often acute bleeding, accompanied by symptoms of shock.
The main complications of erosive gastritis include shock, recurrent bleeding, anemia, infection with Helicobacter and other microorganisms, the formation of gastric ulcers, strictures and deformations of the cavity.
Erosive gastritis should be differentiated from other diseases manifested by gastric bleeding: peptic ulcer, stomach cancer and polyps, Mallory-Weiss syndrome, esophageal varices; injuries, burns and radiation damage to the gastric mucosa.
Description of code 25.9
An unspecified type of acute ulcer or chronic course without signs of perforation and bleeding is characterized by a sharp development of symptoms.
Dyspeptic disorders noted:
- nausea;
- vomiting (rare);
- heartburn;
- pain 1.5 hours after eating;
- bloating, flatulence;
- the passage of gases through the oral cavity with specific sounds.
During endoscopic examination, multiple small ulcers (up to 2 cm) in diameter are often found. Damage to the epithelium heals with the formation of delicate light scars.
The choice of treatment method, conservative or surgical, is chosen based on the presence of complications, the course of the disease and concomitant diseases. For each code according to the international classification, there are recommendations in the Orders of the Ministry of Health and Social Development on methods and methods of medical care.
Treatment of erosive gastritis
Treatment of erosive gastritis should be comprehensive; the direction of therapy largely depends on the etiology of the disease.
Treatment of erosive gastritis should be comprehensive; the focus of therapy largely depends on the etiology of the disease
Urgent measures include correction of anemia and hemodynamic disorders through transfusion of blood products and blood substitutes; medical and surgical hemostasis (electrocoagulation or endoscopic clipping of a bleeding vessel).
Etiotropic therapy for erosive gastritis usually includes gastric lavage, eradication of the infectious agent (by prescribing antibacterial, antifungal, antiviral or antiparasitic drugs).
To prevent complications of erosive gastritis, it may be necessary to prescribe medications that inhibit the secretion of gastric juice (H2-histamine receptor blockers, proton pump inhibitors, somatostatin analogues), gastroprotectors. It is mandatory to follow a therapeutic diet (in the first hours - therapeutic fasting, a gradual transition to diet No. 0, then No. 1). Antacids have a weak preventive effect against erosive gastritis.
Symptomatic treatment is aimed at eliminating the signs of the disease: if pain relief is necessary, narcotic analgesics are administered (the use of NSAIDs for acute and chronic gastritis is prohibited); antispasmodics (atropine, papaverine, platyphylline). Prokinetics (metoclopramide, domperidone) are usually used to eliminate nausea and vomiting.
Definition of illness
The symptoms of erosive gastritis are in many ways similar to the manifestations of diseases such as oncology, stomach ulcers, and varicose veins in this organ.
Therefore, it is very important to carry out a correct diagnosis of the disease in order to establish the real diagnosis as accurately as possible. What will the medical examinations include?
First of all, the patient will be asked to take a blood test (to identify inflammatory processes, complications and pathologies) and stool (to detect bloody impurities). It will also be necessary to provide vomit for examination (to identify bacteria and parasites).
A possible next stage of diagnosis would be an x-ray of the abdominal organs. This examination is performed in several projections, taking into account the different positions of the patient’s body (standing and lying). Half an hour before the procedure, the patient will need to put several Aeron tablets under the tongue to relax the organ being studied.
You may also need to conduct an ultrasound examination of the gastrointestinal tract, carried out in two stages on an empty stomach. First, an examination of the internal organs will be performed at rest. The patient will then be asked to drink a little more than half a liter of water, and the ultrasound will continue.
All of the above manipulations are very important. However, the most effective diagnostic method is endoscopy.
Erosive gastritis ICD 10
The healthcare system uses the international classification of diseases ICD-10. But the average person does not always understand how this phrase is related to the disease. Everything is very simple. This classification is intended to provide statistics on all existing diseases and health-related problems. And the number 10 in this phrase indicates the frequency with which this statistical information is collected (10 years).
Very often among the types of gastrointestinal tract there is erosive (hemorrhagic) gastritis or bulbitis. This disease is not only unpleasant, but also dangerous. Indeed, with its development, the entire gastric mucosa is affected by small, but quite numerous erosions, which not only cause pain, but also bleed quite often.
If a sick person sees the ICD-10 code, erosive gastritis, in his medical documents, a description of it, if desired, can be found in a reference book containing information about various diseases. But it is worth firmly remembering that any self-medication for this disease is fraught with serious complications. All medical prescriptions are the prerogative of the doctor! And the ICD was created only for medical specialists.
According to the ICD, the code for chronic gastritis is K-29.0. For the average person, this is an ordinary set of letters and numbers, but for a doctor it says a lot. Just seeing it in a medical document, a gastroenterologist will immediately say that it is acute erosive gastritis, complicated by bleeding.
It is dangerous because it is a precursor to an ulcer, and if treatment is ignored, it quickly develops into one. Its development is accompanied by inflammation in certain areas of the stomach and focal lesions appearing there, which have very thin, often bleeding, vessel walls.
It is needed in order to have optimal conditions for processing and analyzing all statistical data obtained from different regions and countries on morbidity and mortality. In ICD-10, verbal diagnoses are converted into an alphanumeric code, which greatly facilitates not only analysis, but also storage and retrieval of data.
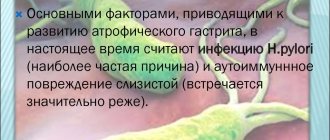
Classification of chronic gastritis
ICD 10 classifies any chronic gastritis under the Latin letter K, which includes diseases of the digestive system.
- The sign K 29.3 means a superficial chronic process.
- Atrophic chronic gastritis is encrypted under the heading K 29.4.
Chronic gastritis
- Unspecified gastritis is labeled K 29.5. It is divided into antral and fundal subspecies.
- The heading of other diseases, encrypted with code K 29.6, refers to certain types of rare chronic syndromes - giant hypertrophic syndrome, Ménétrier's disease.
- The unspecified form of the disease is coded as K. 29.7 (unspecified chronic gastritis).
- Under headings K 29.8 and 29.9 duodenitis and gastroduodenitis are coded.
Erosive gastritis acidity
Disruption of the normal level of stomach acidity leads to its improper functioning, and it is important to know its level in order to take appropriate measures.
Violation of the normal level of stomach acidity leads to its improper functioning and it is important to know its level in order to take appropriate measures
Food is not completely digested, there is a decrease in immunity, and loss of strength. How to determine acidity in gastritis? What devices should I use for this? What are the most common signs and symptoms of changes in gastric acidity?
Signs of low acidity of erosive gastritis
When the acidity of gastric juice decreases, the process of disinfection of consumed food is disrupted. This leads to additional inflammation of the mucous membrane, creating conditions for the proliferation of harmful bacteria. In some cases, a zero acidity level may be observed.
If gastritis with low acidity lasts long enough, the following symptoms are observed:
- heartburn;
- belching with the smell of rot or rotten eggs;
- stool disorders;
- metallic taste in the mouth;
- flatulence, bloating;
- anemia;
- vitamin deficiency;
- feeling of heaviness in the stomach after eating.
In some cases, immediately after eating, the patient may feel a dull pain in the epigastrium. The pain is especially pronounced when there is zero acidity. In severe forms of the disease, weakness is felt, weight loss is recorded, and a desire to lead a sedentary lifestyle is observed. Due to the fact that the lack of acidity is accompanied by impaired protein digestion, the development of hypoproteinemia is likely. All these symptoms should be a reason to visit a doctor.
Signs of increased acidity of erosive gastritis
The first symptom of increased acidity of gastric juice is almost always heartburn, which is felt after eating. The first symptom of increased acidity of gastric juice is almost always heartburn, which is felt after eating.
If a person suffers from gastritis with high acidity, the symptoms are pronounced, indicating serious irritation of the gastric mucosa. Painful sensations can occur both after eating and if a person has not eaten for a long time (“hunger” pain). Pain in the stomach area is often accompanied by a feeling of heaviness after eating, vomiting, belching with a rotten or sour odor, and all sorts of stool disorders. The symptoms not only cause some discomfort, but can also affect the functioning of the nervous system (chronic fatigue syndrome, poor sleep, irritability).
Often, with gastritis at an early stage, the patient does not feel any discomfort, however, if treatment is not carried out, an exacerbation of the disease will inevitably occur. Typically, deterioration in general condition occurs in the autumn and spring periods. These symptoms should not be ignored.
How to quickly determine acidity for gastritis
There is only one way to reliably find out the level of acidity of gastric juice when obvious symptoms of gastritis are observed - using pHmetry, however, the procedure is carried out only in medical institutions. Sometimes it becomes necessary to determine the acidity level of gastric juice at home as quickly as possible. The folk method will solve this problem. You only need one lemon.
Lemon, being an acidic product known to absolutely everyone, can become the basis of the simplest test for the level of acidity of gastric juice, and will not affect the symptoms in any way. It must be cut, smelled and tasted.
If the acidity is increased, after performing these steps a person will feel a “sour sensation” in the mouth and a huge amount of saliva will be produced. If the acidity is reduced, then a person will react to lemon calmly, without disgust, and will be able to eat it without any problems even without sugar.
Some tips
Almost all doctors say that you need to monitor your diet . This will help reduce the chance of gastritis. Stressful situations, for example at work or at home, directly affect not only the digestive system, but also the state of health in general.
Another common problem is self-medication. Gastritis is a complex and dangerous problem. Trying to deal with it on your own is obviously a false path. In order to prescribe adequate treatment, a correct diagnosis is needed. Making a diagnosis at home is almost impossible. The best solution when the first symptoms occur is to contact the appropriate specialists.
Diet for exacerbation of erosive gastritis
Erosive gastritis is a chronic disease of the stomach, in which small defects and an inflammatory process occur in its mucous membrane. The disease occurs with periods of exacerbation and remission.
Diet is, of course, very important for any disease of the gastrointestinal tract. A special regime and diet during the period of exacerbation of gastritis will help speed up the onset of remission. The diet for erosive gastritis must be followed constantly; often, it is when it is grossly violated that an exacerbation of the disease occurs.
Since erosive gastritis causes defects in the gastric mucosa, it is important to prevent mechanical, thermal and chemical damage to it. Therefore, it is necessary to exclude rough, as well as very hot and cold foods from the diet. For the same reason, all foods that irritate the mucous membrane of the digestive tract and cause increased secretion of gastric juice should be removed from the diet.
The diet for erosive gastritis is divided, 5-6 times a day, in moderate portions, preferably at the same time, the last meal shortly before bedtime (it is enough to drink a little milk or cream). You should not overeat, since it is undesirable for food to linger in the stomach for a long time, and due to long breaks between meals, the constantly secreted gastric juice will irritate the damaged mucous membrane.
Food should be chewed thoroughly; if this is not possible, food should be taken in pureed and mushy form. The method of preparing dishes is also important; fried and fatty foods take longer to digest, so it is recommended to boil, steam, stew or bake foods.
Traditional recipes for the treatment of duodenal erosion
If there is an initial stage of the disease, treatment is performed in this way. Folk remedies cannot fully replace drug therapy, especially if there is bleeding.
The main methods of treatment with folk remedies are the use of decoctions. They help eliminate inflammation and help heal wounds.
Chamomile especially has this effect; it helps eliminate painful sensations.
Sea buckthorn oil is good for restoring the stomach. It is sold in pharmacies in capsule form. To improve the functioning of the gastrointestinal tract, taking a capsule before eating food will help.
But there is a limitation in use: this is a violation of the functioning of the gallbladder and liver.
Using herbal remedies, duodenal erosion can be cured. The best options are mint, St. John's wort, chamomile and yarrow.
The decoction has analgesic, anti-inflammatory and antibacterial properties. It is necessary to combine so that each ingredient is in equal proportions.
You need to take 2 tablespoons of the mixture and pour 0.5 liters of hot boiled water. It must be left in a dark room for several hours. Must be consumed before meals.
There are also folk recipes for the treatment of duodenal erosion. For example, combine carrot juice and raw egg. The egg must be pre-cooked and washed well.
De Nol tablets for erosive gastritis
The medicine for gastritis of the stomach De-Nol today is one of the most common and effective drugs to combat this disease. In addition, the medicine is also actively used to treat other diseases associated with the gastrointestinal tract.
The medicine for gastritis of the stomach De-Nol today is one of the most common and effective drugs for the fight against gastritis
De-Nol relieves inflammation from the gastric mucosa, envelops it and helps to heal damaged cells as quickly as possible. In addition to all this, De-Nol is also recommended for gastritis in children. In case of illness in a child, the drug is calculated by weight and taken on average in half a tablet. On the Internet you can find a huge number of reviews of people taking De-Nol for gastritis.
De-Nol is sold in packages. One box can contain 56 or 112 tablets of medicine. Adults are recommended to consume De-Nol 30 minutes before meals 3 to 4 times a day. Children are supposed to be given 8-10 mg of medication per 1 kg of child weight. When taking each tablet, you should take it with plenty of liquid.
On average, all treatment with De-Nol takes place in 5 or 6 weeks, but in some cases these periods can increase to 8 weeks. It is important to remember that pharmacists and gastroenterologists strongly do not recommend taking medications that may contain bismuth for at least one and a half to two months after taking a course of De-Nol. If you are taking De-Nol medicine for gastritis of the stomach, then it is very important to know what side effects it can cause.
Like any other drug, it has a set of quite standard side effects, such as:
- feeling of nausea;
- gagging;
- problems with stool;
- rash or itching on the skin.
However, if you follow the required dosages of the drug and carry out treatment strictly as prescribed by the gastroenterologist, then these side effects may well not manifest themselves.
De-Nol penetrates into the protein base of ulcers and forms a layer of protection around them, simultaneously curing each individual affected area
De-Nol for erosive gastritis
Like other diseases, gastritis can occur in different ways, have different forms and, therefore, be treated with greater or lesser intensity of therapy. Is it possible and worth taking the medicine for gastritis of the stomach De-Nol with erosive gastritis? It is possible and necessary.
Erosive gastritis differs from ordinary gastritis in that it causes erosion to form on the gastric mucosa (ulcers in larger or smaller numbers). You already know that De-Nol has an enveloping effect.
By restoring and regenerating cells that have been damaged, it can also cope with erosion. De-Nol penetrates into the protein base of ulcers and forms a layer of protection around them, while simultaneously healing each individual affected area.
Gastroduodenitis – gastritis + duodenitis
Gastroduodenitis is a mutual disease of two organs: the stomach and the upper bulbous round part of the duodenum. Typically, chronic gastroduodenitis ICD 10 develops in the presence of inflammation in the antral - lower and pyloric compartment of the stomach, usually this is gastritis in a chronic form:
- surface;
- catarrhal;
- atrophic;
- diffuse.
The localization of the disease may be limited to only one part of the stomach or the inflammation may spread throughout the entire mucous membrane. At the same time, along with processed foods, a large amount of acid and bacteria enters the duodenal bulb. This irritates the walls, causing inflammation of the mucous membrane.
At the same time, a weakened valve and a disturbance in the contractions of the stomach and also the duodenum provokes the reverse release of alkali from the bulbous section into the stomach - reflux.
The lower sphincter, a valve, separates not only two organs: the stomach and intestines, but also juices that are completely different in composition - enzymes. In the stomach, hydrochloric acid and pectin predominate; in the intestines, alkaline enzymes break down the gruel from the stomach and, with the help of intestinal bacteria, sort out nutritious and harmful elements. These are mainly the well-known bifidobacteria and lactobacilli.
Why does pathology occur?
To understand the causes of ulcers, you must first understand the functioning of the mucous membrane lining the stomach. There is always a destructive effect on it - these are normal phenomena. A layer of mucus acts as protection. It covers the walls of the stomach. The juice it produces has a destructive effect. It contains pepsin and hydrochloric acid. The microbe Helicobacter pylori (if infected) can also have a destructive effect.
When aggressive factors have a strong impact or protection is weakened for natural reasons, one or more ulcerative lesions appear on the wall of the stomach. A person’s quality of life deteriorates as symptoms of gastric ulcer begin to appear (according to ICD-10 - K25).
Gastrointestinal tract and its ulcerative deformities in ICD
Thanks to a fundamental change in the coding of disease states of patients, the case arose for the classification of ulcers taking into account several factors. For example, the use of an additional digit in the code indicates the course of the disease or the cause that caused it. When specifying the medication that caused gastric damage, an additional code for external causes is used. The tenth revision uses nine options for classifying subtypes of ulcers. Acute hemorrhagic erosive gastritis and peptic ulcer NOS are assigned separate numbers.
Perforation is one of a number of symptoms involved in determining the course of the disease. Perforation of the wall of the stomach or duodenum is a hole that occurs as a result of exposure to aggressive factors. Due to the imbalance of protective forces and aggressive influence, the wall becomes thinner. Over time, a hole is formed through which the contents of the stomach are poured into the abdominal cavity.
Gastric ulcer according to ICD-10 is expressed in code K25. The subspecies include four acute, four chronic and one unspecified. Acute and chronic forms are divided into diseases that occur with or without bleeding, with or without perforation. As an additional digit, 0,1,2,3,4,5,6,7,9 are added through a dot.
Duodenal ulcer according to ICD-10 is designated by code K26. The principle of designating subtypes of the disease remains similar to the description of stomach ulcers. There are 9 clarifications, which include 4 acute forms: K26.0 - with bleeding, K26.1 - with perforation, K26.2 - with bleeding and perforation, K26.3 - without them. 4 chronic or unspecified forms (K26.4, K26.5, K26.6, K26.7) are classified in a similar way. The ninth form - K26.9, is unspecified, acute or chronic without bleeding or perforation.
https://youtu.be/Q08I9k1re20
And finally
As you can see, erosive gastritis is a very serious disease, accompanied by unpleasant symptoms and manifestations. To recover from the disease, it is important to consult a doctor in time and strictly adhere to the prescribed treatment.
Along with drug therapy, it is recommended to use diet and moderate exercise. You can also turn to a traditional first aid kit for help.
Any branch of healthcare has its own statistical and methodological standards, as well as a system according to which gradation is carried out. In the section that combines the diseases described to date, this is the International Classification of Diseases, 10th revision. In daily clinical practice, for convenience, this classification is usually called ICD-10. It is international in nature and designed to provide common starting points for diagnostic criteria for known diseases.