Superficial gastritis is an inflammation of the gastric mucosa, not accompanied by a violation of secretory function. The disease is persistent in nature, that is, it is characterized by a long course with periodic exacerbations. In the medical literature, this pathology is often called “type B gastritis” or “non-atrophic gastritis.”
Helicobacter pylori infection is one of the causes of the development of superficial gastritis
There are no exact statistical data on the incidence of superficial gastritis, since in most cases it occurs without any pronounced clinical manifestations, and patients do not seek medical help. According to experts, the disease affects at least 50% of the population of our planet, regardless of age. Superficial gastritis affects men somewhat more often than women.
Timely diagnosis and treatment of superficial gastritis is one of the most important problems of modern gastroenterology, since over time the disease progresses and can be complicated by the formation of ulcers, as well as a malignant tumor of the stomach.
Features and consequences of the disease
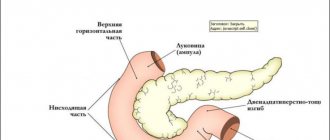
Superficial gastritis is common among all groups of the population and is considered the No. 1 pathology diagnosed when a patient complains of constant pain in the stomach. Against this background, secondary duodenitis often develops - inflammation of the mucous membrane of the small intestine - or bulbitis (damage to the upper intestinal bulb).
In the first stages of development, the disease affects the antrum - the section of the stomach bordering the upper bulb of the small intestine. A focal type of damage to the organ membranes appears. As it develops, diffuse gastritis occurs - inflammation of the entire gastric mucosa or most of it.
Important! With prolonged damage to the antrum and other parts of the stomach in a diffuse form, the disease enters a chronic stage, which is difficult to overcome.
The antrum contains cells responsible for the production of gastric secretions. Chronic pathology affects their activity, leading to irreversible processes and death. In severe cases, when the patient completely ignores diet and treatment, a diffuse type of damage to the membranes leads to the degeneration of cells into malignant ones.
Therapy
Treatment of superficial gastritis is carried out by a gastroenterologist. The nature of therapy and its duration depend on the primary etiological factors, such as morphological changes in the surface layer of the stomach, and the level of acidity. Treatment of the disease is often carried out on an outpatient basis. Hospitalization to the gastroenterology department is indicated for progressive deterioration of health and the need for in-depth examination. Active gastritis with superficial lesions in a severe stage should be treated in a hospital until remission occurs.
Drug treatment includes taking:
- drugs to suppress excessive secretion - Omez, Ranitidine;
- drugs to reduce the secretion of hydrochloric acid in the stomach - Pantoprazole;
- antacids for enveloping and protecting the inflamed membrane - Almagel, Phosphalugel;
- antibacterial agents to suppress pathogenic microflora (in the presence of Helicobacter pylori) - Metronidazole, Amoxiclav.
After the active inflammatory process subsides and enters stable remission, sanatorium-resort treatment in specialized sanatoriums is useful. Their choice depends on the characteristics of the course of gastropathy. So, for superficial gastritis of the hypoacid type, rest in Kislovodsk will be useful, for hyperacid type - in Zheleznovodsk, Pyatigorsk. Sometimes, during the period of subsidence of the disease, courses of physiotherapy (magnetic therapy, ultrasound, electrophoresis) are additionally prescribed.
Causes and mechanisms of inflammation
Mechanisms causing focal or diffuse type of pathology include:
- Metabolic and circulatory dysfunctions caused by poor blood flow . The integrity of the lining of the stomach and intestines is compromised, which can be caused by problems with blood vessels, heart failure and hypertension. With antral, diffuse disease and duodenitis (bulbitis), this leads to a reduction in the production of digestive juices. Favorable conditions are created for the growth of bacteria. Helicobacter pylori is activated - a pathogenic microorganism that, with normal immunity, remains dormant for years. In other cases, the disorder is provoked by renal failure, leading to stagnation of fluids and swelling.
- Psychosomatic factors including stress, worries and anxiety . Anxiety affects the autonomic nervous system, this negatively affects the mucous membranes of the stomach, leading to spasms and immune disorders. Reduced barrier function causes inflammation, which spreads to the upper intestines and causes duodenitis (bulbitis).
- Reverse outflow of contents - gastric reflux . Pathology occurs as part of duodenitis or antral gastritis. When the pyloric sphincter, which separates the antrum from the intestine, is damaged, partially digested food along with bile flows back into the digestive organ and aggressively affects its lining.
- Activation of Helicobacter pylori (HP) . Bacteria multiply in favorable conditions, causing chronic antral gastritis, and with it bulbitis and other forms of inflammation of the mucous membranes. The microorganism destroys thin epithelial cells.
The provoking factors of superficial gastritis primarily include chronic infections occurring in the body. These may be lesions of the ENT organs, as well as other bacterial infections that penetrate the digestive organ. Chronic tonsillitis is one of the most common pathologies that provoke gastritis.
Fact! Increased acidity occurs as a result of various reasons, often developing against the background of gastric reflux. Due to the aggressive action of acid, the walls of the stomach are destroyed, which causes inflammation.
A separate group of causes that cause antral, focal gastritis, bulbitis and gastric reflux are bad habits and poor diet . People who smoke more than 20 cigarettes a day have an extremely high risk of the superficial form of the disease. This is due to the negative effect of nicotine on the mucous membranes and pyloric sphincter.
Alcohol, coffee, tea - especially on an empty stomach - irritate the mucous walls. Spicy, peppery, too salty foods, preservatives, dyes and flavors have a similar effect. Poor nutrition provokes the appearance of focal and diffuse gastritis even in completely healthy people (without chronic infections in the body).
Another group of factors is uncontrolled or forced use of medications. These include: indomethacin, salicylic acid, digitalis, corticosteroids, NSAIDs. Most drugs negatively affect the mucous membranes.
Classification and stages of pathology
Superficial gastritis is classified depending on the area of inflammation, the histological features of damage to the gastric epithelium, the provoking factor and the level of acidity. From the point of view of localization of the superficial form of gastropathy, the following are distinguished:
- distal gastritis - pathological processes cover a third of the most distant part of the stomach;
- antral gastritis, with characteristic inflammation in the outlet part;
- fundal - catarrhal changes affect the bottom of the organ;
- gastritis with damage to the body of the stomach;
- pangastritis is an inflammation that completely covers the entire epithelial layer of the organ.
Classification according to provoking factors includes:
- medicinal superficial gastritis, which occurred in response to uncontrolled use of medications that irritate the stomach (aspirin, antibiotics, hormone-containing drugs) or during long-term treatment without taking into account side effects;
- endogenous - appeared as a result of an imbalance of metabolic processes, dysfunction of the gastrointestinal tract;
- bacterial - inflammation of the epithelium and mucous layer against the background of activation and proliferation of pathogenic flora (Helicobacter pylori);
- superficial reflux gastritis is one of the dangerous forms of pathology caused by the ingress of acidic masses during reflux from the duodenum into the stomach cavity.
Superficial gastritis sometimes affects the mucous membrane selectively - a focal form. It is typically characterized by the presence of small inflamed islands scattered throughout the mucosa. Based on the level of acidity, the disease is divided into hyper-, hypoacid and gastritis with normal secretion of gastric juice.
The disease occurs in several stages:
- mild (initial) - minimal cell degeneration is observed in the epithelial layer against the background of a weak inflammatory process;
- medium - moderately severe catarrhal process with an increase in the number of epithelial cells that have undergone degeneration; along with superficial inflammation, the process of infiltration develops;
- strongly expressed - an acute pathological process involving the entire muscular structure of the mucous membrane in infiltration; severe gastritis is characterized by signs of active dystrophy, the number of cells with defects exceeds the number of healthy ones.
Difference between chronic, active and acute disease
A big problem for many patients is understanding how active gastritis differs from acute and chronic:
- The acute form of inflammation manifests itself with dangerous, severe symptoms. In addition to abdominal pain, vomiting, belching, nausea, flatulence, and a feeling of heaviness occur. The patient is uncomfortable doing usual activities. Without taking pills it becomes difficult.
- Chronic superficial gastritis develops against the background of all forms of pathology: bulbitis in combination with the antral type of the disease, due to focal or diffuse pathology, gastric reflux. In the chronic course, the symptoms are not as strong as in the acute stage of inflammation. Often this form develops due to untreated aggravated gastritis. In some patients, superficial chronic inflammation occurs without unpleasant symptoms.
- The active stage of the disease accompanies the acute and initial stages of gastritis. But, unlike them, it is manifested not only by symptoms, but by the progression of the disease. It reaches the deeper layers of the mucous membrane. The antral, focal form at this stage becomes erosive - not only the mucous membrane is affected, but also other structures.
The combination of superficial gastritis with bulbitis and damage to the antrum cannot be determined without diagnostic procedures. Symptoms of pathology are often ignored or not noticed by patients. But, if you are able to recognize them in the first stages, it is easy to stop the development of the disease.
Traditional methods of elimination
According to popular belief, for this disease, it is recommended to take magnesium sulfate (on the tip of a knife) after meals. It is advisable to drink green tea; you should add as much boiled beets and buckwheat porridge to your diet as possible.
Since ancient times, bitter herbs have been considered the main healer of gastritis. This is due to the fact that bitterness excites the nerve endings in the walls of the stomach. As a result, the production of gastric juice and appetite increase, food does not stagnate in the stomach. These herbs relieve constipation and kill pathogens. Treatment includes the following recipes:
- Apply a quarter glass of blackcurrant juice 3 times a day. Used for decreased secretion of gastric juice.
- Drink 3/4 cup of potato juice on an empty stomach 1 hour before meals. Used for high acidity.
- Aloe juice is consumed several spoons 3 times half an hour before meals for a course of up to 2 months. Used for gastritis with constipation.
- Treatment is possible with infusion of plantain. Pour 15 g of crushed herb leaves into 1 cup of boiling water. Leave for 10 minutes, then strain. Drink in small sips 1 hour before.
- Infusion of burdock roots. Pour 5 g of crushed root into 2 cups of boiling water. Leave for 12 hours, then strain. Drink half a glass 3 times a day.
Symptoms of superficial gastritis
Catarrhal disease is difficult to notice in the first stages; most often, patients pay attention to the symptoms of the acute stage:
- appetite decreases or disappears;
- severe weakness appears;
- dizziness and headaches develop;
- pain in the epigastric region;
- acid belching appears;
- an unpleasant taste appears in the mouth;
- bad breath is noted;
- saliva viscosity increases;
- increased gas formation and flatulence;
- the pain is localized on the right side in the hypochondrium, flows into other parts of the abdomen;
- yellow, white or gray coating may form on the tongue;
- At the peak of the disease, blood pressure decreases and the heart beats faster.
These signals indicate a rapid progression of the disease and require an immediate review of diet, giving up bad habits, followed by contacting a doctor for examination.
Allowed and prohibited foods for gastritis and stomach ulcers
Diet for gastritis and proper nutrition for stomach ulcers have similar principles. If an exacerbation of diseases occurs, you need to avoid irritating foods. In this case, daily meals may include the following products:
- Dried or slightly stale wheat bread.
- Puréed cereal or milk soups.
- For gastritis and ulcers, steamed meatballs and cutlets are allowed.
- Soufflé with lean fish, poultry, lean meats.
- If you have gastritis, you must consume low-fat milk, cottage cheese, cream, and sour cream.
- For gastritis, proper nutrition involves eating oatmeal, semolina, and rice porridge.
- Vegetables (beets, potatoes, zucchini, carrots) are allowed in the form of puddings.
When diagnosing ulcers and gastritis, daily nutrition should exclude the following foods:
- In order not to irritate the stomach, you need to avoid salty, spicy, fatty, and fried foods.
- For gastritis and ulcers, proper nutrition prohibits fatty meat, canned food, strong broths, hot sauces, and various marinades.
- Salty cheeses.
- Puff pastry is prohibited for ulcers and gastritis.
- The consumption of salt is minimized, because it not only retains excess water in the body, but also irritates the gastric mucosa.
- Spinach, white cabbage, cucumbers, sorrel, onions.
- Carbonated drinks and strong coffee are strictly prohibited for gastritis and ulcers.
- Fresh bread, baked goods, sweet pastries.
- Whole milk products.
- Grape.
- Legumes.
Methods for diagnosing the disease
The way to make an accurate diagnosis is fibrogastroduodenoscopy (FGDS). With the help of special equipment, the doctor is able to examine the cavity of the internal organs: the upper and lower sections of the stomach, antrum, and intestines. With its help you can find out about the onset of superficial gastritis. Other techniques - ultrasound, x-rays using a contrast agent - are informative at more serious stages of the disease.
During the preliminary diagnosis, procedures such as a breath test are carried out (determination of ammonia, which is formed during the activity of Helicobacter pylori). The patient is prescribed tests to identify the bacteria, as well as a standard set of laboratory tests: stool, urine, and blood. To determine acidity, stimulation with pentagastrin is prescribed.
Etiology
In almost all cases, the causative agent of superficial chronic gastritis is the bacterium Helicobacter pylori. But an exacerbation of the condition occurs under the influence of predisposing factors, which are divided into external and internal. The first group of reasons includes:
- poor nutrition, eating large amounts of fatty and spicy foods, preparing food from low-quality products, poor chewing of food and frequent overeating;
- addiction to alcoholic beverages, nicotine and drugs;
- Regularly taking medications without following the dosage or doctor’s prescription. These medications include hormones, corticosteroids, anti-inflammatory agents, and some types of antibiotics. Such drugs not only lead to thinning of the gastric mucosa, but also lead to a decrease in immunity;
- harmful working conditions – constant contact with dust or chemicals.
Internal factors include:
- diabetes;
- dysfunction of the endocrine system;
- diseases of the cardiovascular system;
- reflux gastritis;
- emotional disturbances;
- adrenal, pulmonary and heart failure;
- anemia;
- lack of one or a group of vitamins in the body;
- worms;
- autoimmune processes.
Establishing the cause of the disease is an important part of diagnosing and treating the disease.
Pathology treatment methods
Superficial gastritis with duodenitis, or without involvement of the upper intestines, is treated only with an integrated approach. Excluding diet, but taking medications, or using only folk remedies is ineffective.
Diet for gastritis
When treating a disease, diet is a prerequisite for recovery. Patients are prescribed treatment table No. 1A during exacerbation, No. 1B after symptoms subside. In the future, the person sticks to table No. 1. Basic rules when creating a menu:
- the use of products that do not stimulate the production of gastric juice (lean meat and fish, low-acid cottage cheese, soups with secondary broth, steamed vegetables, omelettes, jelly and compotes);
- food should be warm - hot and cold dishes irritate the stomach;
- overeating should not be allowed - eat 5-6 times a day in small portions;
- ideal serving form - pates, finely chopped dishes, absence of coarse fibers in food;
- complete exclusion of rough types of food - chops, pieces of meat, fried foods, sour fruits and juices, vegetables, alcohol, spices.
During an exacerbation, soups are prepared only from semolina, rice or oatmeal; vegetables are completely excluded from the diet. It is forbidden to eat crackers - they injure the membrane and can spread inflammation.
The most preferred fruits during the diet are sweet varieties of apples and bananas, but citrus fruits are prohibited. Among the juices are apricot, peach, pear. Sweet dishes are not prohibited during this period, but they must be homemade: mousses, marshmallows, marshmallows, jam and preserves, berry jelly.
Compliance with the principles of therapeutic nutrition will help eliminate antral gastritis and bulbitis. The enveloping effect of non-acidic foods soothes the irritated antrum, as well as other parts of the intestines and stomach. Only thanks to a gentle diet can you get rid of painful sensations for a long time.
Drug treatment of the disease
To cure superficial gastritis to complete remission, you need to use medications. They should be prescribed by a doctor. With the help of drugs, symptoms are eliminated, Helicobacter activity is reduced, and restoration of the mucous membrane is stimulated:
- Proton pump inhibitors . They block the excessive activity of acid-producing cells in the digestive organ. Omeprazole, Esomeprazole, and Lansoprazole are highly effective.
- Regenerative acid blockers . Otherwise, they are called histamine H blockers. They help moderate the main symptom in the form of pain and negative reactions: Cimetidine, Ranitidine, Famotidine.
- Antacid substances . Neutralize acid and protect organ walls: “Maalox”, “Almagel”, “Phosphalugel”, “Gastratsid”.
- Medicines to relieve spasms . Relaxes the intestinal muscles and relieves pain: “Papaverine”, drugs based on drotaverine.
- Antibiotics to eliminate Helicobacter . The most effective against bacteria are Metronidazole, Flagyl, Clarithromycin.
Since superficial gastritis with bulbitis, damage to the antrum or the entire mucous membrane weakens a person and is associated with a decrease in immunity, vitamins are additionally prescribed. These can be either multivitamins or individual preparations with ascorbic acid and B12. Most often they are used during the rehabilitation period.
Physiotherapeutic treatment
Microwave therapy can relieve the patient from pain associated with various forms of gastritis. The action of microwaves relieves inflammation, stimulates the fight against bacteria, relieves pain and improves recovery processes in the antrum and other parts of the organ. For severe pain, a course of mud treatment with peat, sulfide, silt and sapropel compounds is prescribed.
Folk remedies
It is possible to treat the superficial form of the disease (including bulbitis, gastric reflux or duodenitis as secondary forms of gastritis) using folk remedies if approved by the doctor.
Important! Each recipe is discussed individually. The specificity of the use of natural components lies in the variability of their effectiveness. What helps one person may negatively affect the health of another and complicate treatment.
Dosages are also monitored by the doctor and, if necessary, changed. In the treatment of superficial gastritis with the addition of bulbitis, methods based on the use of:
- honey and apple cider vinegar diluted in water - the combination restores the pH of the gastric environment and suppresses the activity of bacteria;
- yogurt as a sauce - daily use normalizes digestion and intestinal microflora;
- soda - exclusively as an emergency remedy for severe heartburn, but not too often;
- aloe vera diluted in water - the product relieves irritation and inflammation;
- ginger, turmeric - these spices act as natural antibiotics, suppress inflammation and irritation;
- cabbage or potato juice - when fresh, the liquid restores the acidity balance and relieves inflammation;
- coconut water and oil - used as vitamins and anti-inflammatory agents;
- almond milk – relieves inflammation;
- green tea with honey - the drink fights irritation and saturates with vitamins;
- cumin tinctures – seeds relieve gas formation, help if the stomach starts to hurt;
- non-acidic kefir - acts like yogurt;
- ripe pineapple – the fruit fights bacteria, improves digestion, but only if it is perfectly ripe (green pineapple irritates the stomach);
- oatmeal - porridge from this cereal envelops the walls of the organ, reduces acidity;
- medicinal marshmallow - root, diluted in water, soothes irritated membranes, suppresses heartburn;
- rosemary – in the form of a decoction, the herb fights pain, heartburn and other symptoms of the disease.
Superficial gastritis is a form of the disease that is best treated. In fact, the affected mucous membrane without deep erosions is capable of regeneration. But such a result is only possible if the patient makes every effort to undergo treatment and follows the recommended diet.
Nutritional Features
Diet for superficial gastritis is an integral part of complex therapy. The point of the diet is to create a minimal load on the gastrointestinal tract through chemical and temperature sparing. When creating a menu for patients, the type of acidity is always taken into account. Nutrition principles, the observance of which will speed up the restoration of the functionality of the stomach and digestive tract:
- eating in small portions, no more than 250 ml of food per meal;
- fractional meals, at least 5 meals per day;
- the correct temperature when serving food is 50–55°;
- the correct consistency of food - in the form of a homogeneous puree, in a semi-liquid form (especially during the period of relapse);
- exclusion of foods with coarse fiber (raw cabbage, nuts, beans, bran), high content of extractive substances (strong meat broths, sauces).
The menu for patients with superficial gastritis includes:
- pureed soups from potatoes and other soft vegetables;
- pureed mucous porridge (oatmeal, rice, buckwheat);
- boiled lean meat (rabbit, veal);
- minced fish dishes, fish allowed with low fat content;
- low-fat dairy products (snowball, fermented baked milk);
- jelly, compotes without sugar;
- non-acidic fruit juices (apple, peach).
Treatment measures
Therapy involves a complex effect, including dietary nutrition along with taking medications. For mild gastritis, therapy consists of prescribing anti-inflammatory drugs. If there is no positive dynamics, then antibacterial drugs are prescribed. If an increased number of Helicobacter pylori is detected, antibacterial therapy is mandatory. The following types of medications are used:
- Amoxiclav;
- Azithromycin;
- Levofloxacin;
- Metronidazole;
- Amoxicillin.
To protect the gastric mucosa, antacid and enveloping drugs are prescribed. Taking them reduces the increased acidity of the stomach (Phosphalugel, Rennie, Almagel, Maalox). If pain is severe, analgesics and drugs that block the effects of acetylcholine (anticholinergics) are prescribed. They affect the receptors of nerve endings and relieve pain (Platifillin, Metacin and Atropine). To regulate the production of hydrochloric acid, proton pump inhibitors are prescribed. These include Omez, Omeprazole and Pantoprazole.
Manifestations of gastritis in adolescents and children
The first symptoms of gastritis in adolescents and children are somewhat different from those in adults. More precisely, the symptom complex is similar, but manifests itself differently.
- Moderate or severe pain in the solar plexus area, often local, without irradiation to other parts of the abdominal cavity;
- Heartburn, which occurs mainly after physical activity (in adolescents after passing physical education standards at school, in children - after sports games with jumping and sharp bends);
- Belching (sometimes with small amounts of food eaten);
- Discomfort in the epigastrium after eating;
- Loss of appetite;
- Severe and sharp pain in the epigastric region upon palpation.
In children, the signs of hypovitaminosis due to gastritis are more pronounced than in adults. The skin becomes pale, sometimes bluish. The general condition is regarded as lethargic - the child becomes capricious, refuses previously captivating entertainment, and loses his addiction even to his favorite delicacies. Sleep and daily routine are disrupted. Many children complain of fatigue after eating - as if they were “tired” while eating it. Signs of dyspepsia are almost always accompanied by signs of anemia.
In acute gastritis, symptoms include nausea and vomiting. They can appear together, or replacing each other. In severe cases, vomiting becomes unproductive and indomitable, causing general dehydration of the baby's body. Persistent diarrhea, which is also often observed with gastritis in children, can increase dehydration.
We recommend: Heartburn during pregnancy
Since the first manifestations of gastritis in adolescents and children are noticeable, the prognosis for treatment is better than in adults who are accustomed to ignoring changes in the body until the last moment. If your baby has any of the above complaints, you should urgently visit a pediatric gastroenterologist.
The symptoms of gastritis in children are discussed in more detail in this article.
Sample menu for the day
It is advisable to chop vegetables.
An individual diet is selected for each patient, but most often it looks like this:
- First breakfast: grated rice porridge with milk;
- unpalatable cracker;
- cup of cocoa.
- baked red apple.
- light broth soup with cereals and vegetables;
- tea with milk;
- boiled fish with a side dish - buckwheat or other porridge;
If a person’s stomach becomes inflamed due to reduced enzyme formation, broths, tomatoes, pickles, kefir, yogurt, cottage cheese, still mineral water, and berries are added to the menu. When chronic gastritis worsens, the diet is supplemented with puree soup, soft-boiled eggs, lean meats and fish.
https://youtu.be/dG-skMegvik
Site for women: relationships, beauty, fashion, children
Superficial gastritis is one of the most common diseases, the scourge of modern man with his frantic rhythm, quick snacks, fast food, etc.
Superficial gastritis is a chronic form of inflammation of the gastric mucosa. Its main difference from other types of gastritis is that inflammation affects only the upper layer of the mucous membrane, without damaging deeper tissues. Often superficial gastritis is accompanied by inflammatory processes in the duodenum (duodenitis).
In the absence of treatment and a special diet, superficial gastritis becomes atrophic, when inflammation invades the gastric glands.
The main causes of superficial gastritis are: irregular food intake, infections, the predominance of salty, smoked and spicy foods in the diet, smoking, alcoholism, genetic predisposition, various diseases of other organs and systems.
Medication
Drug therapy includes:
- coating substances to protect the mucous membrane;
- antisecretory drugs that reduce the secretion of hydrochloric acid;
- antacids that reduce HCl levels;
- antibiotics affecting Helicobacter pylori.
Subsequently, vitamin therapy may be needed for rapid recovery, increasing the body's resistance and overall immunity.
Diet menu for chronic and erosive gastritis?
Erosive gastritis is the first stage of a stomach ulcer, so this disease is considered very serious. It is characterized by the appearance of ulcers on the gastric mucosa, and there can be many reasons: liver disease, lung disease, burns, kidney failure, and so on. The diet for erosive gastritis is based on several principles:
- Food should be strict and gentle.
- Liquid, warm grated food without fat for several years.
- A complete ban on alcohol, smoking, raw vegetables, strong broths, carbonated drinks, fried foods.
- Give preference to cereal soups, porridges, soufflés, casseroles, and jelly.
Professor gastroenterologist and Dr. Nonna will tell you how to eat properly and what diet to follow for erosive gastritis in the video below:
https://youtu.be/YJjoc_CMthQ
For any disease detected in the gastrointestinal tract, the patient must be prescribed a diet. And superficial gastritis, despite the fact that it is considered a fairly mild version of this difficult disease, is no exception to this list.
A diet with it is not only a special diet that facilitates the functioning of an inflamed stomach, but is the most important means of treatment, thanks to which taking prescribed medications becomes most effective. If it is strictly followed, the digestion process is completely normalized.