Why do most people with gallstones have pancreatic problems? Acute pancreatitis, as well as exacerbation of gallstone disease, are life-threatening conditions. Photo: Commons.Wikimedia
According to statistics, 70% of patients with gallstones develop inflammation of the pancreas.
Articles on the topic
- “Cleansing” the liver
- How to lose weight without harming your liver
- Fitness for the liver. Pilates
- Lift my eyelids: why do you want to sleep after eating?
- How to help yourself after New Year's Eve. Step-by-step recommendations
Author of the article:
Karina Tveretskaya
- Site Editor
- Work experience - 11 years
Views: 47434
Reading time: 3 min.
The human body is a mechanism in which every detail is in its place and each performs a vital function. At the same time, the parts do not work separately: they are connected into a single system, so as soon as one element “falls out of life,” all the others are at risk. It's the closest neighbors who have the hardest time. This explains the statistics according to which 70% of patients with cholelithiasis (GSD) have problems with the pancreas. The most common complication of cholelithiasis is pancreatitis.
Which UDCA drug is more effective for cholelithiasis: a study. Candidate of Medical Sciences, hepatologist Sergei Vyalov, in his new study, compared the effectiveness of three UDCA-based drugs in patients with cholelithiasis and biliary sludge.
How cholelithiasis causes pancreatitis
The combined ducts of the organs constantly interact with each other, therefore, with cholelithiasis, a stone pushed out of the gallbladder, having passed the bladder duct and the common bile duct, “stagnates” where they merge and flow into the intestine. This pathology in case of cholelithiasis is most common and is explained by the fact that the area of the nipple of Vater (where the ducts flow into the intestine) is the narrowest place in terms of patency in all biliary tracts.
The pancreas and liver produce secretions and bile. During an exacerbation of cholelithiasis, both fluids entering the canals do not find an outlet into the intestines - it is blocked by a stone. The pressure in the ducts increases, which leads to rupture. The contents enter the pancreatic tissue. Enzymes that break down carbohydrates, fats and proteins are inactive while in the duct. But when the gland cells rupture, the enzymes are activated, triggering the process of self-digestion of the organ, which causes an attack of acute pancreatitis or pancreatic necrosis - a disease most dangerous to human life.
It is precisely this mechanism for the development of pancreatitis that is observed in gallstone disease, which is caused by gallstones that block the duct. To prevent pancreatitis and pancreatic necrosis, doctors urge patients to promptly and promptly remove stones from the gallbladder and to be careful when taking choleretic preparations and medications with such a diagnosis. After all, it is impossible to predict how the stone will react to “persecution”, whether it will be able to slip into the duodenum without getting stuck along the way, causing an attack of acute pancreatitis.
Diet and nutrition for cholelithiasis and pancreatitis
For cholelithiasis and pancreatitis, it is recommended to minimize the amount of consumed foods that contain large amounts of cholesterol. Regulating cholesterol metabolism in the body involves reducing the calorie content of food consumed. Often, patients with this diagnosis need to completely avoid foods such as liver, fatty fish, egg yolk, as well as lard and animal fats. At the same time, the diet of a patient with gallstones and pancreatitis should contain foods rich in magnesium salts. This element helps remove cholesterol from the body, which provokes exacerbation of cholelithiasis.
In order to prevent attacks of cholelithiasis, it is necessary to eat a diet that allows you to constantly maintain the cholesterol contained in bile in a dissolved state. A diet that includes alkaline mineral waters and plant foods leads to an increase in alkali in bile, and, as a result, the dissolution of cholesterol. It is important to note that for a speedy recovery, it is important for a patient with cholelithiasis and pancreatitis to eat a large amount of vegetables, and also to cook only steamed, baked and boiled dishes.
Postoperative period
Treatment in the postoperative period consists, first of all, of following a proper diet. This is how you can avoid exacerbations of pancreatitis.
When there is no gallbladder in the body, the secreted bile gradually flows into the intestines, constantly, and not only when a person eats food.
This phenomenon reduces the resistance of organs and causes inflammatory foci in the pancreas, which is called pancreatitis. In addition, a disorder of the intestinal microflora can lead to constipation and diarrhea.
To prevent inflammation, the patient is prescribed diet number five according to Pevzner, with adjustments by the gastroenterologist if necessary. The basic rules of this diet are as follows:
- Fractional meals in small portions;
- Increased number of small meals - up to six, seven times a day;
- Limiting fatty and spicy foods;
- Limiting pickles, canning - both homemade and store-bought, in particular;
- Preference is given to boiled, stewed and baked foods;
- The food should be served neither hot nor cold, the temperature should be slightly above room temperature;
- Products that cause fermentation processes in the intestines are excluded: baked goods and rye products, confectionery, pickles, apples, cabbage;
- Products made with preservatives, substitutes, dyes, flavors, and flavor enhancers are excluded.
How to treat chronic pancreatitis and cholecystitis?
Have you been struggling with LIVER PAIN for many years without success?
Head of the Institute of Liver Diseases: “You will be amazed at how easy it is to heal your liver just by taking it every day.
Pathology of the pancreas and gall bladder occupies a significant place among diseases of the digestive organs. Often, with chronic cholecystitis (inflammation of the gallbladder) or against the background of cholelithiasis, pancreatitis (inflammation of the pancreas) develops. Conversely, cholecystitis can be a complication of chronic pancreatitis as a result of damage to the gallbladder when pancreatic juice enters it.
Functioning of the gallbladder and pancreas
The pancreas and gallbladder play an extremely important role in the digestive process, and the activity of these organs is interconnected. The pancreas produces hormones (insulin, etc.) and digestive enzymes. They enter the duodenum through the bile duct, where they come into active form, mixing with other enzymes and bile and digesting fatty and protein foods.
The gallbladder stores bile produced by the liver. Concentrated bile enters the duodenum through the bile duct. Thus, diseases of the gallbladder and ducts can contribute to the development of pancreatic pathology.
Causes of diseases
Long-term inflammation of the gallbladder is often a consequence of cholelithiasis, which is manifested by the formation of stones in the organ. A person may not know about his disease. Sudden pain when stones enter the bile ducts indicates an exacerbation of the disease. This is how biliary colic occurs, accompanied by vomiting and acute pain under the right hypochondrium. In addition, the causes of chronic cholecystitis are:
- dyskinesia of the bile ducts, leading to stagnation of bile;
- infection with bacteria (Escherichia coli, Streptococcus, Salmonella, etc.);
- infection with parasites (Entamoeba histolytica, Enterobius, Ascarididae, etc.);
- pathological change in the wall of the gallbladder that develops when pancreatic secretions penetrate or blood supply decreases;
- hereditary predisposition and psychogenic factors.
Chronic pancreatitis develops when the removal of secretions from the pancreas is impaired. This leads to self-destruction of the gland tissue by enzymes, its inflammation and, subsequently, to the formation of scars.
Chronic pancreatitis most often affects men, and chronic cholecystitis affects women over 50 years of age who are overweight.
Pancreatitis occurs against the background of:
- alcohol abuse (more than 65% of cases);
- diseases, surgical interventions and anomalies of the digestive system;
- poisoning, trauma or abdominal wounds;
- post-infectious complications (viral hepatitis, mumps, etc.);
- hereditary pathology of the digestive organs;
- deviations in hormonal status and metabolism;
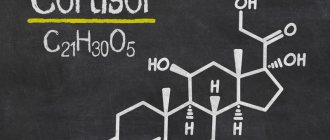
- consequences of the use of medications (estrogens, in particular, cortisol and antibiotics).
Consequences of the operation
If pancreatitis is a consequence of cholelithiasis, then cholecystectomy can improve the general condition, remission will last longer, and the intervals between periods of remission will decrease. This usually happens when the operation was successful and was performed in the initial stage, when the disease has not yet advanced.
Then the elimination of bile duct obstruction caused by the presence of stones helps to improve the health of the pancreas. The function of pancreatic juice secretion returns to normal in 62.55% of patients.
Timely surgery leads to recovery in more than half of cases
But in many cases, after surgery to remove the gallbladder, a syndrome called postcholecystectomy may appear.
Typically this condition develops for the following reasons:
- incorrectly chosen tactics of the operation or errors during its implementation;
- disorders in the functions of individual organs after removal of the gallbladder;
- existing liver diseases;
- adaptive restructuring of the digestive system with the possible formation of pathologies after cholecystectomy.
With the development of postcholecystectomy syndrome, chronic pancreatitis is often associated. Although no exact figure can be given, the detection rate varies widely from 5% to 90%.
Postcholecystectomy syndrome can occur both after abdominal and after laparoscopic surgery, if errors were made during the intervention
Healthy eating for cholelithiasis and cholecystitis
Gallstone disease (calculous cholecystitis, gallstones) is characterized by the formation of stones in the gallbladder and ducts and inflammation of their mucous membranes. According to statistics, the risk of developing this disease in women is much higher than in men.
However, in men, stones (calculi) in the gallbladder are also quite common. Doctors say that every tenth man suffers from this disease. Stones can be cholesterol (the most common type), calcareous, pigment, or a combination type.
Symptoms and complications of calculous cholecystitis
The period of asymptomatic course of this disease can be very long, when the stones in the gall bladder reach a large size, discomfort begins to appear.
The main reasons for the appearance of stones are chronic infectious diseases, poor nutrition, changes in the structure of bile in women under the influence of hormonal levels, and genetic predisposition.
GSD is often accompanied by disturbances in the digestive tract (for example, nausea, constipation and loose stools, bitterness in the mouth). Inflammation of the mucous membrane of the gallbladder can cause an increase in body temperature. Large stones in the gallbladder cause pain in the right hypochondrium. Calculous cholecystitis leads to the appearance of yellowness of the skin and sclera of the eyes (in case of blockage of the bile ducts by stones).
An attack can be triggered by stress, hypothermia, or physical exertion. Symptoms worsen 2-4 hours after eating fried, smoked or fatty foods, as well as food with hot pepper, vinegar and other seasonings.
Possible complications of calculous cholecystitis:
- transition to chronic and acute pancreatitis;
- biliary peritonitis;
- gallbladder gangrene;
- hepatic colic.
Principles of diet for joint illness
The combination of cholelithiasis and pancreatitis requires adherence to fairly strict nutritional principles:
- exclusions from the menu of foods containing high amounts of cholesterol;
- minimizing bile concentration;
- selection of products containing a fairly large amount of magnesium salts and unsaturated fatty acids in order to remove excess cholesterol;
- increasing the share of fresh vegetables in the menu;
- replacing all methods of heat treatment of food with one - steaming.
Meals should become fractional - food should be taken up to 6 times a day, but in small portions. Fluid intake should be increased to at least 2 liters per day.
What products should be included in the diet?
The recommended diet for a combination of cholelithiasis and pancreatitis should include foods containing plant fiber, vitamin complexes, and magnesium salts. In this case, the food must be pureed and the drink heated. This diet provides:
- stimulation of intestinal peristalsis;
- reduction of inflammatory phenomena;
- weakening of spasms.
The table below indicates which products and in what form are acceptable for people diagnosed with gallstone disease in combination with pancreatitis:
| Food group | Permitted varieties |
| Meat | Chicken, rabbit, lean beef, lean river fish. |
| Eggs | Protein omelet, whole, hard-boiled. |
| Fats | Vegetable, without exacerbation - butter. |
| Flour | Cookies based on rye bread. |
| Pasta, cereal | Buckwheat and oatmeal porridges, pasta, except durum varieties. |
| Soups | Vegetables. |
| Milk | Whole milk, low-fat cottage cheese, kefir. |
| Vegetables fruits | Any, except greens and sour varieties. |
Drinks include teas, compotes and juices. If you are overweight, the patient should greatly limit sweets, cereals, and baked goods.
Products prohibited for pathologies
With this combination of pathologies, the diet should not include the following food items:
- salo;
- coffee;
- greenery;
- pork;
- sausages;
- alcohol;
- margarines;
- smoked meats;
- offal;
- fatty milk;
- sour varieties of berries;
- rich broths;
- fatty preserves;
- smoked cheeses;
- carbonated drinks;
- durum pasta;
- baked goods, pies, varieties of white bread.
But food should also not contain seasonings such as pepper, vinegar and mustard. It is not recommended to eat immediately before going to bed, and the lunch meal should be leisurely.
Sample menu for cholelithiasis and pancreatitis
For a patient suffering from a combined pathology of this kind, various diets are used, depending on the phase of the disease.
For the remission period, for example, the following menu is suitable:
- Breakfast: steamed meatballs combined with carrot salad.
- Lunch: rice or cottage cheese casserole with vegetable salad.
- Lunch: steamed fish cutlets with rice.
- Afternoon snack: white omelet.
- Dinner: potato soup with pumpkin-apple salad.
Drinking liquid after meals is allowed no earlier than a quarter of an hour (with the exception of lunch and afternoon snack) in the form of:
As soon as one week of such nutrition has passed, the patient should arrange a fasting day with a reduced calorie content: for breakfast, lunch, lunch, afternoon snack and dinner, 0.9 liters of kefir and a mixture of 0.15 kg of sugar with 0.3 kg of cottage cheese are equally divided.
In the summer-autumn season, the optimal solution would be a fasting day, during which the only food product is fruit.
In cases where the disease has worsened and there is severe pain, eating food is prohibited. The patient should limit himself to drinking water for two to three days. During this time, the pancreas and vesica biliaris have time to rest, and the release of bile becomes less. On the 4th day, the patient can be transferred to table No. 5. In this case, food should be divided into small portions, and meat and broths should be excluded.
Example 5 of a dietary table for gallstone disease
Food is served fresh, boiled or stewed. This set of products has a contractile effect on the gallbladder, leading to the flow of stagnant bile, preventing unnecessary stress on the organ and providing it with rest.
Approximate menu for one day:
- Breakfast: oatmeal soup with a slice of cheese on rye bread.
- Lunch: juicy pear.
- Lunch: boiled rice with fish meatballs, washed down with fruit compote.
- Afternoon snack: soft crackers with a glass of low-fat milk.
- Dinner: add a vinaigrette in vegetable oil with boiled egg yolk and wash it down with a glass of kefir with the addition of softened dried apricots.
The exacerbation phase of a combination of pathologies requires being on such a diet for at least a week. More than one review from people suffering from these diseases claims that the longer and stricter the diet is followed, the longer the remission will be.
What products are prohibited?
Various diseases of the gastrointestinal tract, including pancreatitis due to the removal of the gallbladder, imply a stop list for many products. Among these are the following:
- mushrooms;
- baked goods and confectionery (cakes, sweets);
- various sauces, mustard, mayonnaise;
- spices with a pronounced taste effect (curry, pepper, cinnamon, coriander);
- sparkling water;
- marinade, pickled vegetables, preserves;
- ice cream.