Exacerbation of pancreatitis occurs against the background of an acute illness. Every patient with pancreatitis should understand that the disease can manifest itself only six months later, immediately after its onset.
During this period of time, doctors diagnose a relapse of the acute form. If treatment is not started in time, the patient’s condition worsens, causing an exacerbation of chronic pancreatitis. Let's look at the main signs and find out what to do in case of exacerbation of pancreatitis.
Recommendations from Elena Malysheva in the special issue “Live Healthy!” on how to overcome pacreatitis using the healing effects of natural remedies.
First symptoms
An attack of pancreatitis has pronounced symptoms and it usually begins with pain , which is localized in the following parts of the body:
- Upper abdomen.
- Back.
- Shoulder blades.
- Small of the back.
The pain syndrome is cutting, dull or encircling in nature and can even cause shock and fainting. The patient is unable to lie down; relief occurs only in a sitting position with the legs pressed to the stomach.
Then the person begins to vomit, food and bile come out of the stomach. There is no appetite, the stomach may swell. There are also symptoms of indigestion - diarrhea or constipation. The stool is foul-smelling, as if “greasy”, and is difficult to wash off. It may contain patches of undigested food.
Exacerbation of pancreatitis is also accompanied by additional characteristic signs:
- Frequent belching followed by hiccups. The mouth feels dry, difficulty swallowing occurs, and the tongue becomes covered with a whitish coating.
- The body temperature is subfebrile or febrile (especially at night), but the patient is shivering.
- Shortness of breath, decreased or persistent increase in blood pressure.
If treatment is not started immediately after the first symptoms of an exacerbation appear, after 1–2 days the skin turns gray or yellow, and its elasticity decreases. The patient gradually loses weight, he develops signs of dehydration and hypovitaminosis.
Main signs of the disease
Symptoms of a pancreatic attack develop completely suddenly. The main manifestation is severe cutting pain that occurs first on the right side of the chest and gradually spreads to the left half. This is due to irritation of nerve endings, which are located in large numbers in the endocrine gland. As a result of swelling of the organ and impaired outflow, the secretion accumulates in the pancreas, which leads to the digestion of its own tissues, resulting in severe pain. Unpleasant sensations often radiate under the shoulder blade or to the back. These signs can lead to an error in diagnosis, as a result of which it is necessary to carry out a differential diagnosis with myocardial infarction, which has similar manifestations. When the peritoneum is involved in the inflammatory process, new symptoms appear. These include increased pain when stroking the abdomen. Moreover, if you put pressure on it, the condition may improve for a short time.
An important symptom is disruption of the digestive tract. Intense pain is accompanied by bouts of vomiting, which does not provide relief and is debilitating. After some time, bile appears in the vomit, and if the stomach is completely empty, only strong urges and nausea remain.
Stool disorder in the form of diarrhea develops. As a result of accelerated intestinal motility, remains of undigested food are present in the stool. However, after a few days, constipation may develop. Flatulence is observed, which leads to severe bloating. A white coating appears on the tongue.
Additional symptoms include a significant increase in body temperature. The person becomes weak and cannot stand on his feet. Any movement is accompanied by pain, so the patient tries to find a comfortable position that brings at least a little relief.
Other signs of acute pancreatitis include surges in blood pressure, which can either increase or decrease significantly. The pulse becomes weak and rapid. As a result of severe vomiting, hypovolemia develops, the symptoms of which are dry mouth and a change in skin color to an unhealthy grayish tint.
The occurrence of these clinical manifestations indicates a severe impairment of the patient’s health, especially if for several days the person tried to cope with the problem on his own and did not seek medical help.
Causes of exacerbation
The onset or activation of the inflammatory process in the pancreas can occur due to the pathological effects of various factors:
- Abuse of fatty or unhealthy foods, alcohol.
- Diseases or surgical interventions on the gastrointestinal tract, gall bladder.
- ERCP.
- Injuries or wounds of the pancreas, abdomen.
- Infectious diseases or infection with worms.
- Treatment with antibiotics, estrogens.
- Acquired anatomical pathologies of the pancreatic duct or blockage with stones.
- Cardiovascular abnormalities.
- Changes in hormonal levels, including during pregnancy.
- Disturbance of metabolic processes.
- Oncology.
Statistics show that in 30% of all patients with exacerbation of pancreatitis, it is not possible to identify the cause of this condition.
Causes of acute pancreatitis in women
- presence of injuries.
- allergic reactions.
- presence of viral infections.
- stomach ulcers.
- intoxication of the body.
- incorrect structure of the gland.
Chronic
If treatment of the acute form is ignored, the disease quickly becomes chronic. In addition, it should be taken into account that there are many diseases that contribute to the appearance of chronic pancreatitis. These are: cholecystitis, the presence of gallstones, frequent flatulence. The disease begins to manifest itself in the form of frequent intakes or continuous diarrhea.
Sores in the mouth area
The appearance of chronic pancreatitis can be identified independently by the following signs:
- Dryness of the upper layer of the epidermis.
- Hair fragility.
- The appearance of wounds in the corners of the mouth.
- Lack of iron in the body.
- Daily nausea, leading to vomiting.
- Aversion to food and sudden weight loss.
Causes of chronic pancreatitis in women.
- alcohol dependence (small percentage).
- diseases of the biliary tract.
- improper diet associated with strict diets, work associated with harmful working conditions).
https://youtu.be/-tt3a55I0Ig
First aid
Exacerbation of the inflammatory process in the pancreas does not require treatment at home ; the patient must be admitted to the inpatient department of the surgical department of medicine. institutions. In severe cases, the person is sent directly to intensive care.
As soon as the first symptoms appear, you must call an ambulance. However, until medical assistance is provided, the patient’s relatives can try to relieve an attack of pancreatitis on their own at home. The first thing to do is to make sure that the patient does not take any food or even liquid, because this can trigger the production of digestive enzymes and further aggravate the person’s condition.
To relieve pain, stop the inflammatory process and relieve swelling, you can place a cold compress, a heating pad filled with ice water, or, better yet, a plastic bag with ice on the upper abdomen (the area between the navel and the diaphragm).
Next, you need to do everything possible to provide the patient with peace. It is desirable that the person is completely immobilized. This will help reduce tension and saturate blood flow in the affected area.
If possible, it is recommended to give the patient an analgesic or antispasmodic drug available in the home medicine cabinet. This could be No-shpa, Spazmolgon, Maxigan, Drotaverine. Such drugs will help reduce the severity or completely eliminate pain.
But this does not mean that the attack has passed and treatment is no longer required. After all, all these measures are symptomatic first aid provided if clinical manifestations arise suddenly, and not etiotropic therapy, which is needed by a patient with exacerbation of pancreatitis.
Nutritional nature
What can you eat after an attack of pancreatitis? Compliance with a special diet plays an important role in the successful recovery of the patient. This will reduce the load on the pancreas and achieve stabilization of well-being.
After an exacerbation of pancreatitis, you can eat no earlier than 2–3 days later. In this case, you need to start by eating a small amount of food. Food should be ground and not hot. You need to eat often - up to 5-6 times a day.
Treatment with diet involves the use of steamed, baked or boiled dishes. Under no circumstances should you eat fried, smoked or pickled food. Excessive consumption of salt, sugar, pepper and other spicy seasonings should be avoided while cooking. Alcoholic and carbonated drinks, as well as products classified as semi-finished or fast food, are strictly prohibited. They contain a large amount of trans fats, which have a pronounced adverse effect on the functioning of the pancreas.
Red meat, avocados, sugar, white bread, etc. are prohibited.
A diet after an attack of pancreatitis can normalize the functioning of the endocrine organ. The patient can eat the following dishes and foods:
- Low-fat varieties of fish - hake, pike, carp, cod, pike perch, etc. It is advisable to bake the product to preserve all the useful components.
- Dietary meat - rabbit, turkey, veal, chicken breast, etc. It contains a large amount of proteins, amino acids and trace elements necessary for the human body. Meat can be stewed, steamed or added to soups.
- Boiled or stewed vegetables. They are characterized by a rich composition - they contain vitamins, microelements, antioxidants and other components. The ideal option is puree soup, which is extremely easy to digest and does not contain coarse food particles. The diet for pancreatitis excludes the consumption of raw vegetables.
- Cereals. Preference should be given to products containing complex carbohydrates. These include rice, buckwheat, and millet. Oatmeal has a positive effect on the gastric mucosa, the treatment of which is indicated not only for diseases of the gastrointestinal tract, but also pancreas.
- Low-fat lactic acid products - yogurt, cottage cheese, cheese, kefir. Helps restore normal microflora of the gastrointestinal tract. Approved for use no earlier than 2 weeks after an attack.
- Vegetable and butter. Used to add small quantities to prepared dishes.
- Herbal tea has a pronounced positive effect, which will not only help restore water balance and quench thirst, but also saturate the human body with useful substances.
After a pancreatic attack, a special diet should be followed for life. If you violate the doctor's recommendations and consume prohibited foods, exacerbation of pancreatitis is possible. Therefore, you need to lead a healthy lifestyle to prevent relapse.
Pancreatitis is a severe inflammatory disease that affects the pancreas. Its development can occur in both acute and chronic forms, but in both the first and second cases, patients often experience attacks characterized by severe pain. And in this case, it is necessary to clearly know not only the symptoms of a pancreatic attack, but also how to provide first aid to the patient. After all, if a person does not receive the necessary treatment in a timely manner, this can lead to sad and irreversible consequences.
Causes of an attack
A pancreatic attack, as a rule, occurs completely suddenly, and there are several reasons for this:
- errors in nutrition;
- stress;
- drinking alcohol (even in very small quantities);
- smoking;
- inflammation of the gallbladder;
- infectious diseases;
- liver diseases;
- pathologies of the cardiovascular system;
- congenital anomalies in the structure of the pancreas, etc.
And despite the fact that there are many factors that can provoke attacks of pancreatitis, the main cause of their occurrence is poor nutrition. After all, the pancreas is the main organ for the synthesis of digestive enzymes. And if a person regularly eats food that is “heavy” for the gastrointestinal tract, the gland becomes overloaded, its work fails, which entails the occurrence of inflammatory processes in the pancreatic parenchyma.
This, in turn, causes edema, as a result of which the organ increases in size and a narrowing of the lumen of the excretory ducts is noted. Such phenomena provoke stagnation of pancreatic juice inside the gland, since its release into the duodenum cannot occur through narrowed ducts. And it contains digestive enzymes, the work of which is activated immediately after their production. And given the fact that they remain inside the organ, they begin to digest its cells, which provokes a painful attack.
Poor nutrition is the main cause of the development of acute pancreatitis and exacerbation of chronic
Important! It is for this reason that doctors strongly recommend that all their patients (even those who do not suffer from pancreatitis) adhere to proper nutrition. After all, only it will help avoid attacks and maintain pancreatic functionality.
Symptoms of an attack
Before telling how to relieve an attack of pancreatitis, it is necessary to say a few words about what signs characterize the occurrence of this condition. And these include:
- severe pain of a girdling nature, which is initially localized in the left or right hypochondrium, then begins to spread to the sternum, lumbar region, and shoulder blades;
- mechanical jaundice, manifested by yellowness of the sclera;
- yellowing or blanching of the skin;
- temperature increase;
- nausea that develops into vomiting, after which the person does not feel relief;
- weakness;
- dizziness;
- fatty loose stools.
These manifestations of pancreatitis indicate the development of acute inflammation of the pancreas, during which it is under no circumstances possible to stay at home. It is necessary to immediately call a team of doctors, since only timely qualified medical assistance will help to quickly stop an attack and prevent the development of complications against it.
The pain that occurs during a pancreatic attack is very severe and can lead to shock
Possible consequences and complications
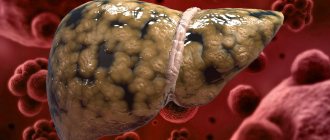
Pancreatitis is a serious disease that affects the cells of the pancreas. When an attack occurs, they die and are no longer restored, which entails disruption of the functioning of not only the gland, but also other organs, since the work of all internal organs and human systems is interconnected.
Inflammation of the pancreas disrupts the functioning of the intestines, liver, gallbladder, kidneys and vascular system. And if pancreatitis affects the exocrine cells of the gland, then this also leads to the development of diabetes mellitus, since the death of these cells disrupts the production of insulin, which is responsible for the breakdown and absorption of glucose in the body.
Moreover, if acute pancreatitis is manifested by an increase in temperature to 38 degrees and above, then this already indicates the development of purulent processes in the pancreas, which can cause sepsis or an abscess.
It should also be noted that due to numerous cell deaths in the pancreas, necrosis begins to develop, leading to complete dysfunction of the organ and severe intoxication of the body. And this can also lead to death.
Therefore, under no circumstances should you joke with pancreatitis. If it has been diagnosed, it must be treated immediately. This will reduce the frequency of attacks and the risks of serious complications arising from them.
Pancreatic necrosis is a common complication of attacks of pancreatitis, the consequences of which are considered irreversible
What to do if an attack occurs?
Every person should know what to do and what to do if a pancreatic attack occurs, since no one is immune from pancreatitis. It can manifest itself completely suddenly and at any time of the day.
If a person has the first symptoms of an attack (vomiting, pain in the upper abdomen, etc.), you should immediately call a team of doctors. Remember that you should not attempt to relieve a pain attack on your own, as this will only worsen the patient’s condition. But first aid should still be provided before the doctor arrives. And it is as follows:
- prohibit the person from taking enzyme preparations (in this case they will increase the pain syndrome);
- give the patient an intramuscular injection of No-shpa or Papaverine (they will relieve spasms in the ducts of the gland and improve the patency of pancreatic juice, thereby reducing the manifestations of pain);
- apply a cold compress to the pancreatic area for 10-15 minutes (this will also help alleviate the patient’s condition);
- in case of severe vomiting and diarrhea, it is necessary to give the person ¼ cup of water to drink every 10-15 minutes (such measures will help prevent dehydration);
- sit the person on a chair or armchair, raising his legs to his stomach and tilting his torso slightly forward (this position will improve the outflow of bile and pancreatic juice).
There is no need to do anything else! Further relief of the attack will be carried out in a hospital setting with the help of special medications.
If a pancreatic attack occurs, you should immediately call an ambulance. Any delay in this case can lead to dire consequences.
Important! Remember that an attack of pancreatitis occurs due to acute inflammation and swelling of the pancreas, which causes pancreatic juice to stagnate in it. And during this period, you should under no circumstances take medications in the form of tablets, especially those containing enzymes. The tablets penetrate the stomach, thereby giving the pancreas a command to activate the synthesis of digestive enzymes, which only increases the amount of pancreatic juice and accelerates the processes of self-digestion.
Treatment of a pancreatic attack
Treatment of an attack of pancreatitis is carried out only in a hospital setting. It involves the use of special medications that are administered intravenously or intramuscularly.
As a rule, therapeutic therapy includes the use of the following medications:
- antispasmodics (Dratoverine, Papaverine, etc.);
- non-steroidal anti-inflammatory drugs (Ibuprofen, Aspirin);
- painkillers (Analgin, Ketarol);
- antienzyme drugs (Nizatidine, Famotidine).
In the event that a person experiences necrotic or purulent processes in the pancreatic parenchyma, aseptic and antibacterial drugs are used that help prevent the occurrence of complications against them. In more severe situations, surgical intervention is performed.
In addition to drug therapy, treating an attack of pancreatitis also involves following a fasting diet. It helps reduce the production of digestive enzymes, which helps reduce pain and relieve stress on the gland. A starvation diet is prescribed for 2-3 days until the attack is completely stopped. During this period, only drinking in small quantities and at regular intervals is allowed.
As soon as the patient's condition stabilizes, treatment tactics change. He is prescribed treatment table No. 5 and medications that help improve digestive functions, that is, enzyme preparations (Pancreatin, Creon, Mezim, etc.).
Enzyme preparations
Since such medications contain enzymes that are activated immediately after entering the stomach, the risk of a recurrent attack increases several times. Therefore, they must be taken correctly - during or immediately after meals. Remember, you cannot take enzyme preparations even 5-10 minutes before meals, it is dangerous!
In addition to these medications, the patient must also take antispasmodics for some time (about 2-3 weeks). They prevent the occurrence of spasms in the ducts of the gland and improve the outflow of pancreatic juice. Only now they are not administered intramuscularly, but taken orally.
As for food, during this period you can eat:
- liquid mashed potatoes prepared with water and without oil;
- crackers;
- skim cheese.
Compote, jelly and weak unsweetened tea are allowed to drink. This diet will need to be followed for at least 5 days. Then, if the patient’s condition remains stable, the diet is expanded and, in addition to the products described above, includes:
- boiled or steamed meat or fish dishes made from lean meats and fish;
- secondary meat and fish broths;
- vegetable soups;
- porridge with water;
- low-fat dairy and fermented milk products;
- biscuits.
How exactly the patient follows the diet after pain relief depends on his condition in the future. If the rules of therapeutic nutrition are violated, a second attack may occur.
If the patient’s condition remains stable within 2-3 days after introducing these products into the diet, he is discharged. But at home he must also follow this diet for several more weeks.
As soon as the patient’s condition completely returns to normal, the use of antispasmodics and treatment table No. 5 are canceled. But you will now have to constantly take enzyme preparations and adhere to certain dietary restrictions. Patients with pancreatitis are strictly prohibited from eating:
- fried and fatty foods;
- salo;
- smoked meats;
- mushrooms;
- confectionery;
- ice cream;
- pickles;
- hot spices and sauces;
- fast food;
- sausages;
- baked goods;
- carbonated and alcoholic drinks.
Even if a person has a stable phase of remission, it is still necessary to follow a diet. Because during the attack, some of the pancreatic cells died and stopped functioning. And any error in nutrition can overload the organ and provoke a repeat attack. Therefore, after being discharged from the hospital, a person must be aware that his well-being and state of health now depend only on him. Proper nutrition, regular use of medications, giving up bad habits, strict adherence to all doctor’s recommendations - this is the key to successful and “shared” living with pancreatitis!
Inflammation of the pancreas is, as a rule, a chronic disease that has a recurrent course. Currently, pancreatitis is considered to be a multifactorial disease: many factors lead to its development, including bad habits, alcoholism, poor diet, etc. One way or another, once it occurs, pancreatitis will not be completely cured. The overwhelming percentage of patients who have had inflammation of the pancreas experience an exacerbation of the disease in the future.
A new acute condition occurs due to errors in diet or poor lifestyle. It is not difficult to suspect another attack; it is enough to know the main symptoms and promptly contact your doctor for help.
Diet after an attack
Upon leaving the medical facility, you must adhere to a special diet. Meals should be as frequent as possible. It is optimal to eat 6–8 times a day, consuming small portions. Food should be liquid or pureed, steamed or boiled.
It is recommended to eat the following dishes:
- Boiled beef, steamed cutlets, pollock, flounder or cod.
- A small amount of dairy products (low fat).
- Porridge with water or mashed potatoes.
- Fresh vegetables and fruits, puree soup from them.
- Drinks include rosehip or blackcurrant decoction.
Eliminate fried, smoked, fatty, canned, salted and peppered, pickled, and flour foods from your diet. Don't indulge in sweet foods. You should only eat homemade, freshly prepared food and avoid visiting fast foods. You can learn more about special nutrition by asking about the 5P diet.
Types of pancreatitis
Depending on the characteristics of the inflammatory process, this disease is divided into several types. Treatment is prescribed taking into account the form of the disease and other factors. Experts distinguish 3 main types of pancreatitis:
- Acute is a dangerous type of pathology that can lead to death in the absence of the necessary treatment.
- Chronic pancreatitis accompanies the patient throughout his life. It is characterized by alternating remissions with exacerbations.
- Reactive is a mildly expressed type of disease. This form of pancreatitis can develop into a more serious one if the patient refuses to be monitored by a doctor.
- How to play Battleship: rules
- How to freeze chanterelles for the winter
- Which is the best printer-scanner-copier for the home?
Drug therapy
Due to the fact that the patient is experiencing severe pain, doctors prescribe painkillers.
An acute attack of pancreatitis can be treated with a blockade. For example:
- Sacrospinal novocaine blockade.
- Intravenous administration of Baralgin.
In order to quickly improve microcirculation, it is necessary to administer a Reopolyuglykin solution IV. If the patient is allergic to the drug, then Hemodez IV drops are prescribed.
Treatment must be comprehensive, so it is necessary to correct electrolyte deficiency. For this purpose droppers are used.
Solutions:
- Sodium chlorine.
- Potassium chlorine.
Additional therapy includes medications that will help reduce the production of pancreatic enzymes. Most often, doctors prescribe statins, inhibitors or proteases. The most famous and effective drugs that help cure the disease are Somatostatin, Gordox.
Also read: Chronic parenchymal pancreatitis
In rare cases, doctors prescribe a course of antisecretory drugs. They may prescribe one of the drugs: Omeprazole or Kvamatel.
Important! The drugs described above cannot be used independently in the treatment of acute disease. Each medicine has its own list of side effects and contraindications, so only a doctor prescribes treatment.
Forced diuresis will help remove excess enzymes.
After drug therapy, which usually consists of medicinal solutions for IV administration, doctors prescribe diuretics. In most cases, one drug is used - Lasix. If the patient is intolerant to the composition, then analogues are prescribed, but this happens extremely rarely.
Every doctor is afraid of complications after therapy. In order to prevent purulent complications of pancreatitis, doctors must prescribe a course of broad-spectrum antibiotics.
Prescribed:
- Imipenem.
- Metronidazole.
Surgery
When is surgical treatment performed? This question worries almost every patient with this disease. Of course, if drug therapy does not bring a positive result, then doctors have no choice but to perform surgery. Surgical treatment is prescribed only to those patients in whom the acute course of the disease has progressed to the purulent stage.
Surgery on the affected organ is performed under general anesthesia. First, anesthesia is administered with intubation of the lungs, after which areas of necrosis are removed. To make it clear what necrosis is - this is dead tissue, which is what doctors remove from the affected pancreas.
Possible consequences and complications
Pancreatitis is a serious disease that affects the cells of the pancreas. When an attack occurs, they die and are no longer restored, which entails disruption of the functioning of not only the gland, but also other organs, since the work of all internal organs and human systems is interconnected.
Inflammation of the pancreas disrupts the functioning of the intestines, liver, gallbladder, kidneys and vascular system. And if pancreatitis affects the exocrine cells of the gland, then this also leads to the development of diabetes mellitus, since the death of these cells disrupts the production of insulin, which is responsible for the breakdown and absorption of glucose in the body.
Moreover, if acute pancreatitis is manifested by an increase in temperature to 38 degrees and above, then this already indicates the development of purulent processes in the pancreas, which can cause sepsis or an abscess.
It should also be noted that due to numerous cell deaths in the pancreas, necrosis begins to develop, leading to complete dysfunction of the organ and severe intoxication of the body. And this can also lead to death.
Therefore, under no circumstances should you joke with pancreatitis. If it has been diagnosed, it must be treated immediately. This will reduce the frequency of attacks and the risks of serious complications arising from them.
Pancreatic necrosis is a common complication of attacks of pancreatitis, the consequences of which are considered irreversible