Esophageal candidiasis is a fungal disease that affects the food tract. It is worth noting that thrush of this nature is not an independent disease. This type of disease always accompanies general candidiasis, but the esophagus can be affected through the oral cavity or intestines.
The appearance of esophageal candidiasis, like any type of thrush, is caused by the opportunistic fungus Candida. This fungus is called conditionally pathogenic due to the fact that it is present in the orgasm of almost any person, but is in the so-called sleep mode, without causing any inconvenience. However, as soon as the human immune system shows weakness, the fungus wakes up and begins to actively reproduce, which causes the appearance of thrush. It should be noted that esophageal candidiasis is usually a consequence of the visceral course of ordinary thrush. Candidiasis is the most common infectious disease affecting the esophagus. Treatment of esophageal candidiasis must be timely, since any fungal disease has a high tendency to progress quickly.
Classification of esophageal candidiasis
The disease goes through several stages of development:
- Catarrhal esophagitis is a pathology of 1st degree (initial). Light whitish spots appear on the mucous membrane of the esophagus, similar to an accumulation of spider threads. These spots cover no more than 50% of the walls of the upper tract of the digestive system. There is no penetration of microorganisms into the deep layers of the esophageal walls yet. There is no redness or swelling of the tissues, but contact bleeding is already possible.
- Fibrinous esophagitis – 2nd degree. The esophageal walls are covered with a grayish-white convex plaque, which is quite large (up to 5 mm) round spots. Plaque covers more than 50% of the mucous membranes. Contact bleeding is pronounced, the esophageal walls turn red and become swollen.
- Fibrinous-erosive esophagitis – grade 3. The infection penetrates into the inner layers of the esophageal wall. Fungal spots merge, forming folded structures that narrow the lumen of the esophagus. Superficial tissues turn red, swell, and become covered with ulcers.
- Erosive esophagitis – 4th degree. The mucous membranes become loose and covered with numerous ulcers. Continuous plaque has the appearance of a fringe, stretching along the ridge-like surface inside the esophagus. The fringe does not blow away when exposed to air currents. Beneath it is an eroded surface. The eroded areas have different shapes and reach 4 mm in diameter. Contact bleeding is intense, and there is severe swelling of the mucous membranes.
Clinical picture
Symptoms of mycosis depend on the stage of development of the disease.
How and how to treat armpit fungus
- Catarrhal mycosis - the mucous membrane of the esophageal tube has some swelling, hyperemia, individual white “islands” of pseudomycelium of the fungus are observed.
- Fibrinous esophagitis - characterized by pain, increased tendency to bleeding of the affected areas.
- Fibrinous-erosive esophagitis is accompanied by total contamination of the esophageal tube, the surface of which resembles a fringe with separate long ribbons of films.
For mycosis, the development of the disease is more typical of the fibrous type, when the walls are covered with a white or yellowish loose coating. Underneath it is determined a hyperemic, very sensitive mucous membrane.
The resulting ulcerative lesions of the mucous membrane due to a fungal infection indicate the presence of additional pathology in the digestive tract. For independent mycosis, the formation of ulcers is not typical.
For the patient, esophageal candidiasis develops in most cases asymptomatically. Only a quarter of patients experience significant symptoms. More intense damage is accompanied by the following complaints:
- Dysphagia – difficulty moving food or drink;
- Constant heartburn;
- Sore throat;
- Odynophagia – pain when swallowing in the sternum;
- Vomiting with films (pseudomycelium);
- Decreased appetite;
- Weight loss;
- Diarrhea.
If the development of the disease reaches the stage of erosive damage to the walls of the esophagus by the fungus, then patients may experience blood in the vomit, bleeding, complete failure of food to pass through, tissue necrosis, and perforation. Often, in patients with weakened immunity, candidal stomatitis and thrush on the mucous membranes of the genital organs are diagnosed.
Causes of esophageal candidiasis
Penetration of infection into the body occurs when:
- consumption of contaminated products;
- contact with an infected person;
- using contaminated hygiene equipment and household items.
The outcome of the human body’s contact with infection depends on the state of the immune system. The situation can develop in three directions:
- the person who catches the infection does not get sick;
- acquires the status of a carrier of infection;
- gets sick.
In most cases, infected people are classified as carriers of the fungus.
The following factors contribute to the occurrence of the disease:
- a large amount of infection that has entered the body;
- weak level of the body's defenses (immunity);
- violation of the integrity of the mucous membranes of the digestive tract;
- changes in the activity of digestive enzymes produced in the stomach;
- weakening of leukocyte function;
- the presence of diverticulosis, polyposis, burns of the mucous membranes.
The causes of esophageal candidiasis in people with weakened immune systems cannot always be determined. The risk group includes:
- children;
- old people;
- people with allergies and autoimmune pathologies;
- pregnant women;
- cancer patients;
- people on low-protein diets to lose weight;
- patients with tuberculosis and other chronic infectious diseases that debilitate the body;
- patients with adrenal insufficiency;
- people with immunodeficiency.
Esophageal candidiasis is a thrush that is localized not on the mucous membrane of the genitourinary system, but on the walls of the intestinal tract. The pathogenic fungus enters the human body in the following ways:
- Improper food processing.
- Sharing household items with an infected person.
- Unprotected sexual intercourse with a carrier of the fungus.
- In the presence of candida in the body, the fungus begins to develop rapidly due to weak immunity from past viral and infectious diseases.
- Injuries to the walls and mucous membrane of the esophagus.
Candidal esophagitis occurs with diabetes mellitus, insufficient protein content in the body, or low stomach acidity. The disease can occur in women during pregnancy, with allergic reactions of the body to certain foods, or due to decreased activity of the adrenal glands.
The risk group includes heavy smokers and people who abuse alcoholic beverages.
Types of candidiasis and severity of symptoms
Esophageal candidiasis, depending on the stage of development of the pathogenic fungus, has two stages:
- acute candidal esophagitis. Symptoms develop quickly, the patient experiences fever, diarrhea, and vomiting. As a rule, the acute form of the disease is characterized by infection of the lower esophagus;
- chronic stage - occurs in the absence of timely treatment of acute candidiasis. Symptoms are mild. Chronic intestinal candidiasis, as an independent disease, is a rare case.
Depending on the location of the candida fungus, candidal esophagitis has three stages of development:
- the first stage - the fungus forms a whitish coating on the epithelial ball of the walls of the esophagus;
- second stage - the film grows, touching the mucous membrane and submucosal tissue of the esophagus;
- development of pseudomembrane-type deposits, with the penetration of candida into the muscular musculature of the esophagus.
At the third stage of the disease, the patient may experience internal bleeding of the esophagus, narrowing of the walls of the digestive tract, development of ulcers, necrosis of the soft tissues of the intestine.
How esophageal candidiasis will proceed depends on the spread of infection throughout the mucous membrane, the area of the affected surface, and the penetration of Candida deep into the epidermis and other tissues. The combination of these factors determines the severity of the disease.
| Degrees of candidiasis | Localization and manifestations of infection |
| 1st degree | The fungus invades the surface epithelial cells, forming sparse whitish cobwebs, spots and islands scattered throughout the esophageal mucosa |
| 2nd degree | Pathogenic forms of Candida (elongated cells, pseudomycelium) grow deep into the mucous membrane, one after another capturing its layers Extensive, overgrown films and a coating of fungus appear on the inner surface |
| 3rd degree | The fungus invades vessels and tissues located outside the esophagus The process is accompanied by the appearance of necrotic ulcers (areas of dead tissue), complicated by the addition of a bacterial infection (phlegmon), bleeding from blood vessels and ruptures of the damaged mucosa In the lumen of the organ, in addition to the fused plaque and islands of fungus protruding above the surface, numerous films (pseudomembranes) are formed, blocking the lumen of the esophagus and making swallowing difficult. |
Phlegmon
Clinical picture
Symptoms of mycosis depend on the stage of development of the disease.
- Catarrhal mycosis - the mucous membrane of the esophageal tube has some swelling, hyperemia, individual white “islands” of pseudomycelium of the fungus are observed.
- Fibrinous esophagitis - characterized by pain, increased tendency to bleeding of the affected areas.
- Fibrinous-erosive esophagitis is accompanied by total contamination of the esophageal tube, the surface of which resembles a fringe with separate long ribbons of films.
For mycosis, the development of the disease is more typical of the fibrous type, when the walls are covered with a white or yellowish loose coating. Underneath it is determined a hyperemic, very sensitive mucous membrane.
The resulting ulcerative lesions of the mucous membrane due to a fungal infection indicate the presence of additional pathology in the digestive tract. For independent mycosis, the formation of ulcers is not typical.
For the patient, esophageal candidiasis develops in most cases asymptomatically. Only a quarter of patients experience significant symptoms. More intense damage is accompanied by the following complaints:
- dysphagia – difficulty moving food or drink;
- constant heartburn;
- sore throat;
- odynophagia – pain when swallowing in the sternum;
- vomiting with films (pseudomycelium);
- loss of appetite;
- weight loss;
- diarrhea.
https://youtu.be/bZe8GNtPp5U
Complications
In the human body, fungi first adhere to the walls of the esophagus, penetrate epithelial tissue, and enter the bloodstream through capillaries. The infection travels through the blood through the body, capturing new structures in the human body.
At the first stage, the infection captures only the superficial layer of mucous membranes. Esophageal candidiasis of the 2nd degree is characterized by the introduction of fungal microorganisms into the internal layers of the walls of the organ. With an advanced disease, the fungal fringe can grow so that the lumen of the esophagus becomes blocked.
The above complications pose a danger to human life. Disastrous consequences can be avoided by starting therapy in a timely manner.
There are several degrees of esophageal candidiasis:
- Stage I infection means that the fungus has not yet penetrated deeply, and there is plaque only in certain areas of the esophagus.
- In stage II of the disease, the fungus penetrates the mucous membrane, and plaque spots begin to merge into large areas.
- Grade III characterizes the penetration of the fungus into the muscles, the development of a bacterial infection and tissue necrosis is possible.
If treatment is not done in a timely manner, complications such as:
- ulcer;
- bleeding;
- phlegmon (purulent inflammation);
- stricture (reduction of the lumen of the esophagus);
- rupture of the esophageal tube;
- tissue death;
- death.
Therefore, it is very important to start therapy in a timely manner and not only act on the pathogen, but also eliminate concomitant diseases.
How to identify pathology
It is quite difficult to determine esophagitis only from complaints and during examination of the patient. All of these symptoms may indicate a disease whose causes are associated with bacteria and viruses. Therefore, additional diagnostic methods are prescribed to confirm the diagnosis.
The most revealing is endoscopic examination of the esophagus. As a result, severe inflammation of the organ walls is revealed. Often the mucous membrane is covered with a fibrin film.
Blood and urine tests will be required. To exclude bacterial flora, a mucosal smear is prescribed. Only after this candidiasis esophagitis is treated.
Diagnostic methods
Complete cure of candidiasis is possible with grade 1 in 65–70% of cases. In grades 2 and 3, the outcome depends on the severity of the concomitant disease, the state of the body’s immune defense, the correct treatment regimen and the sensitivity of the fungus to the prescribed drugs.
To treat the disease, a complex is prescribed, consisting of a combination of different antifungal agents (triazoles, polyene antibiotics, imidazoles) in the form of tablets and solutions for administration (intravenously, intramuscularly).
The duration of treatment, combination and dosage of medications depend on the severity of the disease. Usually the doctor selects them individually.
| Group of drugs | Name and form of the drug |
| Imidazole derivatives | Ketoconazole (Oronazole) tablets |
| Clotrimazole (Imidil, Candide) in the form of liquid and spray for irrigation | |
| Miconazole (Dactocin, Dactanol) injections | |
| Triazole derivatives | Fluconazole (Forcan, Diflucan, Fucis) in tablets or liquid for injection |
| Itraconazole tablets and oral solution | |
| Polyene antibiotics | Amphotericin B (Ambisome, Fungizone, Amphocil) in solution for intravenous drip administration |
| Nystatin (Fungicidin, Mycostatin) | |
| Kandina | Caspofungin in solution for intravenous administration |
The difficulty of treatment lies in the rapid decrease in the sensitivity of the fungus to certain medications. Because of this, it is recommended to increase the drug dose, change the form of the drug (from tablets to injections) and switch to another medication in the series.
During treatment of the disease and during the recovery period, patients are advised to adhere to a strict diet.
During the acute (difficulty swallowing and pain) and recovery period, meals (and drinks) should be:
- warm (not higher than 40°C);
- soft (boiled porridge, pureed vegetables, meat, slimy soups, purees);
- gentle (not irritating the mucous membranes, without pepper, vinegar, or any seasonings).
| The diet for esophageal candidiasis should include | Completely excluded from the diet |
| Lean meat (veal, rabbit, chicken) and fish | Jam, honey, sugar syrups, sugar and sugar substitutes |
| By-products (liver) | Confectionery, baked goods, white bread |
| Cabbage, carrots, wheat sprouts, cucumbers, asparagus, spinach, green salad | Candy and chocolate |
| Green apples, plums | Fresh milk |
| Walnuts | Potatoes, starch, sugar beets, rice |
| Beans, beans, lentils, chickpeas | Kvass, alcohol and beer, carbonated drinks, nectars and juices with fruit pulp |
| Millet, oatmeal, buckwheat, brown rice | Sweet fruits |
| Homemade fermented milk products with beneficial lactobacilli | Chips, nuts, semi-finished products, smoked meats, canned food |
| Eggs | |
| Butter and vegetable oil | |
| Seasonings: ground cinnamon, cloves, bay leaf | |
| Onions and garlic (as prebiotics, during the recovery period) |
Coffee can be replaced with a weak chicory drink, black tea with green tea, or a decoction of rosehip or chamomile without sugar.
Click on photo to enlarge
Treatment of candidal esophagitis should be timely, as soon as the first signs of illness are detected. The primary diagnosis is made based on the clinical picture and patient complaints. To confirm the diagnosis, an endoscopic examination of the esophageal mucosa is performed. Depending on the condition of the esophagus, candidiasis is divided into three groups:
- catarrhal endophagitis - the mucous membrane of the esophagus is swollen, diffuse hyperemia is observed. When you press on the mucous membrane, it begins to bleed, and a whitish coating forms at the site of the wounds. There is no erosion;
- fibrinous esophagitis - plaque and round plaques are present on the walls of the esophagus. Contact with the mucous membrane causes damage;
- erosive esophalitis - plaque on the walls of the esophagus looks like fringed ribbons, the color is gray. Erosion is present. When pressure is applied to the mucous membrane, it is damaged and bleeds.
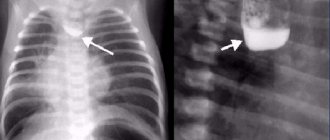
In case of candidiasis of the third stage of development, the patient must undergo an x-ray with the introduction of a contrast agent. An additional diagnostic method that allows you to quickly identify a pathogenic fungus is the introduction of an instrument through the nasal sinus, with which a mucus sample is taken for laboratory analysis. A mucus analysis will show the fungus' resistance to antibiotics.
Treatment
Treatment for fungal disease of the esophagus includes:
- taking antifungal drugs based on triazole, imidazole;
- polyene antibiotics - Nystatin, Natamycin;
- a gentle diet;
- the use of enterosorbents to remove fungal waste products;
- stimulating the body's defenses with the help of immunomodulatory drugs.
Effective antifungal agents:
- Ketoconazole is applicable in high doses; side effects are possible when interacting with other drugs. Toxic to the liver.
- Fluconazole is used for various forms of mycosis, is compatible with many medications, and is well absorbed.
- Itraconazole – used for renal failure,
- Amphotericin B is prescribed when other drugs are ineffective. Side effects are reversible, that is, they disappear when the drug is discontinued.
- Capsofungin is the newest generation of antifungal drugs. Changes the synthesis of microorganism cells, causing its death.
In complicated cases, medications are used in the form of injections, high-intensity laser radiation, and endoscopic injection of granulocyte concentrate are used.
Prevention
To prevent esophageal candidiasis, you must:
- Maintain oral hygiene by brushing your teeth twice a day;
- do not get carried away with eating sweets;
- undergo regular preventive examinations with a dentist;
- during antibiotic treatment, take antifungal drugs in prophylactic doses and probiotics to restore the microflora of the digestive tract;
- strengthen the immune system.
To reduce the risk of developing candidiasis, it is important to follow some preventive measures:
- do not cause any diseases or infections;
- use personal hygiene products (especially a toothbrush!);
- use individual dishes;
- exclude contact with patients with candidiasis;
- strengthen the immune system.
Candidiasis of the esophagus is not a rare disease, but does not have pronounced symptoms (at the initial stage). When symptoms appear, it is important to start diagnosis in a timely manner. Delayed treatment can lead to unnecessary complications. It is also important to always remember basic preventive measures - they can save you from many problems.
People's Pharmacy
Do not forget that folk remedies should not replace medicinal medications. For candidiasis of the esophageal tube, they are used for symptomatic therapy, as well as to strengthen the immune system.
Auxiliary treatment with various herbal infusions and decoctions has a positive effect on recovery.
- decoction of calendula , chamomile , oak bark - helps fight inflammation, relieves pain when swallowing. One tbsp. dry raw materials need to be poured with 200 ml of boiling water and boiled in a water bath for 20 minutes;
- Kombucha infusion - take half a glass 4 times a day.
Therapy
It is necessary to treat candidiasis of the gastrointestinal tract comprehensively. Diet and taking antifungal drugs can quickly cure the disease. With a weakened immune system, the patient is prescribed immunostimulants. Candida fungus can migrate to neighboring internal organs of the gastrointestinal tract, so not only the affected area is treated, but the entire digestive system. Otherwise, the disease may recur.
The main drugs for the treatment of esophageal candidiasis are Clotrimazole, Fluconazole, Ketoconazole. The dosage and course of administration are selected by the attending physician, depending on the stage of the disease, the severity of the clinical picture and the individual characteristics of the body.
For the treatment of severe stage esophagitis with pronounced symptoms, drugs are prescribed that help remove toxic products from the body - Atoxil, activated carbon, Polysorb, Antralen. In particularly severe cases, medications are administered intravenously. Additional methods of treating esophageal candidiasis are endoscopic injection of high-concentration granulocytes and laser irradiation with high-intensity pulses.
Forecast
The prognosis is determined by the degree of development of the disease. It is easiest to treat esophageal candidiasis at the initial stage, before the infection has penetrated deep into the epidermal tissue. In this case, therapy does not take more than 2 months, and 70% of patients achieve complete cure.
Once the disease has developed, it is more difficult to treat. In cancer patients, HIV-infected people and other people with immunodeficiency, the disease in most cases is not completely cured, since recovery is hampered by the underlying pathology.
In 35% of patients with immunodeficiency, advanced disease leads to generalization of the infectious process and death.
The prognosis for the disease depends entirely on the severity of the disease. In grade 1, until the fungus has slightly invaded the mucous membrane of the organ and has not penetrated into the deep layers of the epidermis, treatment may take from 3 weeks to 2 months. Complete cure occurs in 65–70% of cases.
The second and third degrees of esophageal candidiasis are much more difficult and longer to treat. Typically, such forms of fungal infection develop against the background of serious immune disorders (HIV, oncology). To eliminate them, it is necessary to get rid of the underlying disease, and this is not always possible.
As a result, in 34–36% of patients, a fungal infection of the esophagus is complicated to a systemic, generalized process with a fatal outcome.
Diet
During treatment, the patient must adhere to a strict diet. Marinades and pickles, seasonings and spices are excluded from the diet - products that strongly irritate the mucous membrane of the esophagus. It is not recommended to eat fatty meats and fish, flour products and sweets. Dishes must be steamed or baked.
It is strictly forbidden to drink alcoholic beverages, carbonated water, or coffee. Limit tea. Daily meals should include garlic, cabbage and rice. Allowed drinks are green tea, rosehip, kefir. Garlic should be consumed daily, a few cloves at a time. Decoctions based on medicinal herbs replace tea and other drinks. They should be consumed every day, hot or cold.
The disease cannot be cured with diet alone, so changing the diet must be accompanied by taking medications.