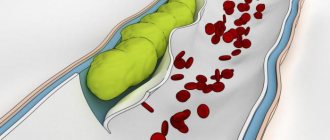
Ulcerative lesions occur in every part of the large intestine and have different origins and pathogenetic mechanisms of formation. An ulcer in the large intestine represents a violation of the integrity of the epithelial cover and is common in both sexes. Ulcerative lesions occur single and multiple.
No specific symptoms of peptic ulcer in the large intestine have been identified to date. Clinical symptoms of ulcerative lesions of the large intestine coincide with a number of other diseases.
Symptoms
The listed diseases have specific symptoms from the affected intestines and the body as a whole. They reach their greatest severity during periods of exacerbation, which disrupts a person’s quality of life. Duodenal ulcer, nonspecific ulcerative colitis and Crohn's disease are characterized by a chronic course with relapses as a result of exposure to provoking factors.
Intestinal manifestations
Characteristic signs of exacerbation of the disease:
- periodic or constant acute pain in the epigastric region of the abdomen;
- nausea, often leading to vomiting;
- increased pain on an empty stomach, at night;
- frequent belching with a rotten smell;
- flatulence;
- loss of appetite.
The intensity of pain depends on the duration of the process, the number of ulcers and the person’s pain threshold. The nature of nutrition also plays a certain role.
Crohn's disease is a systemic pathology in which segmental damage most often occurs to the small intestine with the formation of erosions, ulcers of various sizes and stenoses.
Symptoms of the disease:
- cutting or aching pain in the abdominal area that does not have a clear localization;
- flatulence after eating;
- loose stools up to 4-10 times a day;
- the appearance of blood impurities in the stool.
The severity of the described signs depends on the degree of activity of the inflammatory process in the gastrointestinal tract. The most severe disease occurs with combined damage to the stomach, small and large intestine.
With nonspecific ulcerative colitis, chronic inflammation of the intestine is determined, in which ulcers, microabscesses and polypous growths appear over time. Local signs of colitis:
- stool with pathological impurities (blood, mucus and sometimes pus);
- diarrhea up to 5-12 times a day;
- cutting pain in the lower abdomen;
- constant flatulence.
We recommend reading:
H2-histamine blocking drugs and their use in gastroenterology
Usually the disease is severe with a clear clinical picture. UC is more common in men aged 20 to 60 years.
Extraintestinal manifestations
In addition to local intestinal symptoms, ulcers may be accompanied by pathological changes in the skin, eyes, and joints.
A duodenal ulcer is characterized by:
- “jams” in the corners of the mouth, or angular stomatitis;
- desquamative glossitis (deep folds on the tongue, its redness);
- increased fragility of hair and nails.
In UC or Crohn's disease, extraintestinal symptoms are systemic and more severe:
- increased body temperature, chills;
- general weakness, poor appetite;
- progressive weight loss;
- inflammation of the membranes of the eye (conjunctivitis, uveitis, iridocyclitis);
- muscle and joint pain;
- skin rashes of various types (ring-shaped erythema, etc.);
- damage to small vessels (vasculitis).
Symptoms
The signs of an intestinal ulcer at an early stage will be almost identical to how the inflammatory process occurs in this organ.
Symptoms of a small intestinal ulcer are as follows:
- a pain syndrome of a pulling, cramping nature, which often radiates to the retrosternal region, to the spine;
- heartburn, which intensifies after eating, while diet does not play a special role;
- repeated vomiting, which intensifies after eating and does not always bring relief;
- stool becomes black, which will indicate rectal or internal bleeding (a solitary rectal ulcer may be suspected);
- diarrhea, in especially severe cases, pus will be present in the stool;
- loss of appetite;
- weight loss;
- pale skin, increased sweating at night;
- increased body temperature;
- weakness;
- symptoms of anemia.
With an exacerbation of the pathological process, the clinical picture will be characterized as follows:
- high body temperature – up to 39 degrees;
- increased flatulence;
- cramping abdominal pain;
- diarrhea up to 10-15 times a day, mixed with blood and mucus.
Such clinical signs require immediate medical attention, since in its advanced form, an intestinal ulcer leads to perforation of the intestinal walls and even death.
Causes and risk factors
Intestinal ulcer is considered a multifactorial disease, the occurrence of which may involve an infectious process, genetic predisposition or autoimmune inflammation.
Main causes of diseases:
- Infections. Active helicobacteriosis in the gastrointestinal tract, severe intestinal infections.
- Autoimmune process. This theory centers on the fact that the human body produces antibodies against the normal cells of its own intestines.
- Chronic inflammation. The predominance of pro-inflammatory factors (interleukins, tumor necrosis factor) in the human body can trigger ulcer formation processes.
- Genetic predisposition. People whose relatives suffer from intestinal ulcers are much more likely to get sick than people with no family history.
- Medicines. Long-term use of certain medications (corticoid hormones, aminoglycosides, NSAIDs) can lead to similar changes in the intestines.
Sometimes not one, but a whole combination of factors is involved in the development of pathology.
Amoebiasis
This disease is also infectious in nature. It is more relevant for countries with a tropical climate, and can be brought to the European continent by numerous tourists. The causative agent of amebiasis is a specific protozoan – Entamoeba histolytica, which persists for a long time in soil, water and some products. Symptoms of intestinal ulcers in amebiasis and shigellosis are largely similar. Amebiasis can be distinguished (a specialist can do this) by the following signs:
- the disease begins gradually, sometimes a person is a carrier of amoebiasis for many months and even years, releases the pathogen, infects others, but does not notice any symptoms of the disease;
- symptoms of general intoxication increase slowly, the condition resembles the course of a malignant neoplasm;
- abdominal pain is localized in its left half;
- feces of normal volume, but liquid consistency, mixed with blood (the so-called “raspberry jelly”).
The final diagnosis of amebiasis is confirmed by microbiological examination and sigmoidoscopy. In this disease, the rectal ulcer is located on a practically unchanged mucosa. The main direction of treatment is antibiotics (Metronidazole), which affect all types of pathogens. If the treatment of amebiasis is not effective and intensive enough, then the formation of secondary lesions in the tissues of the brain and liver is possible.
Diagnostics
Diagnosis of pathology can be carried out by a therapist, gastroenterologist or surgeon.
Data collection and inspection
In the first stages, it is important to interview the patient, during which the doctor finds out the complaints, their nature, duration and frequency. It is mandatory to establish the onset of the disease, find out the hereditary history, and the plan for previous treatment.
A detailed examination will help the doctor detect inflammatory lesions of the eyes, skin or tongue, and joint contractures as a result of long-term arthritis. Palpation of the abdomen is carried out to determine the area of pain, pathological changes in the shape and size of the intestine, and bloating.
Instrumental studies
Invasive techniques allow a more detailed and “personal” examination of the intestinal mucosa, detect the nature and number of defects on it, perform a biopsy and even minor operations if necessary.
We recommend reading:
Gastroenteritis: how is the pathology manifested and treated?
To establish a diagnosis, the following types of instrumental diagnostics are prescribed:
- Fibrogastroduodenoscopy (with/without urease test). This is an examination of the upper segment of the gastrointestinal tract using an endoscope (from the esophagus to the duodenum). It is the “gold” standard for diagnosing peptic ulcer disease.
- Fibercolonoscopy. The rectum and colon are examined; It is possible to perform a biopsy and minor surgical interventions (stop bleeding, remove polyps).
- Contrast irrigography. X-ray examination of the intestine using a contrast agent and taking a series of images.
In addition to a visual assessment of the condition of the intestinal mucosa, a biopsy is required, followed by a histological examination of the collected material. This helps not only confirm the diagnosis, but also exclude oncology.
Laboratory research
Laboratory tests include clinical and biochemical blood tests (decrease in hemoglobin and albumin levels, appearance of C-reactive protein and fibrinogen). In some cases, they resort to immunological analysis, which detects the presence and amount of plasma antibodies.
A coprocytogram and bacteriological examination of stool can show the presence of undigested particles, leukocytes and a high concentration of pathogenic microbes. Equally important is a stool test for occult blood.
Ulcerative colitis
Ulcerative colitis is very similar in etiology to peptic ulcer disease, but most often it is impossible to establish the primary cause of erosions in the large intestine. Most doctors are inclined to think that this disease is entirely associated with hereditary predisposition. The symptoms of ulcerative colitis are similar to peptic ulcers. The only exception is that colitis develops over a long period, without a sharp exacerbation. In this case, not only the colon, but also other parts of the digestive tract can be affected. Treatment is predominantly symptomatic combined with diet. In critical cases, surgery is performed.
In summary, a colon ulcer is a dangerous disease that occurs at an initial stage without noticeable symptoms. The patient complains only of gastrointestinal upset and infrequent constipation, exacerbation of hemorrhoids (if there is a tendency to it). The symptoms of the ulcer are similar to colitis. When these diseases are identified, drug therapy and strict adherence to a strict diet are prescribed. If an aggravation is allowed, then surgery will definitely be required. The worst scenario is the transformation of an ulcerative lesion into a malignant tumor (and it develops very quickly, since atrophy of part of the intestine will occur).
Treatment
The treatment is complex. Therapy should include dietary advice, medications and, if necessary, surgery.
Diet
It is important to maintain a balanced diet both during and outside of exacerbations. You should avoid overeating, eating dry or on the go, excessive consumption of carbonated drinks, and fast food. Food should be prepared using gentle methods (baking, boiling) and served at the optimal temperature (20-40 °C).
| Recommended Products | Not Recommended Products |
|
|
The presence of frequent diarrhea implies an increase in daily calorie intake and the amount of fluid consumed. This will avoid dehydration and sudden weight loss.
Drugs
Medications that can be used include:
- Antibiotics. Designed to fight infection (penicillins, cephalosporins, fluoroquinolones).
- Antisecretory, antacid drugs. Reduce acidity, protect the walls of the gastrointestinal tract (omeprazole, rabeprazole, Maalox, Almagel).
- Corticosteroids. They have anti-inflammatory activity and inhibit autoimmune processes (Prednisolone, Budesonide).
- Aminosalicylates/cytostatics. Prevents the progression of autoimmune inflammation in the intestines (Sulfasalazine/Methotrexate).
We recommend reading:
Antisecretory agents: list and types of drugs, application features
In addition, symptomatic therapy is prescribed: painkillers, vitamins.
Surgery
Surgical interventions are indicated in case of steady progression of the disease, development of complications, and ineffectiveness of drug therapy. Statistics indicate a high relapse rate (up to 45%) 3-5-7 years after the intervention. Surgeries for duodenal ulcers are most effective.
Types of operations
- Necrectomy. Excision of ulcerative defects.
- Vessel ligation. Used to stop bleeding.
- Bowel resection with/without anastomosis. Removal of the most altered segment of the intestine with or without the formation of an anastomosis with another part of the gastrointestinal tract.
Recovery period
In most cases, the recovery period takes from 2-4 weeks to several months, which depends on the degree of intestinal damage and the timeliness of therapy. In some cases, remission is achieved for years or the disease leads to disability.
Folk remedies
There are many different folk remedies that have proven themselves in the treatment of intestinal ulcers. So, you can be treated:
- Propolis. To prepare the tincture, 200 g of this product is crushed and poured with 100 ml of alcohol with a strength of 70%. It is infused at room temperature for three days, and during this time the bottle is shaken occasionally. Take 20 drops 2-3 times with warm water an hour before meals.
- Butter with propolis. Place 1 kg of butter in an enamel saucepan, bring it to a boil, remove from heat. Add 150 g of propolis, cut into small pieces and stir until it dissolves. Take a course of 21-30 days, 1 tsp. an hour and a half before meals.
- Aloe with honey and red wine. Pass enough aloe leaves through a meat grinder to make half a glass. Add honey (¾ cup) to them and place in a dark place for three days. Pour natural red wine (1 glass) into the mixture and leave in the dark for another day. Use 1 tbsp three times a day. l. tinctures before meals for one or two months.
- Raw egg. Mix one egg white with olive oil (1 tbsp) and powdered sugar (1 tsp). Consume 1 tbsp for 10 days. l. this mixture on an empty stomach in the morning.
- Kalinov infusion. Take 2 tbsp. l. berries and grind them in a mortar. Slowly pour a glass of boiling water, let it brew for four hours and strain. Drink ¾ glass daily.
Possible consequences and prognosis for life
Late diagnosed pathology can lead to the development of complications:
- total damage to the gastrointestinal tract;
- perforation of the intestinal wall;
- internal bleeding;
- malignancy;
- sepsis;
- abscess formation.
With a mild or moderate course, the prognosis for life is relatively favorable (provided that all treatment recommendations are followed). Severe and complicated forms in 40-70% of cases lead to disability and, less often, death.
Prevention
Primary prevention:
- rational, balanced nutrition;
- taking medications strictly as prescribed by the doctor;
- timely treatment of acute infections, autoimmune processes.
Secondary prevention:
- adherence to a therapeutic diet and recommended regimen;
- exclusion of alcohol, smoking;
- therapeutic and prophylactic administration of drugs;
- regular examination, even during remission.
In continuation of the topic, be sure to read:
- Intestinal erosion: causes, symptoms and treatment methods
- Duodenal erosion: symptoms, treatment and prognosis for life
- Gastroduodenitis: how is the pathology manifested and treated?
- Stomach ulcer: how is the pathology manifested and treated?
- Duodenal ulcer: how is the pathology manifested and treated?
- Erosive gastroduodenitis: symptoms and methods of treating pathology
- Gastric and duodenal ulcers: signs and treatment methods
- More about Helicobacter pylori: diagnosis and treatment of the pathogen
- Antiulcer drugs for the stomach and duodenum
- Bismuth preparations: list of medications and their use for the stomach