All articles by the author
Author of the article: Ekaterina Sergeevna Churaeva
Practicing obstetrician-gynecologist, ultrasound diagnostics doctor
Oligohydramnios during pregnancy occurs on average in up to 5 cases per 100 women for reasons related to the health of the expectant mother and developmental defects of the child. A moderate form of reduction in the amount of amniotic fluid does not pose a serious threat to the pregnant woman and the fetus.
When the amount of amniotic fluid decreases to critical levels, it is necessary to take therapeutic measures to prevent miscarriage or premature birth, which is dangerous due to severe oligohydramnios.
What is oligohydramnios during pregnancy: risks
The volume of amniotic fluid is 300-500 ml; if it is less, then oligohydramnios is diagnosed. A pathology that can lead to serious consequences for both the baby and the mother, which is why it is so important to know its signs and consider them in time. Timely medical intervention will avoid developmental problems and abnormalities. Statistics show that most often the diagnosis is made at the 37th week of pregnancy, and the reason for this is the aging of the placenta, a decrease in its activity.
1st trimester
If oligohydramnios is diagnosed from the very beginning of pregnancy, then it is not dangerous, because it does not affect the fetus. There is still time to get everything back to normal before the baby grows up. It can be diagnosed at 16 weeks during a routine ultrasound. The cause may be the incompetence of the membranes, which I do not perform the functions assigned to them.
2nd trimester
Oligohydramnios becomes a dangerous diagnosis from the 26th week, because if the condition worsens, the doctor will not carry out delivery. At this stage, the cause may be leakage of amniotic fluid, which can lead to premature birth, and at such a stage the baby may not survive. Such an unfavorable diagnosis can lead to:
- Complications in the development of the unborn child - malnutrition, hemiccephaly, amniotic bands, limb deformities.
- To premature birth or termination of pregnancy.
- To a difficult, long birth.
3rd trimester
The diagnosis at the end of pregnancy is dangerous, but the timing allows for delivery. If your water levels have been normal throughout your pregnancy, and in recent months a problem has been discovered, then you should prepare for a long labor process. With oligohydramnios, the bladder becomes flat and cannot act as a wedge when stimulating cervical dilatation. Doctors are trying to prescribe a caesarean section.
Why does oligohydramnios occur?
The amount of water inside the placenta changes depending on the needs of the baby and the length of pregnancy; it is clear that at 20 weeks the volume of water is less than at 37 weeks. By the 38th week of a normal pregnancy, the fluid volume is 1500 ml, and at 39 and 40 weeks it begins to gradually decrease.
Most often, signs of oligohydramnios are detected in the second trimester (by about 20 weeks), but if oligohydramnios is detected at 30–32 weeks, this can lead to serious problems.
If at 30–32 weeks the amniotic fluid is less than 1000 ml, then we are talking about oligohydramnios. Depending on the amount of fluid deficiency in the placenta, severe or moderate oligohydramnios during pregnancy is diagnosed. Ultrasound is most often used for diagnosis.
Sometimes moderate oligohydramnios during pregnancy is the result of poor nutrition. In such a situation, a pregnant woman does not require treatment; it is enough to establish a routine and diet. Typically, doctors prescribe a gentle regimen in such a situation, which includes eating a variety of foods rich in vitamins and minerals. In parallel with the diet, it is important to be periodically examined by a doctor.
If the ultrasound showed severe oligohydramnios, then serious measures will be required, including drug treatment. In such a situation, the woman will be kept in a day hospital. The more severe the oligohydramnios, the more serious the consequences for the baby. Severe oligohydramnios threatens the development of the following pathologies:
- deformations of the child’s skeletal system,
- asphyxia, which can lead to disruption of the nervous system and negatively affect brain activity,
- abnormal development of the limbs in the fetus.
A pregnant woman should know that a decrease in the volume of amniotic fluid in the later stages (37, 38, 39 weeks) is not considered pathological. This is a natural process of preparation for childbirth, which in most cases occurs at 39 or 40 weeks.
What types of low water are there: pronounced, moderate and relative?
Oligohydramnios occurs in several types. The diagnosis, consequences, symptoms are radically different:
- Moderate oligohydramnios is diagnosed with minor deviations from the norm. It is often detected early, so it can be eliminated quickly. Various diets are prescribed and nutrition is adjusted. With the right lifestyle, it is possible to bring the level of amniotic fluid to normal. The moderate form has no obvious symptoms, the woman feels normal. Only an ultrasound will allow us to come to such a diagnosis. But even with moderation, healthy babies are born, you just have to follow the doctors’ recommendations. Statistics show that such a diagnosis occurs in only 5 percent of pregnant women by the end of their term.
- With severe oligohydramnios, significant deviations from the norm can be observed. To avoid possible consequences, hospitalization and constant medical supervision are required. When expressed in form, the following features are characteristic:
- Painful sensations during active movements of the fetus;
- Aching pain in the lower abdomen;
- Reduction in the size of the uterus, and with it the abdominal circumference;
- Deterioration in health.
Only with this type of oligohydramnios is a long labor possible and an increased risk of bleeding after childbirth. To avoid complications during childbirth, doctors try to perform a caesarean section.
- Relative oligohydramnios occurs in the last months of pregnancy and is most often associated with aging of the placenta. If such a diagnosis is made, you should not be upset, because proper treatment will determine the causes and return everything to normal. The main thing is that the development of the fetus is not impaired with such a diagnosis. It’s just that a pregnant woman will be under stricter control from doctors.
Symptoms of oligohydramnios
The most dangerous thing about this condition is that there are no obvious signs of oligohydramnios. Physically, the woman feels great and her health does not deviate from the norm. Only sometimes, when the fetus moves, a woman may feel pain in the lower abdomen, but this is an unreliable symptom.
Only a specialist can accurately determine whether a pregnant woman has oligohydramnios. So, an experienced doctor can diagnose pathology in the case of:
- lag in size or discrepancy in the height of the uterine fundus,
- its serious discrepancy with the timing of pregnancy,
- insufficient abdominal size for this period.
If such symptoms are detected, the doctor may come to the conclusion that the pregnant woman has oligohydramnios. Every doctor knows the consequences of oligohydramnios if left untreated. The risk of giving birth to a baby with developmental pathologies is very high, especially with severe oligohydramnios.
In order to refute or, conversely, confirm this diagnosis, it is necessary to conduct an ultrasound, on the basis of which a diagnosis can be made. An ultrasound examination will allow you to accurately determine the amount of fluid inside the placenta, and when confirming the diagnosis, the doctor will use ultrasound to assess the severity and condition of the fetus. If you suspect the presence of oligohydramnios, a pregnant woman should undergo an examination by a gynecologist.
Oligohydramnios can be diagnosed at 20, 30 and 37 weeks. Although oligohydramnios in the classical sense can be diagnosed only at 39 or 40 weeks, if the fluid volume has decreased to 500 ml or less.
However, the classical definition is outdated; in modern medicine, we can talk about oligohydramnios starting from the 20th week. The closer the due date (37, 38, 39 weeks), the more the placenta ages and the more often oligohydramnios is detected.
How is it diagnosed?
The doctor makes a diagnosis after performing certain procedures. First, the volume of the abdomen and the height of the uterine fundus are measured; if there are obvious deviations from the norm, the specialist sends for an ultrasound. The examination will determine the amount of amniotic fluid and diagnose fetal development according to the gestational age.
Attention is paid to the amniotic fluid index. If it is 5-8, then all indicators are within normal limits. If 2-5 – moderate oligohydramnios; less than 2 - pronounced oligohydramnios. To determine the condition of the fetus, Doppler sonography is often prescribed, which shows the level of oxygen and nutrient supply. Cardiac monitoring may also be prescribed.
Examinations and tests for oligohydramnios
Before starting treatment, the doctor needs to determine what led to the pathology and conduct a diagnosis. First of all, it is important to clarify the reason that resulted from insufficiency of amniotic fluid and the severity of oligohydramnios. In this case, you need to undergo a series of tests and studies:
- Ultrasound examination and Dopplerography, as a result of which you can:
- determine the amount of water in the fertilized egg;
- determine the degree of developmental delay of the child;
- assess the quality of blood flow in the uterine arteries of a pregnant woman, as well as in the umbilical cord and cerebral artery of the fetus.
- general urine test, general blood test, smear for possible infections and other sexually transmitted diseases. These tests will exclude the possibility of infection of the fetus, as a result of which oligohydramnios develops;
- CTG to determine the well-being and condition of the fetus.
In addition, it is extremely important to conduct an oral interview with the pregnant woman. The more honest her answers are, the faster the cause of oligohydramnios will be found out. It is important to clarify whether she abused any products, drank alcohol, or whether the pregnant woman smokes. The sooner the cause of oligohydramnios is determined, the sooner treatment can begin, which means saving the child.
If oligohydramnios is diagnosed at an early stage, the pregnant woman will need to undergo additional examinations throughout the entire gestation period to identify the amniotic fluid index (AFI). For each week, starting from 16, it is necessary to determine the AFI. The frequency of determination is 20, 30, 32, 34, 35, 36, 37, 38, 39 and 40 weeks of pregnancy (provided that birth by cesarean section does not occur at 37 weeks).
Is it possible to determine on your own?
It is impossible to determine oligohydramnios on your own; the diagnosis can only be made by a specialist after additional research.
A woman can feel the first ailments and share them with a doctor, who, after certain tests, will make his assumptions. Self-medication in this case can only do harm, which is why consultation with a specialist is so important. As a rule, with a severe form of oligohydramnios, some symptoms appear, but with minor deviations, only a gynecologist can suspect something is wrong.
Causes
The causes of oligohydramnios during pregnancy can be divided into several groups:
- chronic diseases of a pregnant woman that provoke a decrease in the amount of amniotic fluid (severe arterial hypertension, heart failure with edema, vascular pathology of the extremities, systemic lesions, rheumatoid arthritis, thyroid disease, obesity, diabetes, alcoholism);
- acute painful conditions of the expectant mother (intoxication with diarrhea and vomiting, poisoning with alcohol, nicotine, toxic products);
- late-term toxicosis (gestosis) is often the cause of oligohydramnios during pregnancy in the 3rd trimester;
- pathology of the placenta, which is associated with developmental defects, circulatory disorders, necrotic lesions, sclerosis, traumatic injuries from the outside;
- rupture of the membranes and leakage of amniotic fluid due to injury, physical stress, infection;
- pregnancy post-term for more than 41 weeks;
- multiple pregnancy;
- Rh conflict when the Rh blood type of mother and baby does not match;
- uncontrolled use of painkillers by the expectant mother (Indomethacin, Diclofenac);
- infections of a pregnant woman that are transmitted to the fetus and affect its membranes (chlamydia, ureaplasma, herpes viruses, cytomegalovirus);
- congenital genetic defects of the fetus associated with the kidneys, urethra, ureter;
- acquired defects due to the impact of adverse factors (toxic, infectious) on the developing organs of the baby.
Risks of oligohydramnios for a child
Possible risks:
- The fetus becomes vulnerable under the influence of external factors. There is a high probability of compression of internal organs, development of clubfoot and curvature of the spine.
- Physical activity is disrupted, because movements are constrained, the baby cannot rotate in the womb like others.
- If there is not enough water, the metabolic process between mother and child may be disrupted, which can lead to developmental delays and sometimes even a frozen pregnancy. In this case, it is necessary to act quickly, conduct an ultrasound and verify the condition of the fetus, and promptly remove it in order to save the woman.
- Lack of oxygen during the baby's development affects the development of the nervous system.
- Children are born underweight and with certain developmental disabilities.
- The likelihood of umbilical cord compression increases.
- The skin also suffers and gradually dries out, and malnutrition may develop.
- Frequent contact of the fetus with the membrane can lead to fusion in it.
Treatment of oligohydramnios
Treatment methods for this disease may vary. It all depends on the severity of oligohydramnios, the reasons for its occurrence and the timing of pregnancy. For example, in case of metabolic disorders and obesity at 30 or 32 weeks, a woman is prescribed medications that normalize the activity of the placenta.
The doctor will also create a special diet. If the pregnancy is 33 or 34 weeks or more, then complex treatment is prescribed, which includes taking drugs that improve metabolism in the placenta, vitamins, and medications for the main cause of the disease.
Treatment can take place in two options: outpatient – for moderate degrees of oligohydramnios, or in a hospital – if the degree of oligohydramnios is severe. Outpatient treatment consists of:
- restriction of physical activity,
- maintaining a gentle regime,
- excluding heavy physical activity,
- taking medications prescribed by the doctor,
- periodic visits to the antenatal clinic.
Typically, outpatient treatment is prescribed if a woman is in the second trimester of pregnancy. A woman is admitted to hospital if:
- if oligohydramnios is severe;
- if the amount of amniotic fluid is slightly below normal, but uterine tone is detected;
- oligohydramnios at 34–35 weeks of pregnancy and later.
If oligohydramnios is diagnosed, the doctor may prescribe a weekly ultrasound, starting at 34 or 35 weeks, fetal CTG and Doppler ultrasound. Such measures are extremely important in order to control the pathology. Then, if something goes wrong, you can take the necessary measures in time.
If oligohydramnios is severe and the severity of the pathology threatens the health of the child, then the doctor is obliged to take action and perform a caesarean section. In this case, early birth is possible only if the pregnancy is 33 weeks or more.
However, whenever possible, doctors try to do everything to maintain the pregnancy until at least 35 weeks, since the fetus is considered fully mature only at the end of the 36th week. But this does not mean that you need to refuse surgery at 34 or 35 weeks, since with oligohydramnios the fetus can be seriously damaged.
How to treat with medication?
Treatment is aimed at restoring blood flow in the uterus and placenta. It is important to identify the cause that caused the problem and eliminate it. During the treatment, measures are taken to normalize the flow of oxygen from the mother to the fetus through the placenta. There is no such treatment, because it is impossible to artificially increase the amount of water. The goal is to improve the condition of the mother, and with it the baby.
Treatment is selected taking into account the duration. If the problem is detected in the third trimester, the woman is hospitalized, where she receives vitamins, as well as medications that help restore oxygen levels and improve blood circulation.
They are trying to normalize blood sugar levels and eliminate possible infections that could provoke pathology. A CTG is performed every day, which allows us to determine the condition of the fetus. An ultrasound or Doppler test is prescribed once every five days. Doctors are trying to prolong the pregnancy and reach a natural birth. If the baby’s health worsens, a caesarean section is performed.
If the problem is identified at week 28 and serious deviations in the process of fetal formation are established, then some experts suggest interrupting it, because the outcome is difficult to predict. For moderate oligohydramnios, treatment is carried out at home, but it is important to adhere to the recommendations - take medications, eliminate exercise and spend more time in the fresh air, increasing the number of walks.
Doctors are trying to identify and treat the disease that caused oligohydramnios. Having determined the cause, it is always easier to eliminate the consequences. Thus, oligohydramnios can be caused by a metabolic disorder in a pregnant woman, then a diet is prescribed that will bring all indicators back to normal.
Causes of oligohydramnios
If a doctor diagnoses oligohydramnios during pregnancy, the causes of this condition may be different. Experts to this day cannot come to a common opinion on why oligohydramnios occurs. From a long list of reasons, scientists have pinpointed the following:
- Reduced function of the secretion of the membrane that forms the fertilized egg, insufficient or improper development of the epithelium covering this membrane. If a pregnant woman does not know the dangers of oligohydramnios during pregnancy, then this is even better. What causes the most difficulty for doctors is not diagnosis, but “false symptoms” that arise as a result of stimulation of a woman’s nervous system.
- Abnormal fetal development. Other types of abnormal development include hereditary anomalies in the development of the face and kidneys. This can be clarified between 20 and 30 weeks, when the second mandatory ultrasound examination has already been carried out.
- High blood pressure in a pregnant woman. Naturally, throughout the entire period of pregnancy, blood pressure will be elevated, but its fluctuations will be insignificant. If the blood pressure surges too high, it can cause oligohydramnios. In the case of hypertension, fetal development may be delayed, its growth may slow down, or fetal death may occur. This happens especially often after 20 weeks.
- Another cause of oligohydramnios is all kinds of bacterial infections that were suffered by a pregnant woman and were not properly treated. Sometimes the danger is hidden in infections that a woman had long before pregnancy. In such a situation, pathogenic microflora is detected using tests both in the birth canal and in the amniotic fluid. The manifestation of such a danger can be detected at 20 weeks of pregnancy, when, under the influence of hormones, the infection begins to progress, in parallel with this, oligohydramnios develops. At 30 weeks, oligohydramnios becomes more pronounced.
- Oligohydramnios is often observed in cases of multiple pregnancies. The cause of this disease in such a situation may be the uneven distribution of blood flow in the placenta. In this case, one child receives more oxygen and nutrients than the other. Such a situation can lead to the death of a weaker embryo, so inpatient monitoring is necessary.
- Another reason for oligohydramnios is postmaturity. At 36 or 37 weeks, the baby is already fully formed and can appear at any time. Sometimes women carry a baby for over 40 weeks, but it is important to know that starting from 38 weeks, oligohydramnios can develop. The reason for this is the “expiration date” of the placenta, which has already served its allotted time and is beginning to age. Sometimes obvious aging of the placenta is observed as early as 37 weeks. As a result, it peels off and is unable to perform its functions. Under such circumstances, doctors raise the question of a caesarean section or inducing labor by piercing the placenta. Don't be alarmed if doctors suggest surgery at 37 or 38 weeks. By this period, the child is already completely ready to be born.
- Oligohydramnios can develop gradually, starting from the first week of pregnancy, and can be detected at 12 weeks or after 20 weeks during an ultrasound scan. It may be caused by obesity in a pregnant woman as a result of serious metabolic disorders. In such a situation, it is important to know how pronounced it is and how seriously it affects the development of the fetus. If oligohydramnios has not yet become pronounced and critical, then the child can be saved. To do this, the pregnant woman is placed in a hospital, where she will be under the supervision of doctors throughout the entire gestation period. With such a pathology, you need to introduce a strict diet and find out the causes of obesity. Even in the best case scenario, the baby will be born no later than 37 or, at most, 38 weeks. This is due to the death of the placenta. In this case, a caesarean section is mandatory.
Prevention
The earlier oligohydramnios is detected, the greater the chance of restoring the amount of water and returning to normal levels.
Prevention allows you to prevent a problem. A pregnant woman is advised to avoid stressful situations and increase the number of walks in the fresh air. The diet should include not only vitamins and minerals, but also plenty of fluids. Not only water, but also milk, compotes, juices.
To prevent oligohydramnios even before pregnancy, it is worth undergoing certain tests that will allow you to identify deviations and eliminate them in a timely manner. Solve problems of the cardiovascular and urinary systems, if any. To refuse from bad habits.
Low water is not the final verdict. You need to believe in yourself and be positive about childbirth. It is important to listen to the recommendations of doctors and everything will be fine. Even with such a diagnosis, healthy children are born, it’s just that the development process requires more careful monitoring.
Diagnosis of oligohydramnios
During an ultrasound examination, the doctor makes some measurements and calculations to determine the amount of amniotic fluid, after which he makes a conclusion about oligohydramnios, a normal amount of water, or polyhydramnios.
A gynecologist can also assume low or high hydramnios at the next measurement of the abdominal circumference and the height of the uterine fundus, but a more accurate diagnosis can only be made with the help of an ultrasound.
At home, you can only conduct a test for leakage of amniotic fluid. If watery discharge is often observed in the underwear, and the baby’s kicks have become painful for the pregnant woman, although such discomfort was not felt before, or the size of the abdomen is too small, although the pregnancy has already exceeded 20 weeks, then it is advisable to conduct a special test. Perhaps the reason for everything is oligohydramnios, caused by leakage of water due to a violation of the integrity of the membranes.
The test can be carried out at home by observing the discharge for some time, or by purchasing a special test for leakage of amniotic fluid at the pharmacy and using it.
The “free” test is carried out as follows: empty your bladder, take a shower (without douching and possible water getting inside the vagina), wipe yourself dry with a towel and lie down on a dry diaper. Lie motionless for 15 minutes, and then get up and see if a wet spot appears on the diaper. Normal discharge is not capable of forming and flowing out so quickly; most likely, it is amniotic fluid leaking. You can find out more accurately by contacting the LCD with a complaint about unusual discharge. There they will conduct a special test and say it is water or normal vaginal discharge.
The pharmacy test looks like a pad, the surface of which will change color to blue or green if amniotic fluid leaks.
Coloring also occurs with bacterial/viral discharge, so if you notice blue-green spots on the surface of the pad, contact your gynecologist.
Any test for leakage of amniotic fluid is recommended to be carried out 12 hours after the last sexual intercourse, douching or use of vaginal suppositories.
How to prevent a decrease or increase in the volume of amniotic fluid?
By following a few simple rules, you can prevent the occurrence and worsening of oligohydramnios and polyhydramnios:
- prepare for pregnancy (future parents undergo examinations, normalize their condition and improve their health);
- regularly consult with a doctor and carry out the necessary diagnostic procedures;
- walk at least 4000 steps a day;
- avoid excessive physical activity and heavy lifting;
- stop drinking alcohol, smoking and other bad habits;
- maintain a balanced diet;
- do not be exposed to stress and excessive fatigue.
Loading...
Share with friends!
Treatment of oligohydramnios
Expectant mothers should not panic when they hear or read about oligohydramnios in their medical records, because modern medicine has many methods for getting rid of this condition. First of all, the woman and baby need timely diagnosis, constant monitoring and adequately selected treatment.
The doctor determines the treatment tactics after receiving the results of the study and determining the causes of the development of oligohydramnios:
- post-term pregnancy requires amniotomy and stimulation of labor;
- oligohydramnios, which appears due to leakage of amniotic fluid (amnionic hydrorrhea), requires treatment in a hospital with mandatory bed rest, constant monitoring of the condition of the fetus and the use of vitamins and medications that reduce the tone of the uterus and prevent infection of the membranes;
- infection with the virus requires home treatment with the use of antiviral restorative medications, drugs that improve blood circulation;
- anomaly in the development of fetal membranes suggests the need for therapy to maintain pregnancy and prevent possible infection of the fetus.
Drug therapy
Treatment of oligohydramnios during pregnancy is carried out using various combinations of the same drugs, depending on the identified cause of oligohydramnios. The most commonly used drugs are:
- vitamin complexes, in which water-soluble vitamins B and C predominate;
- angioprotector "Trental", which enhances blood microcirculation and increases its rheological properties;
- antihypoxant "Actovegin" in the form of tablets, ointments or solutions in ampoules, which improves cellular nutrition and accelerates regeneration and metabolism;
- antiplatelet and immunomodulator “Curantil” (tablets), which supports the functionality and youth of the placenta by improving blood circulation in small vessels (we recommend reading: how to drink Curantil during pregnancy?).
Folk remedies
The effectiveness in solving the problem of reducing amniotic fluid was shown by the folk methods used by our ancestors:
- A decoction of 1 teaspoon of young birch buds and leaves has a diuretic effect. It should be taken three times a day.
- Juice from chokeberry berries or 50 grams of the berries themselves before meals. Helps lower blood pressure and replenish vitamin C deficiency.
- Infusion of lingonberry leaves - 1 tablespoon is added to a glass of boiling water and infused for 30 minutes. It is necessary to take ¼ cup before meals to have an anti-inflammatory and diuretic effect.
- Infusion of valerian or motherwort to relieve stress, excess nervousness and normalize sleep.
- A decoction of a mixture of crushed strawberry leaves, yarrow, birch buds, bean leaves and peppermint, rose hips, nettle leaves and string. All ingredients are mixed in equal proportions and poured with a liter of boiling water. This decoction is taken half a glass 3 times a day to relieve the inflammatory process.
The expectant mother needs to remember that before trying this or that ancient method on herself, she needs to consult with the supervising doctor and get his approval. A herbal remedy can weaken or, conversely, enhance the effect of a particular drug.
Does a pregnant woman’s lifestyle affect the volume of water?
Many women ask questions: why does pathology occur and what determines the appearance of oligohydramnios, what consequences does it have? Experts do not give any special recommendations regarding the prevention of such a problem as oligohydramnios, but note that women who lead a healthy lifestyle and do not have a tendency to smoke or drink alcohol are less susceptible to a decrease or increase in the amniotic fluid index.
Having one sexual partner, as well as using the correct methods of contraception and planning your pregnancy in advance, you can get rid of the factors that provoke oligohydramnios or polyhydramnios, and the manifestation of unpleasant symptoms. It is especially important to adjust the lifestyle of a pregnant woman before childbirth if moderate polyhydramnios is observed.
In which trimester is it most often diagnosed?
Based on the time of occurrence, oligohydramnios is divided into 2 types.
- Early oligohydramnios is observed according to the results of ultrasound examination after the 16th week of pregnancy. The condition is unfavorable for the development and growth of the child, so the cause should be identified as soon as possible and treatment should begin.
- Late oligohydramnios is considered after the 26th week of pregnancy (at the end of the second trimester) and most often depends on functional problems in the pregnant woman’s body.
Oligohydramnios during pregnancy in the third trimester should be closely monitored and corrected. At this time there is a risk of premature birth.
A moderate decrease in amniotic fluid is characteristic of the prenatal period, the so-called oligohydramnios at 40 weeks, which is the norm. This is one of the reasons for the negative impact of postterm pregnancy (over 41-42 weeks) on the child’s body.
Signs
The severity of clinical manifestations of oligohydramnios directly depends on the degree of reduction in the volume of amniotic fluid. Moderate oligohydroamnion is said to occur in cases where the amount of amniotic fluid is reduced slightly, by no more than 400–700 ml. This pathology occurs without any objective symptoms and is diagnosed only by ultrasound.
The diagnosis of “severe polyhydramnios” is made to patients in cases where the deficit in amniotic fluid volume exceeds 700 ml. This condition is always accompanied by the appearance of clinical signs, which include:
- dry mucous membranes;
- dizziness;
- nausea, vomiting;
- reduction in abdominal circumference;
- painful fetal movements.
Oligohydramnios in pregnant women - what is it?
Throughout its development, the unborn child is surrounded by membranes and the placenta. These organs are formed and perform their work exclusively during gestation, which is why they are called pregnancy organs.
Their main function is to create and maintain optimal conditions for the development and formation of the unborn child, and amniotic fluid plays a significant role in this process.
The aqueous membrane, also called the amnion, is a sac that contains the fetus, which is surrounded by amniotic fluid. It adjoins the internal cavity of the uterus and passes to the umbilical cord, and its walls are responsible for the production of amniotic fluid.
By the end of pregnancy, their number can reach from 800 to 1500 ml. This liquid contains hormones, proteins, salts and carbohydrates, without which it is impossible to ensure the full metabolism of the fetus . By the second half of pregnancy it becomes a little cloudy.
The amount of amniotic fluid gradually increases. It expands the walls of the uterus, providing more space for the actively growing fetus. Amniotic fluid is of great importance for the unborn child, creating a unique habitat.
They provide him with the opportunity to move, allow him to develop normally, and protect him from external influences and compression by internal organs. In addition, a water-filled amniotic sac is of great importance in the speed and degree of dilatation of the cervix at the initial stage of labor.
There are different degrees of deviation of fluid volume from normal. In medical practice, moderate (it occurs much more often) and severe degrees are distinguished, and in the second case the decrease can reach 3 times.
Oligohydramnios during pregnancy, the causes and consequences of which can be different, is rare: less than 6% of cases. Moreover, moderate oligohydramnios is much more common - a condition that is not considered critical. With rare exceptions, in the first and third trimesters, moderate oligohydramnios does not in any way threaten the unborn child.
What is amniotic fluid and how does it work:
Varieties
Medicine has several different classifications of oligohydramnios. Depending on the root cause of development, this deviation is divided into two main types:
- Primary. Such oligohydramnios occurs against the background of intact membranes.
- Secondary. It develops as a result of rupture of the amniotic membranes, leading to leakage of amniotic fluid.
Article on the topic: Hypertensive heart disease - provoking factors, manifestations and treatment regimen
According to the nature of the course, oligohydramnios is divided into acute and chronic. In the first case, the cause is infectious diseases suffered by the mother. Oligohydramnios here is often functional. Chronic oligohydramnios accompanies a woman throughout almost the entire pregnancy and requires closer study. Depending on the gestational age, oligohydramnios occurs:
- Early. Diagnosed at 14-20 weeks of pregnancy. More often associated with insufficient functions of the amniotic membranes.
- Late. Occurs at 21-40 weeks of pregnancy due to damage to the membranes.
Development mechanism
Maintaining a certain volume of amniotic fluid (amniotic fluid) is a dynamic process that includes:
- Synthesis of amniotic fluid by special glandular cells.
- Reabsorption (resorption) of amniotic fluid.
The mechanism of development (pathogenesis) of oligohydramnios is a decrease in the production of amniotic fluid or excessive resorption. A change in the activity of the processes of maintaining the level of amniotic fluid in most cases occurs with the development of pathological processes in the body of the fetus or pregnant woman.
What are the consequences for the child?
What threatens a child with oligohydramnios becomes clear by studying the functions of amniotic fluid. Amniotic fluid is needed for:
- fetal nutrition;
- maintaining constant temperature and pressure;
- protection from mechanical and noise environmental influences;
- protection against infectious agents;
- ensuring free smooth movement and lubrication of the skin.
With oligohydramnios, viruses, bacteria and toxins pass through the placental barrier more easily, which can lead to infectious diseases and poisoning of the fetus. If there is a lack of nutrition due to a small amount of water, the growth and development of the baby may be delayed. Signs of hypoxia appear.
Injuries, skeletal distortions, skin damage, and fusion with the amniotic membranes occur due to the fact that the baby does not have enough fluid to move freely in the uterus. The severity of the disorders depends on what pathology contributed to the oligohydramnios.
Severe developmental defects lead to miscarriages. Pathological changes acquired in late gestation can cause premature birth or intrauterine fetal death.
A pregnant woman should know that all the causes and consequences of oligohydramnios, with the exception of severe malformations, can be corrected with well-chosen treatment.
Clinical picture at different stages
The clinical picture does not have any specific symptoms:
- bothered by painful sensations in the abdomen when the fetus moves;
- decreased activity of the child.
During examination, the discrepancy between the timing of pregnancy and the size of the uterus is determined, since when the amount of fluid in the fetal sac decreases, the volume of the uterus also decreases. But it is impossible to make a reliable diagnosis only on the basis of objective status:
- there is always a possibility of incorrect calculation of the gestational age,
- Similar symptoms are observed in a number of other diseases.
A completely different picture is observed if leakage of amniotic fluid occurs outside the onset of labor. This indicates a defect in the lining of the bubble. In this case, there is a high probability of bacterial infection penetrating through the damaged membrane of the fetal sac. To prevent infection of the fetus, it is necessary to study the microflora of the vagina and the composition of the amniotic fluid.
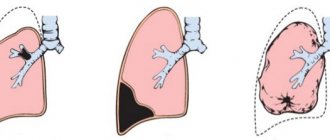
Leakage can initiate premature labor. Medical tactics in such cases depend on the duration of pregnancy. If this happens before 34 weeks, when the lungs are not formed, medication is taken to speed up the process of their development.
Functions of amniotic fluid
Amniotic fluid performs various functions:
- favorable habitat and fetal formation;
- protect from traumatic environmental influences;
- prevent fusion of the fetal skin with the amniotic sac;
- promote full motor activity of the fetus;
- protect the placenta and umbilical cord from damage;
- help the fetus take the correct intrauterine position;
- mediate timely dilatation of the cervix during labor.
What is the danger of a lack of amniotic fluid?
Any person in their right mind will ask the question: are these waters so important and is their quantity critical? Is it possible to rely on chance and let the body bring everything back to normal?
In general, it all depends on the specific situation. Depending on the stage of pregnancy, as well as the severity of the suspected oligohydramnios, the actions of the mother and medical staff vary significantly.
Let's look at the problem.
1. In the first trimester, the lack of amniotic fluid is not given much importance. This means you don’t need to panic either. Now I will explain why.
In the first weeks of fetal development, oligohydramnios is not dangerous to the baby's health. The cause of the deviation can be determined and treated.
It often happens that the amount of water normalizes on its own by the end of the first trimester.
2. Low water in the second trimester is the most dangerous manifestation of this scourge.
The fact is that the problem of a reduced amount of amniotic fluid has not been thoroughly studied, and as such it is very difficult to choose a treatment. But if the amount of amniotic fluid does not return to normal, the consequences can be catastrophic. The risk increases significantly:
- Child injury before birth
- Curvature of the spine and pelvic bones
- Fetal hypoxia
- Intrauterine growth retardation
- Miscarriage
- Difficult delivery with very painful contractions
- And, the most dangerous thing, fusion of the fetus with the walls of the amniotic sac. This threatens serious damage to the child’s tissues and even amputation of limbs.
Why is oligohydramnios dangerous during pregnancy?
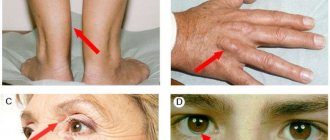
Oligohydramnios can cause many different complications. When a woman has little amniotic fluid during pregnancy, the baby begins to experience too much pressure from the walls of the uterus, which compress the amniotic sac. As a result, the fetus takes on an uncomfortable and unnatural position, which is fraught with the development of the following pathologies in the baby:
- curvature of the spine;
- clubfoot;
- deformations and dislocations of the hips;
- fetal hypoxia and developmental delay (hypotrophy).
For a woman, oligohydramnios is dangerous due to miscarriage and the development of complications during childbirth. With a reduced volume of amniotic fluid, the cervix may not dilate enough during delivery. Labor is weak, contractions are painful, but not strong. After childbirth, oligohydramnios can cause bleeding in a woman. If the pathology was discovered late and there are irreversible developmental disorders of the child, doctors may insist on early termination of pregnancy.
Articles on the topic
- Low blood pressure during early pregnancy - why hypotension occurs and methods of treatment
- Dental treatment during pregnancy - when and how it is safer to do it, contraindications and restrictions
- Formidron - instructions for use, side effects, contraindications, mechanism of action and analogues
Diagnostics
Clinical symptoms and objective signs only allow us to suspect the development of oligohydramnios. For reliable diagnosis, especially when the pathological process is not expressed, an ultrasound examination is required, with the help of which several important indicators can be determined:
- The volume of amniotic fluid is the main criterion on the basis of which the severity of oligohydramnios is determined.
- Condition of the placenta.
- Condition of the fetus.
- Frequency and rhythm of fetal heart contractions in later stages of pregnancy.
To determine the cause of the development of oligohydramnios, the gynecologist may prescribe additional tests. They include a clinical analysis of blood, urine, studies for the presence of infectious processes, and functional tests. The final diagnosis, including the severity, as well as the cause of the development of oligohydramnios, is established based on an analysis of all the results of an objective examination of a pregnant woman (ultrasound, CTG or fetal cardiotocography, tests for sexually transmitted infections).
Symptoms
In addition to ultrasound examination, the problem can be recognized by the following signs:
- painful and severely uncomfortable sensations during normal fetal movements until the end of the second trimester;
- persistent feeling of dryness of the oral mucosa;
- abdominal girth is too small, does not correspond to the deadline;
- measurements of the height of the uterine fundus do not correspond to the norm and differ to a lesser extent;
- aching feeling in the stomach.
If oligohydramnios is mild, the listed symptoms sometimes do not manifest themselves at all, but the problem can be identified as a result of an examination. You should not resort to self-medication and try to diagnose the pathology yourself, without the help of a specialist.
Possible complications and consequences of oligohydramnios
Oligohydramnios during pregnancy, the causes and consequences of which are different, is primarily dangerous because the fetus is not protected by a sufficient amount of amniotic fluid from external influences.
This can lead to a number of complications:
- An increase in the number of contacts between the fetus and the amniotic sac. This sometimes causes them to grow together.
- The mother's internal organs may begin to squeeze the unborn child. This leads to clubfoot, curvature of the spine, disorders of skeletal formation, hip dysplasia, and malformations of the skull.
- Impaired fetal mobility associated with a lack of amniotic fluid leads to developmental delays. There may be problems with growth and development of the nervous system.
- Increased risk of having an underweight baby. The probability of this pathology is less than 10% with a moderate form of oligohydramnios and more than 75% with a severe form.
- Drying of the skin of the unborn child.
- Oxygen starvation of the fetus.
- Deficiency of nutrients supplied with amniotic fluid.
In addition, oligohydramnios affects the course of pregnancy, childbirth and the postpartum period:
- A low-water pregnancy often ends prematurely and requires surgical intervention in the form of a cesarean section.
- Weakness of labor associated with oligohydramnios leads to a protracted labor process.
- High risk of postpartum hemorrhage.
In most cases, the listed consequences relate to a pronounced degree of oligohydramnios. The moderate form rarely causes significant complications, but requires observation by a specialist. Oligohydramnios can occur at almost any stage of pregnancy, and its main symptom, which the woman herself can recognize, is a relatively slow increase in abdominal volume for the current period.
Oligohydramnios carries certain risks, but is one of the most serious pathologies that occur in pregnant women.
With moderate oligohydramnios, the likelihood of fetal pathologies is extremely low, especially if the expectant mother follows the doctor’s recommendations and follows the treatment plan.
Despite the fact that the causes of oligohydramnios during pregnancy may not be obvious and do not always lead to serious consequences, during the process of bearing a child it is important to pay attention to any changes in health status and unusual symptoms.
If you mention them during a routine examination, this can help to diagnose oligohydramnios in a timely manner and provide the expectant mother with appropriate qualified assistance.
Article design: Svetlana Ovsyanikova
Diagnostic criteria for determining oligohydramnios in pregnant women
A doctor may suspect the presence of this problem during routine examinations.
Signs of oligohydramnios are:
- insufficient increase in abdominal circumference and uterine height during pregnancy. Indicators do not meet deadlines;
- insufficient activity of the developing child (less than 12-10 signs of movement per day);
- low AFI (amniotic fluid index). It will be discussed in more detail below.
Please note: initially suspected oligohydramnios is not the basis for a diagnosis, but only a functional disorder.
The painful condition is confirmed after dynamic monitoring of the development of pregnancy, based on repeated examinations (at least 3, with an interval of 2 weeks). If during this time the problem does not go away, then the specialist has every reason to make a diagnosis of oligohydramnios.
More accurately, this condition is detected by ultrasound. But still, to confirm pathological rather than functional oligohydramnios, confirmation of 3 studies performed at the above-mentioned time interval is required.
If, after the first ultrasound diagnosis, the doctor still suspects the onset of the development of true oligohydramnios, then he prescribes cardiotocography (CGT), which accurately determines whether the fetus has a problem or not. If changes in the placenta are suspected, Doppler testing is recommended. If the indicators of these studies are problematic, a diagnosis of pathological oligohydramnios can be immediately made, without waiting for dynamic ultrasound data.
With the functional version, it is recommended that the pregnant woman undergo vitamin therapy and drink Curantil for a month, then do an ultrasound again . In 95% of cases, oligohydramnios is no longer detectable. If pathology is present, further examination is carried out and the necessary treatment is prescribed.
Additional examination includes detection and identification of pathogens of infectious diseases using blood tests and determination of Rh conflict. Of diagnostic value are the AFP (alpha-fetoprotein) test to detect fetal defects, hCG (human chorionic gonadotropin), to identify placental problems, certain types of pregnancy pathologies, and chromosomal genetic abnormalities.
In the most serious cases, amniocentesis (examination of amniotic fluid by puncture) is indicated, followed by karyotyping. This study makes it possible to identify abnormalities at the gene and chromosomal levels.
Amniotic fluid index values during pregnancy
When considering the diagnosis of oligohydramnios, it is worth mentioning the determination of the amniotic fluid index (AFI).
Before the concept of the AFI index was introduced, the sonographer measured the longest gap of free amniotic fluid, which is located between the mother's anterior abdominal wall and the developing fetus (vertical pouch).
When establishing IAF, the doctor identifies 4 vertical pockets in certain study squares. The sum of these pockets represents the desired index, which is the main indicator of the presence or absence of oligohydramnios during ultrasound diagnostics.
Each stage of pregnancy has a corresponding index, which can be seen in the table:
Please note: AI standards vary from country to country, sometimes significantly.
Oligohydramnios is established when the index value is below normal. With a slight deviation (up to 10-15%), the doctor determines moderate oligohydramnios, and with large numbers - oligohydramnios.
If the values are sharply reduced, severe oligohydramnios is diagnosed. It requires continued examination of the pregnant woman to establish in more detail the cause, find the corresponding disease, defect, and determine the prognosis of the pregnancy.
Reasons for the development of oligohydramnios during pregnancy
Among the factors that contribute to oligohydramnios, there are several that can be considered in groups:
Congenital malformations of a developing child. These include: absence or insufficient degree of development of the valve apparatus of the urethra, absence or significant narrowing of the canal, pronounced narrowing of the ureters on both sides, complete absence of kidneys, lack of muscles of the anterior wall in a developing child (undercut belly syndrome), polycystic kidney pathology (Potter syndrome I, and Potter syndrome II).
- Acquired pathology of the developing fetus. Intrauterine infection with certain types of pathological microorganisms - cytomegaloviruses, chlamydia, ureaplasma, etc., developmental delays, chromosomal pathologies (eg Down syndrome).
- Diseases of a pregnant woman. Cardiovascular pathology (hypertension, diseases of the arteries and veins), severe toxicosis of pregnancy, systemic connective tissue diseases (systemic lupus erythematosus, rheumatoid arthritis, etc.), metabolic pathology - diabetes mellitus, alimentary obesity, endocrine diseases (thyroid gland ), conditions that cause severe dehydration in a woman (vomiting, diarrhea), chronic intoxication (alcohol, smoking).
- Placental pathology. Functional insufficiency of the placenta, heart attacks, anomalies (atrophic and sclerotic changes in the membranes, necrosis of the amnion).
- Rest. This group includes: post-term pregnancy, disruption of the integrity of the membranes (tear, complete rupture), intrauterine death of a child, oligohydramnios with an unknown cause, drug-induced oligohydramnios (while taking Indomethacin, Naproxen and other drugs).
Please note: oligohydramnios, caused by most causes, can be successfully treated therapeutically, except for developmental defects.
Among the many reasons for this condition, the main ones can be identified:
- gestosis (pregnancy toxicosis), leading to fluid loss;
- hypertension in a pregnant woman. Constantly elevated blood pressure numbers lead to disruption of water-salt metabolism, leading to oligohydramnios;
- diabetes. Hormonal-enzymatic disruptions in this condition cause disruption of the formation and functionality of amniotic fluid;
- infectious diseases - acute forms of tonsillitis, bacterial kidney damage (nephritis, pyelitis), moderate and severe forms of viral infections (influenza, torch complex - herpes, rubella measles, toxoplasma);
- state of chronic hypoxia in a developing child.
Causes and signs of oligohydramnios during pregnancy
Often a woman does not notice the changes; some pregnant women may experience pain when the baby begins to move. A pregnant woman may experience nausea, weakness, and unpleasant dryness in her mouth.
Scientists are still studying oligohydramnios as a pathological process. It is believed to be caused by a previous infection. Low hydramnios can result from:
- Sudden changes in blood pressure.
- Metabolic problems.
- Disruptions in a woman's hormonal system.
- Late toxicosis.
- Fetal defect during intrauterine development.
- Several fruits available.
- Reduced excretory function of the aqueous membrane.
- Post-term pregnancy, in this situation the placenta loses its quality and begins to age.
- Abuse of bad habits.
- Inflammatory process, infectious or bacterial disease.
- Exacerbation of a chronic disease.
If you suspect oligohydramnios, it is necessary to exclude congenital defects of the fetus. It is especially important to do this in the first trimester. When the fetus is infected early, the woman has suffered a serious illness. In this situation, it is necessary to be examined in order to promptly find out about a hidden infection. Oligohydramnios occurs when the fetus's urine output decreases due to hypoxia.
Often in a pregnant woman with oligohydramnios, the size of the baby changes. With a sharp decrease in amniotic fluid, the fetus can be squeezed by the walls of the uterus, this is dangerous, the baby does not have enough oxygen. Everything can end in the death of the fetus. Sometimes the skin of the fetus fuses with the walls of the uterus. If you want to save the baby, you must be provided with timely assistance.
Oligohydramnios can be diagnosed using ultrasound. Without examination, a doctor may suspect oligohydramnios:
- When a woman’s abdomen and the height of the uterine fundus do not correspond to the period of pregnancy.
- If the fetus practically does not move.
- When the doctor touches the uterine area, it immediately becomes dense.
- If the gynecologist observes a flat bladder.
Principles of nutrition and drinking regime
A woman diagnosed with oligohydramnios should adhere to the following dietary rules:
- give preference to a protein-vegetable diet;
- exclude sugar, salt and various spices and marinades;
- enrich your diet with foods containing potassium (raisins, figs, grapes, watermelon, dried apricots, melon);
- stimulate the functioning of the urinary system by daily consumption of kefir, herbal infusions and weak tea with lemon;
- eat more vegetables that have undergone minimal heat treatment and retain fiber;
- Divide food into 5-6 small portions.