Oophoritis is an inflammatory process of paired female reproductive glands. It can be either one-sided or two-sided. It often occurs with simultaneous inflammation of the fallopian tubes (salpingitis), in acute or chronic form.
In the first case, intense pain in the lower abdomen, urination disorders, fever, and pathological discharge (leucorrhoea) are noted.
The chronic form is characterized by the presence of pain and metrorrhagia (menstrual irregularities).
The accumulation of pus in the ovaries can lead to the development of pelvioperitonitis, and subsequently to secondary infertility as a result of impaired ovarian function.
- 2 Symptoms and signs - acute, subacute and chronic form
- 3 Effect on pregnancy
- 4 Unilateral oophoritis (right-sided or left-sided)
- 5 Bilateral oophoritis
- 6 Diagnostics
- 7 Treatment
Types of disease
There are different classifications of this disease. Oophoritis is divided into two types:
- Specific. The disease appears due to sexually transmitted infections.
- Non-specific. Caused by bacteria that are found in the intestines or vagina. This form of the disease may be preceded by abortion, various gynecological manipulations and decreased immunity.
According to the nature of their course, several forms of oophoritis are distinguished:
- Acute form. During acute oophoritis, there are very pronounced symptoms, which manifest themselves in the form of muscle and headache, general weakness and fever. All this negatively affects the general condition of the patient.
- Chronic form. In this case, the symptoms are not very pronounced. Only during exacerbations are minor pains in the lower abdomen observed.
- Subacute form. Develops against the background of mycotic infection or tuberculosis. It is quite rare.
The ovaries are a paired organ, so sometimes not all ovaries are affected, but only part of them. On this basis, the following forms of oophoritis are distinguished:
- double-sided;
- left-handed;
- right-sided
Right-sided oophoritis
The pathology is characterized by an inflammatory process in the right ovary. Often, right-sided inflammation is confused with appendicitis, due to very similar symptoms: sharp girdling pain in the lower abdomen, radiating to the lower back. The causative agents are microorganisms and infection. Without timely medical care, inflammation can spread to a healthy ovary.
The cause of inflammation of the right ovary can be gynecological manipulations and operations, intrauterine device, abortion. The disease does not develop if you have a strong immune system. Lack of personal hygiene, adherence to strict diets, frequent changes of sexual partners and alcohol consumption are factors that provoke the disease.
Symptoms of right-sided oophoritis:
- pain in the lower abdomen on the right side
- temperature rise
- weakness and severe fatigue
- vaginal bleeding
- pathological vaginal discharge
- pain during intercourse
- the onset of menstruation at the wrong time (broken cycle)
During treatment, it is important to maintain sexual rest and fully follow the recommendations of the attending physician.
Bilateral oophoritis is diagnosed if the right and left ovaries are inflamed at the same time. The reasons are the same as for unilateral oophoritis. The main manifestations are intense pain in the groin, lower abdomen and lower back. Pathological discharge, vaginal discharge and other symptoms that are characteristic of the unilateral form of the disease are also characteristic of bilateral ovarian pathology.
Bilateral oophoritis develops from a unilateral ovarian lesion. This happens when pathogenic microorganisms pass from the fallopian tubes through the abdominal lining. And salpingoophoritis develops if simultaneous infection of the ovaries and uterine cavity occurs.
The main cause of 2-sided oophoritis: genital infections or microorganisms of normal microflora that began to multiply under the influence of certain factors. In this case, the provoking factor for exacerbation of the disease is unprotected sexual intercourse, hypothermia, a decrease in the protective properties of the immune system, infectious processes in the body, emotional and nervous shocks.
Diagnostics reveals swelling of the ovaries and the appearance of an abscess, which can be felt as a small lump. It is necessary to perform laparoscopy to determine the stage of the disease and the location of the inflammation. If necessary, the doctor may prescribe a puncture and administration of medications.
The goal of treatment is to eliminate intoxication of the body and weaken the inflammatory process. Broad-spectrum antibiotics are used to treat the acute stage. Treatment also includes anesthetics, immunostimulants and vitamin complexes to fight infection. In chronic cases, the patient should be prescribed anti-inflammatory medications and physical therapy.
Prevention of inflammation is a mandatory step. It is necessary to exclude unprotected sexual intercourse, abortion and cooling of the genitourinary system. At the first manifestations of ARVI, it is necessary to urgently treat the disease, preventing its development and chronicity.
Causes of oophoritis
Such inflammation necessarily appears due to some reason. The ovaries are located in such a way that the primary penetration of infection into them is impossible. Inflammation of the ovaries appears in the uterine tubes. However, this is not the only source of inflammation. The disease can even appear due to appendicitis. In this case, inflammation appears due to staphylococci, streptococci and E. coli.
Oophoritis can occur if a person has infections. Infectious agents include various viruses.
There are factors that contribute to the appearance of oophoritis. These include:
- sexual contacts without protection;
- long-term use of an intrauterine device;
- non-regular sexual partners;
- stress, which negatively affects the protective properties of the immune system;
- smoking and drinking alcohol, which, when ingested, contributes to changes in the composition of mucus;
- problems with the genitourinary system;
- presence of chronic infections;
- problems with the endocrine system;
- hypothermia.
In addition, ovarian inflammation can be caused by diseases such as tuberculosis, gonorrhea, chlamydia, mycoplasmosis and trichomoniasis.
Diagnostics
The diagnosis is made based on the anamnesis (history) and symptoms of the disease. An additional diagnostic method is ultrasound examination of the pelvic organs and hysterosalpingography. In doubtful cases, diagnostic laparoscopy is possible - examination of the uterus and appendages using an endoscope through a puncture in the abdominal wall. The latter method is the most informative in the diagnosis of oophoritis and its complications.
The microflora of the cervical canal and vagina is examined. Serological blood tests for chlamydia help in diagnosis. If tuberculosis is suspected, diagnosis is carried out at an anti-tuberculosis dispensary. It includes diagnostic curettage, culture of menstrual blood for mycobacteria, tuberculin tests, metrosalpingography and other methods.
It is necessary to examine the sexual partner, since in most cases the cause of oophoritis is sexually transmitted diseases.
Differential diagnosis is carried out with tubal pregnancy, appendicitis, ovarian apoplexy, rupture of an ovarian cyst. It must be remembered that a combination of appendicitis and right-sided oophoritis is possible. Therefore, when clinical symptoms of the disease appear, the patient should be examined by a surgeon.
Mechanism of disease development
The spread and development of infection in the body does not occur immediately. First it enters the uterine cavity and spreads to the tubes. At the very beginning of the development of the disease, the mucous membrane suffers. After this, the muscular and serous layers are affected. The fallopian tube becomes denser and lengthens. Inside, purulent fluid appears and is secreted.
Over time, the process moves to the ovaries. Their tissues are damaged by the pus that is released from the fallopian tubes. This leads to the appearance of adhesions. Sometimes changes can even affect the surrounding peritoneum.
This process is called periadnexitis. The secretion that has accumulated as a result of the development of infection may contain pus or be completely transparent. Pus accumulated in the ovaries leads to the appearance of pyovar. If the infection continues to develop, it will spread beyond the ovary, which will lead to the appearance of pelvioperitonitis.
Causes
The main reasons for the development of oophoritis include:
- Infections.
- Injuries of the pelvic organs.
- Diseases of organs adjacent to the appendages of infectious origin.
- Structural changes in the ovaries that develop as a result of the formation of cysts and other neoplasms.
Worth knowing! Penetration of infection into the organs of the reproductive system is the main cause of the development of oophoritis.
Depending on the type of microorganisms that caused the development of the inflammatory process, oophoritis can be:
- Specific:
- Trichomonas;
- gonococcus;
- chlamydia;
- mycoplasma;
- tuberculosis bacillus.
- Non-specific:
- staphylococcus;
- streptococcus;
- candida;
- coli.
The following factors can contribute to the spread of pathogenic microorganisms into the tissues and cavity of the ovaries:
- Violation of intimate hygiene rules.
- Frequent and intense douching.
- Use of antibacterial drugs.
- Hormonal disorders.
- Decreased general immunity.
- Unprotected sex
- Abortion.
- Diagnostic curettage.
- Installation of an intrauterine device.
- Menstruation.
- Childbirth.
In some cases, the infection penetrates into the ovaries from neighboring organs, most often this occurs when:
- appendicitis;
- peritonitis;
- cystitis
Chronic oophoritis develops as a result of undertreatment of the acute form of the disease. Exacerbations of a chronic disease occur under the influence of the following factors:
- hypothermia of the body and organs of the genitourinary system;
- nervous fatigue;
- intense physical activity;
- problems in the functioning of the endocrine system;
- chronic infectious diseases;
- decreased immunity due to poor nutrition and lack of essential vitamins and microelements in the body.
Symptoms of ovarian inflammation
The disease has various symptoms. The acute form is expressed by the following symptoms:
- sexual intercourse is accompanied by field sensations;
- bleeding between periods;
- fever and fever;
- often purulent and serous discharge comes out of the genital tract;
- pain when urinating;
- The lower abdomen can be very painful, sometimes the pain extends to the lower back and sacrum.
Symptoms of chronic oophoritis include:
- problems with the menstrual cycle;
- relapses of the disease that appear after severe hypothermia;
- sexual intercourse is accompanied by pain in the lower abdomen.
If the disease is not cured in time, exacerbations may occur. They have the following symptoms:
- the appearance of white discharge;
- decreased libido, problems with sexual function;
- ovarian function is impaired;
- severe pain that may be in the vagina and lower abdomen;
- increased pain before the onset of menstruation.
During an examination by a gynecologist, it may be discovered that the size of the ovaries has increased. Sometimes the chronic form is the cause of disturbances in the neuropsychological sphere of a person. Disorders include increased irritability, sleep problems, decreased levels of performance, and fatigue. Sometimes the chronic form does not have pronounced symptoms.
If some of the above symptoms are detected, it is recommended to consult a gynecologist.
Complications
Acute oophoritis with timely, high-quality diagnosis and treatment in most cases ends with the patient’s complete recovery. If the disease has been neglected or is not fully treated, it becomes a chronic process with periodic exacerbations.
Chronic oophoritis can cause the following complications and concomitant diseases:
- Peritonitis (purulent inflammation of the abdominal tissues).
- Abscess of any organ of the genitourinary system.
- Internal bleeding.
- Infectious diseases of the gastrointestinal tract.
- Diseases of the excretory system (pyelonephritis, cystitis).
- Diseases of the thyroid gland (occur against the background of long-term hormonal imbalance caused by impaired ovarian function).
- Infertility (occurs when the patency of the fallopian tubes is disrupted by an adhesive process caused by infection).
- Menstrual irregularities (delayed menstruation, cycle irregularity, heavy discharge).
- Sexual dysfunction (pain during sex, decreased libido).
- Increased likelihood of ectopic pregnancy and spontaneous miscarriage.
Important! The only way to prevent the development of complications is to regularly visit a gynecologist and follow all his recommendations regarding the prevention and treatment of certain diseases of the reproductive system.
Oophoritis during pregnancy
Disturbances in the functioning of the ovaries have a bad effect on the course of pregnancy in women. The ovaries are responsible for producing the required amount of sex hormone. The maturation and release of the egg also depend on them. All this affects not only the pregnancy itself, but also fertilization. Sometimes the disease leads to infertility in a woman.
If chronic oophoritis does not lead to infertility, then before conception you must make an appointment with a doctor for examination. This will avoid the following complications:
- Hormonal imbalance, which sometimes leads to miscarriage.
- Infertility. Due to impaired functioning of the ovaries, problems with the production of eggs may occur, which make the process of ovulation impossible.
- Ectopic pregnancy.
- Oophoritis often leads to the appearance of adhesions. Because of them, fertilization can occur in the fallopian tube rather than in the uterus.
- Fetal infection. It is carried out due to an infection that is present in the woman’s body. In this case, infection occurs not only during pregnancy, but also during childbirth.
It is for these reasons that it is better to visit a doctor before planning a pregnancy.
What is chronic oophoritis?
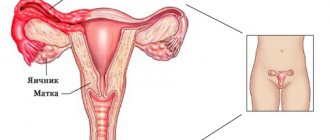
The ovary (ovarium) is a paired hormonally active organ of the female reproductive system. Located in the pelvic area, on both sides of the uterus. Contacts the uterus through the fallopian tubes (salpinx).
The ovaries together with the fallopian tubes are often called the uterine appendages.
Follicles with eggs develop in the ovaries, and the bulk of female sex hormones (estrogens, progesterone) are produced.
Ovaries, fallopian tubes and uterus - location
Oophoritis is an inflammatory disease of the female genital area associated with infectious or immune damage to ovarian tissue.
Isolated oophoritis is extremely rare (6-10%). Usually the fallopian tubes are involved in the inflammatory process. In this case, the disease is called salpingoophoritis or adnexitis.
The course of oophoritis is more often of a primary chronic nature - the disease develops gradually, without obvious clinical manifestations, seriously complicating diagnosis and timely treatment. Chronic inflammation is periodically complicated by exacerbations.
In rare cases, the disease begins clinically acutely, and then, with inadequate treatment or the influence of other factors, takes a subacute or chronic form.
Oophoritis (inflammation of the ovaries): types of course
ICD-10 code
N70.1 Chronic oophoritis/salpingitis N70.9 Oophoritis/salpingitis, unspecified
Chronic unilateral oophoritis - what is it?
If the inflammatory process affects only one ovary (the other remains healthy), then the painful condition is one-sided.
Long-term inflammation of the left ovary is called chronic left-sided oophoritis, and the right ovary is called chronic right-sided oophoritis.
Localization of inflammation during oophoritis
Chronic bilateral oophoritis - what is it?
Long-term, low-grade inflammation of both ovaries is called chronic bilateral oophoritis.
Without treatment, chronic oophoritis in women often becomes a source of ectopic pregnancy, infertility, and acute surgical pathology
Consequences of chronic oophoritis
- Decreased ovarian function, anovulation, menstrual irregularities
- Dishormonal diseases of the genital organs
- Spontaneous miscarriage
- Ectopic pregnancy
- Adhesive process
- Infertility
- Persistent pain syndrome
- Involvement of neighboring organs in the chronic inflammatory process: bladder, intestines, etc.
Dangerous complications of the disease
- Purulent tubo-ovarian "tumor"
- Ovarian abscess
- Piovar
- Peritonitis
Return to contents
Diagnosis of the disease
Diagnosing this disease is difficult. The most common symptom of the disease is acute pain in the abdominal area. It can also appear in other diseases. Other signs of oophoritis can appear in various diseases of the abdominal organs.
Oophoritis is often diagnosed if a woman complains of problems with her menstrual cycle. To establish the most accurate diagnosis, the following examinations are carried out:
- Carrying out analyzes in the laboratory. They are done to determine the level of white blood cells in the urine and blood. It increases if there is inflammation of the ovaries.
- Gynecological history. Determines the location and nature of pain.
- Ultrasound. It is carried out to examine the pelvic organs.
- Gynecological examination. Abnormalities in uterine mobility and ovarian size are checked.
- Hysterosalpingoscopy. With its help, you can identify modifications of the uterine tubes.
The most informative and effective diagnostic methods include laparoscopy. During which a visual examination of the uterus, its tubes and ovaries takes place. It is performed if the patient has pain in the lower abdomen. During the examination, the doctor may identify adhesions and low patency of the fallopian tubes.
Prevention
Prevention of oophoritis includes:
- Regular gynecological examinations. Every woman should visit a gynecologist at least once a year for preventive purposes, since many female diseases can be asymptomatic.
- Timely detection of inflammatory processes in the reproductive organs (any harmless vaginitis or cervicitis can become a source of infection for the uterus and its appendages).
- Protection against sexually transmitted infections.
- Diagnosis and treatment of inflammatory diseases of organs located near the ovaries.
- Healthy lifestyle. Proper nutrition, giving up bad habits, physical activity, adequate sleep and rest - all these factors increase the female body’s ability to resist infections.
It is important to remember that the ovary is an organ on the condition of which a woman’s ability to have children depends. Therefore, any pathological changes in it affect reproductive function. Chronic inflammatory processes are especially dangerous. Against the background of chronic oophoritis, problems with conception arise, and in the event of a long-awaited pregnancy, various pregnancy complications arise.
Zubkova Olga Sergeevna, medical observer, epidemiologist
29, total, today
( 57 votes, average: 4.77 out of 5)
Emergency contraception methods - types, effects on the body, disadvantages and contraindications
Hormonal contraceptives: tests for selection
Related Posts
Treatment methods
Most often, the course of treatment consists of antibiotics. Many of them are in the group of penicillins and cephalosporins. The most popular drugs include Cefatoxime, Timentin and Amoxiclav.
Antimicrobial agents are also used during treatment. They are very effective in treating the chronic form of the disease. Medicines such as Tinidazole and Metromindazole are often used.
Oophoritis is accompanied by severe pain. To relieve them, drugs related to anti-inflammatory non-steroidal drugs are used. This group includes Ibuprofen, Indometac and Diclofenac. In gynecology, suppositories or tablets with indomethacin are often used.
Treatment of the disease must be carried out comprehensively. The bulk of treatment is aimed at treating the infection, with additional measures aimed at supporting the body's immune system. To increase the effectiveness of the immune system, immunomodulating agents and vitamins are prescribed. Many gynecologists use the drug Vagilak, which places lactobacilli in the vagina. This allows the natural acidic environment to be restored.
Care should be taken to ensure that the ovaries are completely “rested” from the resulting inflammatory shock. In this case, combined oral contraceptives will help. With their help, the menstrual cycle is regulated, which allows you to preserve the required number of eggs.
Treatment
To avoid chronicity of the process and infertility, treatment of ovarian inflammation must be carried out on time and in full. During the period of acute manifestations of the disease, the patient is hospitalized in a gynecological hospital, she is prescribed bed rest and diet.
The main goal of therapy is to eliminate the pathogen with antimicrobial drugs. Chronic oophoritis is treated on an outpatient basis, in this case immunocorrection and normalization of local blood circulation come first.
Acute stage of the disease
During acute manifestations of oophoritis, food should be easily digestible and contain a lot of protein, dietary fiber and vitamins. You should temporarily avoid marinades, smoked meats, fatty meats and fish. During the period of fever, a woman should drink a large amount of warm liquid: compote, berry juice, still mineral water.
Applying ice to the lower abdomen for 10-15 minutes every hour will help reduce the severity of pain and reduce inflammatory damage to ovarian tissue. After acute symptoms subside, you can use a warm heating pad - it promotes resorption of the infiltrate and healing.
, broad-spectrum antibiotics are used for treatment
- Ampcillin;
- Oxacillin;
- Ampiox;
- Doxycycline (Unidox);
- Cefazolin.
The course of treatment depends on the type of pathogen and the drug, on average it lasts from 7 to 21 days. If the chosen remedy is ineffective, it is changed to another within 3 days. By this time, the culture result is usually ready, so the gynecologist can prescribe a specific antibiotic for this pathogen. Treatment of chlamydial infection lasts at least 2 weeks: this is the only way the drug will have an effect on all active forms of the parasite.
From 3-5 days of antibacterial therapy, antifungal drugs are added to prevent genital candidiasis:
- Ketoconazole 0.4 g per day for 5 days;
- Miconazole 0.25 g 4 times a day for up to two weeks.
Pathogenetic (affecting the links of the pathological process) treatment of oophoritis includes:
- Desensitization – to prevent autoimmune processes and chronic disease. For this purpose, calcium chloride is administered intravenously or antihistamines (Zodak, Tavegil, Diazolin) are taken orally.
- Anti-inflammatory drugs - to reduce the area of inflammatory damage to ovarian tissue. The most effective for this are glucocorticoids, which are taken orally 2-5 tablets per day (celeston, triamcinolone). Non-steroidal anti-inflammatory drugs (NSAIDs) are widely used - diclofenac, naproxen, nimesulide.
- Vitamins – have a general strengthening effect, accelerate the tissue healing process. For oophoritis, vitamins A, E, C are prescribed orally, and B1 intramuscularly.
- Absorbable drugs - prevent the formation of adhesions in the pelvis and fallopian tubes. In gynecology, Wobenzym, Serta, lidase, crystalline trypsin and magnesium sulfate are used.
- Stimulators of the immune response - improve tissue protection from the pathogen, promote its elimination (removal from the body). They are represented by preparations of animal (polybiolin, plasmol, placenta extract) and plant (aloe extract, peat, fibs) origin.
Local treatment of oophoritis includes irrigation of the vagina with an antiseptic solution (weak manganese solution, chamomile decoction), after which the following is administered:
- A tampon soaked in diluted dimexide and Vishnevsky ointment;
- Anti-inflammatory suppositories with indomethacin.
Chronic stage
Oophoritis after its chronicity should be treated with restorative methods:
- Gynecological massage;
- Physiotherapy - ultra-high frequency (UHF) electric field, ultraviolet irradiation, intravenous laser irradiation of blood, electrophoresis with anti-inflammatory, analgesic, vasodilating drugs;
- Plasmapheresis – purification of blood plasma from toxins;
- Therapeutic gymnastics – training in deep breathing techniques, exercises at a slow pace for the joints of the upper and lower extremities, pelvis;
- Sanatorium-resort treatment - balneotherapy for normal ovarian function (Sochi, Nalchik, Pyatigorsk); in case of ovarian failure, resorts with radon and iodine-bromine waters should be avoided.
Twice a year, a woman should take multivitamin preparations; in addition, the doctor prescribes immunomodulators (Licopid).
Traditional treatment
Folk remedies have an anti-inflammatory effect and can be used at any stage of the disease. Some recipes:
- Mix the herb of sweet clover, centaury and coltsfoot flowers in equal quantities, leave 1 tablespoon of the mixture in 250 ml of boiling water for an hour. Take the infusion 1/3 cup 6 times a day for one month.
- Mix 2 parts of mallow flowers and oak bark, 3 parts of sage leaves, 5 parts of chamomile flowers. Infuse 2 tablespoons of the mixture into 1 liter of boiling water, use the resulting mixture for douching the vagina and soaking tampons before insertion.
- Infuse 50 g of juniper stems and berries in a bucket of boiling water for 2 hours, use the infusion for baths.
Acute oophoritis and each exacerbation of chronic oophoritis lead to irreversible damage to ovarian tissue. Infertility can develop after the first episode of the disease, so it is extremely important to immediately consult a doctor and begin treatment.
Barrier contraception, a regular sexual partner and annual examination for sexually transmitted infections are the main methods of preventing oophoritis associated with STDs.
Prevention of oophoritis
To avoid the appearance of this pathology, you need to follow some rules. These include the following points:
- you should lead an active lifestyle;
- avoid hypothermia;
- do not forget about personal hygiene;
- use different methods of contraception;
- be regularly examined by a gynecologist.
The above rules must be followed from adolescence. It is very important that parents explain to teenage girls how to prevent the occurrence of inflammatory processes. This will help in the future to avoid the occurrence of diseases such as oophoritis.
Share the article on social media. networks:
How to treat oophoritis on the right
In case of acute right-sided inflammation and exacerbation of chronic oophoritis on the right, it is necessary to treat with antibiotics, starting therapy as quickly as possible. Typically, the doctor will not wait for the results of bacterial culture and will prescribe a combination of antimicrobial drugs (an antibiotic in combination with Metronidazole). In addition, anti-inflammatory drugs and local therapy for vaginal inflammation will be required.
In case of chronic right-sided adnexitis with oophoritis, antibiotic therapy can be avoided: in the absence of high fever and severe pain, the use of anti-inflammatory therapy in combination with drugs to increase immunity and improve blood flow in the uterine appendages is sufficient. An important condition for successful treatment is taking hormonal drugs to correct endocrine disorders caused by ovarian damage.
If purulent tubo-ovarian formations (pyovar, tubovar, pyosalpinx, abscess) are detected, surgery will be required. The most commonly used method is laparoscopic tumor removal.
As the inflammatory process subsides and in case of chronic oophoritis, it is necessary to conduct a course of physiotherapy (magnetic therapy, electrophoresis, phonophoresis) and sanatorium procedures (baths, mud).
Pathogenesis
The female urogenital tract is normally protected by several natural barriers that prevent infection from penetrating into the overlying organs. They are:
- 1Closing of the labia.
- 2The acidic environment of the vagina, which is provided by lactobacilli. This requires an optimal level of nutrient substrate (glycogen) and an equilibrium state of the vaginal microflora.
- 3Regular desquamation of the vaginal epithelium. When the epithelium is rejected, pathogenic microorganisms are also released.
- 4 The presence of cervical mucus (mucous plug) in the cervical canal, which contains mucopolysaccharides, lysozyme, and immunoglobulins.
- 5Desquamation of the functional endometrium according to the menstrual cycle.
- 6Contraction of the muscular layer of the fallopian tubes (peristalsis) and flickering of the ciliated epithelium towards the uterine cavity also contribute to the elimination of pathogens.
Under the influence of risk factors, natural barriers are destroyed, which leads to the penetration of infection and the proliferation of microorganisms.
In the pathogenesis of oophoritis, both the ascending mechanism of infection spread and the hematolymphogenous one are important.
As mentioned above, isolated oophoritis is quite rare. In this case, the infection is most often introduced from nearby organs:
- 1From the rectum and sigmoid colon with the development of left-sided oophoritis, and then salpingitis.
- 2From the appendix with the development of right-sided oophoritis and salpingitis.
The ascending route of infection occurs in the presence of risk factors and dysfunction of the barriers of the urogenital tract described above. In such cases, normal elimination of the pathogen from the lower parts of the reproductive system does not occur, so the infection penetrates deeper and deeper.
Pathogenic microorganisms begin to produce exo- and endotoxins, pathogenicity factors. Inflammation of the ovaries occurs with five classic signs, described by Hippocrates: edema, hyperemia (redness), microcirculation disorder, dysfunction and pain.
Very quickly, the infectious process from the ovaries moves to the fallopian tubes with the development of an adhesive process in them.
In the presence of an active immune response to inflammation and adequate antibacterial therapy, the symptoms gradually subside, the infectious agent is eliminated and recovery occurs.
The pathogenesis of the chronic process is distinguished by the launch of an autoimmune reaction. That is, in response to the initial introduction of the pathogen, the body is not able to provide full protection and respond with a normal immune response.
Description
Bilateral oophoritis is a consequence of infection of the ovaries through the lymphatic or circulatory system. Typically, the appendages become infected ascendingly through the uterus and its tubes, causing an extensive inflammatory process, so this pathology is rare. Women with weakened immune systems are most susceptible to oophoritis.
As the disease progresses, the functionality of the appendages is impaired. Inflammatory and infectious processes prevent the correct flow of the menstrual cycle and the maturation of eggs. This is manifested by irregular menstruation and the inability to get pregnant. The longer bilateral oophoritis occurs, the more severe degenerative processes occur in the appendages. With timely treatment, the disease goes away quickly and does not cause any complications.
Is pregnancy possible?
The presence of chronic bilateral oophoritis does not exclude pregnancy. Conception is possible in the presence of ovulation, which can occur at least once every few cycles. However, it is recommended that a woman become pregnant only after complete recovery. This is explained as follows:
- Increasing the timing of the planned pregnancy. Associated with menstrual irregularities, periodic lack of ovulation, and insufficiency of the corpus luteum of the ovary. Conception can occur both in the first planned cycle and after several years. Its likelihood is determined by the severity of bilateral oophoritis.
- Possibility of fetal damage. An extensive inflammatory process negatively affects the development of the embryo, and the infection can penetrate the placenta and infect it. This can lead to the birth of a child with multiple pathologies, intrauterine death, spontaneous miscarriage or premature birth.
- Risk of exacerbations during pregnancy. The chronic form of bilateral oophoritis is most dangerous during gestation. This is explained by the natural decrease in a woman’s immunity during pregnancy, which increases the likelihood of an exacerbation of the disease. The second important factor is the inability to take most types of medications to relieve symptoms and eliminate pathology due to their negative impact on the development of the embryo.
If there is an infection in the genital tract and there is a high chance of infecting the child, delivery is carried out by cesarean section.
In the absence of exacerbations of bilateral ovarian inflammation during pregnancy, there is a high probability of giving birth to a healthy child. To prevent intrauterine infection, the doctor must periodically prescribe the woman antimicrobial and other drugs approved during gestation. Additionally, progesterone levels should be monitored in the first trimester. If the ovaries fail, a pregnant woman should take hormone-containing medications to support the proper development of the fetus.
Risk factors
There are genital, extragenital and social risk factors for the occurrence of oophoritis/salpingo-oophoritis.
Genital (that is, associated with the female reproductive system) include:
- 1Infections transmitted through sexual contact (including history).
- 2Vaginal dysbiosis.
- 3Inflammation of the vaginal mucosa, cervix.
- 4Medical and instrumental termination of pregnancy.
- 5 Interventions involving instrumental expansion of the cervical canal (hysteroscopy, hysterosalpingography, diagnostic and therapeutic curettage of the uterine cavity).
- 6Installation of an intrauterine device within the last 6 weeks increases the risk of inflammation by 2-9 times.
- 7In vitro fertilization.
Extragenital risk factors:
- 1Endocrine pathology.
- 2Taking systemic glucocorticosteroids.
- 3Urinary tract infections.
- 4Immunodeficiency states (taking cytostatics, HIV infection).
Social factors that increase the incidence of this pathology:
- 1Promiscuous sex life.
- 2 Change of permanent sexual partner (especially during the previous 3 months).
- 3Early onset of sexual life.
- 4Chronic stress.
- 5Non-traditional sexual contacts.
- 6Forced sexual intercourse (including history).
In pathogenesis, one can note a combination of reasons that provide conditions for the occurrence of an infectious process.
Treatment of oophoritis
Oophoritis is an inflammatory process occurring in the ovaries. Now this is a fairly common disease, so alternative treatment for oophoritis is widely practiced. Its diagnosis and treatment are often difficult, since it is often accompanied by concomitant inflammatory processes developing in neighboring organs. In the absence of proper treatment, this situation can lead to serious disruptions in the functioning of the digestive, endocrine, and nervous systems.
Traditional treatment of oophoritis
Experts believe that traditional treatment for oophoritis should be used only in the chronic stage of the disease. Its main recipes include the following:
1.
To treat oophoritis, mix dried linden and chamomile flowers in a 3:2 ratio. After this, to treat oophoritis, take five to six spoons of the resulting mixture, add 1 liter of water, boil and let the broth brew for half an hour. When it has cooled to body temperature (36.6 degrees), strain it through double cheesecloth. The resulting infusion can be used for baths or for vaginal douching. Sometimes you can add the herb cinquefoil to the collection for traditional treatment;
2.
Prepare a mixture of the following medicinal herbs for treatment: take sandy immortelle flowers, birch leaves, wild strawberries, yarrow, mint herb, nettle leaves, string, rose hips and rowan berries in the ratio 2:2:2:2:2:3:3:3 :1. All ingredients for the traditional treatment of oophoritis should first be cut into medium-sized pieces. Place 2-3 tablespoons of the resulting mixture in 0.5 liters of boiling water and leave the mixture for 10 hours, then strain the solution. The infusion should be taken for oophoritis, 0.5 cups three times a day.
Try using the above folk methods for treating oophoritis, and you will soon feel relief.
Symptoms of the disease
At stage 1 of the disease, the symptoms are minimal. A woman may experience minor pain in the lower abdomen and unpleasant vaginal discharge. As the infection spreads, the following symptoms appear:
- increased abdominal pain;
- increased body temperature with evening chills;
- painful and frequent urination;
- violation of menstruation (delay of the next menstruation, prolonged bleeding, painful onset of menstruation);
- signs of deterioration in general condition (weakness, rapid onset of fatigue, decreased performance).
Signs of suppuration and formation of an ovarian tumor are manifested by a deterioration in health, a sharp increase in temperature and severe pain. It is optimal to identify an acute inflammatory process in the ovary in the early stages, when the risk of dangerous complications is minimal.
Diagnostic measures
6.1. Anamnesis
When collecting anamnesis, it is necessary to clarify the time of onset of symptoms, their connection with any medical intervention, or casual sexual contact. The doctor will definitely ask if this is the first time the woman has noticed such symptoms.
Information about concomitant extragenital pathology and recent infectious diseases (including ARVI) is of great importance.
Competent collection of anamnesis and full provision of information by the patient allows us to narrow the range of necessary diagnostic procedures and prescribe adequate drug therapy.
6.2. Gynecological examination
When examining the vagina in the speculum, the following are observed:
- 1Pathological discharge.
- 2Hyperemia of the mucous membrane, swelling of the tissues.
- 3Painful sensations when installing mirrors.
These signs are associated with concomitant colpitis and/or cervicitis. But this cannot be evidence of damage to the overlying structures of the urogenital tract.
According to the latest European, American, and Russian recommendations, reliable minimum diagnostic criteria for bimanual examination are:
- 1Pain when palpating the area of the appendages on the affected side (on the right - with right-sided oophoritis, on the left with left-sided oophoritis, on both sides - with bilateral oophoritis).
- 2Painful sensations when the cervix is displaced.
- 3In an acute inflammatory process, bimanual examination is usually difficult due to the sharp pain that occurs and the woman’s natural resistance. But if the examination was successful, the doctor will find swollen, hardened, enlarged ovaries.
- 4In a chronic process, pain on palpation is not so intense, so examination is possible. The uterine appendages are somewhat painful on palpation, heavy, dense to the touch. It is possible to identify round formations in the area of the appendages (hydrosalpinx, tubo-ovarian formations).
- 5One of the signs of the adhesive process is the retroposition of the uterine body (Russian national recommendations, 2015).
6.3. Pregnancy test
One of the diagnostic methods necessary for adequate differential diagnosis of oophoritis and salpingoophoritis is a pregnancy test. Ectopic (tubal, ovarian, abdominal) pregnancy can occur with similar clinical symptoms. The pregnancy test must be negative.
6.4. Microscopy of smear for flora
The results of a smear on the flora may indicate the presence of:
- 1Specific inflammation – in the presence of trichomonas or gonococci in the smear.
- 2 Nonspecific inflammation - with an increase in the number of leukocytes in the smear (10 or more) and the predominance of coccal flora over rod flora.
- 3 Bacterial vaginosis – if there are “key cells” in the smear.
6.5. Clinical and biochemical blood tests
The results of the CBC may indicate the presence of an inflammatory process in the body:
- 1increased level of leukocytes;
- 2increase in ESR;
- 3increased levels of C-reactive protein.
- 4 protein imbalance (dysproteinemia) with a predominance of globulins (a sign of acute inflammation).
6.6. Culture of the contents of the cervical canal
By bacterial culture of the contents of the cervical canal, it is possible to detect the causative agent of the infectious process and assess its sensitivity to antibacterial drugs.
6.7. PCR diagnostics
PCR diagnostics of the contents of the vagina and cervical canal is the most sensitive and specific method for assessing not only the qualitative, but also the quantitative composition of the flora.
This diagnostic method is relevant in the presence of hidden infections (chlamydia, mycoplasmosis, viral infections). It is these pathogens that often cause chronic oophoritis and salpingoophoritis.
6.8. Ultrasonography of the pelvic organs
Ultrasound criteria for inflammation in the ovaries and fallopian tubes are:
- 1Presence of fluid in the retrouterine space (in case of chronic oophoritis, the study is carried out only from the 4th to the 11th day of the menstrual cycle).
- 2Presence of fluid in the fallopian tubes.
- 3Thickening of the fallopian tubes.
- 4Increase in ovarian size.
- 5Visualization of tubo-ovarian formation, abscess.
Ultrasonography also evaluates the blood supply to the ovaries and fallopian tubes using Doppler. The presence of pathology is indicated by an increase in their blood supply due to vasodilation against the background of an inflammatory reaction.
6.9. Laparoscopy
Diagnostic laparoscopy is the most informative, but at the same time the most invasive and expensive method for verifying oophoritis and salpingitis. When it is performed under general anesthesia, a laparoscope is inserted into the abdominal cavity, which allows for visualization and assessment of the condition of the pelvic organs.
During laparoscopy, it is possible to remove tubo-ovarian formations, chromohidrotubation (assessment of the integrity of the fallopian tubes using fluid), assessment of the condition of the ovaries, detection and, if possible, dissection of adhesions.
As already mentioned, this procedure is a full-fledged operation and is more often performed either for inflammatory processes that do not respond to long-term conservative therapy, or when there are indications for emergency surgery.
Etiology
As we mentioned earlier, the cause of the disease can be a specific and nonspecific infection.
The most common pathogens are representatives of normal microflora:
- 1Staphylococcus.
- 2Streptococci.
- 3 Escherichia coli.
- 4Protea.
- 5Gardnerella vaginalis and many others.
With nonspecific inflammation, polymicrobial associations are more often found. In 15-20% of cases of oophoritis and salpingitis, the pathogen cannot be identified at all.
With specific inflammation, Chlamydia trachomatis (30%), Neisseria gonorrhoeae (50%), Mycoplasma hominis (in 30% of cases), and cytomegalovirus infection (diagnosed in 20.4% of cases) are most often detected.
Treatment tactics
The main goals of treatment for oophoritis are:
- 1Complete elimination of the pathogen.
- 2Preventing the process from becoming chronic (in acute oophoritis).
- 3 Elimination of pain syndrome.
- 4In case of exacerbation of a chronic process, its relief and achievement of remission.
- 5In case of chronic asymptomatic course – prevention of complications.
Severe disease with severe intoxication and lack of effect from outpatient treatment are indications for hospitalization (CDC Sexually Transmitted Diseases Treatment Guidelines, 2015).
Failure of conservative therapy in the hospital after 72 hours is an indication for surgery (level of evidence - IIC).
At the moment, the following regimens for the use of antibacterial drugs are recommended for the treatment of oophoritis and salpingoophoritis (see Table 1).
Table 1 - Schemes for the use of antibiotics for oophoritis and salpingo-oophoritis according to Russian clinical protocols and CDC recommendations. To view, expand the table
The basic principles that any of the above treatment regimens must meet are:
- 1Empirically prescribed combinations of antibacterial drugs must have a broad spectrum of action and be active against all possible pathogens.
- 2Empirical antibacterial therapy is prescribed only for acute inflammatory processes; for chronic oophoritis, treatment is prescribed only based on the results of bacteriological examination and PCR.
- 3Exacerbation of chronic oophoritis is treated according to the same principles as the acute process, with the prescription of empirical antibiotic therapy.
- 4All patients should be screened for sexually transmitted infections, including HIV (Level IVС).
- 5Patients with mild and moderate forms of the disease can be treated on an outpatient basis, provided that all doctor’s recommendations are strictly followed.
- 6The use of local forms of medications (suppositories, vaginal tablets) is ineffective in the treatment of oophoritis. Vaginal suppositories and ovulation are used only in the presence of concomitant colpitis, cervicitis or bacterial vaginosis.
- 7If allergic reactions to the administered drugs occur, their use should be stopped immediately and the regimen should be changed to one of the alternatives (Evidence level Ib, A).
- 8If there is no positive dynamics during therapy within 72 hours, the treatment regimen should be changed.
The effectiveness of therapy for acute oophoritis is assessed 72 hours after the start of treatment. At this point, the results of bacteriological examination and the sensitivity of identified microorganisms to prescribed antibacterial drugs are retrospectively assessed.
It must be remembered that for oophoritis, treatment at home with folk remedies and unconventional methods is unacceptable!
Without etiotropic treatment, the disease can be complicated by tubo-ovarian abscess, pelvioperitonitis, and infertility. Other complications, including chronic pelvic pain, ectopic pregnancy, tubal infertility (TFI), and IVF failure, may occur in up to 25% of patients with salpingitis and oophoritis.
Unilateral oophoritis
If one ovary is affected, left-sided oophoritis or right-sided oophoritis is diagnosed. The causes of the disease are the same: gynecological manipulations, infections of the genital and other organs, weak immunity (autoimmune oophoritis occurs), stress, hypothermia. Symptoms:
- pain in the lower abdomen (if left-sided oophoritis is present, the pain is localized on the left, if right-sided, the pain is localized on the right);
- elevated temperature, which is not affected by antipyretics;
- discharge;
- bleeding between periods;
- weakness, fatigue, irritability;
- pale skin;
- decreased libido.
Inflammation can move from the right tube to the left and vice versa. Right-sided oophoritis can be confused with appendicitis, so careful diagnosis is required.
Complications of bilateral lesions
The likelihood of complications with bilateral oophoritis is higher than with unilateral oophoritis. This is explained by the extensiveness of the inflammatory and infectious process, the difficulty of normalizing reproductive function due to damage to both ovaries. Possible complications of the disease:
- persistent pain syndrome;
- menstrual irregularities with lack of ovulation;
- amenorrhea;
- infertility;
- miscarriage;
- ovarian tumors and abscesses;
- spread of pathology to the nearest pelvic organs;
- decline in immunity;
- hormonal imbalance;
- adhesions in the genitals.
The longer bilateral oophoritis occurs, the higher the likelihood of developing negative health consequences. The most common complications occur in the chronic form of the pathology.
Bilateral oophoritis is an infectious disease that requires complex drug therapy. Lack of treatment for its acute and subacute forms often leads to the development of chronic oophoritis. Compliance with all doctor’s recommendations and regular examination by a gynecologist increases the chance of successful recovery.
Prevention of 2-sided oophoritis
After the main treatment has been carried out, patients need to follow simple preventive measures to avoid relapse of the disease.
- Use of barrier methods of contraception (condom) and avoidance of promiscuity. Seek medical help in a timely manner to prevent complications and the disease from becoming chronic. 3. An integrated approach to treatment, compliance with all doctor’s recommendations. 4. Preventing hypothermia in the autumn-winter period. 5. Strengthening the immune system with the help of special medications, vitamin complexes, as well as proper nutrition and daily routine.
Bilateral oophoritis - inflammation of both ovaries. Occurs as a result of extensive spread of infection throughout the body. It responds well to drug treatment when carried out in the first stages of the disease.