How do antibiotics work?
We recommend reading: How to take antibiotics: basic rules
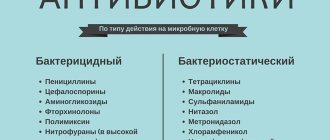
All antibacterial drugs can be divided into two large groups according to their effect on microorganisms:
- bactericidal - directly cause the death of microbes;
- bacteriostatic – prevent the proliferation of microorganisms. Unable to grow and reproduce, bacteria are destroyed by the immune system of a sick person.
Antibiotics exert their effects in many ways: some of them interfere with the synthesis of microbial nucleic acids; others interfere with the synthesis of bacterial cell walls, others disrupt protein synthesis, and others block the functions of respiratory enzymes.
Mechanism of action of antibiotics
What is an antibiotic
This is a group of drugs that have the ability to block protein synthesis and thereby inhibit the reproduction and growth of living cells. All types of antibiotics are used to treat infectious processes that are caused by different strains of bacteria: staphylococcus, streptococcus, meningococcus. The drug was first developed in 1928 by Alexander Fleming. Antibiotics of certain groups are prescribed for the treatment of oncological pathologies as part of combination chemotherapy. In modern terminology, this type of medication is often called antibacterial drugs.
Antibiotic groups
Despite the diversity of this group of drugs, all of them can be classified into several main types. This classification is based on chemical structure - drugs from the same group have a similar chemical formula, differing from each other in the presence or absence of certain molecular fragments.
The classification of antibiotics implies the presence of groups:
- Penicillin derivatives. This includes all drugs created on the basis of the very first antibiotic. In this group, the following subgroups or generations of penicillin drugs are distinguished:
- Natural benzylpenicillin, which is synthesized by fungi, and semi-synthetic drugs: methicillin, nafcillin.
- Synthetic drugs: carbpenicillin and ticarcillin, which have a wider spectrum of action.
- Mecillam and azlocillin, which have an even wider spectrum of action.
- Cephalosporins are the closest relatives of penicillins. The very first antibiotic of this group, cefazolin C, is produced by fungi of the genus Cephalosporium. Most drugs in this group have a bactericidal effect, that is, they kill microorganisms. There are several generations of cephalosporins:
- I generation: cefazolin, cephalexin, cefradine, etc.
- II generation: cefsulodin, cefamandole, cefuroxime.
- III generation: cefotaxime, ceftazidime, cefodizime.
- IV generation: cefpirom.
- V generation: ceftolozane, ceftopibrol.
The differences between the different groups are mainly in their effectiveness - later generations have a greater spectrum of action and are more effective. 1st and 2nd generation cephalosporins are now used extremely rarely in clinical practice, most of them are not even produced.
- Macrolides are drugs with a complex chemical structure that have a bacteriostatic effect on a wide range of microbes. Representatives: azithromycin, rovamycin, josamycin, leucomycin and a number of others. Macrolides are considered one of the safest antibacterial drugs - they can even be used by pregnant women. Azalides and ketolides are varieties of macorlides that have differences in the structure of the active molecules.
Another advantage of this group of drugs is that they are able to penetrate the cells of the human body, which makes them effective in the treatment of intracellular infections: chlamydia, mycoplasmosis.
- Aminoglycosides. Representatives: gentamicin, amikacin, kanamycin. Effective against a large number of aerobic gram-negative microorganisms. These drugs are considered the most toxic and can lead to quite serious complications. Used to treat urinary tract infections and furunculosis.
- Tetracyclines. These are mainly semi-synthetic and synthetic drugs, which include: tetracycline, doxycycline, minocycline. Effective against many bacteria. The disadvantage of these drugs is cross-resistance, that is, microorganisms that have developed resistance to one drug will be insensitive to others from this group.
- Fluoroquinolones. These are completely synthetic drugs that do not have their natural counterpart. All drugs in this group are divided into first generation (pefloxacin, ciprofloxacin, norfloxacin) and second generation (levofloxacin, moxifloxacin). They are most often used to treat infections of the ENT organs (otitis media, sinusitis) and respiratory tract infections (bronchitis, pneumonia).
- Lincosamides. This group includes the natural antibiotic lincomycin and its derivative clindamycin. They have both bacteriostatic and bactericidal effects, the effect depends on the concentration.
- Carbapenems. These are one of the most modern antibiotics that act on a large number of microorganisms. Drugs in this group belong to reserve antibiotics, that is, they are used in the most difficult cases when other drugs are ineffective. Representatives: imipenem, meropenem, ertapenem.
- Polymyxins. These are highly specialized drugs used to treat infections caused by Pseudomonas aeruginosa. Polymyxins include polymyxin M and B. The disadvantage of these drugs is their toxic effect on the nervous system and kidneys.
- Antituberculosis drugs. This is a separate group of drugs that have a pronounced effect on the tuberculosis bacillus. These include rifampicin, isoniazid and PAS. Other antibiotics are also used to treat tuberculosis, but only if resistance to the drugs mentioned has developed.
- Antifungal agents. This group includes drugs used to treat mycoses - fungal infections: amphothirecin B, nystatin, fluconazole.
Antibiotics - main types
The names of antibiotics differ because their main active ingredients differ. Based on this criterion, we distinguish the following types of antibiotics:
- β-lactams (penicillins, cephalosporins, monobactams, carbapenems, trinemms, penems and β-lactamase inhibitors);
- aminoglycosides, which are divided into streptidine aminoglycosides, deoxystreptamine aminoglycosides and aminocyclometols;
- peptide antibiotics (this group includes polypeptides, streptogramins, glycopeptides, lipopeptides, glycolypeptides, glycolipodeptides);
- tetracyclines in two forms - tetracycline and glycycycline;
- macrolides;
- lincosamides;
- amphenicolines;
- rifamycin;
- pleuromutilin;
- mupirocin;
- fusidic acid.
In addition, antifungal drugs and anti-tuberculosis drugs should not be confused with antibacterial antibiotics.
Antibiotics vary in their degree of absorption. Some of them are very well absorbed from the gastrointestinal tract, so they can be taken orally, while others must be administered intravenously or intramuscularly because they cannot be absorbed from the gastrointestinal tract. Intramuscular administration is mainly required for cephalosporin.
Another difference between antibiotics is how they are eliminated from the body. The vast majority of antibiotics are excreted in the urine; only a few are excreted in the bile.
In addition, antibiotics are also distinguished by the ease with which they penetrate tissue. Some of them quickly penetrate the body's tissues, while others do so extremely slowly.
The use of antibiotics and their choice in a particular case largely depends on the diseases from which the patient suffers. For example, a person suffering from kidney disease should not be prescribed a drug that is excreted in the urine, as they can cause various complications.
Methods of using antibiotics
Antibacterial drugs are available in different forms: tablets, powder from which an injection solution is prepared, ointments, drops, spray, syrup, suppositories. The main uses of antibiotics:
- Oral – taken by mouth. You can take the medicine in the form of a tablet, capsule, syrup or powder. The frequency of administration depends on the type of antibiotic, for example, azithromycin is taken once a day, and tetracycline is taken 4 times a day. For each type of antibiotic there are recommendations that indicate when it should be taken - before, during or after meals. The effectiveness of treatment and the severity of side effects depend on this. Antibiotics are sometimes prescribed to young children in syrup form - it is easier for children to drink the liquid than to swallow a tablet or capsule. In addition, the syrup can be sweetened to eliminate the unpleasant or bitter taste of the medicine itself.
- Injection - in the form of intramuscular or intravenous injections. With this method, the drug reaches the site of infection faster and is more active. The disadvantage of this method of administration is that the injection is painful. Injections are used for moderate and severe diseases.
Important: injections should only be given by a nurse in a clinic or hospital setting! It is strictly not recommended to inject antibiotics at home.
- Local - applying ointments or creams directly to the site of infection. This method of drug delivery is mainly used for skin infections - erysipelas, as well as in ophthalmology - for infections of the eye, for example, tetracycline ointment for conjunctivitis.
The route of administration is determined only by the doctor. In this case, many factors are taken into account: the absorption of the drug in the gastrointestinal tract, the state of the digestive system as a whole (in some diseases, the absorption rate decreases and the effectiveness of treatment decreases). Some drugs can only be administered one way.
When injecting, you need to know how to dissolve the powder. For example, Abactal can only be diluted with glucose, since when sodium chloride is used it is destroyed, which means the treatment will be ineffective.
Aminoglycosides (aminoglycoside aminocyclitols)
Methods of administration
- Injections and local.
Types of antibiotics
Streptomycin, Amikacin, Dibekacin, Gentamicin, Netilmicin, Sizomycin, Spectinomycin.
Indications for aminoglycosides
- Tuberculosis (streptomycin);
- Urinary tract infections (amikacin, dibekacin, gentamicin, netilmicin, sisomycin, spectinomycin).
Possible side effects of aminoglycosides
- Hearing problems;
- Nephrotoxicity (renal toxicity).
Main contraindications
- Allergy;
- Myasthenia.
Antibiotic sensitivity
Any organism sooner or later gets used to the harshest conditions. This statement is also true in relation to microorganisms - in response to prolonged exposure to antibiotics, microbes develop resistance to them. The concept of sensitivity to antibiotics was introduced into medical practice - the effectiveness with which a particular drug affects the pathogen.
Any prescription of antibiotics should be based on knowledge of the sensitivity of the pathogen. Ideally, before prescribing a drug, the doctor should conduct a sensitivity test and prescribe the most effective drug. But the time required to carry out such an analysis is, in the best case, several days, and during this time the infection can lead to the most disastrous result.
Petri dish for determining sensitivity to antibiotics
Therefore, in case of infection with an unknown pathogen, doctors prescribe drugs empirically - taking into account the most likely pathogen, with knowledge of the epidemiological situation in a particular region and medical institution. For this purpose, broad-spectrum antibiotics are used.
After performing a sensitivity test, the doctor has the opportunity to change the drug to a more effective one. The drug can be replaced if there is no effect from treatment for 3-5 days.
Etiotropic (targeted) prescription of antibiotics is more effective. At the same time, it becomes clear what caused the disease - using bacteriological research, the type of pathogen is established. Then the doctor selects a specific drug to which the microbe does not have resistance (resistance).
Inexpensive new generation antibiotics
The cost of new generation antibiotics is never low, so you can save money only by buying inexpensive analogues. They are produced on the basis of the same active ingredients, however, the degree of chemical purification of such drugs may be lower, and the auxiliary substances for their production are the cheapest.
You can replace some expensive antibiotics using the following table:
| Expensive drug | Inexpensive analogue | Average price of analogue, rub. |
| "Sumamed", "AzitRus" | "Azithromycin" | 130 |
| "Flemoxin Solutab", "Flemoklav Solutab" | "Amoxicillin" | 50 |
| "Rulid" | "Roxithromycin" | 120 |
Another way to save money is to buy older antibiotics, not the latest generation.
For example, in many cases the following proven antibacterial drugs can help out:
- "Erythromycin";
- "Ceftriaxone";
- "Bicillin";
- "Cefazolin";
- "Ampicillin."
If more than 72 hours have passed after starting treatment with inexpensive antibiotics, and no improvement is observed, you should urgently consult a doctor and change the drug.
Are antibiotics always effective?
Antibiotics only act on bacteria and fungi! Bacteria are considered single-celled microorganisms. There are several thousand species of bacteria, some of which coexist quite normally with humans—more than 20 species of bacteria live in the large intestine. Some bacteria are opportunistic - they cause disease only under certain conditions, for example, when they enter an atypical habitat. For example, very often prostatitis is caused by E. coli, which enters the prostate ascendingly from the rectum.
Please note: antibiotics are absolutely ineffective for viral diseases. Viruses are many times smaller than bacteria, and antibiotics simply do not have a point of application for their ability. That's why antibiotics have no effect on colds, since colds in 99% of cases are caused by viruses.
Antibiotics for coughs and bronchitis may be effective if they are caused by bacteria. Only a doctor can figure out what causes the disease - for this he prescribes blood tests, and, if necessary, an examination of sputum if it comes out.
Important: It is unacceptable to prescribe antibiotics to yourself! This will only lead to the fact that some of the pathogens will develop resistance, and next time the disease will be much more difficult to cure.
Of course, antibiotics are effective for sore throat - this disease is exclusively bacterial in nature, caused by streptococci or staphylococci. To treat sore throat, the simplest antibiotics are used - penicillin, erythromycin. The most important thing in the treatment of angina is compliance with the frequency of dosing and the duration of treatment - at least 7 days. You should not stop taking the medicine immediately after the onset of the condition, which is usually noted on the 3-4th day. True tonsillitis should not be confused with tonsillitis, which can be of viral origin.
Please note: untreated tonsillitis can cause acute rheumatic fever or glomerulonephritis!
Pneumonia (pneumonia) can be of either bacterial or viral origin. Bacteria cause pneumonia in 80% of cases, so even when prescribed empirically, antibiotics for pneumonia have a good effect. For viral pneumonia, antibiotics do not have a therapeutic effect, although they prevent the bacterial flora from joining the inflammatory process.
Tetracyclines
Methods of administration
- Injections, orally and locally.
Types of antibiotics
Doxycycline, Limecycline, Metacycline, Minocycline, Oxytetracycline, Tetracycline.
Indications for use
- Infections of the genital organs;
- Lung infections;
- Cholera;
- Typhus.
Side effects of tetracyclines
- Allergic reactions;
- Gastrointestinal toxicity.
Main contraindications
- Children under 8 years old;
- Pregnancy;
- Allergy.
Antibiotics and alcohol
Taking alcohol and antibiotics at the same time in a short period of time does not lead to anything good. Some drugs are broken down in the liver, just like alcohol. The presence of antibiotics and alcohol in the blood puts a strong strain on the liver - it simply does not have time to neutralize ethyl alcohol. As a result, the likelihood of developing unpleasant symptoms increases: nausea, vomiting, and intestinal disorders.
Important: a number of drugs interact with alcohol at the chemical level, as a result of which the therapeutic effect is directly reduced. These drugs include metronidazole, chloramphenicol, cefoperazone and a number of others. Concomitant use of alcohol and these drugs can not only reduce the therapeutic effect, but also lead to shortness of breath, seizures and death.
Of course, some antibiotics can be taken while drinking alcohol, but why risk your health? It is better to abstain from alcoholic beverages for a short time - the course of antibacterial therapy rarely exceeds 1.5-2 weeks.
Ansamycins (rifamycins)
Methods of administration
- Injections and orally.
Types of antibiotics
Rifamycin, Rifampicin.
Indications for use
- Rifamycin: Local application.
- Rifampicin: Tuberculosis.
Side effects of rifamycins
- Rifamycin: Allergic reactions.
- Gastrointestinal toxicity;
Main contraindications
- Allergy.
Antibiotics during pregnancy
Pregnant women suffer from infectious diseases no less often than everyone else. But treating pregnant women with antibiotics is very difficult. In the body of a pregnant woman, the fetus grows and develops - the unborn child, which is very sensitive to many chemicals. The entry of antibiotics into the developing body can provoke the development of fetal malformations and toxic damage to the central nervous system of the fetus.
During the first trimester, it is advisable to avoid the use of antibiotics altogether. In the second and third trimesters, their use is safer, but should also be limited, if possible.
A pregnant woman cannot refuse to prescribe antibiotics for the following diseases:
- Pneumonia;
- angina;
- pyelonephritis;
- infected wounds;
- sepsis;
- specific infections: brucellosis, borelliosis;
- sexually transmitted infections: syphilis, gonorrhea.
What antibiotics can be prescribed to a pregnant woman?
Penicillin, cephalosporin drugs, erythromycin, and josamycin have almost no effect on the fetus. Penicillin, although it passes through the placenta, does not have a negative effect on the fetus. Cephalosporin and other named drugs penetrate the placenta in extremely low concentrations and are not capable of harming the unborn child.
Conditionally safe drugs include metronidazole, gentamicin and azithromycin. They are prescribed only for health reasons, when the benefit to the woman outweighs the risk to the child. Such situations include severe pneumonia, sepsis, and other severe infections, in which, without antibiotics, a woman can simply die.
Which drugs should not be prescribed during pregnancy?
The following drugs should not be used in pregnant women:
- aminoglycosides - can lead to congenital deafness (with the exception of gentamicin);
- clarithromycin, roxithromycin - in experiments they had a toxic effect on animal embryos;
- fluoroquinolones;
- tetracycline – disrupts the formation of the skeletal system and teeth;
- chloramphenicol is dangerous in late pregnancy due to inhibition of bone marrow functions in the child.
For some antibacterial drugs there is no data on negative effects on the fetus. This is explained simply - experiments are not carried out on pregnant women to determine the toxicity of drugs. Experiments on animals do not allow us to exclude all negative effects with 100% certainty, since the metabolism of drugs in humans and animals can differ significantly.
It should be noted that before a planned pregnancy, you should also stop taking antibiotics or change your plans for conceiving. Some drugs have a cumulative effect - they can accumulate in a woman’s body, and for some time after the end of the course of treatment they are gradually metabolized and eliminated. It is recommended to become pregnant no earlier than 2-3 weeks after finishing taking antibiotics.
Sulfonamides
Methods of administration
- Injections, orally and locally.
Types of antibiotics
Sulfadiazine, Sulfamethoxazole, Sulfamoxole.
Indications for use
- Infections of the genital organs;
- Urinary tract infections;
- Infections of the ears, nose, throat;
- Lung infections.
Side effects of sulfonamides
- Allergic reactions;
- Kidney toxicity;
- Digestive disorders.
Main contraindications
- Pregnancy;
- Lactation;
- Allergy.
Consequences of taking antibiotics
The entry of antibiotics into the human body leads not only to the destruction of pathogenic bacteria. Like all foreign chemicals, antibiotics have a systemic effect - to one degree or another they affect all systems of the body.
There are several groups of side effects of antibiotics:
Allergic reactions
Almost any antibiotic can cause allergies. The severity of the reaction varies: rash on the body, Quincke's edema (angioedema), anaphylactic shock. While an allergic rash is practically harmless, anaphylactic shock can be fatal. The risk of shock is much higher with antibiotic injections, which is why injections should only be done in medical institutions - emergency care can be provided there.
Antibiotics and other antimicrobial drugs that cause cross-allergic reactions:
Toxic reactions
Antibiotics can damage many organs, but the liver is most susceptible to their effects - toxic hepatitis can occur during antibiotic therapy. Certain drugs have a selective toxic effect on other organs: aminoglycosides - on the hearing aid (cause deafness); tetracyclines inhibit bone growth in children.
Please note: the toxicity of a drug usually depends on its dose, but in case of individual intolerance, sometimes smaller doses are sufficient for the effect to appear.
Effects on the gastrointestinal tract
When taking certain antibiotics, patients often complain of stomach pain, nausea, vomiting, and stool disorders (diarrhea). These reactions are most often caused by the locally irritating effect of the drugs. The specific effect of antibiotics on the intestinal flora leads to functional disorders of its activity, which is most often accompanied by diarrhea. This condition is called antibiotic-associated diarrhea, which is popularly known as dysbiosis after antibiotics.
Other side effects
Other side effects include:
- immunosuppression;
- emergence of antibiotic-resistant strains of microorganisms;
- superinfection – a condition in which microbes resistant to a given antibiotic are activated, leading to the emergence of a new disease;
- violation of vitamin metabolism - caused by inhibition of the natural flora of the colon, which synthesizes some B vitamins;
- Jarisch-Herxheimer bacteriolysis is a reaction that occurs when using bactericidal drugs, when, as a result of the simultaneous death of a large number of bacteria, a large amount of toxins is released into the blood. The reaction is clinically similar to shock.
Anti-tuberculosis drugs
Methods of administration
- Orally.
Types of antibiotics
Ethambutol, Isoniazid, Pyrazinamide, Rifampicin, Rifabutin.
Indications for anti-tuberculosis drugs
- Tuberculosis.
Possible side effects
- Toxic liver damage;
- Neurological toxicity;
- Vision problems;
- Allergic reactions.
Main contraindications
- Optic neuritis;
- Liver failure;
- Kidney failure;
- Lactation;
- Allergy.
Can antibiotics be used prophylactically?
Self-education in the field of treatment has led to the fact that many patients, especially young mothers, try to prescribe themselves (or their child) an antibiotic at the slightest sign of a cold. Antibiotics do not have a prophylactic effect - they treat the cause of the disease, that is, they eliminate microorganisms, and in their absence, only side effects of the drugs appear.
There are a limited number of situations when antibiotics are administered before clinical manifestations of infection, in order to prevent it:
- surgery - in this case, an antibiotic present in the blood and tissues prevents the development of infection. As a rule, a single dose of the drug administered 30-40 minutes before the intervention is sufficient. Sometimes even after an appendectomy, antibiotics are not injected in the postoperative period. After “clean” surgical operations, antibiotics are not prescribed at all.
- major injuries or wounds (open fractures, soil contamination of the wound). In this case, it is absolutely obvious that an infection has entered the wound and it should be “crushed” before it manifests itself;
- emergency prevention of syphilis is carried out during unprotected sexual contact with a potentially sick person, as well as among health workers who have had the blood of an infected person or other biological fluid come into contact with the mucous membrane;
- penicillin can be prescribed to children to prevent rheumatic fever, which is a complication of tonsillitis.
Quinolones
Methods of administration
- Injections and orally.
Types of antibiotics
- Simple quinolones: Nalidixic acid, Oxolinic acid, Pipemidic acid, Rosoxacin, Flumekin.
- Fluoroquinolones: Pefloxacin, Ofloxacin, Ciprofloxacin, Lomefloxacin, Norfloxacin, Levofloxacin, Sparfloxacin, Moxifloxacin, Gemifloxacin, Gatifloxacin, Sitafloxacin, Trovafloxacin.
Indications for use
- Infections of the genital organs (quinolones, fluoroquinolones);
- Urinary tract infections (quinolones, fluoroquinolones);
- Intestinal infections (quinolones);
- Acute infections (fluoroquinolones).
Side effects of quinolones
- Quinolones: Allergic reactions;
- Hearing problems.
- Tendinitis;
Main contraindications
- Quinolones: Epilepsy;
- Pregnancy;
- Lactation;
- Allergenic child.
- Allergy;
Antibiotics for children
The use of antibiotics in children is generally no different from their use in other groups of people. For young children, pediatricians most often prescribe antibiotics in syrup. This dosage form is more convenient to take and, unlike injections, is completely painless. Older children may be prescribed antibiotics in tablets and capsules. In severe cases of infection, they switch to the parenteral route of administration - injections.
Important : the main feature in the use of antibiotics in pediatrics is the dosage - children are prescribed smaller doses, since the drug is calculated per kilogram of body weight.
Antibiotics are very effective drugs, but at the same time they have a large number of side effects. In order to be cured with their help and not harm your body, they should be taken only as prescribed by a doctor.
What types of antibiotics are there? In what cases is taking antibiotics necessary and in what cases is it dangerous? The main rules of antibiotic treatment are explained by pediatrician Dr. Komarovsky:
Gudkov Roman, resuscitator
98, total, today
( 175 votes, average: 4.72 out of 5)
Medicines for flatulence and bloating
Hexicon suppositories: instructions for use, indications and contraindications
Related Posts
Macrolides
Methods of administration
- Injections, orally and locally.
Types of antibiotics
Azithromycin, Roxithromycin, Clarithromycin, Dirithromycin, Flurithromycin, Erythromycin, Oleandomycin, Midecamycin, Spiramycin, Leukomycin, Josamycin.
Indications for use
- Infections of the genital organs;
- Ear, nose and throat infections;
- Lung infections.
Side effects of macrolides
- Allergic reactions;
- Gastrointestinal infection;
- Toxic liver damage.
Main contraindications
- Interactions with other drugs;
- Allergic reactions.
Groups of antibiotics according to the mechanism of inhibitory action on different cell structures
Antibiotics have a detrimental effect on the microbial cell. Their “targets” are the cell wall, cytoplasmic membrane, ribosomes and nucleotide.
Antibiotics that affect the cell wall
This group of drugs is represented by penicillins, cephalosporins and cycloserine.
Penicillins kill microbial cells by inhibiting the synthesis of peptidoglycan (murein), the main component of their cell membranes. This enzyme is produced only by growing cells.
Antibiotics that inhibit the synthesis of ribosomal proteins
The largest group of antibiotics that are produced by actinomycetes. It is represented by aminoglycosides, the tetracycline group, chloramphenicol, macrolides, etc.
Streptomycin (a group of aminoglycosides) has an antibacterial effect by blocking the 30S ribosomal subunit and disrupting the reading of genetic codons, resulting in the formation of polypeptides unnecessary for the microbe.
Tetracyclines disrupt the binding of aminoacyl-tRNA to the ribosome-matrix complex, as a result of which protein synthesis by ribosomes is suppressed.
In small bacteria, intracellular parasites, tetracyclines suppress the oxidation of glutamic acid, the starting product in energy metabolism reactions. Levomycetin, lincomycin and macrolides suppress the peptidyl transferase reaction with the 50 S ribosomal subunit, which leads to the cessation of protein synthesis by the bacterial cell.
Antibiotics that disrupt the function of the cytoplasmic membrane
The cytoplasmic membrane is located under the cell wall and is a lipoprotein (up to 30% lipids and up to 70% proteins). Antibacterial drugs that disrupt the function of the cytoplasmic membrane are represented by polyene antibiotics (Nystatin, Levorin and Amphotericin B) and Polymyxin. Polyene antibiotics are adsorbed on the cytoplasmic membrane of fungi and bind to its substance ergosterol. As a result of this process, the cell membrane loses macromolecules, which leads to cell dehydration and death.
Antibiotics that inhibit RNA polymerase
This group is represented by rifampicins, which are produced by actinomycetes. Rifampin inhibits the activity of DNA-dependent RNA polymerase, which leads to blocking protein synthesis when transferring information from DNA to RNA.
Rice. 10. Damage to the membrane of a bacterial cell by antibiotics leads to its death (computer modeling).
Rice. 11. The photo shows the moment of protein synthesis from amino acids by the ribosome (left) and a three-dimensional model of the ribosome of the bacterium Haloarcula marismortui (right). It is ribosomes that often become the “target” for many antibacterial drugs.
Rice. 12. The photo shows the moment of DNA doubling at the top and the RNA molecule at the bottom. Rifampin inhibits the activity of DNA-dependent RNA polymerase, which leads to blocking protein synthesis when transferring information from DNA to RNA.
Traditional medicine
Antibacterial drugs are synthetic, semi-synthetic, and also created on a natural basis. This means that for some remedies you can find analogues among traditional medicine recipes. In the early stages of the disease, treatment with natural antibiotics is very effective and safer than using tablets.
Basil
A natural antibacterial agent that can cleanse the body of various infections. They are eaten fresh in unlimited quantities - they can be added to salads, sandwiches or ready-made first and second courses. Basil should not be frozen, as its beneficial properties are lost and it becomes a common herbal seasoning for food.
- The medicinal decoction is effective for sore throat, gastritis and colitis. To prepare, you need to chop 4 tablespoons of leaves, pour a quarter liter of boiling water over them and let it brew for 15-20 minutes.
It is not recommended for women to abuse basil during pregnancy and lactation, as well as in the presence of hormonal disorders. People with a predisposition to blood thickening, diabetes mellitus, as well as those who have suffered a heart attack or stroke should include the herb in their diet with caution.
Cowberry
The sour berry, which grows in swamps, is widely used in cooking - compotes, fruit drinks, and jam are made from it. But few people know that lingonberries contain more than 60 beneficial vitamins and minerals, including benzoic acid, which is a natural bacteriostatic agent.
- Lingonberries are taken for inflammation of the urinary system, to reduce high fever, and also to restore the immune system after a severe or long-term illness.
The berry is most effective if consumed fresh, but fruit drinks, compotes and vitamin teas using it also help well. To enhance the anti-inflammatory effect, you can grind lingonberries into puree, mix with honey and take as a dietary supplement to dessert, tea or coffee.
It is not recommended to eat a lot of berries for people who have increased stomach acidity and other problems with the gastrointestinal tract.
Blueberry
Large blue berries are very tasty and are a source of vitamins. In addition, blueberries are a natural analogue of aspirin.
- It helps reduce temperature, relieves pain and blocks the development and spread of bacteria in the body. Blueberry compotes and fruit drinks are effective aids in the fight against inflammatory processes in the lungs and organs of the urinary system.
The maximum concentration of nutrients is found in fresh berries. If you want to stock up on blueberries for future use, you don’t have to freeze them - just grind the fruits into a pulp, mix with sugar and roll them into jars. When a cold occurs, this jam is used to make a fruit drink or use it as a dessert.
Ginger
There are legends about the miraculous properties of ginger in Japan. It is believed that the plant helps get rid of parasitic infestations, and therefore it is added to dishes eaten raw. By the way, this is one of the main reasons why such a famous dish as rolls is served with pickled ginger.
- Laboratory studies have proven that the root of the plant helps get rid of microbes and has anti-inflammatory and antipyretic properties. It is used to treat acute respiratory diseases, rhinitis, sore throat, and bronchitis.
Ginger is taken fresh, as an additive to tea, or pickled as a seasoning for a main dish - fish or meat.
Caution should be exercised when using ginger for people with diseases of the gastrointestinal tract, cardiovascular system, and allergy sufferers during exacerbations.
Cinnamon
This spice is popular in cooking - it is added to baked goods, it is used to decorate ready-made desserts, and coffee with cinnamon warms up well after a long walk on a frosty day. And few people know that cinnamon is the strongest natural antibiotic, which also activates the immune system and tones the body.
- Increased consumption of cinnamon is recommended for colds, migraines, flatulence and diarrhea. The aromatic spice has also been proven to help relieve depression and seasonal gloom.
Cinnamon can be taken as an additive to various drinks - tea, coffee, hot milk. A decoction of cinnamon sticks will help cope with sore throats when gargling systematically. And the alcohol infusion helps treat tuberculosis. It is recommended that women during pregnancy avoid premature birth, as well as people prone to internal bleeding, should not consume too much cinnamon in their diet.
When including natural antibiotics in your diet, you should remember that they are most effective in preventing various diseases, and not in treating them. If the patient’s condition rapidly worsens, then it is imperative to consult a doctor for traditional treatment.
Did you find the article useful? Share with your friends.
Facebook Twitter VKontakte Google+
How to choose antibiotics depending on the disease
When choosing an antibiotic, it is necessary to take into account three groups of factors that influence the duration, effectiveness and possible adverse reactions, namely:
- characteristics of the causative microorganism (variety, sensitivity to certain types of drugs, acquired resistance, localization in the body);
- state of human health (age, physiological characteristics of the gastrointestinal tract, state of the immune and excretory systems, likelihood of allergies);
- properties of antibiotics (absorption, minimum concentration for therapy, features of distribution in the body and effect on the pathogen).
ENT diseases
Most acute diseases of the ENT organs are caused by a viral infection, for which antibiotics are not required. If bacterial microflora joins the pathological process, which often happens with otitis media, tonsillitis, and sinusitis, then it is necessary to use broad-spectrum antibacterial drugs for oral administration, taking into account the likely strains of pathogens.
| Disease | Antibiotic names |
| Acute sinusitis | Amoxicillin, clavulanate, levofloxacin |
| Subacute and recurrent sinusitis | Amoxicillin, ceftriaxone, moxifloxacin |
| Sinusitis | Ceftazidime, cefepime, ticarcillin |
| Otitis | Clavulanate, ceftazidime, moxifloxacin |
| Tonsillitis (tonsillitis) | Amoxicillin, erythromycin, ceftriaxone, ciprofloxacin |
| Pharyngitis | Cefuroxime, azithromycin |
Respiratory tract infections
Effective antibiotics for the treatment of diseases of the respiratory system of a bacterial nature are the latest generation macrolides (azithromycin, clarithromycin), which have an immunomodulatory and anti-inflammatory effect, as well as the ability to concentrate as much as possible in the lung tissue and bronchial secretions.
If the disease is caused by viruses, for example, acute respiratory disease (ARI), flu, colds, bronchitis, then the use of antibiotics is not advisable, since it does not eliminate the symptoms, does not treat cough and high temperature.
Infections of the genitourinary system
For bacterial infection of the genitourinary system (acute and recurrent cystitis, urethritis), new generation broad-spectrum antibiotics such as pivmecillinam, nitrofurcntoin, co-trimoxazole are prescribed, and alternative drugs are ciprofloxacin, levofloxacin, norfloxacin - stronger drugs that are used for the development of resistance or the occurrence of an allergic reaction.
If the course of the disease is severe, as well as in the presence of acute pyelonephritis, stronger fluoroquinolones antibiotics are prescribed, and if gram-positive microorganisms are detected, cefotaxime, gentamicin, and amikacin should be used.
Eye diseases
The list of eye diseases that can develop as a result of the penetration of bacteria includes keratitis, dacryocystitis, conjunctivitis, blepharitis, corneal ulcer, barley.
To treat ophthalmic diseases of a bacterial nature, as well as to prevent postoperative infections in the eyes, antibiotics are used in the form of drops and ointments, which have a local effect directly at the site of infection.
| Active substance | Drug names |
| Fluoroquinolones | Floxal, Tsiprolet, Norfloxacin, L-optik, Uniflox, Signicef |
| Sulfonamides | Sulfacyl sodium |
| Erythromycin | Erythromycin ointment |
| Tetracyclines | Tetracycline ointment |
| Fusidic acid | Fucithalmic |
| Gentamicin and dexamethasone | Dexa-gentamicin (drops, ointment) |
If there is no improvement within 3 days after using antibacterial drops or ointments, you should choose a medicine with a different active ingredient.
Dentistry
The use of antibiotics in dentistry is intended in the case of acute purulent-inflammatory processes in the jaw and face (pericoronitis, periostitis, infected hilar cyst, abscess, periodontitis), as well as after surgical interventions, for example, tooth extraction.
Most often in dentistry, antibiotics are used in tablets or capsules, which have a systemic effect on the body:
Why are antibiotics harmful to the body?
The harm from the use of such dosage forms is due to the fact that they affect internal organs and systems. The negative effect is also caused by the decay products of pathogenic bacteria, which have a toxic effect on the organs and tissues of the body.
Liver after taking antibiotics
The liver is most susceptible to harmful effects, since the breakdown products of one or another antibacterial drug pass through it. The following phenomena may be observed:
- The appearance of inflammatory processes both in the liver itself and in the gall bladder.
- Negative impact on the metabolic process, which can lead to serious consequences.
- Pain syndrome occurs when the course of treatment with drugs of this group is prolonged.
- Gallbladder dysfunction.
Depending on the properties of the particular drug, other effects may occur.
Stomach and pancreas after taking antibiotics
Antibiotics affect the stomach and pancreas. The main harm is an increase in the acidity of gastric juice. Symptoms such as diarrhea, nausea and vomiting often occur when the dosage of drugs is exceeded.
How antibiotics affect the heart
Medicines can be harmful to the cardiovascular system. This usually manifests itself as:
- Jumps in blood pressure, both in the form of an increase and a decrease.
- Arrhythmias, pulse disorders.
Some drugs can increase the risk associated with dangerous situations, including cardiac arrest. This is relevant for people suffering from cardiovascular diseases.
Effect of antibiotics on the kidneys
The kidneys are the second organ most susceptible to the harmful effects of drugs of this type. Negative manifestations are expressed in:
- Renal dysfunction.
- Changes in urine parameters, its smell and color.
Antibiotics are harmful to the kidneys because they can have a destructive effect on the epithelium that covers the outside of the organ.
The effect of antibiotics on the nervous system
Certain medications may cause adverse reactions from the nervous system. These include:
- Lethargy and significant slowdown in reaction.
- Dysfunction of the vestibular apparatus, loss of coordination and dizziness.
- Deterioration of short-term memory and concentration.
Therefore, doctors recommend refraining from activities associated with these risks, including driving vehicles, during a course of treatment with certain antibacterial drugs.
Effect on blood and urine tests
Medicines in this group affect the main parameters of blood and urine, which must be taken into account when taking tests.
Plants with bactericidal action
Some plants also have the ability to destroy bacteria. They are less effective than antibiotics and act much slower, but are often used as an auxiliary treatment. The following plants have a bactericidal effect:
- aloe;
- black elderberry;
- burnet;
- celandine;
- plantain;
- sea kale.
Four generations of penicillins
In medical In practice today, four types of antibiotics from the penicillin group are used:
- The first generation is medicines of natural origin. This type of drug has a very narrow range of applications and is not very resistant to penicillinases (β-lactamases).
- The second and third generations are antibiotics that are much less susceptible to the destructive enzymes of bacteria, and therefore more effective. Treatment with their use can take place in a fairly short time.
- The fourth generation includes broad-spectrum penicillin antibiotics.
The most famous penicillins are the semisynthetic drugs Ampicillin, Carbenicillin, Azocillin, as well as the biosynthetic Benzylpenicillin and its durant forms (bicillins).
Local disinfectants
Such preparations, which have a bactericidal effect, are used to treat hands, equipment, medical instruments, floors and plumbing. Some of them are safe for the skin and are even used to treat infected wounds. They can be divided into several groups:
- chlorine preparations: bleach, “Chloramine”, “Javel”, “Chlorsept” and others;
- oxygen-containing products: hydrogen peroxide, “Hydroperit”;
- iodine preparations: alcohol solution, Lugol, Iodoform;
- acids and alkalis: salicylic acid, boric acid, sodium bicarbonate, ammonia;
- preparations containing metals - silver, copper, aluminum, lead and others: alum, lead water, zinc ointment, Xeroform, Lapis, Protorgol;
- as well as phenol, formalin, tar, Furacilin and others.
Synonyms of antibiotics
| INN/Composition | Trade names |
| 1 | 2 |
| ANTIBACTERIAL MEDICINES | |
| Penicillins | |
| Azlocillin | Azlocillin sodium salt, Securopen |
| Amoxicillin | Amoxicillin, Amoxicillin 1000 Stada International, Amoxicillin 250 Stada International, Amoxicillin trihydrate, Amoxicillin-Ratiopharm 250 TC, Amoxone, Amosin, Atoxylin, Ospamox, Ranoxil, Upsamox, Flemoxin Solutab, Hiconcil |
| Amoxicillin/clavulanate | Amoclan Hexal, Amoxiclav, Augmentin, Kuram, Moxiclav, Ranklav |
| Ampicillin | Ampirex, Ampicillin, Ampicillin injection, Ampicillin-AKOS, Ampicillin-KMP, Ampicillin sodium salt, Ampicillin trihydrate, Ampicillin trihydrate-Darnitsa, Zetsil, Pentrexil, Standacillin, Upsampi |
| Ampicillin/sulbactam (Sultamicillin) | Sulacillin, Sultasin, Unazin |
| Benzathine benzylpenicillin | Bicillin-1, Benzicillin-1, Retarpen, Extensillin |
| Benzathine benzylpenicillin/ Benzylpenicillin/ Benzylpenicillin procaine | Bicillin-3, Benzicillin-3, Dicillin-3 |
| Benzathine benzylpenicillin/Benzylpenicillin procaine | Bicillin-5, Benzicillin-5, Dicillin-5 |
| Benzylpenicillin | Benzylpenicillin-KMP, Benzylpenicillin potassium salt, Benzylpenicillin sodium salt, Benzylpenicillin sodium salt crystalline, Penicillin G sodium salt |
| Benzylpenicillin procaine | Benzylpenicillin novocaine salt, Procaine-benzylpenicillin, Procaine penicillin G3 Mega |
| Carbenicillin | Carbenicillin disodium salt |
| Oxacillin | Oxacillin-AKOS, Oxacillin sodium salt, Prostaflin |
| Piperacillin | Pipracil, Picillin |
| Piperacillin/tazobactam | Tazocin |
| Ticarcillin/clavulanate | Timentin |
| Phenoxymethylpenicillin | V-Penicillin Slovakofarm, Ospen, Ospen 750, Phenoxymethylpenicillin |
| Cephalosporins | |
| Cefadroxil | Biodroxil, Duracef |
| Cefazolin | Vulmizolin, Zolin, Zolfin, Intrazolin, Ifizol, Kefzol, Lizolin, Natsef, Orizolin, Prozolin, Reflin, Totacef, Cezolin, Cefazolin, Cefazolin Nycomed, Cefazolin-KMP, Cefazolin-Teva, Cefazolin sodium salt, Cefamezin, Cefaprim, Cefzolin |
| Cefaclor | Alphacet, Vertsef, Ceclor, Cefaclor Stada International |
| Cephalexin | Ospexin, Palitrex, Sporidex, Cefaclen, Cephalexin, Cephalexin-AKOS, Cephalexin-Teva |
| Cefepime | Maxipim |
| Cefixime | Suprax, Cefspan |
| Cefoperazone | Dardum, Medocef, Cephobid, Cefoperabol |
| Cefoperazone/sulbactam | Sulperazon |
| Cefotaxime | Duatax, Intrataxime, Kefotex, Clafobrine, Claforan, Liforan, Oritaxim, Talcef, Cetax, Cephabol, Cephantral, Cefosin, Cefotaxime, Cefotaxime "Biochemi", Cefotaxime sodium salt, Cefotaxime-KMP, Ceftax |
| Ceftazidime | Biotum, Vicef, Kefadim, Mirocef, Tizim, Fortazim, Fortum, Cephazid, Ceftazidime, Ceftazidime-M.J., Ceftidine |
| Ceftibuten | Tsedex |
| Ceftriaxone | Biotraxon, Ificef, KMP-Ceftriaxone sodium salt, Lendatsin, Longacef, Oframax, Rocephin, Torocef, Triaxone, Troxon, Forcef, Cefaxone, Cefatrin, Ceftriabol, Ceftriaxone, Ceftriaxone-AKOS, Ceftriaxone "Biochemi", Ceftriaxone-KMP, Ceftriaxone na tri salt |
| Cefuroxime | Aksetin, Zinacef, Ketocef, Multisef, Supero, Cefuxime, Cefurabol |
| Cefuroxime axetil | Zinnat |
| Carbapenems | |
| Imipenem/cilastatin | Tienam |
| Meropenem | Meronem |
| Monobactams | |
| Aztreons | Azaktam |
| Aminoglycosides | |
| Amikacin | Amikacin, Amikacin sulfate, Amikin, Amikosit, Likacin, Selemicin, Hematcin |
| Gentamicin | Gentamicin, Gentamicin, Gentamicin K, Gentamicin sulfate, Gentamicin-M.J., Gentamicin sulfate-Darnitsa, Gentina, Gentacyclol |
| Kanamycin | Kanamycin-AKOS, Kanamycin monosulfate, Kanamycin sulfate |
| Neomycin | Neomycin sulfate |
| Netilmicin | Netromycin |
| Streptomycin | Streptomycin, Streptomycin sulfate, Streptomycin-KMP, Streptomycin-calcium chloride complex |
| Tobramycin | Brulamycin, Nebcin, Tobramycin sulfate |
| Quinolones/fluoroquinolones | |
| Nalidixic acid | Nevigramon, Negro |
| Oxolinic acid | Gramurin, Dioxacin |
| Pipemidic acid | Palin, Pimidel, Pipegal, Pipem, Uropimid, Urotractin |
| Levofloxacin | Tavanik |
| Lomefloxacin | Lomflox, Maxaquin, Okatsin |
| Moxifloxacin | Avelox |
| Norfloxacin | Girablok, Loxon 400, Nolitsin, Norilet, Normax, Renor, Youtibid |
| Ofloxacin | Vero-Ofloxacin, Glaufos, Zanotsin, Quiroll, Oflo, Ofloxacin-ICN, Ofloxin 200, Oflomak, Tarivid, Tarifedrin, Taritsin |
| Pefloxacin | Abaktal, Pelox-400, Perti, Peflacine, Pefloxacin mesylate, Unikpef |
| Sparfloxacin | Respara, Sparflo |
| Ciprofloxacin | Aquacipro, Vero-Ciprofloxacin, Ificipro, Quintor, Quintor-250, Quipro, Liproquin, Medociprin, Microflox, Neofloxin, Procipro, Recipro, Siflox, Tseprova, Ciloxan, Ciplox, Tsiprinol, Tsiprobay, Tsiprobid, Tsiprovin 250, Tsiprodar, Tsiprolet, Tsipromed , Cipropane, Ciprosan, Ciprofloxacin, Ciprofloxacin Hydrochloride, Ciprocinal, Citeral, Cifloxinal, Cifran |
| Macrolides | |
| Azithromycin | Azivok, Azithromycin, Azithrocin, Zimax, Zitrolit, Sumazid, Sumamed, Sumamed forte |
| Josamycin | Vilprafen |
| Clarithromycin | Klabaks, Klacid, Klacid SR, Kriksan, Fromilid |
| Midecamycin | Macropen |
| Roxithromycin | BD-Rox, Brilid, Vero-Roxithromycin, Roximizan, Roxithromycin Lek, Roxide, Rulid, Rulitsin |
| Spiramycin | Rovamycin |
| Erythromycin | Synerit, Eomycin, Erythromycin, Erythromycin-Teva, Erythromycin phosphate, Ermitsed |
| Tetracyclines | |
| Doxycycline | Apo-Doxy, Vibramycin, Dovicin, Doxidar, Doxilan, Doxycycline, Doxycycline 100 Stada International, Doxycycline-AKOS, Doxycycline hydrochloride, Medomycin, Tetradox, Etidoksin, Unidox Solutab |
| Tetracycline | Tetracycline, Tetracycline hydrochloride |
| Lincosamides | |
| Clindamycin | Dalatsin, Dalatsin T, Dalatsin C, Dalatsin C phosphate, Klimitsin, Clindamycin, Klindafer |
| Lincomycin | KMP-Lincomycin, Lincomycin hydrochloride, Lincocin, Medoglycin, Neloren |
| Glycopeptides | |
| Vancomycin | Vancoled, Vancomycin, Vancocin, Vanmiksan, Editsin |
| Teicoplanin | Thargocid |
| Oxazolidinones | |
| Linezolid | Zyvox |
| Polymyxins | |
| Polymyxin B | Polymyxin B sulfate |
| Polymyxin M | Polymyxin M sulfate |
| Sulfonamides and co-trimoxazole | |
| Sulfadiazine | Sulfazine |
| Silver sulfadiazine | Dermazin, Sulfargin |
| Sulfadimethoxine | Sulfadimethoxine, Sulfadimethoxine-Darnitsa |
| Sulfadimidine | Sulfadimezin |
| Sulfalene | Sulfalene, Sulfalene-meglumine, Sulfalene-NS. |
| Silver sulfathiazole | Argosulfan |
| Co-trimoxazole | Bactrim, Bactrim Forte, Berlocid 240, Berlocid 480, Bicotrim, Biseptin, Biseptol, Dvaseptol, Duo-Septol, Co-Trimoxazole, Co-Trimoxazole-480, Co-Trimoxazole-ICN, Co-Trimoxazole-Acri, Co-Trimoxazole-Biosynthesis , Co-Trimoxazole-Rivofarm, Co-Trimoxazole-Teva, Cotripharm 480, Oriprim, Rancotrim, Septrin, Sumetrolim, Trimezol, Ziplin |
| Nitrofurans | |
| Nitrofurantoin | Furadonin |
| Nifuratel | McMirror |
| Nifuroxazide | Diastat, Nifuroxazide, Ersefuril |
| Furazidin | Furagin |
| Furazolidone | Furazolidone |
| Nitroimidazoles | |
| Metronidazole | Aquametro, Apo-Metronidazole, Klion, Medazol, Metrogyl, Metroxan, Metronidazole, Metronidazole IV Brown, Metronidazole hemisuccinate, Metronidazole Nycomed, Metronidazole-Teva, Trichopolum, Flagyl |
| Ornidazole | Tiberal |
| Secnidazole | Secnidazole |
| Tinidazole | Vero-Tinidazole, Tiniba, Tinidazole, Fazizhin |
| Drugs of other groups | |
| Dioxidine | Dioxidine |
| Mupirocin | Bactroban |
| Nitroxoline | 5-Nitrox, 5-NOK, Nitroxoline |
| Spectinomycin | Kirin, Trobitsin |
| Fosfomycin | Monural |
| Fusidic acid | Diethanolamine fusidate, Fusidic acid, Fuzidin, Fuzidin sodium, Fucithalmic |
| Chloramphenicol | Levomycetin, Levomycetin-Darnitsa, Levomycetin-KMP, Levomycetin stearate, Levomycetin succinate soluble, Levomycetin succinate sodium salt |
| ANTI-TUBERCULOSIS DRUGS | |
| Isoniazid | Izozid 200, Isoniazid, Isoniazid-Darnitsa, Isoniazid-NS. |
| Capreomycin | Kapastat |
| Para-aminosalicylic acid | Sodium paraaminosalicylate |
| Pyrazinamide | Linamide, Macroside, PZA-Siba, P.T.B., Pyrazinamide, Pyrazinamide-ACRI, Pyrazinamide-NIKKa, Pyrafate, Tibimid, Tizamid |
| Prothionamide | Petecha, Pronicide, Prothionamide, Prothionamide-ACRI |
| Rifabutin | Mycobutin |
| Rifampicin | Benemicin, Makos, R-Tsin, Rimaktan, Rimpacin, Risima, Rifadin, Rifamor, Rifampicin, Rifampicin-M.J., Tibitsin, Eremfat 600 |
| Rifampicin/isoniazid | Rifinag |
| Rifampicin/isoniazid/Pyridoxine | Rifacombe |
| Rifampicin/isoniazid/pyrazinamide | Rifater |
| Thioacetazone | Thioacetazone, Tibon |
| Ftivazid | Ftivazid |
| Cycloserine | Cycloserine |
| Ethambutol | Apbutol, Ekoks, Emb-Fatol 400, Li-butol, Mycobutol, Sural, Ebutol, Ethambusin, Ethambutol |
| Ethambutol/isoniazid/rifampicin | Mairin |
| Ethionamide | Myobit-250, Reginicide, Ethide, Ethionamide, Etomide |
| ANTIFUNGAL MEDICINES | |
| Amorolfine | Lotseril |
| Amphotericin B | Amphotericin B, Fungizone, Fungilin |
| Amphotericin B liposomal | Ambizom |
| Bifonazole | Bifonazole, Bifosin, Mikospor |
| Griseofulvin | Griseofulvin, Griseofulvin-Forte |
| Isoconazole | Gyno-Travogen, Travogen |
| Itraconazole | Kanazol, Orungal |
| Ketoconazole | Ketoconazole, Mycozoral, Nizoral, Oronazole |
| Clotrimazole | Antifungol, Imidil, Yenamazole 100, Candibene, Candide, Candide-B6, Kanesten, Kanizon, Clomazole, Clotrimazole, Clotrimazole-Acri, Menstan, Funginal, Funginal B |
| Levorin | Levoridon, Levorin, Levorin sodium salt |
| Miconazole | Ginezol 7, Gyno-Dactanol, Gyno-Mycosal, Dactanol, Daktarin, Mycozon |
| Natamycin | Pimafucin |
| Naftifin | Exoderil |
| Nystatin | Nystatin |
| Oxiconazole | Mifungar |
| Terbinafine | Lamisil, Lamisil Dermgel, Fungoterbin, Exifin |
| Fluconazole | Diflazon, Diflucan, Medoflucon, Mikomax, Mikosist, Fluconazole-Vero, Flucoral, Flukorik, Flusenil, Flucostat, Forkan |
| Ciclopirox | Batrafen |
| Econazole | Gyno-Pevaril, Pevaril, Ekalin, Ecodax |
| ANTIVIRAL MEDICINES | |
| Abacavir | Ziagen |
| Amprenavir | Agenerase |
| Acyclovir | Acigerpin, Acyclovir, Acyclovir Hexal, Acyclovir Stada International, Acyclovir-ACRI, Acyclovir-BMS, Acyclovir-NS, Acyclostad International, Atsik-Ophtal, Vero-Acyclovir, Vivorax, Herpevir, Herperax, Herpesin, Zovirax, Xorovir, Lovir , Medovir, Supraviran, Cyclovir, Cycloviral, Sedico, Citivir |
| Valaciclovir | Valtrex |
| Ganciclovir | Cymevene |
| Didanosine | Videx |
| Zalcitabine | Hivid |
| Zanamivir | Relenza |
| Zidovudine | Retrovir AZ and Ti, Timazid (Azidothymidine) |
| Indinavir | Crixivan |
| Interferon alpha | Alphaferon, Viferon, Human leukocyte interferon, Recombinant human interferon, Intron-A, Reaferon, Eberon alpha R |
| Interferon alpha-2a | Interal, Infagel, Lipint, Reaferon-ES, Reaferon-ES-Lipint, Roferon A |
| Interferon alpha-2b | Realdiron |
| Interferon alpha-n1 | Wellferon |
| Lamivudine | Zeffix, Epivir Tri Ti Si |
| Nevirapine | Viramune |
| Nelfinavir | Viracept |
| Oseltamivir | Tamiflu |
| Peginterferon alfa-2b | Pegintron |
| Ribavirin | Virazol, Rebetol, Ribavirin Meduna, Ribamidil |
| Rimantadine | Algirem, Polyrem, Remantadin, Rimantadin, Rimantadin-NS. |
| Saquinavir | Inviraza, Fortovaza |
| Stavudin | Zerit |
| Famciclovir | Famvir |
| Foscarnet | Gefin |
| Phosphazide | Nikavir |
| ANTIPROTOSAL MEDICINES | |
| Artemether | Artenam |
| Artesunate | Artesunate |
| Halofantrine | Galfan |
| Dehydroemetine | Dehydroemetine dihydrochloride |
| Diloxanide furoate | Furamide, Entamizole |
| Meglumine antimonate | Glucantim |
| Mefloquine | Lariam |
| Paromomycin | Monomycin |
| Pyrimethamine | Chloridine |
| Pyrimethamine/sulfadoxine | Fansidar |
| Primaquin | Primaquin |
| Quinine | Quinine hydrochloride, Quinine sulfate |
| Chloroquine | Delagil, Hingamin |
| Emetine | Emetine hydrochloride |
| Etofamide | Kythnos |
| ANTIHELMINTHIC MEDICINES | |
| Albendazole | Albendazole |
| Diethylcarbamazine | Ditrazine citrate |
| Levamisole | Decaris, Levamisole hydrochloride |
| Mebendazole | Vermox, Vero-Mebendazole, Vormin, Mebendazole, Telmox 100 |
| Niclosamide | Fenasal |
| Pyrantela pamoate | Helmintox, Nemocid, Pirantel |
| Praziquantel | Biltricide |
*Not registered in Russia
List of antibiotics in alphabetical order: classification, rules of administration
What types of antibiotics are there?
A question that is definitely worth asking yourself before taking medication. There is a common myth among Russian residents that many diseases can be cured by taking the same drug. Lack of awareness of people and mistrust of doctors can cause negative consequences. The Russian Union of Doctors is directing all its efforts to eliminate medical illiteracy among the population in order to prevent the spread of incorrect information.
There are several classifications of antibiotics. These are drugs with a universal scope of application. They are used when it is not possible to identify the exact cause of the disease. This list contains groups such as penicillins, tetracyclines, chloramphenicol, streptomycin, azithromycin and others. These medications are used in tablets and capsules, as well as in the form of injections.
Currently, thanks to purification of the composition, antibiotics with a wide range of applications are less toxic and cause less harm to the body.
The following names of antibiotics are included in the group of narrowly targeted drugs. These include the following medicines:
- Drugs used in the treatment of bronchitis. Identifying the causative agent of the infection takes seven days, so the patient is prescribed a centrally acting substance. It is similar to drugs of universal application, with the largest number of bacteria sensitive to it.
- Medicines for angina.
- Medicines for the treatment of flu and colds.
- In the treatment of sinusitis.
Some drugs, both broad and narrow spectrum, can be represented by the following list:
- drugs starting with the letter a: abactal, avelox, azactam, azivok, azlocillin, acametro, aquacipro, axetin, alfacet, amikacin, amikin, amikosit;
- drugs starting with the letter b: bactrin, bactroban, benzicillin, berlocid, bicotrim, biodroxil, biotraxon, biotum, biseptin, biseptol, bricillin, brilide;
- drugs starting with the letter D: dalacin, dardum, dvaseptol, dermazin, diastat, dioxocin, dioxidin, dicillin, dovicin, doxidar, doxilan, doxycycline;
- antibiotics starting with the letter z: zanocin, zetsil, zyvox, zimax, zinacef, zinnat, zitrolit, zolin, zolfin;
- antibiotics starting with the letter L: chloramphenicol, lendacin, lysolin, licacin, lincomycin hydrochloride, lincocin, liproquine, liforan, loxon, lomflox, longacef;
- antibiotics starting with the letter m: makmiror, macropen, maxaquin, maxipim, medazol, medoglycine, medomycin, medocef, medocyprin, meronem, metrogil, metroxan;
- antibiotics starting with the letter T: tavanic, tazocin, talcef, targocid, tarivid, tariffedrin, taritsin, tetradox, tetracycline, tiberal, tienam, tizin;
- antibiotics starting with the letter f: fasigin, phenoxymethylpenicillin, flagyl, flemoxin solutab, fortazim, fortum, forcef, fromilid, fusudic acid, fuzidin, furagin, furadonin;
- antibiotics starting with the letter c: cedex, cesolin, ceclor, ceprova, cetax, cephabol, cefazide, cefazolin, cephaclen, cefaxon, cephalexin, cephamezin.
List of antibiotics in alphabetical order - a list of all naturally occurring drugs in this series. In fact, not all of them may be needed in life. Seeing in front of you a list of antibiotics from A to Z, you need to know the classifications of drugs and their scope of action, in order to be able to quickly navigate at the right time.
Antibiotics are natural or semi-synthetic substances that lead to the destruction of harmful microorganisms or to a reduction in their growth. The herbal antibiotic is harmless to the body, is not addictive and has no side effects, but is inferior in strength to the synthetic drug.
The main problem with antibiotics is that the increase in the number of different drugs leads to an increase in the number of harmful bacteria that have the qualities necessary to resist these drugs.
Herbal and synthetic antibiotics differ in their composition and scope of application. We can say that harmful substances mutate due to the successful development of the medicinal industry, so the development of pharmaceuticals does not stand still, finding more and more new ways of protection.
All medications are prescribed by a doctor. Their purpose depends on the disease, its severity, and the group of medications used previously. Self-use of antibiotics is contraindicated, as this can lead to addiction, poisoning and other negative consequences.
The effect of medications on the body, manifested in any form, should be immediately reported to your doctor. If the drug does not achieve the desired effect and side effects appear, you should immediately inform your doctor.
Independently extending the time of antibiotic use and increasing or decreasing the dosage are also contraindicated. It is recommended to take antibiotics at the same time, since the concentration of substances in the blood should remain at the same level.
- biochemical;
- in accordance with their spectrum of action.
The spectrum of action refers to the list of types of bacteria that a given antibiotic actively affects. A broad-spectrum antibiotic acts on a large number of bacteria - bacilli, gram-positive and negative cocci.
- bactericidal agents that inhibit the synthesis of bacterial membranes:
- beta-lactams;
- glycopeptides;
- fosfomycins;
- antibiotics that inhibit protein synthesis by binding to the bacterial ribosome:
- macrolides;
- tetracyclines;
- aminoglycosides;
- chloramphenicol;
- antibacterial drugs whose action is based on inhibition of nucleic acid synthesis:
- quinolones;
- rifampicins;
- sulfonamides.
Considering the long and long-term confrontation between bacteria and bactericidal agents, all these types of drugs are represented by several generations. Each subsequent generation is distinguished by a more advanced degree of purity of the composition, which makes them less toxic to humans.
- "Avelox";
- "Azithromycin";
- "Amoxiclav";
- "Hepacef";
- "Doxycycline";
- "Clarithromycin";
- "Klacid";
- "Lincomycin";
- "Naklofen";
- "Rovamycin";
- "Roxithromycin";
- "Rulid";
- "Suprax";
- "Tazid";
- "Fuzidin";
- "Cephabol";
- "Cefodox";
- "Cefumax".
- "Amoxiclav";
- "Amoxil";
- "Amoxicillin";
- "Ampioks";
- "Arlet";
- "Grunamox";
- "Zitrolide";
- "Macropen";
- "Ospamox";
- "Rovamycin";
- "Cefazolin";
- "Cephalexin";
- "Cefotaxime";
- "Ceftriaxone";
- "Tsifran".
- For inflammatory diseases of the bronchi and lungs:
- "Amoxiclav";
- "Amoxicillin";
- "Ampicillin";
- "Augmentin";
- "Flemoxin Solutab".
- For the treatment of ENT diseases:
- "Zinacef";
- "Zinnat";
- "Cefutil".
- For bacterial respiratory tract infections:
- "Azithromycin";
- "Hemomycin."
What diseases and viruses can be treated with antibiotics?
Treatment with antibiotics becomes simply necessary when the disease passes into an inflammatory form.
Acute inflammatory diseases:
- Pneumonia.
- Bronchitis.
- Pleurisy.
- Sinusitis.
- Pyelonephritis.
- Follicular tonsillitis.
- Purulent otitis.
- Pharyngitis.
- Sinusitis.
- Salpingo-oophoritis.
- Urethritis.
Inflammatory diseases of the gastrointestinal tract:
- Gastritis.
- Peptic ulcer disease.
Bacterial infections causing poisoning and intoxication:
- Tetanus.
- Diphtheria.
- Botulism.
Antibiotics are also necessary during postoperative rehabilitation and for the treatment of chronic diseases (for example, cystitis).
Classification of chronic prostatitis
There are three main forms of chronic prostatitis:
- Chronic bacterial prostatitis is a lesion of the prostate gland associated with the development of pathogenic microflora. The symptoms are similar to those of acute prostatitis (pain when urinating, the presence of pus and blood in urine, and so on), but have more blurred (lightened) manifestations.
- Chronic prostatitis of a non-bacterial type is a type of damage to the male prostate gland, caused by reasons other than damage by pathogenic bacteria (for example, trauma or the formation of stones in the prostate), detected in the presence of infectious diseases. However, the name of the pathology concerns only the etiology of the disease, and not its course, since in the process of pathogenesis there is the development of pathogenic microflora identical to other types of prostatitis.
- Chronic asymptomatic prostatitis is a pathology of the prostate gland, caused by the presence of pathogenic microflora in the prostate area and proceeding asymptomatically or practically asymptomatically. Important! If this type of disease is suspected, usually detected during diagnosis based on the presence of pathological phenomena such as leukocyturia and/or bacteriuria, additional diagnostics must be performed. This is due to the similarity of the course of chronic asymptomatic prostatitis with prostate cancer.
Thus, regardless of the type of chronic prostatitis, the use of antibiotic drugs is recommended in all cases. The drugs that are the drugs of choice when prescribing therapeutic practice will be discussed below. And we need to start by offering readers a list of antibiotics for chronic prostatitis.
Reviews from men
Some reviews from men who treated prostatitis with antibiotics:
- Andrey, 42 years old: “During the next exacerbation of prostatitis, after tests, they prescribed Flemoxin Solutab and Vitaprost suppositories. After a course of such combination therapy, it became much easier, but, fearing a relapse, I myself drank propolis tincture for some time.”
- Oleg, 33 years old: “I had acute prostatitis, I underwent antibiotic therapy with Tetracycline tablets - the only one that worked, because in general there are few antibiotics that are suitable for treatment. I felt better almost immediately. The antibiotic helped quickly. The only thing is that I had heartburn in the morning, so I took medicine to restore the flora.”
- Dmitry, 39 years old: “Blurred symptoms in the form of problems with urination periodically bothered me, but I attributed them to exacerbations of hemorrhoids. As a result, a diagnosis of “asymptomatic bacterial prostatitis” was made. I was injected with Ceftriaxone for a long time, at the same time I put on Prostatilen suppositories, and at the end of the course, also suppositories with sea buckthorn. Overall the result is positive."
- Sergei, 40 years old: “During an exacerbation of chronic prostatitis, Gentamicin injections were prescribed, after which the leg and gluteal muscles ached greatly, but the effect was felt almost immediately. At the end of the course, I put on Uroprost suppositories and took immunomodulators. So far the prostate doesn’t remind me of itself, although six months have passed.”
To effectively cure a disease, it is necessary to carry out a diagnosis that will show the type of bacteria that cause the disease in a particular patient and their sensitivity to medications.
Based on the test results, the doctor decides what means to treat chronic prostatitis or the acute form of the disease. Prostatitis in men: first signs and treatment Prostate adenoma - what is it? Symptoms and treatment Prevention of prostate adenoma Pyelonephritis Urethritis in men, what is it? Symptoms and treatment of Cystitis in men
Types by chemical composition
The classification of antibiotics into groups in this case is as follows:
- Penicillins. This is the oldest group with which, in fact, the development of this direction of drug treatment began.
- Cephalosporins. This group is used very widely and is characterized by a high degree of resistance to the destructive action of β-lactamases. This is the name given to special enzymes secreted by pathogenic microorganisms.
- Macrolides. These are the safest and quite effective antibiotics.
- Tetracyclines. These drugs are used mainly to treat the respiratory system and urinary tract.
- Aminoglycosides. They have a very wide spectrum of action.
- Fluoroquinolones. Low-toxic bactericidal preparations.
These antibiotics are used most often in modern medicine. Besides them, there are some others: glycopeptides, polyenes, etc.
Where are such funds required?
A bactericidal effect is a property of some substances that a person constantly needs in economic and household activities. Most often, such preparations are used to disinfect premises in children's and medical institutions, public places and catering establishments. They are used to treat hands, dishes, and equipment. Bactericidal preparations are especially needed in medical institutions, where they are used constantly. Many housewives use such substances at home to treat their hands, plumbing fixtures and floors.
Medicine is also an area where bactericidal drugs are used very often. In addition to hand treatment, external antiseptics are used to cleanse wounds and fight infections of the skin and mucous membranes. Chemotherapy drugs are currently the only means of treating various infectious diseases caused by bacteria. The peculiarity of such drugs is that they destroy the cell walls of bacteria without affecting human cells.
Where did antibiotics come from?
Back in the 19th century, some scientists came up with the idea of fighting germs with the help of microbes of other species. For example, it was found that anthrax bacteria are killed by the influence of certain microorganisms. However, large-scale studies on this topic were not carried out at that time.
The impetus for the discovery of a magical weapon against microbes was an accident - Alexander Fleming, who was studying the properties of Staphylococcus aureus at that time, left his laboratory unattended for a month.
When he returned, he discovered on some plates with staphylococcal cultures the common green mold that appears on stale bread. The staphylococcal colonies that lived on these plates died from such proximity. The opening took place on September 3, 1928.
It took about 10 more years to isolate the active substance, penicillin, from moldy fungi of the genus Penicillum. This was done in 1938 by scientists Howard Florey and Ernst Chain. However, problems arose with the mass production of penicillin, as the common mold originally used in the experiments did not reproduce fast enough to produce large quantities of antibiotics. Through many searches and experiments, another form of mold was found that has extraordinary fertility - this golden mold was discovered by chance on a rotten cantaloupe melon.
The production of antibiotics on a large scale was established by 1943, since during the Second World War the need for such a medicine became simply enormous.
Prescription of universal antibiotics
Prescribing the described medications is justified in the following cases:
- Therapy is selected based on clinical symptoms, i.e. without identifying the pathogen. This is relevant for active illnesses, for example, meningitis - a person can die in just a couple of hours, so there is no time for complex measures.
- The infection has not one, but several sources.
- The microorganism that causes the disease is resistant to narrow-spectrum antibiotics.
- A set of preventive measures is carried out after the operation.
Penicillins
With the discovery of benzylpenicillin, scientists came to the conclusion that microorganisms could be killed. Despite the fact that, as they say, “a lot of water has already flown under the bridge,” this Soviet antibiotic has not been discounted. However, other penicillins were created:
- those that lose their qualities when passing through the acid-base environment of the gastrointestinal tract;
- those that do not lose their qualities when passing through the acid-base environment of the gastrointestinal tract.
Ampicillin and Amoxicillin
Special attention should be paid to antibiotics such as Ampicillin and Amoxicillin. In terms of action they are practically no different from each other. Able to cope with:
- gram-positive infections, in particular staphylococci, streptococci, enterococci, listeria;
- gram-negative infections, in particular, Escherichia coli and Haemophilus influenzae, salmonella, shigella, pathogens of whooping cough and gonorrhea.
But their pharmacological properties are different.
- bioavailability – no more than half;
- the period of elimination from the body is several hours.
The daily dose varies from 1000 to 2000 mg. Ampicillin, unlike Amoxicillin, can be administered parenterally. In this case, injections can be done both intramuscularly and intravenously.
In turn, Amoxicillin is characterized by:
- bioavailability – from 75 to 90%; does not depend on food intake;
- The half-life is several days.
The daily dose varies from 500 to 1000 mg. The duration of treatment is five to ten days.
Parenteral penicillins
Parenteral penicillins have one important advantage over Ampicillin and Amoxicillin - the ability to cope with Pseudomonas aeruginosa. It leads to the formation of purulent wounds and abscesses, and is also the cause of cystitis and enteritis - infections of the bladder and intestines, respectively.
Antibiotics - how to take them correctly
We often don't realize that the effects of antibiotics depend on how we take them. It's worth getting acquainted with some basic rules. Thanks to their observance, we will recover faster, and the infection will not recur.
The effectiveness of antibiotics depends on their type. Some agents target many types of bacteria, others target specific types. Recently a new drug has appeared that is taken for three days, and only one tablet per day. Patients often abuse this drug, leading to immunization. Treatment has to be repeated.
Not everyone knows that antibiotic treatment must be preceded by an antibiogram. This is a test that involves taking a swab from the site of a bacterial infection (throat, nose, sometimes blood or urine samples) and using special tools to check the effectiveness of the antibiotic. The wait for the test result can take up to 7 days.
Antibiotics should be taken one hour before meals or two hours after meals. Then the effectiveness of the drug will be maximum. Do not chew the tablets or pour out the contents of the capsule. Drugs must reach the stomach coated and in full, otherwise they will not be absorbed properly.
Do not drink antibiotics with milk or lemon juice, especially grapefruit juice.
The compounds contained in these drinks make it difficult for the drug to be absorbed from the gastrointestinal tract. Milk and its products have a particularly negative effect: kefir, cheese, yogurt. These foods have a lot of calcium, which reacts with the drug. Antibiotics should be taken two hours after consuming dairy products. Creamy juice combined with some antibiotics can cause serious changes in our body and can even cause hemorrhage. Antibiotics should be taken with plenty of still water.
Antibiotics should be taken at the prescribed time, and this principle cannot be abandoned. Typically, antibiotics are taken every 4, 6, or 8 hours. A constant level of drug concentration in the blood must be strictly maintained. When there is too little antibiotic, bacteria will begin to fight it.
If you are one hour late, take your pill and then return to your regular schedule. If the time gap is greater, this dose should be skipped. Never take a double dose.
Combination of antibiotics
If we use antibiotics, we should avoid alcohol. Sometimes this increases or prevents the body from absorbing the antibiotic, sometimes it increases side effects. During treatment with antibiotics, you should not take medications such as iron, calcium and medications used for hyperacidity of the stomach. All of them interfere with the absorption of antibiotics.
Do not stop antibiotic treatment after symptoms have subsided. The duration of treatment depends on the doctor's opinion, sometimes this process takes up to 10 days. If we stop treatment too early, the bacteria may multiply again and, in addition, they will be immune to this antibiotic.
It is important not to take the antibiotic yourself. Even doctors often make mistakes in diagnosis. Taking a random antibiotic can only harm us and weaken our immune system.
At the end of treatment, more precisely after taking the last dose of the drug, we must take care of restoring the natural bacterial flora of our body. Fermented milk products will help.
The best broad-spectrum antibiotics
Antibiotics refer to potent drugs that are of natural or artificial origin. The choice of drugs should be taken carefully; the instructions indicate what negative consequences antibiotics can cause. The list of the best remedies includes tablets that successfully treat the most common diseases.
Tetracycline
A broad-spectrum antibiotic inhibits the synthesis of the pathogen’s protein, causing the bacteria to die. It is taken for bronchitis, pneumonia, sore throat, cholecystitis, intestinal infections, gonorrhea, syphilis, conjunctivitis. Sold in the form of an ointment for external use and an eye ointment, which helps eliminate some problems locally.
Treatment is contraindicated in children under 8 years of age, with liver failure, leukemia, leukopenia, pregnancy and lactation. The drug is sold in packs of 10 and 20 pieces. The adult dosage is 250-500 mg three times a day, children take 25-50 mg for each kilogram of weight.
Advantages:
- It acts quickly and helps against many diseases;
- This is one of the cheapest antibiotics;
- Effectively treats persistent coughs and colds;
- Tablets can be bought at any pharmacy.
Flaws:
- Causes intestinal dysbiosis;
- Has a bitter taste;
- With long-term treatment, the color of tooth enamel changes;
- There are many contraindications and side effects.
The medicine destroys and inhibits the growth of bacteria, helping to cope with severe forms of the disease. With frequent use of such tablets, the patient develops addiction, so they should be prescribed by a doctor based on the patient’s age. This is not the best remedy for children.
Sumamed
The drug is available in the form of capsules, tablets and powder for suspension. It is prescribed for upper and lower respiratory tract infections, skin infections, stomach diseases, as well as utetritis and cervicitis.
Taking the medicine is prohibited for people with allergies to macrolides or impaired kidney and liver function. The adult dosage is 500 mg once a day, therapy is carried out for three days. Children from 3 to 12 years old are prescribed medicine at the rate of 10 mg per kilogram of weight. A suspension is used to treat infection in infants.
Advantages:
- Improves condition on the first day;
- Short course of admission;
- Just three pills for recovery;
- The capsules are easy to swallow.
Flaws:
- May cause severe allergies;
- Unpleasant taste;
- It takes a long time to be eliminated from the body.
After taking the drug, you may experience nausea, dizziness, headache, drowsiness, nervousness, and sometimes loss of taste. Flatulence, diarrhea, and bloating are very often observed; this is due to a violation of the intestinal microflora. To avoid this, doctors recommend additionally taking medications containing lacto and bifidobacteria.
Augmentin
The drug in low dosage treats skin infections, soft tissue infections and tonsillitis. High dosages are used for otitis media, sinusitis, infections of bones and joints, and disorders of the urinary tract and lower respiratory tract.
Augmentin belongs to the group of penicillins, it contains amoxicillin and clavulanic acid. The medicine is sold in the form of tablets and powder for suspension. A special form of antibiotic for injection is also available for sale. The dosage is determined by the doctor based on the patient’s weight and the severity of the disease.
Advantages:
- Allowed for breastfeeding;
- Contains clavulanic acid;
- A short period of time is accepted;
- Available in the form of a suspension.
Flaws:
- Short shelf life;
- Many side effects;
- High cost of the drug;
- Large tablet size.
Due to the content of clavulanic acid, the drug can act on a large number of bacteria. The minimum course of therapy is five days. Adults and children over 12 years of age take one tablet three times a day. In infancy, a dosage of 20 mg per day per kilogram is used.