Chronic and acute tracheobronchitis: ICD-10, symptoms and treatment.
The lower respiratory tract consists of the trachea, bronchi and bronchioles.
Inflammation of the mucous tissue of these organs, caused by a virus or infection, is diagnosed as acute tracheobronchitis.
The signs and treatment of the contagious stage of the disease differ from chronic tracheobronchitis, which can be accompanied by bronchial asthma, emphysema and difficulty breathing for more than three months a year.
Acute tracheobronchitis often occurs as a complication of respiratory and other diseases caused by a viral infection (influenza, measles, whooping cough, adenovirus).
Pathogens can be streptococcus, staphylococcus.
Chronic tracheobronchitis develops due to complications of the disease, against the background of weak immunity, poor lifestyle, or when the patient is prone to asthma.
- International classification ICD 10
- General characteristics of the disease
- Causes of chronic tracheobronchitis
- Acute tracheobronchitis
- Chronic tracheobronchitis
- Allergic tracheobronchitis
- Diagnosis of tracheobronchitis
- Treatment of tracheobronchitis
- Prevention of tracheobronchitis
What is tracheobronchitis
According to ICD-10, this disease has code J 06-J 21. It is deciphered as a complex of interconnected diseases that occur at the same time - bronchitis and tracheitis. The pathology is a chronic or acute inflammation of the epithelium of the tracheobronchial tree with its infiltration and hyperemia. The process involves the trachea, bronchi and their processes (bronchioles), and intact lung tissue. The disease has a severe course, so treatment is often carried out in a hospital setting.
Pathogens
The pathology may be bacterial or viral in nature . In the first case, the cause of the disease is pathogenic bacteria that enter the body in different ways. Among these microorganisms, tracheobronchitis is caused by:
- hemophilus influenzae;
- staphylococci;
- mycoplasma;
- streptococci;
- pneumococci;
- Moraxella;
- Klebsiella;
- pseudomonas.
Tracheid bronchitis can develop as a secondary disease against the background of not only bacterial, but also viral pathologies. This happens when the body is damaged:
- influenza virus;
- parainfluenza;
- adenovirus;
- respiratory syncytial virus;
- coronavirus;
- rhinovirus.
Routes of infection
A person suffering from viral or bacterial tracheobronchitis can infect others if they come into close contact with them. Routes of infection with this pathology:
- Aerogenic (airborne). This is the main route of infection, observed in 95-97% of cases. When coughing and talking, the patient releases drops of saliva and phlegm, which remain in the air in the form of an aerosol.
- Bronchogenic. Another common route of infection of lung tissue. The spread of microorganisms occurs during microaspiration of the contents of the oropharynx. This leads to intubation tracheobronchitis, which is observed in 35-40% of patients.
- Hematogenous. With this method of infection, viral particles from the source of inflammation enter the patient’s bloodstream and spread throughout the body.
Forms
- acute tracheobronchitis. This form of the disease lasts for 10 days. Throughout this period, the patient is contagious to others, so he must be isolated. Acute tracheobronchitis is characterized by extensive inflammation of the mucous membrane of the trachea and throat;
- protracted form of tracheobronchitis. The development of this pathology is indicated if the symptoms of the disease do not disappear within a month;
- chronic tracheobronchitis. The duration of the illness is more than 3 months. Often this pathology is diagnosed in people who are too fond of smoking. Together with chronic tracheobronchitis, other respiratory tract pathologies can develop;
- allergic tracheobronchitis. This form progresses due to the penetration of various allergens into the human body. Its peculiarity lies in the fact that the patient’s condition does not worsen, but there is a rapid manifestation of symptoms: hoarse voice, severe itching, cough. Allergic tracheobronchitis is more susceptible to people who live in unfavorable areas where there are many toxic substances in the atmosphere;
- infectious-allergic tracheobronchitis. In this case, the allergic form of the pathology begins to progress against the background of the infectious one.
Types and forms of the disease
Tracheobronchitis has several classifications. According to the nature of its course, it is divided into acute and chronic . In the first case, bronchotracheitis lasts about 10 days and is characterized by a more pronounced intoxication syndrome. The acute form develops as a secondary pathology against the background of:
- measles;
- whooping cough;
- typhoid fever;
- pneumonia;
- ORZ.
In terms of symptoms and the nature of its course, its protracted form is very similar to acute tracheid bronchitis. It differs in that it lasts a little longer. The chronic form of the disease lasts for an even longer period. It can also be accompanied by other pathologies of the ENT organs. Taking into account the nature of the disease, tracheobronchitis is divided into two more subtypes:
- Allergic. Infection occurs when allergens enter the respiratory organs.
- Infectious-allergic. In this case, the respiratory organs are affected by allergens against the background of another ENT infection.
Acute tracheobronchitis
In most patients, this form of the disease develops as a complication of acute respiratory infection . In this case, tracheobronchitis is indicated by the symptoms of nasopharyngitis:
- nasal congestion;
- sore throat;
- rhinorrhea;
- dryness in the nasopharynx;
- hoarseness of voice;
- pain when swallowing.
As the infection progresses, it spreads to the lower respiratory tract. This is indicated by painful and raw sensations in the chest, a dry and hysterical cough. What happens next is:
- Breathing becomes harsh.
- On auscultation, dry rales begin to be heard.
- After 2-3 days, the cough becomes productive and wet.
- The separation of mucopurulent or mucous sputum begins.
- The low-grade fever persists for several days.
- After 8-10 days, recovery occurs.
- A residual cough may persist for up to 3 weeks.
Protracted form of the acute stage
If the above symptoms do not go away within a month, then the patient has a protracted form of tracheid bronchitis. More often it occurs as a result of untimely or improper treatment of an acute type of disease. The patient may suffer from a severe cough and fever. The fight against this form takes longer, since gas exchange in the lungs is impaired. If etiotropic therapy for acute bronchotracheitis lasts 7-10 days, then protracted bronchotracheitis is treated on average for 15-30 days.
Chronic tracheobronchitis
This form of tracheid bronchitis is characterized by a relapsing course. During an exacerbation, symptoms are more pronounced. In the acute phase there are:
- low-grade fever;
- sweating;
- cough of varying intensity;
- shortness of breath at rest and during exercise;
- wheezing;
- weakness.
When coughing, sputum of different colors and consistency may be produced, more often purulent or serous-purulent. During remission, patients note shortness of breath during physical exertion and periodic coughing. Emphysema or obstructive pulmonary disease are possible as complications of the disease. Chronic tracheobronchitis is more often observed in people who work in high dust conditions, for example, miners or employees of metallurgical shops. The same applies to people with bad habits such as alcoholism and smoking.
Allergic (obstruction)
This form of the disease is accompanied by acute inflammatory damage to the respiratory tract due to contact with allergens. It most often affects people living in areas with high levels of toxic substances in the atmosphere. A characteristic symptom is a cough - dry, with mucous discharge. It is combined with the following characteristics:
- skin itching;
- rhinitis;
- decreased appetite;
- lethargy;
- lacrimation.
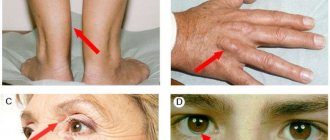
Allergic inflammation is indicated by a feeling of pain and burning behind the sternum. The temperature remains normal; attacks of suffocation may occur due to bronchial obstruction. Allergic tracheobronchitis can be combined with hay fever, atopic dermatitis and other allergies. When examining blood, specialists detect an increased level of eosinophils.
Infectious-allergic
This form of damage is characterized by a combination of symptoms of infectious and allergic tracheobronchitis. The cause is microbes: staphylococci, streptococci, pneumococci. Allergies develop as a reaction to the proliferation of these microorganisms. The disease is accompanied by:
- soreness behind the sternum;
- increased body temperature;
- dry cough, which becomes wet over time;
- wheezing when breathing, it becomes harder.
The disease often develops in winter, and relapses are observed in smokers and people prone to pathologies of the ENT organs. If the disease develops into a protracted form, then other pathologies may join: bronchiectasis, sinusitis, allergic reactions. Hypoxia and blockage of small bronchi develop as complications of the disease. They occur only in the absence of proper therapy.
Symptoms of tracheobronchitis
Clinical signs of the disease largely depend on the cause of the pathological process.
General symptoms of tracheobronchitis in adults are presented in the table:
| Type of tracheobronchitis | Cough and runny nose | Sputum | General malaise and intoxication | Body temperature | |
| Spicy | Dry, paroxysmal, which over time becomes moist with the release of a small amount of sputum. Often a cough occurs simultaneously with profuse rhinorrhea (serous or mucous discharge from the nose) | Absent at first, as the disease progresses it is released in a small amount of mucous nature | The patient complains of general weakness and lethargy, nausea, drowsiness, severe pain in the chest, especially during and after a coughing attack. | Increases to 38.0-39.0 degrees, lasts 3-4 days, after which it returns to normal | |
| Chronic | With an exacerbation of the disease, a dry cough in the form of an attack, worsening at night. | After a coughing attack, a small amount of viscous sputum of a mucous or mucopurulent nature is released, sometimes with an unpleasant odor | Complaints of constant pain in the chest, dizziness after a coughing attack | As a rule, it remains within normal limits, but during periods of exacerbation it can rise to 38 degrees | |
| Allergic | It occurs suddenly without visible symptoms or signs of a cold. It is characterized by a paroxysmal course; during coughing, the veins in the patient’s neck swell, the face turns red, and at the end of the attacks, vomiting may occur | Practically not excreted or present in small amounts of mucous nature, glassy, thick, viscous | Complaints of chest pain after a coughing attack and difficulty breathing | Remains within normal limits | |
Important! Do not self-medicate and do not start taking any medications for tracheobronchitis without examination and examination - this makes it difficult to make a correct diagnosis and can lead to a number of complications, especially in the allergic form of the pathology.
When the larynx is involved in the pathological process, laryngotracheobronchitis develops, which is characterized by the following clinical symptoms:
- hoarseness or complete aphonia (loss of voice);
- obsessive cough in the form of an attack, reminiscent of a dog barking;
- complaints of difficulty breathing and a feeling of a lump in the throat;
- shortness of breath and blueness of the fingertips, ears and nose during a coughing attack.
Tracheitis occurring simultaneously with laryngitis and bronchitis can lead to spasm of the larynx or the development of stenosis. Children and patients prone to allergic reactions are especially susceptible to this complication.
Causes of tracheobronchitis
The main cause of the development of the disease is bacteria and viruses that disrupt the microflora of the mucous membrane. They enter the body in different ways: bronchogenic, aerogenic, hematogenous. Activation of viral or bacterial flora occurs as a result of deterioration of the body's protective functions. A separate risk group includes people who often suffer from mood swings and nervous fatigue. These include women during pregnancy. Regardless of the risk group, weakened immunity occurs as a result of:
- hypothermia;
- trauma to the tracheal mucosa;
- sinusitis, pharyngitis;
- poisoning with iodide or potassium bromide;
- drinking and smoking;
- vitamin deficiency and hypovitaminosis;
- long-term artificial ventilation;
- heredity;
- inflammation of the tonsils - tonsillitis;
- bad environment;
- deformities of the nose or chest;
- asthenia of the body;
- poor nutrition;
- contact with patients.
General characteristics of the disease
The acute form of tracheobronchitis develops abruptly and is most often contagious, since the causative agent is a bacterial infection.
Without complications, treatment lasts from 6-7 days to two weeks. The disease can be dangerous for weakened patients: children, the elderly, women during pregnancy. To avoid complications, treatment for tracheobronchitis should be started as soon as possible.
The most obvious and unpleasant symptom of the disease is a hacking cough without sputum, or a cough in which a lot of yellow and white purulent mucus is coughed up. As a result of a convulsive, sharp cough, the sternum and abdominal muscles begin to ache.
Tracheobronchitis in children is accompanied by a runny nose, sore throat and fever. Inflammation of the mucous membrane can rise to the upper respiratory tract or fall below, causing complications in the lungs, including pneumonia.
You can treat tracheobronchitis at home with:
- expectorants, painkillers, sputum thinners;
- sulfa drugs;
- antibiotics;
- physiotherapeutic procedures.
Symptoms and signs
Symptoms common to all forms of tracheobronchitis are a strong persistent cough, heavy inhalations and harsh breathing. When coughing, sputum with pus is released and pain in the sternum is observed. The acute form causes a number of unpleasant symptoms:
- fever;
- dysphonia;
- hoarseness;
- difficulty breathing in and out;
- wheezing, harsh and noisy breathing;
- dry mouth;
- blue lips;
- heartache.
Article on the topic: Acute obstructive bronchitis
In a chronic course, the symptoms of tracheobronchitis are not so pronounced. The cough remains persistent, prolonged and paroxysmal. Against this background, shortness of breath, wheezing, burning and aching pain in the chest appear. The following signs also indicate chronic tracheobronchitis:
- sleep disturbance;
- hypertrophy or atrophy of the tracheal mucosa;
- serous-purulent sputum in the morning;
- “hoarse” voice and laryngitis.
The infectious-allergic form is distinguished by the symptoms of two types of tracheid bronchitis, since the body develops a negative reaction to the action of microbes. Allergic tracheid bronchitis lasts until the allergen is eliminated from the body. After this, the inflammatory signs completely disappear. A characteristic symptom is breathing problems when lying down. Other clinical signs of the allergic form of the disease:
- apathy;
- loss of appetite;
- low-grade fever;
- dry cough and pain in the diaphragm;
- drowsiness, lethargy;
- decreased performance.
Chronic tracheobronchitis
Manifestations of chronic bronchitis are individual and depend on the cause of the disease.
Symptoms of chronic tracheobronchitis
- Chronic dry cough.
- Cough with sputum.
- Excess mucus in the upper respiratory tract.
- Moderate chest pain.
- Frequent rise in temperature to 37‒37.5°.
- Constant cold in the cold season, which disappears with the arrival of warmth.
- Lack of air at rest.
- Shortness of breath and chest pain during exercise.
- Blueness of the skin (cyanosis).
- Thickening of the fingers in the area of the nail plate.
- Recurrent diseases of acute tracheobronchitis.
- Fatigue and malaise.
Possible complications
- Acute bronchitis.
- Bronchopneumonia.
- Bronchiectasis.
- Increase in heart size.
- Emphysema.
- Increased risk of mortality.
Diagnosis of the disease
Tracheobronchitis is a serious disease that requires preliminary diagnosis. When the first signs appear, you need to contact a pulmonologist and allergist. During the examination, the doctor performs percussion and auscultation to listen to the lungs. To confirm, the specialist prescribes a number of laboratory and instrumental diagnostic procedures, such as:
- Tracheobronchoscopy. This study is endoscopic, and therefore reveals purulent secretion, fibrinous deposits, hyperemia and ulceration of the mucosa.
- X-ray of the lungs. This study is not very informative, but if a chronic form is suspected, it helps to identify the imprint of pathology on the pulmonary pattern.
- Microscopic examination of sputum with identification of atypical cells. They help confirm the diagnosis and differentiate pathology from lung cancer, tuberculosis, and bronchial asthma.
- Sputum culture. The material is taken to identify the bacterial pathogen.
- Skin allergy tests. Their results confirm the allergic genesis of the disease.
Causes of inflammation of the tracheal mucosa
Acute tracheobronchitis is caused by several reasons:
- penetration of bacterial or viral infection;
- colds;
- smoking;
- bad ecology;
- inhalation of harmful substances at work;
The disease is easier to tolerate than bronchitis, but it all depends on the patient’s immunity. Sometimes shortness of breath and wheezing may occur. It is important to begin treating this disease in time so that it does not begin to manifest itself in a chronic form.
Treatment of tracheobronchitis in adults
Uncomplicated forms of tracheid bronchitis are treated at home. In acute cases of pathology, the patient is prescribed bed rest. The patient must limit contact with others, and the room in which he is located must be regularly ventilated. In case of minor ailments, while following the regimen, the patient is prescribed physiotherapeutic procedures: inhalations and electrophoresis. Rubbing with warming ointments, warm compresses, and mustard plasters help restore the drainage function of the bronchi.
Tracheobronchitis of severe form or with complications is treated in an inpatient setting in the pulmonology department. The treatment regimen includes the following activities:
- Taking antitussives in the first days when you have a severe cough. They use drugs such as Butamirate, Codeine, Prenoxydiazine.
- Alkaline inhalations. Promotes the removal of sputum.
- Taking mucolytic and expectorant drugs, such as Mucaltin, Ambroxol, Lazolvan, Thermopsis.
Depending on the nature of the disease, antibacterial, antiviral or antihistamine drugs are prescribed. Vitamins and immunomodulators help increase the overall resistance of the body. Additions to the general treatment regimen include:
- Physiotherapeutic procedures. These include vibration and percussion massage, UV therapy, electrophoresis on the chest, laser therapy, halotherapy, and breathing exercises.
- Traditional methods. They are used only as an adjuvant treatment. Traditional treatment consists of inhalation, gargling, applying compresses and mustard plasters, and drinking special vitamin teas.
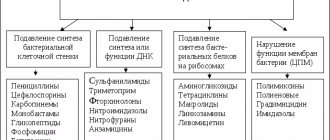
Antibacterial or antiviral therapy
Tracheobronchitis can be viral or bacterial in nature. For this reason , timely diagnosis to identify the causative agent of the disease is very important . To cure it, it is necessary to influence it with the help of certain drugs:
- Antibacterial. They are prescribed if tests have determined that the cause of the disease is bacteria. Certain drugs are selected taking into account the sensitivity of pathogenic microorganisms to them, which is detected during bacterial culture. Antibiotics are used from the groups of cephalosporins, penicillins, fluoroquinolones: Augmentin, Oxacillin, Amoxicillin. Local antibacterial agents are also used, for example, the drug for irrigation of the mucous membranes Bioparox.
- Antivirus. Prescribed for viral nature of the pathology. These drugs are ineffective against bacteria. Examples are Interferon, Isoprinosine, Kagocel, Arbidol.
Symptomatic therapy
Tracheobronchitis is treated not only with antibacterial or antiviral drugs. Additionally, symptomatic therapy is carried out. From its name you can understand that this type of treatment helps to get rid of not the cause of the disease, but its unpleasant symptoms. For tracheid bronchitis, the following drugs are used for this purpose:
- Expectorants. These are mucolytic drugs necessary to facilitate coughing and sputum discharge. They make a dry cough moist and productive.
- Antihistamines. The indication for their use is allergic tracheobronchitis.
- Nonsteroidal anti-inflammatory drugs. Taking these drugs is indicated in case of elevated temperature and fever. Effective in this category are Ibuprofen, Nurofen, Erespal.
Non-drug therapy
Non-drug therapy also helps to cure tracheobronchitis more quickly. It is carried out only after the patient’s body temperature has subsided. Non-drug treatment measures:
- Massage. The vibrating type of this procedure is especially effective, due to which it is easier to release mucus from the bronchi.
- Inhalations. They are carried out using nebulizers and ready-made inhalers. Due to spraying, the smallest particles of the drug more easily penetrate the bronchioles and bronchi.
- Foot baths. This is a very simple procedure that warms up the lower limbs, causing the blood to move more actively. Thanks to increased fluid outflow, swelling of the mucous membranes decreases - it becomes easier to breathe, headaches and nasal congestion gradually disappear.
- Therapeutic physical education (physical therapy). Facilitates the release of mucus and restores normal nasal breathing. Without getting out of bed in the morning, you need to tilt your upper body down, as if hanging from the bed. This will help clear your throat. It is good to combine this procedure with percussion massage.
- Physiotherapy. Due to them, inflammation is stopped, swelling of the bronchi and trachea is reduced, and normal mucus secretion is restored. These properties include lidocaine electrophoresis, magnetotherapy of the interscapular region, oxygen therapy, and ultraviolet radiation to the neck and sternum.
Manifestations of the disease in children
Acute tracheobronchitis is a common disease in young patients. Their immune system is not yet able to fight the attack of harmful substances on the mucous membrane of the respiratory tract. The disease in children has more pronounced symptoms. The child has noisy breathing, which may not be constant (long intervals between inhalations and exhalations). Due to a hysterical cough, children suffer from gag reflexes at the end of an attack.
The disease is dangerous due to its complications:
- Dysfunction of the nervous system – the child may experience increased excitability and sleep disturbances.
- Impaired heart function - manifestations of tachycardia may occur.
- Pneumonia - the inflammatory process can spread to the lungs, focal pneumonia occurs.
To avoid such dangerous conditions, you need to know how to cure this disease. Treatment for patients must be individually prescribed by a doctor after certain diagnostic measures.
How to treat
Tracheobronchitis requires complex treatment, so for complete recovery in most cases it is necessary to take several medications at once . The main ones are antibiotics or antivirals. Other remedies are prescribed depending on the symptoms. Commonly used drugs are described in the table:
| Group of drugs | Name of the drug | Mechanism of action | Admission rules | Daily dosage | pros | Minuses |
| Antiviral | Interferon | Blocks the reproduction of viruses when they penetrate the cell. | No more than 1,000,000 IU per day. | 2 tablets 2 times. | Restores immunity in a short time. | Lots of side effects. |
| Remantadine | Take orally after meals. | Day 1 – 100 mg 3 times, days 2 and 3 – 100 mg 2 times. | Rapidly absorbed in the intestines. | You need to take it at the first symptoms, otherwise there will be no effect. | ||
| Arbidol | Take before eating. | 200 mg. | No serious side effects. | Efficacy has not been proven. | ||
| Antibacterial | Augmentin | Provokes the destruction of bacteria. | Consume immediately before meals. | 375 mg 3 times. | Possible diarrhea after taking. | It is available in different forms, so the drug can be selected for any age. |
| Sumamed | Suppresses protein synthesis of microbial cells. | There is no need to chew the tablets. Take 1 hour before meals or 2 hours after. | 500 mg. | Short course of treatment – 3 days. | Almost everyone experiences severe cutting pain 25 minutes after taking it. | |
| Biseptol | Blocks bacterial metabolism. | Use with caution in case of bronchial asthma. | 960 mg once or 480 mg 2 times. | Well tolerated. | Toxic to the body. | |
| Antipyretics | Ibuprofen or Nurofen | Reduces inflammation, inhibits platelet aggregation, eliminates hyperemia. | The first dose is taken in the morning, then throughout the day after meals. | 200 mg 3-4 times. | Its safety has been studied and clinically tested. Does not affect the secretion of breast milk. | Frequent development of side effects. |
| Paracetamol | Affects pain and thermoregulation centers. | Do not take longer than 5-7 days. | Up to 4 tablets. | Prevents seizures in babies. | Blocks the production of interferon, which resists viruses. | |
| Ibuklin | Antipyretic, anti-inflammatory, analgesic. | Take before meals, do not chew. | 1 tablet 3 times. | A strong, fast-acting drug. | The capsules are large and difficult to swallow. | |
| Immunomodulators | Imunorix | Stimulates the effect on cellular defense mechanisms. | Take before meals. | 2 bottles. | Pleasant to the taste. | May cause allergies. |
| Immunal | Stimulates the function of the immune system. | Do not take longer than 8 weeks. | 3-4 tablets. | Plant origin. | Not included in any drug standards. | |
| Estifan | Increases the activity of macrophages and neutrophils. | Take after meals for 10-21 days. | 1-2 tablets 3 times. | Well tolerated. | Incompatible with immunosuppressants. | |
| Expectorants | Bromhexine | Liquefies and depolymerizes mucoprotein fibers of bronchial secretions. | Can be taken regardless of food. Drink 100-200 ml of water. | 8-16 mg up to 3-4 times. | Pronounced secretolytic effect. | Can't cope with a sore throat. |
| Ambroxol | Stimulates serous cells of the glands of the bronchial mucosa. | Take with a small amount of liquid. | 30 mg 2 times. | Low cost. | Sometimes causes hives. | |
| Mukaltin | Stimulates the secretion of bronchial glands. | Take half an hour before meals. | 2 tablets up to 4 times. | Natural composition. | Peculiar taste. | |
| Antihistamines | Suprastin | Blocks H1 histamine receptors. | Do not crush, do not chew, wash down with water. Do not exceed the dose of 100 mg. | 75-100 mg 1 time. | Performance. | Unpleasant taste, causes drowsiness. |
| Loratadine | In case of severe allergies, it can be combined with immunostimulants. | 10 mg 1 time. | Rapid onset of clinical effect. Does not have a sedative effect. | Not detected. | ||
| Tsetrin | Drink with a glass of water. | 10 mg 1 time. | Valid throughout the day. | Causes headache, drowsiness. | ||
| Multivitamins | Alphabet | Provides the body with vitamins and minerals. | Can be taken continuously or seasonally. | 3 capsules throughout the day at regular intervals. | The active ingredients are divided into capsules, so they are better absorbed. | Not detected. |
| Duovit | Take in the morning after meals, swallowing whole. | 1 red and blue tablet per day. | Vitamins and minerals are divided into different tablets. | Sometimes causes nausea. | ||
| Complivit | By agreement with the doctor, the dose can be doubled. | 1 tablet 1 time. | Can be selected based on age. | Not detected. |
Article on the topic: How to prepare for an ultrasound of the kidneys - indications for the procedure, what you can eat and what foods you should not eat
Treatment of the disease
Tracheobronchitis should be treated using a set of therapeutic measures aimed at removing the symptoms of the disease and general support of the human body. For this purpose, various drugs are used that affect cough, support human immunity, and neutralize the effect of the causative agent of the disease.
Cough treatment
Antitussives and expectorants are used for treatment. DO NOT use them simultaneously. Only in extreme cases is it permissible to use antitussive medications at night - they inhibit the action of cough centers, and the person can sleep peacefully. Expectorants are necessary for the production of bronchial secretions in order to remove pathological microorganisms from the respiratory tract.
Inhalations with expectorants are also used. Sometimes your doctor may prescribe the use of bronchodilators.
Immune support
Immunomodulating agents are used to support immunity. They should be given only after consultation with a doctor, especially when treating children.
The effect of drugs on the cause of the disease
Antiviral agents are used that act on viruses. For bacterial pathology they are ineffective.
Antibiotics should be taken only after diagnosing the bacterial nature of the disease. The course of treatment is determined by the doctor.
Hyperthermia
If the body temperature rises to 38.5 degrees, antipyretic medications must be given.
Folk remedies for tracheobronchitis
Traditional recipes also help to cope with the disease, but they can only complement the main therapy. Substituting non-traditional methods for drug treatment is contraindicated . The following decoctions and herbal infusions help cure tracheobronchitis:
- Mix equal parts of stinging nettle and coltsfoot leaves. Pour a tablespoon of herbal mixture into 1 cup of boiling water. Leave the infusion for 1 hour, then strain. Drink 2 tbsp up to 5 times throughout the day. l. Continue until the condition improves.
- For 200 ml of boiling water, take 15 g of elecampane crushed into powder. Mix well and place in a water bath. Boil over low heat for half an hour, then let cool. Then filter using a strainer, bring the volume to 200 ml, adding boiled water. Take the product warmed 1 hour before meals, half a glass. Repeat three times a day for 2 weeks.
The bronchi are well cleansed by aloe juice mixed in equal proportions with honey. Taking this and other folk remedies internally can cause heartburn, abdominal pain, and even allergic reactions. The latter are manifested by a rash, hyperemia and swelling of the skin. Among external folk methods, rubbing the chest with badger or goose fat is considered effective. They are done every day, preferably at night. This helps relieve cough. The disadvantage of this method is the specific smell of badger fat. Plus - judging by the reviews, this product helps to cope even with an old cough.
For respiratory diseases, it is useful to drink warm vitamin teas to strengthen the immune system. To brew them, it is recommended to use St. John's wort, linden, oregano, mint, licorice root, elderberry, and marshmallow. The advantage of such teas is the ease of preparation. The usual tea leaves are replaced with plant materials, and the drink is ready. Other ingredients can be added for taste. Among the effective recipes for vitamin teas are the following:
- Pour 300 g of elderberry flowers into a liter of boiling water. Add 8 walnut kernels and leave for half an hour. Drink warm 3-4 times throughout the day. You can sweeten it with a spoon of honey.
- Scald 200 ml boiling water 1 tbsp. l. thyme. Use the product throughout the day in 3-4 doses. The effectiveness of this tea is especially great for dry cough.
Causes
In acute tracheal bronchitis, inflammation of the mucous membrane of the tracheal region first develops. Then, falling lower and lower, it also affects the epithelium of the bronchi. In advanced cases, pathology can affect the lungs. The predominant cause of the development of tracheid bronchitis in adults and children is infection.
The disease is often caused by viruses, less often by bacteria, which join the pathological process later. The main channel for the spread of infection in acute tracheobronchitis is airborne, so you should remember that the patient is contagious to everyone around him.
This disease rarely occurs on its own. Most often it is diagnosed as a complication of other infectious diseases:
- ARVI;
- flu;
- tonsillitis;
- pharyngitis;
- sinusitis;
- acute pneumonia;
- whooping cough;
- scarlet fever;
- measles;
- rubella, etc.
Factors of a non-infectious nature can provoke the development of acute tracheobronchitis:
- hypothermia;
- frequent inhalation of too dry or too humid air, harmful chemical fumes;
- long-term residence in an environmentally unfavorable region;
- hypovitaminosis;
- hereditary predisposition to acute diseases of the respiratory system;
- poor, monotonous diet;
- chronic fatigue;
- smoking, alcohol abuse;
- severe stress or frequent conflict situations;
- weakening of the immune system.
Tracheobronchitis in a child
This disease also develops in children. Since the pathology is transmitted by airborne droplets, they easily become infected when visiting kindergarten and school . If tracheid bronchitis is suspected, it is important to immediately exclude the child from the team. In addition to contact with patients, pathology in children can be caused by:
- acute respiratory infections;
- diabetes mellitus;
- dystrophy;
- sinusitis;
- sore throat;
- caries;
- whooping cough;
- pharyngitis;
- frequent hypothermia;
- exudative diathesis;
- weakening of the tonsil function.
The risk of infection for a child increases if there is mold in the apartment. Provoking factors include polyps, adenoiditis, vitamin D deficiency, congenital pathologies of blood vessels, chest, and nasal passages. Tracheobronchitis in children is accompanied by symptoms such as:
- Cough. At night there are severe attacks. Sometimes the cough ends in vomiting and convulsions.
- Wheezing in the lungs. Good audibility when breathing.
- Stridor. This is wheezing, noisy breathing, indicating significant tracheal obstruction.
- Feverish condition. It does not go away for several days, is accompanied by a rapid pulse, profuse sweating, and increased breathing.
- Temperature increase. Rarely exceeds 37 degrees.
- Blue lips. Caused by a lack of oxygen due to poor breathing.
The treatment regimen for tracheid bronchitis is practically no different from the treatment of this disease in children . After determining the cause of the pathology, antiviral or antibacterial agents are prescribed. An alternative to the latter are sulfonamide drugs. In addition to taking medications, it is important to provide the child with a comfortable environment for recovery:
- He must remain on bed rest for a week. Several times throughout the day, the child should be given herbal infusions, juices, and warm tea. Inhalations with herbal decoctions are useful.
- Walking and visiting kindergarten or school are excluded. This is necessary to prevent the epidemic.
Drug treatment must be comprehensive. Don't be surprised if your doctor prescribes several medications at once. This is necessary to influence the causative agent of the disease and relieve its symptoms. The specialist prescribes drugs from the table:
| Name | Purpose | Indications for use | Dosage | Duration of admission |
| Paracetamol | Antipyretic | Pain syndrome, feverish conditions. | For children under 10 years of age – 0.5 tablets of 200 mg every 4-6 hours; 10-12 years – 325 mg 2-3 times a day; from 12 years – 1-3 tablets every 4-6 hours. | 5-7 days. |
| Tsitovir | Antiviral | Viral diseases of the respiratory system. | Up to 3 times a day, depending on age: 2 ml - up to 3 years, 4 ml - 3-6 years, 8 ml - 6-10 years, 12 ml - from 10 years. | 4 days. |
| Diprazine | Antihistamine | Diseases of an allergic nature. | Prescribed according to age: for 1-2 years – 5-10 mg 1-2 times, for 2-5 years – the same 1-3 times, for 5-10 years – 5-15 mg, from 10 years – 5- 20 mg. | Prescribed by a doctor. |
| Pertussin | Expectorant | Tracheitis, acute respiratory infections, pneumonia, whooping cough, bronchitis. | From 2.5 to 10 ml depending on the age of the child. | 10-14 days. |
Tracheobronchitis during pregnancy
Most often, the viral type of pathology develops during pregnancy. As a rule, it begins to progress against the background of acute respiratory infections, tonsillitis or pharyngitis. It is worth noting that the viral type during pregnancy poses a threat to the health and life of the child, so if it progresses, treatment should be started as early as possible.
The bacterial type is also very dangerous. The reason here is that during pregnancy it is not possible to treat with antibiotics, since it can harm the fetus. But so far scientists have not developed another effective method that would help eliminate the bacterial infection. Antibiotics are the only effective treatment.
During pregnancy, a woman should strictly adhere to the basic recommendations for the prevention of this disease. It is necessary to avoid large crowds of people, limit contact with sick people, and avoid hypothermia. It is also important to eat right during pregnancy.
Disease prevention
Tracheobronchitis, like any disease, is easier to prevent than to treat. To do this, it is important to follow the following rules of prevention:
- Treat colds promptly. If a cough appears, immediately start taking antitussive medications.
- Stay outdoors more often. This increases immunity and improves the functioning of the respiratory system.
- To refuse from bad habits. Alcohol and smoking provoke pathologies of the ENT organs.
- Regularly ventilate and clean the room. This will help ensure a favorable microclimate.
- Carry out hardening regularly. Even a regular regular contrast shower strengthens the immune system.
- Eat properly. A person's diet ensures his physiological well-being.
- Sanitate chronic foci of infection in the oropharynx. The drugs Miramistin, Aqualor, Dolphin are suitable for this.
Preventive measures
Preventive measures prevent the development of the disease. Among them:
- Timely treatment of colds and coughs at the first signs of its manifestation
- Constant exposure to fresh air strengthens the immune system and improves respiratory function
- Regularly ventilate and clean rooms in the house to create a favorable microclimate
- Temper yourself with a contrast shower or wiping with a damp towel
- Change your eating habits, switch to proper nutrition
- Sanitate chronic infectious foci in the oropharynx. This can be done with drugs such as Miramistin and Aqualor.
The danger of the disease lies in its complications. If left untreated, tracheobronchitis develops into pneumonia. Do not delay visiting your doctor. This determines how long the pathology itself and the recovery period will last. The doctor decides how to treat her. Do not take medications yourself.
Why does the inflammatory process occur?
Risk factors
The risk group includes children and adolescents; people who have chronic diseases and take medications for them. In order for a person to get sick, certain factors must combine.
This is a weakness of the immune defense, problems in the nasopharynx, nose or bronchi, and a sufficient amount of viruses or bacteria in the aerosol that a sick person releases into the environment. If these factors add up at the same time, then most likely the person will become infected and fall ill.
Direct causes of tracheobronchitis
- Our main enemies when it comes to tracheobronchitis are viruses. These are influenza, parainfluenza, adenoviruses - there are a great many of them.
- In more rare cases, our body also has to fight bacteria . These are mycoplasmas, chlamydia, bordetella, and pneumococci known to us.
- In some cases, acute tracheobronchitis is caused by allergens, toxic and chemical agents . We must not forget about tobacco smoke, dust, animal hair, and polluted air.
The danger of allergic tracheobronchitis
Allergic tracheobronchitis, if treated incorrectly or insufficiently, can lead to many complications that aggravate the course of the underlying disease.
- Pneumonia, which is the most common complication. The process spreads to the lung tissue, acute pneumonia develops, which can later become chronic. After chronicization, processes of fibrosis of the lung tissue begin, which leads to respiratory failure.
- Bronchial asthma, which is a disease accompanied by asthma attacks.
- Pulmonary heart. When the load on the heart increases due to arterial hypertension, its right parts increase.
- Emphysema, which occurs as a result of difficulty in breathing out. The alveoli become stretched and damaged, leading to the formation of air spaces in the lung tissue. Lung function decreases, leading to the development of respiratory failure.
Treatment of allergic tracheobronchitis
Exacerbation period
Therapy of allergic tracheobronchitis during an exacerbation is based on the use of medications, which is combined with regular inhalations.
Proper treatment can significantly improve the patient's condition.
The following drugs are used for therapy
- Antihistamines, which block histamine receptors, helping to reduce the main symptoms. Histamine is the main mediator of the allergic reaction; it determines the phase of clinical manifestations of allergies. Histamine increases vascular permeability, causing swelling and hyperemia. Examples of drugs: Zyrtec, Telfast.
- Enterosorbents. They are used for complex forms of allergic tracheobronchitis. These drugs help remove irritants and toxins from the body. Examples of drugs: polyphepan, activated carbon.
- Expectorants. They improve mucus production by thinning it. Examples of drugs: lazolvan, ambroxol.
- Bronchodilators that improve bronchial patency. They eliminate spasm and dilate the bronchi. Examples of drugs: fenoterol (Berotec).
Prevention of exacerbations
To reduce the likelihood of recurrence of symptoms, proper treatment during an exacerbation is necessary.
A common mistake is uncontrolled use of antitussive drugs. The cough reflex is suppressed, but the mucus is not removed, but accumulates in the bronchi.
This will definitely provoke a new attack. Also, for prevention, it is necessary to reduce contact with possible allergens.
You should give preference to a hypoallergenic diet, and also regularly carry out wet cleaning in the house. Patients are prescribed medications that strengthen the immune system.
Remission period
During this period, when there are no severe symptoms, preference is given to physiotherapeutic methods.
- Breathing exercises. It should be done daily to prevent shortness of breath. Exercise helps strengthen your chest muscles.
- Hypoxytherapy by inhaling a gas mixture in which the amount of oxygen is reduced. This method allows you to activate the immune system, increases the vitality of the body.
- Local ultraviolet irradiation, which gives an anti-inflammatory and bactericidal effect.
- UHF therapy, which helps improve immunity, regulates cell metabolism.
- Inhalations, which are recommended to be carried out 1.5 hours after meals.
Diagnosis of chronic tracheobronchitis in children and adults
When you detect the first symptoms of the disease, especially if it occurs in an acute form and threatens to become chronic, you must immediately make an appointment with a doctor. A therapist deals with such issues, and if possible, then you can also consult a pulmonologist.
Often, in patients who decide that the disease will go away on its own, bronchial asthma develops against the background of incompletely cured tracheobronchitis. Moreover, it occurs much more often in children than in adults.
In addition to the therapist and pulmonologist, the patient is also advised to consult an otolaryngologist and an allergist. It is important to follow all the doctors’ instructions to establish the exact cause of the ailment, since the symptoms inherent in troacheobronchitis are often observed in other pathologies of the respiratory tract.
Diagnostic procedures to make a correct diagnosis often include activities such as:
- Initial examination and history taking based on the patient’s verbal expression of complaints.
- Laryngoscopy, during which a thorough examination of the patient’s pharynx is performed. What type of this procedure (indirect, direct or rigid laryngoscopy) is advisable to perform in a particular case is decided solely by the otolaryngologist.
- Bronchoscopy for a complete assessment of the health of the bronchi.
- Culture of sputum on a nutrient medium.
Taking swabs from the nose and throat for further thorough bacteriological examination. Based on the results obtained, the doctor will be able to judge what exactly led to the development of tracheobronchitis. In particular, this manipulation is carried out in order to determine the type of bacteria that caused the disease.
- General clinical blood test. It is important to note that hemoglobin levels play an important role in this case, especially if a pregnant woman suffers from the symptoms of the disease.
- If the doctor has good reason to suspect the patient has pneumonia, the patient is advised to undergo fluoroscopy. Only a doctor can judge the advisability of performing this diagnostic method in expectant mothers, since X-ray irradiation can negatively affect the intrauterine development of the fetus.
In addition to the above methods for diagnosing tracheobronchitis, allergy tests for sensitivity to drugs that will be used to treat the disease are also mandatory. Since it often involves the use of antibacterial drugs, it is important to know whether this will affect the patient’s well-being.
Etiology
Allergic tracheobronchitis is not a cold. The cause of this disease is the action of allergens. The main etiological factor is exogenous allergens, that is, foreign substances that enter the body from the outside. Allergens are divided:
- for infectious diseases;
- to non-infectious.
Infectious allergens include bacteria, fungi, viruses and helminths. The group of non-infectious substances that cause allergies is more diverse. Such allergens include pollen, animal dander, insecticides, household chemicals, foods and medications.
Predisposing factors
The following factors contribute to the development of allergic tracheobronchitis:
- frequent respiratory diseases;
- insufficient or lack of treatment for respiratory diseases;
- decreased immunity;
- poor nutrition, especially in childhood;
- dysfunction of the endocrine system (for example, decreased adrenal function);
- increasing the permeability of histohematic barriers;
- burdened heredity;
- predisposition to bronchial hyperreactivity (increased formation of IgE).
Diagnostics
The doctor begins the examination of the patient with auscultation - listening with a phonendoscope to the sounds accompanying breathing, and examining the larynx using a laryngoscope. Laboratory tests of blood (general and biochemical) and urine are prescribed. A sputum examination is carried out (culture to identify pathogenic microorganisms). The version about the bacterial nature of acute tracheobronchitis is finally confirmed by the result of a blood test for procalcitonin.
At the same time, the condition of the patient’s respiratory tract is determined using the following methods:
- Ultrasound of the trachea, bronchi, lungs;
- chest x-ray;
- bronchography (X-ray examination of the bronchi using a contrast agent);
- spirometry (measurement of breathing parameters).
The doctor begins the examination of the patient with auscultation - listening with a phonendoscope to the sounds accompanying breathing, and examining the larynx using a laryngoscope.
Most of the symptoms of acute tracheobronchitis are identical to the signs of many other pathologies of the respiratory system and infectious diseases. Therefore, the doctor must conduct a differential diagnosis. The disease must be distinguished not only from ARVI or influenza - this is the simplest thing. Tracheobronchitis can be disguised as eosinophilic bronchitis, obstructive pulmonary disease, bronchial asthma, respiratory mycoplasmosis and other severe lesions of the respiratory system.
About bronchotracheitis
Bronchotracheitis is an inflammatory disease. Affects the trachea and bronchi. It often occurs when influenza is not treated in a timely manner. During coughing, the infection enters deeper into the respiratory tract, onto the mucous membranes of the trachea.
Bronchotracheitis develops well from hypothermia, from dust in the air. Synthetic drugs (aerosols, perfumes, paint) can provoke the disease. Chemicals irritate the membrane and cause coughing. The infection most likely spreads in the respiratory system.
Tracheobronchitis develops quickly. The disease occurs in an acute form. Timely therapy helps the patient quickly cope with bronchotracheitis. If treatment does not produce results or is completely absent, the disease can become chronic.
For information
In order to make such a diagnosis, the listed symptoms or auscultation data alone are not enough. Additional examinations are often prescribed, for example, chest x-ray, tracheobronchoscopy, and laboratory testing of sputum. If we are talking about allergic tracheobronchitis, then it is necessary to identify the main and cross allergens, for which appropriate tests are carried out.
To treat the disease, both pharmacotherapy is used, which involves the use of expectorants and mucolytics, as well as antihistamines for allergic forms, and non-drug methods. The latter include therapeutic breathing exercises, massage, etc.
When considering tracheobronchitis, types, symptoms and treatment methods, it is necessary to take into account concomitant diseases and complications.
Folk recipes
Folk recipes.
Traditional recipes for the treatment of bronchotracheitis are based on the use of herbal remedies.
Recipe No. 1:
- great plantain leaf juice – 1 teaspoon;
- honey – 1 teaspoon.
Mix thoroughly. Drink before meals, several times a day. Be sure to take immediately after preparation.
Recipe No. 2:
- oats – 2 tablespoons;
- raisins – 2 tablespoons;
- honey – 1 tablespoon;
- milk – 1.5 liters.
Cook over low heat until half the water has evaporated. Strain the cooled broth, add honey. Drink one spoon every hour. Store in a cool place.
Recipe No. 3:
- ginger – 5 g;
- cloves – 5 g;
- cinnamon – 5 g;
- hot water – 300 ml.
Mix the ingredients and let stand for 5 hours. Drink four times a day.
Treatment
Tracheobronchitis is a fairly serious disease, but if treated in a timely manner, the inflammation goes away within 1-3 weeks. To improve the patient’s condition during an exacerbation, it is necessary to treat not only the infection, but also individual symptoms of the disease.
Alleviation of the patient's condition
- The room should be ventilated regularly.
- Humidifying the air will reduce coughing.
- Expectorant mixtures.
- Mild teas with honey and lemon to thin mucus.
- Inhalations based on herbal decoctions.
- Oxygen therapy to replenish oxygen in the blood.
- The doctor may prescribe a number of intravenous injections, including medications to improve circulation and breathing.
Fighting infection
Since the disease is most often associated with ARVI, the prescription of antibacterial agents for it is not always required. Indications for the prescription of antibiotics for acute tracheobronchitis include:
- The addition of a bacterial infection, which is expressed in a change in the nature of sputum from mucous to mucopurulent.
- Increasing symptoms of intoxication or weak dynamics of the disease, prolonged persistence of cough with sputum production;
- Children under 3 years of age;
- The presence of concomitant pathology of the respiratory and cardiovascular systems, including developmental anomalies, decompensated diabetes mellitus;
- Initially, the disease occurs with signs of a bacterial infection - purulent sputum, high temperature, leukocytosis with a band shift in the FAC.
The most preferred antibiotics for acute tracheobronchitis are:
- Aminopenicillins, including protected ones (amoxicillin - Flemoxin Solutab, Amoxiclav, Augmentin, Unazin);
- Macrolides (“Azithromycin”, “Macropen”, “Roxithromycin”).
In addition to antibacterial agents, for acute tracheal bronchitis, the following are usually prescribed:
- Expectorants - cough syrups, ambroxol in the form of inhalation through a nebulizer or in the form of syrups;
- Mucolytics – acetylcysteine (AC);
- Abundant drinking regime;
- Vitamins and restoratives (immunal, echinacea).
With proper treatment, the acute form can be cured in 1-3 weeks; the course of the disease for more than three weeks is considered protracted.
Treatment of chronic tracheobronchitis
Chronic tracheobronchitis is based on an untreated acute form, an allergic component, the state of the immune system, lifestyle and concomitant diseases. The fact that there is a chronic inflammatory process in the body is indicated by a frequent slight increase in temperature (low-grade fever). The duration of cough in chronic tracheobronchitis is three months a year or more. The cough is usually unproductive.
Treatment of chronic tracheobronchitis is complex.
- The patient needs to get rid of bad habits: alcohol, smoking.
- The sputum is cultured for microflora, atypical pathogens (mycoplasma, chlamydia) are excluded.
- Allergy tests are carried out.
- Therapy is prescribed by a doctor based on diagnostic results.
The allergic form is treated with:
- expectorants;
- antihistamines;
- inhalations, including with glucocorticosteroids;
- folk remedies;
- physiotherapy.
Non-allergic chronic tracheobronchitis is treated with:
- Bronchodilators (especially M-anticholinergics - ipratropium bromide, tiotropium bromide - Berodual, Atrovent, Spiriva);
- Mucolytic-mucoregulators – acetylcysteine, carbocysteine, erdosteine;
- Inhalations using a nebulizer of ambroxol, alkaline and hypertonic solutions;
- Antibacterial agents - macrolides, 3-4 generation cephalosporins, doxycycline, respiratory fluoroquinolones, amoxicillin/clavulanate;
- Less often there is a need for inhaled glucocorticosteroids - “Pulmicort”, “Benacort”, “Flixotide”, “Beclomet”, “Bekotide”, “Asmanex” “Twistheiler” (the most effective).
Disease prevention
Tracheobronchitis often occurs against the background of ARVI, in order to prevent the development of the disease, you need to:
- start treatment of acute respiratory infections and acute respiratory viral infections on time;
- do not carry the disease on your feet;
- do not overcool when symptoms of illness appear;
- eat fresh fruits and vegetables to replenish natural vitamins;
- Walk a lot and often, thoroughly ventilate the room, maintain the room temperature at about 20 degrees and humidity at about 50%.
- drink teas, warm water with lemon juice and honey to ease expectoration when coughing and not injure the bronchi.
Causes of bronchotracheitis
Bronchotracheitis develops against the background of previous respiratory tract diseases (ARVI, influenza, tracheitis, pharyngitis, laryngitis). The inflammatory process moves from the upper respiratory tract to the trachea and bronchi.
The main causative agents of bronchotracheitis are viruses and bacteria.
Viruses that cause tracheobronchitis:
- parainfluenza;
- flu;
- adenovirus;
- rhinovirus.
Pathogens are transmitted by airborne droplets. More often, children succumb to the viral type of bronchotracheitis. Viruses affect children with weakened immune systems (after a previous illness).
A healthy person has a much lower risk of contracting the viral form.
The cause of bronchotracheitis can also be bacterial flora:
- Pseudomonas aeruginosa;
- Staphylococcus aureus;
- streptococcus;
- mycoplasma.
Harmful microorganisms need warmth and moisture to reproduce. The mucous membranes of the respiratory tract contribute to their reproduction and vital activity.
Causes of allergic bronchotracheitis:
- perfumery;
- chemical compounds (at work involving the use of harmful chemicals, aerosols);
- dust;
- mold spores;
- flower pollen;
- traffic fumes.
Causes of illness in children:
- weak immunity;
- rickets;
- ARVI, influenza, respiratory diseases;
- diabetes;
- muscular dystrophy;
- protein-energy malnutrition.
Bronchotracheitis can occur under unfavorable conditions.
Non-infectious causes of the disease:
- prolonged exposure to cold air, drafts;
- spring lack of vitamins;
- bad habits (smoking);
- respiratory diseases;
- work related to chemicals (if workers do not use respirators or protective masks);
- exhaustion of the body (chronic physical fatigue);
- genetic predisposition;
- nervous disorders (stress, depression).
Non-infectious causes of bronchotracheitis can become the basis for the development of harmful pathogens. A child or adult with a strong immune system may not become infected with a viral infection. Unfavorable environmental conditions provoke the development of pathogens.
Staphylococcus aureus.
Phytotherapy
Phytotherapy.
Treatment with traditional methods can speed up the healing process. Herbal medicine is widespread - the use of medicinal herbs for the prevention and treatment of bronchotracheitis in adults and children.
Medicinal herbs are used to make infusions, teas, balms, and relaxing baths. Herbal medicine helps dilate the bronchi and easy coughing up mucus. Some plants have anti-inflammatory and antipyretic properties. The body is enriched with useful substances, vitamins, and immunity increases.
During illness, the level of intoxication in the body increases. To reduce the amount of toxic substances in the blood, it is recommended to drink a lot. The liquid “cleanses” the body.
Drinks that contain vitamin C:
- rosehip decoction;
- cranberry juice;
- lingonberry juice.
Diuretic herbs cleanse the body well:
- horsetail;
- knotweed;
- bearberry.
Infusions help reduce high fever in children:
- raspberry tea;
- viburnum tea;
- linden decoction.
To treat dry cough, make a decoction of coltsfoot. Pour two liters of boiling water over a glass of dried herb and simmer for 30 minutes. Take one tablespoon of the prepared decoction every hour.
Recipe for easy expectoration:
- marshmallow root – 20 g;
- elecampane root – 10 g;
- birch buds – 10 g;
- oregano – 10 g.
Mix all ingredients. Add a tablespoon of herbal mixture to one glass of boiling water and simmer over low heat for 15 minutes. Drink one spoon every two hours.
Inhalations provide a calming anti-inflammatory effect.
To prepare the solution you need:
- chamomile – 1 tablespoon;
- calendula – 1 tablespoon;
- water – 2 liters.
Bring the water to a boil. Add medicinal herbs and let steep for 5 minutes. Next, breathe in the steam for 15 minutes. After a few days, mucus will begin to separate when you cough.
When treating wet coughs, herbs are used that soften phlegm. Effective onion remedies.
Boil finely chopped onion in milk. Let it brew for several hours and strain. Take a tablespoon of the decoction four times a day.
Onion broth has an unpleasant smell and taste. Children often refuse to take this medicine. You can squeeze out carrot juice. Mix with honey and milk, stand for 5 hours. Drink half a glass four times a day.
With the help of medicinal plants, you can minimize the intake of medications.
- Oak bark, sage, chamomile and calendula help to remove the inflammatory process.
- Icelandic moss, thyme, wild rosemary, eucalyptus, and nettle have an antibacterial effect. They can be taken in the form of infusions and decoctions.
- Physiotherapy
Physiotherapeutic procedures are more suitable as prevention. Treatment using this method helps improve immunity and speed up recovery.
Physiotherapy in the treatment of bronchotracheitis includes the following procedures:
- inhalation - using this method, medicinal substances enter the respiratory tract and act on the site of the disease;
- massage - a specialist performs manipulations so that phlegm is removed from the lungs faster;
- ultra-high-frequency inductothermy (UHF therapy) – I apply a high-frequency electric field to the body in the lung area, helping to reduce pain, relieve inflammation, and remove spasms;
- magnetic therapy – increases the effect of antibiotics, mucosal cells are renewed faster;
- electrophoresis - the charge helps drugs penetrate tissue membranes more intensively, relieves inflammation and swelling;
- halotherapy is a popular method of treating bronchotracheitis; the patient is placed in salt caves, the lungs are ventilated and cleansed;
- mud procedures – the patient is placed in a warm mud bath, blood flow improves, the lungs are saturated with oxygen.
Children's bodies are weaker, so the methods described above are contraindicated. Ultraviolet irradiation is used to treat bronchotracheitis in children. Helps relieve swelling, speed up recovery, and kills harmful organisms.
Complications
Acute tracheobronchitis is dangerous for children. Although respiratory arrest does occur, it is extremely rare. Much more often, young children develop partial bronchial obstruction, which then persists for life. If the disease is not treated, it may cause:
- various dysfunctions of the respiratory organs;
- laryngitis;
- pneumonia;
- pulmonary edema;
- heart diseases;
- severe deviations in the activity of the nervous system.
Basic therapy methods
Treatment of tracheobronchitis includes an integrated approach. Depending on the type and nature of the disease, the following is prescribed:
preventive measures (to eliminate non-infectious causes of bronchotracheitis);
- symptomatic treatment (medicines against cough, fever);
- impact on pathogens;
- traditional methods of treating bronchotracheitis;
- physiotherapy;
- phytotherapy.
Treatment of children often requires hospitalization. Narrowed airways can cause suffocation and complications. The early stages of bronchotracheitis can be treated at home. It is necessary to follow the doctor’s recommendations and carry out medication treatment strictly as prescribed.
Medications
Medications.
When treating bronchotracheitis, several groups of drugs are prescribed depending on the cause of the disease. Antiviral drugs are used to fight viruses:
- “Aflubin” is a homeopathic remedy that has anti-inflammatory, antipyretic effects, strengthens the immune system, and relieves intoxication of the body;
- “Anaferon” is another homeopathic drug that improves immunity and is used to prevent viral diseases;
- "Arbidol" is an antiviral, immunomodulatory agent.
Antibacterial drugs:
- “Umkalor” is a product based on Pelargonium root, kills harmful microorganisms, stimulates the immune system;
- “Biseptol” is a drug from the sulfonamide group, prescribed to infants;
- "Bioparox" is a medicine in the form of inhalation that acts on the site of inflammation.
A dry cough causes severe discomfort. It is difficult to stop a coughing attack, because during coughing sputum is not released, but only the mucous membrane is irritated. In children, this symptom can lead to suffocation; night attacks prevent the child from sleeping.
To alleviate the condition, treatment with antitussives and expectorants is prescribed:
- “Bromhexine” is an expectorant mucolytic drug for dry cough (produced in the form of syrup, tablets);
- "Ambroxol" - syrup for expectoration with wet cough;
- "Libexin" is an antitussive drug for the treatment of respiratory diseases, has an anesthetic and bronchodilator effect (dispensed in tablets).
If bronchotracheitis is accompanied by high fever, take antipyretics. Children are given Nurofen or Ibuprofen. Adults can take Paracetamol.
When treating, it is important to follow your doctor's recommendations and take medications in the dosage indicated in the prescription or instructions.