Nonspecific ulcerative colitis (UC, modern name “ulcerative colitis”) is a chronic disease that manifests itself as purulent hemorrhagic inflammation of the colon wall. The prevalence of the disease in different countries ranges from 50 to 230 people per 100 thousand population. People aged 20–40 years are most often affected, men and women with equal frequency[1]. Typically, several years pass from the appearance of the first symptoms to an accurate diagnosis. Late diagnosis and the resulting inadequacy of treatment often lead to the development of severe complications and relatively high mortality (in Russia - 17 cases per million population, in Europe - 6 cases per million [2]).
Large intestine, how does it work?
The digestive organ is one of the largest organs; all consumed foods pass through it. The size of the organ varies from 4 to 8 m in length.
It is in this department that the absorption of nutrients and vitamins, the processing of carbohydrates and fats that are necessary for the functioning of the body take place.
It produces more than 10 types of hormones necessary for the functioning of the human body. However, these are not all areas of responsibility of the digestive organ.
This organ is extremely important in the process of immune function, since various bacteria live there, for example: bifidobacteria and lactobacilli. They act as the first step of the body’s defense when an infection enters it.
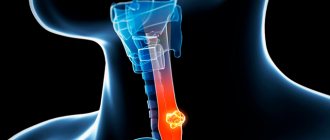
Nonspecific ulcerative colitis affects the large intestine. In diameter, this section ranges from 4 to 10 cm, and its length is 2 meters.
The main functions of the colon are:
- Digestion of leftover food;
- Water absorption (up to 90%);
- Formation and removal of feces;
There are several departments:
- Blind. This section contains the appendix, in which beneficial microflora develop;
- Colonic. The main section, its peculiarity lies in the fact that there is no septum, and the section itself does not participate in the digestion process. The main function is to absorb water and process liquid food. The length of the department is about 1.5 m, the department itself is divided into subsections: Ascending, 20 cm long;
- Transverse, 56 cm long;
- Descending, 22 cm long;
- Warm sigmoid colon;
- Rectum (rectum) 14 – 16 cm;
Quite common is the focus of ulcerative colitis in the rectum, the main function of which is the promotion and removal of food debris from the body.
Those. it serves as a kind of reservoir that does not allow feces to be released arbitrarily.
Diet and lifestyle
For drug therapy to be as effective as possible, patients should adhere to a diet and consume the following foods:
- lean varieties of meat and fish, boiled or steamed;
- low-fat chicken broth and pureed soups based on it;
- boiled vegetables, casseroles;
- thin puree soups;
- slippery porridges made from rice and semolina;
- jelly and compotes;
- oat broth;
- dried gray bread or crispbread;
- It is preferable to eat meat soufflé over all other types of meat products;
- You can eat potatoes and pasta little by little - during remission;
- low-fat fermented milk products in small quantities.
The following products are prohibited:
- fast food, store-bought sauces, ketchup, mayonnaise;
- fatty meats and fish;
- fried, salted, smoked and spicy foods and dishes made from them;
- pickled vegetables;
- any canned food;
- purchased sausages;
- fresh white bread and pastries;
- legumes;
- cabbage in any form;
- dried fruits;
- nuts in large quantities;
- alcoholic drinks;
- strong tea and coffee;
- various cereals with the addition of seeds and cereals;
- buckwheat, oatmeal, pearl barley, barley porridge.
When diagnosing ulcerative colitis, the patient needs to reconsider some habits:
- maintain a daily routine - sleep should last at least 8 hours, since a weakened body needs strength to fight the disease;
- leisurely walks in the fresh air;
- split meals 4-6 times a day in small portions;
- food should be warm, eating too hot or very cold foods is prohibited;
- special attention is paid to thoroughly chewing food for its better absorption;
- in terms of consistency, liquid, puree-like dishes without solid particles are preferred;
- drink enough clean water, as patients often suffer from dehydration.
These measures will help maintain strength in a weakened body and will contribute to a more effective effect of medications.
What kind of disease is UC?
The abbreviation UC stands for nonspecific ulcerative colitis.
The disease is ulcerative-inflammatory and chronic. The main lesion may be in the rectum or colon of the large intestine.
There are no known cases of ulcerative colitis of the small intestine.
- The disease develops gradually and may take a long time to be detected, especially if the patient does not undergo periodic medical examinations.
- The disease occurs cyclically, i.e. Exacerbations may periodically occur, followed by remission.
- The most common symptoms are bloody diarrhea and cramping pain.
Prevention
Prevention of the development of this intestinal pathology consists of proper nutrition and periodic examination. It is important to promptly treat chronic diseases of the digestive tract. The prognosis for ulcerative colitis in the absence of complications is favorable.
Ulcerative colitis is a serious disease that requires immediate and competent treatment. Do not delay visiting your doctor when the first symptoms appear. It is important to remember that in the event of an acute form of the disease, the organ is affected quickly, which can lead to the development of cancer or various complications.
Classification
UC is usually classified according to severity. What it is? The degree of severity is an assessment of the harm caused to a person, which is established according to special standards.
Based on severity, it is classified into 3 categories:
- Easy. Characterized by: Hyperemia (diffuse). Overflow of blood vessels;
- Presence of erosions;
- The presence of a small number of ulcers;
- The main lesion is located in the rectum.
- Change in the structure of the mucous membrane of the large intestine to granular;
- The presence of pseudopolyps;
How to treat ulcerative colitis
Treatment of ulcerative colitis is hard work, since a complete cure is currently impossible to achieve. Treatment allows you to prolong remission, compensate for the patient’s condition, make his life easier, and also prevent the development of complications. Therapy must be comprehensive and ongoing. The doctor should select it based on the characteristics of the pathology, the patient’s condition, the presence of concomitant diseases, and complications. However, the effectiveness of treatment also depends on the patient, since such a diagnosis completely changes the rhythm of life and requires careful attention to oneself.
Diet for ulcerative colitis
Proper nutrition is the key to successful treatment of all diseases of the gastrointestinal tract, and ulcerative colitis is no exception. Such patients quickly lose weight and are prone to exhaustion. In addition, they suffer from massive diarrhea. Based on this, the diet for ulcerative colitis of the intestine should certainly include:
- foods rich in protein (lean meat and fish, soy products, cottage cheese, boiled eggs);
- porridge (rice, buckwheat, oatmeal);
- honey;
- berry and fruit compotes;
- natural jelly;
- homemade jelly;
- steamed or boiled dishes;
- food should be pureed.
It is necessary to exclude “coarse” fiber. It is found in raw vegetables, legumes, fruits, and nuts.
In severe cases, when the patient is unable to eat on his own, enteral or parenteral nutrition is provided for ulcerative colitis of the rectum. For this, pharmacies sell special mixtures enriched with all the necessary nutrients.
Drug treatment
Drug therapy is aimed at eliminating the inflammatory process, alleviating the patient’s condition, and preventing the development of complications. For this purpose, therapy includes:
- 5-aminosalicylic acid preparations. They are the drugs of choice for the treatment of ulcerative colitis. They have pronounced anti-inflammatory and wound-healing effects on the intestinal mucosa. This group includes sulfasalazine and mesalazine.
- hormonal drugs. They have a massive anti-inflammatory effect. Prescribed in cases where drugs of the previous group are not effective. The most common medications in this group are dexamethasone and prednisolone.
- immunosuppressants. Prevents the production of antibodies to your own mucous membrane.
- antibiotics. When the temperature rises, as well as intoxication, it is recommended to take antibacterial drugs. The choice of medication depends on the causative agent of the pathology and the patient’s sensitivity to it.
- antidiarrheal drugs. Allows you to eliminate massive diarrhea. The most popular are Loperamide and Imodium.
- painkillers. Medicines of the NSAID group (non-steroidal anti-inflammatory drugs), such as Ibuprofen, Diclofenac, Naproxen, are usually used here.
- iron supplements. Indicated for heavy bleeding and severe anemia.
If therapy is ineffective, surgical treatment may be prescribed, which consists of removing the pathological area of the large intestine.
Folk remedies
Traditional medicine offers several recipes that can alleviate the condition of patients:
- Decoctions of herbs (raspberry leaves, chamomile, yarrow, wormwood, St. John's wort).
- Sitz baths with herbal teas against colitis.
- Microclysters with sea buckthorn oil.
- Mumiyo.
These techniques cannot completely replace traditional treatment, but only become an assistant in compensating for the condition of a patient with UC.
Reasons for appearance
The causes of this disease are still not precisely known to medicine. However, there are theories and statistics.
According to theoretical data, there are several causes of nonspecific ulcerative colitis:
- Genetic predisposition;
- Immune system error.
Causes of colitis
The disease is one of those whose etiology has not been clearly identified. Previously, the main causes were considered to be poor diet and stress. Now these factors are classified as triggers that can aggravate the condition, but do not cause it.
Possible causes of colitis include:
- heredity – increases the risk of close relatives having not only ulcerative colitis, but also Crohn’s disease. Moreover, the presence of a mutated gene does not mean guaranteed development of colitis; this requires the presence of additional factors that support inflammation;
- a disorder in the functioning of the immune system - in an attempt to resist the invasion of bacteria and viruses, an abnormal immune response is formed, causing the immune system to attack its own cells of the digestive tract;
- external factors - smoking, unbalanced diets, taking contraceptives.
Colitis most often attacks young people under 30 years of age. One of the risk factors is the use of isotretinoin and roaccutane in the treatment of acne.
Symptoms of UC
Depending on the severity of the disease, the symptoms and treatment of the disease will vary.
Like all diseases, ulcerative colitis has characteristic symptoms:
- Cramping attacks of pain, which are accompanied by the desire to empty the intestines;
- Diarrhea with blood (can be both long-term and short-term);
- Having a feeling of fatigue, as well as weight loss due to a violation of the absorption mechanism;
- Increased body temperature (more than 37.5 °C) for a long time;
- Cutting pain in the anus area;
- Bloody discharge, regardless of the presence of bowel movement (traces on paper, linen, etc.);
- Constipation or severely difficult bowel movements;
All of the above symptoms can occur not only with UC, but also with some other diseases, both less and more serious, for example:
- oncology,
- haemorrhoids,
- anal fissures, etc.
An accurate diagnosis can only be made in a medical institution and after all the necessary research has been carried out.
Complications are possible if the disease was discovered late and the degree of damage is high or if it develops quickly.
It is customary to distinguish several types of complications:
- Local, affecting the large intestine;
- Are common. They can manifest themselves in any area and are called extraintestinal;
Symptoms of ulcerative colitis of the intestine
Ulcerative colitis has an acute phase and a remission phase. The disease begins gradually at first, but quickly gains momentum when the symptoms become more pronounced.
Symptoms of ulcerative colitis from the digestive system:
- cramping pain in the abdomen localized predominantly on the left, which is difficult to relieve with medications;
- diarrhea or loose stools mixed with mucus, blood or pus, worse at night or in the morning;
- constipation that replaces diarrhea, which is caused by intestinal spasm;
- bloating (flatulence);
- frequent false urge to defecate (tenesmus), which occurs due to retention of feces above the area with inflammation;
- spontaneous release of mucus, pus and blood (not during defecation) as a result of imperative (irresistible) urges.
In 10% of cases, in addition to the mentioned intestinal and general symptoms, extraintestinal manifestations occur:
- joint lesions;
- various rashes on the skin and mucous membranes (for example, in the mouth);
- eye disorders;
- damage to the liver and bile ducts;
- thrombus formation, etc.
They may precede intestinal disorders. The severity of extraintestinal manifestations sometimes depends on the activity of the inflammatory lesion of the intestine, and in some cases is completely unrelated to it.
With mild ulcerative colitis, patients complain of cramping pain or discomfort in the abdomen, weakness. Semi-liquid stools are possible 2-4 times a day with a small admixture of blood and mucus.
If ulcerative colitis is more severe, then loose stools occur up to 8 times a day with a significant admixture of mucus, blood and pus. With this form of the disease the following are noted:
- pain in the abdomen, often in the area of the left half (flank).
- there is weakness,
- slight fever
- weight loss.
- may be tachycardia,
- pain in the liver.
Symptoms during an exacerbation
During the period of exacerbation, symptoms of intoxication appear:
- fever,
- weakness,
- malaise.
A distinctive sign of ulcerative colitis from simple catarrhal disease is weight loss. Patients often look exhausted. Their appetite is reduced. With intestinal colitis, ulcerative defects are formed. They may bleed as stool passes.
Symptoms may become weaker and then worsen again. If continuous treatment is carried out, a remission phase begins and the symptoms subside. How often relapses occur is determined by the treatment, and not by how damaged the intestines are.
Complications and consequences
Types of complications in UC:
- Profuse bleeding. According to experts, such bleeding from the rectum can cause significant blood loss. Profuse bleeding occurs due to the fact that the intestinal wall is already severely damaged, and a large blood vessel is destroyed. Treated either with hemostatic agents or transfusions, or with resection (removal) of the affected area;
- Expansion or contraction in various areas. The probability of a complication exceeding 50% in moderate and severe forms of UC. It occurs due to dysfunction of the muscles of the large intestine, accompanied by toxic poisoning of the body due to obstruction of fecal masses, as well as dehydration;
- Toxic dilatation (stretching due to pressure). With this complication, cavities appear in areas of the large intestine in which feces collect. It begins to rot, the patient begins to intoxicate the body with all the consequences: deterioration of the condition, fever, vomiting, watery stools and, if there is no help, death;
- Damage (perforation) of the intestine. This type is considered the most severe and requires immediate surgical intervention. Due to the fact that this complication is not common, the mortality rate is high (more than 75%). Accompanied by toxic poisoning of the body, acute pain and fever;
- Peritonitis (local inflammation) can occur at sites of perforation, as well as with toxic dilatation. The mortality rate due to this complication is high due to the fact that the diagnosis is usually made too late;
- Oncology. According to statistics, the number of cases of UC spillover into oncology varies from 4 to 5%. The determining factors are: the duration of the UC disease (usually at least 10 years) and the chronic form of the disease. Prognosis for the detection of this complication depends on the time of detection of the tumor, the number of metastases, etc.;
- Sepsis (inflammation). Occurs in severe forms of UC with the presence of other complications listed above. Antibiotics are used for treatment;
- Pseudopolyps. A fairly common complication. This term refers to the process of proliferation of mucous tissue in the area of ulcers or scars. The probability of occurrence with UC is 50–60%. Occurs due to severe inflammatory processes. Pseudopolyps are benign cancer tumors;
- Arthritis. The dependence of the occurrence of complications on the severity of UC has not yet been established. It is chronic and tends to migrate (affects joints). Arthritis most often affects the knees and elbows;
- Thrombophlebitis (inflammatory process inside the veins with the formation of a blood clot). Appears due to the fact that the blood clotting system is disturbed, usually in the lower part of the body. The complication is more common in women than in men;
- Skin diseases. The probability of occurrence is about 20%. Eczema, dermatitis and rashes, as well as gangrene, may appear;
- Secondary amyloidosis (a general disease with disruption of all organs). It occurs less frequently than all the above complications. At this point in time, no more than 17 cases have been registered;
Folk remedies
In medical therapy, it is also allowed to use folk remedies, but only if the disease is at the initial stage of development and the treatment is agreed upon with the doctor. The most effective ways to treat the disease, according to patients, are fasting, refusing to eat animal foods, and switching to a raw food diet. Herbal remedies include decoctions of yarrow, alder cones, wormwood, sage, and potato juice.
- Pour 100 g of dried watermelon rind with 2 cups of boiling water, leave and strain. Take 100 g up to 6 times a day. This allows you to relieve inflammation in the intestines in acute and chronic forms of the disease.
- Potato juice perfectly relieves inflammatory processes in the intestines. It is enough to grate a potato, squeeze the juice out of it and drink it half an hour before meals.
- Take equal parts of peppermint leaves, chamomile inflorescences, and cinquefoil rhizomes. Infuse 1 tablespoon of the mixture for 30 minutes in 1 glass of boiling water, strain. Take 1 glass 2-3 times a day for colitis.
- Bird cherry helps to cure the symptoms of exacerbation. Traditional healers recommend preparing a decoction (one spoonful of flowers per glass of water). Take three times, ¼ cup every day.
How is diagnosis carried out?
Diagnosis of nonspecific ulcerative colitis is carried out using a number of laboratory and instrumental studies. Namely:
- Blood test (general). One of the characteristic features of the pathology is anemia with varying degrees of severity. And with massive bleeding, it takes the form of acute post-hemorrhagic. If the disease is accompanied by constant but slight blood loss, then the person will experience chronic iron deficiency. It is also possible to develop autoimmune anemia (formation of antibodies to blood cells). And in the acute form or exacerbation of the chronic form, leukocytosis is characteristic;
- Urinalysis (general). Informative only for severe UC. In this case, protein and red blood cells can be found in the urine;
- Blood test (biochemical). In case of UC, the analysis results will show a reduced content of total protein, albumin, as well as a decrease in the amount of iron;
- Stool analysis (scatological and bacterial). With UC, the stool sample will have an increased number of epithelial cells, leukocytes and erythrocytes, the microflora of the digestive organ will be severely disturbed, and the Triboulet reaction (to search for soluble protein) will be positive. A structural change in feces is also recorded; pus, blood, and mucus may be present;
- Endoscopy. Visual inspection of the organ using special instruments, as well as taking a sample of colon tissue for analysis (histological examination);
- X-ray of the colon. Characteristic phenomena are swelling, altered relief of the mucous membrane, ulcers;
Histological examination is designed to examine a tissue sample of the digestive organ. If the severity is mild, a large number of lymphocytes will be found in the sample.
In more severe cases - plasma cells and eosinophils. And in the sample taken from the ulcer there is fibrin (a protein formed during blood clotting) and granulation tissue.
In case of some complications, conducting research is simply dangerous for the patient’s life. For example, during dilatation, X-rays (irrigoscopy) are not performed, since there is a high probability of intestinal perforation. Instead, a general x-ray of the abdominal cavity is taken, which almost always shows the location of the lesion.
Treatment
Treatment of ulcerative colitis is complicated by the fact that its causes are not fully known. Therefore, the goal of therapy is to alleviate the patient’s condition, slow the progression of pathology and prevent complications. This can only be done if you consult a doctor in a timely manner.
Important: in order to achieve stable remission and improve the patient’s quality of life, you must strictly follow all medical recommendations.
In most cases, ulcerative colitis is not completely cured. You can only relieve symptoms for a while, but when exposed to unfavorable factors, they return. Therefore, treatment of pathology must be constant and comprehensive. It necessarily includes taking medications and a special diet. All methods used are selected depending on the severity of the pathology, localization of the inflammatory process and the presence of complications. In case of severe exacerbation, the patient must be hospitalized; in other cases, it can be treated at home.
If conservative therapy is ineffective or if the pathology is severe, the patient may be recommended surgical intervention. Surgery is necessary for severe internal bleeding, intestinal perforation, or the presence of tumors. With the help of resection of the affected area of the intestine, colitis is cured, but the patient must still follow a special diet for the rest of his life.
Diet
Diet is the main method of treating colitis. In its acute course or during an exacerbation, it is necessary to completely refuse food and only drink water. For many patients this is not difficult to do, since appetite is greatly reduced. But it is also important to follow a special diet during the period of remission.
The diet of patients with ulcerative colitis should be gentle. It is necessary to exclude all rough foods, hot spices, marinades, sauces, fiber, and legumes. All products must be boiled and chopped. You need to eat food 5-6 times a day in small portions, warm. The basis of the diet should consist of animal proteins to improve mucosal regeneration processes. These are cottage cheese, white poultry meat, lean fish, and egg whites.
Only the right food choices will help maintain remission.
Medications
Drug therapy is also required to maintain stable remission. Medicines must be taken even in the absence of severe symptoms. These are anti-inflammatory drugs, immunosuppressants and anti-cytokines to suppress the activity of the immune system.
Anti-inflammatory drugs for the treatment of ulcerative colitis include aminosalicylic acid derivatives. This is Mesalazine or Sulfasalazine. In severe cases of pathology, corticosteroids may be prescribed. But they must be used with caution and for a limited time. Drugs are constantly taken to suppress the activity of the immune system. These are immunosuppressants - Methotrexate, Azathioprine, Cyclosporine, and Infliximab.
With exacerbation, the number of medications increases. Antidiarrheals, prokinetics, and painkillers are taken. Sometimes it is necessary to take antibiotics if an infectious inflammation develops; to normalize the electrolyte balance, rehydration solutions, potassium and magnesium supplements are prescribed, and for anemia, iron supplements.
Important: all medications can only be taken as prescribed by a doctor, since many of them can lead to a worsening of the patient’s condition.
Folk remedies
Sometimes, if the disease is not severe, folk treatment will help prolong remission. Various decoctions and infusions of herbs normalize the water-salt balance in the body, stop bleeding, reduce the severity of the inflammatory process, and restore the mucous membrane. The following plants are most effective for UC: nettle, chamomile, yarrow, mint, blueberries, currant leaves, celandine, cinquefoil, wormwood, pomegranate peel.
It is also recommended to do microenemas with sea buckthorn oil, take propolis tincture, and bee bread. Grated apples, vegetable juices, and a mixture of apple juice and honey help alleviate the patient's condition. Ginseng root, which can be drunk in the form of a water or alcohol infusion, is also effective. But any traditional methods can only be used under the guidance of a doctor and in addition to traditional therapy.
Treatment of ulcerative colitis
The main goal of the course of treatment is to suppress foci of inflammation, relieve symptoms, prevent exacerbations and generally improve a person’s quality of life.
Therapy is based on the following means:
- Sulfasalazine;
- Mesalazine;
- Corticosteroid group;
- Immunosuppressive group;
According to studies, some medications, for example, sulfasalazine, cause side effects in almost half of the cases of use.
The reason is sulfapyridine in the drug.
The principle of action is based on the fact that when it is broken down by bacterial waste products, 5-aminosalicylic acid has an anti-inflammatory effect.
The drug mesalazine works a little differently, but is highly effective.
When ingested, the components of the drug block the synthesis of leukotrienes, which are active mediators of inflammation (leukotriene B4, prostaglandins, etc.).
Modern medicine successfully uses several forms of the drug with the active ingredient 5-aminosalicylic acid (5-ASA), but without the use of sulfapyridine. This is required to reduce the occurrence of side effects.
The drugs have different mechanisms for releasing the active substance. As a rule, they are all available in the form of tablets, the dissolution rate of which directly depends on the acidity of the stomach. Such drugs include:
- salofalk,
- pentasa,
- mesacol,
- salosinal.
Diagnostics
One of the main manifestations of colitis is the presence of mucus and blood in the stool and frequent bowel movements. The diagnosis is confirmed by the results of ileocolonoscopy and biopsy.
There are also markers of inflammation in the blood test: leukocytes, platelets, ESR, globulin and C-reactive protein increase, hemoglobin and red blood cell concentration decrease. Inflammation is indicated by an increase in fecal calprotectin levels.
Given the similarity of symptoms, it is important to exclude other pathologies during diagnosis: dysentery, amoebiasis, helminth damage, Crohn's disease, cancer.
Treatment of ulcerative colitis of the intestine
- With moderate exacerbation, colitis therapy is carried out on an outpatient basis.
- Sulfasalazine and tofacitinib are used to heal the mucosa and fight inflammation. Mesalazine, in addition to tablets, is used in local forms, including microenemas, suppositories, and rectal foam.
- In the acute phase, if the effectiveness of 5-aminosalicylic acid decreases, hormones (dexamethasone, prednisolone) are prescribed in combination with mesalazine and sulfasalazine. In case of hormone resistance, biological products are used - Humira, Remicade.
- Immunosuppressants help suppress the abnormal response of the immune system. Antibiotics, antidiarrheal drugs, painkillers, and iron supplements are prescribed (as needed). In case of exacerbation, enteral or parenteral nutrition will be used.
- Surgical intervention (proctocoectomy) is performed in exceptional cases. With ileoanal anastomosis, a fragment of the rectum is left, connecting it to the ileum, which makes it possible to remove waste naturally, without the use of a special reservoir.
Improves the condition and allows you to maintain remission:
1) Therapeutic diet.
You need to eat fractionally, without loading the digestive system and, at the same time, not allowing the body to experience a deficiency of nutrients.
Remove foods that cause an aggressive immune response and inflammation from your diet:
- spices;
- sugar and its substitutes;
- fibrous fruits, vegetables;
- nuts (including oil), seeds;
- dairy products (for lactose intolerance);
- whole grain cereals;
- caffeine, alcohol;
- carbonated drinks;
- legumes;
- popcorn;
- products containing sulfur and sulfates (shellfish, garlic, onions);
- cold drinks.
Allowed:
- white flour crackers, dry white bread;
- weak meat or fish broth (can be added with semolina or rice);
- lean meat, steamed fish, in the form of a soufflé;
- butter;
- steam omelette, soft-boiled eggs;
- pureed cottage cheese.
During the period of remission, crumbly porridges (with the exception of pearl barley and millet), cream, sour cream, yogurt, boiled and then pureed vegetables, peeled fruits, oranges, herbs, marmalade, and marshmallows can be introduced into the diet.
2) Omega-3 fats.
Products with eicosapentaenoic acid block leukotrienes - compounds that provoke allergic reactions and bronchospasms.
As prescribed by your doctor, you can take dietary supplements containing omega-3, fish oil, or replenish reserves of unsaturated acids, including sea fish (mackerel, tuna, catfish) in your diet.
Oleic acid is indicated for colitis. The substance is found in olive oil. For prevention, it is enough to consume 2 tbsp. product per day.
3) Probiotics.
By populating the digestive tract, they support the body’s ability to fight infection and absorb nutrients, displacing pathogenic bacteria, yeast, and fungi.
Normally, the intestinal microflora is filled with 85% beneficial bacteria and 15% harmful ones. If the balance is disturbed in favor of “bad” bacteria, dysbiosis develops.
Probiotic supplements will help restore balance, as will yogurt, miso, pickled vegetables, kimchi, natto and other fermented foods.
4) Iron-containing products.
A lack of red blood cells is one of the signs of colitis. The symptom is anemia. Anemia is caused by bleeding ulcers and blood loss during defecation.
Iron is necessary to support metabolism, energy, and enzyme production. Its deficiency indicates that tissues and cells do not receive enough oxygen. Weakness and chronic fatigue appear.
Iron is contained in beef liver, chard, lentils, spinach, tuna, baked potatoes, buckwheat, oatmeal, and egg yolks.
5) Folates.
Water-soluble compounds are involved in cell regeneration, DNA replication, the functioning of the circulatory system, and support immune function. Reduce the risk of colorectal dysplasia and cancer in chronic colitis.
Asparagus, avocados, broccoli, liver, cabbage, quinoa, wheat germ, leafy greens, and eggs are rich in folic acid.
6) Curcumin.
Long-term use of corticosteroids (relieving pain) is fraught with damage to the mucous membrane. Curcumin heals the intestines by maintaining the integrity of the membranes and the growth of beneficial bacteria. Taking curcuminoid reduces the risk of relapse of colitis, allowing you to maintain remission for a long time.
The anti-inflammatory drink is made from a glass of coconut milk and the same amount of water, a teaspoon of turmeric, honey and ghee (1 tablespoon of each component). Heat milk and water (do not allow it to boil), add oil, honey, turmeric and heat for another 2 minutes. You can beat it with a blender and drink it warm.
Direction of action of drugs and review of effective agents
The purpose of taking these tablets is to relieve the symptoms of the disease and eliminate the cause of its occurrence.
Sulfasalazine
Has a strong anti-inflammatory effect. It is based on the immediate suppression of the focus of pathogenic microorganisms by disrupting the metabolism in their cells.
The active substance does not allow the DNA chain to multiply. Sulfasalazine is indicated for patients over 16 years of age, 1-2 grams 3-4 times a day in the active stage. Next - 500 mg of the substance until the end of the maintenance phase. The medicine has a number of side effects, so it is prescribed only by a specialist.
Mekasol
Also an antimicrobial drug with a wide spectrum of effects. It is produced in the form of tablets that should be consumed an hour before meals 2-4 times a day. If there are no side effects and abnormalities in the liver and kidneys, then the dose is 50 mg per kilogram of the patient’s body weight.
Intestopan
A drug that inhibits the growth of pathogens. Quickly improves the patient's condition, eliminating bloating and relieving intestinal disorders.
At the stage of exacerbation of the disease, take 1-2 tablets 5-6 times a day immediately after meals. The duration of therapy is ten days. Extending the period of use is strictly prohibited.
Mexaza
It has the appearance of pills, prohibited from crushing and chewing. Has enzymatic and antimicrobial effects. Take the medicine with food or immediately before meals.
Take three times a day, one pill at a time. The duration of treatment is a week. In extreme cases, the attending physician may extend the course to four weeks, but under strict monitoring of the patient's vision.
Bifidumbacterin
A drug that populates the intestines with bifidobacteria. The prescription scheme is very simple, so patients often choose to take it. Two capsules of the medicine are taken before meals three times a day, with a couple of sips of water. The duration of therapy is quite long, it is six weeks.
Festal
An enzyme preparation approved for long-term use, up to three months. Prescribe 20 mg of the active substance three times a day after meals. Festal helps improve the digestion of food, preventing it from remaining in the intestinal lumen.
Panzinorm
This is also an enzyme class product. It is taken with every meal. Two tablets - with the main meal and one with a snack. You are allowed to drink up to 15 doses per day.
No-shpa
Antispasmodic. Relaxes the smooth muscles of the intestines, relieving pain. For chronic colitis, take two tablets twice a day; in the acute stage of the disease, it is allowed to increase the number of doses up to three times. Typically the course lasts three days, but if necessary it can be extended to five.
Bellasthesin
Painkiller. Admission - only for therapy in adult patients (over 14 years of age). For any form of the disease, 1 capsule is prescribed three times a day. The maximum course of admission is five days.
Rectal suppositories
Rectal suppositories have powerful local anti-inflammatory properties. This method of treatment has been known for many decades. It has proven its effectiveness in practice.
Rectal suppositories, penetrating the rectum, not only stop the inflammatory process on the mucous membrane of the organ, but also anesthetize this affected area.
It is advisable to use them not only for medicinal, but also for preventive purposes. People often resort to the use of such medications when intestinal inflammation occurs frequently.
One of the most effective suppositories that quickly relieves the symptoms of this pathology is Salofalk.
This is an excellent remedy that has a pronounced analgesic and anti-inflammatory effect. Within just a few days of using it, the patient can feel a positive result.
It is advisable to use Salofalk in the presence of rectal fissures and other manifestations of damage to the tissue surface of the intestine.
The drug has wound-healing properties, which makes it indispensable in the presence of complications of colitis.
Calcium carbonate, acidin-pepsin, hydrochloric acid
For the treatment of colitis, many doctors recommend the use of cholinergic drugs and adrenergic blockers, indicating their high effectiveness. The use of these drugs is allowed only under the supervision of a doctor in a hospital. They can cause complications on the cardiovascular system and provoke exacerbations of other diseases.
Cells that produce mucus in the lining of the intestine begin to intensively produce mucus during inflammation. This mucus has a different chemical composition, different from normal, it is more aggressive. Therefore, being in the intestinal lumen, such mucus in a certain amount is a strong irritant, forcing the intestine to accelerate the expulsion of the contents. To avoid such a process, enveloping and astringent agents are recommended so as not to irritate the intestinal mucosa. As a result, irritation should decrease, and the production of mucus itself will decrease.
Calcium carbonate is considered the best remedy for the treatment of colitis, as well as herbal remedies.
Prescribe 1-1.5 g of calcium carbonate orally after meals, 1.5 hours later. If, with irritable bowel syndrome, a decrease in the acidity of gastric juice is detected in the patient’s body, it is recommended to take acidin-pepsin or hydrochloric acid during meals. It is preferable to take enzyme preparations, for example panzinorma-forte, if there is no reliable data on a decrease in acidity.
Vaseline oil
When treating colitis, Vaseline oil is preferable from oil laxatives, since it lubricates the intestinal wall without irritating it, softens feces, accelerating their movement to the exit (use no more than 2 tablespoons per day orally); olive oil (taken on an empty stomach followed by mineral water 200-300 ml); Castor oil has a very good effect in the treatment of colitis (15-30 ml taken orally), but intestinal reactions do not occur with prolonged use. Castor oil is more appropriate for occasional constipation.
Sources
https://vrachmedik.ru/813-lechenie-kolita.html https://gastrocure.net/bolezni/kolit/lecheniyu-kolita-medikamentoznymi-sredstvami.html https://jeludokbolit.ru/kolit/lechenie-kolita- kishechnika-medikamentami.html https://ozdravin.ru/bolezni-kishechnika/effektivnye-lekarstvennye-preparaty-pri-lechenii-kolita-kishechnika.html https://www.kolit.su/lechenie-kolita/preparaty-dlya- lecheniya-kolita
Diversify your diet
Our body is a complex system of interconnection of everything and everyone. To maintain processes in proper condition, they need food.
By limiting ourselves in one food or another, we deprive our body of the opportunity to receive the necessary nutrients (of course, I don’t mean fast foods and other obviously harmful products). Read more about the benefits of vitamins in the articles “Extraintestinal manifestations of UC and CD: causes, types and methods of treatment” and “Useful supplements to the main therapy of UC and CD.”
Focus your attention on eating protein-containing foods, such as eggs, chicken, turkey, fatty fish, cottage cheese and others like them. Protein is the basis for the synthesis of new cells and restoration of damaged ones.
Omega-3 is the most beneficial fatty acid. Omega-3 promotes the regeneration of damaged tissues (including ulcers and erosions in the gastrointestinal tract), reduces the risk of developing cancer, normalizes hormonal balance, fights depression and allergies, and much more. etc.
Fiber, found in fresh vegetables and fruits, as well as cereals, helps remove toxins from the body. Toxins are poison and need to be gotten rid of. Toxins provoke the synthesis of antibodies by our immune system, and you and I know that it is the excessive activity of the body's defenses that is the presumed cause of ulcerative colitis .
Saturate yourself with beneficial bacteria. The main sources are high-quality fermented milk products (kefir, yogurt, bifidoc, etc.). Good microflora contributes to the coordinated functioning of the gastrointestinal tract and the entire body as a whole. The main activity of beneficial intestinal microbes is to ensure the absorption of substances, lipid metabolism, and the decomposition of bile acids and proteins. Consequently, without good microflora, proper digestion processes are impossible .
By the way, I recently listened to a radio broadcast where a doctor answered questions from listeners. So he said that if it is possible to get vitamins and minerals from regular food, and not from various vitamin complexes, then it is better to take advantage of it.
Examination for suspected colitis
The attending physician must examine the patient. The final diagnosis is made based on the results of colonoscopy or sigmoidoscopy. These studies allow you to assess the condition of the colon mucosa and identify ulcerative defects. Before colonoscopy and sigmoidoscopy, patients need to carefully prepare. It is necessary to cleanse the large intestine.
Irrigoscopy is often performed. It allows you to evaluate the shape, extensibility and condition of the folds of the intestine. Examination of patients often includes contrast radiography. A very effective diagnostic method is computed tomography. Additionally, the following laboratory tests are carried out:
- stool occult blood test;
- coprogram;
- sowing material on nutrient media;
- immunological research;
- general and biochemical blood tests.
Antineutrophil antibodies are often detected in the blood of patients. A cytological examination may be required to assess the condition of the cells. To do this, a piece of the intestinal mucosa is taken at the site of inflammation.
Drug therapy for colitis
When a patient is diagnosed with ulcerative colitis, the doctor develops an individual treatment regimen. Recently, herbal medicine has become increasingly popular, but it can only perform a supportive function and is not suitable as the only method of therapy.
Treatment of ulcerative colitis with drugs is prescribed to achieve the following goals:
- reducing the number of relapses;
- prolongation of remission periods;
- reduction of side effects from treatment;
- improving quality of life;
- minimizing the risk of developing cancer.
After the patient’s condition improves, the doctor must adjust the treatment regimen and dosage, since the drugs used have a negative effect on all organs and systems of the body.
Below are groups of medications that are used to treat ulcerative colitis.
Medicines 5-ASA or aminosalicylates
Drugs in this group are used to stabilize the patient’s condition and increase the duration of remission. In their chemical structure they are close to aspirin. The advantage of such medications is that they can be delivered directly to the inflamed areas through enemas.
The greatest effectiveness was shown by the oral use of such medications, but the problem was that the main amount of the active substance did not reach the colon, since it was absorbed in the stomach and small intestine.
The solution to the problem was the creation of chemically stable formulas that retain their properties when passing through the human gastrointestinal tract and act directly on the diseased areas of the intestine.
In the treatment of ulcerative colitis, drugs such as:
- Mesalamine. The active substance is covered with a special coating that withstands the effects of gastric juice. Thanks to this, the tablets pass through the stomach and intestines without damage, and then dissolve and release the main component 5-ASA. The exact dosage is prescribed by the doctor. The standard treatment regimen is 800 mg 3 times a day for exacerbation, 800 mg 2 times a day for remission. If the drug does not have a significant effect, then corticosteroids are prescribed instead.
- Sulfasalazine. For many years, this drug has been used to prolong remission in patients with mild forms of the disease. It helps reduce the inflammatory process, reduces pain and prevents bleeding. It has side effects such as anemia and gastrointestinal disorders.
- Dipentum, Pentaza, Colazal. These drugs also have the ability to reach foci of inflammation in the large intestine.
Corticosteroids, or drugs containing hormones
They are more powerful anti-inflammatory drugs than 5-ASA. Another advantage is that they are highly effective when taken orally, although they do not directly affect the inflamed area of the intestine. When they enter the bloodstream, they begin to have a healing effect on the entire body. These drugs show high effectiveness in the treatment of ulcerative colitis.
The most well-known medications are Hydrocortisone and Prednisolone.
If the patient is in critical condition, then corticosteroids are administered intravenously; a significant improvement in the patient's condition is observed within a few days. In the treatment of ulcerative colitis, these hormonal drugs are used only during exacerbation of the condition; they are not suitable as maintenance therapy during remission due to the abundance of side effects.
The occurrence of side effects depends on the dosage and duration of medication use. If a patient takes high doses of corticosteroids for a long time, he may develop the following serious complications:
- increased amount of body hair;
- rapid weight gain;
- mental disorders - depression, mood swings, increased nervousness;
- eye diseases (cataracts and glaucoma);
- constant weakness;
- diabetes;
- gradual thinning of bone tissue;
- decreased production of cortisol by the adrenal glands.
When undergoing treatment with corticosteroid drugs, the patient is under constant medical supervision. Dosages are prescribed strictly individually, increasing or decreasing the amount of medications used occurs gradually, usually over the course of a week. This is done in order to reduce possible negative consequences that may occur with a sharp increase in the dose of the drug or with its rapid withdrawal.
In addition, corticosteroid therapy is carried out as soon as possible so that the benefits to the body are greater than the side effects received. During the treatment period, the patient is additionally prescribed calcium supplements and food with a high content of this microelement. This is done to prevent the development of osteoporosis and the leaching of large amounts of calcium from bone tissue.
It is important to remember that self-medication with this group of drugs is unacceptable - it can lead to irreversible consequences, which are sometimes impossible to correct.
Immunomodulators
This group of drugs is used to suppress the patient’s own immunity. The fact is that with colitis, immune cells begin to destroy healthy body tissues and beneficial bacteria. This happens due to an autoimmune failure, the nature of which is not completely clear to doctors.
Immunomodulators weaken the effect of immune cells on the tissues and systems of the body, but at the same time the risk of infectious diseases increases, as the immune system is weakened.
The most popular immunomodulators are:
- Cyclosporine. One of the most powerful medicines. It is used when a patient develops severe colitis or has to delay surgical intervention. The medicine has side effects: the patient experiences seizures, blood pressure increases, and kidney function may be impaired.
- Purinethol. The drug reduces the activity of leukocytes; higher doses are used to prevent organ rejection. Low doses successfully treat ulcerative colitis.
- Methotrexate. A combined drug that has both immunomodulatory and anti-inflammatory effects. Side effects include liver cirrhosis and pneumonia, and it is not used to treat pregnant women.
Preparations containing monoclonal antibodies
These medicines are innovative developments. The principle of their action is as follows: these antibodies specifically interact with inflamed elements.
The body receives a signal about the presence of “problems” and copes with them independently. The huge advantage of such drugs is that they affect only the affected cells, healthy tissues remain untouched.
In addition, in agreement with the attending physician, the patient can use some traditional medicine recipes. For example, drink potato juice, drinks made from raspberry and strawberry leaves, decoctions and tinctures of medicinal herbs. You can do microenemas, use suppositories with sea buckthorn oil. It is possible to prescribe vitamin complexes, since a weakened intestine is not able to obtain the required amount of nutrients from food.
Ulcerative colitis is not a death sentence for the patient. If you follow all medical recommendations, dietary nutrition, correction of your daily routine and great motivation to obtain a positive result, it is possible to achieve long-term remission.
Diet
In case of illness, strict adherence to the diet is necessary:
- exclude fresh fruits, vegetables, canned food,
- food should be mechanically and chemically gentle,
- food temperature - 30-35 degrees,
- fractional meals 4-5 times a day,
- Therapeutic diet No. 4 is recommended.
An imbalance of vitamins and impaired absorption of microelements is compensated by taking complex medications (duodevit, oligovit, unicap, etc.)
Patients with severe forms during periods of severe exacerbation and loss of body weight may be prescribed parenteral nutrition for a short time.
Normalization of stool
Colitis manifests itself as both constipation and diarrhea. Both symptoms are unpleasant and require specific therapy.
What to do if you have diarrhea
Indigestion in the form of diarrhea occurs from inflammation of the cecum and ascending colon. For ulcerative colitis, antibiotic-associated diarrhea, and pseudomembranous colitis, taking medications based on loperamide is prohibited.
To stop diarrhea due to inflammation of the mucous membrane of the large and small intestines:
- Tansal will have an astringent and anti-inflammatory effect for colitis. Contains salicylate and tanalbin. Take a tablet 3 times a day;
- Allylsate is an alcoholic extract from garlic. Suppresses putrefactive phenomena in the intestines, normalizes stool. 10-15 drops of Allylsate are added to 30 ml of milk and drunk three times a day before meals;
- Smecta will stop diarrhea and absorb microbial toxins. Approved for use in infants, pregnant women and lactating women. Dissolve a packet of powder in a glass of water and drink 3-4 times a day;
- Bevisal – contains salicylate, bismuth salt and belladonna extract. It has a complex antimicrobial, relaxing, anti-inflammatory and astringent effect. Take one tablet three times a day.
A dangerous complication of diarrhea is dehydration. The patient needs plenty of warm drink - weak tea, rosehip decoction, compote, clean water. Salt rehydrants - Regidron, Humana, Oralit - replenish moisture loss well. A packet of powder is dissolved in a liter of water and drunk in 3-4 doses.
What to do if you are constipated
Left-sided chronic colitis is manifested by periodic constipation. Pharmacological agents will come to the rescue:
- rectal suppositories Bisacodyl, Dulcolax, as well as suppositories with rhubarb, sea buckthorn, glycerin;
- Guttalax, Regulax, Slabicap drops;
- laxative Forlax or Fortrans;
- syrups with lactulose;
Laxatives cannot be used constantly, constipation will only worsen, and emptying without medication will become impossible.
Surgery
There are absolute and relative indications for surgery.
Absolute readings:
- suspected perforation;
- acute toxic dilatation of the colon that does not stop within 6-24 hours;
- profuse intestinal bleeding;
- paracolic infiltrates;
- intestinal obstruction;
- colon cancer;
- severe perianal lesions;
- fulminant course of ulcerative colitis lasting more than 7-10 days in the absence of effect from conservative treatment.
Relative readings:
chronic continuously relapsing course of UC for 10 years without positive dynamics in the morphology of the colon wall.
The following types of surgical interventions exist:
- palliative operations - ileostomy;
- radical operations - subtotal resection of the colon with the application of ileo- and sigmostoma, colproctectomy with ileostomy according to Brooke or retaining ileostomy according to Kock;
- restorative and reconstructive operations.
Palliative operations
These operations involve temporarily or permanently disconnecting all (ileostomy) or part (colostomy) of the colon.
Recently, ileostomy is more often performed, since in UC the inflammatory process can spread above the stoma.
The most adequate is Brooke's ileostomy - terminal eversion (inverted). It is more secure. With this type of operation, the likelihood of complications (fistulas, abscesses, hernias and retraction of the removed intestine) is minimal. In addition, an ileostomy is easy to care for and can be used with different types of colostomy bags.
In obese patients, a double-barreled ileostomy with one protrusion above the skin according to Thornebull is often performed. However, after its implementation, significant difficulties arise in regulating the release of liquid contents and gases. Recently, a “holding” ileostomy according to Kock has been developed, which minimizes this disadvantage.
There is another type of ileostomy - anal. In this operation, the ileum is brought down into the perineum and a direct ileoanal anastomosis is performed. Many patients insist on this type of surgery to preserve the natural way of excrement. However, in this case, great difficulties may arise when using a colostomy bag.
Radical operations
In severe forms of ulcerative colitis and acute conditions, operations are reduced to ileostomy (preferably with the creation of a valve reservoir according to Kock).
The planned radical operation is a subtotal colectomy with the application of a reservoir small intestinal ileorectal anastomosis. Often this surgical intervention is performed with the imposition of a temporary (unloading) ileostomy.
In young patients with fulminant ulcerative colitis, total colectomy with the formation of an ileorectal pouch should be chosen.
Restorative and reconstructive operations
Some time after the colectomy, it is possible to perform an operation to restore the continuity of the colon and remove the colostomy.
Currently, modern technologies for carrying out such operations have been developed (in particular, at the A.A. Vishnevsky Central Military Clinical Hospital).
These surgical interventions are an important part in the complex treatment of colostomy patients. Medical practice shows that it is advisable to perform operations no earlier than 6 months after the first operation in cancer patients and, if possible, strive for early elimination of colostomy in other cases.
Carrying out restorative and reconstructive operations allows patients to return to a full lifestyle.
Under no circumstances should you self-medicate if you are diagnosed with UC. This disease requires the prescription of serious medications, which only a doctor can correctly determine. However, we hope that this article will help you navigate modern treatment methods.
Prognosis and prevention
Since the cause of the development of nonspecific ulcerative colitis is not clear, it is impossible to prevent its occurrence. There are only a number of certain rules, following which you can increase the duration of remission and reduce the frequency of periods of exacerbation. These include:
- timely visit to the attending physician;
- taking prescribed medications regularly;
- following a special diet;
- stop using non-steroidal painkillers (Ibuprofen, Naproxen); you can replace them with Paracetamol or Efferalgan.
The diet for UC includes avoiding alcohol, spicy, salty foods, as well as coarse vegetables and fruits. In addition, it is recommended to exclude fresh tomatoes from the diet or reduce their quantity to a minimum. Under no circumstances should you eat dry food; the menu should include porridge and soups every day.
In the absence of complications, the prognosis for the treatment of nonspecific ulcerative colitis of the intestine is generally favorable. With timely initiation of therapy and subsequent administration of maintenance medications, relapses in patients with ulcerative colitis occur on average once every 5 years, and in some patients the period of remission can last up to 15 years. According to statistics, surgery is performed in 20% of patients, and the development of malignant neoplasms occurs in only 3–7% of all diagnosed cases.
Share the article on social media. networks:
Symptoms
The leading sign of chronic ulcerative colitis is considered to be persistent, prolonged bowel dysfunction even during remission; in the acute phase there are up to 15-20 bowel movements.
Other symptoms:
- impurities of mucus, pus and blood in the stool;
- pain (for example, cramping during bowel movements);
- psychoneurological disorders with hyperhidrosis, fatigue, excitability;
- rumbling in the stomach, tension in the abdominal muscles;
- flatulence, foul-smelling gases.
An endoscopic examination reveals ulcerative lesions and hyperemia of the mucous membranes . The patient's health suffers moderately, and the temperature rises.
Photo of ulcers on the intestinal wall
Types of colitis
Despite the fact that the causes of this disease are not yet fully understood, several types have been identified based on etiology:
- Infectious colitis. The cause of the disease may be bacteria such as staphylococcus and streptococcus, progressing against the background of dysentery. Infections are usually activated in the body as a result of a sharp decrease in immune activity. In this situation, rapid proliferation of pathogenic microorganisms in the colon is noted.
- Ischemic colitis. This colitis can form as a result of the development of atherosclerosis in the abdominal aorta.
- Radiation colitis. Sometimes isolated cases of this type of colitis are identified, when the causative factor is chronic radiation disease.
- Toxic colitis. A factor that provokes the formation of colitis is the use of certain medications that have a toxic effect on the mucous membrane of the organ. This is usually the unauthorized use of various dietary supplements and non-steroidal anti-inflammatory drugs.
- Ulcerative colitis. This type of disease can be encountered more often than others, but the reasons for its occurrence cannot be fully explained. With ulcerative colitis, ulcers form on the wall of the colon and quickly spread over the entire surface.
Now we should move on to a detailed consideration of methods for diagnosing the disease.
What is chronic ulcerative colitis
Chronic ulcerative colitis (nonspecific ulcerative colitis, abbreviated as UC) is a chronic inflammation of the lining of the colon with the formation of ulcerative defects. Considering the polyetiological nature of the disease, various external and internal factors can be the causes of the development of UC.
The chronic form of the disease alternates between periods of remission and exacerbation . Remission is characterized by the absence of significant symptoms, but there is digestive discomfort and periodic pain. The acute phase of the disease is characterized by a pronounced course with pain in the abdominal space, stool disturbances, fever, intoxication and other manifestations.
Chronic UC occurs in every 3-15 people per 100,000 of the population, with most cases occurring between the ages of 14-35 years, and is less common in elderly and geriatric patients.
Important! UC often disguises itself as Crohn's disease, but in ulcerative colitis, ulceration and inflammation affect only the mucous epithelium of the rectum and large colon.
ICD-10 code - K51.0 - ulcerative (chronic) enterocolitis.
Classification
Nonspecific chronic ulcerative colitis is classified according to severity, complications, frequency of relapses and exacerbations, and cause of occurrence .
The localization of the inflammatory-ulcerative focus is of significant clinical importance:
- left-sided - inflammation occurs in the colon, characterized by diarrhea, blood in the stool, pain in the left side of the peritoneum;
- total - inflammation and ulcerative-erosive process are generalized, this form is the most dangerous for the health and life of the patient, often leading to severe complications, such as massive blood loss, intestinal perforation, peritonitis;
- subtotal - the ulcerative process covers most of the intestinal tract;
- distal - the sigmoid colon is involved in the pathological process (proctosigmoiditis).
According to the nature of the course, ulcerative colitis is distinguished between recurrent, fulminant, acute nonspecific and chronic nonspecific ulcerative colitis.
Danger and complications
Complications of chronic ulcerative colitis can be divided into local and general.
Locals include:
- perforation and damage to the integrity of the colon;
- strictures, adhesions;
- toxic megacolon;
- cracks, fistulas;
- secondary inflammation of the submucosal tissue - paraproctitis;
- massive intestinal bleeding;
- cancer.
General complications are caused by extraintestinal manifestations and occur with aggravated course of the disease. The pathological process involves articular structures, autoimmune disorders, eye and skin lesions occur.