The retina is a very thin layer of tissue made up of nerve cells. The retina covers the inside of the eyeball at the back.
Retinal tissue is a huge number of photoreceptors or light-sensitive cells, the main function of which is to convert light impulses into electrical ones. After such a transformation, electrical signals travel along the branches of the optic nerve to the human brain, where they are deciphered and become visual images, a picture that we see before our eyes.
The pathology “retinal dystrophy” is a general term that characterizes a significant group of various heterogeneous disorders.
Common signs of all types of retinal dystrophy are the progression of visual dysfunction, as well as degenerative changes in the retinal fiber.
Currently, the main causes of early decline in visual acuity, including blindness, are associated with dystrophic diseases of the retina.
Their specificity lies in the fact that the course of the pathology is slow but steady, and is characterized by a gradual decrease in the visual function of the eye.
Factors that can provoke the development of pathology may be:
- old age due to involution processes in the body;
- hereditary predisposition;
- vascular diseases, including hypertension, atherosclerosis;
- diabetes;
- unhealthy diet, vitamin deficiencies;
- smoking;
- excess weight;
- excessive sun exposure;
- some viral diseases;
- stress, nervous shock.
What is retinal dystrophy
Faced with this diagnosis for the first time, people are looking for an answer to the question, retinal dystrophy, what it is. The disease is characterized by damage to the eye tissues, leading to their complete death. The cause may be either a disturbance in the metabolism of nutrients in the body or a lack of nutrients and vitamins. The advanced stage of the disease leads to complete loss of vision, without the possibility of its restoration. It is very important to diagnose the disease in a timely manner and begin its treatment immediately. This diagnosis can be confirmed by contacting a specialist - an ophthalmologist. The risk group for retinal dystrophy includes not only adults, but also children.
Retinal dystrophy is a rather dangerous disease that manifests itself with age-related changes in the functionality of the eyeballs.
Retinal dystrophy is an irreversible degenerative disease.
Prevention
Most often, the risk of developing retinal dystrophy is determined by genetic predisposition. Such heredity cannot be prevented; genes will be systematically passed on from generation to generation. But the problem can be solved if the disease is diagnosed in a timely manner and treatment is started. Therapy should be comprehensive; in addition, it is important to eat rationally and take a course of vitamins.
Often, retinal degeneration goes undetected until the late stages of the disease. In this case, the symptoms become obvious and vision rapidly deteriorates.
It is important to carry out genetic diagnosis of each patient. This makes it possible to determine a clinical diagnosis, determine the mode of inheritance of this incurable disease, as well as provide detailed consultation to the family and indicate the risk of transmission of this pathology.
In addition, consultation with a geneticist is necessary to select the optimal treatment method. New treatment methods are currently being developed, and new drugs are constantly being tested to treat this disease.
Classification of the disease
According to statistical data obtained as a result of a study of the disease, it was revealed that the disease is “getting younger” every year . Today, the group at risk includes not only older people, but also those who have a hereditary predisposition to eye diseases, as well as people leading an unhealthy lifestyle. Another important factor in the development of diseases associated with the sensory organs is ecology. Retinal dystrophy has several typologies.
Central retinal dystrophy
Central dystrophy is a process that originates in the molecular zone of the eyeball, developing due to irreversible aging of the body. The disease is dangerous due to complete, irreversible loss of vision. The treatment process is quite complicated, since the central part of the eye is affected. The diagnosis is divided into dry and wet retinal dystrophy.
Peripheral retinal dystrophy
Changes in the eyeball can be caused by trauma to the visual organs, as well as complications from the treatment of other diseases. Often the disease can be preceded by myopia and myopia at different stages. Today, with timely access to specialists, the disease is successfully treated surgically.
Types of disease
Source: Ayzdorov.ru
Retinal dystrophies can be divided into:
- Central and peripheral. Peripheral retinal dystrophy is most often present in myopic people. Reduced blood circulation in the eye with myopia leads to a deterioration in the delivery of oxygen and nutrients to the retina of the eye.
- Congenital (genetically determined) and acquired.
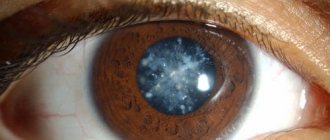
- “Senile” dystrophy develops most often after 60 years. This type of retinal dystrophy can be combined with the development of senile cataracts caused by the aging of the body.
- Retinal pigmentary dystrophy is associated with disruption of the photoreceptors responsible for twilight vision. This type of retinal dystrophy is quite rare and is a hereditary disease.
- White dot retinal dystrophy - usually occurs in childhood and progresses with age. This type of dystrophy is hereditary.
Depending on the nature of the damage, distinguish the following types of peripheral dystrophy:
- Lattice dystrophy. Usually inherited, men are most often affected. The lesion resembles a grate or rope ladder in appearance. As a rule, it affects both eyes at once. Often leads to retinal tears.
- "Snail trail" Dystrophic lesions form ribbon-like zones resembling snail tracks. May lead to large circular retinal tears.
- Frost-like. Usually hereditary, affects both eyes. Has characteristic yellowish-white inclusions on the retina.
- "Cobblestone pavement." The lesions are located far on the periphery, sometimes entire clumps of pigment are separated from them.
- Small cystic. It is distinguished by the presence of small cysts. More often occurs under the influence of injuries.
- Retinoschisis. Retinal dissection. It is more common in the elderly and nearsighted, and is sometimes inherited.
Depending on the size of the pathological process, it is customary to distinguish the following types of peripheral dystrophy:
- Peripheral chorioretinal dystrophy (with this pathology, the lesion affects only the retina and choroid);
- Peripheral vitreochorioretinal dystrophy (damage to the retina, vitreous body and choroid).
Lattice dystrophy is most often detected in patients with retinal detachment. A family-hereditary predisposition to this type of dystrophy is assumed to be more common in men.
As a rule, it is found in both eyes. It is most often localized in the upper outer quadrant of the fundus, equatorially or anterior to the equator of the eye.
When examining the fundus, lattice degeneration appears as a series of narrow white, fleecy stripes, forming figures resembling a lattice or a rope ladder. This is what obliterated retinal vessels look like.
Between these altered vessels, pinkish-red areas of retinal thinning, cysts and retinal breaks appear. Characteristic changes in pigmentation in the form of darker or lighter spots, pigmentation along the vessels. The vitreous body seems to be fixed to the edges of the dystrophy.
Dystrophy of the “snail track” type. The retina shows whitish, slightly shiny, streak-like inclusions with many small thinning and perforated defects.
Degenerative lesions merge and form ribbon-like zones, which in appearance resemble a snail's mark. Most often located in the upper outer quadrant. As a result of such dystrophy, large, round shaped tears can form.
Frost-like dystrophy is a hereditary disease of the retinal periphery. Changes in the fundus are usually bilateral and symmetrical.
On the periphery of the retina there are large yellowish-white inclusions in the form of “snow flakes”, which protrude above the surface of the retina and are usually located near thickened, partially obliterated vessels; there may be pigment spots.
Frost degeneration progresses over a long period of time and does not lead to rupture as often as ethmoid and trace cochlear degeneration.
Cobblestone degeneration is usually located far in the periphery. Individual white lesions are visible, slightly elongated in shape, around which small lumps of pigment are sometimes identified. Most often found in the lower parts of the fundus, although they can be detected along the entire perimeter.
Racemose (small cystic) retinal dystrophy is located at the extreme periphery of the fundus. Small cysts can merge to form larger ones.
In case of falls or blunt injuries, cysts may rupture, which can lead to the formation of perforated ruptures. When examining the fundus, cysts appear as multiple round or oval bright red formations.
Retinoschisis - retinal separation - can be congenital or acquired. More often this is a hereditary pathology - a malformation of the retina. Congenital forms of retinoschisis include congenital retinal cysts, X-chromosomal juvenile retinoschisis, when in patients, in addition to peripheral changes.
If there are also changes in the vitreous body, then tractions (cords, adhesions) are often formed between the changed vitreous body and the retina. These adhesions, joining one end to a thinned area of the retina, greatly increase the risk of ruptures and subsequent retinal detachment.
PRHD and PVHRD - what is the difference?
Peripheral retinal dystrophies are divided into peripheral chorioretinal dystrophies (PCRD), when only the retina and choroid are affected, and peripheral vitreochorioretinal dystrophies (PVCRD), when the vitreous body is involved in the degenerative process.
There are other classifications of peripheral dystrophies that are used by ophthalmologists, for example, according to the localization of dystrophies or the degree of danger of retinal detachment.
Peripheral chorioretinal dystrophy of the retina. In this case, the retina and choroid are damaged. The disease usually develops in people over 50 years of age. With this type, people cannot read books or drive a car.
Important
At the beginning of the disease, there are no symptoms, but then there is a distortion of straight lines, doubling of objects and the appearance of blind spots in the field of vision. In the advanced stage, complete loss of vision can occur.
Peripheral vitreochorioretinal dystrophy of the retina. Pvhrd of both eyes is a type of dystrophy in which the retina, the middle layer of the eye and the vitreous body are damaged so that detachment can even occur. Most often it occurs in people with myopia.
However, even with normal vision, heredity is an important factor. At the initial stage, symptoms do not appear in any way, and this pathology can only be detected using a three-mirror Goldmann lens.
Causes
Identifying the disease at an early stage is only the beginning of a long journey to be taken. It is very important to determine the causes of retinal dystrophy and what led to its development. Ophthalmologists identify the following reasons that can play a decisive role:
- complications after surgery;
- poor diet and bad habits;
- imbalance of nutrients in the body;
- dysfunction of the eyeball vascular system;
- diabetes mellitus, infectious and viral diseases.
With dystrophy, retinal tissue is destroyed, which, in turn, leads to a decrease in visual acuity.
Symptoms
But no disease occurs completely without symptoms.
Therefore, retinal detachment is difficult, but still, one can suspect. What should the patient pay attention to?
- Some patients note that even before diagnosis they noticed the effect of “flickering flies” before their eyes. This happened infrequently, but only after the eyes were under tension for a long time.
- Vision seems to be blurred. It seems that everything around is covered with a white haze. Washing your face, changing your contact lenses, or cleaning your glasses does not help get rid of this feeling.
- The field of view gradually narrows.
- A person is much less able to navigate and see in the dark.
- At the moment of visual strain, bright flashes of light appear.
- A person notices a violation of color perception.
If you notice one or several symptoms at once, you need to urgently visit a doctor.
When such a sensation haunts you constantly, and is not one-time, this means that the pathological process at this stage is in an active stage.
Symptoms
Symptoms of retinal dystrophy manifest themselves gradually and cause many difficulties in life. The early stage of the disease occurs without visible symptoms, but the disease can progress rapidly. A person experiences discomfort when blinking, which can be expressed as a burning sensation in the eyeball, a sharp drop in vision, loss of sharpness and various cloudings are observed. However, these symptoms may also indicate other possible problems in the body. It is very important that the final diagnosis is established after a complete examination and all necessary procedures. Symptoms:
- blurred vision in the evening;
- a veil before the eyes;
- sharp narrowing and distortion of the picture;
- flashes, “floaters” before the eyes;
- distorted perception of shapes, sizes and colors.
Symptoms of the disease
Dystrophic pigmentation is manifested by the following symptoms:
- Hemeralopia. This is a twilight vision disorder. Manifested by weakened vision and spatial orientation at night. Light sensitivity decreases, the process of dark adaptation is disrupted and the field of vision narrows. This sign appears first. Other symptoms appear after a few years.
- Deterioration of peripheral vision. Indicates that the side sticks have been damaged. The field of vision narrows, which means the disease is progressing. The process is gradually moving towards the center. The patient experiences tunnel vision, a condition in which the patient loses the ability to see peripherally. A person perceives an image falling on the central region of the retina.
- Decreased sharpness and color vision. This symptomatology is characteristic of the last stages of the disease. The patient is unable to distinguish one or more colors or their shades. The brightness and saturation of a certain part of the spectrum changes. Visual acuity decreases, and the patient will eventually become blind.
Pigmented foci resembling bone bodies appear on the periphery of the fundus. Their number is growing and occupying a large area. The vessels narrow, some areas of the retina become discolored, and choroidal vessels can be seen.
In the initial stages, the disease may have no symptoms. As a rule, parents begin to worry when the child begins to have difficulty oriented in space (especially in poorly lit rooms).
The most characteristic signs of retinal dystrophy include:
- Deterioration of peripheral vision up to the development of tunnel vision. A person does not notice objects and people located on his side. In the later stages of the disease, the patient may feel as if he is looking through a long tunnel or pipe. At the same time, he perfectly sees things that are right in front of him.
- Hemeralopia (night blindness). It manifests itself as a sharp decrease in visual acuity in the dark. Frequent stumbling and confusion in a dimly lit room is usually the very first sign of retinitis pigmentosa.
- Increased eye fatigue, glare, and in later stages – decreased visual acuity and inability to distinguish colors.
At the initial stage, retinal pathology develops without noticeable signs. After a significant deterioration in local blood supply, patients begin to notice:
- Difficulty in orientation.
- Floaters, bright flashes, lightning, blurry vision.
- Deterioration or complete loss of color vision.
- Blurry, distortion, blurring of side objects.
- Decrease in visual acuity.
- Difficulty reading without bright lighting.
The development of complications is facilitated by any vibrations, including intense physical activity and immersion under water.
Identification of the first warning signs of the disease requires immediate consultation with an ophthalmologist. Failure to see a doctor in a timely manner can result in thinning, rupture, detachment of the retina and complete loss of the ability to see.
Diagnosis of the disease
Dystrophic changes in the retina of the eye require a competent specialist approach and a complete examination of the ocular structure. An integrated approach is more appropriate here, during which a complete history will be prepared. The following activities are mandatory during diagnosis:
- perimetry – study of peripheral vision in order to determine its boundaries;
- ophthalmoscopy – examination of the fundus of the eyeball;
- biomicroscopy – analysis of the structure of the eyeball;
- adaptometry – study of light perception;
- measuring pressure in the visual organs;
- retinal examination;
- Ultrasound of the eyeball;
- visometry is one of the ways to test visual acuity, which involves working with four types of tables.
This disease is the most common cause of visual impairment in old age.
Instrumental examinations of the fundus of the eyeball are also possible. These include:
- Fluorescein angiography is one of the methods for studying the vessels of the eyeball, when an organic pigment is injected intravenously.
- Electrophysiological study - necessary to measure the condition of the retina and nerve cells.
Diagnostics
A comprehensive diagnosis out by an ophthalmologist. The most commonly used procedures are:
- analytical studies (laboratory);
- Ultrasound;
- EPI (study of the functions of the nerves of the eye);
- FA (retinal vascular study);
- study of the fundus.
A correct diagnosis allows you to choose the necessary treatment method.
Treatment of retinal dystrophy
Treatment of retinal dystrophy is determined during a diagnostic study. Most experts give their preference to the following methods:
- laser intervention;
- medical supplies;
- vitreoretinal surgery.
The choice of method by which treatment will be carried out is chosen by the ophthalmologist, based on the information obtained during diagnosis.
Treatment with medications
Treatment based on medication is mainly used in the early stages of the disease. Also, this method is used during the rehabilitation of the patient after surgery. There are a number of medications that have a positive effect on visual acuity, boost the immune system and enrich the body with vitamins. These medications can be divided into the following pharmacological groups: angioprotectors, polypeptides, disaggregants, biogenic stimulants, combined vitamins, as well as drugs that increase blood circulation stimulation.
Physiotherapy
Physiotherapy is an auxiliary method of combating the disease, which will strengthen the eyeball muscle system. Typically, the prescribed procedures are carried out in a specialized center or clinic.
- Electrophoresis is an effect on the body through the supply of low-amplitude current.
- Photostimulation is the effect on the retina using bright flashes of light.
- Magnetotherapy is the effect on the body using a magnetic field in order to change the biological fluid in the body.
The set of procedures can be supplemented with laser radiation to stimulate the retina of the eyeball. This method is extremely effective in trying to stop the development of dystrophy. The essence of the method is that with the help of a laser, the doctor draws a certain boundary between healthy and diseased tissues. While under the influence of the beam, the diseased vessels are “sealed”, and the liquid inside the eyeball stops flowing to them.
Thanks to this procedure, the disease is taken under complete control, and the patient avoids such terrible consequences as retinal degeneration. The laser treatment procedure is quick and simple, but at the same time requires full compliance with the ophthalmologist's requirements during the rehabilitation period.
Very often, degenerative changes in the retina accompany moderate and high degrees of myopia.
Surgical intervention
Surgery is usually required when the disease is diagnosed in the later stages of development, and is the only way to avoid such unpleasant consequences as destruction of the retina. There are two main types of surgical intervention:
- The revascularization procedure is a process of blocking the affected tissues of the eyeball, followed by an increase in the lumen in functioning vessels.
- Vasoreconstructive surgery is performed using special grafts designed to stabilize the microvascular bed of the eyeball.
Laser surgery
The best treatment method for PVCRD is laser coagulation of the retina, the essence of which is gluing the thinned areas of the retina or cutting off torn tissue. Laser coagulation is carried out on an outpatient basis under local anesthesia, its duration is no more than 20 minutes.
Laser intervention is effective and safe, the recovery period is quick and without complications. For the speedy formation of adhesions during the first 2 weeks after surgery, you should refrain from physical and visual stress, thermal procedures and taking alcoholic beverages and vasodilators.
Retinal degeneration: causes and treatment
Retinal degeneration is the irreversible destruction of tissue that leads to complete blindness. The disease occurs mainly among elderly people. Degeneration of eye tissue is extremely rarely diagnosed in children and adolescents.
Today, medicine is unable to answer the question of what causes the degenerative process. It has been scientifically proven that this disease can be hereditary, but it manifests itself only closer to old age. The phenomenon itself may also be associated with a large number of metabolic substances in the eyeballs. The answer to the question of how to treat retinal dystrophy is quite complicated, because the problem itself is not always solvable. Unfortunately, it is impossible to stop the progression of this disease with the help of therapeutic interventions.
Experts recommend that many patients consider laser therapy options, since with such a complex diagnosis this is the only method that can produce tangible results. In addition, photodynamic therapy may be an alternative way to combat retinal degeneration.
Retinal dystrophy may be asymptomatic at first
The essence of this method is to influence only newly formed vessels in which the photoreceptors are not yet damaged. This technique can be combined with other methods of influence.
Diagnostic methods
Peripheral vitreochorioretinal dystrophy is asymptomatic for a long time, which is why it is often diagnosed in the presence of large tears and significant deterioration of vision. It is impossible to detect PVCRD using a routine examination of the fundus, so ophthalmoscopy is performed with maximum pupil dilation and using a special Goldmann lens, which allows for a detailed examination of the most distant parts of the retina.
Read in a separate article: Occlusion of the central retinal artery - treatment
In addition, the following diagnostic measures can be carried out:
- perimetry;
- sclerocompression;
- visometry;
- refractometry;
- optical coherence tomography;
- EFI;
- Ultrasound.
Some modern clinics have special equipment that allows you to study the periphery of the retina in color, detect areas of rupture and estimate their size as accurately as possible.
Preventive standards
To prevent eye diseases, there are several recommendations that people at risk should use. It is necessary to periodically perform eye exercises by performing special exercises. You should beware of harmful radiation, and also spend less time in the sun.
If you have a predisposition to visual dystrophy, you should take vitamin supplements and dietary supplements.
Don't forget that your eyes need rest, which means you need to add time to your schedule when you can relax. Facebook
A little history
Tapetoretinal abiotrophy of the retina is a degenerative disease (pigmentary dystrophy) that is inherited. It occurs with damage to the photoreceptors of the retina, mainly rods. It is quite rare.
The pathology was first described in 1857 by Donders. Then her symptoms and signs were defined as “retinitis pigmentosa.” With a subsequent detailed study of the causes and symptoms of this disease, it began to be called “primary taperetinal dystrophy”, “rod-cone dystrophy”, since the lesion at first mainly affected only the rods. True, in the later stages, the cones also had damage. The final name of the pathology was a term that reflects its essence in detail - “retinal pigment abiotrophy”.
Contraindications
With retinal dystrophy, there is a danger that a person will lose vision. To prevent this outcome, laser coagulation is performed, but even when the disease goes away, it is too early to relax.
There are some restrictions after the laser coagulation procedure. The recovery period lasts from one to two weeks, it all depends on the person’s health.
Doctors recommend avoiding sun exposure to your eyes, so it is best to wear sunglasses until your retina strengthens.
Also not recommended:
- watch TV and sit at the computer;
- strain your eyesight with glasses and contact lenses;
- take hot baths, saunas;
- go to the beach.
It is strictly prohibited:
- eat foods with salt,
- drinking alcohol,
- drink plenty of fluids.
Be sure to use eye drops prescribed by your doctor. It is also necessary to avoid any physical activity or sports for a month. You cannot drive a car for the first week after surgery.
People with diabetes should control their blood sugar to a normal level. If you have problems with the vascular system, you need to constantly maintain normal pressure. After surgery, be sure to visit an ophthalmologist once every three months.
Risk factors
When touching on such an issue as retinal dystrophy, one cannot fail to mention what factors contribute to an increased risk and who is more predisposed to this disease than others:
- these are, first of all, people whose age is over 50 years;
- it was found that women are more likely to suffer from this disease than men;
- hereditary factor;
- people with white skin and blue irises;
- persons who have vascular diseases;
- poor nutrition;
- cholesterol problems;
- smoking;
- obesity;
- frequent stress;
- lack of vitamins in food;
- sunburn of the eye;
- environmental problems.
Risk group
The main causes and factors contributing to metabolic disorders in eye cells, changes in their trophic and hydrophilic parameters and forming risk factors for PCRD:
- infectious and infectious-inflammatory eye diseases (blepharitis, barley, dacryocystitis, keratitis, conjunctivitis, etc.);
- injuries to the face, cervical spine, chest and head (closed fractures of the posterior base of the skull are especially dangerous);
- iatrogenic factor (eye surgery, including laser vision correction, as well as parabulbar and retrobulbar intraocular injections);
- diseases in which the circulation of blood and lymph in the vessels is disrupted, including in the vessels of the fundus (coronary heart disease, arterial hypertension, post-stroke and post-infarction condition, atherosclerosis);
- impaired hemostasis and hematological diseases (hemolytic anemia, hemoglobinopathy, hereditary coagulopathy, hemorrhagic diathesis, etc.);
- diseases of the endocrine system and metabolic disorders, in which beneficial substances do not reach the eye tissues in sufficient quantities (autoimmune thyroiditis, diabetes mellitus, acromegaly, hormonally active adrenal tumors, etc.).
Well-known risk factors that negatively affect the condition of blood and lymphatic vessels are smoking, unfavorable working and living conditions (from an environmental and radiation point of view), alcohol abuse, and stress. Deficiency of vitamins and nutrients necessary to maintain eye and vascular health (zinc, retinol, lutein, ascorbic acid, rutin) can occur due to diet abuse, poor quality or poor nutrition.
Preventive measures
When the question arises about the prevention of such a serious disease as retinal dystrophy, you can follow just a few simple rules. They will help maintain good vision for a long time and get rid of problems:
- The eyes should rest periodically. Avoid overexertion.
- When working with a computer, use special glasses.
- Improve your eye exercises.
- Take vitamin complexes to improve visual function, as well as dietary supplements containing zinc.
- Eat a varied and nutritious diet.
- Get rid of bad habits.
By following these basic rules, you can protect yourself from retinal dystrophy and preserve your vision.
Symptoms of the disease
The characteristic signs of this disease are:
- Lack of central and unclear lateral vision.
- Loss of light perception by the eye and distortion of objects.
- Feeling of black midges and the appearance of a veil before the eyes.
- Decreased vision (or development of farsightedness).
- Difficulty in assessing a moving or static object and others.
If any of the presented symptoms are detected, you should contact an ophthalmologist for advice and undergo tests and relevant tests.
If the disease is confirmed, you should act on the recommendations of a specialist, since the disease in severe cases can lead to retinal detachment, and, as a result, blindness.
Treatment options
Treatment of retinal dystrophy stops the pathological process and prevents complications, but does not restore lost vision. The method of therapy depends on the stage and form of the disease. The initial degree of the degenerative process is treated with drug therapy, including the following medications:
- angioprotectors: Ascorutin, Complamin;
- antiplatelet agents: Ticlodipine, Acetylsalicylic acid;
- drugs to lower cholesterol levels: Simvastatin, Atoris;
- polypeptides: Retinolamine;
- eye drops: Taufon, Emoxipin;
- vitamin complexes: Kombilipen, Milgamma.
Lucentis is also a good remedy for the death of retinal tissue. Properly selected medications dilate and strengthen blood vessels, improve microcirculation, improve material metabolism and promote rapid tissue regeneration. To achieve a better result, in addition to medications, various physical procedures are prescribed:
- magnetic therapy;
- electrophoresis with No-Shpa;
- photostimulation;
- ultrasound;
- electrical stimulation;
- laser stimulation.
In difficult cases, the most effective method of treating retinal dystrophy is laser coagulation. This is a minimally invasive surgical method that is aimed at strengthening the retina and coagulating damaged tissue, providing a targeted effect. In addition to laser photocoagulation, vitrectomy or vasoreconstruction can be performed to restore normal blood supply to the retina. The cost of an operation today depends on many factors and can range from 3-5 thousand to several tens of thousands of rubles.
Some clinics treat retinal dystrophy with stem cells.
Possible complications
If treatment for retinal degeneration was not started on time, then there is a possibility of the following complications:
- retinal rupture;
- retinal disinsertion;
- hemorrhages;
- difficulties with orientation in space;
- decreased visual acuity.
The most severe complication of this disease is complete loss of vision. The appearance of unpleasant consequences can be provoked by factors such as strong physical exertion, vibration or diving under water.
General information
Chorioretinal dystrophy is one of the types of peripheral retinal dystrophies, in which the patient’s quality of anterior (central) vision remains virtually unchanged, but the performance of the peripheral (lateral) analyzer decreases significantly. Based on the localization of destructive foci, equatorial (median), paraoral and combined forms of peripheral retinal degenerations are distinguished.
The retina is the inner layer of the eye, adjacent to the vitreous body on one side and the choroid (choroid) on the other. It plays an important role in the formation of the function of vision, being, in fact, a visual analyzer, due to the large number of light-sensitive neurons - photoreceptors. Photoreceptors are contained in the outer granular layer of the retina and are responsible for the refraction and primary processing of light radiation, as well as the transmission of nerve impulses from the optical system of the eye to the visual center of the brain. Destruction of any part of the retina causes irreversible changes in the functioning of the visual organs and can lead to serious consequences: retinal detachment, chronic low vision and even complete blindness.
Congenital dystrophies of the peripheral retina
The role of hereditary predisposition in the mechanisms of formation of peripheral ocular dystrophies has not been fully studied. But it is known that mutated genes can be transmitted in three main modes of inheritance: autosomal dominant, autosomal recessive and X-linked. With an X-linked mode of inheritance, the disease develops only in males, even if the carrier of the mutation is a woman. That is, a mutating gene can be transmitted from mother to son, but it does not affect girls in any way, and they remain latent carriers of the mutation factor.
Retina in peripheral dystrophy
Treatment
To date, there are no methods that can completely cure peripheral vitreochorioretinal dystrophy of the retina. The progression of the disease can be stopped with the help of medication, physiotherapy, laser and surgical treatment. The correct approach to combating the disease allows you to preserve your vision and avoid dangerous complications. Read more about eye surgeries →
Drugs that help slow the progression of dystrophy:
- Antiplatelet agents (Acetylsalicylic acid, Ticlopidine, Clopidogrel). Useful for hypertension and cardiovascular diseases. They thin the blood and inhibit thrombus formation, thereby protecting the retina from hypoxia.
- Vasodilators and angioprotectors (Actovegin, Vinpocetine, Pentoxifylline). Relieves spasm of retinal vessels and protects vascular walls from damage. They improve blood circulation in the retina, preventing its destruction.
- Vitamin and mineral complexes (Okyuvite-Lutein, Blueberry-Forte). Saturate the retina with nutrients, vitamins and minerals. Slow down the course of degenerative processes. Read more about vitamins for eyes →
- Biological regulators (Retinolamine). Restore the permeability of retinal vessels and normalize the functioning of photoreceptors. They stimulate reparative processes, that is, they accelerate the restoration of the retina.
You can strengthen the retina and prevent its detachment using laser treatment. During the procedure, the specialist solders the retina to the choroid, which is located underneath it. This allows you to limit the foci of degeneration.
What could be the consequences of the disease?
Retinitis leads to deterioration of the visual system, such as loss of peripheral vision.
With pigmentary dystrophy, symptoms occur when the retina is already damaged, so it is difficult to detect a disorder at the initial stage of development. Tissue depletion leads to complications such as:
- loss of peripheral vision;
- decreased ability to see in the dark;
- decreased visual acuity;
- development of cataracts or glaucoma;
- tunnel vision;
- blindness.
Treatment with folk remedies
At the initial stages of the development of the degenerative process, folk remedies are often prescribed simultaneously with drug therapy. The following recipes will help you cope with retinal degeneration:
- Mix 50 ml of warm boiled water and goat's milk, drip a couple of drops of the resulting mixture into the sore eye and place a dark cloth on top of the affected organ of vision for 30 minutes. Repeat this procedure every day for a week.
- Take 1 tablespoon of dried lily of the valley leaves and 5 tablespoons of nettle leaves, combine and pour 250 ml of boiled warm water. Let it brew for 9 hours, then add 0.5 teaspoon of soda and apply the resulting infusion as a lotion on the sore eye.
- Combine a glass of boiling water and 1 tablespoon of cumin in a small saucepan, boil and cook the broth for 5 minutes. Add a tablespoon of cornflower flowers to the resulting infusion, stir, cover with a lid and let it brew for a while. Strain the cooled broth and place 2 drops in each eye twice a day.
- Pour 200 ml of boiling water over a tablespoon of celandine flowers, put on fire and boil for 5 minutes, then let the broth cool, strain and use 3 drops for eye drops three times a day for 1 month.
Another effective remedy for dystrophy for treatment at home is a herbal mixture, which includes ginger, cinnamon, dandelion and bay leaf.
Alternative medicine can strengthen blood vessels, prevent retinal detachment and cope with many eye diseases. However, before starting such treatment, you should consult your doctor.
Fundus of the eye in pigmentary dystrophy
Pigmentary retinal dystrophy is a fairly rare disease. It occurs in 1 person out of 5000, and in total there are approximately 100 million carriers of the defective gene that causes retinitis pigmentosa in the world.
Important
With the development of this pathology, the eye, initially a light-absorbing structure, turns into a light-reflecting structure, which inevitably becomes the cause of blindness. Men are more susceptible to the development of retinitis pigmentosa, and the disease can occur both in childhood and in adulthood.
According to statistics, the majority of patients with retinal pigmentary dystrophy under the age of 20 retain visual acuity above 0.1 and the ability to read, while in 45–50-year-old patients, visual acuity decreases to a value below 0.1, and they can no longer read.
Retinitis pigmentosa or, in other words, retinal pigmentary dystrophy is characterized by degeneration of photoreceptors and pigment epithelium, as a result of which the ability to transmit signals from the retina to the cerebral cortex is lost.
With this pathology, a characteristic accumulation of pigment substance is also clearly observed in the fundus picture. The degenerative process with pigment deposition causes the disappearance of photoperceiving cells and receptors, causing the retina to lose sensitivity to light signals. As a result, the person loses his vision.
Pigmentary dystrophy of the retina was first described in 1857 by D. Donders, and after 4 years the hereditary nature of this pathology was established. The type of heredity affects important indicators of the disease: age of onset, rate of progression and prognosis of visual functions.
The following types of inheritance are distinguished:
- Sex-linked: transmission of a defective gene from mother to son with the X chromosome is the least common, but the prognosis is the most unfavorable;
- Autosomal recessive: defective genes are passed on from both parents;
- Autosomal dominant: transmission of disease genes from one of the parents.
Retinitis pigmentosa often occurs in childhood and is characterized by three symptoms:
- Small accumulations of pigment in the fundus;
- The optic disc has a waxy pallor
- Constriction of arterioles.
In the future, the patient's visual acuity may deteriorate, while pigment changes are observed in the macular area, and macular edema may occur. Patients with retinitis pigmentosa have an increased risk of developing myopia, posterior subcapsular cataracts, and open-angle glaucoma.
In childhood, retinitis pigmentosa is quite difficult to diagnose. The first noticeable symptom that appears in a child at an early stage of the pathological process is poor orientation in the dark - often the disease is detected precisely by this manifestation.
This disorder is also characterized by the inability to distinguish colors in the dark - this is called night blindness. In addition, the initial stages of pigmentary dystrophy, especially in children, manifest themselves with headaches and flashes of light in the eyes.
As the disease progresses, a continuous process of degeneration of the retina occurs, eventually leading to impairment of peripheral vision. According to ophthalmologists, vision becomes tunnel vision - this occurs in the second stage of the disease.
At the last stage of the disease, a person loses not only peripheral, but also central vision. Blindness sets in.
There are currently no effective methods for treating retinal pigmentary dystrophy. Although it should be noted that constant and unsuccessful research is being conducted in this direction. More recently, thanks to new advances in electronics and cybernetics, huge strides have been made in this area.
The essence of the new technique is to install a small photodiode sensor with a transmitter on the retina of the eye. The received light information from the outside world comes to the transmitter through an ultra-thin wire. The perception of information occurs through special glasses with receiving glasses.
Of course, this is not full-fledged vision, but, nevertheless, a person becomes able to see. Experiments have shown that a blind patient gains the ability to distinguish between light and dark, as well as to see the outlines of large objects.
There is no doubt that this development can make the lives of blind people much easier. This experimental technique is currently undergoing testing.
To treat retinitis pigmentosa, a method of slowing down the degenerative process of the retina is also used. It includes the use of stimulating procedures, for example, magnetic stimulation, as well as taking medications with blueberry extract and vitamin A, and parabulbar injections of the drug “Retinalamin”.
In what forms does PVCRD occur?
Doctors distinguish several forms of this disease. Among them:
- Lattice dystrophy. Retinal degeneration looks like a lattice of white stripes - empty vessels. Thinning and gaps appear between them.
- “Snail trail” is a type of PVCRD in which the lesions appear as ribbon-like stripes, reminiscent of the tracks left by a snail.
- Frost-like dystrophy: retinal changes resemble snow flakes.
- “Cobblestone Pavement” is another unusual name for the PVCRD variety. The lesions in this case have an elongated shape, near which there may be pigment spots.
- Small cystic PVCRD is a dystrophy that is localized in the extreme peripheral zone of the retina. Cysts on devices are distinguished as round or oval spots of bright red color.
Any form of dystrophy should be treated as early as possible. If intraocular fluid gets behind the retina when the retina is detached, vision can be lost forever. Detachment is treated using laser coagulation, which is performed on an outpatient basis and involves laser “soldering” of the retina.
What treatment is prescribed?
Drug therapy
If the disease manifests itself in childhood, by the age of 25 the patient’s vision decreases to the point of loss of ability to work.
Emoxipin drops improve microcirculation and lengthen the time to stop bleeding in case of damage to the blood vessels of the eye.
In most cases, treatment of retinal pigmentary dystrophy is carried out through the complex use of medications that normalize blood circulation in the eye and provide the retina with the necessary nutrition. The following remedies are prescribed:
- "Emoxipin". Restores microcirculation.
- "Taufon". Eye drops. Stimulates tissue regeneration of the visual apparatus.
- A nicotinic acid. Normalizes metabolic processes and blood circulation in the body.
- “No-shpa” + “Papaverine”. The combination of drugs provides an antispasmodic effect and a decrease in pressure in the blood vessels.
Hardware Impact
Retinal pigmentary degeneration is treated with photostimulation. The technique consists of provoking stimulation in certain areas of the ocular apparatus. As a result, the development of the disease slows down. Under the influence of radiation, blood circulates better throughout the eyeball, but restores metabolic processes. The technique removes swelling from the membrane of the visual organ and strengthens the retina.
What other treatment methods are used?
Often, drug therapy is complemented by physiotherapy, which speeds up the process of restoration of the damaged inner lining of the eye and activates photoreceptors. In most cases, patients are prescribed ozone therapy, magnetic resonance therapy and electrical stimulation. If the choroid of the eyeball is damaged, surgery is performed.
Causes
The main risk factor for the development of destructive changes in the peripheral parts of the retina is refractive error - refraction of the electromagnetic light flux that occurs under the influence of the law of conservation of energy and impulses.
In almost 40% of cases, the pathology develops in patients suffering from myopia (myopia). With this disease, a person has difficulty distinguishing objects located at a long distance, due to the fact that the electromagnetic flux is focused not on the retina, but in front of it. This leads to an increase in the anteroposterior axis of the eye and stretching of its membranes. The edges of the retina are thinner compared to the macular zone, so they are more susceptible to thinning and further destruction, which determines the high risks of PCRD in patients with various forms of myopia.
Despite the fact that patients with myopia make up a significant portion of the total number of patients with signs of PCRD, neurodegenerative disorders can also occur in people with normal refraction under the influence of traumatic, infectious-inflammatory, iatrogenic and other factors affecting the functional state of the vascular membranes eyes.
Vision with myopia