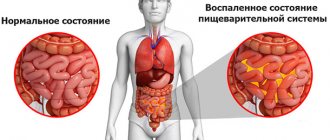
Almost every person has ever experienced acute gastric discomfort, manifested by nausea, vomiting, and diarrhea. Some call it poisoning, others indigestion. In fact, this is a large group of diseases with similar symptoms, united by a common concept - acute gastroenteritis. So, acute gastroenteritis is an inflammatory process of the mucous membrane of the stomach and small intestine with a sudden onset, rapid development of dyspeptic symptoms, intoxication and dehydration of the body. Mild acute gastroenteritis can heal on its own. If the damage to the gastrointestinal tract is serious, the process often becomes chronic.
Prevalence
Gastroenteritis is one of the most common diseases. In terms of incidence, it is second only to ARVI and influenza.
It is believed that 20% of people experience gastroenteritis of varying severity each year. This is especially true for susceptible categories - children of early and preschool age, pregnant women and the elderly. The disease is especially widespread in countries with low levels of development, where hygiene rules are poor and people do not have access to quality food and drinking water.
Preventive measures
Instill good hygiene habits in your child from an early age.
Rotavirus gastroenteritis in children is almost always more severe than in adults. This is explained by the loss of fluid not only during diarrhea or vomiting, but also during the process of skin evaporation. As a rule, the consequences of the disease are dysbacteriosis or gastroenteritis in a chronic form with periodic exacerbations. This may affect the child's development. As a preventative measure, the following measures must be observed:
- From an early age, instill in your child the habit of washing hands before eating and maintaining good hygiene;
- monitor the cleanliness of toys with which the child is constantly in contact; do not allow your child to put dirty objects in his mouth;
- Give your child only boiled or special water from a pharmacy;
- carefully monitor your diet - it should be complete and regular;
- complementary foods are introduced in agreement with the pediatrician. In no case should you eat food from the common table ahead of time, especially spicy and sausage products, pickles and marinades;
- Hazardous chemicals, household chemicals, and medications should be stored in inaccessible places.
In addition, you should cook food responsibly. Meat and fish dishes must be thoroughly boiled. As for eggs, they should be boiled for at least 20 minutes. Personal hygiene of breastfeeding women is also important. Rotavirus gastroenteritis rarely occurs in newborns, since they do not eat food from the common table.
As a rule, the causative agent is rotavirus and bacteria that enter the body from the skin of the hands or chest.
Causes of the disease
The most common cause of gastroenteritis is infection with viruses, especially rotavirus and the bacteria Escherichia coli and Campylobacter, as well as other pathogens. Less common are cases not associated with infection. In children, the risk of infection is increased due to underdeveloped immunity and less compliance with hygiene rules.
- Viruses. The most common causative agents of viral gastroenteritis are rotavirus, norovirus, adenovirus and astrovirus. Rotavirus is the most common cause of gastroenteritis in children and occurs equally frequently in developed and developing countries. 70% of cases of diarrhea in children are caused by a viral infection. In adults, rotavirus is less common due to acquired immunity. Norovirus causes 18% of cases and is the leading cause of gastroenteritis in America, causing 90% of outbreaks. Local epidemics can occur in groups of people spending time in close proximity in close spaces, such as cruise ships, hospitals, restaurants. People can remain infectious after recovery. 10% of cases in children are caused by norovirus.
- Bacteria. The main causative agent of bacterial gastroenteritis in developed countries is Campylobacter jejuni, half of cases of infection are associated with poultry. In children, about 15% of cases of the disease are of bacterial origin; the most common pathogens are E. coli, Salmonella, Shigella and Campylobacter. In food left for several hours at room temperature, the few bacteria present can multiply and pose a threat of disease. Sources of infection can be raw or undercooked meat, eggs, seafood, fresh herbs, unpasteurized milk, fruit and vegetable juices.
- Protista. Among the protist pathogens of gastroenteritis, intestinal lamblia is the most common, dysenteric amoeba and cryptosporidium are less common. In total, protists are the causative agents of 10% of cases in children. Giardia is more common in developing countries, but occurs to some extent everywhere. Most often, it is infected by people who travel a lot in places where it is distributed, in children raised by nannies, among homosexuals, or accompanying natural and humanitarian disasters.
There are also many causes of inflammation of the gastrointestinal tract that are not associated with infections. Gastroenteritis can develop when using certain medications, for example, non-steroidal anti-inflammatory drugs, or when eating food containing substances to which the patient’s body is hypersensitive. These substances can be lactose, or, in case of celiac disease, gluten.
Manifestations of gastroenteritis accompany some diseases of the gastrointestinal tract, such as Crohn's disease. Some foods can cause nausea, vomiting and diarrhea, for example, when consuming certain types of fish, ciguatera can occur, there are cases of poisoning from stale fish, cases of tetrodotoxin poisoning when eating pufferfish, botulism occurs when eating improperly stored food.
Causes of acute gastroenteritis
People who believe that you can get acute gastroenteritis only by eating low-quality foods are mistaken. Nutritional errors are the most common, but not the only factor that provokes the development of the disease. Acute gastroenteritis is divided into two large groups:
- Acute gastroenteritis of infectious etiology;
- Acute gastroenteritis of non-infectious etiology.
Gastroenteritis of infectious etiology
- Viral. Caused by Coxsackie viruses, enteroviruses, rotaviruses, adenoviruses and others.
- Bacterial. The causative agents are bacteria: salmonellosis, dysentery, yersiniosis and others.
A disease of infectious etiology is transmitted from a sick person to a healthy person. The transmission routes are different. Bacteria, protozoa and viruses are excreted in feces and vomit and contaminate water, soil, and food. If you drink contaminated water or food, you can get sick. In addition, viruses enter the environment through coughing and sneezing.
A healthy person inhales tiny particles of saliva teeming with the pathogen and becomes infected. Those who are in close contact with the sick person, for example, family members, children's groups, and work employees, are exposed to infection. Infectious agents enter the body, multiply, and infect the mucous membrane of the gastric tract. Cells of the immune system rush to fight microbes. Substances that damage the virus or bacteria are released. When the pathogen dies, it releases toxins that travel through the bloodstream to other organs and tissues. An inflammatory reaction develops.
Foodborne toxic infections occupy a separate niche among acute gastroenteritis. Clostridium botulinum, when found in food products such as canned food or dried meat, produces large amounts of toxin. Once in the human stomach, botulinum toxin causes severe poisoning. The bacterium itself is not dangerous.
Types of acute non-infectious gastroenteritis
- Nutritional. The disease develops after eating fatty, hot, spicy, excessively salty or sour foods. Very often, symptoms of acute gastroenteritis appear after excessive drinking. Harmful factors irritate the stomach, causing dyspeptic disorders.
- Allergic . Food allergies are most often caused by milk, fish, nuts, and grains. Cells of the immune system, against the background of a lack of enzymes that break down food, recognize food as an enemy. Eosinophils rush into the gastrointestinal tract and damage the mucous membrane. Hence another name for allergic acute gastroenteritis – eosinophilic. May be accompanied by skin manifestations of allergies.
- Toxic. It is provoked by the entry of poisons and toxins into the body. For example, poisoning with plant and animal poisons, consumption of alcohol substitutes, and exposure to household chemicals in the gastrointestinal tract. This also includes drug-induced gastroenteritis, which develops in response to taking certain medications.
- Radiation. It is a complication of radiation therapy. Develops in cancer patients due to radiation damage to the gastrointestinal tract.
- Helminthic. Parasites that live in the intestines usually cause a chronic inflammatory process. However, with massive helminthic infestation, the disease can be acute.
- Hemorrhagic gastroenteritis is not an independent disease, but develops as a complication of a toxic, allergic or bacterial process. Main symptoms: bloody vomiting, diarrhea and thickening of the blood. With timely hospitalization and quality treatment, using injectable antibiotics and infusions, the patient recovers quickly and completely.
Acute gastroenteritis is common everywhere. In developed countries, the incidence of acute gastroenteritis is lower compared to developing countries. However, the problem of viral gastroenteritis is relevant everywhere.
Every year, a large number of people around the world suffer from acute gastroenteritis. In areas with a warm climate, people often get sick in cooler weather. In developing countries with high population densities, mortality from acute gastroenteritis is high, especially among infants.
Symptoms
Doctors consider this pathology extremely rarely as an independent disease - more often gastroenteritis is a symptom. If viral gastroenteritis develops, the onset of the disease will be sudden, and the symptoms will develop into a certain clinical picture:
- Patients complain of intense spastic abdominal pain, nausea, vomiting and diarrhea (diarrhea);
- In some cases, fever, mild muscle pain and general weakness are added;
- There is a strong rumbling in the abdomen, a feeling of bloating and increased gas formation, but there is no discharge of gases from the intestines.
Please note: with the development of gastroenteritis of viral etiology, there is no blood or mucus in the stool, and sometimes abdominal pain is not accompanied by diarrhea (diarrhea).
Doctors often diagnose gastroenteritis as a symptom of a bacterial intestinal disease. And in this case, the patient will experience watery stools, feces mixed with blood and mucus in small quantities, and the frequency of bowel movements per day can reach 30 times.
Chronic form
Gastroenteritis, which has become chronic, is accompanied by general symptoms and signs of local damage to the mucous membrane of the digestive tract. The patient complains of nausea, belching, and aching abdominal pain that occurs 1-2 hours after a meal. In the history of chronic inflammation, there are alternating periods of exacerbations and remissions, provoked by a violation of the diet or concomitant diseases.
The main symptomatic manifestations of this type of disorder include:
- loose stools;
- weight loss due to impaired absorption of beneficial micro- and macroelements;
- irritability;
- insomnia;
- polyfecal;
- rumbling in the right iliac region;
- bloating;
- white coating on the tongue;
- atrophy of nails, skin, hair;
- tachycardia;
- paresthesia (impaired sensitivity).
Treatment of acute gastroenteritis
Having attributed nausea, vomiting and bowel disorder to nutritional errors, a person does not always rush to the clinic. A person who is ill with a mild form of gastroenteritis uses one or another folk method in self-medication or uses familiar medications for indigestion.
Self-medication often helps. But, if the condition does not improve within 24 hours, you need to visit a doctor. In case of moderate or severe illness, it is important to immediately seek medical help. Patients with infectious gastroenteritis, poisoning with poisons or toxins are hospitalized in a hospital.
Severity
Acute gastroenteritis (acute intestinal infection) is divided according to severity:
- First degree – diarrhea 3-5 times a day, single or repeated vomiting, normal temperature, no signs of dehydration.
- Second degree - diarrhea and vomiting 5-10 times a day, abdominal pain, fever up to 38.5oC, signs of mild dehydration - thirst, dry mouth, rare urination, rapid heartbeat, loss of up to 3% of body weight.
- Third degree - diarrhea and vomiting up to 15 times a day, fever up to 40oC, severe signs of dehydration: pale skin, bluish tint on the tips of the fingers, nose, earlobes, cramps of the calf muscles, dizziness, faintness, rare minor urination, impaired consciousness, loss of 4-6% body weight.
Chronic gastroenteritis: diarrhea, nausea, signs of dyspepsia. Local mucosal lesions lead to chronic malabsorption, which is accompanied by weight loss, weakness, increased fatigue, irritability, and sleep disturbances.
Symptoms of acute gastroenteritis
Acute gastroenteritis begins suddenly. The full clinical picture is preceded by an incubation period, the duration of which depends on the etiological factor.
All symptoms of acute gastroenteritis can be combined into several syndromes:
Dyspeptic syndrome includes:
- heartburn;
- burping;
- nausea;
- vomiting;
- flatulence;
- increased intestinal motility, manifested by rumbling in the abdomen;
- malabsorption of nutrients in the small intestine and diarrhea.
The pain syndrome is characterized by pain in the epigastric region and along the intestines. Depending on the etiology and severity of the disease, the intensity of pain varies.
Intoxication syndrome manifests itself:
- general weakness;
- increased fatigue;
- loss of appetite, up to complete refusal to eat;
- sweating
Fever. Accompanies infectious forms of the disease. Body temperature ranges from hyperthermic (above 39.5–40 degrees) to subfebrile (from 37 to 38). With inadequate treatment, serious complications arise. The patient loses water and electrolytes through loose stools and vomiting. The functioning of organ systems is disrupted. The kidneys, liver, and heart muscle suffer. Toxins affect the central nervous system. Multiple organ failure develops.
Diagnostics
The diagnosis is made in stages. Initially, the doctor carries out an examination and collects information based on the patient’s complaints. Depending on the form of the disorder and the severity of its development, tests are prescribed. In addition, the sanitary and epidemiological situation in the region is taken into account.
To diagnose, you need to go through the following procedures:
- coprogram for the presence of mucus, bloody inclusions, undigested fiber, starch, fats, muscle fibers;
- collection of urine and vomit to study pathological dynamics;
- blood donation to identify pathogens, determine leukocytes, signs of hemoconcentration, ESR (erythrocyte sedimentation rate);
- ultrasound examination of the abdominal cavity;
- esophagogastroduodenoscopy to assess the condition of the gastric mucus and initial parts of the small intestine;
- biopsy of tissues and cells for the purpose of histological analysis to identify hyperplasia, atrophy, metaplasia;
- stomach acid test;
- PCR diagnostics (polymerase chain reaction) for the determination of Helicobacter pylori;
- examination of the intestinal contents for helminths and bacteria.
Diagnosis of gastroenteritis in children
To determine the correct diagnosis, anamnesis should be collected in all respects. The doctor should ask the parents in detail about the onset of the disease and the symptoms that appeared at the beginning and in the following days. It should also be determined whether the child has had contact with patients infected with rotavirus gastroenteritis over the past 7 days.
In order to determine the specific causative agent of the disease, it is necessary to conduct a study of feces at the microscopic level and inoculate it on individual nutrient media. Blood samples are taken from the child to check for antibodies to certain microorganisms. However, it must be taken into account that some antibodies are formed in the body only after 5 days from the onset of the disease.
The main signs of infectious gastroenteritis are the determination of insufficient functioning of the pancreas during stool examination. The stool may contain mucus and a large amount of fiber in digestible and indigestible forms. There may be blood in the stool, indicating bleeding in the digestive tube.
A blood test for gastroenteritis may show an increased level of leukocytes, an increase in ESR, and visible changes in the leukocyte formula are noticeable. Biochemical studies most often determine the increase in C-reactive protein and dysproteinemia. The correctness of the diagnosis primarily depends on a correct assessment of the severity of the disease and the degree of dehydration.
How to treat gastroenteritis?
Treatment of gastroenteritis in adults in most cases occurs at home. When the first symptoms appear, you need to immediately take some measures that are aimed at improving the patient’s condition.
Treatment of all forms of gastroenteritis includes the following aspects:
- normalization of water-salt balance in the body;
- the first hours after the onset of the disease - complete refusal of food, after which you need to adhere to a certain diet;
- taking medications that are aimed at stopping vomiting and diarrhea;
- use of antibiotics.
Treatment of gastroenteritis in adults can be done with folk remedies, which are aimed at restoring the mucous membrane of the stomach and intestines. Also, these medications are acceptable for oral use to replenish fluid loss in the body. To improve the patient’s condition, the use of physiotherapy is quite effective:
- paraffin applications;
- warm compresses;
- inductothermy.
After relief of the main symptoms, you need to begin restorative therapy, which is aimed at normalizing the functioning of the digestive system.
Viral gastroenteritis - treatment
If you have symptoms that may indicate the development of the disease, you should contact the on-duty therapist. During the examination, the doctor will determine the treatment tactics. If the patient’s condition does not improve after 1-2 days, a decision is made to place him in a hospital.
The main aspect of the treatment of viral gastroenteritis is the elimination of dehydration. In this case, the use of saline solutions is indicated. Both pharmaceutical drugs and homemade products have a positive effect.
Complex treatment of the disease includes taking the following medications:
- antiviral;
- enzymatic;
- astringents;
- eubiotics.
As a preventive measure against viral gastroenteritis, vaccines are used against certain types of viruses that cause the development of the disease.
Treatment of infectious gastroenteritis
In the presence of the infectious nature of this disease, the use of dehydration therapy is indicated, which is aimed at restoring the water-salt balance. In acute gastroenteritis caused by various bacteria, antibiotics are prescribed. It is strictly forbidden to take them on your own, since if you choose the wrong treatment regimen, this can cause increased dysbiosis.
In the treatment of infectious gastroenteritis, agents are also used that are aimed at eliminating the main symptoms of the disease - fever, diarrhea, vomiting. Enzyme preparations are often prescribed to improve digestion. Also shown are agents that have an enveloping effect on the mucous membrane of the stomach and intestines.
Acute gastroenteritis - treatment
Treatment of the acute form of the disease occurs in a hospital. At the same time, it is important to monitor the patient’s condition and take measures aimed at improving it. In this case, treatment is carried out by a gastroenterologist.
Rehydration of the body in acute gastroenteritis is most often carried out intravenously in several stages. First, the entire volume of the missing fluid is restored, after which special solutions are gradually introduced as diarrhea and vomiting develop.
Also, therapy for acute gastroenteritis includes the following aspects:
- gastric lavage at the first stage of treatment;
- taking symptomatic medications that will help eliminate high fever, diarrhea, vomiting, pain and cramps in the stomach;
- sorbent preparations;
- dietary nutrition;
- medications to restore intestinal microflora;
- enzyme preparations.
Causes and how is it transmitted?
Gastroenteritis in children can occur due to:
- viral and bacterial infections;
- dysbacteriosis – changes in the microflora of the gastrointestinal tract;
- Giardiasis - an increase in the number of parasites in the small intestine;
- negative effects of substances, metals, etc.;
- poor nutrition - consumption of foods with highly allergenic properties or low-quality products, overeating, predominance of food that irritates the mucous membrane.
The most common cause of gastroenteritis is rotavirus. Infection occurs through contact with an infected person. The virus is transmitted both through handshakes and hugs, and by being on objects of common use - underwear, toys, dishes.
Rotavirus progresses most in the first five days from the onset of symptoms. The infection process occurs in the following way. After entering the body, active proliferation of microbes occurs. As a result, the epithelial layer is destroyed, and disruptions in the functioning of the gastrointestinal tract are observed. As a result, acute gastroenteritis develops in children. The duration of the disease ranges from 7 to 10 days, after which complete recovery occurs, but only with proper treatment.
Uncommon, but chronic gastroenteritis may develop. Signs of manifestation are alternating improvements and deteriorations in the child’s condition. The reason in this case should be sought in nutritional disorders. There may be permanent infectious foci in the body. A tendency to gastroenteritis is caused by:
- failure to comply with personal hygiene rules, for example, a child does not keep his hands clean after visiting the toilet, walking, or before eating;
- early age - these children have an underdeveloped digestive system. IgA, which is of great importance in the formation of local immunity, is not enough to perform its functions;
- poor processing of meat and fish products during cooking;
- insufficient cleaning of vegetables and fruits ready for consumption;
- interaction with people with obvious symptoms of intestinal diseases;
- poor hygiene by adults caring for young children. A necessary condition is for parents to wash their hands after changing the baby's diaper. In cases of breastfeeding a newborn, it is necessary to maintain breast hygiene. When bottle-feeding, keep nipples and bottles clean. Toys with which the child is constantly in contact should be constantly treated.
What can and cannot be eaten?
Diet for gastroenteritis is the main focus of treatment. During the period of diarrhea, patients are recommended table No. 4. The food is selected in such a way as to minimize irritation of the intestinal mucosa and eliminate fermentation processes. The diet contains a normal amount of protein - 90 g, a minimum of fat - 70 g, and carbohydrates - 250 g.
Method of preparation: the products are boiled in water or steamed, pureed or chopped with a blender. Diet: 5-6 times a day in small portions. Diet No. 4 is followed for 3-5 days. Then move on to diet No. 2.
Table of permitted and prohibited products:
| Can | Worth abstaining |
|
|
Table No. 2 is prescribed during the recovery period after acute gastroenteritis and in the chronic form of the disease. The purpose of the diet is to normalize the functioning of the digestive organs and provide the patient with adequate nutrition.
Cooking method: boiled, steamed, baked and fried (without crust) dishes. In the diet, the amount of carbohydrates is gradually increased to 400 g, and fats to 100 g (25% vegetable). Squirrel 90-100 g.
Table of permitted and prohibited products:
| Can | It is forbidden |
|
|
Nutrition
An important component of treatment is diet. On the first day, the patient is prescribed fasting. After a day you are allowed to eat. The diet for gastroenteritis should be gentle. Light food that does not irritate the gastrointestinal tract is indicated. On the second day, the patient is allowed wheat crackers, then rice porridge with water. Gradually, boiled vegetables, slimy porridges from various cereals, and baked apples are introduced into the menu.
As recovery progresses, boiled chicken fillet and fish are added. Food is served warm, in small portions 5-6 times a day. After recovery for several months, food should be dietary. Sweets, salty, spicy foods, coffee, chocolate are prohibited. Meat and fish included in the diet are steamed or boiled.
Drinking regime
From the first hours of treatment it is necessary to replenish fluid loss. The patient is advised to drink plenty of fluids in small portions. For drinking, mineral water without gas or special solutions for rehydration are suitable. For frequent vomiting, solutions are administered intravenously.
What is the danger of the disease?
Gastroenteritis is a severe disease that entails undesirable consequences. An advanced acute form of an infectious disease leads to a chronic stage. The following fatal complications have been observed:
- intestinal dysbiosis;
- damage to vital organs;
- dehydration of the body;
- sepsis;
- asymptomatic carriage;
- toxic shock;
- disruption of immunological mechanisms;
- death.
A dangerous pathology is asymptomatic carriage of the infection. Without showing any symptoms of the disease, a person remains a carrier and carrier of the infection. This leads to infection of other people.
General information about the disease
Gastritis and gastroenteritis are associated with inflammation of the mucous membranes. With gastritis, only the mucous membrane of the stomach becomes inflamed, while with gastroenteritis, the mucous membrane of the stomach and small intestine becomes inflamed.
Ways of transmission of gastroenteritis:
- Fecal-oral. It involves contact with a pathogen that is released into the environment with particles of feces or vomit and enters the body through the mouth with contaminated food and water. In everyday life, gastroenteritis is transmitted through dishes, toys, hygiene items and handshakes.
- Airborne dust. The disease is transmitted by inhaling air or dust containing infectious agents. The infection gets into the air when you sneeze or spit.
- Transmissible. Involves transmission of infection through insect bites.
Prevention
To prevent the development of gastroenteritis, the following recommendations must be followed:
- You can eat in public catering establishments only when a person is sure that they monitor compliance with sanitary standards.
- After visiting the toilet you need to wash your hands.
- All foods that a person eats must be fresh.
- When purchasing food products, you need to pay attention to their expiration date.
- After returning home from the street, you need to wash your hands. Be sure to perform this procedure before every meal.
- Before eating fruits and vegetables, you should pour boiling water over them.
- You should not drink raw tap water.
- Greens should be washed under running water.
- Raw eggs should not be eaten.
- The toilet and bathroom should be cleaned regularly using disinfectants containing chlorine.
Infants can become infected from a sick mother or close relatives.
Therefore, if a child lives in the house, you need to carefully monitor compliance with hygiene rules. Before holding the baby in your arms, you need to wash them. Older children need to be closely monitored. You should not allow your baby to put street objects, toys from the sandbox, leaves, sticks, etc. into his mouth. Intestinal flu Botulism Colon cancer Irritable bowel syndrome Intestinal dysbiosis Rotavirus infection
Symptoms and treatment in children
A curious little child explores the world around him with all his senses. Unfamiliar objects need to be smelled, touched, and tasted. The children are friends and communicate closely; they attend kindergartens and schools. Not every child follows basic hygiene rules. Accidentally and on purpose, children try inedible berries, put dirty hands into their mouths, and drink from open reservoirs.
And as a result they get sick. In terms of frequency of cases, the incidence of acute gastroenteritis is in second place after respiratory infections. The etiological classification of acute gastroenteritis in children does not differ from that in adults.
Children suffer from viral gastroenteritis and helminthiasis more often than adults. By contacting a source of infection in a children's institution, preschool children and schoolchildren become infected themselves and bring the pathogen home. Currently, special importance is attached to rotavirus gastroenteritis. This disease is transmitted by airborne droplets. Children under one year of age are especially susceptible and become seriously ill. It is difficult to treat. Due to the imperfection of the immune system, the disease progresses rapidly.
After a short incubation period, pronounced symptoms appear. Often rotavirus infectious gastroenteritis begins with a prodromal period, manifested by cough and runny nose. The child becomes lethargic and whiny. Then vomiting, abdominal pain, and diarrhea occur.
Suspicion of gastroenteritis is a direct indication for urgent medical attention. The smaller the child, the faster the disease develops, the stronger the symptoms of intoxication, and the faster dehydration occurs. Without adequate therapy, the patient's condition progressively worsens, and death may occur.
Diagnostic methods and basic principles of treatment for acute gastroenteritis are the same as for adult patients. To determine weight loss, a sick child must be weighed. Unlike adults and older children, infants need to be fed from the first day of illness.
Fractional feeding is recommended. The baby eats more often, but in small portions. Sick children require special care. Regular ventilation and daily wet cleaning are required. Hygienic procedures are performed after each act of defecation.
Other treatments
Since in medicine there are no methods of influencing the causative agent of the disease, it is necessary to use means to eliminate the symptoms, that is, disturbances of the digestive processes and dehydration. In addition to drug treatment, there are other methods, for example, the use of folk remedies and following a special diet. Let's consider each of these methods separately.
Folk remedies
To treat gastroenteritis in children, many different traditional medicine recipes are used, but they only help with an integrated approach. This means that it is impossible to refuse traditional treatment when using folk remedies. Below are the most effective recipes.
Table. Traditional medicine in the treatment of gastroenteritis.
| Product name, photo | Application |
| Oak bark decoction | You can cope with digestive system disorders using oak decoction. To prepare it, pour 200 ml of boiling water into 2 tbsp. l. crushed oak bark and leave for 30-40 minutes. After infusion, strain the broth through cheesecloth, thereby getting rid of the remaining bark. Take the finished product throughout the day, dividing into 3 servings. The decoction has an astringent effect, which helps with diarrhea. |
| Infusion of blackhead | To prepare this medicine, you need to pour 300 ml of boiling water into 1 tbsp. l. blackhead and leave in a closed thermos for several hours. After straining the infusion, take it 1 tbsp. l. before each meal, that is, 20-30 minutes before meals. |
| Orchis jelly | An excellent remedy with immunomodulatory properties. Used in the treatment of severe gastroenteritis. To prepare medicinal jelly, you need to grind 2 orchis tubers to a powder and pour in 200 ml of warm milk. Take 500 ml of jelly daily. If desired, you can sweeten it a little by adding 1 tsp. honey |
| Cranberry decoction | Another folk remedy used in the treatment of gastroenteritis. It has antiseptic properties, so the maximum effect can be achieved when treating an infectious form of the disease. To prepare the decoction, pour 400 ml of boiling water into 2 tbsp. l. dried berries and cook for 10 minutes over low heat. Strain the finished product and take 50 ml orally 3 times a day, preferably before meals. |
| Mint infusion | It is no secret that mint has medicinal properties, which is why it is included in many traditional medicines. It is also used in the treatment of gastroenteritis. To prepare the infusion, you need to pour 300 ml of boiling water with 30 g of mint leaves and leave for 1-2 hours in a closed thermos. After the product has cooled, strain it through several layers of gauze and take 100 ml daily. |
| Honey and oil | Perhaps the simplest recipe for preparing a folk remedy for the treatment of various forms of gastroenteritis. Mix 1 tbsp in one bowl. l. cow butter and honey, then cook the ingredients in a steam bath, stirring occasionally. After a couple of minutes, add a few drops of iodine and 2 tsp, remove from heat. After cooling, take the prepared product throughout the day. The duration of the treatment course is 30 days. |
Before using any folk remedy, you should definitely consult your doctor. Self-medication can make the situation worse.
Nutrition
A feature of therapeutic nutrition for gastroenteritis is to limit the amount of food consumed. In this case, you need to eat fractionally, that is, in small portions, but often. The diet must include bananas, crackers and rice porridge . During the treatment process, when the symptoms of the pathology gradually subside, the amount of food consumed can be increased. You can add fermented milk products, lean meats, boiled vegetables and various cereals to your diet.
Do's and Don'ts
When treating gastroenteritis, the following must be excluded from the patient’s diet:
- salty, spicy, smoked and fatty foods;
- fast food;
- coffee;
- sweet carbonated drinks;
- bakery products;
- sweets;
- fatty dairy products.
Important! You need to follow this diet throughout the entire treatment period and for another 3-4 weeks after the symptoms of the disease have disappeared. If a child has been diagnosed with chronic gastroenteritis, then he needs to follow a therapeutic diet constantly.
Therapeutic diet
Treatment
Patients diagnosed with moderate and severe degrees of the disease are subject to hospitalization. Treatment is conservative, with strict adherence to diet.
As part of the treatment of acute gastroenteritis, the following medications may be prescribed:
- antispasmodics;
- antibiotics;
- enzymes;
- enterosorbents;
- probiotics;
- antiemetics;
- antidiarrheal.
Enterosorbent drugs
In severe cases, massive infusion therapy is additionally performed.
A diet and plenty of fluids must be prescribed to replenish fluid in the body and restore water and electrolyte balance. Dietary nutrition implies a complete rejection of the following:
- spicy, salty, with a lot of seasonings;
- fried, fatty foods;
- foods that cause fermentation in the stomach;
- fatty fish and meats;
- strong coffee and black tea;
- confectionery, especially with cream;
- legumes;
- alcohol and surrogates;
- foods rich in fiber;
- vegetable and butter;
- dairy products.
The patient's diet should be based on the following recommendations:
- light food, but with sufficient amounts of essential minerals and vitamins;
- The optimal cooking method is boiled, baked without fat or crust, or steamed. Food must undergo heat treatment; raw food should not be consumed until complete recovery;
- The patient's meals should be frequent, but in small portions, with a break between meals of at least 2.5 hours;
- consistency of food – puree, grated, liquid;
- Dishes should only be consumed warm.
You also need to pay attention to the fact that on the first day you should completely refuse food; it is recommended to drink weak green tea without sugar, strengthening herbal decoctions, and still mineral water. Drinking plenty of fluids (at least 2 liters per day, this does not include soups) should be present throughout the entire course of treatment. The exact diet plan is prescribed individually, depending on the form, degree of development of the disease and the individual characteristics of the body.
Development of the disease in children of different ages
The intensity and severity of gastroenteritis depend on the age of the child, the type of pathogen and individual characteristics. Gastroenteritis in infants poses the greatest danger for a number of reasons:
- weak immune system;
- functional failure of the gastrointestinal tract;
- low weight and accelerated metabolism, causing rapid dehydration;
- Difficult diagnosis.
Before the age of one year, gastroenteritis is often caused by overeating caused by switching to artificial formulas. The process of feeding a baby occurs faster, and he does not have time to realize that he is full.
Incorrect (too early) introduction of complementary foods can destabilize the gastrointestinal tract in a child.
Children under 3 years of age are also characterized by a rapid progression of gastroenteritis. Their digestive system contains fewer enzymes than adults, and is often not yet able to cope with heavy, rough or spicy foods. During puberty, hormonal changes can cause the disease.
Some researchers find a relationship between the form of gastroenteritis and the age of the child - for example, children are more likely to suffer from rotavirus gastroenteritis than from bacterial gastroenteritis. However, there is no direct evidence for this theory.
Treatment options
When making a diagnosis, gastroenteritis is differentiated from other infectious and somatic diseases by taking into account general and epidemiological history data, as well as studying laboratory test materials. Tests are performed: blood - for antibodies to infectious agents, stool - for the presence of pathogenic bacteria.
On the recommendation of a doctor, a coprogram is made to detect disturbances in the functioning of the pancreas and hidden bleeding in the gastrointestinal tract.
In severe cases of gastroenteritis, upon admission to a medical facility, the patient's stomach is washed and measures are taken to prevent dehydration. To do this, the child is given plenty of fluids to drink, giving preference to saline solutions (for example, Regidron). In addition to taking fluids orally, it may be advisable to prescribe drip medications. Other medications are used according to indications.
Treatment of gastroenteritis in children is usually carried out in a hospital setting. To avoid infecting other family members, in the case of a viral form, quarantine is observed for a month after recovery. Mild and nutritional forms of the disease can be treated at home under the supervision of a local pediatrician.
Traditional recipes are used only during the recovery period. A drink made from cranberries helps strengthen the immune system, remove toxins and speed up recovery. To prepare it, 20 grams of dry or fresh berries are poured with boiling water and simmered over low heat for 15 minutes. After cooling, drink the drink 3-4 times a day, half a glass.
Causes of gastroenteritis
Provoking factors of pathology are conventionally divided into infectious, which are common, and non-infectious, which are less common.
The following reasons can cause gastroenteritis:
- Bacteria are common causative agents of the disease, including salmonella, shigella, E. coli, staphylococci and campylobacter. They can live in thermally unprocessed meat, fish and eggs, raw milk, juices, and dirty water. In food products left without refrigeration, bacteria actively multiply within an hour.
- Viruses can also cause gastroenteritis. Rotavirus infection is more common in children; adults get it less often due to the formation of acquired immunity. It is easily transmitted and spreads quickly among groups of the population, for example, in a kindergarten.
Gastroenteritis has long been given a second secret name - “dirty hands syndrome”, since the main route of transmission is nutritional or fecal-oral.
Inflammation of the wall of the stomach and intestines can be of a non-infectious nature:
- toxic gastroenteritis - occurs in case of poisoning with various substances - poisons of sublimate and arsenic, mushrooms (pale toadstool and fly agaric), drugs (NSAIDs, sulfonamides);
- nutritional - develops when eating substances that have an irritating effect on the mucous membrane of the gastrointestinal tract (a large number of hot and spicy dishes in the diet, strong alcoholic drinks);
- allergic (eosinophilic) - occurs when foodborne irritants (strawberries, chocolate, nuts, citrus fruits, seafood, honey and others) enter the gastrointestinal tract.
Additional predisposing development factors include vitamin deficiency, intestinal dysbiosis, hypothermia, chronic stress and alcohol-nicotine intoxication.
Classification
If we consider the etiological factor, we can distinguish the following subtypes of acute gastroenteritis in adults or children:
- nutritional – the development of this form of the disease is provoked by systematic overeating, with a predominance of spicy and too salty foods that irritate the intestines, abuse of alcoholic beverages and surrogates;
- acute infectious gastroenteritis - the provoking factor is a certain virus (salmonella, rotavirus, norovirus);
- allergic – with intolerance to certain foods or medications;
- toxic – poisoning by poisons, heavy metals, chemicals, as well as poisonous mushrooms and berries.
Somewhat less frequently, but still, an unspecified form of this disease occurs.
Forms of acute gastroenteritis are also distinguished according to the severity of the development of the pathological process:
- mild – there are no intense symptoms, attacks of vomiting and diarrhea are observed no more than 3 times a day, the patient’s condition normalizes after 1–2 days;
- moderate severity – frequent attacks of vomiting and diarrhea, body temperature rises, symptoms of the initial stage of dehydration may be present;
- severe – loss of consciousness, high body temperature, dehydration accompanied by frequent bouts of vomiting and intense loose stools.
Severity of acute gastroenteritis
The latter form of the disease requires urgent medical intervention, since dehydration is life-threatening and can be fatal.
Prognosis and prevention
With timely and adequate treatment of gastroenteritis, following the rules of diet therapy and prescribing a complex of medications, the outcome of the disease is favorable. Otherwise, the process may become chronic and serious complications will develop. Patients with chronic gastroenteritis are subject to mandatory medical observation and medical examination.
Prevention of pathology consists of following the rules of hygiene, thoroughly washing your hands before eating. Also recommended:
- do not drink water from unverified sources;
- avoid public eating places with a dubious reputation;
- If there is a person sick with gastroenteritis in the house, you should provide him with a separate room and utensils.
Disease prevention
There is a set of measures to reduce the risk of infection with rotavirus gastroenteritis. Pediatricians and infectious disease specialists recommend:
- promptly isolate sick people from others,
strictly observe the rules of personal hygiene,
- eat right, replenish nutrients in the body in a timely manner,
- thoroughly wash vegetables, herbs, berries and fruits,
- drink only well-purified water,
- refuse to consume products that have not undergone the necessary heat treatment,
- treat systemic diseases in a timely manner,
- have a full rest.
Teens and adults can get vaccinated against rotavirus.
Treatment of viral gastroenteritis
Treatment for viral gastroenteritis involves avoiding complications through measures such as maintaining hydration and reducing symptoms with antiemetics. It cannot be treated with antibiotics because it is not a bacterial infection. During oral rehydration, the patient is given water containing some salt and sugar.
Diet
Dietary management is an important factor in the management of patients with acute diarrhea. Of course, the most important thing is to maintain hydration: you need to drink plenty of fluids. Early in the disease, the BRAT diet, which includes four simple foods (the acronym BRAT is a mnemonic for bananas, rice, applesauce and toast), can be used. But prolonged dietary restriction does not help treat diarrhea. On the contrary, it can last for longer periods of time.
Course of the disease
The incubation period is relatively short for most infected individuals who develop symptoms. Signs appear 12-72 hours after infection. Typically, viral diarrhea has an abrupt onset, characterized by sudden intense vomiting, followed 24-48 hours later by watery diarrhea. The average duration of the disease is 1-3 days, sometimes prolonged episodes occur and the condition resolves within 8-10 days.
Regardless of the causative agent, viral diarrhea is assessed for dehydration. The mild form, where there are no signs of dehydration, up to two episodes of vomiting within 12 hours, a relatively low output of watery stool and no fever, will require only observation. Intense vomiting, repeated episodes of diarrhea (for example, 1 per hour, especially profuse viral diarrhea) are the main signs that indicate the need for treatment. The key concept of therapy is restoration of water and electrolyte balance (oral rehydration therapy and intravenous rehydration).
Rotavirus is transmitted through the fecal-oral route, mainly through close contact. Noroviruses are transmitted both directly from person to person (the infection is effectively transmitted by vomiting and airborne droplets), and indirectly through contaminated water and food.
Possible complications
In the absence of proper treatment, serious complications develop:
- Dehydration. Causes many problems, including death. Frequent vomiting and diarrhea lead to disruption of the body's water-salt balance. If the deficiency of fluid, vitamins and minerals is not replenished, further complications develop: convulsions, cerebral edema, renal failure, coma. Then comes death. It is necessary to carefully monitor the amount of fluid ingested and promptly diagnose and prevent dangerous signs of dehydration: dry lips and oral mucosa, small volume of urine, lethargy, sunken eyes.
- Sepsis. If the infection enters the bloodstream and spreads throughout the body, it can be fatal.
- Chronic gastroenteritis. Causes an advanced and untreated acute form of the pathology.
- Asymptomatic carriage. There have been cases where, after the symptoms of the disease disappeared, a person remained a carrier of the infection and infected others.
- There have been cases where reactive arthritis, Guillain-Barré syndrome and renal failure occurred after gastroenteritis.
What is gastroenteritis?
Gastroenteritis (synonyms: stomach flu, intestinal flu) is an inflammation of the digestive tract that affects the stomach and small intestine. The most common symptoms are diarrhea, vomiting and abdominal pain. Other possible symptoms include fever, lack of energy and dehydration. Symptoms usually appear in less than two weeks. Although sometimes called " stomach flu ", the illness has nothing in common with influenza .
Gastroenteritis can be caused by infections with viruses, bacteria, parasites, or fungi. The most common cause is viruses. In children, rotavirus infection is the most common cause of severe illness. In adults, the most common are norovirus and campylobacter. Transmission can occur from eating improperly prepared food, drinking dirty water, or direct contact with an infected person.
Preventative measures include washing hands with soap, drinking only clean water, maintaining sanitation, and breastfeeding newborn babies instead of using infant formula. Rotavirus vaccine is recommended for children. Treatment consists of adequate fluid intake. In mild or moderate cases, this is done with an oral rehydration solution consisting of a combination of water, salts and sugar. For breastfed children, continued breastfeeding is recommended. In more severe cases, intravenous fluids may be required. Children are recommended to take zinc. Antibiotics are usually rarely needed.
two billion worldwide , killing 1.3 million people. The disease mainly affects children in developing countries. In 2011, approximately 1.7 billion cases occurred among children under five years of , resulting in approximately 700,000 deaths. In developing countries, children under two years of often contract six or more infections per year. The disease is less common in adults, partly due to developed immunity.
How to distinguish acute gastroenteritis from other pathologies
The clinical picture of acute gastric inflammation is clear and does not cause difficulty in diagnosis by an experienced doctor. After examining a patient with acute gastroenteritis, the doctor will determine the severity of the disease and decide whether to send the patient to a hospital or treat on an outpatient basis.
The following studies will help clarify and confirm the diagnosis:
- endoscopic examination of the stomach and duodenum;
- general blood, urine and stool tests;
- bacteriological examination of stool, coprogram;
- sensitivity of the isolated pathogen to antibiotics.
The examination will show the gastroenterologist the cause of the disease and the degree of dysfunction of the body. After consultation with a doctor, an individual treatment plan for acute gastroenteritis is selected.
Signs and symptoms
Gastroenteritis usually presents with diarrhea and vomiting, and less commonly with just one symptom. Abdominal cramps may also occur. Symptoms usually begin within 12 to 72 hours of exposure to the infectious agent. If it is viral in origin, the disease usually goes away within a week. Some viral agents may cause associated symptoms such as fever, fatigue, headache, and muscle aches. If there is blood in the stool, the cause is unlikely to be viral and very likely bacterial. Some bacterial infections can be associated with very severe abdominal cramps and may persist for several weeks.
Children who develop gastroenteritis as a result of rotavirus infection usually recover within three to eight days. However, in less developed regions where access to medical care is difficult, diarrhea often persists for a longer period of time. Dehydration is a common complication of diarrhea, and children with significant dehydration may have low blood pressure, cyanosis, and abnormal breathing.
Approximately 1% of those infected with Campylobacter species develop reactive arthritis, and 0.1% develop Guillain-Barré syndrome. Infection with toxin-producing bacteria such as Escherichia coli or Shigella can lead to hemolytic uremic syndrome, which is characterized by low platelet counts, kidney failure, and low red blood cell counts. Children are more likely to suffer from this syndrome than adults. Some viral infections can lead to benign childhood epileptic seizures.