Pileated chest deformity is a pathology of the musculoskeletal system, characterized by protrusion of the chest forward. The sternum and costal cartilages resemble a keel, a “chicken” breast, hence the name keeled breast. The pathology is quite common and ranks second after funnel-shaped deformity.
The anomaly is congenital due to the inferiority of the epiphyseal and apophyseal bone growth zones. In men, the pathology occurs more often than in women and has a cosmetic defect. As a person grows, the chest begins to narrow and begins to compress the internal organs under the ribs.
Treatment with drugs will not have an effect, so the patient is immediately sent for surgery after diagnosis. The operation can be performed by thoracic surgeons, orthopedists, and traumatologists.
Keeled breasts can be combined with a hereditary pathology - Marfan syndrome. Marfan syndrome is a severe lesion in which a person has gigantism, the limbs are greatly enlarged and unnaturally mobile.
With Marfan syndrome, the functions of vision and the cardiovascular system are seriously impaired, and scoliosis of the spine is observed. In addition, with this anomaly, dissection of the aortic aneurysm occurs, which shortens a person’s life.
What is chest deformation and its types
The normal shape of the chest is an irregular cone with four sides. Chest deformity is a congenital or acquired change in shape.
There are the following types of deformation:
- keeled,
- funnel-shaped
- flat congenital.
Acquired deformities:
- emphysematous,
- scaphoid,
- paralytic,
- kyphoscoliotic.
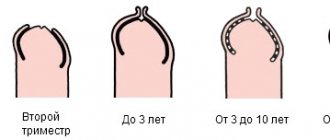
Congenital deformities damage the anterior wall of the sternum. Acquired - posterior and lateral surfaces of the chest. Funnel-shaped deformation is poorly noticeable in young children; by the age of three, as the child grows, it becomes more pronounced, as the depth of the funnel increases to 7-8 cm.
The chest cavity decreases, scoliosis forms, and the development and functioning of the internal organs of the chest cavity is disrupted.
Important! Congenital deformity in a child is treated surgically. Children with this pathology are lagging behind in physical development and often suffer from bronchopulmonary diseases.
Symptoms of keeled chest
Disturbances in any circulatory and respiratory functions do not make themselves felt at the birth of a child, but over time the chest begins to stretch anteriorly. In adolescence, patients complain of palpitations, frequent shortness of breath when playing sports, and fatigue when performing household chores.
During puberty, patients develop depression, increase in aggressiveness, and become withdrawn due to differences with peers. Such dissimilarity from peers makes it difficult to adapt socially, because children are afraid that they will be ridiculed, teased, given bad labels and nicknames.
Causes
Causes of chest pathology:
- diseases of the musculoskeletal system - scoliosis, chondrosis, rickets,
- inflammatory diseases of soft tissues, tuberculosis, asthma, eczema, rib tumors,
- infectious diseases in the first trimester of pregnancy,
- various injuries, burns,
- syndromes - Down, Turner, Wife, ankylosing spondylitis,
- unsuccessful surgical operations,
- strong physical activity,
- metabolic disease.
Complications of pathology
In the presence of congenital chest deformity in children, treatment is usually carried out at the age of 3–6 years. The child is actively growing and developing. If the problem is not given due attention, the pathology can lead to a decrease in lung volume, compression or displacement of vital organs and the development of secondary diseases.
With incomplete lung excursion, the child’s blood is poorly saturated with oxygen, and metabolism suffers. Babies with sternum deformation are stunted, are less resistant to infections and often get sick. During physical activity, sick children get tired faster than their healthy peers. In advanced cases, chest deformation can lead to the development of deadly conditions: arterial aneurysm, aortic rupture, etc.
Classification and characteristics
Medicine divides pathological forms of sternum deformation into:
- congenital - influenced by bad genetics, the pregnant woman’s use of alcohol, tobacco, drugs,
- acquired - due to diseases, burns in the chest area, various injuries.
Acquired deformities:
- Emphysematous - a consequence of pneumonia, emphysema. The front of the chest increases in size.
- Paralytic - lung diseases lead to changes in shape. The chest is reduced.
- Scaphoid - boat-shaped indentations in the upper and middle parts of the chest. This type is formed due to inflammatory processes in the spinal cord.
- Kyphoscoliotic - due to changes in the structure of the spine, the chest acquires asymmetry.
Congenital deformities:
- Keeled - chicken breast. The pathology is characterized by excessive growth of 5-8 costal cartilages. The patient's sternum protrudes forward in the shape of a keel, and the anteroposterior size of the chest increases.
- Flat chest - uneven development of the chest, a decrease in its anteroposterior size, can develop due to developmental delays and frequent colds.
- Emphysematous - develops with chronic pulmonary emphysema. The anteroposterior size of the chest increases, the patient's chest becomes barrel-shaped.
- Paralytic chest - a decrease in the anteroposterior and lateral size of the chest. The intercostal spaces are widened, the shoulder blades lag behind the back, and the collarbones protrude.
- Funnel chest is a defect caused by retraction of the sternum, anterior ribs and costal cartilages. The deformity occurs due to genetic changes in the structure of cartilage and connective tissue. The malformation reduces the volume of the chest cavity, curves the spine, displaces the heart, disrupts the functioning of the lungs, and changes blood pressure.
The convex chest has three degrees of deformation:
- I degree - the funnel is less than 2 cm, the heart is not displaced,
- II degree - funnel 2-4 cm, heart displaced up to 3 cm,
- III degree - the funnel is more than 4 cm, the heart is displaced by more than 3 cm.
Treatment options
Therapeutic tactics for chest pathology are determined based on the degree of deformation and existing dysfunction of vital organs. Some pathological conditions can be corrected using conservative treatment methods. Exercise therapy, massage, special gymnastics and physiotherapeutic procedures help with small funnel-shaped and keeled deformities of the chest. Conservative therapy maintains the proper functioning of internal organs and stops the progression of the pathology, but does not eliminate the cause of the disease.
READ ALSO: how to do gymnastics for a 6-month-old baby at home?
With moderate and severe degrees of sternum deformation, the child needs surgical treatment. After the operation, normal function of the chest organs is restored.
Conservative therapy
The hypotonic muscle with keeled, pectus excavatum and other types of chest deformity reacts poorly to the dynamic load of the antagonist movements, which leads to compensatory hyperactivity of other muscles. With the help of special gymnastic exercises (see the video for more details), massage and physiotherapy, it is possible to solve this problem and prevent further deformation of the bones. Gymnastics normalizes breathing and helps restore the natural functions of internal organs.
Massages are given to babies in courses. To achieve a visible effect, at least 12 courses will be required. General massage is recommended for infants.
READ ALSO: how to massage a 3-month-old baby at home and video tutorials
The doctor may also prescribe hormonal medications, vitamin-mineral complexes and a special diet high in calcium and vitamin D to the small patient. This will strengthen the child’s musculoskeletal system in case of deformities caused by metabolic disorders.
In some cases, special corsets are used to eliminate pathology. Orthoses fix the chest in the correct position. Such devices must be worn for a long time. Their help is resorted to in case of slight curvature of the sternum.
Surgical correction
If the deformation of the chest leads to aggravation of disturbances in the functioning of vital organs, this is a direct indication for surgery. Sometimes surgical correction is performed to eliminate a pronounced cosmetic defect.
In children, the chest is more elastic than in adults, so surgery is less traumatic for them. In total, there are more than 100 methods of surgical intervention for chest pathologies. Of these, operations are distinguished:
- with the introduction of implants;
- using clamps;
- with a 180 degree inversion of the sternum;
- without fixation.
If the operation is simple, then after a few days the patient begins gymnastics. In other cases, bed rest must be observed for 3-4 weeks.
Diagnostic methods
A crooked chest is visible during a routine examination of the patient. The doctor visually determines changes in the shape, symmetry, and circumference of the sternum; when listening, he detects wheezing in the lungs and heart murmurs.
To establish an accurate diagnosis, type and extent of the disease, clinical and instrumental studies are carried out. The patient must undergo a consultation with a thoracic surgeon, orthopedist, or traumatologist.
To diagnose changes in the heart and lungs, the patient is advised to visit a cardiologist, pulmonologist and conduct a series of examinations:
- X-rays of light,
- echocardiography,
- ECG,
- CT scan,
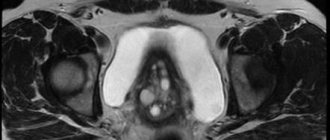
- MRI.
X-rays show a comprehensive picture of the changes - the degree and type of deformation. Computed tomography reveals abnormalities affecting the heart and lungs, and displacement of internal organs.
Magnetic resonance imaging provides data on bone and connective tissues. ECG, echocardiography and spirography show the condition of internal organs.
Diagnostics
Diagnosis of pathology is carried out on the basis of a visual examination. To clarify the characteristics of the deformation and the degree of its severity, the following may be additionally prescribed:
- Radiography. The data from this study help to judge the degree and nature of the curvature. It is carried out in two projections: lateral and anteroposterior. Allows you to determine how much the retrosternal space is enlarged, the heart is deployed and displaced, the costal arches are curved, and the position of the lungs is changed. The method does not make it possible to assess the degree of dysplastic disorders and features of deformation of cartilage tissue.
- CT. A highly informative method that allows you to assess the ratio of the anteroposterior to frontal size of the deformity. Visualizes internal organs, asymmetry of deformation, bone pathologies, damage to the chest, the degree of compression of the lungs, and displacement of the heart. All this data helps during surgery.
If there are complaints or suspicions of dysfunction of the heart or lungs, then additional tests are prescribed: EchoCG (ultrasound of the heart), ECG (heart function test), spirography (lung function test).
Treatment
Treatment methods depend on the degree of deformity, stage and type of disease. Treatment of curvature of ribs in children and adults with minor deviations involves conservative methods:
- massage,
- medical corsets,
- physiotherapy,
- set of physical exercises.
Therapeutic methods and medications do not correct bone curvature, but prevent relapses and help keep the body in good shape. For severe forms of deformity, surgery is performed. Surgical intervention in 90-95% of cases gives a positive result.
Features when treating children
In case of chest defects, the famous pediatrician Komarovsky recommends examining the child for possible pathologies that cause this type of deformation, and then carrying out conservative or surgical treatment, depending on the cause of the disease.
You can find out information about how to correct congenital chest deformity in a child during a consultation with an orthopedist. At the initial stage of funnel-shaped deformation, the vacuum bell method is used.
The procedure is performed on children over four years of age. In cases of complex forms of the disease, especially with a cleft chest, surgery is performed immediately.
The keeled curvature of the sternum is corrected by thoracoplasty. For a sunken chest, conservative therapy is carried out. Therapeutic gymnastics is carried out with 1 and 2 degrees of pathology. For a positive result in treatment, massage is prescribed.
The doctor performs operations in the third stage of the disease on children over the age of 7 years. The doctor implants a magnetic plate into the chest, then puts a special belt with a magnet on the patient from the outside.
The attraction of the magnet and the plate gradually leads to a therapeutic effect - sunken breasts are corrected after 2 years of wearing the plates.
Deformations of the sternum in adolescence occur from 11 to 15 years. The doctor determines how to treat chest wall displacement in adolescents. An effective method is to install a special orthosis, which exerts measured pressure on the sternum and gradually straightens it.
The operation is performed when all the bones are formed - by the age of 20. If the disease progresses, surgery is performed earlier.
Can it be fixed as an adult?
Chicken breasts are common in men. Conservative treatment is carried out comprehensively: therapeutic exercises, massage, painkillers and anti-inflammatory drugs. The therapy strengthens the muscle frame, improves blood supply to the lungs and heart.
If a girl’s bone protrudes forward, it is impossible to cure the disease with exercises alone. To get a positive result, the doctor prescribes surgery. In extremely severe cases, the thoracic vertebrae are fixed to stabilize the patient’s condition and prevent subsequent curvature.
Conservative options
Conservative measures in the treatment of chest deformities in children - exercise therapy, swimming, massage, wearing special compression systems, children's corsets. Exercise therapy for rib asymmetry is used to maintain normal tidal volume of the lungs. Physical exercises to correct a sternum defect help when the child’s chest deformity is minor.
To treat carinatum deformity, the most effective method is used - the Marcelo Ferre system, which eliminates chest asymmetry. The compression system is made of a lightweight aluminum plate that fits over the protrusion of the sternum, a support mechanism, and a compression gauge.
A flat sternum can be corrected with swimming, physical exercise and breathing exercises. In case of funnel-shaped deformity, conservative measures are indicated only for the first degree of deformity. If rickets has caused deformation of the sternum, then for young children the doctor prescribes vitamin D.
Children with chest deformities are always under constant supervision of specialists. Before the operation, a few days before the operation, they are sent for examination to the clinic to identify changes due to growth, progression of the disease and to determine the exact timing of the operation. While observing the child before surgery, the doctor carries out therapeutic measures to correct posture.
Surgical
When the deformation leads to irreversible changes, and therapeutic methods are ineffective, surgery is prescribed. Aesthetic and reconstructive surgery of the chest is performed for congenital and acquired deformities, after injuries, oncology operations, and insufficient development of the pectoral muscles.
Indications for surgical correction in children:
- Pathological changes - the chest compresses the great vessels, heart, lungs.
- Social adaptation - a child with cosmetic deformity develops a social inferiority complex. Children behave isolated in society.
There are several surgical techniques:
- Sternochondroplasty. Mark Ravitch method. The doctor makes a transverse incision on the anterior chest wall, the pectoral muscles are separated, then the costal cartilages are excised. After inserting the plate, the pectoral muscles are sutured and sutures are placed on the wound. This operation is quite effective, but traumatic. Incisions in the front of the sternum reduce the aesthetic result of the operation, so for many patients this treatment is unacceptable.
- The Nuss method is a minimally invasive intervention. The operation consists of making 2-3 cm incisions on both sides of the chest. An incision is made, then metal plates are inserted into the subcutaneous space, under the muscles, inside the chest and behind the sternum. A special steel or titanium plate is sutured to the ribs and muscles. The clamps straighten the sternum and fix it in the desired position. The doctor removes the plate after three years or leaves it for life. The recovery period lasts three weeks, then for three months it is necessary to reduce physical activity. Six months later the patient makes a complete recovery.
The doctor operates on a chest cleft immediately. For children under one year of age, the sternum is partially excised, then it is sutured along the midline. Flexible bones in infants heal quickly. In children older than one year, the operation begins with excision of the sternum, then the chest is expanded using rib grafts.
If necessary, the doctor installs a titanium plate for reliable fixation.
Surgery to correct grade 2 and 3 funnel deformity is performed at the age of 12-15 years. External sutures made of metal or synthetic threads and bone grafts provide fixation.
general characteristics
Keeled chest deformity refers to congenital anomalies of skeletal development. It does not occur so often, in approximately 7% of all cases of violation of the structure of the sternum. Mostly men suffer from this disease; in women, the chest abnormality is 4 times less common, and in addition, in them it is not so noticeable.
This deformity represents a change in the shape of the sternum. The chest bone protrudes forward at an angle or in an arched manner. It becomes similar to the keel of a boat, which is why it got its name. The ribs around the deformation sink and bend on one side or both. Typically, this pathology does not appear over the entire area of the chest; several pairs of ribs are affected - from 4 to 8. Sometimes the anomaly is also called “chicken breast”, since a similar shape of the sternum is observed in birds.
Typically, this pathology occurs separately, but in approximately 15% of patients, other anomalies of the skeletal structure or diseases are observed simultaneously with it. This is due to the fact that such deformation is associated with a disorder in the structure of connective tissue or pathologies that arise during intrauterine development.
Most often, carinatum is diagnosed in patients with Morphan syndrome. This is an anomaly in the structure of connective tissue, in which the structure of the human skeleton is severely disrupted. The patient has an asthenic thin physique, very tall stature, long limbs and an almost complete absence of subcutaneous fat.
Often, keeled breasts also appear in children with congenital curvature of the spine. Severe scoliosis can lead to gradual deformation of the ribs and sternum. In many cases, this pathology is combined with various diseases of the connective tissue, endocrine system, or congenital heart defects.
Surgery
If pectus excavatum causes psychological discomfort and does not affect the functioning of internal organs, surgical treatment can be abandoned. The defect can be visually eliminated using injection techniques or silicone implants.
Patients with stage 3 cobbler's breast and severe functional impairment have only one treatment option - surgery. Surgical intervention is performed using the Nuss method or the Ravich method.
Operation according to Ravich
Treatment using the Ravich method is carried out in several stages:
- The surgeon makes a horizontal incision on the front wall of the chest.
- Deformed cartilage is removed completely or partially.
- The bone located in the front of the sternum is crossed at the top of the socket.
- The lower part of the chest is raised and given the correct shape.
- The sternum is secured in its normal position using a metal plate that is placed under the bone. The edges of the structure are fixed to the ribs.
The metal frame is removed after six months or a year. The Ravich operation can be performed with some modifications. For example, using a supporting mesh or the patient’s own rib on a vascular pedicle instead of a plate. The surgical treatment option depends on the degree of VDHA, the age of the patient and other factors.
Development of pathology
At the birth of a child, the deformation of the formed keeled chest is often subtle. But as the child grows and develops, it progresses significantly. After a certain time, a cosmetic defect forms - its severity can be very different depending on how much the process of intrauterine development was disrupted and what the individual characteristics of the child are.
In contrast to the funnel chest, the keeled variety of its deformity is associated with pathological protrusion of the chest wall. This means that theoretically the chest cavity should not suffer, and at the same time the organs that are located in it should not suffer. However, protrusion is accompanied by changes in the lateral areas of the chest wall - the chest can be not only pointed, like a ship’s keel, but also narrowed.
There is no single “standard” for such a disorder; the chest with carinatum deformity can take on completely different shapes. Therefore, for convenience, this pathology is classified in the clinic. There are several types of classification (systematization) of this pathology, but the systematization of the types of pathology according to Fokin and Bairov (they are Russian clinicians) has the greatest practical importance. According to the classification, there are such types of keeled chest deformity as:
- costal;
- manubriocostal;
- corpocostal.
With the costal type, only the ribs are disfigured, the curvature of the sternum is not observed or is weakly expressed. In the latter case, it can be of a so-called rotational nature - the sternum seems to be slightly rotated around its axis. Deformation of the chest is formed due to the fact that the costal cartilages are bent forward.
With the manubriocostal type, the manubrium of the sternum (its upper fragment), together with 2-3 costal cartilages that articulate with it, is curved in the forward direction. The body of the sternum itself with the xiphoid process (its lower fragment) is displaced backwards.
With the corpocostal type, two options for the development of the keeled chest are possible:
- in the first, the sternum, like an arc, is bent forward in the lower and middle third, and the costal cartilages are curved inward;
- with the second, the sternum is directed obliquely forward and downward, protruding to its maximum in its lower third.
According to the degree of symmetry of the altered halves of the chest, the pathology is:
- symmetrical - both halves are curved to the same extent. But complete symmetry of the altered chest is rarely observed;
- asymmetrical - the ribs develop incorrectly, and the position of the sternum is curved along the axis.
Standard preoperative examination includes:
- Chest X-ray (frontal and lateral projection). It is advisable that the picture is recent, no more than 2 weeks before surgery)
- ECG
- EchoCG
- General tests required before surgery
- CT scan of the chest with 3D reconstruction of the skeleton
- Consultations with specialists (therapist, pulmonologist, allergist, gastroenterologist, urologist, gynecologist) if there is a concomitant pathology
- For hospitalization in the pediatric surgery department, additional tests may be required (stool analysis for the disenteric group, a certificate from an infectious disease specialist).
Why does chest curvature occur in children?
The occurrence of congenital anomalies is facilitated by disturbances in the formation of the child’s skeleton (bones, cartilage, ribs, spine) at the stage of intrauterine development. The causes of chest deformation are not reliably known.
Predisposing factors include:
- Hereditary predisposition . Children whose relatives have spinal curvature are at increased risk.
- Gene mutations . They occur spontaneously or with autoimmune diseases (Marfan syndrome, Down disease). They cause disruption in the formation of connective tissue, the structure of cartilage and bones.
Acquired forms of curvature are a consequence of complications of musculoskeletal diseases or systemic pathologies of internal organs.
The main reasons for the appearance of an anomaly in a child are as follows:
- rickets - abnormal bone development caused by calcium deficiency or metabolic disorders;
- scoliosis – lateral curvature of the spine;
- tuberculosis;
- chondrosis – dystrophic changes in cartilage;
- injuries;
- chest burns;
- malignant tumors;
- osteomyelitis – inflammation of the bone marrow;
- emphysema.
Anatomical classification
Based on the information that doctors received during the analysis of various clinical cases of deformity, it was possible to establish that the defect can be conditionally divided into 3 types:
- manubriocostal (from Latin manubris - handle of the sternum, costa - rib). If this type is diagnosed in a child, as a rule, the handle of the sternum moves forward, along with the nearby two or three costal cartilages. But at the same time, its body and xiphoid process move backward;
- corporocostal (from Latin corpus - body). As a rule, with this type, there is a displacement of the body of the sternum downward and at the same time forward, reaching a maximum in the lower part. This type is often combined with rib defects. This is where the name comes from;
- costal. The name speaks for itself. The cartilages of the ribs often bend forward, the sternum is deformed (curved) minimally.
Signs of chest curvature in a child
The anomaly develops gradually and clearly manifests itself during puberty. In newborns, dimples and bumps on the chest are barely noticeable. In adolescents, the ribs protrude strongly forward or sink, and disturbances in the functioning of all internal organs appear.
In addition to extensive forms of curvature, there are a number of rare pathologies of the sternum, which include:
- Poland syndrome . It is characterized by a set of defects: the child does not have part of the pectoral muscles and mammary glands, the ribs are curved, the layer of subcutaneous fat is very thin, the phalanges of the fingers are underdeveloped or fused.
- Congenital cleft (sternoskisis) . With this defect, the sternum is divided in two in the center. The pathology is diagnosed immediately after birth. In severe cases, the disease is accompanied by respiratory failure and delayed physical development.
- Currarino-Silverman syndrome - concave chest. In young children, the disease does not pose a threat to internal organs. Schoolchildren experience tachycardia, chest pain, shortness of breath on exertion, increased fatigue, and difficulty breathing.
Funnel deformity
This form develops gradually. Symptoms depending on age:
- In infants, the chest sinks when breathing or crying.
- The funnel is noticeable upon external examination in children under three years of age. Such kids are prone to frequent sore throats, bronchitis, and get tired of outdoor games.
- In schoolchildren, the ribs are raised at the edges, the shoulder arches are lowered down, and the stomach protrudes strongly forward. Children are underweight, have pale skin and thoracic kyphosis (hunchback). They complain of shortness of breath, increased sweating, and tachycardia.
Keeled form of pathology
In 90% of cases, such deformation of the ribs in a child does not cause any secondary symptoms and only causes moral discomfort. Only 2% of children have severe curvatures and complain of pressing pain in the heart area, shortness of breath, rapid heartbeat, and dizziness.
Radiation methods in assessing the degree of pectus excavatum (literature review)
Funnel chest deformity (Pectus Excavatum) is a curvature of the sternum and anterior ribs of varying shape and depth, leading to a decrease in the volume of the chest, compression and displacement of the mediastinal organs, causing functional disorders of the cardiovascular and respiratory systems, manifested in varying degrees severity and cosmetic defects [1].
Congenital deformity of the chest in children, according to various authors, ranges from 1% to 4%, of which 91% are the so-called “shoemaker's chest” or funnel-shaped deformity (Pectus Excavatum) of the chest. This pathology occurs 3 times more often in males than in women [2, 3].
Changes in the shape and volume of the chest are manifested by a decrease in the sterno-vertebral distance, which leads not only to a cosmetic defect, which in turn can lead to psychological disorders in the child, but also to a decrease in the excursion of the diaphragm and mobility of the chest, paradoxical or stridor (with compression and mixing of the trachea with the mediastinum) breathing, frequent development of bronchopulmonary diseases, digestive disorders (regurgitation and vomiting after eating), cardiovascular pathologies. [1]
The severity of chest deformation is most objectively determined using radiation research methods - chest x-ray in 2 projections and/or computed tomography.
In recent years, special attention has been paid to the objectification of radiological assessment of changes in the osteoarticular system. Various rating scales have, for example, been widely used in reconstructive spine surgery. [4,5,6,7,8]
One of the first classifications that made it possible to objectify the degree of chest deformation was the classification according to Z. Kopera and W. Krol 1957. The classification was based on determining the ratio of the upper and lower vertebral distance.
The most popular radial index for assessing the degree of deformation of the chest during funnel-shaped deformity is the Gyzicka index (Gyzicka 1962), which distinguishes 4 degrees of deformation [2,9]
The principle of determining the Gizycka index is based on the ratio of two distances - the smallest, determined on radiographs in a lateral projection, between the posterior surface of the sternum and the anterior surface of the vertebral bodies and the largest (Fig. 1).
Rice. 1. Determination of the Gizycka index [10]
A is the smallest distance determined between the posterior surface of the sternum and the anterior surface of the vertebral bodies. B is the distance between the true position of the sternum.
Table 1 shows the severity criteria for chest deformity based on the Giżycka index.
Table 1
The degree of chest deformation based on the determination of the Gizycka index
| Deformation degree | Gizycka index value |
| 1st degree | From 0.9 to 0.7 |
| 2nd degree | From 0.7 to 0.5 |
| 3rd degree | From 0.5 to 0 |
| 4th degree | From 0 to -0.5 |
Rice. 2. An example of determining the Gizycka index
Figure 2 shows a radiograph of a patient at SPBNIIF. The Giżycza index is calculated on radiographs of patients taken in a lateral projection, as shown in the image above. In the example above, we get distance A equal to 7 cm and distance B equal to 8 cm. We find their ratio (IG = A/B = 7/8 = 0.875) and round to the nearest hundredth, IG = 0.88, which corresponds to 1 power deformation.
JA Haller et al. (1987) to determine the severity of VDHA proposed using a computed tomographic index (CT index or Haller index), calculated from axial CT scans at the level of maximum retraction of the sternum. The Haller index is the quotient of the transverse dimension of the chest (the horizontal distance between the inside of the ribs) and the anteroposterior dimension (the distance between the anterior surface of the spine and the posterior plate of the sternum). Normally, the Haller index is about 2.5. With VDHA, the index increases in direct proportion to the depth of retraction of the sternocostal complex. When the Haller index is 3.25 or more, the operation is indicated [11].
Rice. 3. Determination of the Haller index - (Haller index) [12]
Rice. 4. Determination of the Haller index - (Haller index)
In the above example (Figure 4.) we get distance A equal to 28.2 cm and distance C equal to 7.3 cm. We find their ratio (Haller index = A/C = 28.2/7.3 = 3.86) . Thus, surgical intervention is indicated for this patient.
Based on the radiation indices, clinical classifications were developed according to Urmonsan V.K., Kondrashin N.I. (1983) and classification according to Timoschenko V.A. (1995)
The convenience of these classifications lies in the division of patients according to the clinical course of the disease, the form and severity of the deformity.
Numerous studies indicate a correlation between the degree of deformity and the frequency of clinical manifestations [12, 13, 14, 15, 16, 17].
Conclusions.
- Funnel-shaped deformation of the chest leads not only to a cosmetic defect, but also to the frequent development of broncho-pulmonary diseases, digestive disorders (regurgitation and vomiting after eating), and cardiovascular pathologies.
- The severity of chest deformation is most objectively determined using radiation research methods - chest x-ray in 2 projections and/or computed tomography.
- The frequency of clinical manifestations is directly proportional to the severity of chest deformation.
Literature:
1. Vinogradov A.V., Fishchenko P.Ya., Sologubov E.G., Bosykh V.G. Chest deformities as a risk factor for the development of diseases of the cardiovascular and respiratory systems in children // Issues of modern pediatrics. — 2003. — Volume 2. Appendix 1.- P. 62.
2. Isakov, Yu.F., Pectus excavatum deformity./ Isakov Yu.F., Stepanov E.A., Geraskin V.I. // Ruk. on thoracic surgery in children. M. 1978, p. 83–90
3. Roberts, A. The cardiofaciocutaneous syndrome/ Roberts A.// J. Med. Genet.-2006.-No. 11.-C. 833–842
4. Baulin I.A., Gavrilov P.V., Sovetova N.A., Mushkin A.Yu. Radiation analysis of bone block formation using various materials for anterior spinal fusion in patients with infectious spondylitis // Spine Surgery. 2019. T. 12. No. 1. P. 83–89.
5. Baulin I. A., Gavrilov P. V., Sovetova N. A., Mushkin A. Yu. Radiation features of the formation of spinal fusion in patients with spondylitis with various options for stabilizing the spine // Medical Alliance. 2019. No. 1. pp. 154–155.
6. Baulin I. A., Sovetova N. A., Kuklin D. V., Gavrilov P. V., Mushkin A. Yu. Radiation assessment of the formation of spinal fusion using titanium block lattices in patients with spondylitis // Doctor-graduate student. 2013. T. 60. No. 5.3. pp. 401–405.
7. Sang-Hyun S., Ung-Kyu C. Clinical significance of radiological stability in reconstructed thoracic and lumbar spine following body resection. J. Korean Neurosurg Soc. 2019. V. 56, I. 4. P. 323–329
8. D. Grob, S. Daehn, A. F. Mannion. Titanium mesh cages (TMC) in spine surgery. Eur Spine J. 2005. V. 14(3). P. 211–221
9. Goremykin I.V., Pogosyan K.L., Lukyanenko E.A. Correlation of the degree of funnel chest deformity with the severity of connective tissue dysplasia in children // Saratov Journal of Medical Scientific Research. 2012. T. 8. No. 3. pp. 842–845.
10. Razumovsky A. Yu., Savchuk M. O., Pavlov A. A. Pileated chest deformity // Pediatric surgery. 2009. No. 1. P. 45–49.
11. Haller JA, Kramer SS, Lietman A. Use of CT scans in selection of patients for pectus excavatum surgery: a preliminary report. Journal Pediatric Surgery 1987;22:904–6
12. Rebeis EB, Campos JRM, Fernandez A, Moreira LFP, Jatene FB. Anthropometric index for pectus excavatum. Clinics. 2007;62(5):599–606.
13. Ruzikulov U. Sh. State of the cardiorespiratory system with pectus excavatum in children // Doctor-graduate student. 2011. T. 47. No. 4.4. pp. 682–685.
14. Priyma N. F., Komolkin I. A., Popov V. V., Komissarov I. A., Shchegolev D. V. Anatomical and functional changes in the heart with pectus excavatum in children according to echocardiography // Genius of Orthopedics . 2011. No. 3. pp. 86–91.
15. Plyakin V. A. Clinical and morphological criteria for optimizing the surgical treatment of pectus excavatum in children // abstract of the dissertation for the degree of candidate of medical sciences / Scientific Center for Children's Health of the Russian Academy of Medical Sciences. Moscow, 2008
16. Aprosimova S.I. Kirgizov I.V., Dudarev V.A Assessment of the quality of life in children with pectus excavatum before and after surgical treatment // Kremlin Medicine. Clinical Bulletin.-2016.-No. 3.-P.44–48.
17. Kelly, RE Jr. Pectus excavatum: historical background, clinical picture, preoperative evaluation and criteria for operation/ Kelly RE Jr.// Semin. Pediatr. Surg.-2008.-No. 3.-P.181–193
Acquired deformity
Diseases that cause deformity:
- Rickets is a childhood disease in which the body grows too quickly, resulting in impaired bone formation and decreased flow of nutrients;
- Bone tuberculosis is a disease that affects adults and children and develops after direct contact with a carrier of the disease;
- Respiratory diseases;
- Syringomyelia is a disease associated with the formation of extra spaces in the spinal cord. The disease is chronic;
- Scoliosis is a disorder of the shape of the spinal column.
Severe burns and injuries also cause deformation.
Acquired changes are:
Emphysematous – barrel-shaped chest. The pathology develops after suffering a severe form of lung disease. The anterior plane of the chest begins to grow;
- Paralytic, when the diameter of the chest is reduced. The shoulder blades and clavicular bones are clearly defined, there is a large gap between the ribs, and when breathing, it is noticeable that each shoulder blade moves in its own rhythm. Paralytic deformation occurs in chronic diseases of the respiratory system;
- Scaphoid. Begins to develop in people with syringomyelia. A boat-shaped pit appears in the upper part of the chest;
- Kyphoscoliotic. The disorder is typical for people with diseases of the bones and spine, for example, bone tuberculosis. There is no symmetry in the chest, which interferes with the normal functioning of the heart system and lungs. The disease progresses quickly and is difficult to treat.
Prevention
It involves influencing the causes of this condition and includes several recommendations that must be followed unconditionally:
- Regular medical examinations in the therapist’s office (other doctors if necessary).
- Timely provision of therapy for respiratory system diseases.
- Prevention of injuries and burns in the sternum area.
- Children's sports (you can accustom your baby to physical activity literally from infancy, starting with special exercises).
- Observance by a nursing mother of a healthy diet and adherence to the principles of proper nutrition, healthy lifestyle.
The sooner the disease can be diagnosed, the more successful, faster and easier the therapy will be.
- Related Posts
- The appearance of green stool in a baby while breastfeeding: causes, symptoms, what to do
- Allergy to breast milk in infants
- How to treat diarrhea in a breastfed baby
« Previous entry
Types of treatment
In the first and sometimes second degree, treatment of funnel chest is possible without surgery. Patients with the third degree of VDHA need surgical correction due to the detrimental effect of the deviation on the respiratory and cardiovascular system.
Corrective therapy
Therapeutic gymnastics is carried out from the starting position lying, sitting and standing. The total load gradually reaches 20-25 minutes in time
You can treat sunken chest with conservative methods through physical exercises and a vacuum bell.
For people with a mild degree of deviation, the therapeutic complex of physical education is defined as the main therapy. As the disease progresses, surgery is recommended, and physical training at home is used as an aid.
The duration of the strengthening exercise is 30–40 minutes. Start by walking around the room for two minutes. After that:
- Hands down, feet shoulder-width apart. Inhaling, move your left leg back, arms up. As you exhale, return to your original position. Keep your head straight, chin slightly raised. Perform the exercise slowly, alternately for each leg. Repeat 6-8 times.
- Do not change the starting position. As you inhale, gently lower your body and spread your arms to the sides. Exhaling, return to the starting position. Do 6-8 approaches.
- Sit on the floor, straighten your legs, spread them to the sides. Place your hands behind your back and rest on the floor. Inhaling, lift your pelvis and throw your head back. Arch your back slightly. As you inhale, slowly return to the starting position. Repeat 4-6 times.
- Lie on your back, stretch your arms along your torso. Try not to move your diaphragm when breathing. Take 3-4 full breaths.
- Without changing your position, raise your legs, bending your knees, and rotate the imaginary pedals 8-10 times.
- Lie on your stomach, arms along your body. As you inhale, slowly raise your arms and spread your legs. As you exhale, take the starting position. Do 8-10 approaches.
The end of exercise therapy is walking around the hall for two minutes. You should not train with great strength, it is better to gradually increase the load. Corrections to the complex are made only by a doctor and a trainer. There is no other treatment at home; it is impossible to get rid of the problem using folk remedies. In addition to exercise therapy, you can choose a gentle sport, for example, swimming. It is also indicated for the prevention of relapses. But strength training and bodybuilding are not recommended.
Vacuum bell
Correction of chest deformity with a vacuum bell
Prescribed for boys and girls with concave chests. The method is effective if the cartilage tissue and ribs are sufficiently plastic, which is why it is not suitable for adults.
The lift is a device that creates a vacuum and a plastic bowl with edges covered with thick rubber. The soft material prevents injury and allows the device to fit tightly to the sternum.
The bell is placed on the deformation zone and the air is gradually pumped out. The vacuum “pulls” sunken ribs outward and reduces the funnel-shaped depression. Procedures are carried out from 10 months to a year.
When using a bell, there is a risk of cosmetic defects in the area of vacuum action: sagging, swelling or thickening of the skin. Important clarification: the method does not always allow you to correct the “shoemaker's chest”. Sometimes the device only reduces the depression by 2–4 cm.
Types of disease
All chest disorders that are known to specialists can be combined into two large groups. These are deformities such as congenital and acquired. But within each group there is its own classification. Also, depending on the location, a child’s chest deformity has several forms. It is believed that it can be anterior, lateral and posterior. Depending on the degree of impairment, the disease is often not clearly expressed, even practically unnoticeable until the appearance of serious pathologies affecting the functioning of the heart and lungs.
Congenital deformities are divided into the following types:
- Funnel-shaped, in common parlance this type of disorder is called “shoemaker’s chest.”
- Keeled, or “chicken breast”.
- Flat.
- Cleft.
Acquired disorders are divided into:
- Emphysematous.
- Paralytic.
- Kyphoscoliotic.
- Scaphoid.
It should be noted that with congenital deformities of the chest, most often violations occur on its anterior wall. If this is an acquired deformity, then both the lateral and posterior surfaces may be damaged. It is also necessary to know that if there is a congenital deformity of the chest in a child, its treatment is most often surgical.
Consequences and forecasts
During surgery, the patient is under anesthesia. During the operation, there is a risk of complications: respiratory failure, tongue retraction, pneumothorax, blockage of the airways with mucus, etc. Most often, the prognosis is good. After chest reconstruction, in 95% of cases, patients recover quickly. Rarely, a repeat operation is required to correct the defect.
Today, there are many methods for treating chest deformities in children. The pathology can be successfully treated if parents seek medical help in a timely manner.
Loading…
Share with friends!