Classification
According to their clinical course, proctitis is divided into acute and chronic forms.
- The acute form develops quickly, against the background of injury or an infectious disease, and has severe symptoms - pain and diarrhea. Lasts no more than 1 month.
- Chronic form - develops after the acute stage in the absence of necessary treatment. The clinical picture in the chronic process is not so pronounced: frequent diarrhea is noted, and blood and mucus periodically appear in the stool. Pain and itching in the anus occur during exacerbation and errors in diet.
There are cases of primary chronic proctitis, which develops when the rectum is damaged by Crohn's disease or ulcerative colitis (UC), tuberculosis, or tumor.
- Stomach ulcer.
When conducting an instrumental examination (proctoscopy, sigmoidoscopy), clinical forms of colitis are identified, characteristic of both acute and chronic processes:
- Hemorrhagic proctitis - on the inflamed intestinal mucosa there are multiple foci of hemorrhages, bleeding of varying intensity, and fibrin deposits.
- Catarrhal proctitis - colonoscopy reveals slight swelling of the mucous membrane, smoothness of folds, moderate hyperemia of the epithelium. This form of proctitis is the initial stage of the disease.
- Erosive proctitis - at this stage of the disease, multiple defects of the rectal epithelium are noted, but the muscle layer remains unharmed.
- Ulcerative proctitis - multiple, less often single ulcers of the mucous and muscular membranes, covered with fibrin, are noted. Old ulcers in the chronic course of the disease scar, thereby causing a narrowing of the intestinal lumen. Often the ulcerative process destroys the walls of blood vessels, causing bleeding. This form of proctitis is characteristic of Crohn's disease.
- Purulent proctitis is an uncommon form of the disease in which a bacterial infection, destroying the mucous membrane of the rectum, causes the formation of pus. Upon examination, the mucous membrane is highly swollen, hyperemic, and there is yellow-gray purulent content in the folds and crypts.
- Necrotizing proctitis - this form occurs when blood circulation in the rectum is impaired (intestinal infarction). The main reason for the development of this form is thrombosis of the mesenteric arteries, caused by atherosclerotic changes or blood clots “arriving” from the femoral artery or inferior vena cava system.
According to severity, proctitis is usually classified into the following options:
- Mild degree – pain is not intense, bleeding is minor, body temperature is not elevated, diarrhea up to 5 times a day.
- Moderate severity – severe pain during defecation, severe bleeding (even in the absence of feces during defecation), temperature increased to 38°C, diarrhea up to 10 times a day.
- Severe severity - the patient is in serious condition, body temperature is above 38°C, the anus is gaping, bleeding is pronounced from the rectum, hemodialysis is required. Such conditions develop with acute intestinal obstruction, cancer, necrosis of the large intestine, and Crohn's disease.
Symptoms of proctitis
- Pain during bowel movements;
- Constipation and diarrhea;
- Difficulty in determining the location of pain;
- Pain in the lower abdomen, lower back, intimate organs, but when taking an anamnesis at an appointment with a proctologist, it turns out that the source of pain is the area of the sacrum or anus;
- Pain and itching in the anal area, increasing with bowel movements;
- Irritation and sensation of heat in the anus;
- False urge to have a bowel movement;
- Discomfort in the perineum with radiation to the genitals. Common manifestations may be mistaken for another pathology, leading to delayed diagnosis and inappropriate treatment;
- Purulent, bloody or mucous discharge from the intestines.
The following signs indicate serious disorders caused by proctitis, which affect the entire body:
- Temperature increase;
- Loss of body weight;
- Lack of appetite;
- General weakness of the body;
- Psycho-emotional state disorders;
- Joint pain;
- Skin rash;
- Redness of the eyes and involuntary production of tears.
The last 3 signs characterize allergic, immune and infectious proctitis. Often these symptoms occur before local manifestations of the disease begin.
Causes of proctitis
The main reasons for the development of proctitis include the following:
- Infectious – inflammation of the mucous membrane of varying degrees can be caused by bacteria, viruses, fungi, and protozoa.
- Parasitic infestations can also often significantly destroy the wall of the rectum, cause persistent constipation, and are not accompanied by the characteristic discharge of blood and mucus. Colonoscopy often reveals huge conglomerates of parasites localized in the cecum, sigmoid, and less often in the rectum. Even if the helminths are localized quite remotely from the rectum, catarrhal inflammation ( catarrhal proctitis ) occurs, which is associated with the impact of waste products of worms on its walls, as well as a violation of trophism.
- Vascular is one of the most dangerous causes of proctitis in adults (usually in the form of proctosigmoiditis). As a result of cessation of blood circulation in the inferior mesenteric artery, which supplies the large intestine, aseptic necrosis of its tissue develops. In this case, unbearable abdominal pain occurs, usually lasting 2-3 hours, vomiting and diarrhea appear. After 3 hours, the pain subsides - this is called the period of “imaginary well-being”, since at this moment necrosis develops. After 2-3 hours, the patient is in stupor or already in a coma, the body temperature rises, the pulse quickens, the pressure drops - diffuse peritonitis develops. Timely seeking medical help in the first two hours from the onset of the disease saves life. When contacted after 6 or more hours, the mortality rate is 90%. The only treatment for this pathology is surgery.
- Traumatic - damage to the rectal mucosa can occur when inedible objects are ingested (fish bones, paper clips, cloves, etc.). Usually, accidentally (less often on purpose) swallowed objects cause erosive proctitis , less often ulcerative. Injuries can also be caused externally, through improper use of enemas, anal sex, or during medical procedures. Recently, traumatic proctitis is increasingly observed in men who massage the prostate, treat hemorrhoids, and masturbate with objects not intended for this purpose. It should be remembered that in this way you can not only introduce an infection into the intestinal cavity, but also pierce its wall, which will lead to fecal peritonitis and death.
- Tumors are a fairly common cause of proctitis. Tumors of the large intestine in our country rank 2-3 in frequency, second only to breast and prostate cancer. Rectal cancer accounts for 25-30% of the total number of colon cancers. A tumor of even a small size disrupts trophism and patency in the rectum
- Endogenous causes are Crohn's disease and UC.
Causes of pathology
As already mentioned, there can be many reasons for the occurrence of proctitis, ranging from minor trauma to the rectum and ending with serious cancer. The main ones include the following:
- Various injuries. The intestinal mucosa can be injured by frequent diarrhea, chronic constipation, hemorrhoids, or as a result of medical intervention.
- Infectious processes. Various pathogenic bacteria can provoke the occurrence of proctitis. Often the cause of the disease is an inflammatory process in other internal organs caused by the herpes virus, chlamydia, gonococci, cytomegalovirus, tuberculosis bacillus, and spirochete pallidum.
- Eating disorders. Excessive consumption of alcohol-containing drinks, spicy, salty, smoked foods.
- Damage to the body by parasites. For example, pinworms, tapeworms, dysenteric amoeba.
- Diseases of the gastrointestinal tract. General disorders in the digestive system often lead to serious problems, including diarrhea, constipation, and inflammation. Pathologies such as gastritis, cholecystitis, stomach ulcers, cirrhosis, hepatitis, and dysbacteriosis can provoke proctitis.
- Impaired blood circulation in the pelvic organs. This situation leads to the development of stagnation. Improper blood circulation often leads to hemorrhoids, varicose veins or thrombophlebitis.
- Radiation exposure. This therapy is carried out for oncological pathologies and often results in inflammation of the intestinal mucosa.
- Diseases in which the body begins to destroy its own cells are autoimmune diseases. For example, Crohn's disease.
- Malignant neoplasm in the rectum. The tumor provokes the release of toxins that affect the mucous membrane.
Additionally, there are a number of factors that can become a kind of trigger for the development of proctitis. These include malfunctions in the body’s immune system, the process of inflammation in the pelvic organs, frequent acute respiratory viral infections and sudden hypothermia. The so-called risk zone includes people with diseases of the colon, chronic hemorrhoids, anal fissures and those who practice anal intercourse.
Proctitis can also occur in children. Moreover, most often children under the age of one year suffer from it. The reasons for its appearance in children may be the following:
- milk protein intolerance;
- helminthic infestations;
- ingestion of a foreign body;
- poor nutrition;
- intestinal infections;
- incorrect insertion of a gas tube or rectal suppositories;
- congenital anomalies of the development of the digestive organs.
Proctitis in childhood can also be caused by impaired blood supply to the pelvic organs, diarrhea or constipation.
Symptoms
With an inflammatory process in the rectum, the following complaints are typical:
- pain in the anus that occurs during defecation, sometimes abdominal pain of varying intensity - characteristic symptoms of proctitis;
- diarrhea mixed with blood, mucus, and sometimes pus in the stool. With proctitis of parasitic etiology, whole or fragmented helminths can be seen in the feces.
- tenesmus - irritated intestinal mucosa causes a false urge to “go to the toilet.”
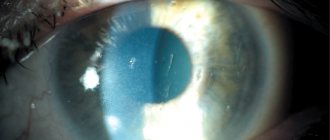
- at the beginning of acute proctitis, a spasm of the rectal sphincter occurs, and subsequently its full opening - a gaping anal hole (see photo above). In chronic forms, diarrhea can alternate with constipation, which is associated with a variety of causes, as well as alternating periods of remission and exacerbations.
- in moderate and severe cases of the disease, body temperature rises, symptoms of intoxication and fever appear.
Forms and types of proctitis
Proctitis is an inflammatory disease that affects the mucous membrane of the rectal wall.
The disease can occur in both chronic and acute forms. The acute form of proctitis, affecting the superficial layers of the mucosa, develops quickly. The symptoms of the disease are pronounced and permanent, but they quickly stop bothering the patient.
In the presence of a chronic form of proctitis, which has a gradual development, deep tissue damage is noted. Symptoms of proctitis are less pronounced, but bother the patient longer. The disease progresses in waves, with periods of exacerbation followed by periods of remission.
Depending on the changes occurring in the rectum, chronic proctitis is divided into:
- Normotrophic. With this type of disease, the mucous membrane has a normal appearance, no noticeable changes occur.
- Hypertrophic. With this pathology, the mucous membrane thickens, its folds are strongly pronounced.
- Atrophic. With atrophic proctitis, the mucous membrane becomes thinner and its folds are smoothed out.
Acute proctitis, depending on the nature of the changes occurring in the mucous membrane, is divided into:
- ulcerative - deep lesions appear on the intestinal tissues - ulcers;
- erosive - the intestinal mucosa becomes covered with superficial lesions;
- catarrhal-mucous - swollen tissues of a bright red color that secrete mucus;
- catarrhal-hemorrhagic - the mucous membrane swells, acquires a bright red color, multiple small hemorrhages are noticeable;
- ulcerative-necrotic - intestinal tissue becomes covered with ulcers, necrosis and rejection of the mucous membrane occurs in small areas;
- polypous - the mucous membrane is covered with polyp-like outgrowths;
- catarrhal-purulent - swollen mucous membrane, pus present;
- catarrhal-fibrous - intestinal tissue covered with purulent-fibrous plaque.
Among the most severe types of the disease are ulcerative, erosive, catarrhal-purulent, and polypous proctitis.
Diagnostics
An examination for inflammation of the rectum consists of a specialized examination, instrumental and laboratory research methods. The entire diagnostic process begins with a survey, examination in the knee-elbow position and digital examination of the rectum.
After the examination, to clarify the diagnosis, take a biopsy, and, if necessary, treatment, one of the following diagnostic procedures is performed:
- Rectoscopy - with a special rigid endoscope, the doctor examines about 20-25 cm of the rectum, which allows you to see all changes in the mucous membrane, the presence of tumors, hemorrhoids;
- Colonoscopy - unlike the previous method, this examination allows you to examine a large part of the colon - up to 150 cm. This method is advisable to carry out in cases where there is a suspicion of a tumor process, Crohn's disease, polyps of the upper parts of the colon. During a colonoscopy, it is possible to perform a biopsy of suspicious areas, as well as laser coagulation of bleeding areas.
- Irrigography is an x-ray research method that allows you to see the contours of the large intestine. This examination shows good diagnostic results for UC and Crohn's disease with damage to the rectum, neoplasms of the large intestine, as well as for identifying malformations (Hirschsprung's disease, aganglionosis, etc.), fistulas and diverticula.
Causes of intestinal inflammation
Rectal proctitis can be caused by general or local factors. The latter include various injuries, chemicals, the introduction of hot or cold solutions into the rectum, neoplasms, and the transfer of infection from nearby organs. Proctitis can be caused by mechanical injuries, self-massage of the rectum, etc.
Proctitis of the rectum, which occurs due to exposure to irritating chemical factors, hot or cold solutions, usually appears during treatment with folk remedies: excessive use of enemas, rectal suppositories, etc. Alcohols, essential oils, turpentine, iodine are irritating to the intestinal mucosa , tinctures of mustard or hot pepper.
Exacerbation of proctitis can occur due to the spread of infection entering the rectum from other organs: vagina, perirectal tissue, bladder, urethra. The causative agents of the infection can be different types of cocci, chlamydia, trichomonas, and E. coli. In cancer patients, proctitis can occur due to the spread of a tumor of the rectum or perineum.
The reasons that led to the development of the inflammatory process include malnutrition, parasitic diseases, intestinal motility disorders, gastrointestinal infections, and radiation exposure. Often the pathology is diagnosed in people suffering from alcohol addiction and lovers of spicy food. Proctitis often occurs when dysentery, salmonellosis, or enterovirus infection are detected. Proctitis can occur upon contact with pathogenic microorganisms of the intestinal mucosa, as well as with prolonged diarrhea.
Proctitis is often detected in people suffering from irritable bowel syndrome, large intestinal dyskinesia, and circulatory disorders. All patients who have pathologies of the gallbladder, liver, and pancreas are at risk.
Treatment of intestinal proctitis
When treating proctitis, both during the period of exacerbation and in the acute form, you should adhere to a mechanically and chemically gentle diet. If flatulence is present, limit the consumption of carbohydrates and dairy products.
If you are prone to constipation, you should eat more fruits, vegetables, and bran bread.
When treating infectious proctitis and colitis, it is preferable to use antiseptics:
- Intetrix - take 2 tablets 2 times a day for 10 days;
- Ersefuril (analogs Enterofuril, Stopdiar, Ecofuril ) is a very effective drug in the treatment of infections of the large intestine, which is highly active against E. coli, salmonella, clostridia, shigella and staphylococci. The drug should not be used under the age of 3 years or during pregnancy. Take the medicine 4 times a day, 1 capsule, for a course of 5-7 days.
For abdominal pain and flatulence, antispasmodics provide good relief:
- Spasmomen is a drug that causes relaxation of the smooth muscles of the intestine. Use 1 tablet 2 times a day for 2-3 weeks. The drug has no contraindications or side effects.
- Dicetel is a drug similar in effect to the previous one, but it cannot be used during pregnancy, childhood, or severe intestinal damage, as it can cause smooth muscle atony.
For persistent diarrhea, astringents (black tea, sage infusion, bird cherry fruits, oak bark), enveloping drugs ( Almagel, Phosphalugel, Maalox ), and sorbents (activated carbon) are prescribed. Enveloping and astringent drugs are especially necessary for erosive proctitis to protect the damaged areas from further destruction.
Imodium (lopreamide) is recognized as the drug of choice for the treatment of diarrhea. The drug Imodiup Plus has also proven itself very well , which includes simethicone, which absorbs intestinal gases, which is very necessary for diarrhea and flatulence.
For constipation, osmotic laxatives are usually prescribed:
- Forlax – take 2 sachets 2 times a day with meals.
- Duphalac is an effective drug that can be used by children from birth, as well as during pregnancy. Dosage for children is 5-15 ml depending on age. In adults, 15-40 ml - for the treatment of infectious proctitis, 20 ml 3 times a day for 10 days.
espumizan is successfully used, 1-2 capsules orally 3 times a day.
For proctitis of any etiology, it is prohibited to take non-steroidal anti-inflammatory drugs and painkillers. These medications may “mask” serious symptoms and treatment may not be started on time.
Treatment
Treatment of proctitis begins with excluding from the patient’s menu certain foods that irritate the rectal mucosa: fatty, spicy, sweet, salty, sour, spices, vegetables, berries, fruits. The following foods are suitable as a diet:
- eggs,
- porridge,
- cottage cheese,
- lean boiled meat and fish,
- soups,
- cutlets,
- jelly,
- stale bread.
Treatment is often carried out at home. Inpatient treatment is prescribed for the most severe forms of proctitis. In this case, the patient must completely give up alcohol. Special physical activity is prescribed. Constantly lying down with proctitis is not recommended, as this contributes to atrophy of the rectal muscles. Even with chronic forms, it is necessary to perform light physical exercises to strengthen the muscles.
How to treat inflammation of the rectal mucosa? Despite the fact that the patient is being treated at home, he must follow the recommendations of the doctor, who prescribes him special medications and enemas:
- Antibiotics: penicillin, macrolides, chloramphenicol, cephalosporin, aminoglycosides, metronidazole, tetracycline.
- Antispasmodics in the form of no-shpa.
- Antihistamines: Vividrin, Nalocrom, Intal, sodium cromoglycate, bicromate.
- Cleansing enemas.
- Therapeutic enemas with collargol, chamomile, sea buckthorn oil, calendula.
- Sitz baths with potassium permanganate.
- Suppositories and injections that improve tissue regeneration.
- Glucocorticoids - improving the hormone of the adrenal cortex: methylprednisolone, hydrocortisone, betamethasone, dexamethasone, triamcinolone, budesonide.
The chronic form of proctitis is treated:
- Sanatorium treatment,
- Mud therapy,
- Massage,
- Radon baths,
- Drinking mineral waters
- Diathermy,
- Therapeutic gymnastics.
Surgery is performed when complications occur:
- In case of paraproctitis, the purulent part of the adipose tissue is excised.
- If the rectum is narrowed, its expansion is prescribed.
- In case of ulcerative colitis, no improvement after medication, or tumors, appropriate operations are performed.
Folk remedies do not have a positive effect. You should follow the advice of a doctor who prescribes the medications, ointments, suppositories, and enemas needed for treatment.
go to top
Prevention
To prevent the development of proctitis, generally accepted rules should be followed:
- Diet. Reduce food intake that irritates the digestive tract - smoked, spicy, fatty foods.
- Observe the rules of personal hygiene - regularly and thoroughly toilet the external genitalia, since infection often enters the intestines from there.
- Avoid unprotected sexual intercourse - to exclude STDs, which can also affect the rectum, especially in men with homosexual orientation.
- Contact a doctor in a timely manner to identify and treat other organs of the gastrointestinal tract. When the first symptoms of proctitis appear, you should seek help from a surgeon or proctologist as soon as possible.
Treatment of erosive proctitis
In case of inflammation of the rectal mucosa of the erosive type, conservative treatment is carried out in a hospital setting. The main goals of therapy are the elimination of all irritating factors that led to the development of the disease, as well as the fight against inflammation and the prevention of erosion becoming an ulcer. It is mandatory to carry out measures to normalize stool.
For infections, antibiotics such as Neomycin sulfate, Kolimycin and other drugs are used to treat proctitis. If the inflammation is caused by parasites, antiparasitic drugs are selected.
For treatment, sitz baths with potassium permanganate solutions are used, suppositories with methyluracil and other drugs are prescribed. The outcome of treatment depends on the willingness of patients to follow all the doctor’s recommendations, as well as on the severity.
Forecast
Depending on the cause of inflammation of the rectum, timely initiation of adequate treatment, the prognosis can be favorable or unfavorable.
For example, if the disease is caused by an infection, and treatment is started from the appearance of the first symptoms at the stage of catarrhal proctitis, recovery occurs in 7-10 days.
The prognosis is questionable and sometimes unfavorable for lesions of the rectum due to ulcerative colitis, tuberculosis, Crohn's disease, and oncological pathology.
Erosive type of pathology
Erosive proctitis is an inflammation of the rectum, in which defects form on the mucous membrane. When healing occurs, no scars remain on the surface of the intestine.
The erosive type is characterized by a sudden onset with an increase in body temperature, false urge to defecate, and chills. Patients are bothered by pain in the rectal area, sometimes radiating to the lumbar region, perineum, and sacrum.
Patients with the erosive form complain of burning, itching, and a feeling of heaviness in the anal area. Their stool is disrupted: it becomes liquid, with impurities of blood and mucus. At the beginning of the pathology, contractions of the sphincter occur, and then it relaxes. This is manifested by the gaping of the anus, the discharge of mucus, liquid feces, and blood.
How intense the clinical picture will be depends on the subtype of erosive proctitis. Thus, the gonorrheal type is characterized by mild symptoms: mild itching, mild burning, minor pain, false urges.
Nutrition for chronic proctitis
All patients are prescribed a special diet. People with proctitis should adhere to the following rules:
- Avoid eating spicy foods;
- give up fatty and fried foods;
- steam food;
- exclude rough foods from the diet.
During an exacerbation, it is necessary to give up sweets, fresh fruits and vegetables for a while. The latter are best consumed boiled. If you have proctitis, it is forbidden to drink carbonated water, coffee and alcohol.
You should not eat a lot of foods rich in coarse fiber.
It is recommended to include in the diet jelly, compotes of dried apricots and apricots, boiled meat, lean fish, porridge, non-rich broths, puree soup, steamed cutlets and boiled vegetables.
Legumes, cabbage and other foods that cause fermentation processes in the intestines are excluded from the menu. During the remission phase, the diet is expanded. An important aspect of proper nutrition is complete abstinence from alcohol. Alcoholic drinks can aggravate the course of the disease and cause complications.
Thus, the chronic form of proctitis most often develops against the background of acute inflammation. With proper treatment, the prognosis is favorable.
Development mechanism
Radiation proctitis occurs after radiation therapy if the total dose of radiation absorbed by tissues exceeds the tolerable value of 50 grams/rad. The higher this indicator, the greater the likelihood of developing pathology.
Under the influence of radiation, cell reproduction (proliferation) in the intestinal tissues is disrupted, exfoliation (desquamation) and atrophy of the epithelial layers occur. The mucous membrane becomes inflamed, and muscle fibers are often involved in negative processes. The blood supply deteriorates, which may result in areas of necrosis and ulceration and cicatricial narrowing of the rectal lumen. Sometimes ulcers lead to the formation of fistulas and intestinal bleeding.
According to the clinical course, the following types of rectitis are distinguished:
- Mild (catarrhal) . This is the initial stage of the disease, characterized by redness and swelling of the mucous membrane.
- Medium (erosive-desquamative) . At this stage, epithelial cells are exfoliated and tissue integrity is disrupted.
- Severe (ulcerative) . The most dangerous stage of the disease, in which ulcers and intestinal obstruction form.
Ulcerative rectitis often becomes chronic and is difficult to treat. Obstruction (blockage) of the rectum requires surgery and a colostomy.
Radiation rectitis
This is a separate type of disease. This type of proctitis occurs rarely. It may appear in patients with cancer after radiation treatment. The pathology mainly affects the female gender.
If the patient was exposed to 65 Gy of radiation, then with a 50% probability we can say that post-radiation proctitis will appear.
As a rule, after radiation therapy, rectitis makes itself felt after 3 months. It can appear immediately in any form, bypassing the initial catarrhal condition.
Reviews
Dear readers, your opinion is very important to us - therefore, we will be glad to receive feedback about the chronic form of proctitis in the comments, this will also be useful to other users of the site.
Tatiana
It all started for me six months ago. At first itching and burning, which I did not immediately pay attention to, after some time I began to notice streaks of mucus and blood in the stool, and this alerted me. Using rectoscopy, the proctologist identified proctitis. I was prescribed Salofalk tablets and suppositories, which I took for a month. At a follow-up appointment, the doctor said that the disease was in remission. I used the same suppositories, but in a lower dosage, for several more months. Since then, the proctitis has not worsened.
Elena
Not a single gastrointestinal disease can be cured unless you follow a diet. I came to this conclusion thanks to my own experience. I have been suffering from proctitis, which has become chronic, for a long time. No treatment helped until she began to abstain from spicy, salty and fatty foods. As soon as I pulled myself together and started eating porridge and steamed food, everything returned to normal by itself. Sometimes, of course, the disease worsens, but this happens extremely rarely. By the way, in addition to following the diet, I also reviewed my drinking. Instead of regular tea, chamomile or rosehip tea, no beer or kvass, I also forgot about carbonated drinks. I wish everyone good health!
Treatment with folk remedies
The use of some natural ingredients and medicinal herbs along with the use of modern medications will also contribute to the process of treating an inflamed rectum.
The list of recipes providing therapy based on folk remedies is quite wide.
Enemas, the main task of which is to relieve inflammation of the mucous membrane of the lower intestine.
- Chamomile microenemas: to perform you will need 3 spoons of flowers, poured with 250 ml of boiling water. The infusion, aged for about two hours, must be filtered, and then injected into the anus using a syringe. If possible, it is recommended to keep the solution inside for 10-15 minutes. Instead of this raw material, it is allowed to use the same number of calendula flowers.
- Wormwood leaves (40 g) also help reduce inflammation and speed up the regeneration of affected tissues. To prepare such a decoction, wormwood needs to be poured with 1.5 liters of boiling water and additionally boiled over fire for 5-10 minutes.
- To achieve a healing effect, it is allowed to perform enemas based on oak bark infusion. Preparing the solution is not difficult: pour 50 g of raw material into a liter of boiling water and keep on fire for at least 5 minutes.
- Using nettle, larkspur roots and thistle inflorescences, you can prepare a more complex, but no less effective, decoction. Approximately 3-4 g of each raw material must be poured into 200 ml of boiling water, then allowed to brew for two hours.
Sitz baths are an alternative to therapeutic enemas.
- 40 g of a collection of dried plants: chamomile, dried flowers, knotweed, eucalyptus and salvia should be poured with two liters of boiling water and left for a short time on low heat. The strained infusion is used for the procedure, which is recommended to be performed for at least 15 minutes.
- Using the same scheme, you can prepare a decoction of 200 g of field pine grass. The cooled infusion should be poured into a basin and lowered into it for 20-30 minutes.
Oils and ointments.
- Sea buckthorn oil is used to reduce inflammation of the mucous membrane. A tampon soaked in this product must be inserted into the anus and left inside for as long as possible. It is wise to perform this procedure at night.
- Propolis and vegetable oil, taken in a ratio of 1:3 and heated by steam, will also serve as an excellent remedy for treating chronic proctitis at home.
- Gill ointment is prepared on the basis of toadflax herb and lard. 30 g of crushed raw materials must be combined with 70 g of fat, and then boil this mixture in a water bath. The resulting pulp must be squeezed out and cooled, then applied to a gauze swab and inserted into the anus.
- In the same proportions you can take lard and a combination of the following herbs: sage, water pepper, oak bark, chamomile flowers and toadflax herb. The crushed mixture should be poured with melted fat and left for 48 hours.
Herbal decoctions are intended for oral administration as maintenance treatment during periods of remission of the disease.
- A collection of dandelion root (20 g), marigold (10 g), nettle (35 g) and plantain seeds (35 g) should be poured into 300 ml of boiling water and kept in a steam bath for 5-7 minutes. It is recommended to take the decoction during the day in small volumes of 50-100 ml.
- A simpler recipe involves the use of chamomile and calendula (7 g of each raw material). 250 ml of boiling water is enough to obtain the desired concentration. The decoction should be drunk every hour, 20-30 ml.
- Tansy flowers, string, valerian root and raspberry stems, taken in equal parts, will help eliminate the symptoms of inflammation. The decoction prepared in 500 ml of water must be cooled and taken 50 ml during the day.
Currently reading: Rectal proctitis
Treatment of the disease with folk remedies during periods of rest is recommended to be carried out in courses, the total duration of which should be at least 1-2 weeks.
Treatment of radiation proctitis
Therapy is carried out comprehensively - with the use of medications, local remedies, vitamins, and a special diet. The therapeutic effect does not appear immediately; patients must have considerable patience. The main condition is the elimination of the disease, due to which it was necessary to use radiation methods.
Systemic medication
Mild and moderate forms of rectitis can be treated on an outpatient basis, under the supervision of a doctor. The following drugs are prescribed:
- Antibiotics . They are used as prescribed by a doctor - in the presence of a bacterial infection, taking into account resistance (immunity) to this group of drugs.
- Desensitizing drugs - Tavegil, Claritin, Fencalor and others. Relieves itching and irritation in the anus.
- B vitamins in injections, ascorbic acid tablets . Normalize metabolism and increase immune defense.
- Novocaine for presacral blockade . An anesthetic is injected into the area of the anterior surface of the sacrum, thereby relieving pain, which is difficult to relieve by other means.
- Antispasmodics - Papaverine, No-shpa, Meteospasmil, Duspatalin and others. Helps cope with tenesmus and cramping abdominal pain.
- Enzymes – Mezim Forte, pancreatin, Festal and other drugs to stabilize digestive processes.
- Laxatives . Prescribed for persistent constipation. Preference is given to drugs with a mild effect - Laminaride, Guttalax, Kafiol, Mucofalk. It is not recommended to use potent drugs, as they can cause spasms and irritation of the mucous membrane.
For diarrhea, take Imodium, Loperamide, Lopedium and other medications prescribed by the doctor that reduce excessive contractions of the intestinal muscles.
It is advisable to treat radiation ulcerative lesions in a hospital. This condition requires strict medical monitoring and immediate surgical measures for possible perforation (through damage) of the colon.
Topical preparations
Suppositories are effective and easy to use, the active ingredients of which actively affect the inflamed areas without penetrating into the blood and without causing collateral damage to other organs. The following rectal suppositories are used in the treatment of radiation proctitis:
- "Proctosan" . They successfully relieve pain because they contain the anesthetic lidocaine. The second ingredient, bufexamak, has anti-inflammatory, regenerating and desensitizing effects.
- "Methyluracil" . They heal minor injuries well, help restore the epithelial layer and strengthen local immunity.
- Suppositories with belladonna . Available by prescription - they contain belladonna extract. They have a pronounced analgesic effect.
- "Ultraproct" . Eliminate inflammation, swelling and burning, tone blood vessels. The active substance is fluocortolone.
- "Relief" . Contains an extract from shark liver. They stop inflammatory processes, heal wounds and cracks in the rectum.
- "Salofalk" . Made on the basis of mesalazine, a potent compound effective in the treatment of ulcers and erosions. Analogs are Pentasa and Asakol candles.
- "Natalsid" . Contains sodium alginate and brown algae extract. Relieves swelling, stops bleeding.
If rectitis is accompanied by a bacterial infection, suppositories are prescribed: Posterizan, Metronidazole, Syntomycin and other rectal drugs that destroy pathogenic microflora.
Microenemas with infusion of chamomile, calendula, collargol solution, sea buckthorn oil, and fish oil have proven their effectiveness. They should be placed after cleansing the intestines, before going to bed. With the permission of the doctor, patients can take sitz baths with potassium permanganate, and also use rectal tampons soaked in medicinal ointments.
Treatment with local remedies does not cancel drug therapy, but only complements and enhances its effect. For radiation proctitis complicated by rectal stenosis, surgery is indicated .
Medical treatment of rectitis in a hospital
What treatment does radiation proctitis require? Today, medical treatment of proctitis is considered a very difficult task. All treatment procedures can be carried out at home; when radiation proctitis is severe, proper treatment is urgently needed. A suitable solution would be to provide high-quality therapy in an inpatient department.
To relieve symptoms and unpleasant feelings, a set of measures is prescribed, which includes:
- Constant treatment regimen.
- Maintaining hygiene.
- Use of medications.
In order to successfully eliminate the signs of post-radiation proctitis, the patient must follow a diet, with the exception of very spicy, salty, sour foods, fresh vegetables and fruits, as well as alcohol, juices and various sweets, as well as take the necessary medications. For this type of disease, it is recommended to consume not very fatty soups and pureed boiled meat. Compliance with the drinking regime is considered more important.
What you need to know about radiation therapy for colorectal cancer
Drugs are prescribed such as suppositories for regeneration, antimicrobial or antiviral agents, sometimes antispasmodics, antihistamines or hormonal versions of drugs.
Antimicrobial therapeutic therapy for proctitis is carried out only after there is a clear sign of an unfavorable response of the digestive intestinal microflora to antibiotics.
To achieve the desired result, stool examination and medications are prescribed. The duration of use and dose of substances should be prescribed only by a specialist.
When is surgical treatment necessary?
Surgical resolution of pathology is indicated in rare situations; as a rule, the indications include severe conditions.
- Proctitis is of the paracancrosis or neoplastic type; it is caused by malignant neoplasms. In the later stages of oncology, ulceration and bleeding are sometimes observed.
- When pathologies such as nonspecific ulcerative colitis, UC, localized atypically low are detected.
- When paraproctitis occurs and there is an encysted purulent focus in the thickness of the pelvic and near rectal tissue.
Advice! There may also be a number of reconstructive plastic manipulations. For example, when treating proctitis of an ulcerative nature, a scar appeared on the mucous membrane, causing its stenosis and problems with defecation. In this case, the surgical procedure is carried out to restore intestinal patency.
Prognosis and prevention
The prognosis for proctitis, in particular in its chronic form, is favorable . If the treatment regimen is drawn up correctly and treatment is carried out in a timely manner, rapid recovery and stable remission can be achieved.
Prevention consists of eliminating negative factors that can affect the development of the pathological process. It is important to maintain hygiene, promptly treat inflammation of the pelvic organs and genitourinary system, lead a healthy lifestyle, and use a condom when practicing anal sex.
Signs of acute proctitis
From the effects of radiation on the colon, there is a disruption of the normal division and maturation of cells, their peeling, atrophy, and covering with scales.
In acute proctitis, symptoms begin to appear at an early stage:
- periodic painful urge to empty the intestines;
- paroxysmal pain that gets worse after going to the toilet
- effusion of blood, pus and anus;
- burning, itching, presence of a foreign object in the anal canal.
Manifestations of the disease
- physical weakness;
- high temperature up to 38 degrees;
- chills with purulent-ulcerative proctitis.
Usually after 3-4 days, acute symptoms begin to subside. Especially if patients are undergoing treatment taking antibiotics and anti-inflammatory drugs. But after a certain time, symptoms can flare up again, as if delayed, 3-4 months after exposure to radiation. Frequent urination, passing feces in small portions, pain in the anus, dull pain in the left iliac region (in the rectal area) begins to bother me.
An obvious sign of radiation proctitis is the passage of stool with mucus. The manifestation of early symptoms cannot be ignored: false urges during bowel movements, paroxysmal intense pain after emptying the intestines and the release of feces, constant secretion of mucus, with intensification after bowel movements, a pulling urge to defecate with pain radiating to the abdominal muscles, rectal bleeding, uncharacteristic mucus discharge , weight loss.
What are the treatment options for post-radiation rectitis?
To treat the pathology, antibiotics are required.
Radiation rectitis is treated with medication. Therapeutic therapy includes:
- use of antibacterial and antihistamine drugs;
- carrying out local anti-inflammatory measures;
- use of vitamin complexes.
The table shows effective pharmaceuticals and their effect on the patient’s body:
| Medication | Therapeutic effect |
| "No-shpa" | Eliminates pain syndrome |
| "Amoxicillin" | Eliminates infection |
| "Colibacterin" | Reduces intestinal motility |
| "Spazmalgon" | Relieves spasm |
| "Hifenadine" | Relieves allergic symptoms |
| Vitamins C, group B | Reduce negative radiation radiation |
| "Bifidubakterin" | Improves the functioning of the gastrointestinal tract |
| "Mesalazine" | Eliminates intestinal inflammation |
Local anti-inflammatory procedures are an important component of complex therapy for post-radiation rectitis. They provide for cleansing the intestines and eliminating inflammatory manifestations. Effective therapeutic effects are provided by:
Therapy is supplemented with a local preparation - suppositories with sea buckthorn oil.
- enemas with chamomile infusion or collargol solution;
- microenemas with fish oil;
- rectal suppositories with sea buckthorn oil;
- sitz baths using potassium permanganate;
- warm shower on the perineal area;
- drinking herbal decoction of sweet clover;
- intestinal lavage with a solution of silver or alkaline mineral waters.
When treating post-radiation rectitis, it is recommended to eat properly. It is necessary to avoid spicy, salty foods, alcoholic drinks, sweets and increase your drinking regime. If fistulas form against the background of radiation rectitis, cicatricial narrowing of the intestine occurs, surgical methods are used to eliminate the pathology. The prognosis for recovery is mostly favorable. Prevention of the disease involves the use of methods for eliminating cancer tumors that have less negative impact on intestinal tissues.
Research methods
To identify the disease, both laboratory and instrumental research methods are used. Diagnosis begins with examining the patient and analyzing his symptoms. A connection between proctitis and radiation is always found.
A general blood test reflects signs of the presence of an inflammatory process - leukocytosis, an increase in ESR, a shift of the formula to the left. This method helps assess the severity of the disease, but cannot be used to make a final diagnosis.
https://www.youtube.com/watch?v=rTQfxpTmdGM
The most informative method of examination is sigmoidoscopy. When examining the walls of the rectum, the following is found:
- hyperemia;
- swelling of the mucous membranes;
- the presence of blood and mucus in the lumen.
In addition, this method allows you to determine the presence of complications such as strictures, ulcers, abscesses and perforation of the organ wall. Erosions are most often found on the anterior part of the intestine, in some cases they lead to the formation of fistulas. The examination should be combined with a biopsy of the mucous membranes.
Histological examination helps to assess the severity of pathological changes in tissues. To identify the causative agent of infection, a bacteriological analysis of a smear from the anus is performed.
Since the disease is defined by the same symptoms as ulcerative colitis, it is necessary to be able to distinguish between these pathologies. The former is supported by previous radiation therapy and the presence of ulcerative defects in the anterior part of the rectum. In colitis, pathological changes are widespread; they affect all mucous membranes of the organ.
The examination of patients begins with a visual examination, examination of existing signs, and identification of the connection of the disease with radiation exposure.
Diagnostic tests
- blood for the ratio of the total leukocytes (in%) to assess the severity of the disease;
- general blood test to determine increased ESR, leukocytes in the blood;
- sigmoidoscopy is an effective informative examination method;
- histological examination to determine the degree of pathological changes in tissues;
- bacteriological smear from the anus to detect infection (a nutrient medium is inoculated to grow colonies of the pathogen);
- stool analysis for occult blood and worm eggs in cases of suspected worm infestation or infestation;
- biopsy of the mucous membrane for complications of proctitis, fistula formation.
In case of erosive sphincteritis of the rectum, the doctor will examine the perineum, note defects: spastic contraction or relaxation of the sphincter, and determine whether blood is bleeding from the anus. Next, he will conduct a rectal examination for swelling and mucous discharge from the rectum.
Other instrumental research methods:
- sigmoidoscopy with the introduction of a sigmoidoscope into the intestinal lumen to view changes in the mucosa;
- rectoscopy with the introduction of a special mirror into the anus to identify redness of the walls, the presence (absence) of fibrinous-purulent plaque;
- biopsy with tissue sampling from different parts of the intestinal epithelium mucosa, followed by histology and cytology examination.
Diagnosis of erosive proctitis is differential. It is important to find differences from similar conditions: anal fissures, oncology (with the disintegration of neoplasms in the walls of the rectum), internal hemorrhoids, non-erosive proctitis.
Therapy for radiation proctitis is complex. The initial goal is to reduce the harmful effects of radiation on the body.
Patients are prescribed:
- vitamins B, A, C to remove and neutralize free radicals;
- antihistamines to relieve itching and swelling;
- antiviral, antibacterial drugs based on test results;
- painkillers for severe pain due to exposure to radiation etiology;
- hormonal agents for restoration of the intestinal mucosa, healing of lesions caused by radiation.
If proctitis progresses, the intestinal canal has clearly narrowed, scars, fistulas and neoplasms have formed, then doctors resort to surgical intervention.