Fistula is a rather serious pathology, characterized by the formation of purulent passages through the intestinal fiber. Depending on the number and location of the holes, the fistula can be complete or incomplete. The entrance hole of a complete fistula is localized on the wall of the rectum, while the exit hole is located on the skin around the anus.
Incomplete internal rectal fistula is a pathology in which there is only an inlet and a blind ending in the perirectal tissue. However, the purulent processes that accompany paraproctitis can cause an incomplete fistula to break out, as a result of which it becomes complete.
What are rectal fistulas
Rectal fistulas (perianal fistula) are purulent formations that represent a passage between the rectum and the outer skin. Sometimes there is no connection with the external environment; the holes are located inside the intestine.
The channel itself is formed under the influence of pathogens that destroy the soft tissues of the organ. Along the fistula canal, branches and pockets of pus can form, which worsens the treatment process and slows down the patient’s recovery.
The risk of getting sick is higher in an adult patient, but children can also be affected by this pathology. The disease in a child develops and proceeds similarly to that in older patients.
What is this
Rectal fistula is a consequence of chronic paraproctitis, in which ulceration of the tissues of the rectum occurs and the formation of a fistula, the channel of which comes out near the anus.
Under the influence of unfavorable factors, not only the tissues of the rectum are destroyed, but also the nearby fiber. Therefore, it is possible that the outlet may appear next to, in front of, or behind the anus.
There are several types of fistulas:
- Full. In this case, the entrance opening of the fistula is located in the rectum, and the exit opening is located next to the anus. During examinations, when a special marker is fed through the rectum, fluid leaks out of the outlet.
- Incomplete. A rectal fistula has an inlet, but no outlet. In this case, secretions and purulent discharge accumulate in the canal. As a result, the purulent contents break through and pour out. Often patients do not suspect the presence of such a pathology and learn about it only when it spontaneously opens.
There are also several forms of fistulas according to the type of formation:
- Transsphincteric. The most common type. It is characterized by a branched system of canals, the presence of suppuration and a large amount of scar tissue around the fistula. Located near the sphincter, the outlet is located directly next to the anus.
- Intrasphincteric. Characterized by a small amount of scar tissue around, the fistula canal is straight, the exit is located near the anus, and the entrance is in any part of the rectum.
- Extrasphincteral. In this case, the perirectal fistula has a curved canal that goes around the sphincter. It is characterized by the presence of numerous scars and ulcers.
There are 4 degrees of complexity that this pathology may have:
- 1st. The fistula canal is short, and there are no signs of scar formation or purulent infiltrates in the surrounding tissues.
- 2nd. It is characterized by the formation of scar tissue around the internal opening of the canal, but there are no ulcers yet.
- 3rd. The entrance channel is narrow, but there are no abscesses or purulent pockets.
- 4th. The entrance hole is wide, with numerous scars. In the surrounding tissues there are many infiltrates and pockets filled with pus.
The treatment strategy is determined based on the nature and condition of the fistula.
Classification of rectal fistulas
Rectal fistulas are classified according to several criteria. They are divided into different types according to their structure and location. The following fistulas are distinguished:
- Complete, incomplete and internal . The latter can be separated into a separate group. Complete ones are characterized by the presence of 2 holes - internal and external, from which pus flows into the external environment. Incomplete fistulas have an internal opening, but no external one. An incomplete fistula ends blindly in the organ cavity, but tissue destruction gradually occurs under the influence of pathogens and an external opening is formed.
- The formations described above are external . As for the internal formations, they are characterized by the presence of 2 holes at once, but the anal fistula itself is located within the rectum; pus does not flow outward, only into the cavity of the organ itself.
- Based on their location relative to the anus, intra-, trans- and extrasphincteric fistulas of the rectum are distinguished. The first may be located slightly inward from the anus or adjacent to the hole itself. Transsphincteric are located directly in the sphincter tissues. Extrasphincteric formations form outside the opening and are easy to detect by visual inspection.
Fistulas can also be divided into straight and branched depending on the configuration of the fistula canal. With the second option, the formation of purulent pockets is possible, which complicates and delays treatment.
Treatment
It is important to understand that fistulas cannot be treated with medications and traditional medicine. The only treatment that can achieve a complete cure for the disease is surgery.
Drug therapy is used solely to relieve symptoms and as an aid to speed up recovery.
From pharmacological groups the following are recommended:
- fourth generation systemic antibiotics for oral administration: Metronidazole, Amoxicillin;
- painkillers: Detralex, Hemoroidin, Phlebodia;
- healing drugs with anti-inflammatory properties (externally): Levosin, Levomekol, Fuzimet.
- full course of physiotherapeutic procedures: electrophoresis, ultraviolet irradiation.
Operation
Treatment for fistula is surgical. The main goal is to block the entry of bacteria into the cavity, clean it and excise (remove) the fistula tract.
The operation to remove a rectal fistula is usually prescribed routinely. When chronic paraproctitis worsens, the abscess is usually opened urgently, and the fistula is removed after 1-2 weeks.
Contraindications for surgery:
- Severe general condition.
- Infectious diseases in the acute period.
- Decompensation of chronic diseases.
- Blood clotting disorder.
- Kidney and liver failure.
Depending on the complexity of the fistula, the following surgical methods can be performed:
- excision along the entire length of the fistula with or without suturing the wound;
- excision with plastic surgery of the internal fistula opening;
- ligature method;
- laser cauterization of the fistula;
- filling the fistula tract with biomaterials.
A competently performed operation in a specialized hospital guarantees a complete cure in 90% of cases. But, as with any operation, there may be undesirable consequences:
- Bleeding both during and after surgery.
- Damage to the urethra.
- Suppuration of a postoperative wound.
- Incompetence of the anal sphincter (incontinence of feces and gases).
- Recurrence of the fistula (in 10-15% of cases).
Staying in the hospital after surgery:
- The first days when the patient is in the hospital, a gas tube is placed, analgesics and antibiotics are prescribed, and dressings are performed.
- From the 2nd day, food is allowed - gentle and easily digestible pureed food, drinking plenty of fluids. Sitz baths with a warm antiseptic solution, pain-relieving ointments, and, if necessary, laxatives and antibiotics are prescribed.
- The length of hospital stay after the intervention can vary - from 3 to 10 days, depending on the volume of the operation
After discharge from the hospital, the patient needs to be especially attentive to his own well-being and immediately consult a doctor if the following symptoms occur:
- Sudden rise in temperature
- Constant pain in the abdominal area
- Fecal incontinence, excess gas
- Painful bowel movements or urination
- The appearance of purulent or bloody discharge from the anus.
It is very important that the patient did not have stool for the first 2-3 days after the operation. This will provide the wound with sterile conditions for healing. Subsequently, the diet expands, but it is necessary to avoid constipation, which can cause sutures to separate. Additional recommendations:
- Meals should be fractional, 6 times a day in small portions.
- It is important to drink enough fluids, at least 2 liters of water per day, so that the body recovers faster and also to prevent constipation.
- You should not eat foods that irritate the intestines. These include carbonated and alcoholic drinks, large quantities of chocolate, hot spices and flavorings, chips, fatty meats, etc.
Forecast:
- Intrasphincteric and low transsphincteric fistulas of the rectum can usually be permanently cured and do not entail serious complications.
- Deep transsphincteric and extrasphincteric fistulas often recur.
- Long-term fistulas, complicated by scarring of the rectal wall and purulent leaks, may be accompanied by secondary functional changes.
Causes of rectal fistula
Rectal fistulas are formed when bacteria penetrate the organ tissue. Inflammation occurs, which is called proctitis. The pathological process is able to penetrate into the surrounding soft tissues and become infected. This disease is called paraproctitis, it occurs in acute and chronic forms.
With these pathologies, purulent contents accumulate in a limited cavity, that is, an abscess is formed. Then the pus breaks out, the abscess cavity communicates with the environment. This is an anal fistula. In such cases, pus can leak not only onto the patient’s skin, but also into the internal cavities of the body.
In the pathogenesis of fistulas, the timeliness and completeness of treatment of the underlying disease, concomitant pathologies of the digestive tract, especially gastric ulcers, Crohn's disease, diverticulosis, tuberculosis and cancer of any part of the intestine, hemorrhoids are important.
People with fungal infections, immunodeficiencies, and syphilis are predisposed to the formation of fistulas.
Rectal fistulas can form after proctological and gynecological surgical interventions.
Classification
Clinical classification of osteomyelitis is carried out according to many criteria. The more precise the diagnosis, the clearer the treatment tactics become.
Types of disease depending on the pathogen:
- caused by nonspecific microflora (gram-positive or gram-negative): staphylococcus, pneumococcus, streptococcus, proteus, Escherichia coli and Pseudomonas aeruginosa, less commonly anaerobes:
- caused by one type of microbe (monoculture);
- associated with the association of 2 or 3 different types of microorganisms.
- specific for infectious pathology:
- syphilitic;
- leprous;
- tuberculosis;
- brucellosis;
- other.
- no pathogen was detected.
Bactericidal damage to bone layers.
There are clinical forms of the disease:
- hematogenous:
- after an infection of another organ;
- post-vaccination;
- other.
- post-traumatic:
- after fractures;
- after operation;
- when using spoke devices.
- firearms;
- radiation;
- atypical (primary chronic):
- Brody's abscess;
- Ollier and Garré osteomyelitis;
- tumor-like.
Flow options:
- generalized:
- septicotoxic;
- septicopyemic;
- isolated toxic.
- focal:
- fistulous;
- fistulaless.
Character of the current:
- acute (in particular, lightning);
- subacute;
- primary chronic;
- chronic.
The following stages of the osteomyelitic process are distinguished:
- acute;
- subacute;
- ongoing inflammation;
- remission;
- exacerbation;
- recovery;
- convalescence.
Phases of defeat:
- intramedullary (only the bone marrow is affected);
- extramedullary.
Based on localization, osteomyelitis of tubular and flat bones is distinguished. In long tubular bones, different parts can be affected: epiphysis, diaphysis, metaphysis. Among the flat bones affected are the skull, vertebrae, shoulder blades, sit bones and ribs.
Local complications of osteomyelitis:
- sequestration;
- fracture;
- bone, paraosseous or soft tissue phlegmon;
- pathological dislocation;
- formation of a false joint;
- ankylosis;
- joint contractures;
- violation of bone shape and development;
- bleeding;
- fistulas;
- vascular complications;
- neurological complications;
- muscle and skin disorders;
- gangrene;
- malignancy.
Variants of the disease with common complications:
- amyloid damage to the kidneys and heart;
- severe pneumonia with lung collapse;
- inflammation of the pericardium;
- sepsis;
- other.
The most common variants of the disease are acute hematogenous (in childhood) and chronic post-traumatic (in adult patients).
The disease most often affects certain bones of the human body.
Osteomyelitis of the thigh
Symptoms of femoral osteomyelitis.
It is observed in people of any age, most often of hematogenous origin, but often develops after surgery on the bones. Accompanied by swelling of the thigh, fever and impaired mobility of adjacent joints. A large fistula forms on the skin, through which pus is discharged.
Osteomyelitis of the leg bones
Signs of osteomyelitis of the lower leg bone.
It is observed more often in adolescents and adults, and often complicates the course of tibia fractures. Accompanied by redness and swelling of the lower leg, severe pain, and the formation of fistula tracts with purulent discharge. The tibia is affected first, but then the fibula always becomes inflamed. The patient cannot step on his foot.
Osteomyelitis of the calcaneus
Signs of osteomyelitis of the calcaneus.
Unlike the forms described above, it usually has a long course and often complicates infectious diseases of the foot, for example, diabetes. The main signs are pain and swelling in the heel, redness of the skin, and the formation of an ulcer with the release of purulent contents. The patient may have difficulty walking while resting on the front of the foot.
Osteomyelitis of the shoulder
It often occurs in childhood, has an acute course, accompanied by fever, swelling, and pain in the arm. As the disease progresses, pathological fractures are possible.
Metatarsal osteomyelitis
Signs of osteomyelitis of the metatarsal bone.
It develops when the surgical treatment of a wound resulting from a foot injury is insufficiently thorough. It can also complicate the course of diabetes. Accompanied by pain and swelling of the foot, difficulty walking.
Vertebral osteomyelitis
Develops mainly in adults against the background of immunodeficiency or septic condition. Accompanied by back pain, headache, palpitations, weakness, fever.
The vast majority of cases of the disease are caused by staphylococci.
These microorganisms are widely distributed in the external environment. They are found on the surface of the skin and in the nasal cavity of many healthy people.
Damage to staphylococcal infection.
Microbial agents can penetrate bone matter in different ways:
- Through blood vessels. Bacteria that cause inflammation in other organs, for example, pneumonia or pyelonephritis, can spread through the vessels into the bone tissue. In children, the infection often penetrates into the growth areas - the cartilaginous plates at the ends of the tubular bones - the humerus or femur.
- Infected wounds, endoprostheses. Microorganisms from puncture, cut and other wounds enter the muscle tissue, and from there spread to the bone substance.
- Fractures or operations when infectious agents enter directly into the bone substance.
The bones of a healthy person are resistant to the development of osteomyelitis. Factors that increase the likelihood of pathology:
- recent injury or surgery to bones or joints, including hip or knee replacement;
- implantation of a metal bracket or wires during osteosynthesis;
- animal bite;
- diabetes with high blood sugar;
- peripheral arterial diseases, often associated with atherosclerosis and smoking, for example, atherosclerosis or obliterating endarteritis;
- the presence of an intravenous or urinary catheter, frequent intravenous injections;
- hemodialysis;
- chemotherapy for cancer;
- long-term use of glucocorticoid hormones;
- injection drug addiction.
Symptoms of rectal fistula
Patients with this disease note the appearance of purulent discharge (see photo) on underwear or clothes, which brings significant discomfort to the patient’s daily life.
With a large amount of pathological discharge, irritation of the skin occurs, and complaints of itching and burning in the anal area appear.
Another inconvenience is that the pus has an unpleasant odor. Other complaints of patients with rectal fistulas:
- Presence of pain syndrome. Its severity depends on the type of fistula. If it is external and complete, then the pain is minimal. In the case of an incomplete fistula, especially an internal one, the symptoms are more pronounced. The intensity of pain increases with prolonged exposure to an uncomfortable position, sudden movements, prolonged walking, or during defecation.
- Intoxication of the body may occur with complaints of high temperature, weakness, headaches, decreased ability to work, and emotional lability.
- Rectal fistulas tend to have an undulating course, with exacerbations and remissions. During decompensation, patients experience the complaints described above. During the period of remission, the general condition of the patients does not suffer, but purulent discharge may be present in small quantities.
- With a long course of the disease, gradual depletion of the body occurs, and even during remissions there are complaints of general weakness, increased irritability, poor sleep, increased body temperature, headaches and dizziness.
External rectal fistulas are easy to detect during external examination. To diagnose internal formations, instrumental methods are required. Rectal fistulas are an extremely unpleasant pathology, but possible complications pose a particular danger.
Stages and manifestations
The fistula canal in the rectum is formed over a short period of time, depending on the stage of development, the patient is bothered by certain complaints:
| Stage of development and course of pathology | Clinical manifestations |
| First stage | Already at the very beginning of the development of the fistula canal, the patient begins to be bothered by unpleasant sensations, which are still moderate in nature. This:
|
| Development and exacerbation | The clinical picture becomes more obvious. Signs such as:
|
| Chronization of the process | In the absence of therapy, the pathology becomes chronic. Symptoms such as:
|
| Remission stage | Despite the fact that the pain syndrome disappears at this stage, the patient still has other, very unpleasant signs that indicate the presence of pathology. This:
|
Complications
It is important to know why rectal fistula is dangerous. An acute process threatens the spread of infection to the entire body, that is, sepsis. This complication has a high risk of death.
Also, pathology can become chronic, which affects the general condition of patients. They become emotionally labile, irritable, and their level of ability to work is significantly reduced.
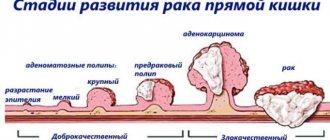
With a long course of the disease, malignant degeneration of tissues can occur, that is, rectal cancer is formed. Also, an anal fistula can lead to scarring and narrowing of the anal sphincter, which negatively affects its full functioning.
Symptoms of bone osteomyelitis
- fever and chills;
- bone pain;
- swelling of the affected area;
- dysfunction of the affected limb - inability to raise an arm or step on the affected leg;
- the formation of fistulas - holes in the skin through which pus is released;
- poor health, in children – irritability or drowsiness.
Sometimes the disease occurs with almost no external manifestations.
You should seek medical help if you have a combination of fever and pain in one or more bones.
The doctor must conduct a differential diagnosis with the following diseases:
- rheumatoid arthritis;
- infectious arthritis;
- synovitis;
- intermuscular hematoma, including festering;
- bone fracture.
Chronic osteomyelitis of bone
This form most often serves as the outcome of an acute process. A sequestral cavity is formed in the bone substance. It contains loose pieces of dead bone tissue and liquid purulent discharge. The contents of the sequestration box are released through the fistulas onto the surface of the skin.
Fistulas on the surface of the skin.
The development of the disease is wave-like: the closure of the fistula is replaced by a new phase of inflammation and pus discharge. When the exacerbation subsides, the patient's condition improves. Skin temperature normalizes, pain disappears. Blood counts are approaching normal. At this time, new sequesters are gradually formed in the bone substance, which begin to be rejected and cause an exacerbation. The duration of remission can be several years.
Signs of relapse resemble acute osteomyelitis. Inflammation and pain occur in the affected area, a fistula opens, and soft tissue phlegmon may develop. The duration of relapse is determined by many conditions, primarily the effectiveness of treatment.
Primary chronic forms occur without signs of an acute stage. Brodie's abscess is a single round cavity in the bone substance, surrounded by a capsule and located in the bones of the leg. The abscess contains pus. There are no pronounced symptoms of the inflammatory process, the disease is sluggish. During exacerbation, pain occurs in the leg, especially at night. Fistulas do not form.
Sclerosing osteomyelitis is accompanied by an increase in bone density and periosteal layers. The bone thickens and takes on a spindle shape. The medullary canal narrows. This form is difficult to treat.
Acute osteomyelitis
The most common variant of this process is hematogenous. It is observed mainly in boys. Phlegmonous inflammation of the bone marrow canal develops.
The toxic variant occurs at lightning speed and can lead to the death of the patient within a few days. The septicopyemic variant is characterized by the presence of ulcers not only in the bone substance, but also in the internal organs.
Most patients have a local form of the disease. The disease begins suddenly. There is a feeling of fullness and intense pain in the limb, often near the knee, shoulder or elbow joints. It intensifies with movement. Body temperature rises.
There is pallor of the skin, rapid breathing and pulse, lethargy and drowsiness. The limb is in a bent position, movements in it are limited. Swelling and redness of the skin occurs above the area of inflammation. There is severe pain when tapping in the affected area or in the direction along the bone axis.
X-ray changes appear only 2 weeks after the onset of the disease.
Diagnosis of rectal fistulas
The doctor analyzes the patient’s complaints, collects anamnesis, conducts a general examination and rectal examination. The patient is prescribed a general blood and urine test, blood biochemistry . After this, they begin instrumental research methods, namely: colonoscopy, sigmoidoscopy and irrigoscopy . They allow you to determine the location of the fistula.
To clarify its location and structure of formation, probing is required, sometimes together with a dye test or fistulography. They allow you to determine the nature of the fistula tract, the presence of pockets and the amount of pus.
If necessary, female patients are prescribed a gynecological examination; all patients can undergo an ultrasound of the abdominal and pelvic organs . Sometimes an ultrasound examination of the rectum and sphincterometry - a method to determine the full functioning of the anus.
Diagnostics
The doctor examines the area around the affected bone to look for swelling, redness, and tenderness of the tissue. A blunt probe is used to examine fistulas.
Blood tests reveal signs of inflammation - an increase in ESR and the number of white blood cells. Blood and fistula discharge are subjected to microbiological examination to recognize the type of microorganism and determine antibacterial agents that effectively destroy it.
The main diagnostic procedures for osteomyelitis are imaging tests.
The area around the affected bone is swollen, red and tender.
X-ray of bones is used to identify necrotic areas of bone - sequestra. Fistulography - the introduction of a radiopaque substance into the fistula tract - is used to study the internal structure of the fistula. In the early stages of the disease, X-ray examination provides little information.
A CT scan is a series of x-rays taken from different positions. When analyzed, a detailed three-dimensional picture of the affected bone is formed.
Magnetic resonance imaging is a safe research method that allows you to recreate in detail the image of not only the bone, but also the soft tissue surrounding it.
A bone biopsy is performed to confirm the diagnosis. It can be performed in the operating room under general anesthesia. In this case, the surgeon cuts the tissue and takes a piece of the inflamed material. A microbiological examination is then carried out to identify the causative agent.
In some cases, a biopsy is taken under local anesthesia using a long, strong needle passed to the site of inflammation under X-ray guidance.
Treatment of rectal fistulas
Treatment without surgery cannot lead to a complete recovery, so doctors always resort to surgical removal. Surgical intervention is carried out in the acute period, since when the process subsides it is impossible to accurately determine the location and structure of the fistulas.
If the operation is performed under general anesthesia, the doctor excises the fistula completely, while capturing the surrounding tissue, the edges of the wound are stitched together, and the area is washed with antiseptics. Healing occurs within 45 days; in addition, patients take broad-spectrum antibiotics and analgesics. Physiotherapy is also prescribed - ultraviolet irradiation, electrophoresis , which accelerate tissue healing, stimulate blood flow and metabolism in the surgical area.
After surgery, it is important to follow a diet, you must follow all recommendations on personal hygiene, physical activity should be limited and increase gradually. Sitz baths with herbs are recommended to reduce pain and improve healing.
With this type of intervention there is a risk of relapse and postoperative complications. If you have complaints of severe pain in the perineum, the appearance of pathological discharge, difficulty urinating and defecating, or an increase in body temperature, you must immediately inform your doctor. More often in such situations, repeated surgical treatment cannot be avoided.
Minimally invasive methods are becoming increasingly common. As for fistulas, laser treatment, electrocoagulation and filling . These operations are performed under local anesthesia, are characterized by a minimal risk of complications, they are bloodless and quick. The recovery period after surgery is also significantly reduced, and the risk of relapse is also reduced to a minimum.
Laser treatment involves cauterizing the fistula using a special tube with an emitter. The edges of the wound are sealed with special glue, and several sutures of threads made of absorbable material are also applied.
Rectal fistula in patients is treated using electrocoagulation according to a similar scheme, only tissue cauterization is carried out with a thermal knife.
A good result is shown by filling with a so-called collagen plug, which behaves like a body graft and stimulates epithelization of the affected area. The patient's rectal fistula itself is sutured in a circle, fixed and excised. The resulting area is filled with cork and fixed. The technique is also bloodless, with a minimum of complications, but expensive.
The principles of treatment of rectal fistulas in children are the same as in adult patients. Sometimes doctors recommend refraining from operations if we are talking about a patient under 1 year old. If this does not affect the general condition of the little patient (this often happens), then the intervention is carried out a little later. But in emergency situations, there is no delay in operations.
Important! Treatment with folk remedies for this disease is ineffective and can lead to a worsening of the patient’s condition, especially if these are children. Therefore, it is important to consult a doctor as early as possible for timely and complete treatment.
Fistula on the gum
A fistula on the gum is formed as a consequence of the development of another disease associated with infection of the tooth or gum.
It is believed that there are three main causes of dental fistula:
1. Advanced caries. If caries is not treated, pulpitis may occur, and as a consequence, an inflammatory process in the pulp of a carious tooth. 2. Tooth perforation. When installing a post or performing root canal treatment, inflammation and complications are not uncommon. 3. Poorly sealed tooth canals. If the canal is not completely cleaned and carefully sealed, there is the possibility of a remaining infection developing, which often leads to the appearance of a fistula.
The appearance of a fistula on the gum becomes noticeable when its entrance is clearly formed. Once the bacteria multiply, pus will begin to ooze from the outer edge of the fistula. Sometimes, as the disease develops, the body temperature may rise. For some, the growth of the fistula is accompanied by pain.
To diagnose a fistula, it is recommended to take an x-ray. Only the image will show the size, depth of location, degree of neglect and inflammation of the dental fistula. After diagnosis, the doctor will be able to find out the cause of the appearance and, accordingly, will be able to prescribe the necessary treatment. Of course, treatment will begin directly with saving the tooth. Treatment of infected canals and cleansing with special solutions is the main stage of the process of treating a fistula on the gum.
If the inflammatory process has been started and the fistula canal has touched the periosteum, surgical intervention cannot be avoided. A large granuloma is removed with radical surgery, but almost always the doctor tries to save the patient’s tooth. In such cases, the treatment process will be long and gradual. After the operation, rehabilitation will follow, requiring repeated visits to the dentist. Being under the constant supervision of a specialist, you will be able to finally get rid of the problem that has arisen, so try to seek help in a timely manner.
In addition to filling the cavity of a previously affected tooth, there will be a need for a comprehensive fight against infection, so the doctor may prescribe antibiotics that reduce the intensity of inflammation and other drugs.
As additional methods for treating gum fistulas, laser tissue treatment is used, and ultrasound is also used.
The ultimate goal of all manipulations is the complete restoration of gum and tooth tissue, removal of the source of infection and the consequences of bacterial growth.
A fistula on the gum is formed as a consequence of the development of another disease associated with infection of the tooth or gum
Prevention of such a disease does not include any special procedures or actions. It is enough to regularly brush your teeth and rinse your mouth after each meal. Professional cleaning of teeth from plaque and tartar is also an element of hygiene, so it is necessary to periodically contact your dentist for such a procedure and a thorough examination of your teeth. Sometimes some problems are not visible and do not have pronounced symptoms, while the doctor will immediately see deviations from the norm.
A fistula on the gums of a child requires a different approach. As in adults, it appears as a result of advanced dental disease. If the fistula is ignored and a doctor is not consulted, the infection will spread and affect healthy tissue. It is possible to avoid destruction of the tooth root, gums and the tooth itself only with timely treatment. A peculiarity of the treatment of dental fistula in children is the mandatory extraction of the tooth. Due to the high probability of infection of a permanent tooth (which is located above the temporary, milk tooth), dentists try not to leave a damaged tooth to children.
Even cleaning the canal and high-quality filling does not provide a 100% guarantee of eradicating the infection, so it is preferable to simply remove the temporary baby tooth.
Treatment of a fistula with traditional methods involves only external healing, while complete cleansing of infection using rinses is impossible.
Prevention of rectal fistula
Rectal fistula in patients can be prevented with timely treatment of diseases not only of the organ itself, but also of all parts of the digestive tract. Other preventive measures:
- compliance with personal hygiene rules;
- cessation of smoking and drinking alcohol (recommendation for adult patients);
- it is important to prevent constipation;
- regular physical activity.
To prevent disease in adults and children, it is important to rationalize their diet. You should avoid fatty, fried foods, spices, sweets, and herbs. The menu should include lean meats and fish, dairy products, vegetables and fruits. It is recommended to drink at least 1.5 liters of clean water per day.
Prevention
Rectal fistulas occur as a consequence of chronic untreated paraproctitis, so it is extremely important to fully cure all gastrointestinal pathologies. A fistula with paraproctitis occurs gradually, so patients have a time reserve to prevent the development of this pathology.
It is important to monitor the state of the immune system, strengthen it through lifestyle correction, and introduce the principles of proper and healthy nutrition. If you suspect systemic diseases, you must immediately seek professional medical help and not self-medicate.
Rectal fistula is a disease that causes a lot of suffering to the patient and requires mandatory examination and surgical treatment. If assistance is not provided on time or self-medication, a significant deterioration in the patient’s condition is possible – even to the occurrence of severe complications.
Forecast for life
In most cases, rectal fistulas can be successfully treated. It is important to see a doctor in a timely manner and follow all the specialist’s recommendations. The prognosis for life is also positive. The exception is complicated cases of the disease in which there is a threat to the patient’s life. We are talking about sepsis and malignant degeneration.
We can summarize that it is necessary to have an idea of the signs of the disease and to know why rectal fistula is dangerous, and what methods of treatment and prevention are available today. This will help to quickly get rid of the pathology without any harm to the body, while maintaining the full functioning of the rectum.
Folk remedies for bone osteomyelitis
After treating osteomyelitis in a hospital and discharging the patient home, you can use some folk recipes to prevent the transition to a chronic form or the development of an exacerbation:
- make a decoction of oat grass (in extreme cases, oat bran will do) and make compresses from it on the sore limb;
- make an alcohol tincture of lilac: fill a full three-liter jar of flowers or buds with vodka and leave in a dark place for a week, use for compresses;
- take 3 kg of walnuts, remove the partitions from them and fill these partitions with vodka, leave in a dark place for 2 weeks; take a tablespoon three times a day for 20 days;
- lubricate the affected area with aloe juice or make a compress from crushed leaves;
- grate a large onion, mix with 100 g of laundry soap; Apply the mixture to the skin near the fistula at night.
Causes of intestinal fistulas
Intestinal fistula occurs due to an inflammatory process complicated by an abscess. Inflammation tends to involve surrounding structures, creating adhesions between tissues. The abscess sometimes breaks down, creating a tubular path that passes through the various structures involved in the inflammation.
The fistula tends to become chronic when:
- persistence of the infection, which continues to produce pus and inflammatory materials;
- the appearance of other biological substances in the fistula organ: saliva, urine or feces.
In some cases, the fistula is replaced by fibrous scar tissue, which tends to close it completely or sometimes partially. This explains why fistulas are divided into complete and incomplete, and in the latter case, remaining open on one side or the other, they are called internal or external.
Important! In some cases, the process that led to the formation of the fistula may recur. The pus present in the new abscess may follow a new path, creating a new fistula. This is the mechanism that explains why fistulas can be unique or multiple, simple or branched.
After a difficult bowel movement, the vesicointestinal fistula ruptures and releases blood and pus mixed with bacteria. In this case, the patient is treated with simple oral antibiotics and frequent internal irrigation without the need for drainage surgery.
Fistulas can be congenital, artificially created and pathological:
- Artificially created fistulas are created during surgical interventions. For example, an external gastric fistula serves to provide artificial nutrition to the patient.
- Congenital fistulas occur at birth due to prenatal developmental disorders. Such fistulas usually close and dissolve before birth. An example is a urachal fistula, which preserves the connection between the bladder and the umbilicus.
- Pathological fistulas are caused by inflammation; the body may release pus through fistulas from the affected tissue to the outside. Often these fistulas are formed due to inflammation of the teeth or intestinal Crohn's disease, in which a fistula occurs in the anal area.
Fistulas are the result of various pathologies
Rectal fistulas are found in both sexes, regardless of age, but it is generally accepted that various forms of this pathology are more common in men. Many people are sure: since the fistula can be removed from the body on its own (along with feces), the pathology does not pose a danger. This is an erroneous opinion, because when the contents of the abscess leave the body with feces, the inflammation in the anal sinuses does not disappear anywhere, and the infection continues. The fistula can take on recurrent forms. To treat a pathology, doctors first need to establish its causes and a list of factors provoking the disease.
There are groups of people who are most predisposed to the development of fistulas. Failures in the immune system, HIV, AIDS often become causes of pathology. It can be caused by cancer and chlamydia. The list of causes of the disease includes the following ailments:
- tuberculosis of the rectal canal;
- complications after gynecological operations;
- diverticular bowel disease;
- hernias;
- ulcerative colitis:
- syphilis;
- enteritis.
The disease often occurs in women who have suffered birth injuries. The causes of pathology include various surgical interventions in the perineum, genitals, and areas of the gastrointestinal tract. In patients who have undergone rectal resection, fistulas form quite often. Among the factors that provoke the appearance of fistulas, the most common are hernial inflammatory protrusions of the walls of the rectum. As for a disease that has a tuberculous etiology, tuberculosis of the rectum or rectum most often develops as a secondary disease. First, the disease affects the lungs of a person, and then infection of the internal organs continues in a descending manner.
Fistulas should never be taken lightly.
Most cancers of internal organs are asymptomatic at first. Therefore, if a person is found to have fistulas, he certainly needs to be examined for the presence of cancer. This rule also applies to recurrent fistulas, which are considered the primary signs of the presence of malignant neoplasms. It is important to know: fistulas accompany rapidly progressing malignant intestinal tumors.
Reasons for formation
- acute or chronic paraproctitis;
- consequence of rectal surgery;
- tuberculosis of the digestive system;
- Crohn's disease;
- diverticular disease of the intestine and inflammation of pathological processes (diverticulitis);
- specific infections (syphilis, chlamydia, HIV infection and AIDS, actinomycosis);
- advanced course of hemorrhoids;
- birth injuries in women (rupture of the birth canal, breech birth, use of obstetric aid, prolonged labor);
- terminal colorectal cancer;
- in rare cases - fistulas of iatrogenic origin (violation of the technique of gynecological manipulations).
Excision of a fistula without a scalpel
Most proctological surgeons consider surgical treatment to be the most effective method of treating various fistulas, since during the operation the doctor can remove all damaged tissue, which significantly reduces the risk of relapse. Excision of fistulas using a scalpel is an invasive, highly traumatic operation that requires a long recovery period, so many patients are looking for ways to treat fistulas without surgery. They will be discussed below.
Types of rectal fistula
Laser treatment without surgery
This is one of the safest, most effective and least traumatic methods of treating fistula tracts, which has several advantages. Laser treatment, if indicated, can be carried out even in children and adolescents, although some doctors do not recommend using this technique in children under 10 years of age. The impact of laser beams does not cause discomfort or pain, and after the procedure there is no need for a rehabilitation period
After excision of the fistula with a laser, there are no scars or scars left on the skin, which is important if the operation is performed in the anorectal area.
Treatment of fistula tracts with laser
Despite the large number of advantages, laser treatment also has significant disadvantages, including:
- high cost (in different clinics the cost can vary from 20,000 to 45,000 rubles);
- a fairly high probability of relapses and complications (about 11.2%);
- side effects in the form of anal itching and burning at the site of excision of the fistula;
- impossibility of use for purulent fistulas.
Note! Laser excision of fistula tracts is practiced in all private clinics in large cities, so there are usually no problems finding a laser proctologist surgeon. .
Laser excision of fistula
Radio wave therapy
A more modern way to remove rectal fistulas is radio wave therapy. The method is suitable for the treatment of all types of fistulas, and its main advantage is the absence of the need to go to the hospital. The patient can go home 10-20 minutes after the procedure, since it does not require general anesthesia: the doctor performs all actions under local anesthesia (traditionally Lidocaine or Ultracaine is used).
"Lidocaine"
Complete healing and tissue restoration after radio wave excision of a fistula occurs within 48 hours, so if the fistula was removed on Friday, the patient can go to work on Monday (the standard recovery period after surgery is at least 14 days). To determine the most suitable treatment method for himself, the patient can use the comparative characteristics given in the table below.
Table. Comparative characteristics of various methods of treatment of rectal fistulas.
| Need for hospitalization | Usually not required (in some cases, the doctor may recommend observation for 1-2 days). | Not required. The patient can leave the clinic 20 minutes after the procedure. | The patient must be hospitalized in a hospital 2-3 days before the scheduled operation. After excision, the patient remains in the hospital for about 2-3 weeks. |
| Use of general anesthesia | Not required. | Not required. | Depending on the shape of the fistula and the extent of tissue damage, general anesthesia may be required. |
| Scars and scars after surgery | The probability is less than 5%. | The probability is less than 1%. | The probability is more than 92%. |
| Postoperative pain | None. | None. | They may bother you for several months, especially if the patient has a tendency to have stool disorders. |
| Healing and recovery period | From 2 to 5 days. | 48 hours. | Three weeks. |
| Probability of relapses and complications | About 11.2%. | Practically absent. | Complications may occur. |
| Price | 20-45 thousand rubles. | 14,000 rubles. | It is carried out free of charge under the compulsory medical insurance policy. |
Surgery
The main treatment method for rectal fistulas is surgery. Conservative treatment can be used, but only as a concomitant therapy preparing the patient for surgery.
It is strictly forbidden to use folk remedies instead of consulting a doctor.
Purulent inflammation, which necessarily occurs when a fistula forms, can spread to surrounding tissues and damage the organs of the abdominal cavity and pelvis. Therefore, the disease requires mandatory medical intervention, which must be carried out as soon as possible.
Intervention procedure
The volume and radicality of the operation depends on the extent of the pathological process. Typically the procedure includes the following steps:
- Providing access to the fistula tract.
- Excision of pathological tissues.
- Inspection of surrounding tissues for purulent leaks and pockets.
- Excision of found cavities.
- Installation of drainage.
- Plastic surgery of the internal opening of the fistula using a mucomuscular flap.
- Suturing the external hole.
The operation is performed after mandatory hospitalization of the patient. For pain relief, in most cases, general anesthesia is used; local anesthesia is ineffective for this intervention.
Postoperative rehabilitation
Proper management of the rehabilitation period reduces the risk of developing postoperative complications. A bandage is applied to the patient's postoperative wound, and a special hemostatic sponge and a gas outlet tube are inserted through the anus into the rectum. A day after the intervention, a dressing is made and the tube is removed. During dressing, the postoperative wound must be inspected.
In complex fistulas with a large number of purulent pockets, skin suturing is not performed immediately after surgery. It is necessary to re-inspect the wound cavity a week after the intervention. If no new pathological changes are detected, then the wound is sutured. The procedure is also performed under general anesthesia.
In the first few weeks after the operation, the patient is in the hospital department where he undergoes dressings. Manipulation of the wound can cause severe pain, so local analgesics - gels or ointments - are used during the procedure. During the rehabilitation period, the patient is prescribed special sitz baths with herbal decoctions or other medications. Such procedures help relieve pain and speed up wound healing.
We recommend reading:
Intestinal inflammation: signs of pathology, use of diet and drugs for treatment
Diet after surgery
The patient should not take anything orally for several hours after the operation, after which he is allowed to drink. In the first 2-3 days, you can only drink water or kefir, as well as a little boiled rice. A drinking diet is necessary so that the patient cannot form formed stools. Feces can infect the postoperative wound, which will lead to relapse of the disease. Therefore, the consumption of solid foods during this period is limited.
In the future, the patient should switch to proper nutrition:
- It is recommended to eat food 5-6 times a day in small quantities;
- It is necessary to exclude from the diet everything too fatty and fried;
- do not eat hot or cold foods, adhere to normal temperature conditions;
- carbonated drinks, spicy and smoked foods are prohibited;
- It is recommended to include in the diet a large amount of vegetables and fruits that are rich in fiber;
- you need to consume more fermented milk products, which helps to normalize stool character and restore normal intestinal motility.
Only surgery can help
According to the location of the fistula entrance, the pathology is divided into:
- intrasphincteric;
- extrasphincteric;
- transsphincteric.
The first type of disease is distinguished by the direct form of fistulas, the absence of scars and the presence of an external opening of the fistula located next to the anus. Extrasphincteric fistulas, on the contrary, have a tortuous shape and greater extent. With this form of pathology, purulent leaks form much more actively, as do scars around the fistula canal. Extrasphincteric pathology is usually classified into 4 stages. The first is characterized by the absence of purulent streaks and scars. The last stage is indicated by multiple scars, a wide opening of the fistula, the presence of infiltrates, ulcers.
The transsphincteric fistula is located at different depths and goes through the external sphincter of the rectum. This form of pathology is also characterized by purulent leaks and the formation of scars that cover the sphincter, causing its deformation and dysfunction. When choosing a method of combating a disease, it is necessary to take into account the form in which the pathology develops, the severity of ulcers and scar formations. Today, the only effective way to treat fistulas is surgery. In modern medicine, there are various methods of surgical interventions, but treatment with any of the surgical methods certainly includes excision of the rectal fistula. If measures against the disease are not taken in a timely manner, it can develop into a malignant form. Therefore, medical experts advise patients not to delay surgical intervention unless there are contraindications for its use.
Before surgery, the patient undergoes antibiotic therapy and may be prescribed physiotherapeutic procedures. During remission, surgery is not performed. In the postoperative period, conservative treatment is carried out. Patients are prescribed painkillers and anti-inflammatory drugs. Warm baths with antiseptic solutions have proven themselves to be one of the effective methods used after surgery. Wound healing lasts on average a month. The duration largely depends on the rate of tissue regeneration in the patient. After the operation, physical activity is prohibited to speed up the healing of the wound and restoration of the body.
Differential diagnosis
Differential diagnosis is one of the stages of making a final clinical diagnosis. It is carried out by comparing data from laboratory and instrumental methods of studying diseases that are similar in clinical picture and excluding those that are inappropriate according to all criteria.
Diseases for which differential diagnosis of paraproctitis with fistula is carried out:
- rectal tumor - determined using graphic research methods (CT, MRI, ultrasound). Malignant tumors are characterized by the release of serous-bloody fluid from the lumen of the fistula;
- Teratoma of perirectal tissue is a benign tumor that also causes fistulas. Distinctive symptoms will be: absence of pain in the anus, presence of a dense formation upon palpation, increasing defecation disturbance, absence of intoxication syndrome. Diagnosed on the basis of ultrasound, X-ray examination, puncture biopsy (histological examination);
- pouch of Douglas abscess is a focal purulent inflammation (connective tissue capsule with pus), which is located in the recess between the uterus and rectum in women, and the rectum and bladder in men. An abscess is most often formed against the background of current or previous appendicitis, adnexitis, intestinal perforation, etc.
Diagnosed based on X-ray data, puncture of the abscess cavity and obtaining purulent contents. It is treated promptly.
Course of the postoperative period
The rehabilitation period after removal of a rectal fistula takes from 3 to 6 weeks.
At this time, all means are aimed at eliminating pain, normalizing stool, accelerating the healing of postoperative wounds and preventing complications. For this purpose, patients are prescribed a special liquid diet, painkillers and healing agents, antibacterial and, if necessary, laxatives.
24 hours after surgery, the gas outlet tube and hemostatic sponge are removed from the rectal canal. The manipulation is carried out under local anesthesia, as this procedure is quite painful.
Dressings are carried out once a day for 2-3 weeks. The postoperative wound is washed with an antiseptic (hydrogen peroxide, Chlorhexidine), a healing and/or antibacterial ointment is applied, and then a sterile gauze bandage is applied.
In the case of an extensive operation for complex fistula tracts, after about 5-7 days, dressing is performed with a deep revision of the wound and tightening of the ligatures. The procedure is also performed under anesthesia.
The patient's stay in the hospital takes from 7 to 10 days.
The patient's stay in the hospital takes from 7 to 10 days. After discharge from the department, you will need to come for an examination by the surgeon who performed the operation. The doctor will set a date for the re-examination.
In the postoperative period, you need to carefully monitor your well-being and if you experience any unpleasant sensations in the problem area, you should contact your attending proctologist.
The following symptoms may indicate the development of complications:
- sudden increase in body temperature;
- pain in the lower abdomen and anus;
- flatulence;
- leakage of feces or pus from the rectal canal;
- bleeding from the anus;
- pain during bowel movements;
- pain during urination;
- an admixture of blood or pus in the stool.
Treatment methods
Traditional methods of treating intestinal fistulas are often tedious and accompanied by relapses. In particular, intestinal fistulas located higher in the intestinal region can only be operated on in the usual way with great effort.
The goal of various procedures is to cut out the fistula and reduce inflammation by suturing the musculature at the opening of the internal fistula in the rectum. The internal suture is then covered with a tissue strip from the intestinal mucosa. The external wound usually remains open.
Anal fistula fissure is the most common treatment: superficial fistulas can achieve almost 100% treatment success. The incidence of continence disorders is described in the literature as relatively low. However, this poses serious consequences. In either case, the incidence of urinary incontinence increases with the size of the torn sphincter muscle.
Often severe sphincter damage followed by reconstruction must be undertaken. Laser treatment for intestinal fistulas, however, is usually very gentle. This is especially suitable for patients who have not been cured by previous attempts at therapy. During treatment, a laser is inserted through a cannula into the fistula area. To do this, you only need to install a few small punctures. Then the intestinal fistula is reduced with a laser: as a result of its thermal effect, the walls of the inflamed cavity are compressed.
Important! During laser treatment, healthy tissue is not damaged. Subsequently, the channel of the emptied fistula is destroyed by the immune system. The entire procedure is carried out under ultrasound control.
Some time after the procedure, the patient can stand up again. This is usually followed by a 4 to 6 day hospital stay. So the healing process can be clearly observed. Ancillary measures such as sitz baths can help with treatment. Because the procedure is particularly gentle, no special dietary measures are usually required. After discharge, the family doctor can continue treatment.
Today, removal of a fistula, which causes varying degrees of complexity related to the location and organs involved, is called a fistulectomy. Sometimes fistulotomy is used. In some circumstances, surgery may eventually be required to create a fistula. This is a case of hemodialysis in which an arteriovenous fistula is created, which provides vascular access.
Surgery is only recommended in some cases, given that the success rate of the operation is 60% for the first operation (the fistula can recur), but is close to 100% if more operations are performed.
Sometimes, for example, with rectovaginal (intestinal-vaginal) fistulas (typically: release of air and mucus, possibly also from stool into the vagina), it may be necessary to temporarily create an artificial intestinal outlet (stoma).
However, fistulas in the rectal area pose a particular risk: they can lead to involuntary bowel movements. However, up to a third of all chronic intestinal fistulas already cause damage to the sphincter muscle before surgery.
Therefore, for chronic fistulae and those who have already had sphincter surgery, anal manometry (pressure measurement) should be performed before any surgery to identify previous damage to the sphincter muscle.
In addition to fecal incontinence, the fistula procedure can also cause scarring to form in the anal area, causing it to narrow. However, the most common complication of such an operation is relapse. This means that the fistula is returning. Years of existing fistulas can also be a starting point for the development of anal cancer.
Prevention and prognosis
To prevent people from having to undergo an operation to excise a fistula, they only need to follow a few simple rules:
- undergo full treatment and recovery after acute paraproctitis;
- avoid trauma to the perineum and rectum;
- completely give up bad habits;
- eat rationally and balanced;
- lead a moderately active lifestyle;
- identify and eliminate diseases that cause pathology at an early stage;
- regularly undergo a complete preventive examination in the clinic.
The prognosis is often favorable - even in situations where patients have undergone surgery to remove the fistula. The likelihood of complications is low, but relapses are common.