Hernia defects of the groin area are a disease in which the internal organs of the abdominal cavity, while maintaining the integrity of the peritoneum, push through the inguinal canal and the anterior abdominal wall of the groin on the left or right. In women, the hernial protrusion has a spherical shape ranging in size from 1 cm to 10 cm or more.
In representatives of the weaker sex, this disease is rare - about 8-10% of all cases of hernia defects in the groin area. The reason is the different structure of the canalis inguinalis (inguinal canal) in women and men.
Among women:
- The inguinal space is smaller (hernia gate)
- The inguinal canal is narrower and has the shape of a narrow slit.
- Inside the inguinal canal in women is the round ligament of the uterus, in men the spermatic cord
- The structure of the aponeurosis of the external oblique abdominal muscle in the groin area has a more dense structure.
Among women
INGUINAL REGION - part of the anterior abdominal wall, bounded above by a horizontal line connecting the superior anterior iliac part with the outer edge of the rectus abdominis muscle, below - by the inguinal ligament and from the inside - by the outer edge of the rectus abdominis muscle.
Inflammatory diseases of the uterine appendages (adnexitis, salpingoophoritis, parametritis). These diseases cause acute pain in the groin, increased body temperature, deterioration of general condition, and painful sensations when palpating the lower abdomen.
In the female body, the groin is located in the lower abdominal region. Large vessels and the round ligament of the uterus pass through the inguinal canal.
Inguinal hernia in women: what are the causes?
Not all women are at risk of developing an inguinal hernia, but only those who have a combination of factors that provide favorable conditions for hernia disease. These factors include the following:
- weak constitution;
- physical inactivity;
- genetic predisposition to hernia disease;
- congenital pathology of the muscular and ligamentous apparatus of the groin area.
Also, the presence of the above factors in a woman is not a sign that she will definitely develop an inguinal hernia, since this still requires the presence of a provoking factor.
Let's consider the provoking factors of an inguinal hernia.
1. Increased pressure inside the abdominal cavity, which can be caused by various reasons, namely:
- frequent and prolonged screaming or crying, especially in infancy;
- chronic cough;
- frequent diarrhea, constipation and/or vomiting;
- disturbance of the outflow of urine from the bladder;
- difficult childbirth;
- features of the profession (playing a wind instrument, lifting heavy loads, blowing glass, etc.).
2. Weakness of the muscular system of the anterior abdominal wall, the appearance of which may be due to such reasons as:
- sedentary lifestyle;
- physical inactivity;
- excess weight;
- “sedentary” profession (cashier, programmer, clerk, needleworker and others);
- pregnancy;
- difficult childbirth;
- abdominal injuries;
- laparotomy.
The highest risk of developing an inguinal hernia is in girls between one and two years of age and in women over 40 years of age. Moreover, in infancy, the main role in hernia formation is played by congenital malformations of the muscle fibers and ligaments of the anterior abdominal wall, and in older women - a combination of provoking factors (excess weight, chronic constipation, sedentary lifestyle, injuries, etc.).
Etiology
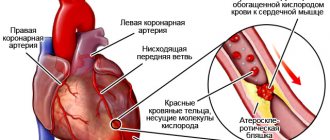
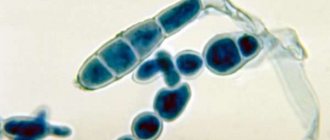
Athlete's foot is a dermatomycosis caused by the fungus Epidermophyton floccosum. This is an anthropophile that grows and develops only on the human body. It is located in the scales of the epidermis and nail plates. Under a microscope, fungal spores and well-branched mycelium are determined in skin scrapings. After isolating a pure culture, the mycelium becomes yellow and the spores look larger.
Fungi are resistant to environmental factors. They grow and develop quickly at high humidity and temperature.
In medical, preventive and public institutions, neglect of sanitary norms and rules can provoke an entire epidemic of mycosis.
Factors contributing to infection:
- Hyperhidrosis,
- Stress,
- Skin microtraumas
- Tight clothes,
- Obesity,
- Failure to comply with sanitary rules and regulations,
- Decreased immunity
- Hormonal disbalance,
- Metabolic disorders.
Where are the inguinal lymph nodes located?
Inguinal lymph nodes are localized in the perineum (in the folds between the legs and pelvic region). They can also be felt in the femoral triangle, inside and outside the thighs. A diagram will help you understand where these formations are located.
Layout of inguinal lymph nodes and lymphatic vessels
The location of the inguinal lymph nodes in humans suggests their division into 3 groups:
- in the area of the thighs, lower abdomen and buttocks there is the upper level of glands;
- near the anus, external genital organs - the average level of immune links;
- close to each other, lower level formations are located on the leg.
Lymph nodes located between the groin and thigh can be palpated. In this case, round formations of soft consistency are determined, easily moving under the skin. If they are no larger than a pea, then there is no need to talk about pathology.
The links of immunity in the groin area are deep and superficial. The latter lie in the thickness of the connective tissue of the abdominal wall. The deep glands are located near the femoral vein. They are responsible for filtering lymph coming from the external genitalia and lower extremities.
Treatment
In P. o. The inguinal triangle is isolated, formed by a horizontal line running from the border of the outer and middle third of the inguinal ligament to the outer edge of the rectus abdominis muscle (top), the inguinal ligament (bottom) and the outer edge of the rectus abdominis muscle (inside). In the inguinal triangle, between the lower edges of the internal oblique and transverse abdominal muscles and the groove of the inguinal ligament, there is a muscle defect called the inguinal gap (Fig. 1).
In the lower inner corner of the inguinal triangle there is the inguinal canal (see), which contains the spermatic cord in men and the round ligament of the uterus in women. Skin in P. o. thin, mobile, it contains sweat and sebaceous glands, as well as hair follicles. Subcutaneous tissue is two-layered, permeated with connective tissue fibers.
At the site of the inguinal ligament, where these fibers are connected to the fascia lata of the thigh, an inguinal fold is formed. The superficial fascia consists of two layers, of which the deep one is more dense and is called the iliopectineal (Thomsonian) fascia. The subcutaneous tissue contains the superficial epigastric artery (a. epigastrica superficialis), the superficial artery circumflexing the ilium (a.
circumflexa ilium superficialis), and the external genital artery (a. pudenda ext.), accompanied by veins of the same name (Fig. 2). Lymph vessels in the subcutaneous tissue form looped plexuses and flow into the superficial inguinal nodes. Skin P. o. innervated by the branches of the 12th intercostal nerve, iliohypogastric (n. iliohypogastricus), ilioinguinal (n.
ilio inguinalis) and femoral-genital (n. geni-tofemoralis) nerves. The fascia proper covers the external oblique muscle of the abdomen and, together with the deep layer of the superficial fascia, is attached to the inguinal ligament. The lateral muscles of the abdominal wall are the external and internal oblique abdominal muscles (mm. obliqui ext. et int. abdominis) and the transverse abdominal muscle (m.
transversus abdominis)—are located sequentially in three layers (see Abdominal wall). The lower edge of the aponeurosis m. obliqui ext. abdominis participates in the formation of the inguinal ligament and is divided into 2 legs: medial (crus med.) and lateral (crus lat.). In 10% of cases there is a bent ligament (lig. reflexum). The medial and lateral legs, attaching to the pubic tubercle and the upper edge of the symphysis, form a superficial inguinal ring, which is limited externally by arcuate fibers.
The inguinal (Pupart's) ligament is a complex formation in its structure; it involves not only the three lateral abdominal muscles that originate from it, but also the fascia of the abdominal wall and thigh. In the intermuscular spaces of the lateral abdominal muscles there are fascial sheets, loose tissue and branches of the 12th intercostal nerve, iliohypogastric and ilioinguinal nerves.
Muscle fibers are separated from the internal oblique and transverse (in 25% of cases) muscles, forming the muscle that lifts the testicle (m. cremaster). The transverse abdominal muscle in the inguinal region has an arcuate course of muscle fibers, forming an inguinal arch above the inguinal ligament. There are 2 shapes of the inguinal space: slit-oval and triangular.
At the inguinal ligament, the transverse muscle covers the deep ring of the inguinal canal, then passes into the tendon aponeurosis, spreading over the spermatic cord, and ends at the pubic tubercle, intertwining with the lacunar ligament and forming the inguinal falx (falx inguinalis). Sometimes there is a joint tendon of the internal oblique and transverse abdominal muscles.
On the lateral side, the inguinal space is strengthened by the interfoveal ligament (lig. interfoveola). Deep layers of P. o.: transverse fascia, preperitoneal tissue and peritoneum. The transverse fascia (fascia transversalis) at the inguinal ligament has a denser structure, forming a strip 1 cm wide (iliopubic cord). The outer part of the transverse fascia is fused with the inguinal ligament, and the inner part with the pubic (Cooper's) ligament.
Preperitoneal tissue is a layer of loose connective tissue. The parietal peritoneum forms in P. o. a series of folds and pits (see Abdominal wall). The spermatic cord is accompanied by: cremasteric arteries and veins (vasa cremasterica), testicular artery and veins (vasa testicularia), artery and veins of the vas deferens (a. et v.
What does your nose shape say about your personality? Many experts believe that you can tell a lot about a person's personality by looking at their nose. Therefore, when you first meet, pay attention to the stranger’s nose.
Why do you need a tiny pocket on jeans? Everyone knows that there is a tiny pocket on jeans, but few have thought about why it might be needed. Interestingly, it was originally a place for storage.
How to look younger: the best haircuts for those over 30, 40, 50, 60 Girls in their 20s don’t worry about the shape and length of their hair. It seems that youth is created for experiments with appearance and daring curls. However, already last.
Unforgivable Movie Mistakes You Probably Never Noticed There are probably very few people who don't enjoy watching movies. However, even in the best cinema there are mistakes that the viewer can notice.
20 photos of cats taken at the right moment Cats are amazing creatures, and perhaps everyone knows this. They are also incredibly photogenic and always know how to be in the right place at the right time.
7 Body Parts You Shouldn't Touch with Your Hands Think of your body as a temple: you can use it, but there are some sacred places that you shouldn't touch with your hands. Research showing.
1. Pathologies of the genitourinary system:
- kidneys (urolithiasis);
- gynecological diseases (adnexitis, endometriosis, endometritis, painful menstruation, tumors of the female genital organs);
- acute cystitis;
- diseases of the male genital organs (orchitis, epididymitis, vesiculitis, spermatic cord cyst, prostatitis, testicular torsion, varicocele).
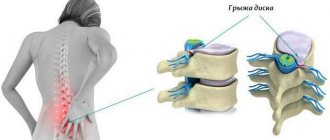
Diseases of the musculoskeletal system:
- radiculitis of the sacrolumbar region;
- compression of the nerve root between the vertebrae (5th lumbar and 1st sacral);
- compression of the 4th lumbar nerve root.
2. Hip joint:
- inguinal hernia;
- abdominal proptosis (deformation of the anterior abdominal wall due to muscle weakness).
Diseases of the nervous system: pinched pudendal nerve.
1. Inguinal lymphadenitis (inflammation of the lymph nodes).
2. Aneurysm (enlargement) of the femoral artery.
1. Trauma to the groin area.
2. Tumors of various localizations.
3. Genital (genital) herpes in men.
4. Psoas abscess (focus of suppuration in the tissue covering the iliopsoas muscle).
5. varicose node of the leg saphenous vein.
1. For inguinal hernia.
2. For renal colic.
3. For appendicitis.
- inflammatory diseases of the genitourinary organs (cystitis, urethritis, adnexitis, endometritis, orchitis, etc.);
- fungal diseases of the skin of the feet;
- benign or malignant tumors of the pelvic organs (in this case, the inguinal lymph nodes enlarge, remaining painless);
- syphilis (primary stage);
- sexually transmitted infections (AIDS, chlamydia, mycoplasmosis, genital herpes, ureaplasmosis, etc.).
Therefore, if you find an enlarged and painful lymph node (or group of nodes) in your groin, you need to pay close attention to this symptom and immediately consult a doctor.
Acute
- urolithiasis;
- acute cystitis;
- arthrosis of the hip joint;
- pinched pudendal nerve;
- inflammation of the inguinal lymph nodes.
In case of urolithiasis - examination by a therapist and urologist. Depending on the location and size of the stone, medical or surgical treatment is carried out.
The most common cause of groin pain in women is inflammatory diseases of the genital area. The woman's general condition worsens, her body temperature rises, and pain occurs if she touches her stomach.
One of the common pathologies is appendicitis, which manifests itself as severe pain in the right groin. First, throbbing pain occurs in the epigastric region and eventually descends below. The patient begins to feel even worse during movement and experiences pain when lying on his left side. Other symptoms of appendicitis are nausea, vomiting, and problems with bowel movements.
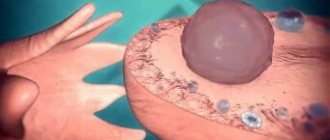
Cystic formations affecting the internal genital organs cause pain in the groin area. They are characterized by nagging painful sensations and when the cyst ruptures they become more acute: the patient’s general condition worsens, vomiting occurs, body temperature rises, and blood pressure drops.
Severe pain in the groin bothers a woman during an ectopic pregnancy. The pain is cramping in nature and intensifies over time.
A rupture of a femoral artery aneurysm is expressed by intense pain in the groin and causes bleeding.
Intestinal diseases cause pain in the groin. In addition, malignant tumors, intestinal obstruction, and diverticulitis contribute to pain. The main symptoms of these pathologies: bloated stomach, problems with stool.
A stone stuck in the ureter causes pain on one side of the groin area. The painful sensations are acute and sharp in nature and last for several minutes or throughout the day. The pain is localized in the lumbar region, and the irradiation point is the groin.
When the lymph nodes in the groin become inflamed, pain occurs near the affected area. The node becomes thicker and becomes larger.
In rare cases, pain occurs due to an inguinal hernia, since in the female body the inguinal gap is not as wide as in men, and the tissue is stronger.
Muscle pain in the groin is mainly observed in female athletes after heavy exertion or competition. Muscles suffer in those who play volleyball, tennis and basketball. The pain is nagging or aching, but with injury it becomes more acute.
Pain in the groin area during movement is caused by a chronic form of hip disease. The symptom appears on one side of the groin, may begin while walking and disappear over time, but reappear during a long walk.
Pain in the groin also occurs in pregnant women; it develops for the following reasons:
- weakening of cartilage due to hormones;
- the fetus puts pressure on the pelvic bones;
- stretching and weakening of the ligaments that attach the uterus to the walls of the pelvis;
- increased myometrial tone and threat of miscarriage;
- deficiency of calcium and magnesium.
- The initial stage is characterized by increased proliferation of the fungus in the epidermis and the appearance of pink spots with papules and vesicles on the skin.
- Clinical signs of the acute stage are weeping spots that grow, itch and are replaced by rings with scalloped edges.
- Chronic stage - lesions on the skin periodically lighten, and then become inflamed again under the influence of unfavorable factors.
- The advanced stage develops with a complicated course of the pathology. If left untreated, large blisters appear on the skin, which become infected when damaged. The blisters are opened, necrotic tissue is removed and the wound is treated.
Rice. 1. Boundaries of the groin area (ABE), inguinal triangle (CDE) and inguinal space (F).
Rice. 2. Superficial vessels, nerves to the lymph nodes of the inguinal region: 1— aponeurosis of the external oblique muscle of the abdomen; 2—superficial epigastric artery and vein; 3— superficial inguinal ring; 4—medial and 5—lateral legs of the aponeurosis; 6— spermatic cord; 7— ilioinguinal nerve; 8—external genital artery and vein; 9—great saphenous vein of the leg; 10—lateral cutaneous nerve of the thigh; 11—superficial inguinal lymph nodes; 12—superficial artery and vein, circumflexing the ilium; 13—inguinal ligament.
Rice. 3. Schematic representation of the groin area of a man (on the right - the internal oblique abdominal muscle with nerves located on it, on the left - the transverse abdominal muscle with vessels and nerves located on it): 1 - rectus abdominis muscle; 2, 4, 22, 23 - intercostal nerves; 3 - transverse abdominal muscle; 5 and 24 - external oblique abdominal muscle; 6 and 21—internal oblique abdominal muscle; 7 and 20 - iliohypogastric nerve; 8 and 19—ilioinguinal nerve; 9— deep artery, circumflex ilium; 10—transverse fascia and internal spermatic fascia; 11—vas deferens; 12—interfoveal ligament; 13— inguinal sickle; 14— pyramidal muscle; 15—medial leg of the aponeurosis (cut off); 16—curved ligament; 17—muscle that lifts the testicle; 18—genital branch of the femoral-genital nerve.
What complications can occur with an inguinal hernia?
With an inguinal hernia, various complications can occur, among which the most common are the following:
- inflammatory process;
- intestinal obstruction;
- pinched inguinal hernia.
Inflammation of the contents and/or walls of the hernial sac can manifest itself in the form of acute appendicitis, colitis, oophoritis, salpingitis, salpingoophoritis, etc. Like the inflammatory process of any localization, inflammation of the inguinal hernia is accompanied by symptoms of intoxication (fever, general weakness, fatigue ). It is also important to understand that inflammation contributes to the formation of adhesions, as a result of which the hernia cannot be reduced. A complication such as acute appendicitis requires surgical treatment.
Intestinal obstruction with a groove hernia occurs when part of the colon is located in the hernial sac. Fecal blockage threatens necrosis of a section of the intestine, which can also be treated promptly. Most often, intestinal obstruction appears in old age or in obese people.
A strangulated hernia is the most dangerous complication of hernia disease, since it develops almost at lightning speed. When strangulated, the contents of the hernial sac, that is, the organs and tissues of the abdominal cavity or pelvis, are subject to compression, which can lead to disruption of blood flow and innervation.
A pinched hernia is manifested by a certain symptom complex, namely:
- a previously reduced hernia suddenly stops being reduced;
- severe pain in the groin or entire abdomen, up to painful shock, especially when the uterus or its appendages are pinched;
- the hernia becomes tense and dense;
- nausea and vomiting;
- fever.
Symptoms
single spot of athlete's foot
With inguinal athlete's foot, pink or red-brown spots appear on the skin, having a round shape and a diameter of no more than one centimeter. The spots are located symmetrically, itch, peel and gradually grow. Along the periphery of the spot on hyperemic and edematous skin, multiple blisters, pustules, suppurations, crusts and small flaky inclusions appear.
As the inflammatory process subsides, the central part of the spot becomes clean, pale and slightly sunken. This gives foci of epidermophytosis a special appearance of rings and is a pathognomonic sign of pathology. Fungus in the groin in men itches and burns, and severe discomfort occurs when walking. The areas are painful to the touch. Vesicles and pustules can burst, forming erosions and ulcers. When a secondary bacterial infection occurs, severe complications develop.
Symptoms and clinical signs of inguinal hernia
Symptoms of inguinal hernia in women
The development of a direct (subcutaneous) hernia is an acquired pathology that develops in women over forty years of age. It is a consequence of various influences that provoke increased pressure on internal organs. As a result, they begin to fall out of the peritoneal cavity from the internal (medial) zone of the inguinal fossa, forming a protrusion in the area of tissue connections around the uterus and vaginal opening.
The pathological process develops quite slowly, but the characteristic signs are difficult to miss. One of the first symptoms of a hernia is pain in the groin area. Pain and discomfort in the lower abdomen increases when lying down. This type of inguinal hernia in women appears as a small tumor that may disappear if you lie on your back. With these first signs, the disease can be stopped quite easily with timely treatment.
Pain syndrome has its own characteristics. It can be intense and pronounced.
- If the disease develops in an acute form, symptoms may manifest as unexpectedly severe pain and a characteristic hernial protrusion.
- With the slow development of the pathological process, pain may not be observed at all or it will be mild. At the same time, the size of the hernial sac is completely small.
- With a chronic course or large size of the hernia, pain in the groin does not stop and can radiate to the abdomen, sacrum and lumbar area. Worse with coughing, laughing and defecation. Pathology may be accompanied by:
- constipation and problems with urination;
- discomfort in the form of burning, weakness and pain even when walking slowly;
- tachycardia;
- changes in the color of the skin in the groin;
- slight low-grade fever;
- frequent vomiting and nausea (if one of the gastrointestinal tracts is pinched).
The femoral type of hernia is the second most common type after the inguinal hernia.
It occurs due to stretching and muscle weakening of the internal opening of the femoral ring and intra-abdominal fascia. It develops as a result of prolonged exposure to strong intracavitary pressure on the muscles, or its sharp, unexpected surges. This causes a displacement of organs from the peritoneum to the thigh area and the development of a hernial formation in the fold below the inguinal ligament.
Such hernias can manifest themselves either unilaterally or bilaterally, and are:
- reducible, which can be put back into the canal;
- irreducible, which cannot be reduced;
- pinched, in which compression of the hernial formation requires urgent surgery.
The formation is due to the gradual development of:
- At the beginning, a hernial sac is formed, but it still remains in the peritoneal cavity and the pathological process is asymptomatic. Sometimes (at the beginning of development) its partial infringement may be noted.
- The second stage is characterized by the penetration of the bag into the cavity of the femoral canal. However, it is still difficult to identify the pathological process, since the bulge is completely invisible during examination.
- Only at the third stage does the hernial protrusion, passing through the subcutaneous tissue layers, appear in the groin area or on the outer labia.
Basically, signs and symptoms of a femoral hernia in the groin in women appear in mothers who have given birth frequently and are aged 30 years or older. A characteristic symptom is chronic pain in the pelvic area. The character is absolutely varied - it can be acute or stabbing, manifest episodically and in the form of prolonged attacks. When lifting weights, moving or under the influence of any loads, an increase in the intensity of the pain syndrome is characteristic.
In addition to pain in the pelvic area, symptoms of an inguinal hernia may include:
- involuntary sudden spasms of hernial formation;
- lumbago in the vaginal and thigh area;
- painful bowel movements;
- radiating pain to the ovaries;
- pain during sexual intercourse.
Due to its characteristics, the disease is (most often) diagnosed only at a late stage of development, after a long time - months and years after formation. And throughout this period, the woman is susceptible to pelvic and abdominal pain, which is often attributed to gynecological causes.
Pathology
From congenital anomalies and acquired defects in the structure of P. o. the most common are hernias (see).
Of the inflammatory processes, a furuncle (see), carbuncle (see), hidradenitis (see), lymphadenitis of superficial lymph nodes (see Lymphadenitis), which develops as a result of the transfer of infection from inflammatory foci localized in hl., are often observed. arr. on the skin of the external genitalia and the anteromedial surface of the thigh, sometimes the lower leg and foot.
From congenital anomalies and acquired defects in the structure of P. o. the most common are hernias (see).
Of the inflammatory processes, a furuncle (see), carbuncle (see), hidradenitis (see), lymphadenitis of superficial lymph nodes (see Lymphadenitis), which develops as a result of the transfer of infection from inflammatory foci localized in hl., are often observed. arr. on the skin of the external genitalia and the anteromedial surface of the thigh, sometimes the lower leg and foot.
Afterword
There are many organs and structures in the groin area: for this reason, various diseases can cause pain, most of them have a strong impact on the female body, and therefore require prompt consultation with a doctor.
Read
Also:
- Anatomy of the uterus: location, structure and functions
- Causes and symptoms of inflamed lymph nodes in the groin, treatment tactics
- What healthy labia should look like
- Labia in women: anatomical structure, indications for labiaplasty
Operations
By. is of great interest in surgery from the point of view of choosing the safest surgical approaches to the iliac blood vessels, abscesses and phlegmons located in the subperitoneal section of the small pelvis (see Pirogov incision). In addition, through P. o. operational access is made to the contents of the inguinal canal (see) for inguinal hernias (see) and for funiculocele (see Spermatic cord).
Bibliography: Venglovsky R.I. About the descent of the testicle, in the book: Works of the hospital. hir. clinics, ed. P. I. Dyakonova, vol. 1, p. 7, M., 1903; aka, Development and “structure of the inguinal region, their relation to the etiology of inguinal hernias,” M., 1903; 3 o-Lotareva T.V. Surgical anatomy of the anterolateral abdominal wall, in the book: Surgeon. Anat, belly, ed. .A. N.
G. E. Ostroverkhov, A. A. Travin.
By. is of great interest in surgery from the point of view of choosing the safest surgical approaches to the iliac blood vessels, abscesses and phlegmons located in the subperitoneal section of the small pelvis (see Pirogov incision). In addition, through P. o. operational access is made to the contents of the inguinal canal (see) for inguinal hernias (see) and for funiculocele (see Spermatic cord).
Bibliography: Venglovsky R.I. About the descent of the testicle, in the book: Works of the hospital. hir. clinics, ed. P. I. Dyakonova, vol. 1, p. 7, M., 1903; aka, Development and “structure of the inguinal region, their relation to the etiology of inguinal hernias,” M., 1903; 3 o-Lotareva T.V. Surgical anatomy of the anterolateral abdominal wall, in the book: Surgeon. Anat, belly, ed. .A. N.
Inguinal hernia in women: symptoms
An inguinal hernia in women can be identified by the following symptoms:
- visualization of a tumor-like protrusion in the groin;
- pain in the lower abdomen and groin, which can radiate to the lumbar region, sacrum and coccyx. Pain syndrome may increase due to sneezing, coughing, physical activity, menstruation;
- dyspepsia in the form of diarrhea, constipation, flatulence.
With a small inguinal hernia, symptoms may be absent or erased.
Diagnostics
Diagnosis and treatment of fungus in the groin area is carried out by dermatologists and mycologists. After collecting a history of the disease and listening to the patient’s complaints, they begin an external examination of the lesion and laboratory research methods. In some cases, consultation with an infectious disease specialist, venereologist, or immunologist may be required.
To confirm or refute the alleged diagnosis, it is necessary to conduct a microscopic and bacteriological examination of scrapings from the lesions for pathogenic fungi. To do this, prepare a smear for microscopy and inoculate the test material on Sabouraud’s selective medium. The crops are incubated in a cooling thermostat at 22 degrees for 5 days.
Examination under a Wood's lamp will help exclude other diseases with a similar clinical picture.
What diagnostic methods are used for inguinal hernia in women?
After collecting complaints and anamnesis of the disease, the surgeon begins to examine and palpate the inguinal hernia.
Upon examination, you can see the presence of a tumor-like formation in the groin area, which is reduced or not reduced when the patient takes a horizontal position.
Upon palpation, the doctor must determine the symptom of a “cough impulse”, which can be negative and positive. To do this, the patient is asked to cough, and if the vibration is transmitted to the hernia, this means that the symptom is positive.
Also, an inguinal hernia that occurs against the background of an adhesive process is characterized by a “tight string” symptom. With this symptom, a woman experiences a feeling of tension in the muscles of the anterior abdominal wall when straightening her body.
The degree of hernia reducibility is diagnosed using ultrasound, which visualizes the organs trapped in the hernial sac.
A rectovaginal gynecological examination allows you to find out whether the uterus or its appendages are included in the contents of the hernial sac.
In men
Everyone should know the structure of the human body. Let's consider where the groin is located. This area is located below the abdominal region and adjacent to the thigh. The groin area is distinguished by its regular shape, resembling the outline of a right triangle.
A person's groin is located in the lower part of the abdominal region. A canal passes through the groin, which contains the large veins and arteries of the thighs and the inguinal cord (in men) or the ligament of the uterus (in women). The word “Groin” itself, in the dictionary of V.I. Dahl, is interpreted as a depression, depression.
Pain in the groin area most often occurs due to a hernia, which is treated with massages and physical therapy. They can also occur due to tumors, colliculitis and proptosis. Groin injuries can occur due to too much physical exertion during work or sports (weightlifting, bodybuilding, etc.).
Treatment of inguinal hernias, surgery
Inguinal hernias that appear in women of a certain age category are not amenable to either medication or physiotherapeutic treatment. The only way to get rid of the pathology is a herniotomy operation.
Operation
Today, in Russian medical clinics specializing in the treatment of hernias, the following surgical methods of hernioplasty are used:
- Tension (during the operation the doctor uses the patient’s tissue, so the second name is autohernioplasty);
- Tension-free (during surgery, a mesh prosthesis is used).
Removal of an inguinal hernia in women is most often performed using a synthetic implant. During surgery, the surgeon strengthens the hernial orifice from the inside using a special mesh made of polypropylene.
Subsequently, it will act as a frame that prevents the internal organs from going beyond the boundaries of the abdominal wall.
Mesh hernioplasty is currently considered as the main method of surgical treatment of inguinal hernias, inferior to autohernioplasty.
hernia surgery photo
Surgical treatment of inguinal hernias today is carried out both through abdominal intervention and more gentle methods, for example, laparoscopy.
Bandage
Bandage
In some cases, doctors try non-surgical methods for treating an inguinal hernia and prescribe a bandage to patients. This technique is indicated for patients who do not have indications for emergency surgery, as well as patients with the following pathological conditions when surgery may pose a high risk:
- diseases of the heart and blood vessels;
- young or old age (after 60 years);
- lung diseases;
- early recurrence of inguinal hernia, etc.
Regular wearing of the bandage will prevent the protrusion from increasing in size and minimize the risk of pinching.
Rehabilitation after surgical treatment of inguinal hernias
When surgery is performed correctly, patients undergo a rehabilitation period without complications. They do not require hospital observation, so literally a few hours after the operation, performed under local anesthesia, they can go home.
If the surgeon used a more complex technique that required general anesthesia, the patient will have to spend the night in the hospital, under the supervision of medical personnel. He will be able to go home the next day if there are no complications after anesthesia or after surgery.
After surgery, it is necessary to follow the instructions of the attending physician; in this case, women will be able to return to their normal rhythm of life in just a month.
- Compliance with the recommendations will prevent relapse of the disease, especially if there is a family history.
Treatment prognosis
When surgically treating inguinal hernias, doctors usually give positive prognoses to their patients. In isolated cases, they develop a relapse or experience a complication in the form of strangulation or inflammation of the appendix.
After returning to the usual rhythm of life, women should be more attentive to their health. Strong physical stress on the abdominal cavity is strictly contraindicated for them - constipation, heavy lifting, cough due to smoking, etc.
Many women, after surgical treatment of inguinal hernias, successfully endured more than one pregnancy, as they followed all the instructions of the specialists.
- In this case, it is recommended to wear the bandage from an early stage - from about 11-12 weeks.
Unilateral (right or left) groin pain
3. For appendicitis.
Acute
Treatment of inguinal fungus is carried out in the acute period, when the patient suffers from itching and burning. Antihistamines come to the rescue, eliminating irritation and discomfort in the groin - Cetrin, Zyrtec, Zodak, Diazolin.
After eliminating the symptoms of inflammation, the foci of epidermophytosis are treated with a Fukortsin solution, which has a fungicidal and antimicrobial effect. Patients are prescribed lotions with Resorcinol, sulfur-tar, Wilkinson and zinc ointments, Triderm. A silver solution will help cope with inflammation and serous blisters.
During illness, the patient's immunity is greatly reduced. To strengthen it, it is recommended to use light immunostimulants - “Immunal”, “Imunorix”, “Licopid”. Complications of bacterial origin require treatment with antibiotics.
In the presence of extensive lesions, desensitizing therapy, antibiotic therapy, vitamin therapy, and autohemotherapy are carried out in a hospital setting.
If personal hygiene is not observed, drug treatment does not give a positive result. Patients need:
- Wash daily, paying special attention to the treatment of skin folds;
- Take baths with infusions of medicinal herbs that have anti-inflammatory and antiseptic effects;
- Wear loose underwear made from natural fabrics.
ethnoscience
Currently, there are a large number of traditional medicine recipes intended for the treatment of inguinal epidermophytosis at home.
- Infusion of St. John's wort, chamomile and lingonberry leaves is taken 100 ml daily for a month.
- Lotions made from a decoction of string, yarrow, and oak bark give good results. After the procedure, zinc ointment is applied to the skin.
- Radish seed pulp is applied to the affected areas of the skin.
- An alcohol tincture of poplar and birch buds is used to treat inflamed areas.
- Crushed celandine is applied to the lesions of inguinal athlete's foot for half an hour.
- Onion gruel helps get rid of pathology.
- A thick paste is prepared from soda, which is rubbed onto the affected skin.
- Ointment with essential oils is rubbed into the affected areas daily.
- Almond essence will help cure athlete's foot in the groin.
Inguinal hernia in pregnant women: symptoms and treatment
During pregnancy, the symptoms of a hernia in the groin are the same as in non-pregnant women.
Women are concerned about a tumor-like protrusion in the groin area with discomfort and pain. Moreover, the intensity of pain depends on the duration of pregnancy, since intra-abdominal pressure increases with the increase in the size of the uterus. Women also notice that the size of the hernia increases after physical activity.
In addition to the symptoms described, the expectant mother feels discomfort when walking or exercising, especially if the size of the hernia is large enough.
The decision on the method of delivery is made by an obstetrician-gynecologist together with a surgeon. The choice of method is influenced by the size of the hernia, complications of the hernia and characteristics of the course of pregnancy.
For small, uncomplicated hernias, a natural birth is possible, during which the doctor will hold the hernial sac to avoid strangulation.
For small complicated and large inguinal hernias, as well as when there is a pathology of pregnancy, childbirth is carried out by cesarean section.
Throughout pregnancy, women suffering from hernia disease should wear bandages that minimize the risk of hernia enlargement and complications. You can buy such a bandage at a pharmacy or stores that sell medical supplies. You should also avoid excessive physical activity and heavy lifting.
There are specially designed sets of exercises that can strengthen the abdominal muscles.
In addition, diet is a mandatory component of the treatment of inguinal hernia.
In most women, after the birth of a child, an inguinal hernia goes away without any treatment.
Topographic anatomy of the inguinal canal
Between both legs there are transverse tendon fibers (fibrae intercrurales), which limit the superolateral side of the external inguinal ring. The external inguinal ring is projected on the skin slightly higher and lateral to the pubic tubercle. The internal opening of the inguinal canal, located corresponding to the external abdominal fossa (fovea inguinalis externa), is projected on the skin 3 cm inward and downward from the superoanterior spine. Thus, the course of the inguinal canal is located at a slight angle relative to the pupart ligament.
The boundaries of the inguinal canal are as follows: in front - the aponeurosis of the external oblique muscle, behind - the transverse fascia, below - the Poupartian ligament, above - the edges of the internal oblique and transverse muscles. In men, the spermatic cord is located in the inguinal canal, represented by the vas deferens (ductus deferens), spermatic artery, vein, nerve and lymphatic vessels.
In women, only the round ligament of the uterus (lig. teres uteri) passes through the inguinal canal. The testicles and appendages are located in the scrotum; The epididymis, consisting of a head, body and tail, which passes into the vas deferens, is adjacent to the superoposterior surface of the testicle.
Inguinal hernia: what is it?
An inguinal hernia is the slippage of abdominal and pelvic organs into the inguinal canal through its internal ring. The hernia consists of the gate, the sac and its contents. The gate in this case is the inner ring of the inguinal canal. The hernial sac is formed from fascia, peritoneum, muscles, subcutaneous tissue and skin. In women, most often the contents of an inguinal hernia are the omentum, part of the small intestine and/or colon, the uterus and/or its appendages (fallopian tubes, ovaries), and sometimes the spleen, gall bladder or stomach.
You can see what an inguinal hernia looks like in the presented photos.
Depending on which side the hernial sac is located, the following types of inguinal hernias are distinguished:
- left-handed;
- right-sided;
- two-sided.
Also, hernias in the groin area are usually classified by location, namely:
- direct inguinal hernia (the hernial sac passes only through the inner ring of the inguinal canal). This type of hernia is also called internal;
- indirect inguinal hernia (the hernial sac passes through the lateral inguinal fossa, which is the most common type of hernia);
- superficial subvesical inguinal hernia (the hernial sac passes between the middle and medial umbilical folds of the peritoneum).
If we talk about the degree of reducibility of hernias, then it must be said that some can be reduced independently in a certain position of the body, for example, when the patient lies on his back. Other inguinal hernias are difficult to reduce or cannot be reduced at all. Hernias become unreducible due to adhesions that appear as a result of the inflammatory process of the walls and organs that have slipped into the inguinal canal.
Prevention
Preventive measures to avoid the appearance of fungus in the groin:
- Disinfection of patient care items and common areas,
- Boiling and ironing linen, socks, shoe treatment,
- Use of removable shoes in baths and saunas - slates or rubber slippers,
- Fighting sweating
- Regular hygiene procedures,
- Wearing underwear made from natural fabrics in hot weather,
- Daily treatment of skin folds with cologne, salicylic alcohol, resorcinol and powdering them,
- Examination of contact persons,
- Prevention of stress,
- Strengthening the immune system.
The prognosis of the disease is favorable. Acute and chronic stages of inguinal athlete's foot respond well to therapy. Modern antimycotic drugs can prevent relapse and re-infection.
The main causes of inflammation of the lymph nodes in the groin area in women
Doctors identify the following main causes of inflammation of the lymph nodes in the groin area:
- Inflammatory process in the bladder. Sometimes the described disease is provoked by urethritis.
- Sexually transmitted diseases. For example, syphilis or gonorrhea. These diseases often cause damage to the lymph nodes.
- Diseases of the reproductive system, incl. associated with the external genitalia (often colpitis or balanoposthitis).
- Skin inflammation of the groin area, allergic reactions.
- Oncological diseases (malignant tumors of organs located in the groin area).
- Fungal diseases of the skin of the feet.
- Consequences of influenza, acute respiratory infections.
If the inflammation of the lymph nodes has reached a late stage, other symptoms may appear, indicating the poor condition of the human body as a whole, and often that there are other diseases in the woman’s body.
But you should not make hasty conclusions on your own, but first of all you need to contact a specialist.
Structure of the groin area
It appears not only in the groin, but also on the stomach. It is distinguished by a clear location in these places, red spots that itch and peel.
In this case, the vagina is not affected. Mycosis develops mainly in older people due to improper hygiene or if a woman wears a wet synthetic swimsuit for a very long time.
Doctors here advise treatment not internally, but externally with the help of various ointments, gels and creams: econazole, clotrimazole. It is also recommended to change your underwear to something thin and without irritating edges. Then you can get rid of the unpleasant disease and try to cure the bad symptoms.
But only a specialist will be able to distinguish mycosis from another disease - psoriasis. Please note that psoriasis usually causes itching. Mycosis can occur not only in intimate places, but also on the arms, legs, torso or throughout the body.
This disease manifests itself in the form of a bright red rash that affects the folds in the groin. It occurs in both men and women. The occurrence of such a symptom indicates the activity of candida fungus. In appearance, such a rash in the groin resembles burns. The following methods are used as home treatment:
- refusal to wear uncomfortable underwear;
- regular showering;
- applying antiseptic and antifungal agents to the groin area.
In the latter case, Lamisil, Ketoconazole, Naftifine, Econazole, Wilkinson's tar ointment, Miconazole and Triderm have proven themselves well. If bubbles appear on the affected areas, they are burned with brilliant green or iodine. In stationary conditions, such formations are pierced with a sterile needle and bandaged.
A comparative examination of the right and left sides of the groin area and scrotum should be carried out with the patient standing and lying down. To more clearly determine the shape, size, identify initial and canal inguinal hernias, and the reducibility of hernial protrusions, the examination is supplemented with techniques that increase intra-abdominal pressure: coughing, straining, a 10-20 minute walk.
Among the layers in this area are:
- skin;
- subcutaneous tissue;
- fascia - the sheath of muscles;
- internal muscles: transverse and oblique;
- preperitoneal tissue;
- peritoneum.
The groin area is characterized by significant development of sebaceous and sweat glands. The layer of subcutaneous fat is expressed differently in women and men. The thickness of this layer becomes greater directly at the inguinal ring. The following arteries pass through the subcutaneous tissue:
- superficial epigastric;
- superficial surrounding iliac.
The nerves passing through the fiber belong to the terminal branches. The muscle fibers lie parallel to the inguinal ligament, a fibrous band that covers the space in front of the pelvis. Women have more developed oblique muscles than men.
The inguinal canal runs towards the center of this area and ends at the outlet, also called the superficial ring. The following are the walls of the inguinal canal:
- upper, consisting of fibers of the abdominal muscles;
- the lower one, which looks like a shallow trench;
- anterior, formed by the external and internal oblique muscles;
- posterior, formed by thickened fascia.
The approximate length of the abdominal canal in an adult is about 4 cm; in children it is much shorter.
Now you know where the inguinal canal is located and what are the features of its structure. You may also find the article What to do if your groin smells useful.
Cause of hernia defects
- A congenital anomaly of the development of the connective tissue of the body, which means weakness of the connective tissue of the entire body, and not just the groin area. The chance of hernias appearing in other parts of the abdominal cavity also increases.
- Damage to the groin area as a result of mechanical trauma. (Accidents, martial arts, etc.)
- High intensity of physical labor (quick lifting of heavy objects leads to a sharp increase in intra-abdominal pressure).
- Attacks of severe coughing, chronic constipation (during coughing, sneezing or straining, the abdominal muscles tense and lead to sharp increases in intra-abdominal pressure)
- Excess body weight is also a risk factor for developing inguinal hernias.
Features of the inguinal lymph nodes
Inguinal lymph nodes in the human body are large in size and superficial in location. Their number depends on the physiological characteristics of a person. The lymph nodes in this area can almost always be palpated. They are located in the subcutaneous fat layer just below the inguinal fold. Palpation problems sometimes occur in overweight people. Otherwise, the location of the lymph nodes in the groin makes it quite easy to palpate them, and you can do this yourself.
Lymph nodes in the groin provide lymph flow to this area. They can increase against the background of inflammatory diseases of the pelvic organs. As a rule, enlarged lymph nodes in the pubis indicate problems with the genitourinary system, but in some cases it can be a symptom of systemic infections and autoimmune diseases.
In order to promptly detect alarming symptoms, you need to know where the lymph nodes are located in the groin. As a rule, the symptoms of disease in the lymph nodes of this area are quite specific, which makes it possible to promptly detect signs of pathology and, without delay, consult a doctor.
Anatomy and functions of lymph nodes
When an infection occurs, the lymph nodes in the groin become inflamed smoothly as the disease progresses, and when the groin area is injured, inflammation occurs quickly
Lymph nodes are small formations in the subcutaneous fat layer. These organs of the lymphatic system are predominantly bean-shaped or oval in shape. First, you need to understand the peculiarities of the location of lymph nodes in men and women. In fact, there are no gender differences in the location, number and size of lymph nodes in this area. In both women and men they are located in the upper thigh. Lymph nodes are located in a chain along the inguinal fold and along the great saphenous vein of the leg.
In general, they can be divided into three groups: upper, middle and lower groin lymph nodes.
The main function of lymph nodes is to filter lymph and enrich it with necessary substances (antibodies, etc.). Intercellular fluid from surrounding tissues and organs is supplied through lymphatic vessels to the lymph nodes, where it is cleared of toxins and infections, and then enriched with immune cells. The lymph, cleared of harmful impurities, then enters the blood. This ensures immunity support and blood saturation with necessary substances.
Sizes and palpation of inguinal lymph nodes
The number of lymph nodes in the groin varies from 3 to 20 on each side. As a rule, there are fewer of them on the left than on the right. So, a person can have up to 20 nodes on the right, and no more than 14 on the left.
Normally, the size of the inguinal lymph nodes ranges from 3 to 22 mm, according to other sources – from 5 to 20 mm. The largest are the upper lymph nodes, located above the inguinal fold. Their sizes can reach 2 cm in diameter. The lower groin lymph nodes are the smallest.
Knowing where the lymph nodes are located in the groin, many are lost, unable to palpate all the nodes, because they simply do not know what size they should be. It should be noted that palpation of large inguinal lymph nodes is almost always successful; palpating them is quite simple, but even a doctor cannot always cope with the lower nodes due to their small size.
Having figured out where the lymph nodes are in the groin, you should know how to palpate them. To do this, it is better to take a horizontal position and place your palm on the upper thigh so that your fingers touch the inguinal fold. Lymph nodes in the groin are palpated with soft movements of the fingers resting on the fold. Normally, it is not difficult to palpate the upper inguinal lymph nodes, since their sizes are quite large. The middle and lower lymph nodes may be difficult to palpate due to their small size.
Palpation of the lymph nodes should not cause pain. However, slight discomfort when pressing is not a deviation from the norm, but is associated with mechanical irritation of the nerve endings of the tissues in the palpated area. Normally, the contours of the lymph node are smooth, the structure is quite dense and homogeneous.
Symptoms of strangulated PG
PGRs can significantly impair a person's quality of life. But the most dangerous situation is when the hernia is strangulated in the hernial orifice. When the hernial sac is infringed, blood circulation in the part of the organ that is trapped in the hernial sac is sharply disrupted. If the patient is not provided with emergency surgical care, very serious consequences are possible: intestinal obstruction, necrosis (death) of a section of the intestine, fecal peritonitis - these are serious threats to life.
The body signals the development of strangulated PH by a sharp increase in pain and a change in its character. Typically, strangulation is provoked by a sharp increase in intra-abdominal pressure, for example, when lifting weights.
(if the table is not completely visible, scroll to the right)
| Strangled organ | Symptoms |
| Intestine | Acute pain appears in the area of the abdominal cavity, which quickly spreads throughout the abdomen. In the first minutes and hours, there may be a urge to defecate, and loose stools appear. But after some time, all stool disappears (although unproductive urge to go to the toilet may still occur), and with it the passage of gases also stops. The most important symptom of a strangulated hernia: when straining or coughing, the hernial protrusion does not increase in size as it did before the strangulation. |
| Intestines | Nausea quickly increases and vomiting occurs. If you delay a visit to the doctor, vomiting becomes uncontrollable. The temperature often rises, the heartbeat becomes rapid, and blood pressure drops. Without treatment, shock can lead to death. |
| Ovary | In this case, the picture is not so bright: the pain may be quite tolerable, and the general state of health does not raise suspicions of emergency surgical pathology. In men, as a result of a strangulated inguinal hernia, ischemic orchitis (inflammation of the testicle due to disruption of its blood supply) may develop, which is manifested by redness, tension and pain in the scrotum on the affected side. |
| Bladder | Acute urinary retention may develop. |
General concepts about the groin area
The groin is the connecting part between the abdomen and the thigh, depicted in the shape of a triangle. The key role here is played by the Poupartian (fallopian) ligament (ligament inguinale). It limits the groin area from below and from the outside. The groin is separated from above by a line passing between the anterior superior iliac spines; inside the separator is the lower edge of the rectus abdominis muscle. The groin area is not fully covered by muscles, so it is quite vulnerable.
Surgical method of treatment
At the time of the operation, the surgeon can use the patient’s native tissue or use special implants (mesh). In most cases, open surgery is used, where special equipment is used to control the operation.
If surgical intervention is used in young patients, then in almost all cases the doctor uses the patient’s own tissue, since at this age the risk of relapse is extremely low.
For older patients, surgery using an implant is recommended to reduce the risk of re-development of the pathology.
Another method of surgery, which is more gentle, can be performed - laparoscopy. The operation involves incisions of no more than 1 cm, which reduces trauma to the skin. It is performed under general anesthesia using carbon dioxide. This operation is preferable, since its minimal trauma helps to reduce the rehabilitation period.
Hernia in children
Signs and treatment of inguinal hernia
A hernia in the groin area manifests itself in children in the form of a protrusion, which is imperceptible in a calm state and increases in size when restless and screaming. At an older age, education can only manifest itself when doing physical exercise, coughing, or straining.
In both adults and children, surgery is performed to treat an inguinal hernia. The intervention is performed under anesthesia, so it can be performed even on newborn children.
The formation of an inguinal hernia in children has one complication: pinching of an internal organ or its death (intestine, ovary) may occur.
Inguinal hernia in girls
The process of formation of an inguinal hernia in girls is significantly different from a hernia in boys. This is caused by the peculiarities of the intrauterine development of the female reproductive system. Such cases are quite rare, but require prompt treatment.
Causes:
- Injury to the abdominal wall;
- Congenital anatomically vulnerable places in the abdominal cavity or on the abdominal wall (umbilicus, inguinal canal);
- Excess weight (relevant for children under 6 years of age);
- Diseases that provoke an increase in intra-abdominal pressure (constipation, debilitating cough, tumors).
Therapeutic measures
The only method used to treat hernias in children is surgery. If not treated promptly, major complications can occur.
The operation is possible if: the child has no diseases of any kind, good test results, and no colds. If the child has any health problems, then the operation is adjusted until the child recovers. Only if an inguinal hernia is strangulated, removal is carried out on an emergency basis.
Signs of a hernia in boys
Symptoms of a hernia in the groin in boys include pain and protrusion. The protrusion can be observed in the scrotum or in the groin itself, and in both cases it brings considerable discomfort. In a calm state, the formation is not visible; it appears only when crying or coughing. During the examination, the pediatric surgeon will palpate the testicles and groin to make an accurate diagnosis.
The child may also complain of nausea, stool retention, and excessive gas formation.
Treatment
Under the age of 5 years, surgery is contraindicated. In such situations, the boy must wear a special bandage, with a minimum period of time for rest. After 5 years, intervention is allowed to remove the hernial sac.
A hernia in the groin in boys is quite complicated.
The operation lasts about 20-30 minutes and is performed under general anesthesia. After 4-5 days, the child can be taken home. When applying regular rather than absorbable sutures, they must be removed after 2 weeks.
What is a strangulated hernia?
A pinched hernia occurs when treatment is delayed or not treated at all. With constant enlargement of the hernia, the child feels constant discomfort. The hernia is visible to the naked eye and, when pinched, looks like a stone. In such situations, operations are carried out immediately.
A strangulated hernia requires surgical intervention, regardless of the child’s age, as this can cause serious complications, including death.
Photos of an inguinal hernia in children and its strangulation can be viewed on the Internet or on the websites of clinics that treat this problem.
Only a negligent attitude of parents towards a child can lead to a strangulated hernia. If any symptoms occur, you should contact a specialist.
Prevention of inguinal hernia formation
To prevent pathological protrusion in the lower abdomen, a woman must follow the following recommendations:
- Healthy food;
- control weight, avoid obesity;
- lead an active lifestyle, move more, walk, play sports;
- wear protective equipment during training if the groin area may be injured;
- limit physical activity, avoid lifting heavy objects, if a person has prerequisites for the formation of a hernia or poor heredity.
Rehabilitation and recovery after surgery
The duration of rehabilitation after surgery to remove an inguinal hernia in women depends on the method used. Thus, with laparoscopic or endovidoscopic intervention, it takes an order of magnitude less time than with tension gherinoplasty.
To quickly recover and reduce the risk of complications such as suture dehiscence, it is recommended to wear a bandage (for inguinal hernia in women, this device is also used to prevent strangulation of the hernia before surgery). In addition, the doctor may prescribe painkillers.
In general, rehabilitation after removal of a hernia in the groin is divided into several periods:
- Outpatient – lasts up to 10 days after surgery.
- Rehabilitation – begins 2-3 weeks after surgery.
- Final – lasts from a month to six months, depending on the presence of complications and/or relapses.
During the outpatient recovery period, patients are advised to minimize physical activity. Bed rest with a gentle diet is preferable. The recovery period involves a gradual increase in physical activity without active use of the abdominal muscles. It is during this period that it is recommended to wear an inguinal bandage.
The final stage of rehabilitation is the creation of a strong muscle corset.
It is recommended to perform the following exercises:
- "Scissors". Performed in a supine position. The legs are raised in relation to the body by 45 degrees, slightly spread to the sides, and then crossed. Repeat 507 times in the first days, then the number of movements is gradually increased to 15-20.
- “Bicycle” or leg rotation from a lying position. The duration of execution in the first week is about 1-3 minutes, followed by an increase to 5-7 minutes per approach.
- Raising the straightened leg back from a standing position in a knee-elbow position. At the initial stage, it is enough to straighten the leg not completely, and then the amplitude of the swings is gradually increased. The number of exercises per approach is 3-5 at the initial stage with a gradual increase to 15-20.
Important! If any discomfort occurs in the form of pain, burning in the scar area or weakness, it is recommended to stop exercising.
Types of hernias in the groin in women
Depending on which side of the body the protrusion is located, it is customary to distinguish left-sided, right-sided, and bilateral pathologies. Another classification divides hernias based on how they pass through the inguinal canal:
- Oblique. The most common type is in which the sac, deviating to the side, passes through the lateral fossa, often descending into the labia majora.
- Direct (internal). The hernial sac protrudes through the medial inguinal fossa.
- External superficial supravesical. The sac exits through the supravesical fossa, between the medial and middle umbilical folds of the peritoneum. A rare form of protrusion.
Hernias are divided according to the degree of reducibility. Some formations can return to the abdominal cavity on their own or with light pressure on the protrusion when the patient takes a certain body position (lies on his back). This occurs with a wide gate, if the organs that have penetrated the inguinal canal have not fused with each other. Other protrusions are difficult to reduce or do not do so at all.
The main reasons are the presence of adhesions due to inflammation of the walls and the fusion of organs that have slipped into the inguinal canal. With an unreducible hernia, the internal organs in the sac are constantly injured. This leads to the appearance of adhesions, impaired blood circulation, and lymph outflow.
Such protrusions are dangerous and require surgical intervention, as they can grow to enormous sizes.
Articles on the topic
- Hormonal imbalance in women - symptoms during pregnancy, menopause, after an abortion and in adolescence
- Diseases of the rectum: signs and diagnosis
- Compression stockings for surgery and recovery period - how to wear and how long to wear
Reasons why lymph nodes in the groin may become inflamed
Covering areas of the body with the current, the lymph enters the infected organs, capturing the infection and continuing its journey. The glands located in the groin area may become swollen. The cause of swelling may be an infection that has been captured by the lymph. The lymph node thus became infected, resulting in swelling. Pain appears in the groin, legs, lower abdomen, buttocks, anus, external genitalia, perineum.
The groin area, an important area of the immune system, contains many nodes containing white blood cells (lymphocytes) that fight infection. If the infection is weak, then the gland will destroy this infection, the swelling will be slightly painful.
In the event of an illness that does not cause pain, it can lead to an advanced stage of the disease, complicating the treatment process. The acute stage of the disease turns into a chronic disease (gonorrhea, chlamydia, syphilis).
The inguinal node can become inflamed due to allergies or infection in the area. Swelling of the lymph nodes can be caused by syphilis, chancroid, ponococcal infection, herpes simplex, lymphogranuloma venereism, which are sexually transmitted.
- Cat scratches on the skin are dangerous and sometimes lead to inflammation.
- Canditis fungus can lead to swelling of the groin nodes as a result of thrush.
- Malignant tumors also cause inflammation of the gland in the groin.
- Hernia – femoral or inguinal.
- Benign cysts, such as Bartholin's cyst, which are located near the vagina. Such a cyst is filled with air, liquid or semi-solid substances. If the cyst gets infected, it will fester.
- Chronic diseases (sarcoidosis, arthritis, chronic lupus erythematosus and others) lead to swelling of the glands.
If the inguinal glands are swollen, then this is a clinical sign of pathology in the groin, legs, buttocks or abdominal wall.
Diseases in the groin leading to inflammation of the lymph glands:
- Bubonic plague. In this case, the skin above the groin becomes inflamed and red.
- Infectious mononucleosis, a viral infection, causes swollen nodes in the groin. The infection can spread throughout the body, causing glands in other parts of the body to swell, such as the neck and armpits.
- Toxoplasmosis caused by the parasite Toxoplasma gondii. Most adults are not dangerous from this parasite. No treatment is required. It is dangerous for people only with low immunity, and those with HIV/AIDS. For them it manifests itself as a serious infection. It is also dangerous for babies if mothers are infected.
- Some types of cancer lead to lymphadenopathy in the area where the nodes are located, which is accompanied by swelling of the gland. A malignant tumor may form.
- The inguinal node may become swollen due to a bacterial infection in the skin, muscles and bones of the lower leg, pelvis, and subcutaneous tissue.
The following types of bacteria cause disease:
- spherical (streptococci, staphylococci, meningococci, pneumococci)
- rods (intestinal, tuberculosis, mycobacteria, shigella, tetanus, diphtheria, yersiniosis)
- convoluted (syphilis, leptospirosis)
- spirochetes (borreliosis, tick-borne)
- flagellates (cholera)
Possible complications
An inguinal hernia can cause consequences that are extremely dangerous to the health and life of the patient. Here are several of the most serious types of complications. Development of the inflammatory process
Often, if the pathology is not treated in a timely manner, women develop inflammation. This happens against the background of such serious diseases as appendicitis, colitis, and various diseases of the female genital organs. Symptoms may not be intense.
This is a slight increase in body temperature and malaise. The main danger is the formation of adhesions, due to which a reducible hernia becomes unreducible.
If pronounced symptoms, fever, nausea, vomiting, or problems with the digestive system appear, you should immediately consult a doctor. Such signs may indicate the development of appendicitis and other dangerous pathologies.
Blockage. When part of the colon gets into the hernial sac, fecal blockage occurs. This process causes intestinal obstruction, which entails disruptions in the functioning of the gastrointestinal tract, and in some cases, necrosis of intestinal tissue. Blockages most often occur in older patients and require surgery.
Infringement. Strangulation is considered the most dangerous complication. Under the influence of certain reasons, the contents of the sac are strangled in the hernial orifice. This process leads to poor circulation and death of healthy tissue. Symptoms of infringement include:
- strong pain;
- inability to straighten the contents of the bag;
- if the uterus is pinched, pain can cause loss of consciousness;
- nausea, malaise, vomiting;
- The temperature often rises.
If you notice such symptoms, you should immediately consult a doctor. A timely reaction and competent medical care will help avoid serious consequences in the future.
Symptoms of other complications of inguinal hernia
In addition to strangulation, which occurs in 10–20% of people with inguinal hernias, other conditions can become complications of a hernia: inflammation of the intestinal tract or coprostasis (stagnation of feces).
With coprostasis (stagnation of feces), in response to coughing and straining, a further increase in hernial protrusion occurs (differential diagnosis with strangulated PG). The hernia itself increases significantly in size, and upon palpation it acquires a dough-like consistency. If measures are not taken, the situation may end in fecal impaction.
When the hernia is inflamed, the skin over the hernial protrusion becomes red, and pain appears when palpating the hernia or trying to reduce it. The addition of symptoms such as fever, vomiting, chills, and impaired gas discharge may indicate the transition of inflammation to a purulent form. Purulent inflammation, like a strangulated hernia, requires surgical treatment.
Rehabilitation after surgery to remove an inguinal hernia
Important points of rehabilitation after inguinal hernia surgery in older men that you should pay attention to:
- Pain. In the first days after surgery, an elderly patient may feel intense pain. In such cases, the doctor prescribes painkillers.
- Seams. After a few hours, it is necessary to replace the bandage and begin treating the seam with resorption ointments and antiseptic preparations. Neglect of this rule leads to the development of infectious complications. In such cases, frequent seam treatment is required. The doctor prescribes antifungal and antibacterial drugs to the patient.
- Movement. An elderly patient is prohibited from getting out of bed without the doctor's permission. The doctor regulates physical activity taking into account the patient’s condition. Staying in bed for longer than expected can also lead to complications.
- Dieting.
- Elimination of physical activity.
Symptoms
Patients may not always detect a protrusion in their groin area. This is due to the fact that the early signs of the disease are erased. The increase in pain during menstruation is explained by the fact that part of the genital organs has entered the hernial sac.
Characteristic manifestations of hernia in women:
- the appearance of pain in the abdominal cavity (they can radiate to the sacral and lumbar regions);
- increased discomfort and pain during coughing movements, intense exercise;
- increased formation of gases;
- burning in the abdominal cavity;
- diarrhea;
- constipation.
A characteristic manifestation of a hernia in women is diarrhea.
Depending on the type of hernial protrusion, the following characteristic signs in women are distinguished:
- In the case of a reducible hernia, there is a sudden, less often a gradual onset of the disease. There is no vomiting or fever. The hernia is within the sac and is not growing. A cough impulse is diagnosed. The formation can be reduced and has a different consistency to the touch.
- With an irreducible hernia, the onset of the disease is gradual. The woman notes moderate pain, sometimes vomiting. The hernia is in the sac and has no tendency to grow. The protrusion is soft to the touch. There are no symptoms of intestinal obstruction.
- With fecal stagnation, the pain is moderate. Due to the accumulation of fecal breakdown products in the digestive tract, the patient experiences repeated vomiting. Sometimes body temperature rises. The hernia cannot be reduced and gradually increases. Feels tense to the touch. Symptoms of partial intestinal obstruction are observed.
- Inflammation of the sac in which the protrusion is located begins suddenly. The pain is most often moderate, localized only within the inflammation. Severe vomiting and increased body temperature are observed. The protrusion gradually increases and can sometimes be reduced. When palpated, it is always tense and painful. Sometimes the patient develops shock.
- Infringement always develops suddenly. The woman feels too much pain throughout her abdomen. There is sudden and continuous vomiting and elevated body temperature. The size of the hernial protrusion gradually increases. No cough impulse is observed. The formation cannot be reduced, it is solid.
With fecal stagnation, the pain is moderate.
Methods for diagnosing inguinal lymphadenitis
If there is an enlargement of the lymph node in the groin of women, the causes of this phenomenon can be determined with high accuracy only through laboratory and instrumental studies. Their list is determined based on the presence of additional symptoms.
- General clinical analysis of blood and urine;
- Blood for RW (if there are signs of syphilis);
- PCR analysis for suspected viral and bacterial genitourinary infections;
- Blood chemistry;
- Inoculation of discharge to determine STIs in a nutrient medium or for PCR analysis or enzyme-linked immunosorbent assay (ELISA).
In addition, additional blood testing is carried out for HIV, cytomegalovirus, herpes virus and papillomavirus.
If you suspect inflammatory, non-infectious or oncological diseases of the genitourinary system, it is recommended to undergo additional laboratory diagnostics:
- Ultrasound examination of the pelvic organs;
- Computed or magnetic resonance imaging;
- X-ray of the pelvic organs.
If there is a high probability of Hodgkin's disease (cancer of the lymphatic system), an examination of the contents of the affected nodes will be proposed - a biography.
Causes
Itching in the groin is caused by external and internal causes. The first arise due to the use of certain substances or hygiene factors. The latter indicate the presence of some serious disease. Here's the full list:
- lack of hygiene;
- candidiasis;
- allergy;
- bacterial vaginosis (gardnerellosis);
- gonorrhea;
- chlamydia;
- trichomoniasis;
- genital herpes;
- psoriatic lesion;
- lichen planus;
- menopause;
- scabies;
- lice pubis;
- pathologies of internal organs (anemia, diabetes, hepatitis and others).
Poor hygiene
The most common cause of itching in the groin area is neglect of personal hygiene rules. Caring for this area should be done daily. You need to wash yourself with running warm water in the direction from the vagina to the anal area. If you do not do this, the consequences will be as follows:
- white vaginal discharge (“leucorrhoea”) accumulates on the genitals;
- diaper rash occurs;
- spill elements are formed;
- irritation appears on the vaginal mucosa.
Thrush (candidiasis)
Fungi of the genus Candida are constantly present in the female body. But if the immune system fails, then they begin to actively reproduce.
This entails swelling and redness of the genitals, pubic itching, severe burning, and the appearance of cheesy vaginal discharge with a sour odor.
Allergy
Allergic reactions develop due to various circumstances. Here is their list:
- Use of medications . Many medications have a contraindication such as dry mucous membranes. It is the dry mucous membrane that causes itching in the groin. Women with individual intolerance to a certain drug are especially susceptible to this factor.
- Inaccurate depilation of the bikini area . In such a case, damage to the epidermis occurs, which entails the occurrence of a symptom.
- Hygiene products (pads) . Improper use of panty liners or regular pads also causes itching in the groin. Experts advise changing regular pads every two hours, and daily pads every four hours. The presence of fragrances and fillers may not be suitable for a particular person. Therefore, when purchasing these products, you need to pay attention to their hypoallergenicity. During menstrual periods, you need to perform genital hygiene after each change of pad (use only gels or soap with neutral pH).
- Incorrectly selected underwear . Fabrics should not be synthetic, as they create a greenhouse effect and interfere with normal air exchange. In addition, synthetics themselves irritate the skin. Doctors are categorically against wearing thongs and tango panties. These types of underwear fit tightly to the skin and contribute to friction, which is the primary source of the problem.
Bacterial vaginosis (gardnerellosis)
Its development is due to the fact that the vaginal microflora turns from normal into opportunistic. The main symptoms are severe itching and gray discharge from the genital tract with a rotten fishy smell.
Gonorrhea
This infectious disease at the initial stage is asymptomatic. Then it begins to itch in the groin area, and profuse vaginal discharge appears. The genitals become swollen and red. Lack of therapy threatens the formation of adhesions and infertility.
Chlamydia
This disease is manifested by itching and discomfort in the genital area. These symptoms are accompanied by vaginal discharge that is yellowish in color. Often patients complain of burning or tingling during urination. If the infection gets into the ovaries and fallopian tubes, then pain and tension appear in the lower abdomen.
Genital herpes
The primary symptom of herpes infection is severe itching in the groin and the appearance of rashes in the form of small blisters. They are filled with white liquid contents. If there are multiple foci of rashes, then pain is added to the unbearable burning sensation.
Trichomoniasis
The infection manifests itself as itching in the groin area, hyperemia and swelling of the genitals, and purulent discharge with an unpleasant odor.
Painful sensations may occur during sexual intercourse. The disease is dangerous with a large number of complications.
Psoriasis
This dermatological disease can affect the skin throughout the body. In the groin it appears as scaly, bright red papules. The occurrence of rashes is accompanied by a strong feeling of itching.
Climax
During menopause, reproductive function fades and disruptions occur in the female hormonal system. Because of them, the environment on the mucous membrane of the genitals changes, and itching occurs.
Scabies
This is a contagious disease caused by the scabies mite. Severe itching appears due to the activity of mites on the skin. It worries mainly at night, when the parasite is most active.
Pediculosis pubis
In another way, this pathology is called phthiriasis. It occurs due to lice that settle in the area of the inner thighs, labia, and anus. Because of the bites, not only itching appears, but also small bluish spots.
Causes of pain on the left side
The development of the inflammatory process in organs such as the appendix, intestines, ureter, fallopian tube, uterus, ovary leads to pain. Since all these organs are located completely or partially in the groin area on the right, localization of pain on this side may indicate the following conditions:
- Appendicitis. This is an inflammation of the appendix, a process located in the lower part of the intestine. Accompanied by nausea, vomiting, fever. When painful sensations appear on the right side, they first try to exclude appendicitis from the list of possible causes.
- Ectopic pregnancy. Just like appendicitis, it should be excluded from the list of possible causes of pain at the very beginning. Occurs when the embryo is not attached correctly (in the fallopian tube, ovary, abdominal cavity). The growth of the embryo in organs not intended for this purpose leads to the rupture of the latter. The appearance of blood from the genital organs, loss of consciousness, and sweating are typical. This is a serious threat to a woman’s life, requiring hospitalization and surgery.
- Rupture of the right ovarian cyst. A cyst located in it and not causing concern can suddenly rupture. In this case, the liquid from it enters the abdominal area, which is a direct threat to the woman’s health. There is a high probability of nausea, increased gas formation, and increased temperature. Requires immediate hospitalization.
- Apoplexy of the right ovary. A condition characterized by a sharp rupture of the tissues of this organ, leading to bleeding into the abdominal cavity. Nausea, vomiting, dizziness, and weakness are typical. This is an extremely serious condition that requires urgent medical attention.
- Ovulation in the right ovary. The release of a mature follicle is often accompanied by pain. This is a normal phenomenon and does not require emergency measures.
- Infectious bowel diseases. They occur in different ways: with vomiting or diarrhea separately or simultaneously, with blood in the excrement and stool disorders, or affecting the entire intestine. From the gastrointestinal tract, Crohn's disease is also likely, characterized by the formation of granulomas (nodules) in any part of the gastrointestinal tract.
- Passage of stone through the ureter in urolithiasis. Causes severe pain radiating to the right side, characterized by general weakness, nausea, vomiting, flatulence.
Possible causes partially overlap with their appearance on the right side of the groin area: rupture of an ovarian cyst, ovarian apoplexy, ectopic pregnancy, ovulation, Crohn's disease.
Localization of pain in the left part of the groin area signals possible diseases of the kidneys, spleen, small intestine, sigmoid part of the colon, and may indicate the presence of:
- Chronic myeloid leukemia is a form of leukemia in which the spleen becomes enlarged due to an excessive number of granular leukocytes and their accumulation in the spleen. This is a serious cancer that can only be diagnosed by blood tests.
- Urological disorders - urolithiasis, inflammation of the left kidney or hydrocele of the kidney, as well as inguinal and femoral hernia.
- Functional or organic lesions of the gastrointestinal tract:
- colitis (inflammation of the mucous membrane of the large intestine), accompanied by a false urge to defecate, as well as diarrhea with mucus;
- ulcerative colitis, characterized by bleeding from the anus, frequent bowel movements;
- prolonged constipation, leading to overflowing of the intestines with feces;
- ulcers and tumors in the sigmoid colon, parasites in the small intestine.
Pain affecting the groin area on the right and left is often the main or sometimes the only symptom of chronic inflammation of the appendages, external genital endometriosis, and tumors of the internal genital organs.
If you add school knowledge of anatomy, you can remember that in the groin area on the left side of a person there are the following organs: intestines, kidneys, part of the bladder, and in women, also part of the uterus, the left ovary and one of the fallopian tubes.
Here are some of the main reasons for the appearance of such pain:
- The spleen is quite vulnerable, as it is very close to the surface of the body, so even a simple injury can cause a lot of trouble. It is also possible to have tumors that “give” to the groin. The same effect will occur from blocked urinary ducts
- Various pathologies in the intestines - constipation, disorders, bloating from increased gas formation - cause pain in the left lower abdomen. Benign and malignant tumors of the small intestine cause similar symptoms
- Kidney disease, also accompanied by fever, difficulty urinating and burning sensation during the process itself
- Problems “feminine”, which include endometriosis, which worsens during menstruation. Pain is accompanied by brown discharge with clots
- An ectopic pregnancy, in which the fertilized egg is attached not in the uterine cavity, but on one of the fallopian tubes or in the ovary, can cause nagging pain in the groin on the left
- During ovulation (when an egg is released from the ovary), a woman may experience aching pain associated with hormonal changes in the body.
- With ovarian apoplexy, a woman experiences throbbing pain, accompanied by fever, general weakness and bleeding.
- Adhesions formed after surgery or untreated inflammation can cause pain
Pain in the left side of the groin in women can signal the development of an ectopic pregnancy.
The causes of pain in the groin area on the right are not much different from the causes that cause them on the left. To the above, we can add that pain can also occur:
- during menstruation, which is associated with the physiology of a particular organism.
- Occasionally, pain is observed during the formation of a hernia
- Another common cause is inflammation of the appendages, which includes all female organs: the uterus, ovaries and tubes.
Pain in the groin area on the right can occur during menstruation.
The main cause of groin pain in older women is the physiological restructuring of the body at a certain age - menopause.
For each, it occurs at a different age and is accompanied by hormonal changes, which, in addition to sweating, dizziness, and nervous instability, are characterized by pain in the genitourinary system. This feeling is very strong during the so-called hot flashes.
Menopause is the main cause of groin pain in older women
Pain and burning in the groin can be caused by a variety of reasons. One of the most common is common irritation associated with poor personal hygiene.
It could also be an allergic reaction to various irritants:
- frequent use of regular toilet soap in the intimate area, which over time disrupts the alkaline balance and leads to candidiasis
- wearing tight synthetic underwear
- reaction to certain drugs (antibiotics, contraceptives, etc.)
In other cases, pain and burning indicate the presence of infection in the body, which indicate the following diseases:
- venereal, sexually transmitted: chlamydia, genital herpes, trichomoniasis, etc.
- inflammation of the urinary tract
Pain and burning in the groin in women often occurs due to infections
Typically, this pain syndrome accompanies diseases that require prompt surgical intervention.
The most common among them:
- appendicitis
- sigmoid volvulus
- rupture or torsion of the pedicle of a cyst in the ovaries
- rupture of the ovary itself
- ectopic pregnancy
Pain in the groin when moving in women is a sign of appendicitis.
Pulsating groin pain, which has a unilateral localization, is usually caused by an attack of appendicitis.
Another cause of pain of this nature is a rupture of a femoral artery aneurysm. As a result, a hematoma forms, spreading to all nearby tissues.
Throbbing pain in the groin in women may indicate a ruptured femoral artery aneurysm
Possible causes of pain that occurs in the groin area:
- Ectopic pregnancy. The pain appears suddenly and intensifies over several days. It has a cramping nature and may be accompanied by a disturbance in the patient’s general well-being - increased sweating, weakness, nausea.
- Intestinal pathologies. This includes both structural and functional disorders, such as intestinal obstruction, diverticulitis, cancer, flatulence and other conditions. Typical manifestations are vomiting, diarrhea, constipation, bloating, and an increase in general body temperature is also possible.
- Ovarian cyst or its complications. An increase in size of the cyst, its torsion or rupture leads to a sharp deterioration in the patient’s general well-being and causes severe pain in the groin area.
- Inflammatory process in the fallopian tubes or ovaries. With salpinginitis, adnexitis, parametritis and other similar conditions, a woman may feel acute pain in the groin, which intensifies with palpation and is accompanied by an increase in general body temperature.
- Stone in the kidney or ureter. The pain appears sharply and suddenly. Its duration can be from a few minutes to more than a day.
- Appendicitis. A characteristic feature is sharp pain on the right side when pressed. Inflammation of the appendix requires immediate hospitalization of the patient and provision of qualified assistance. Unpleasant sensations intensify while walking and can radiate to the rectal area.
Consequences of inguinal hernia surgery in elderly men
After surgery to remove a hernia in older men, the edges of the incision gradually heal, the doctor removes the stitches, and the patient gradually begins to increase physical activity. A scar in the peritoneal area remains a reminder of the surgical intervention.
But in rare cases, complications may occur after surgical treatment:
- When removing a sliding hernia by an insufficiently experienced specialist, there is a risk of damage to the spermatic cord or disruption of the integrity of the intestinal wall.
- Applying rough sutures can cause damage to the hip joint.
- Due to postoperative swelling, hydrocele of the testicle and enlargement of the scrotum may develop. This will lead to the need for repeated surgery.
- Infectious complications are a special form of nosocomial infection.
- Hematomas, the occurrence of which could not be prevented by applying ice immediately after surgery.
- Passive lifestyle of the patient during the rehabilitation period.
- Failure to follow the doctor’s recommendations or heavy lifting leads to divergence of the tightening seam and other complications.
Read material on the topic: Incontinence in older men: causes, diagnosis, treatment methods
Feeling of pain in the central part of the groin
The occurrence of pain in the midline of the abdomen, in its lower part, may indicate the presence of problems with such pelvic organs as the uterus, bladder, and rectum. It can be:
- Chronic and acute inflammatory diseases of the uterus and appendages, adhesions formed after surgical interventions. Inflammation of the appendages (fallopian tubes, ovaries and ligaments) is adnexitis or salpingoophoritis. The process can be either acute or chronic. There are unilateral salpingoophoritis (inflammatory process on one side only) and bilateral adnexitis (on both sides). In case of illness, hospital treatment is recommended.
- Benign or malignant tumor of the uterus and appendages. For example, uterine fibroids.
- Inflammation of the bladder (cystitis), which is caused by rectal bacteria entering the bladder. Accompanied by frequent urge to go to the toilet, sometimes false, and the discharge of blood along with urine. Inflammation of the rectum (proctitis) - it is characterized by chills, false urge to defecate due to constipation, and purulent discharge.
- Internal endometriosis II-III degree. A serious disease in which the endometrium grows uncontrollably not only in the uterine cavity, but also in other tissues and organs, causing an inflammatory process. The symptoms are initially very similar to premenstrual symptoms, but each time the pain becomes stronger, preventing the woman from leading her usual life, including sexual intercourse. In women of childbearing age, endometriosis is considered the most common cause of pain in the groin area.
- Symphysiolysis. With this pathology, the bones of the symphysis pubis diverge or become more mobile.
- Allen-Masters syndrome is a traumatic injury to the uterine ligaments. It occurs as a result of abortions, rapid labor, surgical interventions in the pelvic organs, as well as when the fetus is too large and is in a breech position. It is accompanied by venous stagnation, leading to varicose veins of the small pelvis, which can also cause pain. It often occurs in women who are forced to spend a lot of time on their feet during the day, as well as due to constant sexual dissatisfaction.
Features of surgery to remove an inguinal hernia in elderly men
1. Important points.
Inguinal hernia surgery in elderly men is aimed at removing the pathological formation. The surgeon places the internal organ in its natural place and removes the hernial sac.
It is not necessary to use general anesthesia for the operation. This type of anesthesia is necessary to ensure a calm state for children, adolescents and overly impressionable patients. To reduce pain sensitivity, an elderly man only needs local anesthesia.
The duration of the operation is affected by:
- General health of the patient.
During one operation, only unilateral protrusion can be removed; bilateral pathology is eliminated in two stages. At least six months must pass between two planned surgical interventions.
2. Methods for removing inguinal hernia in elderly men.
When choosing a method for removing a hernia formation, it is better to trust a specialist. The surgeon will analyze all the features of the course of the disease, take into account the health status of the elderly man, and choose the most appropriate and safe method of intervention.
Inguinal hernia surgery in older men is performed in two ways:
- Open.
An incision is made in a specific area of the peritoneum. The surgeon opens the hernial sac and checks the condition of the prolapsed organs. If no defects are identified, the organ is reset to its natural place. If pathological changes in organs are detected, the doctor makes the necessary correction. Next, the hernial sac is ligated, stitched, and removed. A special mesh is sewn into the peritoneum, which will support the muscles and prevent the re-formation of the hernial sac. - Laparoscopy. The operation is performed in the same sequence, but instead of an open incision on the body, the surgeon makes three punctures in the peritoneum. The condition of the internal organs and all surgical procedures are displayed on the monitor screen. This allows the doctor to control the correctness of his actions.
Both surgical methods are quite effective. Inguinal hernia surgery in elderly men follows standard clinical recommendations. The choice of method for performing the operation depends on the capabilities of the medical institution, the characteristics of the hernia pathology, and the patient’s condition.
Advantages of the methods:
- Laparoscopy – no scars are left on the body, the risk of infection is reduced, and it helps reduce the duration of the operation and the rehabilitation period. Patients return to a full life after two weeks.
- The open method allows you to operate under local anesthesia and remove hernia sacs of any size. It is considered a more affordable method, as it does not require the use of expensive equipment. Provided the patient follows all the doctor’s recommendations, relapse of the disease is completely excluded.
Disadvantages of methods:
- Laparoscopy is not recommended for elderly people and patients who have previously had lower abdominal surgery. This is a complex surgical procedure, so the doctor must be experienced and well trained. Not every specialist will undertake laparoscopic surgery if he does not have enough practical skills. This type of surgery is performed only under general anesthesia. A complication can be caused by the installation of a supporting mesh. It is not always possible to secure it properly, so recurrence of the hernial protrusion cannot be ruled out.
- The open method of surgical intervention often leads to the development of various postoperative complications. The rehabilitation period lasts at least three weeks. The patient can return to a full life only after three months.
Read material on the topic: Nails of older people: age-related changes and methods of care