All kinds of blood diseases (hemorrhagic) are a common phenomenon in modern medicine. About 50% of cases are thrombocytopenic purpura, the causes of which are numerous and not similar to each other. This disease affects the human body at any age.
What is thrombocytopenic purpura in children?
Thrombocytopenic purpura (TP), or Werlhoff's disease , is a blood clotting disorder characterized by a decrease in the number of platelets in the blood.
Platelets are cells in the blood that help stop bleeding. Their decrease leads to easy bruising, bleeding gums and internal bleeding.
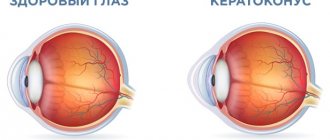
The term "thrombocytopenia" refers to a decrease in the number of platelets in the blood, and "purpura" refers to the presence of purple spots and petechiae on the skin (hemorrhages) caused by internal bleeding from small blood vessels.
The disease is caused by an immune reaction to your own platelets.
Diet for thrombocytopenic purpura
There is no special nutrition for Werlhof's disease. It is important that dishes are consumed lukewarm or cool. Natural vegetables for thrombocytopenic purpura, like fruits, are very useful, but they should not cause allergies. The list of recommended products includes:
- porridge – buckwheat, corn, oatmeal;
- fruits and vegetables in the form of juices - carrot, apple, beetroot, pomegranate, tomato;
- berries - currants, blackberries, raspberries;
- seafood;
- meat - beef.
The following should be excluded from the diet:
- salty foods;
- smoked meats;
- seasonings and spices;
- pickled vegetables;
- fast food products;
- carbonated drinks;
- coffee;
- alcohol.
Causes
Etiological factors
The exact cause of TP is unknown, so it is sometimes called idiopathic . The disease is not contagious, that is, a child cannot “catch” it while playing with other children with TP.
Often, a child may have a viral infection three weeks before developing TP. It is believed that the body, while creating antibodies against the virus, “accidentally” also produces an antibody that sticks to platelets.
The immune system identifies any cells with antibodies as foreign bodies and destroys them.
Helicobacter pylori infection is associated with autoimmune diseases, including TP; the pathology can also occur with HIV and other hematological disorders, including chronic lymphocytic leukemia, lymphogranulomatosis, and non-Hodgkin's lymphoma.
Genetic variations in several genes are found in some patients with LT and may increase the risk of developing abnormal immune responses. However, the contribution of these genetic changes to the development of immune thrombocytopenia is unclear.
There have been studies looking at some drugs that cause AFL . Some medications can cause changes in platelet function. At present, no direct link has been found to any specific drug that may cause AFL.
In newborns, LT can be caused by maternal antibodies transferred to fetal platelets. Differences in fetal and maternal platelet antigens can lead to the destruction of fetal platelets.
Predisposing factors for the development of chronic TP in children
They are:
- frequent and persistent bleeding observed six months before acute AFL;
- there is no connection between exacerbation and the impact of any provoking criteria;
- the patient has chronic foci of infection;
- development of TP in girls during puberty.
Etiology of the disease
In most cases, it is impossible to determine the causes of thrombocytopenic purpura, although scientists have been able to find out that genetic defects do not play a major role in its development. Sometimes it occurs against the background of hereditary pathologies associated with impaired production of thrombocytopoietins in the body or a decrease in enzymes included in the Krebs cycle, but these are isolated cases.
The most likely causes that can cause purpura, doctors include:
- disruptions in the functioning of the hematopoietic system caused by the development of aplastic anemia;
- tumor lesions of the bone marrow;
- the harmful effects of radiation on the human body, which causes disruption of myelopoiesis - the process of development and maturation of blood cells;
- a previous bacterial or viral infection (statistically, in 40% of cases Werlhof’s disease occurs precisely because of this);
- vascular replacement surgeries that could cause mechanical damage to platelets;
- pathological reaction of the body to the administration of gamma globulin;
- use of certain contraceptive drugs;
- chemotherapy for the treatment of cancer.
Sometimes the cause of the development of the disease in adults is collagenosis of an autoimmune nature, prolonged blood stagnation or pregnancy (this fact has been confirmed by few scientists and doctors, so it is rarely mentioned).
Classification
| Criterion | Characteristic | ||
| Development mechanism | Heteroimmune, occurs when the antigenic structure of platelets is modified due to the influence of certain factors (viruses, new antigens, semi-antigens), characterized by an acute course | Autoimmune, occurs when autoantibodies are produced that attack their own unchanged platelets; characterized by a chronic, relapsing course | |
| Period | Exacerbations (crisis) | Remissions | |
| Clinical: no hemorrhages, but platelet count is reduced | Clinical and hematological – there are no clinical and laboratory signs of platelet deficiency | ||
| Severity of pathology | Mild: bruising and petechiae, occasional minor nosebleeds, very minor disruption of daily life | Moderate – more serious damage to the skin and mucous membranes, more profuse nosebleeds; platelet count 55 – 105 x 10*9 /l | Severe – long and heavy bleeding, skin manifestations, platelet level 35 – 55 x 10*9 /l, posthemorrhagic anemia, symptoms that seriously affect the quality of life |
| Flow | Acute (less than six months) | Chronic (more than six months): with rare relapses or regularly recurring | |
Schamberg's disease (chronic pigmentary purpura hemosiderosis of the skin)
General recommendations 1) hypoallergenic diet - exclude allergenic foods (citrus fruits, chocolate, spicy foods, strong coffee and tea, fried and smoked foods, alcoholic drinks). 2) regimen - avoid heavy physical activity and injury in order to prevent damage to skin vessels
Therapeutic 1) systemic glucocorticosteroids (Prednisolone, Methylprednisolone) - eliminate the inflammatory process in blood vessels 2) antiplatelet agents (Acetylsalicylic acid) - prevent hemorrhages into the skin, increasing the strength of the vascular wall, eliminates vascular inflammation 3) angioprotectors (Escin, Methylethylpyridinol, Ascorbic acid + rutoside) – reduce the permeability of the vascular wall, preventing blood from leaving it (hemorrhage) 4) calcium and potassium preparations – strengthen the vascular wall
Purpura
is a symptom of a pathological condition called thrombocytopenia. It is associated with a reduced number of platelet cells in the peripheral blood.
Thrombocytopenia is manifested by various blood diseases and is accompanied by hemorrhagic blood syndrome of the petechial-bruise type, i.e. like purpura.
Symptoms
Manifestations of purpura in newborns
A baby should be suspected of having TP if petechiae appear throughout the body soon after birth and blood tests show severe thrombocytopenia. Clinical manifestations may range from limited or widespread cutaneous petechiae or skin bruising to excessive bleeding or intracranial hemorrhage.
Manifestations in children
A previously healthy child suddenly develops generalized petechiae. Parents often state that the child felt fine the day before, but is now covered in bruises and purple spots. Bleeding from the gums and mucous membranes often occurs, especially with deep thrombocytopenia. There may be a previous viral infection 1-4 weeks before the onset of TP. Splenomegaly, lymphadenopathy (enlarged spleen and lymph nodes, respectively), bone pain and pallor are rare.
The presence of abnormal findings, such as hepatosplenomegaly (enlarged liver and spleen), bone or joint pain, or severe lymphadenopathy, indicates other diseases (eg, leukemia).
Manifestations in adults
In adults, chronic TP is often observed, which develops slowly.
Symptoms include:
- petechiae;
- bruising;
- bleeding from the nose and gums;
- black blisters in the mouth;
- fatigue;
- heavy menstrual periods in women.
Rarely, the following symptoms may occur:
- hemorrhages in the retina and brain;
- bleeding from the ears;
- blood in urine;
- bleeding in the intestines.
Clinical picture
Patient complaints are related to changes in the appearance of the skin.
Purpura pigmentosa progressive of Schamberg
It is characterized by the appearance on the lower extremities of asymmetrical, irregularly located plaques and spots of a brownish-red hue. The lesions persist for many years, gradually enlarging and becoming darker in color. This type of lesion is also called petechial, it occurs due to pinpoint hemorrhages from inflamed capillaries. After an accidental injury or blow, new rashes appear on the skin - this is the so-called Koebner phenomenon.
Eczema-like form
Reminiscent of Schamberg's disease, but more common in mature men. The lesions are located on the thighs, torso, and arms and may be accompanied by itching. The disease is recurrent and can disappear or worsen spontaneously. With itchy purpura, the lesions are larger and are accompanied by severe skin itching. The skin swells, turns red, and blisters and crusts appear on it.
Eczema-like Doukas-Kapetanakis purpura
Chronic pigmentary purpura
A distinctive feature is the characteristic speckled color. Lesions are more often localized on the legs, and itchy purpura is characterized by more generalized skin involvement.
Chronic pigmented purpuric dermatosis
Lichen aureus
In lichen aureus, a single skin lesion or a limited group of golden-brown lesions is observed. They can be located on any part of the body, but usually affect the legs symmetrically. Sometimes there is skin itching. Unlike other forms of pigmented purpura, in this variant the lesions are sometimes located within an area of the skin supplied by a single artery or innervated by a single nerve trunk (dermatome).
Majocchi disease
It is characterized by small ring-shaped plaques containing dilated vessels - telangiectasia; in the center of the plaques there are small foci of skin atrophy. They are located mainly on the legs, less often on the torso and arms. Mostly girls and young women are affected. The disease has a long, relapsing course, but over time it may disappear, and therefore treatment for this form is often not prescribed.
Lichenoid purpura
It resembles Schamberg's disease, but in addition there are red-brown or flesh-colored scaly raised areas (papules) and nodules. The pathology does not occur in children.
Purpura pigmentosa during pregnancy does not pose a danger to the baby. After childbirth, its manifestations may spontaneously disappear, so special treatment is not required at this time.
Diagnostics
To diagnose FL, you need to rule out other possible causes of bleeding and low platelet counts, such as an underlying medical condition or medications your child may be taking.
The specialist will need to take a medical history, perform a physical examination, and perform several laboratory tests.
Complete blood count
This test is used to determine the number of blood cells, including platelets, in a sample. In LT, the white blood cell and red blood cell counts are usually normal, but the platelet count is decreased.
Blood smear examination
This method is often used to confirm platelet levels found on a complete blood count. The blood sample is placed on a slide and examined under a microscope.
Bone marrow examination
This test helps determine the cause of a low platelet count, although some hematologists do not recommend this test for children with AFL.
In patients with LT, the bone marrow will be normal because the low platelet count is due to the destruction of these cells in the bloodstream and spleen, not due to abnormalities in the bone marrow.
Other studies
Blood testing for HIV should be carried out in risk groups, especially among sexually active adolescents. A direct antiglobulin test should be done if there is unexplained anemia to rule out Evans syndrome (autoimmune hemolytic anemia and thrombocytopenia).
Chronic pigmentary purpura, as the cause of the appearance of a scattering of spots on the skin
Pigmentary purpuric dermatosis, or chronic purpura pigmentosa, is a group of skin diseases with very characteristic external manifestations. They are accompanied by the release of red blood cells from the vessels and a significant deposition of erythrocyte pigment - hemosiderin - in the skin. The cause of these diseases is unknown.
There are several types of pathology:
- Schamberg's disease - progressive pigmentary dermatosis;
- ring-shaped telangiectasia (Majocca's disease);
- lichen aureus;
- itchy purpura;
- eczema-like form of Doukas-Kapetanakis;
- pigmented purpuric lichenoid dermatosis of Gougerot and Bloom.
Many doctors consider the itchy, eczema-like purpura to be a variant of Schamberg's disease.
All of the listed dermatoses have similar treatment and prognosis, as well as a similar histological (microscopic) picture. Chronic pigmentary purpura refers to dermal angiitis, that is, inflamed vessels are located in the middle layer of the skin.
Treatment
The goal of care for a patient with AFL is to increase the platelet count to a safe level. There is no cure for TP, and relapses can occur years after seemingly successful medical or surgical treatment.
Drug therapy
Steroids
The use of steroids is the mainstay of treatment for this disorder. This group of drugs helps suppress the immune system. The route of administration and dosage is determined by the platelet count and the presence of any active bleeding. Intravenous infusions of methylprednisolone or dexamethasone may be given in emergency situations. For milder forms, oral forms of prednisolone can be used.
As the platelet count normalizes, the dosage of steroids is gradually reduced. Almost 60%-90% of patients experience relapses during dosage reduction or discontinuation. Long-term use of steroids is not recommended as it can cause various side effects.
Immunosuppressants
Immunosuppressants such as azathioprine and mycophenolate mofetil are becoming increasingly popular due to their effectiveness in treating LT. For chronic and persistent pathologies, when the immune pathogenesis has already been established, a chemotherapeutic agent, vincristine, can be used. However, the drug causes serious side effects and should therefore be used only with caution in the treatment of TP. This is especially important for children, as they are more vulnerable.
Immunoglobulin
This medicine contains antibodies that are a product of human blood, meaning that the antibodies were collected from multiple donors. It is not known exactly how the drug works to treat TP, but the additional antibodies are thought to stop white blood cells from destroying platelets. The drug works quite quickly, usually within a few days. Unfortunately, the effect does not last long (only a few weeks). Medicine is usually given before surgery, or if there is significant bleeding and platelet levels need to be increased urgently.
Rituximab
This drug was originally used to treat cancer, but it has also been used in the treatment of LT for almost 20 years. Like steroids, it stops the immune system from destroying platelets, but has fewer side effects than steroids. This is an artificially created antibody that affects white blood cells. It is not made from human donor blood. Effects are usually achieved within a few weeks, although some people respond to treatment after several months.
Thrombopoietin receptor agonists Romiplostim and Eltrombopag
These two drugs have become available in the last few years. Thrombopoietin receptors are found on the surface of the cells that make platelets in the bone marrow; these drugs use these receptors to tell the cell to make more platelets. The drugs can only be used in combination with other treatment methods. Romiplostim is used as a subcutaneous injection, usually once a week. Eltrombopag comes in tablet form that you take once a day. The substance is not absorbed by the intestines without calcium, so it is necessary to eat foods high in calcium within four hours before or after taking the drug.
Therapy should be continued until clinical and laboratory manifestations disappear; this may take several years. Medicines do not cure the underlying problem; they simply encourage the body to produce more platelets to replace those that are destroyed.
Treatment of Helicobacter Pylori
Some children with LT have a stomach infection called Helicobacter pylori. Sometimes treating her with antibiotics and antacids for two weeks can cure or improve TP. The increase in platelets after treatment of an infection is not always permanent, but the therapy is relatively safe and can therefore be recommended for children.
Dapsone
It is an antibacterial agent but can also be used to treat TP. It is not known exactly how the drug works, but it appears to reduce the autoimmune process, which may stop the immune system from attacking platelets. It is taken as a tablet once a day and has several side effects.
Tranexamic acid
This drug helps blood clots last longer once they form. The clots are more stable than usual and more persistent. The drug does not treat AFL, but may be useful for bleeding while the platelet count is low. The tablet is taken 3 or 4 times a day. There are contraindications.
Why shouldn't platelet transfusions be given?
The platelets produced by the bone marrow are healthy. Their low number is due to the immune system attacking them. If a patient receives platelets from a donor, they will be destroyed by your immune system. Platelet transfusions are useful as emergency treatment if there is severe bleeding, as they will help form a clot, but this method is not effective in preventing bleeding long-term.
Surgery
Because platelets are mostly destroyed while they are in the spleen, removing it (splenectomy) can cure the pathology. Splenectomy has been used to treat TP for decades and offers the best chance of cure. Of every three people who have surgery, two will not need further treatment.
Splenectomy results in a lifelong increased risk of sepsis from bacterial infection.
In children, the risk of bacterial sepsis after splenectomy is estimated at 1-2%. Many pediatricians recommend delaying surgery until children are 5 years old.
If a splenectomy is planned, the child should be vaccinated against Haemophilus influenzae 14 days before surgery. Also, children over two years of age must be vaccinated against Streptococcus pneumoniae and meningococcal infection.
Diet
Diet plays a role in the treatment of TP. Eating the right foods will help your child feel better and more energetic.
Some nutrients, such as vitamin K and calcium, have natural components that are important for blood clotting. They are rich in dark leafy greens (spinach). Dairy products contain a lot of calcium, but experts do not recommend consuming it in excess, as it can worsen the symptoms of autoimmune diseases. Vitamin D supplementation also plays a role in boosting the immune system in LT.
Tips for organizing meals are as follows:
- If possible, it is recommended to consume only natural products;
- animal and artificial fats should be replaced with vegetable ones;
- it is necessary to limit the consumption of red meat;
- Potentially antiplatelet fruits such as berries, tomatoes and grapes should be avoided.
Purpura pigmentosa chronic
Purpura pigmentosa chronic
The disease is always chronic, lasts for quite a long time and is essentially an inflammatory process in the walls of small capillaries of the skin and internal organs. The smallest capillaries in the skin are affected - those that come closest to its surface. Depending on the signs of the disease and the predominance of one or another type of rash, it is customary to distinguish several types of pigmentary chronic purpura:
1) petechial type with a predominance of multiple small subcutaneous hemorrhages;
2) telangiectatic type, which is based on cystic dilation of individual areas of the subcutaneous capillaries;
3) lichenoid type;
4) eczematoid type, reminiscent of skin eczema.
Petechial type of disease. On the skin of a patient with this disease, a large number of tiny areas of hemorrhage appear, which have a point size. These spots are purely hemorrhages; they are never accompanied by swelling of the skin. Subsequently, the blood released from the capillaries undergoes a series of transformations, as a result of which the spots acquire a brownish-yellow color, which is given to them by a special substance formed from hemoglobin iron - hemosiderin. The spots can have a wide variety of sizes and shapes. Most often, these lesions occur in the lower extremities. The patient does not experience any unpleasant sensations at all. It is interesting to note that the disease is detected almost only in males. The development of this type of purpura in women is extremely rare.
Telangiectatic type. In most cases, the cutaneous manifestations of the disease are a kind of medallion spots. They have this appearance due to the fact that their center is mainly formed from areas of small cystic expansions of capillaries, and along the periphery there are spots of hemorrhages, described above in the paragraph “Petechial type of disease”.
Lichenoid type. It is named so because with this type of disease, small nodules are located on the patient’s body in large numbers in almost all places, which have a shiny surface and the color of practically healthy skin. Such formations are most often not present separately, but are combined with multiple areas of small subcutaneous hemorrhages, brownish-yellow spots containing hemosiderin, and sometimes small areas of cystic-dilated capillaries may appear.
Eczematoid type. In fact, with this form of pathology, the lesions on the skin have the same appearance as with the petechial variety: fresh areas of hemorrhage in combination with old ones containing hemosiderin. However, with the eczematoid type, these lesions are combined with manifestations characteristic of eczema: areas of edema, nodules, blisters, small crusts. All this is accompanied by itching of the skin in the area of pathological formations, which ultimately brings the patient to the clinic.
Recommendations for parents
If a child has TP, parents need to learn how to best prevent injury and bleeding:
- For a small child, make the environment as safe as possible. Padding the bed with soft materials, helmets and protective clothing are necessary when the platelet count is low;
- contact sports, cycling and rough play should be limited;
- Avoid medications containing aspirin because they may interfere with the body's ability to control bleeding;
- Until recovery from illness, the child should not receive vaccinations, especially those containing live attenuated viruses. These include measles, mumps, rubella, and oral polio vaccines. In addition, you should not inject into a muscle.
Prevention
- The cause of the disease is unknown, so preventive measures are aimed at maintaining overall cardiovascular health:
- avoid hypothermia, excessive tanning and injury;
- timely treat vascular diseases such as varicose veins, hypertension, diabetes;
- avoid putting unnecessary strain on your legs;
- lead a healthy lifestyle.
If signs of the disease appear, it is recommended to consult a dermatologist. Additional consultations with an allergist, immunologist, hematologist, vascular surgeon, endocrinologist, cardiologist and other specialists may be needed to determine risk factors for the disease and eliminate them.
How to treat?
It is necessary to treat the disease (especially in advanced cases) in a hospital setting, because the first task of doctors is to stop the processes of platelet destruction and increase their concentration in the blood.
Drug treatment begins with eliminating the symptoms of the disease - local (skin) and general bleeding; for this purpose, drugs that have a hemostatic effect (Ascorutin, Thrombin) are used. Subsequently, the patient is prescribed glucocorticoids (“Prednisolone”) and immunoglobulins. If there is no positive effect from drug therapy, doctors prescribe surgical treatment, in the form of splenectomy - removal of the spleen. The method is used in extremely rare cases when there is a threat of extensive hemorrhage in the brain.
If possible (if the pathological process is slow), the patient is prescribed several sessions of plasmapheresis (helps cleanse the blood of antibodies to platelets). A transfusion (infusion) of platelets from a donor is also possible.
Considering that thrombocytopenic purpura in children is not uncommon, the responsibility for its successful treatment lies with the parents, who should regularly show the child to the doctor and teach him a healthy lifestyle (hardening, physical activity and proper nutrition will significantly reduce the likelihood of a relapse).
Werlhof's disease is a very serious pathology of the circulatory system, which in some cases can cause the death of the patient, however, with high-quality and timely treatment, the prognosis for most patients will be favorable.
Prevention
The appearance of purpura in childhood and adolescence is the most common occurrence, so it is necessary to pay special attention to the health of children who have suffered severe infectious diseases. The most competent decision of parents should be observation by a hematologist for several years.
Preventive measures regarding relapses come down to maximum avoidance of viral infections and prevention of bacterial diseases.
It is necessary to be exposed to direct sunlight as little as possible, and it is better to completely eliminate such situations.
In addition, preventive measures consist of eliminating foci of infection as much as possible: caries, tonsillitis, etc.
Possible complications
There is an increased risk of heavy hemorrhage in the gastrointestinal tract. The chronic form of the disease is also a cause of hemorrhagic stroke.
Damage to the mucous membranes causes retinal detachment. Thrombocytopenic purpura, in the absence of drug therapy and timely measures to eliminate it, threatens the patient with death or disability.
To prevent the development of complications, it is necessary to detect the symptoms of the disease in time and begin treatment.
Factors influencing the onset of the disease in adults
In adult patients, Moschkowitz disease is often of unknown origin. Known causes typically include:
- The influence of immunosuppressive drugs (for example, Cyclosporine) and antitumor chemotherapeutic drugs (Mitomycin).
- Presence of pregnancy (often indistinguishable from the development of severe eclampsia).
- Development of hemorrhagic colitis resulting from exposure to E. coli.
Predisposing factors for many patients are a congenital or acquired form of deficiency of special enzymes in the blood plasma, which should break down and eliminate abnormal multimers that can cause platelet clots. Now we will talk about the factors of manifestation of the pathology in question and the variants of its symptoms.
Further forecast
In isolated cases, idiopathic thrombocytopenic chronic purpura leads to death due to hemorrhage in the patient's brain.
An unfavorable prognosis is also observed in situations where surgery to remove the spleen does not produce a noticeable result. If the patient does not have complications such as cerebral hemorrhage, gastrointestinal bleeding or anemia, the prognosis is generally optimistic. But it is worth noting that in some situations the disease becomes protracted.
In the vast majority of cases, patients with thrombocytopenic purpura return to normal life. With timely treatment, the probability of recovery is approximately 75–90%. In this case, the patient is recommended to periodically visit a hematologist. He should not take drugs that affect the aggregation properties of blood platelets. Caution should be exercised when vaccinating children who have previously been treated for thrombocytopenic purpura. The time spent in direct sunlight is strictly limited.
Contraindications
It is prohibited to use the medical drug in question in the development of hemorrhagic diathesis, against the background of bleeding, high blood pressure, streptococcal sepsis, stomach ulcers, septic endocarditis, severe forms of diabetes. The drug should be prescribed with caution in case of severe kidney damage and in the case of tuberculosis in the active phase.
"Heparin"
Direct anticoagulant, belongs to the group of medium molecular heparins, slows down the formation of fibrin. The price of Heparin will be presented below.
Indications: thrombosis, thromboembolism (prevention and treatment), prevention of blood coagulation (in cardiovascular surgery), coronary thrombosis, disseminated intravascular coagulation, postoperative period in patients with a history of thromboembolism. Prevention of blood clotting during operations using extracorporeal circulatory methods.
Manifestations
Werlhof's disease can be recognized by the following signs:
- hemorrhagic rash of red or purple color on the outer layer of the dermis, mucous membranes;
- blood clots in saliva and urine;
- increased bleeding time with minor skin injuries;
- tachycardia;
- slight dizziness;
- vomiting with blood.
The initial stage of the disease can be detected by the results of a blood test.
Symptoms
With this disease, the appearance of a spotted-bruised rash on the skin and hemorrhages in the mucous membranes is noted. Elements of the rash can be of varying sizes, externally resemble bruises, are painless when pressed, are located asymmetrically, and can appear without trauma, most often at night. The color of the rash varies: from bluish to yellow.
Hemorrhages can occur not only on the mucous membranes of the oral cavity and tonsils, but also in the eardrum, vitreous body, sclera and fundus of the eye. Rarely, cerebral hemorrhage is possible, which significantly worsens the patient’s condition. This is preceded by the appearance of dizziness and headache, as well as bleeding in other organs.
When the platelet level decreases to less than 50x10 9 /l, nosebleeds and gum bleeding appear, which are more dangerous when a tooth is removed. In this case, bleeding occurs immediately and usually does not resume after it stops. In teenage girls with thrombocytopenic purpura, uterine bleeding during menstruation poses a certain danger.
Other skin changes
A common symptom of a violation of certain liver functions as a result of liver disease is allergic dermatitis, which occurs due to a violation of the detoxification function of the liver. Most often, skin manifestations of dermatitis are bright red spots and plaques; sometimes pustular dermatitis occurs with rashes (folliculitis, furunculosis).
Manifestations of secondary hormonal imbalance in liver diseases are atrophic stripes (stretch marks or stretch marks) located on the buttocks, thighs, and lower abdomen.
The mechanism of occurrence of Werlhof's disease
Depending on the cyclical course of the disease, thrombocytopenic purpura comes in several forms: acute, recurrent, chronic.
For example, if hemorrhagic diathesis occurs in an acute form, the platelet level remains below the optimal 150x109/l for six months from the onset of the disease. Chronic thrombocytopenic purpura is said to occur when the process of normalizing platelet levels is delayed for a long time: more than six months. The presence of recurrent thrombocytopenic purpura in a person is indicated by a repeated decrease in the level of blood platelets after its recovery.
Thrombocytopenic purpura is also called Werlhof's disease.
Indications for use of "Streptokinase"
A drug is prescribed to treat embolism (that is, to eliminate blockage) of the pulmonary arteries and its branches. The drug is also used to treat thrombosis (when blood clots form in the vessels), when the peripheral arteries are blocked. It is also advisable to use it against the background of the development of venous thrombosis of deep ducts located close to the skin. The presented medication is no less effective in the treatment of acute myocardial infarction in the first twelve hours and in cases of damage to vascular networks.
This remedy can activate the fibrinolytic enzyme system, which is capable of dissolving clots and breaking down the fibrin contained in blood clots in the vein. Actually, thanks to this, blood clots that clog the vessels dissolve (manifestation of thrombolysis).
Kinds
TP is classified according to etiological, pathogenetic and clinical features. The classification reflects the cause of the disease and helps to find adequate treatment.
Pathology happens:
- idiopathic thrombocytopenic purpura (Werlhof's disease);
- symptomatic thrombocytopenia (Werlhoff symptom complex).
TP is also classified according to the nature of its course:
- Acute form. Usually seen in children. Lasts up to six months. After normalization of platelets, relapses are not observed.
- Chronic form. Lasts more than six months and is more common in adults. Refers to recurrent forms. Repeats cyclically. The platelet level is unstable. After normalization, platelet deficiency occurs.
Doctors use another classification of TP. It divides pathology into several immune forms:
- Isoimmune. It is usually observed after blood transfusions. There is also a congenital pathology. Develops due to an immune conflict with platelet antigens that occurs between the mother and fetus. The peculiarity of this clinical form is regular relapses.
- Autoimmune. It appears due to the fact that the body forms a lot of platelet antibodies to its own platelets.
- Heteroimmune. This form is usually provoked by taking medications. In this case, the individual sensitivity of the child is of great importance. Due to intolerance to certain substances contained in the drugs, children develop specific symptoms - purple rashes. They arise as a result of numerous hemorrhages.
- Transimmune. The development of this form is preceded by an antigenic conflict and the accumulation of antiplatelet antibodies during pregnancy. These antibodies, entering the child’s body through the placental bloodstream, cause the development of hemorrhagic syndrome.
"Streptokinase"
The active ingredient of this medication is streptokinase. The medicine is produced in the form of a powder, which is the main one for preparing an injection intended for intravenous drip, and sometimes for intra-arterial administration. The product is produced in bottles with different dosages: starting from 100,000 to 1,500,000 IU (units of measuring the amount of substance).