Every day a person puts his delicate mucous membrane of the gastrointestinal tract at risk.
Overly spicy or hard foods that are not completely ground, aggressive substances in food and medications, alcohol, pathogens and other irritants can severely damage the lining of the digestive tract. Such negative effects can lead to the formation of erosions and ulcers. When damage to the inner surface of the stomach occurs, gastritis is diagnosed, and when the duodenal mucosa (duodenum) is affected, duodenitis is diagnosed. If the inflammatory process is concentrated only in the initial (bulbar, bulbous) part of the duodenum, gastroenterologists indicate the occurrence of bulbitis (bulboduodenitis). Bulbit is one of the most common types of duodenitis.
Signs of the disease
The following symptoms are characteristic of erosive bulbitis:
- pain in the epigastric region ("epigastric area"), occurring 1.5-2 hours after eating and at night (therefore they are also called "hunger pains");
- heartburn;
- belching with a sour or bitter taste (air or stomach contents);
- constipation;
- nausea and vomiting mixed with bile (yellowish vomit);
- flatulence;
- feeling of fullness in the stomach.
Pain in the epigastric region can radiate to the left hypochondrium and periumbilical region. As a rule, they disappear or decrease after drinking milk or a small amount of food. Also, pain subsides after vomiting.
Important: when the first signs of the disease appear, you should immediately consult a doctor.
Usually, to establish a diagnosis, FEGDS is performed - fibrogastroduodenoscopy. If erosive bulbitis is not treated on time, it can develop into duodenal ulcer. You can learn about how this complication looks on FEGDS from the video at the end of the article.
What is it - chronic bulbitis?
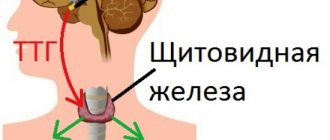
The appearance of the pathology is associated with one of the forms of duodenitis. This disease in medicine is designated by ICD-10 and has code K29.8. The inflammatory process in this disease occurs in the bulb, which is located in the duodenum. Chronic bulbitis is often observed with gastritis. It can be difficult to detect the disease due to similar symptoms. Therefore, when diagnosing the chronic form, doctors use the designation – stomach bulbitis.
The danger of the disease lies in the pancreatic bulb. Its function is based on the digestive process. When foods enter the stomach, they are digested under the influence of hydrochloric acid. Gastric juice should not enter the intestines. Otherwise, the microflora will be destroyed.
The bulb is responsible for neutralizing concentrated gastric juice. During the movement of the food coma through the duodenum, the secretion created creates a safe microflora for the further movement of products through the intestines. A situation occurs when undigested food carries hydrochloric acid with it. Such a bolus of food enters the intestines, and its microflora is disrupted.
During the passage of digested products through the bulb (bulb), gastric juice is neutralized. When the integrity of the gland shell is compromised, the penetration of bacteria or viruses into it creates inflammatory processes. As a result, the functioning of the entire digestion is disrupted. Chronic bulbitis has superficial, erosive and catarrhal forms.
The disease is more complicated in the erosive type. Chronic bulbitis has a complication in the form of duodenal ulcer. During the pathology, damage to the bulb occurs, which is expressed in specific symptoms.
Reasons for the development of erosions in the duodenal bulb
The main factor provoking the occurrence of erosive bulbitis is increased acidity of gastric juice. In turn, this condition is usually caused by Helicobacter gastritis and stomach ulcers. The disease can also be caused by the following reasons:
- giardiasis,
- helminthic infestation (enterobiasis, ascariasis, etc.),
- acute intestinal infection (dysentery, salmonellosis),
- unhealthy diet (consumption of foods that irritate the mucous membranes of the gastrointestinal tract - spicy, fried, alcoholic drinks),
- foreign bodies trapped in the duodenal bulb,
- poisoning with chemicals (alkalis, acids),
- long-term use of anti-inflammatory drugs (hormones and non-steroidal drugs).
With erosive bulbitis, surface defects appear on the mucous membrane of the duodenal bulb that do not affect the muscular wall of the organ.
The causes of acute erosive bulbitis are most often gastrointestinal infections, anti-inflammatory drugs and aggressive chemicals. Other factors usually cause chronic inflammation that progresses slowly.
Diagnosis of chronic bulbitis
In order to make an accurate diagnosis, it is necessary to carry out a comprehensive examination, which will include laboratory and instrumental methods.
Diagnosis and treatment for diseases of this nature are carried out by a gastroenterologist.
Establishing a diagnosis involves the following diagnostic procedures:
- A complete blood count can reveal the presence of anemia, which often occurs as a result of internal bleeding.
- Blood chemistry. In this case, decreased levels of protein and iron may be detected.
- FGDS is the most effective because it allows you to examine the entire duodenal bulb and determine the extent of damage. This will help the doctor determine the form of the disease. The examination is carried out using an endoscope.
- X-ray examination - this diagnostic method is the most ineffective, since it does not allow assessing the condition of the mucous membrane. X-rays are used only if there are any contraindications to endoscopic examination.
The following methods are used as additional diagnostics:
- external examination of the patient and determination of the intensity of symptoms;
- laboratory tests of gastric juice;
- breath test system (helps detect the presence of pathogenic microorganisms).
After the results of all examinations are received, the doctor prescribes appropriate treatment.
Treatment of erosive-ulcerative bulbitis
To treat erosions in the duodenal bulb, medications from the following groups are used:
- antacids,
- proton pump inhibitors,
- antibiotics (in the presence of Helicobacter pylori infection),
- blockers of H2 receptors for histamine in the stomach.
Antibiotics act as etiotropic treatment, as they eliminate the cause of the disease - the Helicobacter bacterium. Antacids protect the gastric mucosa and bulbs from the action of acidic contents, and proton pump inhibitors and H2 receptor blockers reduce the production of hydrochloric acid in the stomach. To speed up the healing of erosions, sea buckthorn oil is used.
Medical nutrition
With erosive bulbitis of the duodenum, diet is a necessary condition for successful treatment. During the acute period, the following should be excluded from the diet:
- spicy, hot, fatty;
- fried and salted;
- marinades;
- smoked meats;
- rich broths;
- products with a high content of extractive substances (onions, garlic, etc.);
- sour fruits and juices;
- carbonated drinks;
- alcohol.
During the treatment of erosive bulbitis, the diet can include vegetable and cereal soups, semi-liquid porridges, compotes, and jelly. It is better to choose low-fat varieties of meat products and fish and remove all visible fat before cooking. It is advisable to eat food at the same time, preferably more often (5-6 times), but little by little. At first, all dishes must be rubbed through a sieve or crushed in a blender and consumed warm. Cold and hot foods can additionally irritate the mucous membrane of the bulb and disrupt intestinal motility.
Treatment of chronic bulbitis with medication
It is necessary to treat the chronic form of bulbitis using complex therapy.
In this case, both medicinal and non-medicinal means, as well as traditional medicine methods, are used.
The choice of medications for this disease directly depends on the factor that provoked the pathological process.
When treating Helicobacter pylori infection, the doctor prescribes eradication therapy, which involves eliminating the Helicobacter pylori bacterium.
In this case, antibiotics and drugs that reduce the level of acidity in the stomach are used.
The duration of treatment and dosage of certain drugs is determined by the attending physician.
In most cases, anti-inflammatory drugs are prescribed to help restore the normal state of the mucous membrane.
To eliminate pain, it is strictly forbidden to use non-steroidal anti-inflammatory drugs, since they have a damaging effect on the mucous membrane.
As painkillers, the doctor may prescribe antispasmodic drugs such as Duspatolin and Trimedat.
To reduce acidity, antacid drugs are used, for example Maalox, Reni, Almagel.
Of the non-drug methods, physical therapy is considered the most effective.
Traditional treatment
In the case of erosive bulbitis, treatment with folk remedies often gives good results, especially against the background of therapy prescribed by a doctor. Here are several effective traditional medicine recipes for the treatment of erosions of the duodenal bulb.
Infusion of chamomile and Icelandic moss
This remedy quickly relieves inflammation and intestinal spasms. To prepare, take 2 tablespoons of plants, mix and pour boiling water (0.5 liters). Boil the plant material for 30 minutes in a water bath, cool and filter. Take ½ glass 3 times a day before meals (30 minutes before).
Chamomile decoction soothes the inner lining of the duodenal bulb, relieves inflammation and spasm
Oak bark infusion
For erosive bulbitis, treatment with oak bark infusion can reduce the effect of digestive juices on the mucous membrane of the bulb. Place 1 teaspoon of crushed bark in a thermos and add 200 ml of boiling water, close and shake. Leave to infuse overnight. Drink 1 tablespoon before each meal (about 5 times).
Infusion of marshmallow root and flax seeds
Equal quantities of flax seed and marshmallow roots are crushed and mixed. You can add the same amount of Icelandic moss. Place 2 tablespoons of the mixture in cold water (2 glasses), leave overnight, bring to a boil in the morning and boil for 5-6 minutes. Leave for another 2 hours, take 100-150 ml 3 times a day shortly before meals.
Flax seed jelly
Wash 2 tablespoons of flaxseed in cold water and brew 1 cup of boiling water, continue to boil the product until the mass takes on a viscous jelly-like consistency. The mixture is cooled slightly; for a better effect, you can add a few drops of propolis. Then you should divide the decoction into 3 equal parts and take them in the morning on an empty stomach, before lunch and dinner. Flaxseed jelly envelops the walls of the stomach and duodenum and accelerates the healing of erosions.
Important: before treating erosive bulbitis using traditional recipes, you should consult a doctor. Some of these remedies may not be right for you.
One of the unpleasant types of inflammation of the duodenum is bulbitis. Its section is adjacent to the walls of the stomach and has an acute or chronic nature of the disease.
This is an inflammatory disease that can be caused by a number of provoking factors. The treatment is complex and requires special nutrition for bulbitis.
Since this disease is common with gastritis, a special diet is prescribed, which is aimed at eliminating, and sometimes completely eliminating, all symptoms.
Diagnostics
The initial diagnosis is carried out in the doctor's office. This is a visual inspection of the abdominal area and palpation. The doctor makes a preliminary conclusion based on the clinical picture.
To confirm the diagnosis, the patient is given a referral for instrumental diagnostic methods and laboratory tests.
Only after a comprehensive diagnosis does the doctor make a final diagnosis of bulbitis and prescribe treatment.
Diagnostics includes the following instrumental techniques and analyses:
- manometry. The study is carried out to measure pressure during contraction of the stomach;
- FGDS - used to determine swelling, bleeding and hemorrhage in the esophagus, stomach and duodenum;
- fractional duodenal intubation;
- stool analysis for the detection of Helicobacter pylori;
- pH-metry and electrogastroenterography of the gastrointestinal tract are performed.
How to recognize the disease
Symptoms of the disease depend on the degree and nature of its development. The main symptom is pain, and its intensity depends on the degree of development of the disease.
With catarrhal bulbitis of the stomach, minor pain is noted, and with erosive it is sharp and severe.
An inflammatory process occurs in the duodenal bulb, so accompanying symptoms are noted that are also characteristic of gastritis - nausea, vomiting, heartburn, bitter belching and active loss of appetite.
If bulbitis is not treated, it will further develop, turning into a more severe form. The erosive process is characterized by the presence of ulcerative lesions that can damage blood vessels.
As a result, internal bleeding may occur, which is accompanied by weakness, vomiting with bloody spots, and a feeling of severe and acute pain.
And severe blood loss can lead to hemorrhagic shock.
In acute bulbitis, an increase in body temperature, nausea, vomiting and intestinal disorders are observed. It occurs due to a toxic food infection.
Due to a lack of enzymes for processing food, problems occur in the stomach and the entire digestive system. This leads to flatulence, dysbacteriosis and stool disorders.
Symptoms of bulbitis
The most common sign of the disease is pain in the epigastric region.
The pain is aching in nature, sometimes patients report sharp pains and stabbing spasms. Symptoms of bulbitis depend on the clinical type. In this way, doctors are able to promptly determine the type of disease and begin treatment before diagnosis in order to prevent deterioration and complications.
However, there are common symptoms of bulbitis in adults and children. They do not differ depending on age categories.
Clinical signs:
- discomfort in the upper part of the peritoneum;
- nausea;
- vomiting, in severe cases with blood;
- belching after eating or between meals;
- during an exacerbation, body temperature rises;
- diarrhea begins and flatulence worries.
Sometimes bulbitis occurs in a hidden form. Many patients are unaware of the existence of the disease, and some symptoms are similar to diseases of the gastrointestinal tract, so it is difficult to independently differentiate the pathology.
Causes of the disease
Bulbit occurs due to Helicobacter pylori infection. With increased acidity, a favorable environment is created for the colonization of bacteria of this infection.
They feel comfortable in this environment, creating a protective alkaline barrier around themselves.
Substances that cause an inflammatory process are produced, which destroys the mucous membrane.
As a result, erosive bulbitis develops, and if left untreated, ulcers appear. Only diet can alleviate symptoms and improve digestion.
This disease can occur for anatomical reasons. In this case, during embryonic development, the mesentery remains at the duodenum.
It looks like a loop in which highly acidic food coming from the stomach stagnates. Under these conditions, bacteria actively develop, which leads to the destruction of the mucous membrane.
One solution to this problem is a special diet.
Associated causes of the disease:
- Decreased immune system.
- Genetics.
- Poor nutrition.
- Other concomitant serious illnesses.
Prevention
Measures to prevent pathology at different stages have their own characteristics. To prevent erosive bulbitis, it is necessary to adhere to a healthy lifestyle, reduce the influence of stress factors, refuse self-medication, take a differentiated approach to the treatment of associated diseases, and observe sanitary and hygienic standards.
Secondary prevention comes down to timely treatment of inflammatory processes of the digestive tract in compliance with doses and treatment regimens.
At the last stage, the patient is rehabilitated in order to prevent relapse of erosion and the development of complications. Much work in this direction is carried out by gastroenterologists in outpatient clinics and specialists from sanatorium-type institutions.
Important tips when creating a menu
When suffering from bulbitis, it is important to eat properly and safely. The diet for bulbitis and gastritis should include all useful elements, vitamins and substances.
But all food should be gentle and should not irritate the mucous membrane of the stomach and duodenum. To achieve the desired effect, you need to adjust the menu.
- Meals should be frequent (at least 5 times a day), and portions should be small.
- The diet provides for breaks between meals of no more than 3 hours.
- In order not to burden the intestines and stomach, they switch to fractional meals.
- All dishes on the menu are steamed, boiled, baked or stewed.
- Food should be gentle, this also applies to temperature conditions. All food and drinks should never be hot.
- The consistency of ready-made dishes on the menu is soft and liquid. These are various porridges, meatballs, steamed cutlets. Avoid solid, heavy and tough foods.
- Drink clean water. The volume of fluid consumed varies from 1.5 liters to 2 liters per day.
Treatment
Treatment of bulbitis should be carried out comprehensively. In case of a mild form of pathology, if there is no bacterial infection, it implies giving up bad habits (overeating, drinking alcohol, smoking), adjusting the character and diet, and normalizing the psycho-emotional state.
When inflammation is pronounced, treatment must include medication and physical therapy.
Treatment with medications
Drug therapy is aimed at stopping the inflammatory process. Antacids (Almagel, Phosphalugel) are prescribed enzyme preparations (Wobenzym, Serox, Enzistal) to facilitate the functioning of the gastrointestinal tract.
Antibacterial therapy is prescribed when Helicobacter pylori is detected. For this purpose, antibiotics of different groups are used: Amoxicillin, Metronidazole, Clarithromycin, Tetracycline, etc. Most often, therapy involves a combination of 2 antibiotics and acid-regulating drugs (Omez, Ranitidine, Pantoprazole, etc.).
For the erosive form, painkillers are prescribed. (Baralgin, No-shpa, Drotaverine, etc.).
Diet
The diet for bulbitis is not rigid, but there are restrictions. It is necessary to exclude products that have an irritating effect on the mucous membrane of the stomach and duodenum or stimulate the production of hydrochloric acid (canned foods, fried and spicy foods, strong tea, coffee, seasonings, alcohol, smoked sour fruits). Minimize salt intake.
Meals should be fractional, 5 - 6 per day in small portions.
Liquid dishes, jelly, mucous infusions (oats, rice) are preferred. Fruits and compotes made from them saturate the body with vitamins, but they should not be very acidic.
Other permitted products:
- low-fat cottage cheese and sour cream;
- yesterday's bread made from wheat flour;
- dietary meat and fish;
- pasta.
For bulbitis, it is useful to drink boiled milk, up to 5 glasses a day, as it improves the functioning of the intestines.
Recommended diet for bulbitis
The diet for bulbitis must be strict, and compliance with it is a prerequisite. A sample menu for one day is offered:
- Breakfast starts at 08:00. It includes yesterday's white bread, steamed omelette, meat soufflé and sweet tea with milk.
- Snack after breakfast at 11:00. This is carrot puree and sweet tea with cream.
- Light snack at 12:00. Take a decoction of rose hips. A very useful drug.
- Lunch at 14:00. Rice soup with tomato juice, yesterday's bread, boiled or steamed fish, mashed potatoes, jelly.
- Afternoon tea at 17:00. Sweet tea with milk and sweet crackers.
- Dinner at 19:00. Lazy dumplings, sour cream, pudding (crackers and apple puree), sweet tea with milk.
- Late dinner 21:00. Skim milk or kefir – 1 glass.
Contraindications
In order to completely cure chronic bulbitis and prevent possible relapses, the patient will have to completely change their lifestyle and find a replacement for their usual pleasures in other areas. However, some restrictions will benefit not only the diseased organ, but also the entire gastrointestinal tract, and this, in turn, will have a beneficial effect on the functioning of the body as a whole.
Currently reading: What is bulbitis duodenitis - symptoms and treatment
In fact, strict restrictions are only needed during exacerbation:
- Complete cessation of alcohol, smoking and carbonated drinks;
- Exclusion from the diet of strong coffee, tea, chocolate with high cocoa content;
- Temporary transition to semi-liquid pureed food;
- Refrain from eating foods that serve as snacks: anything spicy, sour, salty, pickled, spicy;
- Cooking by boiling in water and steaming, baking, stewing.
As soon as the acute period has passed, you can gradually introduce cocoa, weak tea and solid food into the menu, and occasionally treat yourself to a slice of pickled cucumber or a piece of soaked herring. Don't be afraid of dietary dishes. There are hundreds of thousands of people in the world with gastrointestinal problems. It’s hard to imagine that they all stoically eat only semolina porridge. The difference between dietary nutrition and regular food is only in the method of preparing food and the speed of its absorption.
For many patients, the most difficult task is not physical, but psychological limitations. Remember how you react to a cat meowing under your balcony, a long wait for a bus, a television advertisement... You feel irritated, right? How often do you, in a rage, kick a punctured tire or, God forbid, spank your own child who doesn’t want to fall asleep? By giving vent to your bad manners, you not only appear in an unfavorable light in front of those closest to you, but also provoke the development of a bully. Do you think it’s too late for you to re-educate? Then consult a neurologist, drink tea with mint or a decoction of St. John's wort (the latter, by the way, helps get rid of even many years of severe depression, but it will take a long time to drink).
Diet for erosive bulbitis
With erosive bulbitis, the mucous membranes of the intestine are affected, which requires immediate treatment. During this period, all symptoms worsen, and the presence of drug treatment is simply necessary.
In addition to medications, a diet is prescribed for erosive bulbitis. Nutrition is based on a list of specific foods that can be eaten and vice versa.
In the acute form of this disease, it is recommended to completely abstain from food for several days. During this time, the walls of the mucous membranes will be restored and all the unpleasant symptoms of the disease will go away.
A special diet will help you recover and prevent the recurrence of symptoms. Such treatment is mandatory, otherwise the disease may develop into a chronic form.
The diet includes:
- Vegetable-based puree soups
- Light omelettes
- Stewed, baked or boiled fish, chopped into pieces, in the form of soufflés or mousses
- Meat and vegetable puree
- Porridge
- Low chicken broth (chicken breast based)
- Mashed potatoes
- Weak tea
- Kiseli
This diet is designed for the first week of treatment. It is suitable for other diseases of the digestive system, for example gastritis, which often accompanies bulbitis.
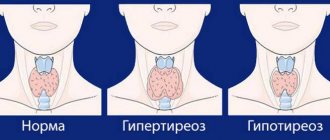
Classification
Depending on the characteristics of the course, acute and chronic forms of pathology are distinguished. The inflammatory process can be focal or diffuse in nature, if the mucous membrane of the duodenal bulb is completely affected.
According to the degree of activity, they are distinguished:
- catarrhal - under the influence of a disturbed pH balance, irritation develops, which later develops into inflammation. The walls of the bulb swell, more mucus is released, and the digestion process suffers. If you contact a specialist in a timely manner, this form has a favorable prognosis;
- erosive-ulcerative - develops as a result of inflammation occurring for a long time and is characterized by the formation of single or multiple lesions on the mucous membrane;
- follicular - provokes tissue changes at the micro level: the follicles covering the walls of the duodenum become larger, the mucous membrane acquires a nodular structure.
What to give up
In order for the diet to be beneficial and the treatment to achieve the desired result, it is necessary to give up some foods and establish a healthy diet. All food should be low-fat, not heavy and not salty.
Avoid aggressive components that can irritate mucous membranes. For bulbitis, exclude horseradish, mustard, mayonnaise, ketchup and hot sauces. Smoked meats, pickles and marinades are also harmful.
Food dyes and other harmful substances that are part of many industrial products cause lasting harm to health and the entire immune system.
By refusing them, you can protect the body from their harmful effects. Alcohol and cigarettes take an active part in the destruction of the immune system and all mucous membranes.
This entails a lot of unpleasant consequences both from the gastrointestinal tract and the whole body.
Among the products, you should avoid those that can cause flatulence. These include beans, peas and cabbage.
A strict diet for bulbitis involves a complete rejection of fresh bread and yeast products.
At the first signs of the disease, you should seek help from a doctor. Only he will be able to diagnose the disease and make the correct diagnosis.
Self-medication is unacceptable and leads to bad consequences.
Symptoms
Pronounced symptoms are characteristic of the acute form of bulbitis. A chronic disease can go unnoticed or have mild symptoms, which is why the patient himself sometimes cannot understand the reasons for the ailment that besets him. Very often, chronic bulbitis is discovered by chance, when visiting a doctor for a completely different reason, which does not make it any less dangerous.
When, at the request of the doctor, the patient tries to remember whether he recently experienced any unpleasant sensations, he will probably answer that there were cramping pains in the stomach, nausea and severe vomiting of bile, repeated many times during the day, after which several more days There was a bitter taste in my mouth. The patient himself believes that he was poisoned by something, and often this is true: an acute attack of bulbitis can in fact be provoked by severe poisoning or uncontrolled use of medications. The fact is that the tablets contain substances that are powerful irritants for the gastric mucosa.
Why are there no symptoms now? When the acute phase gives way to the chronic phase, the discomfort fades away, because the surface of the mucous membrane remains almost intact: traces of exposure to aggressive substances are very small, there are no large lesions - clearly visible erosions and ulcers - on it. Instead of pain and vomiting, other signs of the disease appear.
Currently reading: Symptoms and treatment of erosive bulbitis
Types of disease
Bulbitis, like any other inflammation, can:
- be in acute or chronic forms;
- affect the entire intestinal wall (diffusely) or occupy a specific focus;
- divided into catarrhal, ulcerative and follicular forms.
The last division is especially important, as it is decisive in choosing tactics for treating gastric bulbitis. It is worth noting that it is impossible to identify a particularly noticeable difference between the three types of the disease; these forms can only be differentiated by endoscopic examination.
Catarrhal form
Catarrhal bulbitis.
Catarrhal bulbitis is a superficial inflammation of the duodenal bulb with a predominance of edema of the intestinal wall and desquamation of the epithelium. Catarrhal bulbitis can be serous, mucous or purulent, depending on the nature of the effusion, or it can gradually replace the exudate as the disease develops. But most often, catarrhal bulbitis occurs without pus and in acute form. It is believed that catarrhal bulbitis has the mildest course and usually does not leave behind any residual effects.
Ulcerative-erosive form
Ulcerative bulbitis (or ulcerative-erosive) is characterized by the appearance on the mucous membrane
Erosive bulbit
gut eroded areas or individual ulcers. The disease requires increased attention and treatment, since this condition can cause secondary peptic ulcers, intestinal bleeding (with wall perforation), and peritonitis. It is equally common in both acute and chronic forms. For the patient, ulcerative bulbitis is perceived as much more difficult, and it is much more difficult to treat.
Follicular form
In this division, the follicular form of inflammation of the duodenum stands apart. It develops as an immune reaction to infection or aggressive agents. Lymphoid follicles in the intestinal wall enlarge and become inflamed, giving a clinical picture similar to catarrhal bulbitis.
Causes
There are a variety of reasons why erosive bulbitis (erosive gastritis) occurs, which include the following:
- violation of nutrition rules;
- prolonged stress;
- infectious processes in the digestive organs;
- genetic factor;
- deterioration of immunity.
Each of these factors in itself is very important and indicates a high risk of a pathological process. Among the main causes of the disease is the aggressiveness of one’s own immune system, which negatively affects pathogens and healthy cells of the body.
Treatment of bulbitis and medications used
Treatment of bulbitis can be etiotropic, pathogenetic and symptomatic.
Etiotropic treatment involves eliminating the cause of the disease, for example, eradication (eradication) of Helicobacter pylori infection, which is carried out according to regimens with the prescription of several antibiotics, metronidazole, bismuth preparations and other agents.
Pathogenetic therapy is aimed at reducing inflammation of the mucous membrane of the bulb. For this we use:
- Diet. It should be aimed at complete sparing of the intestine: thermal, mechanical and chemical. Both table No. 1, 1a, when the stomach is involved in the process, and table No. 4, which is indicated for intestinal diseases, including infectious ones, can be used. Spicy, sour, fried, fatty and smoked foods are excluded. Protein should be digestible, steaming, pureed vegetables, cereals without coarse fibers, non-acidic jelly and fruit drinks, and cottage cheese casseroles are encouraged. Treatment with mineral waters without gas is indicated;
- Prescription of proton pump blockers (drugs such as omeprazole). Their task will be to reduce acidity in the bulb area, which will lead to a reduction in inflammation;
Finally, symptomatic therapy is treatment that leads to improvement of the condition by relieving individual symptoms. This leads to the disappearance of certain unpleasant symptoms: pain, heartburn, nausea, bloating, heaviness and other symptoms. Most often used to treat bulbitis:
- Antacid drugs. By reducing the acidity of gastric juice and having an enveloping effect, they reduce pain. These are “Maalox”, “phosphalugel”, “almagel-a” containing anesthesin, “gastal” and other drugs. But you need to understand that they do not cure, but help in the complex treatment of inflammation. They begin the treatment of erosive bulbitis, since the first step is to prevent the transformation of erosion into an ulcer;
- Antispasmodics of myotropic action. These drugs relieve spasms of smooth muscles, easing pain and reducing peristalsis. These drugs include “no-spa”, “baralgin”, papaverine and many others.
In the case of secondary bulbitis, caused, for example, by an acute intestinal infection, it is necessary to use parenteral administration of crystalloids (ionic solutions) for the purpose of detoxification; the use of enterosorbents and antibacterial drugs is indicated, followed by correction of dysbiosis.
In the event that bulbitis is combined with chronic pancreatitis, the use of enzyme preparations, such as Creon, Festal, Enzistal, Panzinorm, is indicated to facilitate digestion.
Forecast
We looked at the main symptoms and treatment regimens for bulbitis, an inflammatory disease of the initial part of the duodenum. In the vast majority of cases, the disease can be stopped and even radically cured, but only if you are treated by a qualified and experienced gastroenterologist, and the patient strictly follows all his recommendations.
Many patients are surprised that treatment begins with a recommendation to categorically give up alcoholic beverages and smoking. Some cannot withstand this, and the disease progresses, gradually leading to ulcerative defects that require surgical treatment.
In order to avoid exacerbations during a chronic process, you need to follow the principles of proper nutrition, eat healthy foods, eat often, but little by little. It is advisable to try to avoid taking large amounts of medications without a doctor's prescription, as they can cause aggravation, and also wash your hands before eating, since any intestinal infection can cause an exacerbation of inflammation. In order to monitor the condition of the mucous membrane of the duodenum, it is enough to undergo a planned FGDS once a year, which will allow you to monitor the condition of the digestive organs.
Tags: stomach, intestines
Causes of the disease
Damage to the mucous bulb can be primary or secondary:
- Primary inflammations are caused by malnutrition (nutritional), exposure to bacteria, viruses, fungi or parasites, allergic and autoimmune reactions, chemical agents, neuroendocrine disorders.
- Secondary inflammation appears against the background of gastritis, cholecystitis and pancreatitis, duodenal ulcers, circulatory disorders, heart and vascular diseases, and immunodeficiency states.
Bulbitis develops for reasons of heredity or congenital defects in organ development.
A predisposition to inflammation occurs when the function of the duodenum is impaired, in which acidic food chyme is processed with bicarbonates from the pancreas. Pathology is possible with dyskinesia, disorders of the nervous regulation of sphincters between parts of the gastrointestinal tract, anatomical features of the intestine, which make it difficult for juices or food to enter.
Causes of bulbitis additionally include:
- food poisoning;
- alcohol abuse;
- long-term medication use;
- chronic stress, spasm of the diaphragm, disorders of the nervous regulation of gland function;
- smoking;
- helminths, opisthorchiasis, lamblia, shigella, salmonella;
- Botkin's disease;
- inflammatory bowel processes.
Spicy, fatty foods, when combined with other physiological factors, can provoke damage to the mucous membrane.
Diet
Diet is the key to the effectiveness of treatment and the absence of relapses in the patient, so you need to pay special attention to nutrition. In severe advanced cases and in the acute stage, it is better to completely eliminate food intake for a while until pain, swelling and inflammation decrease, and then gradually add porridge with low-fat milk and water.
In the non-acute stage, nutrition for bulbitis includes fermented milk products, vegetable broths, and white bread crackers. All products must be boiled or steamed. The beneficial effects of natural jelly and enveloping cocktails. As a sweet treat, oatmeal cookies are perfect for such patients.
You should forever give up carbonated drinks, spicy and fried foods, and smoked foods. A patient with a predisposition to gastrointestinal diseases should never stop eating properly.
RepostTweet
Classification of the disease and pathogenesis
Chronic bulbitis is an inflammation that affects the mucous membrane of the duodenal bulb, which occurs when stomach contents penetrate the intestine and due to gastritis. Chronic gastric bulbitis has certain symptoms. As a rule, it is accompanied by pain of varying degrees of intensity, ulcers, hemorrhage, and gastrointestinal disorders.
Chronic bulbitis can be confirmed using the following diagnostic methods: endoscopic examination, biopsy, pH-metry, test for gastritis with Helicobacter pylori, contrast radiography. Treatment of pathology directly depends on what causes it. For treatment, anti-Helicobacter antibacterial drugs are used, as well as drugs taken for gastritis with high acidity of gastric juice. It is also necessary to take medications that restore the damaged mucous membrane of the duodenum.
According to gastroenterologists, at present, chronic bulbitis caused by Helicobacter is not common. This is due to the fact that an effective therapy strategy is used that destroys this bacterium in the stomach cavity during gastritis. In case of untimely treatment, chronic bulbitis can have many complications that threaten not only health, but also life. In this situation, surgery may be required.
Considering the nature of the pathology, there are acute and chronic forms.
Acute bulbitis is characterized by nausea, vomiting, intense pain, and a bitter taste in the mouth. The chronic form of the disease occurs against the background of aching or bursting pain concentrated in the solar plexus area. Attacks of nausea may bother you, but vomiting does not occur. This type of bulbitis lasts for years, manifesting itself as seasonal exacerbations.
This bulb is important in the digestive process. It is located near the pancreas, gallbladder and stomach, and looks like a ball. The process of digestion of food takes place in the cavity of the stomach, then penetrates further through the gastrointestinal tract and only then enters the intestines.
Gastric juice takes part in the breakdown of food, exerting an aggressive effect due to the hydrochloric acid contained in the composition. For this reason, peptic ulcers and bulbitis may appear. If food is not completely digested, hydrochloric acid in the bolus enters the intestines. This provokes an imbalance of microflora. Once in the bulb, the acid is immediately neutralized and becomes safe. Then the food enters the rest of the intestinal sections.
The following forms of the disease are distinguished:
Chronic erosive bulbitis is more complicated than other forms. This pathology often becomes the focus of duodenal ulcers. A through type of bulb lesion is observed. The main symptom of this disease is the presence of erosions, as well as hemorrhage. The erosive type of bulbitis is a pathology that has a clear clinical picture.
The main symptoms of erosive bulbitis:
- severe weakness;
- irritability;
- nausea and vomiting after eating;
- dizziness and headaches.
Provoking factors of the chronic form of erosive gastritis:
- alcohol abuse;
- various injuries;
- use of certain medications;
- poisoning of various pathogenesis;
- the presence of a viral infection that has infected the body due to penetration with food.
The superficial form of bulbitis deserves special attention, which is considered the easiest and safest, as it affects the outer parts of the duodenal mucosa. Pathology can have a hidden clinical picture. The danger of a mild form is that, against the background of hidden symptoms, an exacerbation of bulbitis may occur. As a result, the pathology is transformed into an erosive form. To avoid complications, it is necessary to undergo regular examinations and pay attention to manifestations in the body.
Causes of superficial bulbitis:
- alcohol and smoking;
- weakened immune system;
- genetic predisposition;
- irrational and unhealthy diet.
Catarrhal bulbitis is considered an intermediate stage. It appears due to an increased level of acidity of gastric juice in the area of the duodenal bulb, against the background of Helicobacter pylori, as well as due to irritation of the mucous membrane itself. The main symptom of the pathology is severe pain in the abdomen, headaches and the presence of a sour taste in the mouth.
Diagnosis and treatment
If chronic bulbitis is suspected and the diagnosis is confirmed, the following manipulations are prescribed:
- clinical blood test;
- blood biochemistry;
- stool analysis for possible blood impurities;
- Helicobacter tests;
- X-ray or ultrasound of the abdominal organs.
The most accurate method for identifying bulbitis is considered to be an endoscopic examination - duodenoscopy, in which the mucous membrane of the duodenum and its bulbs are examined.
Treatment of the disease with drugs is based on the following principles:
- antacid drugs (neutralizing acid): “Maalox”, “Gastal”;
- increasing mucosal immunity: “Biogastron”, “Solcoseryl”, “Dalargin”;
- restoration of intestinal motility: “Cerucal”, “Motilium”;
- normalization of enzyme production: “Venter”, “Enprostil”;
- probiotics: Lactobacterin, Linex;
- antihelminthic therapy: "Pyrantel", "Levamisole".
Taking medications should be prescribed by the attending physician; independent treatment of gastric bulbitis leads to complications of the disease.
ethnoscience
When erosive bulbitis occurs, folk remedies and methods for treatment are widely used. They are used as an adjunct to drug therapy. Good means are:
- propolis tincture;
- wheat sprouts;
- sea buckthorn oil;
- green apples.
For prolonged pain, propolis tincture helps to cope with the problem. Another good way to get rid of inflammation and soreness is sea buckthorn oil. You can purchase it ready-made or prepare it yourself.
Before carrying out treatment with traditional methods, you must first consult with your doctor, as they may have certain contraindications.
Features of WPC and classification of bulbite
The duodenum is located in the initial part of the small intestine. It has a horseshoe shape. The upper part acts as an anatomical extension of the gastric pylorus, called the bulb.
In the area of the descending section there is a special formation, which is called the major nipple, where the ducts of the pancreas and gall bladder are located. Food enzymes and bile pass through these ducts into the intestinal lumen, ensuring proper and complete digestion.
The main functions of the duodenum:
- regulation of the production of food enzymes, bile in a certain concentration;
- preparing the food bolus for subsequent processing, creating the desired pH;
- humoral effect on the activity of secretory cells of the stomach.
The following forms of this disease are distinguished:
- erosive - numerous erosions on the surface of the mucous membrane;
- atrophic – total atrophy of the mucous membrane, thinning, flattening of the villi;
- focal - a large area of damage, erosion in the form of clusters of lesions;
- superficial – dystrophic processes affecting the upper part of the epithelium.
About diagnostics
As elsewhere, in the internal medicine clinic, they question, examine and palpate the abdomen. Usually you can detect pain in the epigastrium, as well as some tightening of the muscles of the anterior abdominal wall (protective tension).
Of course, some clinics use fluoroscopy with a barium suspension, which allows you to see the dynamics of the motility and work of the stomach and intestines, but the “gold standard” of diagnosis is an FGDS with a biopsy, ultrasound of the abdominal cavity, as well as pH-metry of the gastric juice to understand how much the acid-base balance changes in the bulb area. This must be done to determine treatment tactics.
With FGDS, you can assess the severity of inflammation, find areas of erosion and ulcerative defects, determine places of hypertrophy and atrophy of the epithelium, find islands of dysplasia and perform a biopsy. Based on the results of the biopsy, it is possible not only to perform histological and cytological examination, but also to identify the presence of Helicobacter pylori infection.
The use of ultrasound allows one to assess the condition of other organs of the hepatobiliary zone: liver, gallbladder, pancreas. This helps with making related diagnoses.
In addition, in specialized gastroenterology clinics, electrogastroenterography can be performed, as well as antroduodenal manometry, which will show the “strength” of the sphincter and its strength between the stomach and intestines. Sometimes routine tests may be required - determining blood leukocytosis as a marker of inflammation, performing a stool test for occult blood, and many other studies at the discretion of the doctor.