Congenital hypothyroidism is a pathology that develops against the background of insufficient production of thyroid hormones. The disorder may be caused by the immunity of organ cells to tropic hormones, which are produced by the pituitary gland to regulate the functioning of elements of the endocrine system.
Congenital hypothyroidism is a pathology that develops against the background of insufficient production of thyroid hormones.
If this disorder is accompanied by the development of diffuse goiter, the disease in the international classification is listed under code E03. The congenital form of hypothyroidism, characterized by diseases such as myxedema or atrophy, is listed in ICD-10 under code E03.1.
Violation can provoke a lag in the mental and physical development of the child.
The lack of the required level of thyroid hormones in the body provokes severe deviations in the functioning of all systems. Children suffering from this disease are given a disability.
Only with timely identification of the problem and initiation of replacement therapy can significant improvement be achieved.
What is the thyroid gland needed for?
The thyroid gland is the most important organ of the human endocrine system. It performs a huge number of functions that are necessary for the full development of every child. The brain receives all information from the outside through the perception of light, sounds, and smell. The human body functions with the help of biochemical substances - hormones. The endocrine system, in turn, acts as a kind of intermediary between the brain and the body.
The pituitary gland and hypothalamus are the main organs that process all information. They are the ones who give the “command” to the gland about which hormone the body needs.
Basic functions of the thyroid gland
- stimulation of the growth process in children;
- control of metabolism and body temperature;
- participation in intellectual development;
- formation of vitamin A in the liver;
- lowering cholesterol levels;
- regulation of calcium, protein, fat and carbohydrate metabolism.
This organ contributes to the full development of the child’s body. At the same time, it plays one of the leading roles in the formation of the skeleton and nervous system. A healthy thyroid gland produces the hormones thyroxine (T4) and triiodothyronine (T3). With congenital hypothyroidism in newborns, their production decreases.
A deficiency of the hormones mentioned above can lead to inhibition of the baby’s physical and mental development, his growth also slows down, the child gains excess weight, he has chronic fatigue syndrome, and blood pressure and heart rate are disturbed. In addition, the intestines malfunction, resulting in bone fragility.
Causes
The main ones identified by doctors and included in statistics:
- Anomalies in development. Caused by environmental and drug exposures both during pregnancy and after birth.
- Complete or partial absence of organs.
- The location of organs in places where they should not be is associated with the embryonic period.
Hypothyroidism from birth can be caused by a number of consequences and factors:
- Dysfunction of the hypothalamic-pituitary complex.
This disease occurs in the early stages of pregnancy, as it is associated with the egg and tubes of the woman’s uterus. The hypothalamus performs the function of controlling all organs of the endocrine system. The slightest malfunction or violation entails consequences, as a result, it affects the production of hormones. This slows down the baby’s development process, causing pathology of the thyroid gland. - Violation of the hormone-synthesizing function of the thyroid gland. It occurs when there is not enough iodine in the body, or it is simply not completely absorbed by the endocrine gland.
- The body's resistance to taking thyroid hormones. Occurs in women during pregnancy as a result of receiving or administering various medications that affect the hormones of the endocrine gland.
- Genetics. Congenital hypothyroidism is inherited from relatives.
- Poisoning by toxic substances or radiation. For example, alcohol products, pesticides or nicotine.
- Viral and infectious diseases.
Causes of congenital hypothyroidism and risk factors
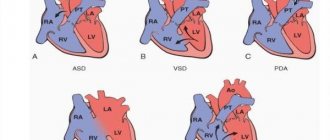
In approximately 80 - 90% of cases, the disease is caused by malformations of the thyroid gland : for example, hypoplasia or dystopia (displacement) into the retrosternal or sublingual space. About 2% of cases of congenital hypothyroidism are caused by genetic mutations . At the same time, the child often also has other developmental anomalies: cleft lip and hard palate (the so-called “cleft lip” and “cleft palate”), congenital heart defects, etc.
approximately 5% of cases, the cause of the pathology is hereditary diseases , which lead to disruption of the production of thyroid hormones or their interaction with each other. In other cases, congenital hypothyroidism occurs as a result of various lesions of the hypothalamic-pituitary system caused by birth trauma, asphyxia of the newborn, pituitary aplasia, abnormalities of brain development or tumor processes.
Risk factors for congenital hypothyroidism
- iodine deficiency in the body of a pregnant woman;
- toxic effects of chemicals or certain medications on the developing fetus;
- adverse effects of ionizing radiation;
- infectious or autoimmune diseases of the expectant mother.
Causes of congenital hypothyroidism
The main ones:
- Absence/underdevelopment of the thyroid gland, genetically determined;
- Genetic disorders of the biosynthesis of thyroid hormones;
- A lack or excess of iodine in a pregnant woman’s diet can lead to hypothyroidism in the newborn;
- Excessive amounts of thio- and isocyanates, as well as cyanogenic glycosides in the diet. In the medical community, these substances are usually called strumogenic and they are found in regular cabbage, Brussels sprouts, cauliflower, rapeseed, turnips, sweet potatoes... The list goes on, but this does not mean that these foods should be excluded from the diet during pregnancy. It is enough just not to consume them in very large quantities;
- Quite rarely - exposure to radioactive iodine consumed by a pregnant woman. From about 10–12 weeks, the fetal thyroid gland already accumulates iodine, including radioactive one;
- The rarest and least promising cause of congenital hypothyroidism in terms of treatment is a pathology of thyroid hormone receptors. In this case, there is a lot of TSH, T3, and T4 in the blood, but hypothyroidism is still observed. Only two hundred families with this type of congenital hypothyroidism have been described.
Congenital hypothyroidism, if diagnosed in a child, is usually called cretinism. Indeed, a lack of thyroid hormones slows down a person’s psycho-emotional development. Myxedema is spoken of in severe hypothyroidism, including congenital, when characteristic hypothyroid or myxedematous edema develops.
Classification of congenital hypothyroidism
Congenital hypothyroidism has several classifications, which are based on the severity of symptoms and the level of the hormone thyroxine, the location of the disorder, the duration of the disease and compensation during treatment.
Forms of hypothyroidism by origin
- Primary (thyroidogenic) - changes occur directly in the tissues of the thyroid gland itself.
- Secondary - the functioning of the adenohypophysis is disrupted, resulting in a lack of synthesis of thyroid-stimulating hormone (TSH).
- Tertiary - deficiency of thyrotropin-releasing hormone (hypothalamic hormone). Together with the secondary form of the disease, it is classified as central hypothyroidism.
- Peripheral - insufficiency of the effect of hormones, which is due to the absence or defect of receptors in tropic tissues or a violation of the conversion of thyroxine (T4) to triiodothyronine (T3).
By duration
- transient hypothyroidism , developing against the background of exposure to the mother’s antibodies to the child’s thyroid-stimulating hormone (TSH); its duration ranges from 7 days to 1 month;
- permanent hypothyroidism requires lifelong replacement therapy.
Depending on the severity of clinical manifestations and the level of thyroxine in the blood, the pathological process can be latent (subclinical), manifest and complicated . The latent form is characterized by a normal T4 level against the background of an increase in thyroid-stimulating hormone, while symptoms do not appear, or they are subtle and nonspecific. With manifest hypothyroidism, the level of thyroxine is slightly reduced against the background of a high concentration of TSH, as a result of which the classic symptoms of the disease develop. The complicated form occurs with a high level of thyroid-stimulating hormone and a sharp deficiency of T4. In addition, disturbances of other systems occur: heart failure, cretinism, polyserositis, and less commonly, pituitary adenoma.
Depending on the effectiveness of treatment, there are:
- compensated hypothyroidism - symptoms disappear during treatment, and the concentration of hormones in the blood is within normal limits;
- decompensated hypothyroidism - there are laboratory and clinical manifestations of the disease even with adequate treatment.
Children with congenital hypothyroidism are more susceptible to frequent infections and colds.
Prevention
- The use of various medications and prevention begins in the womb, when the mother is planning or is already carrying a child. This means that medications containing iodine should also be used.
- Before planning a baby, you should initially undergo a full examination so that no problems or diseases arise in the future. Contacting a genetics specialist will reveal whether there is a predisposition to hypothyroidism among relatives. It is also worth undergoing a full examination and passing clinical tests. It is necessary to make sure that future parents are healthy and fully prepared to conceive a new life.
- Consultation with an endocrinologist and further treatment of existing hypothyroidism. It is worth registering and coming to appointments during periods of exacerbation and the appearance of the first symptoms. And also use medications in the required proportions, which were prescribed by specialists.
Prevention should begin when the child is in fetal form, especially in families with thyroid pathology.
Symptoms of congenital hypothyroidism
Congenital hypothyroidism symptoms in newborns depend on the severity of the disorder and the form of the pathology. The first signs of the disease can appear at different ages.
The main clinical manifestations of hypothyroidism in newborns and older children
- birth later than 40 weeks;
- signs of immaturity, despite full-term or post-term pregnancy;
- the child’s weight at birth is more than 4 kg;
- delayed passage of meconium (original stool);
- swelling of the face, swollen “pads” on the back of the hands and feet;
- poor healing of the umbilical wound;
- prolonged course of jaundice in newborns;
- slow weight gain;
- rough low crying of the baby, weak sucking of the breast, apathy;
- cyanosis (blue skin) and episodes of apnea (short-term cessation of breathing) during feeding;
- dry skin, cold hands and feet;
- weakening of reflexes and muscle tone;
- flatulence and constipation;
- macroglossia (abnormally large tongue);
- dyspeptic symptoms;
- delay in closure of fontanelles and teething;
- delayed mental and physical development, manifested already in the first months of life.
Primary congenital hypothyroidism in children develops in stages. Pronounced symptoms of the disease are observed at the age of 3 - 6 months. The skin is dry, thickened, icteric-gray in color, and sweating is sharply reduced. Myxedema (“mucous swelling” of organs and tissues), atrophy of hair and nail plates develops. The child's voice becomes rough, low and hoarse. There is a lag in physical and psychomotor development, teeth erupt and are replaced with a delay. In the future, mental retardation is noted, which is manifested by a decrease in intelligence and poverty of vocabulary and is prone to progression up to mental retardation.
Since congenital hypothyroidism involves partial or complete deficiency of thyroid hormones, this pathology is dangerous to the life and health of the child. Their deficiency inhibits the development of the inner ear, brain and spinal cord, nerves and other structures of the nervous system. At a certain stage, the disorders become irreversible and can no longer be treated.
Symptoms
Congenital hypothyroidism in newborns manifests itself:
- Slow or absent production of thyroid hormones. As a result, children's physical and mental development slows down. Diagnostics notices this a few months after birth.
- Most often, such children are born later than the due date.
- Large weight of a newborn (more than 3.5 kg).
- A blue tint appears above the upper part of the lip.
- Swelling of body parts.
- The mouth is constantly open.
- Skin color may be yellowish.
- Changes in voice to lower tones when crying.
- Heart problems.
After three months of life, the following signs of hypothyroidism are also found:
- dry skin;
- brittle hair;
- loss of appetite;
- temperature below normal is observed for a long time;
- constipation or difficulty going to the toilet;
- long hardening of the crown;
- disorders in the skeletal system.
Congenital hypothyroidism and its symptoms are no different from ordinary hypothyroidism.
Diagnosis of congenital hypothyroidism
Diagnosis of congenital hypothyroidism in children includes taking a medical history, an objective examination of the child, instrumental research methods, as well as general and specific laboratory tests. When interviewing the baby's parents, it is possible to identify the presence of predisposing factors: mother's illnesses during pregnancy, family history, nutritional disorders, use of obstetric aids during childbirth, etc. When examining the child, a decrease in heart rate, blood pressure, reflexes, moderate hypothermia (decrease in temperature) is revealed. body), developmental delay.
Laboratory research methods include general and biochemical blood tests. Specific tests - measuring the level of thyroxine (T4) and thyroid-stimulating hormone (TSH) in the blood plasma.
Neonatal screening
After birth, all newborns undergo so-called neonatal screening. This procedure is an effective method for identifying the most common hereditary diseases: adrenogenital syndrome, congenital hypothyroidism, galactosemia, cystic fibrosis and phenylketonuria.
A few drops of blood are taken from each child’s heel in the maternity hospital. The sample is taken three hours after feeding on the fourth day of life in full-term infants and on the seventh day in premature infants. The blood is applied to a special test form, which is then sent to the laboratory, where genetic research is carried out.
X-ray of extremities
It makes it possible to determine the violation of the order and delay in the formation of ossification nuclei, their asymmetry, as well as a specific sign of hypothyroidism - epiphyseal dysgenesis (impaired development of the epiphyses of bones). An electrocardiogram (ECG) reveals sinus bradycardia and widening of the QRS complex. Ultrasound examination (ultrasound) of the thyroid gland can determine dystopia (change in position), hypoplasia or absence of the organ.
Molecular genetic methods
, molecular genetic research is used to identify gene mutations .
If a central origin of hypothyroidism is suspected, computed tomography and magnetic resonance imaging (CT and MRI) of the pituitary gland are performed.
As a rule, in the absence of timely treatment, congenital hypothyroidism leads to damage to the central nervous system with the development of oligophrenia.
Diagnostics
It is impossible to diagnose hypothyroidism only based on the symptoms that appear in children, therefore, every maternity hospital has a rule according to which early screening is required, on the 4th day from the date of birth of the baby. This requires taking blood from the heel of a small patient.
For diagnosis, blood is taken from the heel of a small patient.
The laboratory determines the level of thyrotropin, triiodothyronine and thyroxine. If the indicator exceeds 100 mU/l, then primary hypothyroidism is diagnosed. If the analysis result shows 20-50 mU/l, then the study is repeated, but only the dried blood spot is analyzed. If the indicator again exceeds 20 mU/l, then the level of TSH in the blood serum is determined. The disease code according to ICD 10 is E03.
The Apgar score has also been developed to diagnose hypothyroidism. It is a test based on the summation of points for each question about the presence of a particular characteristic. This table looks like this:
| Signs | Points |
| Is there constipation? | 2 |
| Is there any swelling on the face? | 2 |
| Is there an umbilical hernia? | 2 |
| Has neonatal jaundice been present for 3 weeks or more? | 1 |
| Is your skin pale? | 1 |
| Is the tongue enlarged? | 1 |
| Is there muscle weakness? | 1 |
| Was the child born weighing more than 4 kg? | 1 |
| Is the fontanelle open? | 1 |
| Was the pregnancy longer than 40 weeks? | 1 |
If the total score exceeds 5, then hypothyroidism can be suspected.
Treatment of congenital hypothyroidism
Therapy for congenital hypothyroidism should begin immediately after confirmation of the diagnosis. The likelihood of complications in this case will be minimal. Treatment is based mainly on hormone replacement therapy. This allows the body to function normally, but the thyroid gland will no longer produce hormones on its own.
Congenital hypothyroidism is a disease in which medication is required for life. If the dosage of the drug prescribed by the doctor is selected correctly, the child will develop fully, keeping up with his peers. He will not experience any difficulties in communication or studies.
The drug of choice for the treatment of congenital hypothyroidism is L-thyroxine . It is used as hormone replacement therapy and is a synthetic analogue of thyroid hormones. The dosage of the drug is selected strictly individually. If necessary, it can be mixed with breast milk. The effectiveness of treatment is assessed by the level of thyroxine and thyroid-stimulating hormone in the blood, as well as the disappearance of symptoms of the disease.
Symptomatic medications and multivitamin complexes may also be additionally prescribed.
Treatment
- Artificial medications containing TSH are prescribed. Doses and method of administration depend on the individual characteristics of the child. Thus, thyroid substances return to normal, and the baby’s development continues without consequences.
- L-thyroxine is currently very popular and is a high-quality analogue of thyroid hormones. The result: stable hormonal levels and maintaining balance in the body for a long period.
Visible results after taking the correct doses of medications are already noticeable in the first week. And normalization occurs within two months. For older children and adults, treatment takes longer and results appear later. If assistance is not provided and diagnosis is delayed, a hypothyroid coma may occur. This is the moment when all the symptoms of hypothyroidism worsen and lead to danger to a person’s life. Treatment is carried out in a hospital.
But there are exceptions:
- If the disease initially implied the absence of a thyroid gland, radiation therapy was performed, or the patient suffered from Hashimoto's disease, then hypothyroidism is incurable.
- When dysfunction of the endocrine glands is caused by other pathologies, their cure will also have a positive effect on this disease.
- It is possible that some medications were prescribed side effects related to the thyroid glands and when they are discontinued, everything will return to normal.
- The latent form of congenital hypothyroidism does not affect health in any way, but constant monitoring by specialists is necessary.
Selected names of drugs that contain levothyroxine sodium that help in therapy:
- Levoxide (used to treat liver diseases);
- Synthroid (is a thyroid hormone);
- Levothroid (contains L-thyroxine, which helps with growth and metabolism).
Symptoms
Despite the fact that the causes of the disease in children are quite diverse, the clinical picture can manifest itself at different ages. For some babies this happens in the first week of life, while for others it occurs between 2 and 6 years. What factor influences the timing of the onset of symptoms remains unknown.
Symptoms of congenital hypothyroidism are as follows:
- problems with the passage of meconium (the first stool released by the newborn’s intestines);
- high birth weight (more than 4 kilograms);
- prolonged course of physiological jaundice, characteristic of all infants;
- swelling of the face, lips and eyelids;
- constantly open mouth and spread tongue;
- frequent episodes of regurgitation;
- tendency to constipation;
- short-term cessation of breathing during breastfeeding or sleep;
- joint dysplasia in the hip area;
- increased size of fontanelles;
- skin cool to the touch.
When the pathology manifests itself in older children, the presence of the following symptoms is noted:
- dryness and roughness of the skin;
- increased hair fragility;
- separation and deformation of the nail plates;
- decreased sweat production;
- poor appetite;
- disruption of the process of swallowing not only solid food, but also liquids;
- muscle hypotension;
- decreased temperature;
- late eruption of primary or permanent teeth;
- change in facial features;
- low blood pressure;
- rare pulse;
- increase in heart size.
If you do not start treatment for such symptoms, there is a high probability that oligophrenia will develop with congenital hypothyroidism.
Congenital hypothyroidism in a child
Subclinical form
Subclinical hypothyroidism in children is most often observed in children 2-4 years old. Its picture, especially when conducting a blood test, is quite clear: the T4 hormone is within normal limits, while TSH is increased. This disease can be detected in girls for the first time at the age of 5, but in childhood it can be treated quite effectively.
The cause of the development of such hypothyroidism is a primary disease - autoimmune thyroiditis, in which the cells of the thyroid gland themselves are destroyed. In fact, the body perceives the gland as a source of foreign bodies - increased T4. And the antibodies are aimed at neutralizing the source.
If the disease is detected and treated in a timely manner, further therapy is completely unnecessary. Symptoms of subclinical hypothyroidism are as follows:
- Reduced body temperature;
- Weak sucking reflex;
- Refusal of breastfeeding;
- Dry skin;
- Swelling of the arms, legs, eyelids, face.
These symptoms accompany subclinical hypothyroidism in infancy. But it can also be found in children over 5 years of age. In this case, complications associated with the development of the skeleton and brain are possible. Possible vision impairment.
To treat this form, hormonal replacement therapy is used, the dosage of which is calculated by the endocrinologist individually based on the diagnostic results.
Forecast
When treatment is started early, the prognosis is generally favorable. Hormone replacement therapy leads to rapid compensation of the sick child’s condition and subsequently his psychomotor development occurs in accordance with age-related characteristics.
If replacement therapy is prescribed after the child develops signs of cretinism, it can only prevent their further progression. In such cases, the child experiences irreversible and profound changes leading to disability.
Children suffering from hypothyroidism are under constant supervision of an endocrinologist, pediatrician, and neurologist. They should measure the level of thyroid-stimulating hormone in the blood at least once a quarter.
Hypothyroidism in children causes significantly more serious consequences than in adults. The younger the child, the greater the danger a deficiency of thyroid hormones poses to his health.
Preventive actions
To avoid the occurrence of hypothyroidism in a child, you need to follow a number of certain rules:
- constant monitoring of iodine levels in the expectant mother during pregnancy;
- timely examinations that help identify defects in fetal development during pregnancy, including screening tests;
- giving up bad habits at the stage of planning and bearing a baby;
- protection against colds and infectious diseases during pregnancy (if possible);
- constant monitoring of the expectant mother’s weight;
- avoiding excessive physical activity during pregnancy;
- nutritious nutrition for the child;
- regular intake of vitamin complexes;
- daily walks with the child in the fresh air, sports, hardening;
- if symptoms of hypothyroidism appear, exclude simple carbohydrates from the diet.
Loading...
Share with friends!
Signs of hypothyroidism in preschoolers and adolescents
Symptoms of the disease are detected in preschool age, but do not always manifest themselves as impaired mental development. In contrast, children with hypothyroidism during puberty are obese and experience rapid weight gain and stunted growth.
Attention! The production of sex hormones decreases. In girls, this can cause a late onset of menstruation. In addition, mental retardation leads to decreased school performance.
Hypothyroidism is characterized by disorders of the digestive system - gastritis, constipation, poor appetite. There is a decrease in hearing due to swelling of the auditory tubes.
Changes in the nasal mucosa are accompanied by impaired nasal breathing. On the part of the heart, sinus bradycardia develops. The main symptom of the congenital form of the disease is the accumulation of fluid in the pericardium.
Children with hypothyroidism are characterized by certain appearance features. They have dry skin with a marbled pattern, which is associated with reduced function of the sebaceous and sweat glands. Hair is brittle and dull, prone to loss and slow growth. Nails become flaky and prone to cracks.
Children with insufficient levels of thyroid-stimulating hormones are characterized by short stature and an underdeveloped facial skeleton with a sunken bridge of the nose. There is a delay in sexual development.
Signs and symptoms
Typically, babies with congenital hypothyroidism are born at term or a little later and look completely normal. The vast majority of them do not have any manifestations of thyroxine deficiency. This is partly due to the supply of maternal thyroid hormones through the placenta. Within a few weeks after birth, the clinical signs and symptoms of hypothyroidism become more obvious. Newborns' brains are at risk of permanent damage. Because of this danger, it is important to begin treatment as soon as possible.
For the above reasons, each child born is subjected to various examinations. One of them is neonatal screening. With its help, hypothyroidism can be detected in many newborns before symptoms appear. Screening is done 4-5 days after birth. Previously, such an examination was not carried out due to the risk of getting a false positive result.
In other cases, when a woman's body does not receive enough iodine during pregnancy, the baby may show early signs of hypothyroidism after birth, such as:
- puffy face;
- swelling around the eyes;
- enlarged swollen tongue;
- bloated stomach;
- constipation;
- jaundice (yellowing of the skin, eyes and mucous membranes) and increased bilirubin;
- hoarse cry;
- poor appetite;
- decreased sucking reflex;
- umbilical hernia (protrusion of the navel outward);
- slow bone growth;
- large fontanel;
- pale dry skin;
- low level of activity;
- increased drowsiness.
Diagnostic measures
To diagnose hypothyroidism in a baby during embryonic development, a special screening study is carried out. Congenital disease is diagnosed using the same method by drawing blood from the heel of a 3-5 day old infant.
Despite the fact that this disease is characterized by pronounced specific clinical manifestations, a comprehensive approach is required to make a diagnosis. Information on the diagnostic methods used is presented in the table.
| Diagnostic method | Description of the diagnostic method | Purpose of the procedure |
| Survey |
|
|
| History taking | Analysis of the presence of genetic factors, severe pathologies in the baby’s history, the first manifestations and duration of the disease, features of the child’s embryonic development. | Determining the source of the disease |
| Inspection to obtain objective information |
| Determination of the intensity of manifestations of signs of the disease and the nature of the course of the pathological process |
| Laboratory research | Blood analysis:
| Study of the following indicators:
|
| Test with thyrotropin-releasing hormone. | ||
| Instrumental diagnostics | Ultrasound examination of the thyroid gland | Definition:
|
| Magnetic resonance imaging of the brain | ||
| Computed tomography of the brain | ||
| Survey scintigraphy | ||
| X-ray of tubular bones and knee joints |