Superficial or hemorrhagic gastritis is a subtype of erosive disease and is characterized by damage to the surface layer of the mucous membrane in the stomach by hemorrhages. Hemorrhages are lesions with weak blood vessels that are prone to bleeding due to thinning and increased permeability of the walls. This increases the risk of severe bleeding with associated complications.
Description
Hemorrhoidal gastritis is an inflammation that affects the mucous membrane in the stomach. At the initial stage, microcirculatory vascular dysfunction occurs in the near-surface layer, which leads to hemorrhages of blood-soaked mucous tissues or thrombosis of small vessels. The mucous membrane becomes inflamed due to hemorrhagic changes occurring and disruption of the blood supply to the tissues. Infiltration of leukocytes occurs with the formation of small near-surface hemorrhages. They can be single or multiple.
Hemorrhagic gastritis is often accompanied by gastric bleeding of varying intensity due to the pathological weakness of the blood vessels. When defects are localized on the anterior, posterior wall, or fundus of the stomach, the risk of bleeding is minimal. When the area of the lesser curvature with large vessels is affected, bleeding develops more often. The muscle tissue is not affected, so superficial hemorrhages with proper treatment tend to heal without scarring. Hemorrhagic gastritis occurs in acute or chronic form. Hemorrhagic gastropathy does not depend on the secretory activity of the digestive organ. Predisposing factors:
- Uncontrolled use of non-steroidal anti-inflammatory drugs.
- Any viral infections.
- Severe stress.
- Mechanical internal irritation of the stomach.
- Crohn's disease is a granulomatous inflammation of the gastrointestinal tract.
- Any blood lesions.
Classification of the disease
Hemorrhagic gastritis is a disease that cannot be asymptomatic. According to the nature of the course, it can be acute or chronic, which largely depends on the cause of the disease. Chronic hemorrhagic gastritis can lead to dangerous consequences and provoke the formation of stomach ulcers with perforation of its walls.
According to the results of additional studies, two more varieties are distinguished, which are difficult to distinguish only by symptoms:
- focal hemorrhagic gastritis - the appearance of small individual areas with hemorrhages;
- diffuse variant - damage to most of the mucosal surface.
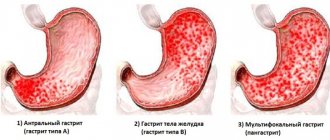
The first option is easier to treat, since most of the functional cells of the mucous membrane are preserved. What diffuse hemorrhagic gastritis is and how to treat this disease depends on the results of additional studies. The most common diagnosis is antrum gastritis, an inflammation of the lower part of the stomach.
Causes of hemorrhagic gastritis
Hemorrhagic gastritis does not appear on its own. Gastropathy with a hemorrhagic component appears with prolonged exposure to the stomach of several provoking factors:
- Incorrect diet and poor quality nutrition: dry food, snacks on the go, regular fast food meals. Such food and improper diet injure the stomach, which reduces local immunity.
- The emergence of pathogenic Helicobacter bacteria that are able to survive in an aggressive gastric environment. Parasitizing on the surface of the mucosa, they cause necrotic tissue damage in areas of inflammation.
- More often, hemorrhagic gastritis appears in people who abuse alcohol, sour, salty, peppered foods. These products and strong alcoholic drinks irritate the mucous membranes, and with prolonged exposure, foci of inflammation form.
- Thinning of the blood vessels in the gastric walls can cause accidental ingestion of chemicals: salts, alkalis, acids or other toxic compounds. They can enter the body by ingestion through the mouth or inhalation through the nose. In this case, acute inflammation occurs. The same form can be caused by some medications, in particular antibiotics. The reasons from the above list contribute to the chronic development of the pathology.
Acute hemorrhoidal catarrh occurs due to:
- suffered shock;
- sepsis;
- injury or burn;
- kidney or liver dysfunction.
Disease prevention methods
The consequences of erosive hemorrhagic gastritis can be life-threatening, so it is worth taking care of the health of the digestive tract in advance. Prevention of the disease is nonspecific and includes a set of general measures to prevent inflammation of the stomach and intestines. Doctors recommend following general recommendations:
- follow the principles of healthy eating, eat little and often;
- get rid of bad habits;
- devote enough time to proper rest;
- do not take any medications unless prescribed;
- When the first signs of illness appear, get examined.
Hemorrhagic inflammation of the stomach walls is a dangerous disease. Its development may be associated with an unhealthy diet, as well as many pathologies of the blood vessels and organs of the digestive tract. Treatment for this type of gastritis is medicinal, and full recovery will require a large amount of time.
The best way to avoid many problems and the need to take medications is prevention, which consists of taking care of your own health, proper nutrition and proper rest.
We recommend: Is it possible to eat bananas if you have gastritis?
Signs and symptoms
The manifestations of hemorrhagic gastropathy are nonspecific, so it is often confused with other types of pathology and gastrointestinal ulcers. Symptoms may appear all at once, or they may develop gradually:
- Complaints. The man points:
- for epigastric pain, especially after eating;
- the appearance of gastric disorders, characterized by heartburn, belching, heaviness, nausea, loss of appetite;
- symptoms of gastric bleeding: tarry vomiting, dizziness, black feces.
- On examination, the following symptoms are visualized:
- pale skin;
- thick coating on the root of the tongue;
- pain in the stomach upon palpation;
- cold extremities;
- drop in blood pressure and increased heart rate with heavy bleeding.
- Diagnosis reveals:
- single hemorrhage or multiple clusters that bleed on blood-soaked mucosa;
- high or normal acidity;
- negative test for Helicobacter;
- anemic signs in the blood test.
Methods of diagnosis and differential diagnosis
Symptoms of hemorrhagic gastritis may resemble other types of inflammation of the mucous membrane, as well as peptic ulcers of the stomach or intestines. At the initial examination, it is necessary to determine the localization of the pain syndrome. It most often appears in the epigastric region, but can spread to other areas.
Additional diagnostic methods include laboratory and instrumental studies:
- Ultrasound to detect the inflammatory process;
- blood, urine and stool tests;
- esophagogastroduodoscopy (EFGDS).
The most informative study is endoscopy of the stomach and duodenum with examination of their contents. The procedure consists of the patient swallowing a probe with a sensor at the end. With its help, you can examine in detail the mucous membrane of the digestive organs and make an accurate diagnosis.
Acute hemorrhagic lesion
Food poisoning can cause this disease.
When the disease first appears, the symptoms of inflammation are more pronounced, and the disease develops quickly. In this case, an acute form of hemorrhagic gastritis is diagnosed. The peculiarity of this pathology is the low risk of developing gastric bleeding. Provoking factors:
- food poisoning from spoiled or low-quality products, food with a high content of toxic substances;
- poisoning with industrial chemicals, poisons, salts of heavy metals;
- poisoning with strong or low-quality alcohol;
- the presence of connective tissue pathologies;
- severe intoxications causing microcirculatory disturbances in the blood vessels of the organ;
- closed injury with stomach contusion;
- damage to the mucosa when using instrumental diagnostic methods.
The form is characterized by a rapid onset. The pathology has no connection with secretory dysfunction. General symptoms of the disease:
- constant discomfort in the upper abdomen, especially after eating heavy food;
- losing weight while refusing to eat due to association with pain;
- nausea with periodic vomiting;
- heartburn with increased acidity;
- bloating, heaviness, belching with periodic regurgitation against the background of dyspeptic gastric disorders;
- the presence of blood in feces and vomit.
What kind of disease is this
Pathology refers to complications of chronic or acute gastritis. It is characterized by the appearance of foci of cell damage on the gastric mucosa. As the pathological process develops, bleeding erosions form.
The following reasons can provoke hemorrhagic erosive gastritis:
- long-term use of antibiotics and non-steroidal anti-inflammatory drugs;
- the predominance in the diet of products that have an aggressive effect on the gastric mucosa (chips, crackers, low-quality sausages, smoked and spicy foods, sweet carbonated drinks);
- contamination of the stomach lining with the bacterium Helicobacter pylori;
- alcohol and nicotine abuse;
- state of chronic stress;
- work in hazardous production.
If you experience discomfort in the stomach after eating or drinking hot drinks, you should not delay going to the doctor. These may be the first signs of the development of gastritis.
Symptoms
A preliminary diagnosis can be made based on the following signs:
- pain in the epigastric region that occurs during the day on an empty stomach, as well as at night;
- feeling of heaviness in the stomach;
- bad breath;
- heartburn;
- belching with a sour taste;
- vomiting at the peak of an attack of pain, often mixed with blood;
- constipation followed by diarrhea.
One of the characteristic signs of erosive gastritis is gastric bleeding. Its development is accompanied by general weakness, dizziness, pale skin, and fainting. Minor bleeding may not cause significant symptoms. It can be detected using a stool occult blood test.
Erosive gastritis, which is caused by taking medications, occurs in a latent form for a long time. The patient may experience minor symptoms of dyspepsia, such as heartburn and heaviness in the stomach. At this stage, symptomatic treatment is carried out. At the same time, the process of erosion development continues.
Clinical examination
- Collection of information about the patient.
- Analysis of complaints and patient's condition.
- Inspection and palpation.
Based on the data obtained, a further diagnostic plan is drawn up. Then laboratory tests are carried out:
- Blood test: general, biochemistry.
- Urine examination.
- Assessment of the characteristics of feces: comprogram for occult blood.
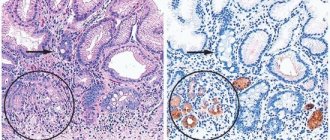
Gastroscopy with biopsy
A probe with a camera, lighting equipment and a biopsy probe at the end is inserted into the stomach through the mouth. The internal condition of the walls is examined, the nature and extent of damage, and the location of hemorrhages are assessed. A sample is taken from the most damaged area of the mucosa and sent for histological analysis. As the mucous membrane is examined, swollen areas with redness and erosive single or multiple lesions from which blood oozes can be detected.
Ultrasound
Ultrasound scans all the organs of the abdominal cavity. The liver, pancreas, and gallbladder are especially carefully examined, disturbances in which can provoke hemorrhagic inflammation of the mucous membrane. The method allows you to detect a tumor in time.
Electrogastroenterography
A study of the motor-evacuation function of the digestive organ is being conducted. The process of moving food through the gastrointestinal tract with its mixing and processing by gastric juice is analyzed. The quality of the stomach is assessed.
X-ray
The method is used as a differential diagnosis of gastritis with separation from ulcers and cancer. The degree of development of gastritis cannot be determined using this method. If ulcers and tumors are not detected, other methods for diagnosing gastritis are used.
How is diagnosis carried out?
Erosive-hemorrhagic gastritis is diagnosed by a gastroenterologist during examination.
Stages:
- When interviewing the patient, associated symptoms are identified.
- During an external examination, the skin and the condition of the nails are assessed.
- The abdomen is examined and palpated.
- Laboratory tests are carried out to compare the samples obtained with the norm (general and biochemical blood tests, general urinalysis, taking a coprogram).
- Conducting instrumental studies allows you to clarify the preliminary diagnosis.
An informative study is esophagogastroduodenoscopy, which allows you to evaluate the gastric mucosa, determine changes in its structure, the source of erosion and the presence of blood discharge. An examination is carried out using an internal examination of the gastric contents using a probe with a sensor at the end. The patient, under the supervision of a doctor, swallows the tube, what happens is visible on the screen. A biopsy is taken - pinching off the required part. The process lasts no more than 5 minutes, but becomes a fundamental study for establishing a final diagnosis.
Esophagogastroduodenoscopy
When conducting clinical studies, the level of acidity must be determined to exclude other diseases of the gastrointestinal tract; the symptoms are sometimes similar.
Treatment with medications
Taking medications is permissible only after consulting a doctor.
The first step is strict fasting for several days and taking special medications to relieve inflammation, regenerate damaged areas of the mucosa, and protect them from further destruction. Sometimes endoscopic bleeding control or emergency surgery is required.
It is unacceptable to take medications on your own, including traditional medicine recipes, without consulting a doctor. Drug treatment of gastropathy is carried out in an outpatient clinic under strict control of taking prescribed medications. Acute hemorrhagic manifestations of gastritis require emergency hospitalization.
Medicines
Types and forms of medications, the course of treatment is selected individually. Usually prescribed:
- antacids: Maalox, Phosphalugel, Gaviscon;
- acidity correctors in the form of H2-histamine receptor blockers: Cimetidine, Ranitidine;
- inhibitors that block acid secretion: Omeprazole, Pantoprazole;
- M-anticholinergics: “Gastrocepin”;
- enveloping, astringent medications: Denol, Sucralfate;
- antibiotics for infections;
- mucus-forming drugs: “Liquiriton”, “Flocarbin”;
- Remarks: “Methyluracil”, sea buckthorn oil, “Oxyferriscorbone”.
Hemostatic therapy is carried out when bleeding develops, which includes the appointment of:
- intravenous infusion of a solution of aminocaproic acid and adrenaline, “Tranexam”;
- intramuscular injection or intravenous infusion of Vikasol, Etamzilate or Dicynone.
For hemorrhagic shock, anti-shock blood substitutes are used or plasma and blood products are infused.
More about pathology
Both men and women are susceptible to the disease. In recent years, statistics indicate a 10-fold increase in cases of detection of this pathology.
Hemorrhages can be single or multiple, located close to each other. The degree, severity and type of the pathological process are determined by their number and size. If proper treatment is provided in a timely manner, then, as a rule, hemorrhages heal without scarring or impaired contractility of the stomach.
Most often, the precursors of gastritis are the following diseases: stress and disorders of the nervous system; improper use of non-steroidal anti-inflammatory drugs; viruses, bacteria, fungi and other pathogens that can cause various diseases of the gastrointestinal tract; irritation of the gastric mucosa due to the use of alcohol or chemicals; disease Crohn's is a chronic disease of the gastrointestinal tract, which is characterized by inflammation of any part of the digestive system, diseases of the circulatory system - blood clots, blockages, any types of embolism, infectious blood lesions, varicose veins, thrombosis and other pathologies that impair blood circulation and cause various pathological processes.
During the intrahemorrhagic period, fresh or coagulated blood is visible on the wall of the stomach, and the mucous membrane bleeds from multiple bleeding spots, spots, or diffusely. In the early posthemorrhagic period, usually no later than several hours after the bleeding has stopped, lesions in the form of dots or cracks covered with coagulated or modified blood may be visible; later they are covered with hematin residues.
Over 24-48 hours, the lesions gradually change color to pale yellow (fibrin) and disappear. If bleeding recurs several times, symptoms of active (ongoing) and recent bleeding may occur simultaneously. In the intrahemorrhagic and early posthemorrhagic period, contents such as coffee grounds can be found in the lumen.
There are many types of gastritis, and they all occur due to disruption of the digestive system. To avoid complications, you must immediately contact a specialist and undergo an examination so that the doctor can determine the cause and severity of the pathology. Knowing this data, you can organize the most effective treatment.
Gastritis cannot appear on its own or suddenly. This disease develops over a long period of time before it begins to manifest itself.
Nutrition and diet
Mode:
- Fractional meals - up to 6 times a day.
- Small portions.
- Eating boiled or steamed foods.
- Avoid overeating.
- Consumption of liquid and semi-liquid foods.
During the diet it is allowed:
- Lean meat, fish.
- Porridge (buckwheat, rice, oats).
- Slimy soups.
- Puree of boiled vegetables and fruits.
- Kissels, weak green tea, herbal decoctions.
Forbidden:
- Pickles, smoked foods, marinades, baked goods, desserts, chocolate.
- Fatty meat (pork, lamb), fish.
- Alcohol in any form.
- Coffee, soda.
- Canned food.
- Milk, sour cream.
- Cabbage.
- Grape.
- Fresh bread.
- Fresh vegetables and fruits.
- Legumes.
Folk remedies
Recipes:
- Lettuce: 25 g of crushed leaves, pour 250 ml of boiling water and leave for 2 hours. Drink 100 ml 2 times a day.
- Thyme: 100 g of herb, 1 liter of dry white wine. The product is infused for 7 days, brought to a boil and left for 6 hours in a warm place. Drink 50 ml before meals 3 times a day.
- Collection of equal quantities of yarrow, centaury, trefoil, mint. You need to pour 25 g of the mixture into 250 ml of boiling water. The product is simmered over low heat for 15 minutes. After filtering, drink 75 ml three times a day before meals.
- Aloe. The juice from the plant must be boiled. Drink chilled 5 g 30 minutes before meals twice a day. You can add a little honey.
- Propolis. The product is taken on an empty stomach, one small piece at a time, for 30 days.