Malaria is a group of infectious diseases caused by parasites of the genus Plasmodium. Mostly found in tropical countries, where it is spread by mosquitoes. Manifested by fever and severe chills. Malaria can kill if not quickly diagnosed and treated.
One mosquito bite can be enough to contract malaria. The infection is especially dangerous for pregnant women and children.
Story
Malaria is believed to be native to West Africa (P. falciparum) and Central Africa (P. vivax). Molecular genetic evidence suggests that the preparasitic ancestor of Plasmodium was a free-living protozoan capable of photosynthesis that adapted to live in the intestines of aquatic invertebrates. It could also live in the larvae of the first blood-sucking insects of the order Diptera, which appeared 150-200 million years ago, quickly acquiring the ability to have two hosts. The oldest mosquito fossils found containing remains of malaria parasites are 30 million years old. With the advent of humans, malaria parasites evolved that were capable of changing hosts between humans and mosquitoes of the genus Anopheles.
About 2-3 million years ago, a mutation occurred in the hominin population that blocked the production of one of the varieties of sialic acid, Neu5Gc, used by the malaria parasite to attach to the host cell. It is likely that the increase in resistance to malaria caused by the mutation contributed to its later establishment in the population, despite the fact that at the same time its effect could be a decrease in fertility. This may have led to the creation of a fertility barrier between mutation carriers and the rest of the population and, ultimately, to the emergence of the hominin lineage ancestral to modern humans.
Other estimates suggest that humans have been suffering from malaria for at least 50,000 years. Time to last common ancestor (TMRCA) for all haplotypes of the malaria-resistant allele FY*O, which arose in Africa, is 42 thousand years ago (95% confidence interval: 34-49 thousand years ago), TMRCA FY*A in non-Africans - at 57 thousand years ago (95% confidence interval: 48-65 thousand years ago). In modern sub-Saharan populations, the FY*O allele reaches a frequency of 86%. The FY*B and FY*A alleles are common in Europe and Asia, but are also found in Africa.
The first chronicled evidence of fever caused by malaria was discovered in China. They date back to approximately 2700 BC. e., during the reign of the Xia dynasty.
Terminology
First you need to define the concept. Malaria is a group of infectious diseases that are transmitted by insects. The virus enters the human body directly after being bitten by a female mosquito of the genus Anopheles (malaria mosquito). After this, the symptoms of malaria are clearly expressed, in some cases leading to death.
Mosquitoes that carry the infection live in regions with an abundance of swamps and a humid, warm climate. Infection is possible not only through a bite - there is another way. In medicine it is called blood transfusion. Its essence is the transfusion of blood from a sick person to a healthy one. Scientists admit that there is also an intrauterine mechanism of transmission of the disease, that is, from mother to child.
Causes and causative agent of malaria
Many people wonder why malaria is common in wetlands. Malaria is an acute infectious disease that is usually transmitted through blood. The cause of infection is some species of mosquitoes that prefer to live in waterlogged areas with a hot climate.
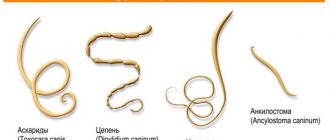
The causative agent of the disease is a parasitic microorganism called Plasmodium. More than 150 varieties of Plasmodium are known, which cause diseases in various animals. Only 5 species among all can infect humans.
Features of types of malaria depending on the type of pathogen:
- Three-day malaria. The incubation period can last from 10 days to 12 months. The prodromal period usually has general symptoms. The disease begins acutely. During the first week, the fever is of an irregular nature, and then a fever is established, in which attacks are repeated every other day. Attacks usually occur in the first half of the day, there is a clear change in the stages of chills, fever and sweating. After 2–3 attacks, the spleen noticeably enlarges, and anemia develops at 2 weeks of illness.
- Ovale malaria in its manifestations is very similar to three-day malaria, but the disease is milder. The minimum incubation period lasts 11 days. Fever attacks most often occur in the evening.
- Quaternary malaria is considered a benign form of malarial infection. The duration of the incubation period usually does not exceed 42 days (at least 25 days), and attacks of fever clearly alternate after 2 days. Enlarged spleen and anemia are rare.
- Tropical malaria is characterized by a short incubation period (on average 7 days) and the presence of a typical prodromal period. Patients with this form of malaria often do not have the typical symptoms of an attack. The period of chills may be mild or absent, the febrile period may be prolonged (up to 30–40 hours), the temperature decreases without significant sweating. Patients experience confusion, convulsions, and insomnia. They often complain of abdominal pain, nausea, vomiting and diarrhea.
The culprit for the development of malaria can only be the mosquito of the genus Anopheles. In total, no more than 20 widows of dangerous mosquitoes are known that can transmit malaria pathogens to humans. Their peculiarity is that they bite at night. In addition, their reproduction occurs in water.
Malaria is a potentially life-threatening parasitic blood disease
Malaria is a potentially life-threatening parasitic blood disease that causes fever and chills.
This disease can be cured if the correct diagnosis is made at an early stage. Unfortunately, this is not always possible in areas of the world that have an underdeveloped health care system and where malaria outbreaks may develop.
What is malaria?
What is malaria?
Malaria is a serious—and sometimes fatal—infectious blood disease caused by parasites that are transmitted to humans through the bite of a female Anopheles mosquito.
According to the World Health Organization, 214 million cases of malaria developed worldwide in 2019, and 438,000 people died from the disease. Most of the dead were children from Africa. Malaria is the most common cause of death of all parasitic diseases.
Causes of malaria
Malaria is caused by infection with Plasmodium parasites, which enter the body through the bite of a female Anopheles mosquito. This is the only type of mosquito that can carry malaria. There are more than 100 species of Plasmodium falciparum that can infect a variety of animal species.
Scientists identify 5 species that specifically infect people:
- Plasmodium falciparum is distributed throughout the world in tropical and suburban areas, mainly in Africa. Most patients who die from malaria die from this type of malarial plasmodium. It can multiply quickly in the body and stick to the walls of blood vessels in the brain, causing the rapid onset of severe illness, including cerebral malaria.
- Plasmodium vivax - common in Latin America, Africa and Asia. It is considered the most common type of malarial plasmodia, in which the high population density in Asia plays an important role. This species can lie dormant in the liver, becoming active and entering the bloodstream months or years after infection, causing relapses in many patients.
- Plasmodium ovale - distributed mainly in West Africa. Morphologically this species is very similar to P. vivax.
- Plasmodium malariae - distributed throughout the world. If left untreated, this type of Plasmodium falciparum can lead to long-term illness.
- Plasmodium knowlesi is common in Southeast Asia and is associated with monkeys. This species multiplies rapidly in the human body, sometimes leading to severe illness.
Each of these malarial plasmodia has its own development cycle duration, which is why, upon infection, a clinical picture of malaria that is specific to each species develops.
How does malaria spread and develop?
How does malaria spread and develop?
The life cycle of malarial plasmodia includes two hosts - a human and a female mosquito from the genus Anopheles. In the human body, parasites first grow and multiply in liver cells, and then in red blood cells. When they multiply in blood cells, plasmodia destroy them, releasing new parasites that continue to penetrate other red blood cells. The multiplication stage of plasmodium in the blood causes symptoms of malaria.
When a female mosquito bites a human, she absorbs the plasmodia in the blood. The parasites in the mosquito's body begin a new cycle of growth and reproduction.
After 10-18 days, the parasites already penetrate the salivary glands of mosquitoes. When insects bite other people, they inject saliva containing plasmodia into their body, which penetrates the bloodstream and first infects liver cells. Thus, the female mosquito carries the disease from one person to another. Unlike the human host, the mosquito vector does not suffer from the presence of parasites.
Because malarial plasmodia are present in the red blood cells of an infected person, malaria can be transmitted through blood transfusions, organ transplants, or sharing needles or syringes contaminated with blood. Malaria can also be transmitted from mother to child before or during childbirth.
Symptoms of malaria
Infection with malarial Plasmodium can lead to a varied clinical picture, ranging from mild symptoms to severe illness and even death. Malaria can be divided into mild and severe (complicated) forms. Basically, it is a curable disease if detected early and treated correctly.
All clinical symptoms associated with malaria are caused by Plasmodium parasites that infect red blood cells. When parasites develop in blood cells, they accumulate numerous known and unknown toxic substances. When infected cells break down and release new plasmodia, these toxins enter the bloodstream and stimulate immune cells to produce cytokines and other substances that cause fever and chills, and also influence other pathophysiological processes associated with malaria.
Symptoms of malaria
Red blood cells infected with Plasmodium falciparum adhere to the vascular endothelium of the venous wall. When this sequestration of diseased cells occurs in the blood vessels of the brain, it results in a severe form of the disease, cerebral malaria. This form is associated with high mortality of patients.
Incubation period
After an infectious mosquito bite, it takes a certain period of time for symptoms of malaria to develop. In most cases, this incubation period ranges from 7 to 30 days. Less time is needed for infection with P. falciparum, more time for P. malariae.
Antimalarial drugs taken prophylactically by travelers can delay the onset of malaria symptoms by weeks or even months. This occurs especially often when infected with P. vivax and P. ovale, which can remain dormant in the liver, becoming active several months after the bite.
This long period of time between infection and the development of symptoms can lead to misdiagnosis because doctors are then unaware of the possibility of malaria. Therefore, people who have traveled in the last 12 months to countries where malaria occurs should always tell their doctors.
Uncomplicated malaria
A classic (but rarely seen) attack of malaria lasts 6-10 hours. It consists of:
- Stages of chills – the patient experiences a feeling of chills and coldness.
- Stage of fever - the patient experiences an increase in temperature, headaches, vomiting, convulsions (in small children).
- Sweating stage – the patient experiences sweating, a return to normal body temperature, general weakness and fatigue.
Classic attacks of malaria occur every second day for infections with P. falciparum, P. vivax and P. ovale, and every third day for infections with P. malariae.
Most often, the patient suffers from a combination of the following symptoms:
- Increased body temperature.
- Chills.
- Sweating.
- Headache.
- Nausea and vomiting.
- Muscle pain throughout the body.
- General malaise.
When examining a patient with malaria, doctors may detect mild jaundice, an enlarged liver and spleen, and an increased respiratory rate.
In countries where cases of malaria are rare, these symptoms may be attributed to the flu, colds, or other common infectious diseases. Conversely, in countries with a high prevalence of malaria, people often mistake these symptoms for malaria and self-medicate without confirming the diagnosis.
Severe malaria
Severe malaria develops when complications of the disease develop.
Manifestations of severe malaria include:
- Cerebral malaria with abnormal behavior, deterioration of consciousness, seizures, coma and other neurological disorders.
- Severe anemia, which develops due to hemolysis (destruction of red blood cells).
- The appearance of hemoglobin in the blood due to hemolysis.
- Acute respiratory distress syndrome is an inflammatory response in the lungs that impairs oxygen metabolism and can develop even after parasites have decreased in response to treatment.
- Blood clotting disorders.
- Fall in blood pressure.
- Acute renal failure.
- Metabolic acidosis (increased acidity of the blood and interstitial fluid).
- Hypoglycemia (low blood glucose levels).
Patients with severe malaria require urgent and intensive treatment.
Relapses of malaria
When infected with P. vivax and P. ovale, patients recovering from the first episode of the disease may have several additional attacks (“relapses”) after months or even years without symptoms. Relapses develop due to the fact that these types of malarial plasmodia can be dormant in liver cells and then activated.
Other manifestations of malaria
Malaria can lead to other symptoms:
- Neurological disorders (problems with movement, paralysis, difficulty speaking, deafness and blindness) may persist after cerebral malaria, especially in children.
- Recurrent infections with P. falciparum can cause severe anemia. This is especially common in children from tropical Africa who have not received adequate treatment.
- Malaria during pregnancy (especially caused by P. falciparum) can cause severe illness in the mother and lead to preterm or low birth weight, stillbirth, miscarriage, and maternal death.
- In rare cases, malaria caused by P. vivax can cause the spleen to rupture.
- Chronic or recurrent malaria caused by P. malariae can cause severe kidney damage.
- Hyperreactive malarial splenomegaly – occurs rarely, due to an abnormal immune response to repeated malarial infections. With this complication, there is a significant enlargement of the spleen and liver, anemia and increased susceptibility to other infectious diseases (for example, respiratory tract infections).
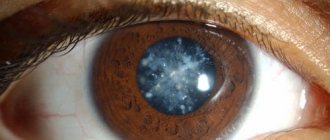
Microscopic diagnosis of malaria
Diagnosis of malaria
It is very important to quickly diagnose malaria in order to provide timely treatment and prevent further spread of the disease in the community through mosquito bites.
The presence of malaria can be suspected based on the person's travel history to countries where the disease is common and the clinical picture. However, laboratory methods are needed to establish a definitive diagnosis.
Microscopic diagnostics
Malarial plasmodia can be detected by examining a thick drop of blood using a microscope. Before examination, the sample is stained to give the plasmodia its characteristic appearance. This method remains the gold standard for laboratory diagnosis of malaria. However, it depends on the quality of the reagents, the microscope and the experience of the laboratory technician.
Antigen detection
Various test kits are available to detect Plasmodium falciparum antigens. These tests are an alternative to microscopic examination in conditions where the latter is not possible. However, for their wider use it is necessary to improve their accuracy and reduce their price.
Molecular diagnostics
Polymerase chain reaction can detect the nucleic acids of Plasmodium falciparum. Although this technique may be more sensitive than microscopy, its use in diagnosing malaria is of limited value. It is most useful for identifying the type of parasite.
Serological tests
Serological tests detect antibodies against Plasmodium falciparum. They do not detect a current infection, but rather indicate a previous infection.
Treatment of malaria
Treatment of malaria
Malaria is treated with antimalarial drugs and medications to control symptoms, including fever medications, seizure medications, solutions, and electrolytes.
The choice of antimalarial drug and duration of treatment depends on:
- A type of malaria.
- The region in which the person became infected with malaria.
- The severity of the clinical picture.
- Whether the patient took antimalarial drugs for prophylactic purposes.
- The patient's age.
- Whether the patient is a pregnant woman.
Antimalarial drugs include:
- Chloroquine.
- Quinine.
- Hydroxychloroquine.
- Combination of artemether and lumefantrine.
- A combination of atovaquone and proguanil.
- Mefloquine.
- Clindamycin.
- Doxycycline.
Doctors may prescribe combinations of different antimalarials to overcome Plasmodium resistance to one drug. These medications are usually taken as tablets or capsules, but in very severe cases intravenous administration may be necessary.
Treatment of malaria during pregnancy is complicated by the fact that many antimalarial drugs are contraindicated during this period. Therefore, it is better for pregnant women to avoid traveling to areas with a risk of contracting malaria.
Prevention of malaria
Prevention of malaria
When traveling to regions where malaria is common, the risk of infection is quite high. Therefore, it is very important to take measures to prevent this disease.
For the prevention of malaria it is important:
- Knowledge about the risk of infection.
- Preventing mosquito bites.
- Taking antimalarial drugs for prophylactic purposes.
Knowledge about the risk of infection
Before traveling to any country, you should find out whether there is a risk of contracting malaria. In addition, the risk of infection is higher for tourists who travel outside cities.
Preventing Mosquito Bites
It is impossible to completely avoid mosquito bites. However, the fewer bites, the lower the risk of infection.
The following measures will help reduce their number:
- You should live in a room with good air conditioning, as well as protective devices on windows and doors. If this is not possible, you need to make sure that the windows and doors close well.
- You should sleep in a well-air-conditioned room or on a bed with an intact insecticide-treated mosquito net.
- You should apply repellent to your skin, even at night before going to bed. The most effective are products containing diethyltoluamide.
- Long sleeved pants and shirts should be worn. This is especially important in the evening and at night, when mosquitoes become especially active.
Taking antimalarial drugs for prophylactic purposes
A person traveling to areas at risk of contracting malaria should always take anti-malarial drugs. With their help, it is possible to reduce the risk of infection by 90%.
The choice of the appropriate remedy depends on the geographic region of travel and the person’s health status. For example, pregnancy, old or young age, the presence of diseases, allergies or hypersensitivity to the drug are of great importance. It is very important to strictly follow your doctor's instructions about taking the antimalarial drug. Most people who contract malaria while traveling do not take preventive medications or follow the correct regimen.
Drug prophylaxis can be carried out before the trip (in order to determine the tolerance of the drug used), during the trip and after returning home (to eliminate all parasites from the body).
Most patients with uncomplicated malaria improve within 48 hours of starting treatment
Prognosis for malaria
Most patients with uncomplicated malaria improve within 48 hours of starting treatment and return to normal body temperature within 96 hours.
Patients with P. falciparum malaria who are not treated have a poor prognosis with high mortality. Early diagnosis and proper treatment make this prognosis favorable.
Most of the patients who died from malaria were children under 5 years of age who lived in Africa.
Cerebral malaria ends in death in 20% of patients.
Cryptosporidiosis is one of the important causes of diarrheal diseases in the world
Symptoms
The disease occurs with periods of exacerbation of fever and normal state. Main symptoms of malaria:
- attacks of fever (chills, fever, sweating);
- anemia (anemia);
- enlargement of the spleen and liver (hepatosplenomegaly);
- decrease in the number of red blood cells and platelets (pancytopenia).
As with most infectious diseases, there are three forms of severity of malaria - mild, moderate, severe.
The onset of the disease is sudden. It is preceded by an incubation period (the period of time from infection to the onset of the disease).
It amounts to:
- vivax malaria – 10-21 days (sometimes up to 10-14 months);
- four-day malaria – from 3 to 6 weeks;
- tropical malaria – 8-16 days;
- ovale malaria – 7-20 days.
Sometimes there is a prodromal period (the time of onset of malaria, accompanied by initial, mild symptoms). The patient experiences weakness, chilling, thirst, dry mouth, pain in the head. Then a fever of the wrong type suddenly appears.
The first week of the febrile period is characterized by attacks occurring several times a day. In the second week, paroxysms acquire a clear cyclic course, repeating every other day or two (with four-day fever).
The duration of the paroxysm is from 1-2 hours to 12-14 hours. A longer period is determined for tropical malaria. It can last a day or even more than 36 hours.
Attack phases:
- chills – lasts 1-3 hours;
- fever - up to 6-8 hours;
- profuse sweating.
Complaints and symptoms during malarial paroxysm:
- hyperthermia – up to 41° C;
- severe headache;
- muscle pain;
- vomiting and severe dizziness are often observed;
- general agitation;
- pain in the lumbar region;
- redness of the face and sclera;
- rapid pulse;
- blood pressure is reduced;
- skin is hot and dry;
- hands and feet are cold;
- on the mucous membranes of the face - the manifestation of herpetic rashes;
- the liver and spleen are enlarged.
After sweating comes sleep. During the interictal period, patients are able to work, but as the disease progresses, their condition worsens, there is loss of body weight, jaundice, and the skin becomes sallow in color.
Tropical malaria is the most severe. In her case, the following are added to the described symptoms of malaria:
- severe pain in the joints and throughout the body;
- signs characteristic of meningitis;
- delusional state of consciousness;
- attacks of suffocation;
- frequent vomiting with blood;
- pronounced enlargement of the liver.
In the first week of illness, attacks can occur, layering on each other. A few months after the onset of the disease, paroxysms begin to recur, but in a milder form.
Of all the described forms of malaria, vivax is the most mild. The largest number of relapses is observed with Chesson malaria (Pacific form).
Specifics of the development of infectious pathology
The morphology of plasmodia provides for a gradual transformation. In the first 30 minutes after human infection, Plasmodium retains the sporozoite form. This stage of the parasite life cycle is called sporogony.
“Several thousand daughter cells can develop from a single sporozoite, enhancing the progression of the disease.”
Subsequent stages of development of the pathogen determine all the pathological processes that characterize the clinical picture of malaria.
- Tissue schizogony.
Moving along with the bloodstream, plasmodia penetrate liver hepatocytes and are divided into forms of fast and slow development. Subsequently, chronic malaria arises from a slowly developing form, causing numerous relapses. After destroying liver cells, plasmodia penetrate blood vessels and attack red blood cells. At this stage, clinical symptoms of malaria do not appear.
- Erythrocyte schizogony.
Having penetrated into erythrocytes, schizonts absorb hemoglobin and increase in size, which causes the erythrocyte to rupture and the release of malarial toxins and newly formed cells - merozoites - into the blood. Each merozoite again invades the erythrocyte, starting a repeat cycle of damage. At this stage of malaria, a characteristic clinical picture appears - fever, enlargement of the spleen and liver.
- Gametocytogony.
The final stage of erythrocyte schizogony, which is characterized by the formation of plasmodium germ cells in the blood vessels of human internal organs. The process is completed in the mosquito’s stomach, where gametocytes enter along with the blood after the bite.
The life cycle of Plasmodium, which causes malaria, is presented in the video below.
Developing in the human body, plasmodia provoke the production of volatile substances, the smell of which attracts other anafeles mosquitoes. Thus, parasites contribute to the spread of infection.
The length of the Plasmodium life cycle affects the incubation period of malaria.
Consequences
There are multiple consequences of malaria. They can occur both in the acute period of the disease (that is, in the stage of early manifestations) and after.
The consequences of malaria are:
- Toxic shock. In this case, damage to vital organs such as the liver, kidneys, and lungs is noted. During shock, blood pressure first drops, sometimes reaching 50 - 40 millimeters of mercury (with a normal range of 90 to 120). The development of hypotension is associated both with a violation of vascular tone (vessels dilate and pressure drops) and with a violation of cardiac activity. In shock, patients' breathing becomes shallow and erratic. The main cause of mortality during this period is developing renal failure. Due to a sharp decrease in blood pressure, hypoperfusion (insufficient blood supply) of the renal tissue occurs, resulting in renal ischemia. Since the kidneys remove all toxins from the body, when they lose their function, all metabolic products remain in the body. The phenomenon of autointoxication occurs, which means that the body is poisoned by its own metabolic products (urea, creatinine).
- Malarial coma. As a rule, it is a complication of tropical malaria, but can also be a consequence of other forms of malarial invasion. This complication is characterized by a staged, but at the same time, rapid course. Initially, patients complain of severe headache, repeated vomiting, and dizziness. They experience lethargy, apathy and severe drowsiness. Over the course of several hours, drowsiness worsens and a soporous state develops. During this period, convulsions, meningeal symptoms (photophobia and muscle rigidity) are sometimes observed, and consciousness becomes confused. If there is no treatment, a deep coma develops, during which blood pressure drops, reflexes disappear, and breathing becomes arrhythmic. During a coma, there is no reaction to external stimuli, vascular tone changes and temperature regulation is disrupted. This condition is critical and requires resuscitation measures.
- Acute massive hemolysis. Hemolysis is the premature destruction of red blood cells. Normally, the life cycle of an erythrocyte is about 120 days. However, in malaria, due to the fact that the malarial plasmodium develops in them, the destruction of red blood cells occurs much earlier. Hemolysis is the main pathogenetic link in malaria. It causes anemia and many other symptoms.
- Acute renal failure. This consequence is due to the massive destruction of red blood cells and the release of hemoglobin from them. Hemoglobin begins to appear in the urine (this phenomenon is called hemoglobinuria), giving it a dark color. The condition is complicated by low blood pressure. Renal failure in malaria is manifested by oliguria and anuria. In the first case, the daily amount of urine is reduced to 400 milliliters, and in the second - to 50 - 100 milliliters. Symptoms of acute renal failure are rapid deterioration of the condition, decreased diuresis, and dark colored urine. In the blood there is a disturbance in the water-electrolyte balance, a shift in the alkaline balance, and an increase in the number of leukocytes.
Pathogenesis
The following factors are essential in the pathogenesis of tropical malaria:
- the high reproductive capacity of sporozoites and erythrocyte polyparasitism with a slow immune response ensure an explosive increase in parasitemia, reaching 10-30%;
- merozoites Pl., which are the causative agent of malaria. falciparum affects erythrocytes of all age groups, including the physiologically most loaded mature erythrocytes;
- massive disruption of invaded and non-invaded red blood cells causes the rapid development of anemia and hemic hypoxia;
- loss of membrane elasticity by invaded erythrocytes, changes in their electrical potential and antigenic structure of the membrane leads to the formation of microconglomerates that “clog” the functioning capillaries of parenchymal organs and tissues, which causes tissue hypoxia, release of biologically active substances, shunting with the inclusion of anastomoses, circulatory and hypoxic hypoxia; “shock” organs are formed: kidneys,
- lungs,
- liver,
- intestines,
- adrenal glands,
- heart,
- brain;
Diagnostics
Diagnosis of malaria is based on identifying the classic symptoms of the disease: paroxysmal fever, enlarged liver and spleen.
Anemia is always detected in the patients' blood. Of great importance is the fact of being in a dangerous area for 3 years before the onset of the disease, or blood transfusion or medical procedures associated with a violation of the integrity of the skin or mucous membrane within 3 months before the onset of fever.
The most accurate diagnostic method is the detection of malarial plasmodium in the blood. Currently, special diagnostic kits are widely used that make it possible to determine the presence of a pathogen in the blood in a short time.
Malaria in pregnant women
Malaria adversely affects the course of pregnancy and its outcome. It can cause abortion, miscarriage and premature birth. Fetal developmental delay and death are often observed. Malaria is often the cause of eclampsia in pregnant women and death. Pregnant women living in areas where malaria is endemic are the most endangered population. Late diagnosis and inadequate treatment quickly lead to the development of “malignant malaria.” The development of hypoglycemia is especially dangerous in pregnant women, which often causes death.
Rice. 18. Placenta infected with malarial plasmoids.
Treatment of uncomplicated cases of malaria
For the treatment of uncomplicated cases of malaria caused by P. falciparum parasites, WHO recommends the use of artemisinin combination therapy (ACT). Combining two active components with different mechanisms of action, ACT is by far the most effective antimalarial agent. WHO currently recommends five ACTs against P. falciparum malaria. The choice of ACT should be based on the results of therapeutic efficacy studies against local strains of the malaria parasite P. falciparum.
ACTs are the main recommended treatment for P. falciparum malaria and their effectiveness must be maintained as alternative drugs to artemisinin derivatives are not expected to reach the market for several years. WHO recommends regular monitoring of the effectiveness of antimalarial drugs used in national malaria control programs to ensure that the chosen treatments remain effective.
In areas of low transmission, antimalarial treatment should be supplemented with a single low dose of primaquine to prevent transmission. However, testing for glucose-6-phosphate dehydrogenase (G6PD) deficiency is not required because a single dose of primaquine is effective in blocking transmission and rarely causes serious toxicity in patients with any form of G6PD deficiency.
Malaria in children
The most vulnerable age is children from 6 months to 4 - 5 years. Malaria is especially dangerous for young children.
In malaria-endemic regions, the disease in children is one of the causes of high mortality. Children under 6 months of age born from immune mothers do not develop malaria.
Types of malaria in children
Malaria in children can be congenital or acquired.
In congenital malaria, parasites enter the fetal blood from the mother's blood through a damaged placenta during pregnancy and through the umbilical cord during childbirth or birth trauma. Children infected in utero are born hypotrophic and premature. After birth, weight gain is slow.
Symptoms of malaria in young children
Malaria in children often develops a fulminant course. Severe anemia and a cerebral form of the disease may develop within a few days. Malaria in children often occurs in a peculiar way:
- the skin is pale, often with an earthy tint, yellowness and waxiness persist for a long time, despite treatment;
- malarial paroxysms (fever attacks) are often absent;
- symptoms such as cramps, diarrhea, regurgitation, vomiting and abdominal pain come to the fore;
- during attacks of malaria there are often no chills at first, and at the end of an attack of fever there is often no sweating;
- a rash in the form of hemorrhages and spotty elements often appears on the skin;
- anemia increases quickly;
- with congenital malaria, the spleen is significantly enlarged, the liver - to a lesser extent.
Symptoms of malaria in older children
In older children, the disease progresses as in adults. During the interictal period, the children's condition remains satisfactory. The fulminant form of three-day malaria is rare, and malarial coma is extremely rare.
Treatment of severe cases of malaria
To treat severe cases of malaria, artesunate injections (intramuscular or intravenous) should be given for at least 24 hours, followed by a full three-day course of ACT as soon as the patient is able to tolerate oral medications. If injectable drugs are not available, children under 6 years of age with severe malaria should be given prehospital treatment with artesunate suppositories, after which they should be immediately referred to a health facility where they can receive adequate treatment.
It is extremely important not to use either injectable artemisinin-based drugs or artesunate suppositories as monotherapy - the initial course of treatment of severe forms of malaria with these drugs must be supplemented with a three-day course of ACT. This is necessary to ensure complete cure and prevent the development of resistance to artemisinin derivatives.
Treatment of P. vivax infection
Treatment of P. vivax infections should be with ACT or chloroquine in areas where P. vivax does not have resistance to chloroquine. In areas where P. vivax has been shown to be resistant to chloroquine, infections should be treated with an ACT, preferably one where the co-drug has a long half-life. With the exception of the combination of artesunate with sulfadoxine-pyrimethamine (AS+SP), all ACTs are effective against the spread of P. vivax infection in the bloodstream.
In order to prevent relapses, primaquine should be prescribed in addition to the main treatment; the dose and frequency of administration should be determined taking into account the enzyme activity of glucose-6-phosphate dehydrogenase (G6PD) in a particular patient.
Expanding access to ACT
Access to ACT has expanded significantly in recent years. By the end of 2016, ACT had been accepted as first-line treatment in 80 countries. Countries administered an estimated 409 million courses of artemisinin combination therapy (ACT) in 2019, up from 311 million courses in 2019.
More than 69% of such courses were distributed through the public sector. The number of ACT courses distributed through the public sector increased from 192 million in 2013 to 198 million in 2016, with the majority (99%) distributed in the WHO African Region.
Antimalarial immunity
Immunity to malaria is classified into 3 types:
- congenital;
- acquired active;
- acquired passive.
Innate immunity is associated with the presence of substances in the body that kill parasites. For example, most Africans have the Duffy group antigen, which makes the body immune to infection with three-day malaria.
And also erythrocyte genetic factors of immunity are:
- a violation of the structure of hemoglobin, which is typical for people with sickle cell anemia;
- low ATP level;
- deficiency of the enzyme glucose-6-phosphate dehydrogenase.
People with these factors are relatively resistant to falciparum and vivax plasmodia.
Active acquired immunity in malaria is formed after infection. It is unstable, short-lived, and is developed only against the erythrocyte stages of Plasmodium.
The indigenous inhabitants of tropical Africa with a high level of malaria, the causative agent of which is Plasmodium falciparum, develop intense passive immunity against the background of repeated reinfections.
Prevention
Preventive measures include timely identification and treatment of patients with malaria and carriers of malarial plasmodium, conducting epidemiological surveillance of endemic regions, extermination of mosquitoes and the use of remedies for their bites.
A vaccine against malaria has not yet been developed. Specific prevention of malaria involves the use of antimalarial drugs. Persons traveling to endemic areas must undergo a course of chemoprophylaxis with Hingamin, Amodiaquine, and Chloridine. For greatest effectiveness, it is recommended to alternate these drugs every month.
You can protect yourself from mosquito bites by using natural or synthetic repellents. They are collective and individual and are available in the form of spray, cream, gel, pencils, candles and spirals.
Mosquitoes are afraid of the smell of tomatoes, valerian, tobacco, basil oil, anise, cedar and eucalyptus. A couple of drops of essential oil are added to vegetable oil and applied to exposed areas of the body.
Data
Malaria is a disease caused by the parasitic protozoan Plasmodium, which infects an average of 200 million people a year around the globe. As a result, 500,000 deaths occur due to this cause. The causative agent of malaria enters the body through the bites of malaria mosquitoes. What happens next? The malaria parasite goes through a complex life cycle in the body of a mosquito and then in the body of the infected person. The cycle repeats if a mosquito bites a person who is already infected and has the parasite in their blood that causes the disease “malaria.” A photo of the pathogen is presented below.
The areas with the highest mortality rates from this disease are Africa, Asia, and Central and South America. Malaria is a disease that affects a very large number of people visiting these areas. In sub-Saharan Africa, the majority of cases (86%) are children under 5 years of age. About 40% of the world's population is at risk of infection. The incubation period ranges from one to three weeks. Some people can become carriers of so-called sleeping parasites. In this case, activation of the infection can occur several months or even years after the malaria plasmodia enter the body.
Summary
The risk of getting this disease exists not only in Africa, but also in some countries in Asia and Latin America.
Susceptible to infection:
- Women during pregnancy. If infected, there is a risk of miscarriage, as well as death of the mother and fetus;
- HIV – infected and sick with AIDS;
- People who are not immune to the disease.
The most effective measures to combat the disease is the destruction of malaria mosquitoes. Indoors must be sprayed with a special agent, and a mosquito net must be installed on the windows.
In addition, before going outside, it is advisable to lubricate the skin with a protective cream. If possible, avoid wearing revealing clothing.
Source: 101parazit.com
Types of disease
The main types of pathogens of the disease were named above. The course of the disease may also vary. Let's name the main types of malaria:
- tropical;
- three-day;
- four-day;
- malaria-ovale.
Quadrennial malaria is characterized by six to ten hour-long bouts of fever that usually begin in the morning or afternoon. Severe consequences rarely develop; the incubation period can be up to 5 months. Tropical malaria is characterized by a high concentration of parasites in the blood, the fever is not clearly expressed, and symptoms such as diarrhea, vomiting, damage to the central nervous system, and renal failure are often present. Complications often develop. Three-day malaria is manifested by severe fever, including chills, increased sweating and fever, but with indistinct alternation with periods of remission.
How is it transmitted?
So, let's take a closer look at how the malaria pathogen enters the body and develops in it. The life cycle of the malaria parasite Plasmodium is complex; the microorganism has two hosts: humans and the malaria mosquito. As mentioned above, the disease is transmitted through an insect bite, in which the parasite enters directly into the blood.
Sporozoites (immature plasmodia) travel through the human bloodstream and enter the liver. There they mature and infect red blood cells - erythrocytes, inside which they develop until the patient is again bitten by the malaria carrier - the mosquito. Once in the body of an insect, plasmodia penetrate its salivary glands, and with the next bite, in the form of sporozoites, they again begin their life cycle in the human blood.
The developmental processes of species such as P. ovale and P. vivax can be even more complex and involve the formation of inactive forms, hypnozoites, which often remain inactive for weeks or even years. In the body of the malaria mosquito, plasmodia go through the sexual period of their life cycle, and in the human body the pathogen remains in an asexual phase, which is also called schizogony. Therefore, the development cycle of Plasmodium in red blood cells is called erythrocyte schizogony.
How is the infection transmitted? Its sources are female malaria mosquitoes and an infected person (both the patient and the carrier). It is worth noting that malaria is a disease that is not transmitted among people either through household or airborne transmission. Infection can only occur if the blood of a sick person enters the body of a healthy person.
Sequence of occurrence of malaria
Plasmodium first enters the human liver. There they grow quietly and gradually develop. This usually takes about 2-4 weeks. As soon as plasmodia mature, they move from the liver into red blood cells, where they continue their active reproduction.
There are other methods of contracting the disease.
In total, there are three variants of transmission of plasmodium:
- A mosquito bite that carries infected blood. This is the most common type of infection.
- Use of medical instruments that have not been sterilized after use on patients with malaria.
- Transplacental.
Outbreaks of the disease have been recorded in the countries of Southern and Western Africa. These countries are considered to be the birthplace of this unpleasant disease. Malaria is also found in the countries of Southeast Asia. In Europe, the disease is the exception rather than the rule. The main cases of infection are imported malaria, which patients become infected with from tourists from African or Asian countries or after traveling to hot continents.
Folk remedies
Medicines are the mainstay of malaria treatment. But many sources indicate the benefits of some natural remedies in the treatment of disease caused by Plasmodium. Here we publish only a few of them, and in no case should these recipes and recommendations be considered as the main means of treatment.
Lime and lemon are beneficial for four day fever. About three grams of chalk are dissolved in 60 ml of water and the juice of one lemon or lime is added. This composition must be drunk before the onset of fever.
Alum is also considered as a supportive agent in the treatment of malaria. They are fried in a hot frying pan and ground into powder. Take a teaspoon of the drug internally four hours before the expected fever and half a teaspoon two hours after it.
Malaria is an infectious parasitic disease with vector-borne transmission, the causative agent of which is protozoan unicellular microorganisms. The main characteristic feature of malaria is the development of fever with enlargement of the liver and spleen.
Disease during pregnancy
Malaria is a serious threat to a pregnant woman and her fetus. Infection significantly increases the risk of preterm birth and stillbirth. Statistics show that in sub-Saharan Africa, up to 30% of children die from malaria every year. Therefore, all pregnant women who live in dangerous areas or are planning a trip there should definitely consult a doctor and take prescribed medications, for example, Sulfadoxine-pyrimethamine. This is a necessary prevention of malaria to avoid infection.
Treatment of the disease in women expecting a child is carried out according to the standard scheme discussed above. However, drugs such as Primaquine, Tetracycline, Doxycycline and Halofantrine are not recommended due to potential danger to the fetus.
How to treat the disease?
There are few drugs available to treat malaria. The most popular drug is considered to be quinine, which has had no analogues for several decades. Doctors from time to time made attempts to replace quinine with other medications, but the results of treatment showed that it was necessary to return to a proven remedy.
It is important for the patient to provide a number of conditions:
- Prevent the possibility of hypothermia.
- Guarantee complete peace.
- Control your drinking regime.
- Follow the special diet prescribed by the doctor.
With proper treatment, the disease recedes. Otherwise, the possibility of relapse of the disease remains. Moreover, this can happen either in a few weeks or in a few months. The reason for relapses is that plasmodia remain in the liver, where they continue to develop and reproduce, only to make themselves felt again in the most unpleasant way after some time.
No one can cope with malaria on their own. At the first hint of this tropical disease, you should urgently seek help from qualified specialists.
Complications of malaria
In weakened or untreated patients, as well as in case of treatment errors, the following complications may develop:
- malarial coma;
- edema syndrome;
- extensive hemorrhages (hemorrhages);
- different types of psychoses;
- renal and liver failure;
- infectious complications;
- splenic rupture.
A separate complication of malaria should be noted hemoglobinuric fever . It develops against the background of massive proliferation of plasmodia, during treatment with medications, due to the destruction of red blood cells (hemolysis). In severe cases of this complication, a progressive decrease in urine production is added to the general symptoms and complaints of an attack of malaria. Fulminant renal failure develops, often with early death.
Preventive actions
Preventive work is carried out at the site of infection through the use of mosquito nets and insecticides, which are used to treat areas where mosquitoes accumulate. At home, it is necessary to use repellents, aerosols and ointments that repel mosquitoes and cause their death.
If a possible infection is suspected, medications are taken in doses prescribed by an infectious disease specialist.
Vaccine prevention is currently being developed.
People located in the epicenter of the epidemic are subject to isolation and laboratory examination if an elevated temperature occurs. The earlier treatment is started, the better the result. People arriving from countries with malaria outbreaks must be examined. Those who have recovered from the disease must be observed by an infectious disease specialist for 3 years.
You will receive more detailed information about the causative agent of malaria, symptoms of the disease and modern methods of treatment by watching the video review:
Lotin Alexander, radiologist
21, total, today
( 156 votes, average: 4.74 out of 5)
Cholera: symptoms, causes, treatment and prevention methods
Types of tapeworms and how to treat them
Related Posts
Vaccine
There are currently no vaccines available for malaria. However, over the past few years, researchers have seen good results with experimental vaccines. The latest large clinical trial involving children in eight African countries, sponsored by the Bill Gates Foundation, found that the drug being studied was effective in half the cases. Many other experiments have also become successful and predict reliable protection against the described disease in the near future. Experts say that a vaccine against malaria will appear within 3-10 years. The intended action is based on interrupting the life cycle of the parasite using a protein drug that produces antibodies against it.
Signs
Malaria is a disease whose symptoms include chills, fever, headaches and muscle pain. Some patients experience nausea, vomiting, cough and diarrhea. A fever that occurs every one, two or three days is the most typical manifestation of malaria. Shivering and a feeling of cold are replaced by the so-called hot stage, which is characterized by high fever, cramps, headaches and vomiting.
Complications are often signs of a form of the disease such as tropical malaria. Due to the destruction of red blood cells and liver cells, jaundice of the skin and whites of the eyes, as well as diarrhea and cough, may occur. In more rare cases, a rash appears on the body in the form of itchy reddish papules. Malaria is determined by these signs. A photo of the carrier of the disease is presented above.
Severe forms, for example, if the causative agent of malaria is Plasmodium falciparum, are accompanied by problems such as:
- bleeding;
- liver and kidney failure;
- shock and coma;
- damage to the central nervous system.
Without timely treatment, these symptoms often lead to death.