Any person over 40 years old has a good chance of discovering an intestinal polyp. Doctors diagnose benign neoplasms of the digestive tract in every tenth patient from this age group. It is important to identify polyps in the intestines as early as possible, while their size is small and the possibility of degeneration into a malignant tumor is low.
What causes polyps in the intestines?
Polyposis (ICD code 10 – D12) refers to diseases with an unknown etiology (occurrence). This means that modern medicine still cannot determine the cause of the appearance of tumors in the intestines. There are three theories that explain the appearance of tumors, but none of them has been proven. Each of them has a scientific basis, but only considers one of the key factors of polyposis:
- Inflammatory theory. The formations represent an intermediate stage between a cancerous tumor and the local inflammatory process of the organ, while being a benign formation.
- The disregenerative theory states that the disease is a violation or too frequent random activation of the process of regeneration of damaged cells, which leads to an increase in growth in this place.
- Embryonic theory. Argues that pathological embryonic development of mucous membranes due to injury or inflammation is involved in the appearance of tumors.
A different approach to the root cause does not contradict the fact that the reasons for the formation of polyps in the intestines are as follows (as most experts agree):
- genetic predisposition (hereditary factor);
- unhealthy diet with dominance of animal fats and carbohydrates;
- sedentary lifestyle;
- reflux disease;
- pathology of the intestines.
Causes
If a person develops polyps in the intestines, the condition is called polyposis. In itself, it is not malignant, but is considered by doctors as a precancerous disease, which, if left untreated, can develop into an oncological tumor.
The following are the causes and contributing factors that can affect the formation of polyps in women and men:
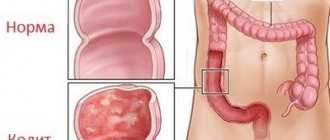
- Chronic colitis, typhoid fever, enteritis or dysentery. In this condition, the large intestine becomes a breeding ground for pathogenic bacteria. Moreover, such diseases provoke stagnation of feces in the intestines, which also increases the likelihood of polyp formation.
- Diseases in which the rectum, as well as other areas of the digestive system, become inflamed. It was found that polyps cannot form in completely healthy tissues. For successful development, they need inflammatory processes that are localized in the mucous membrane and lead to degeneration of the epithelium.
- External factors. For example, smoking, poor diet, stress and abuse of strong alcoholic beverages greatly influence the appearance of polyps. Moreover, living in a polluted ecological environment and consuming products with chemicals have a negative impact on the functioning of the gastrointestinal tract.
- Vascular diseases. Atherosclerosis, which tends to constantly progress, has a particularly negative effect on the condition of the intestinal mucosa.
- An individual genetic predisposition to such a disease can cause the appearance of polyps in a child . Moreover, as recent observations show, unfortunately, intestinal polyposis is “getting younger” and can now easily be diagnosed even in preschool children.
- A food allergy, particularly gluten intolerance. In this state, a person cannot digest protein. When it enters the digestive system, the latter begins to react violently to it. She perceives protein as a foreign component that damages the intestinal mucosa. This can increase the likelihood of polyp formation.
In addition, the following theories of polyp formation are distinguished, which scientists have divided into several sections:
- Formations that arose due to the influence of gastritis and stomach ulcers (read about the diagnosis of stomach ulcers in this article).
- An inflammatory process of the reproductive system in women, which leads to polyposis of the small intestine.
- The influence of cholelithiasis.
Symptoms of polyps in the intestines in adults
A rectal polyp, like a colon polyp, is not detected in most clinical cases and does not have any special symptoms. Treatment is very difficult to start on time. Often therapy begins when the form is already developed. The combined symptoms of polyps in the intestines can make you think about going to the doctor. In case of general manifestations of a possible disease, you should consult a specialist. The signs of the disease are as follows:
- abdominal discomfort with severe pain;
- problematic, uncomfortable bowel movements;
- the presence of blood and mucus in the stool;
- frequent urge to go to the toilet;
- periodic unsystematic loose stools;
- alternating constipation, obstruction, diarrhea;
- abdominal pain, vomiting, itching, burning in the anal canal area, the appearance of mucus stripes on the stool (typical of colon polyposis).
- Can MRI replace colonoscopy?
- Treatment of polyps in the gallbladder without surgery
- Blood from the anus - causes of symptoms, diagnosis of diseases and how to stop bleeding
Other possible complications
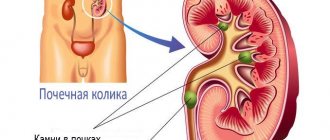
Due to polyps, the intestinal lumen can be blocked and the passage of stool is disrupted. Because of this, abdominal pain and constipation bother me. With large polyps, intestinal obstruction develops - a dangerous condition that requires immediate treatment.
Constant intestinal bleeding leads to anemia - a decrease in the level of red blood cells and hemoglobin in the blood. Signs of this condition: pallor, dizziness, headaches, weakness, increased fatigue, decreased performance.
Symptoms of polyps in the intestines in children
A child cannot independently determine the presence of a disease, so parents should monitor the well-being of their children. The main signs of polyps in the intestines in children are the same as in adult patients. If there is problematic stool or blood formations in the stool, the child should be shown to a doctor. In young patients, there are several types of formations:
- Juvenile polyps. They form at 3-6 years of age, most resolve on their own without consequences.
- Lymphoid polyposis. The development of the disease occurs from six months to the time of puberty. Primary processes are formed at the age of 1-3 years. This form is subject to mandatory treatment due to the danger of pathologies, bleeding, constant discomfort, and problems with bowel movements.
- Peutz-Jeghers syndrome. The disease is predominantly hereditary. The formations are localized in the small intestine or rectum. Long-term development and a positive outlook do not cancel mandatory treatment.
- Adenomatous polyposis (familial polyposis of the colon). Massive growth of formations up to 3000 units of unequal volumes, which tend to malignize.
- Gardner's syndrome. Multiple polyposis when tumors are localized not only in the intestines, but also in the stomach (hyperplastic formations) and the thyroid gland.
Prognosis and prevention
Can a polyp in the intestine disappear on its own? No, such tumors do not resolve; they must be removed surgically.
The prognosis of the disease is favorable if the formation is detected and eliminated in time. The longer the growth exists, the greater the likelihood of it turning into a malignant tumor.
Almost 30% of patients experienced a relapse within several years after removal of tumors (polyps can grow again). People with a history of this disease should have an endoscopic examination every year.
In order to prevent the development of the disease, it is necessary:
- eat right: avoid eating fatty and fried foods, alcohol, carbonated drinks, introduce vegetables, fruits, and seafood into the diet;
- get rid of bad habits;
- treat constipation effectively and promptly;
- lead a healthy lifestyle, play sports, walk in the fresh air.
People who are at risk of developing pathology need to monitor their health especially carefully. If close blood relatives are diagnosed with formations in the intestines, it is necessary to conduct regular examinations.
Types of polyps in the intestines
Depending on the location in the body, the modern endoscopic classification of polyps distinguishes the following types:
- Juvenile. A childhood form of the disease that affects the mucous tissue of the rectum. It looks like a bunch of grapes with a smooth surface (pedunculated polyp). Such formations do not develop into malignant forms.
- Hyperplastic. Cone-shaped formations of small sizes (2-4 mm). Even in large quantities, they manifest themselves as thickening of the intestinal mucosa. They rarely turn into cancer.
- Ferrous. The most common form of the disease, the second name is adenomatous polyps. The formation is round in shape, with a large increase of more than 2 cm, malignancy occurs in 50%.
- Villous - both of the same name and glandular-villous. Such hyperplastic polyps have a carpet or nodular shape, located on a wide base. Localized in the rectum and sigmoid colon. In 90% of cases they turn into an oncological form.
Can a polyp develop into cancer?
This question is asked by almost every patient who is faced with the detection of polyps. Although the formation itself is benign, it has a tendency to degenerate: it all depends on the patient’s age, gender, and localization of the formations. Above were approximate risk groups with the probability of a cancer outcome for various types of neoplasms.
For different locations, the degeneration of a polyp into cancer is predicted as follows:
- Stomach polyp cancer. It is extremely difficult to diagnose because the symptoms have signs of a peptic ulcer. Gastric adenocarcinoma suggests that only 5-15% of patients live longer than 5 years. Only timely diagnosis and complete removal of the tumor at an early stage gives a high chance of a positive result.
- Neoplasms in the uterus. Their formation occurs from excessive growth of uterine tissue. In most cases, they are not dangerous, but in women after 50 years of age, the likelihood of polyposis transforming into cancer increases sharply.
All other localizations of formations are at risk of degeneration into a cancerous tumor. If polyposis is detected, you should be regularly checked by a specialist, and adhere to the prescribed rhythm of life if removal of the formations is impractical. The main thing is to remember that the increase in the likelihood of degeneration into oncology directly depends on the size and composition of the body of the appendage.
Diagnostic methods
Pathological formations in the rectum can be identified using a digital rectal examination. The proctologist performs this procedure during the appointment. To detect bleeding in the intestines, a stool occult blood test ( Gregersen test ) is performed.
The main method for diagnosing tumors in the colon is colonoscopy . During this examination, the doctor inserts a colonoscope - a special instrument in the form of a thin flexible tube with a video camera and a light source at the end. With its help, the intestinal mucosa is examined throughout. During a colonoscopy, you can perform a biopsy - obtain a sample of the changed tissue and send it to the laboratory for examination under a microscope.
Colonoscopy is the main screening method that helps detect the presence of polyps and colon cancer at an early stage. All people are recommended to have a screening colonoscopy after age 50. If a person has risk factors, for example, a family history, hereditary syndromes, inflammatory bowel diseases, he needs to start getting tested at an earlier age.
At the European Clinic, colonoscopy is performed by highly qualified expert doctors; we use modern generation diagnostic equipment from leading manufacturers. Our research is carried out in conditions that are comfortable for the patient, in a state of “medicated sleep”.
A so-called virtual colonoscopy may be prescribed. X-rays, CT or MRI are performed using contrast agents. These diagnostic methods are less accurate and informative compared to endoscopic examination of the intestine.
How to identify polyps in the intestines
Diagnosis of intestinal polyps in most cases is carried out through colonoscopy. This method examines even the uppermost parts of the intestine, incl. remove them if necessary. Modern methods also allow the use of computed tomography or nuclear resonance imaging techniques to build a virtual model of the intestine without directly inserting a probe into the intestine. The following classical methods of detection during examination are used:
- palpation of the rectum;
- sigmoidoscopy;
- irrigoscopy using contrast injection (barium solution);
- biopsy, histological examination.
Prevention
Experts recommend that all people over 55 years of age, regardless of gender, undergo a colonoscopy. People over 60 years of age are often diagnosed with colon cancer.
If there were relatives in the family who were diagnosed with polyposis or intestinal cancer, then the immediate relatives should be examined before the age of 45.
In many countries around the world, colonoscopy is included in the mandatory medical examination procedure after 45 years of age. A stool test for blood is also required.
According to statistics, in recent years, colorectal cancer, which is preceded by polyps in the intestines, ranks second among all diagnosed cancers. Therefore, all people over forty years of age are recommended to undergo a colonoscopy to prevent bowel cancer.
Diet for polyps in the intestines
To reduce the risk of developing polyps and their growth during polyposis, you should follow a few simple nutritional rules:
- Consuming foods containing quercetin and curcumin. The first element is a bioflavanoid, which is found in yellow and red onions, the second is a phytochemical agent, which is maximally represented in turmeric. Taking them reduces the number and size of formations by half after just six months.
- Nutrition for rectal polyps should be as free as possible from the presence of fats of animal origin.
- Normal and sufficient intake of vitamin D. Fish, egg yolk, liver and foods specially fortified with it are rich in it.
- Balanced ratio of magnesium and calcium. The proportion should be 1:2, but the individual perception of these elements by the body should be taken into account.
Symptoms
Small single intestinal polyps do not give obvious symptoms and manifestations in both men and women. Because of this, the disease gradually progresses. Sometimes abnormal growths are found by chance during a colonoscopy (endoscopic examination of the intestines).
Large single formations 30 - 50 mm or more, as well as multiple growths that have spread throughout the mucous membrane of the gastrointestinal tract, begin to appear in the form of the following unpleasant symptoms:
- the appearance of blood on toilet paper or on the toilet after defecation;
- constipation and diarrhea, gas formation;
- painful sensations in the abdomen during emptying: difficult movement of feces causes partial blocking of the intestinal lumen by a large growth or numerous villous polyps;
- itching in the anal canal;
- if a colon polyp occurs, frequent attacks of nausea and sometimes vomiting may occur due to prolonged constipation and poisoning of the body with toxic substances;
- in young children - weight loss, frequent colic, nausea, inhibition of physical development, pallor against the background of iron deficiency anemia;
- bloody-mucous discharge and inclusions of blood in the stool in the form of red streaks or dark staining of the feces.
It should be borne in mind that the above-described signs are not specific - that is, characteristic specifically of polypous growths. Most gastrointestinal pathologies have very similar symptoms, for example:
- bleeding from the rectum occurs due to anal fissure, hemorrhoids;
- Dark coloring of stool is caused by products that contain iron.
Since the symptoms of intestinal polyps are very vague, an accurate diagnosis requires a medical examination by a gastroenterologist.
How to treat polyps in the intestines
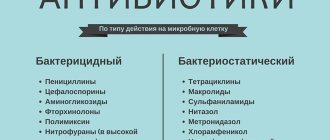
How to get rid of polyps in the intestines? If polyposis is detected, conservative therapy or traditional medicine will no longer help. Treatment of polyps in the intestines is carried out only by surgery. There are several options for surgery, the choice depends on the location of the formation. It is performed endoscopically, transanally and as a colotomy. Regardless of the type of polyposis, his body is sent for histology.
- Intestinal disease: symptoms and treatment
- Causes of mucus in the stool of an adult - diagnosis and treatment methods
- Walnut tincture: uses and recipes
Is it necessary to remove the polyp?
It is solely the doctor who decides whether polyps in the intestines need to be removed. Little depends on the patient's wishes. In 90% of cases, the choice is simple: the formation is removed or excised to avoid pathology, since only juvenile types of formations are predisposed to resorption. Depending on the patient’s condition, the doctor may postpone surgery indefinitely and monitor the dynamics of the disease or its stagnation.
How to remove a polyp in the intestine
Depending on the location and number of formations, one of the following methods is recommended:
- colotomy - removal of polyps in the intestine through an incision in the intestinal wall;
- use of proton pump inhibitors;
- gastroscopy;
- In case of severe malignancy of villous tumors, radical abdominal surgery is performed due to the large volume of the tumor.
Diagnostics
It is not possible to diagnose intestinal polyposis based on patient complaints alone, since this pathology has no characteristic signs.
The therapist can only assume the presence of neoplasms, but to confirm or refute the diagnosis, consultations with a proctologist and endoscopist, as well as a detailed examination, are necessary.
Digital examination of the rectum
The digital examination method is the first procedure prescribed to patients if polyposis is suspected. During the examination, the doctor carefully feels a small area of the rectum.
In this case, the pathology that was the cause of the symptoms can be identified.
X-ray methods
Diagnosis using x-ray methods is based on the use of a contrast agent. If it is necessary to examine the large intestine, a contrast solution is administered to the patient using an enema. After a few hours, an X-ray is taken, in which you can see the structure of the intestinal walls and neoplasms (if any).
If there is a suspicion of polyps in the small intestine, the patient should take the solution orally (drink). As in the previous case, after a few hours X-rays are taken, which are subject to study.
Endoscopic methods
An endoscope is a medical device in the form of a long thin tube. A microcamera and illumination are attached to the end of the tube. When inserted into the anus, the camera captures an image and transmits it to the monitor. Thanks to this, the doctor receives the most comprehensive information about the patient’s intestinal condition. Depending on the characteristics of the procedure, endoscopy is divided into 2 types:
- sigmoidoscopy;
- colonoscopy.
Sigmoidoscopy is a procedure through which a small intestinal section is examined (20-25 cm from the anus). During the procedure, the doctor may:
- get the most detailed picture of the condition of the mucous membrane;
- identify the presence of neoplasms and determine their shape and size;
- if necessary, perform tissue sampling for further histological examination.
Colonoscopy is often called the “gold standard” in diagnosis. This method is used if it is necessary to check the intestines over a long distance (up to 1.5 m). The endoscope allows you to:
- determine the condition of the intestinal sections;
- collect tissue for biopsy;
- remove growths.
Treatment of polyps in the intestines with folk remedies
It is impossible to completely recover from the causes of polyposis using folk remedies without traditional medicine, but herbal decoctions are perfect for normalizing digestion and relieving symptoms of the disease. Herbal medicine is good for prevention: it will prevent the development of cancer. The main thing is to coordinate the treatment of intestinal polyps with folk remedies with your doctor.
Here are some of the most popular recipes for treating symptoms:
- Pour boiling water over yarrow, celandine, St. John's wort and chaga in an amount of 1 teaspoon each and let it brew for 20 minutes. Take half a glass before meals.
- Pour boiling water over 3 tablespoons of viburnum berries and let cool. The drink can be drunk instead of tea and before meals.
- Mix honey and grated horseradish root in equal parts. Take 1 teaspoon on an empty stomach every day.
Find out more about how chaga is used for oncology.
Treatment of rectal polyps with celandine
Medicinal plants become a preventive measure for a whole range of diseases, and polyposis in this case is no exception. Treatment of intestinal polyps with celandine (especially in the rectum and large intestine) is best done using an enema. The simplest and most effective recipe is as follows: 2 parts of yarrow, 1 part of celandine and calendula flowers are poured with boiling water and allowed to cool, the broth is filtered, corn oil is added and shaken well. How to treat: administer into an empty intestine 2 times a day in 50 ml portions.
About the disease
Intestinal polyps are initially benign neoplasms consisting of epithelial glandular cells, attached to its walls with a stalk or a wide base and protruding into the intestinal lumen.
Photo of colon polyp
- Favorite places for intestinal polyps to be localized are different parts of the colon. The time of formation of such polyps most often is adolescence (in children and mature patients this occurs much less frequently). Most experts are of the opinion that polyps in the colon appear due to various inflammatory processes. Colon polyps are detected in 15% of adults over 40 years of age. In patients of childhood and adolescence, this figure is 25%. By the time of detection, 4% of patients have polyps in a precancerous state. 70% of benign tumors of the colon are localized in the tissues of the mucous membranes of the rectum, descending and sigmoid colons. The remaining 30% may be located in the splenic and hepatic angles, in the ascending colon and in the transverse segment of the colon.
- The most common culprits of intestinal polyposis are polyps localized in the rectum. In 8 cases out of 10, they are precursors to cancer of this organ.
- Cases of duodenal polyps are classified as rare pathologies. Almost all patients with this pathology were sent for surgery with the suspicion of having a cancerous tumor. Duodenal polyps, called acid-related, are located next to the duodenal bulb and are found in patients with gastritis with high acidity. Even rarer duodenal polyps, called bile-related polyps, are localized in the sphincter of Oddi region and are typical for patients suffering from cholecystitis and cholelithiasis. Polyps of the duodenum are found in patients of both sexes belonging to the age category of 35-60 years.
- Cases of polyp formation in the small intestine are rare. In half of the described episodes, patients also had polyps located in the colon and stomach. They are detected in patients of a wide age range. In women they are detected somewhat more often.
According to medical statistics, every tenth resident of Russia who has crossed the age of forty is the owner of polyps in the intestines, and it has been proven that men suffer from this disease 1.5 times more often than women.
In the International Classification of Diseases (abbreviated ICD-10), anal canal polyps are assigned code K62.0; rectal polyps are designated by code K62.1.
Diet after intestinal polypectomy
Nutrition after removal of an intestinal polyp should be balanced and meet the recommendations of the attending physician. In most cases, you will have to give up meat fats, alcohol and smoking. The diet must contain fresh vegetables, fruits, cereals, fiber, gluten, fish and seafood. Fermented milk products are included in the diet only after consultation with a nutritionist.
Find out more about what diet you need after intestinal surgery.
Treatment
Based on practice, doctors say that conservative treatment of intestinal polyps does not produce positive results.
Immediate elimination of even small growths of any kind with mandatory biopsy of their tissue is the main measure to prevent malignant processes in the intestine.
A mandatory indication for surgery is a complicated course of the disease: bleeding, polyposis affecting a large area of the mucous membrane of the affected organ, suppuration, fistulas and ulcers caused by pathological growths.
Indications and contraindications for surgery
Several years ago, operations to remove polyps in the intestines were carried out only when they reached large sizes or there were many of them. In the process of studying this problem, it was revealed that polyps of a benign nature very quickly degenerate into malignant neoplasms, so surgical manipulations began to be performed when small formations were detected. Doctors recommend their removal when individuals exhibit signs such as:
- deterioration of peristalsis and weakening of intestinal function;
- internal bleeding causing severe pain;
- difficulties with bowel movements;
- anemia;
- ulcerative lesions and wounds on the intestinal mucosa;
- the appearance of blood and mucus in the stool;
- risk of colon obstruction.
Preparation for the operation begins two days in advance. During this period, liquid and light foods should predominate in the diet. The patient cleanses the body of toxins, waste and feces, using sorbents and laxative medications recommended by the doctor. In some cases, it is possible to use an enema. Dinner is canceled the day before, and even liquid intake is prohibited on the day of surgery.
There are also contraindications to surgical intervention. They are mainly associated with the patient having concomitant pathologies of the cardiovascular system, severe infection, diabetes mellitus, oncology, epilepsy, and inflammation in the colon.
Postoperative period
After removal of the polyp in the intestine, a recovery period begins. During the first two years after surgery, individuals must undergo regular examinations (every four months), the purpose of which is to prevent growths from degenerating into malignant ones, as well as to avoid recurrence. Rehabilitation will be successful if you follow simple rules:
- Do not overcool or overheat.
- Avoid visiting the solarium.
- Reduce time spent in open sun.
- It is prohibited to independently cancel examinations prescribed by the doctor.
- Eliminate all addictions - smoking, alcohol, drug use.
- Avoid heavy lifting or strenuous physical activity, as there is a high risk of internal bleeding.
- Maintain inner calm.
- Avoid excessive fatigue, get plenty of rest.
- Stick to a healthy diet.
- Be sure to perform a set of exercises selected by a medical professional.
If the above recommendations are strictly followed, the risk of complications will be minimized.
Colonoscopy after removal of intestinal polyps is performed annually. If during the rehabilitation period an individual experiences an increase in temperature, swelling in the anus, nausea, vomiting, heaviness in the abdomen, pain, chills, and blood in the stool, then you should immediately visit a doctor. This clinical picture is characteristic of enterocolitis, wall perforation or degeneration of polyps into a malignant tumor.
Will traditional medicine help?
Many people are interested in whether traditional medicine will help with polyps in the intestines? It is worth immediately noting that polypous growths are serious neoplasms, often complicated by colorectal cancer. If the adenomatous polyp or adenopapillary formations are not removed in time, tissue magnetization may occur within several years. Therefore, folk remedies should be considered only as a complement to surgical methods for removing intestinal tumors. Even if the polyp does not show signs of malignancy now, they may appear in a few months or years.
There is still debate in the scientific world about the effectiveness of traditional medicine for polyposis. Many doctors believe that traditional methods can only be used for prophylactic purposes, and polyps should be removed immediately before they become malignant. Whether or not to use traditional methods of treatment is up to you.
One of the well-known ways to combat polyps is to use a special mixture based on pumpkin seeds, chicken yolks and vegetable oil. You need to take 12 dessert spoons of pumpkin seeds, grind them into flour, mix with 7 boiled chicken yolks and 2 cups of vegetable oil. The resulting composition must be thoroughly mixed and kept in a water bath for 15 minutes. After this, treatment can begin. The medication is taken in the morning, before meals, for a week. Single dose - 1 teaspoon.
Anal polyps are removed with a mixture of dry celandine powder and boric vaseline. Tampons with this composition are inserted into the anus several times a day. Polyps are also treated with a decoction of hop cones. The product is used for a week, and then take a short break. Bee products are useful for polyposis. Take natural honey, pollen, and royal jelly regularly. All these products have increased biological activity, the ability to activate the body’s internal reserve reserves and set it up for recovery.
Signs of an intestinal polyp
There are no characteristic signs unique to the polyp.
According to statistics, 10% of the population over the age of 40 are diagnosed with intestinal polyps: colon, rectum; men suffer from this pathology more often than women.
Most often, the pathology develops asymptomatically. Sometimes there may be blood, mucus in the stool, and a tendency to diarrhea or constipation.
Intestinal bleeding is a serious unfavorable sign indicating an oncological process in the intestines.
A large intestinal polyp can be complicated by intestinal obstruction, which is an indication for emergency surgery.
Some patients are concerned about itching in the anus, flatulence, belching, and drooling. Infection of the polyp contributes to the development of rectal fissures, and in severe cases to an abscess. These complaints already serve as a reason for undergoing examination; timely diagnosis of a polyp and timely surgical intervention are an effective measure for the prevention of intestinal cancer.
Intestinal polyps have a different texture, shape, color from reddish-gray to burgundy, with a coating on the surface.
In 30% of cases, polyps are multiple and are found in different parts of the intestine. Constant stool disorder can provoke the development of intestinal polyposis (multiple polyps), bleeding, and an oncological process.
When polyp growths are caused by rare hereditary syndromes, there are additional symptoms. Familial adenomatous polyposis is accompanied by gastric adenomas, with Gardner syndrome - epidermoid cysts, bone tumors (osteomas), with Turcot syndrome - glio and meduloblastomas of the brain, in combination with intestinal polyposis, with Peutz-Jeghers syndrome - spots on the lips and oral mucosa due to disorders of melanin synthesis.
Hereditary polyposis is the most unfavorable in terms of degeneration into intestinal cancer, so detected formations should be removed as quickly as possible.
Causes of this disease
There are several assumptions that explain the occurrence of polyps in this anatomical area. The most common theory is that polyps form against the background of chronic inflammatory changes in the intestinal mucosa. Doctors note that such changes often develop as a result of irregular and unbalanced nutrition, abuse of fast food, fatty, salty, fried, spicy and spicy foods and a lack of fresh fruits and vegetables.
Such a diet reduces intestinal peristaltic activity and increases the amount of harmful substances in the intestinal contents. As a result of peristalsis disorder, feces move more slowly through the intestinal sections, and harmful elements come into contact with the walls of this organ for a long time. This circumstance is aggravated by the fact that the density of feces increases, which, in turn, is due to the absorption of water from too slowly moving intestinal contents. Hardened fecal matter begins to injure the walls when moving. All this causes inflammation of the intestinal mucosa, which gradually becomes chronic.
Classification of polyps
Based on the multiplicity factor, the classification identifies the following groups of neoplasms:
- Single growth. The disease is characterized by the formation of one tumor, which in some cases reaches a large size.
- Multiple (group, scattered). It suggests the presence of a large number of lesions in the colon. Capable of growing in groups.
- Diffuse polyposis. The entire surface of the large intestine is susceptible to neoplasms.
Colon polyps are:
- Adenomatous;
- Hyperplastic;
- Hamartomamic;
- Inflammatory. Acute or chronic inflammatory process of the gastrointestinal tract causes tumor-like cell proliferation.
Adenomatous polyps
The term adenomatous polyp is applicable to neoplasms that in structure resemble a benign glandular tumor - an adenoma. Such formations developing on the surface of the large intestine are associated with a high risk of transformation into a malignant tumor. Adenomatous tumors are considered precancerous and development into colon cancer is likely. The growths reach a size of 1 cm and account for up to 10% of all formations. The epithelium of adenomas has signs of dysplasia of varying severity.
Adenoma or glandular polyp is usually divided into the following types:
- Tubular - common from the class of adenomotous formations, but their development into a malignant tumor is unlikely. They have a smooth and dense, pink surface.
- Villous - distinguished by the following features: they have a bright red color, the surface is covered with small villi. This type most often degenerates into a malignant tumor.
- Tubular-villous - consisting of elements of tubular and villous tumors.
Hyperplastic type
Most tumors of the hyperplastic type are located in the distal colon and rectum. For the most part, neoplasms are benign in nature and are not prone to transforming into cancer, which does not exclude this possibility altogether. This form of the disease is the most common. The disease occurs with virtually no symptoms. It is possible to discover a polyp by chance during the diagnosis of other diseases.
Hamartoma polyps
They are growths consisting of several types of tissues, the cells of which have lost their normal properties. The disease involves benign tumors that cover the wall of the colon.
Juvenile growths are classified as hamartomatous. Often found in patients under 20 years of age. Usually single, causing bleeding. If there are more than 5 formations in the colon, we can talk about a syndrome called multiple polyposis.
Classification
Important: people over 50 years old account for almost 80% of diagnosed colon polyps.
Both single and multiple neoplasms protruding into the intestinal lumen are diagnosed. Diffuse polyposis requires special vigilance. The appearance of polyps can be different: spherical, mushroom-shaped or branched. Some processes have a stalk, while others (the so-called sessile ones) have a wide base.
Most often, polyps are colored grayish-red, less often yellowish or purplish-red.
According to their origin, colon polyps are divided into:
- hyperplastic;
- inflammatory;
- neoplastic.
Hyperplastic growths are formed due to hypertrophy of normal tissue (glandular epithelium). Inflammatory polyps form in areas of the colon mucosa where the inflammatory process takes place. Neoplastic neoplasms pose the greatest danger. They can be either benign or malignant, as they appear when atypical cells grow.
Important: according to leading coloproctologists, colon cancer most often (in 50-75% of diagnosed cases) is a consequence of malignancy of polyps.
Based on their histological structure, it is customary to distinguish the following types of colon polyps:
Most often, dense and smooth adenomatous neoplasms of a round shape are detected.
The growth of villous polyps on the intestinal wall looks somewhat similar to a carpet. This type of growth undergoes malignancy in 40% of cases.
Preventive measures
Prevention of polyps in the large intestine is the reduction or elimination of factors that contribute to their appearance. To achieve these goals, a set of measures is being taken:
- Fighting constipation - this factor often accompanies the appearance of polyps. Normalization of stool is considered one of the important preventive measures. To prevent them, you should reduce your consumption of sweets, flour products, and sandwiches. Do not eat dry food and follow a daily routine. In addition, increasing physical activity, eating foods high in potassium, and avoiding frequent use of laxatives and enemas will help avoid constipation.
- Treatment of chronic pathologies - growths never form in a healthy intestine. Gastrointestinal diseases contribute to their appearance - proctitis, enteritis, hemorrhoids, colitis, Crohn's disease, colon dyskinesia. It is necessary to identify and treat them in a timely manner so that they do not become chronic.
- Changing your diet - you should increase the amount of fiber you eat and reduce the calorie content of your meals. A lack of dietary fiber inhibits the functioning of the intestines, slows down the process of removing processed bile from the body, which contributes to the formation of polyps, as well as their degeneration into malignant neoplasms. In addition, fiber acts as a sorbent and removes toxins and breakdown products from the body.
- Regular visits to the doctor and medical examinations - you now know what polyps in the intestines are and what danger they pose. Therefore, after the age of forty, doctors recommend an annual test for occult blood in the stool. After fifty years, perform an instrumental examination of the colon regularly once every three or five years.
- Prevention of mineral and vitamin deficiencies - a lack of vitamins such as A, C, E, D, B6, B2, as well as selenium, folic acid and calcium provokes the growth of the rectal mucosa. Therefore, when compiling a diet, it is necessary to provide for the presence of all necessary substances. If necessary, use vitamin and mineral complexes.
Removal methods
- Small polyps of the gastrointestinal tract, which are located close to the anus, are excised transanally using special endomicrosurgical instruments.
At a deeper location, an endoscopic method (endoscopic polypectomy) is used to remove the intestinal polyp, a technique similar to colonoscopy. A rectoscope or colonoscope equipped with a loop electrode is inserted through the anal canal. A loop is placed around the stalk or thick base of the polyp and the abnormal growth is cut off. Small shoots are removed by cauterizing with a diathermocoagulator, large tumors are excised in separate parts. Endoscopic removal takes 10 to 30 minutes, which is determined by the location of the polyp, its size and the number of outgrowths. The operation is performed with anesthesia, is easily tolerated by patients (since it is low-traumatic), virtually eliminates bleeding (the dissected vessels are cauterized with a coagulator), and does not require long-term recovery. After endoscopy and in the absence of complications, the patient usually leaves the clinic the next day.
- In case of diffuse damage, surgery to remove intestinal polyps is performed in an open manner (cavitary) with general intravenous anesthesia, since this type of pathology requires excision of the area of the intestine affected by tissue formations (colotomy).