Hyperplasia of the thyroid gland is a benign formation that is a consequence of the proliferation of gland tissue. At the initial stage of development, this pathology does not cause significant harm to health. However, if treatment is not started in a timely manner, the tumor can degenerate into malignant, which entails a direct disruption of the thyroid gland. Statistics show that today the disease is diagnosed in 740 million of the planet's population.
Online consultation on the disease “Thyroid hyperplasia”. Ask a question to the specialists for free: Endocrinologist.
- Etiology
- Pathogenesis
- Symptoms
- Kinds
- Stages
- Diagnostics
- Treatment
- Forecast
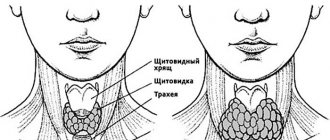
What is hyperplasia
This is an excessive proliferation of cells that can begin in any internal organ in people of any gender and age. The trigger mechanism for this pathology is inflammatory processes, hormonal imbalances, polyps, cysts, tumors. The thyroid gland is considered enlarged when its volume is more than 20 cm³ in women and 23 cm³ in men.
Hyperplasia of this endocrine organ is most often a compensatory response of the body to a deficiency of thyroid-stimulating hormones. The hypothalamus section of the brain forces the gland to function in an enhanced mode, and the cells producing these secretions are forced to increase in number.
There are 2 types of organ hyperplasia:
- diffuse;
- nodal.
The diffuse type of pathology is characterized by uniform tissue growth in the absence of compactions. Such neoplasms may be accompanied by other thyroid diseases:
- autoimmune thyroiditis;
- diffuse toxic goiter;
- hormonal tumors of various organs, etc.
The thyroid gland enlarges unevenly. The nodular type of pathology is manifested by multiple compactions that resemble nodules.
Read more about diffuse changes in the thyroid gland here.
But often the enlargement of the thyroid gland occurs unevenly. The nodular type of pathology is manifested by multiple compactions that resemble nodules. In the international classification, variants of thyroid hyperplasia are classified as diseases of class IV “Diseases of the endocrine system, nutritional disorders and metabolic disorders.” Their ICD-10 codes are E.01, E04, E05, E06, E07.
How does pathology manifest itself?
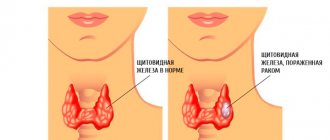
The symptoms of hyperplasia can vary significantly depending on the stage and type of disease. The initial stage is usually asymptomatic. In later stages, it is already possible to visually detect the growth of the thyroid gland.
Also, the growth of the thyroid gland is accompanied by symptoms that indicate improper functioning of the thyroid gland and the development of diseases that led to this. These include increased sweating, constant headaches, increased heart rate, pain in the heart area, difficulty breathing and swallowing. There may be redness of the face, along with a feeling of heat, and a change in voice, especially in people who talk a lot.
Causes
Among the most common reasons:
- long-term iodine deficiency;
- weakening of the immune system;
- long-term use of medications or consumption of foods containing substances that suppress the thyroid gland;
- hypothyroidism;
- thyrotoxicosis;
- birth defects that disrupt hormonal balance;
- tumors.
In approximately 90% of cases, diffuse hyperplasia of the gland becomes a consequence of iodine deficiency. In pregnant women, it can develop against the background of a sharp weakening of the immune system or hypovitaminosis. Some drugs have a negative effect on the organ, for example antibiotics, potassium bromate, amidarone, sweeteners, etc.
In pregnant women, diffuse hyperplasia of the gland can develop against the background of a sharp weakening of the immune system or hypovitaminosis.
Gluten protein, found in many types of baked goods, has a similar effect. Goitrogens, goitrogenic substances that interfere with the absorption of iodine from foods and contribute to the development of gland hyperplasia, also have a negative impact.
Not only cancerous, but also benign tumors can cause organ enlargement. The appearance of goiter in Graves' disease is a consequence of hypertrophied hormone production with clinical manifestations of thyrotoxicosis. Almost always, gland hyperplasia accompanies the early stage of chronic lymphocytic thyroiditis (Hashimoto's disease).
Reasons for development
The pathology, called hyperplasia, is caused by a violation of hormone secretion, which leads to increased stimulation of the thyroid gland. As a result, cells can increase 15-20 times. Considering this type of disease in detail, medicine identifies several of the most obvious causes of its occurrence:
- Infections;
- Presence of “Hashimoto’s goiter”;
- Hormonal drugs that have a depressing effect on the thyroid gland;
- Iodine deficiency (main cause);
- Weak immune system;
- Congenital disorders of the hormonal system;
- Pregnancy;
- Swelling in the area of the pituitary gland or hypothalamus;
Modern medicine has been fighting this disease for many years, identifying new causes and methods of prevention. So, for a long time, scientists considered iodized salt to be the best solution to the problem of diffuse hyperplasia. However, the incidence of pathology has not decreased.
But sometimes doctors still manage to find out the true cause of goiter. As a rule, these are idiopathic diseases. There is an opinion that this is influenced by inflammatory processes in the body.
Symptoms
If the enlargement of the gland is not caused by its functional disorders, the person does not experience any painful symptoms. Only occasionally there may be a feeling of slight discomfort and slight swelling in the neck area. With severe hyperplasia, overgrown tissue begins to compress areas of the larynx or esophagus and shortness of breath or a feeling of a lump in the throat occurs when swallowing. If the enlarged gland compresses the laryngeal nerve, the voice becomes hoarse.
In addition, the following signs of thyroid hyperplasia are often observed:
- painful shine in the eyes, constantly dilated pupils;
- tremor (shaking) of hands;
- rapid pulse;
- sudden changes in mood, sudden depression;
- changes in body weight: either losing weight or gaining excess kilograms with the same diet;
- sleep disturbance;
- rapid development of hypertension.
In children with thyroid hyperplasia, cognitive abilities, memory, and concentration deteriorate. They begin to lag behind in physical development. Constipation, brittle hair, and pale skin may occur. Puberty occurs later. The behavior of such children becomes aggressive.
Hyperplasia of the last stage is manifested by pronounced symptoms:
- the patient has difficulty swallowing food;
- he is overcome by coughing attacks, his breathing becomes shallow;
- in men the timbre of their voice changes;
- the patient's face turns purple.
What to do if you have an enlarged thyroid gland? More details>>
Thyroid in childhood
The following degrees of diffuse nodular hyperplasia can be designated:
- Grade 0 - there are no external signs of an enlarged gland, complaints from patients are rare, but pathological changes are already occurring in the organ, which can be detected using ultrasound diagnostics and laboratory testing.
- 1st degree - enlargement of the gland is diagnosed by a specialist during palpation; hyperplasia can be seen externally only when a person swallows food or water.
- 2nd degree - the gland begins to acquire unattractive contours, visually worsening the shape of the neck - it thickens, characteristic protrusions appear, and the overgrown organ itself begins to put pressure on the esophagus and trachea, interfering with the patient’s well-being.
Signs of thyroid hyperplasia most depend on whether it produces more or less hormones. The type and degree of hyperplasia has less influence on the manifestation of symptoms.
Types of hyperplasia
Depending on the processes in the organ, on what causes the increase in the volume of thyroid tissue, diffuse formuzoba and nodular one are distinguished.
A combination of pathologies is possible; in addition, hyperplasia of the isthmus of the thyroid gland is classified as a separate type. The most common type is diffuse hyperplasia of this organ.
What does diffuse hyperplasia of the thyroid gland mean?
This means that the enlargement of the organ occurs due to the uniform growth of the follicles that make up the gland.
In most cases, this option can be treated quite successfully and does not pose any danger.
This form, unlike the previous one, in which compactions form in the tissues of the gland - overgrown foci, which are called nodes.
Their sizes and quantities may vary. Nodular hyperplasia of the thyroid gland can be dangerous, as it threatens the development of cancer.
It is especially worth paying attention to single nodes larger than 1 cm or multiple formations.
With the diffuse nodular form of hyperplasia of the thyroid gland, a uniform increase in the organ occurs with the formation of one or several nodes.
The nodular form usually proceeds more aggressively, since the seals are often very active and produce excessive amounts of thyroid hormones.
- 0 degree – the organ cannot be palpated, nothing is noticeable externally;
- 1st degree - the isthmus is noticeable when swallowing and palpable;
- hyperplasia of the gland 2nd degree - when swallowing, the organ becomes noticeable and can be clearly felt;
- 3rd degree of hyperplasia – the shape of the neck begins to change;
- 4th degree – changes in the shape of the neck are pronounced;
- With grade 5 hyperplasia, the goiter becomes very large, compresses the trachea, larynx, and makes swallowing and breathing difficult.
The most common type of hyperplasia of the thyroid gland is grades 1 and 2, because the capabilities of modern diagnostics and treatment make it possible to identify the problem in the early stages.
Moderate hyperplasia of the thyroid gland in the absence of discomfort in the patient may not require treatment.
Hyperplasia of the thyroid gland often occurs in children, especially often in adolescence, when the body is rapidly developing and requires a large amount of hormones.
For the prevention and timely detection of thyroid diseases, a medical examination is carried out with an examination by an endocrinologist.
If thyroid hyperplasia is detected in a child, it is necessary to further examine him and prescribe treatment.
Depending on the processes in the organ, on what causes the volume of thyroid tissue to increase, a distinction is made between a diffuse form of goiter and a nodular one.
With an enlarged thyroid gland, the set of symptoms can be quite large, but an asymptomatic course is also possible.
Nodular hyperplasia of the thyroid gland produces more noticeable symptoms than diffuse hyperplasia, because the nodes most often produce large amounts of hormones.
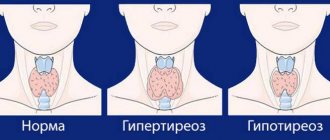
Symptoms and manifestations depend on whether the function of the organ is impaired and what the nature of this impairment is. Hyperplasia may be accompanied by the following hormonal conditions:
- euthyroidism – normal thyroid function, no symptoms,
- hypothyroidism - reduced thyroid function, symptoms are associated with a slowdown in metabolism in the body,
- hyperthyroidism – the function is increased, there are symptoms of thyrotoxicosis and increased metabolism.
With hyperplasia of the thyroid gland already in the 1st degree, all symptoms can manifest themselves fully if there is a noticeable disruption of the organ.
- Apathy, tearfulness.
- Increase in body weight.
- Chilliness.
- Dry skin, brittle hair and nails.
- Swelling all over the body.
- Bradycardia.
During the treatment of diffuse nodular hyperplasia of the thyroid gland, it is most often necessary to reduce the amount of hormones. For this purpose, special medications are prescribed.
The presence of large (more than 1 cm) nodes is a reason for a biopsy, with the help of which the nature of the node is determined (benign or malignant).
Malignant nodes definitely need to be removed. If oncology is not detected, then the decision on treatment is made based on the results of a hormonal blood test.
For hypothyroidism or a slight degree of hyperthyroidism, conservative treatment is possible.
Very high levels of thyroid hormones or multiple nodes are subject to surgical treatment. During the operation, the damaged lobe of the thyroid gland or the entire organ is removed.
An alternative to surgical treatment can be radioactive iodine therapy, which leads to the destruction of gland cells.
After this treatment, the patient will require lifelong hormone replacement therapy because he will no longer produce his own thyroid hormones and will develop a state of hypothyroidism.
Thanks to this treatment, normal hormonal levels can be maintained.
- Cough
- Facial redness
- Nervousness
- Thyroid enlargement
- Excitement
- Changing your voice tone
- Shallow breathing
- Difficulty swallowing
- Pupil enlargement
- Weight fluctuations
- Neck swelling
- Sparkle in the eyes
Hyperplasia of the thyroid gland is a benign formation that is a consequence of the proliferation of gland tissue. At the initial stage of development, this pathology does not cause significant harm to health. However, if treatment is not started in a timely manner, the tumor can degenerate into malignant, which entails a direct disruption of the thyroid gland. Statistics show that today the disease is diagnosed in 740 million of the planet's population.
Diagnostics
It is difficult to recognize the disease in the early stages, since organ hyperplasia manifests itself with clear symptoms only in the last stages of development. By examining, palpating and testing the gland, the endocrinologist preliminarily determines the stage of the disease. Even a slight increase in the isthmus of the gland is best seen, since its contours quickly appear on the neck.
Read more about the technique of palpation of the thyroid gland here.
Suspecting a pathology, the doctor prescribes blood tests for thyroid hormones:
- TSH (thyroid stimulating hormone);
- total and free T3 (triiodothyronine);
- total and free T4 (thyroxine).
Instrumental research methods:
- Ultrasound of the thyroid gland;
- radiography of the organ;
- histological analysis.
Ultrasound is the most accessible and reliable method for diagnosing thyroid hyperplasia.
Ultrasound is the most accessible and reliable method for diagnosing hyperplasia of this organ. His condition is effectively assessed by echo signs. Pathological cells respond to ultrasound signals differently than healthy cells. Thanks to this, ultrasound allows you to obtain data not only on the size, shape, and volume of the gland, but also on the location and structure of its neoplasms.
In women, hyperplasia of the right lobe of the organ can spread to the right mammary gland, since they are interconnected.
Additionally, a mammogram should be done. Overgrown tissue in parts of the left lobe of the thyroid gland is located close to large vessels. Since left-sided gland cancer can develop metastases to the heart, it is also necessary to examine its condition.
Stages of development
There are five stages of development of the disease:
- 0 – changes take place only at the cellular level, there are no external manifestations;
- 1 – when swallowing, the isthmus area begins to stand out on the neck, there are no other symptoms;
- 2 – the organ increases in size;
- 3 - the enlargement of the organ becomes more and more noticeable, the person has difficulty swallowing, and a cough begins;
- 4 - the neck area is significantly deformed, the symptoms are pronounced;
- 5 – compression of the trachea and esophagus, advanced stage of the disease.
Stage 1 hyperplasia of the thyroid gland is most treatable, as it is an early stage of development. But it is worth noting that diagnosing the disease at this stage is quite difficult.
Treatment of thyroid hyperplasia
The moderate diffuse form of this pathology is most common. If the gland does not continue to enlarge, medications for the thyroid gland (Iodomarin, Iodine-active, Potassium Iodide), consumption of iodized salt, seafood and periodic medical supervision are prescribed. In difficult cases, hormonal treatment is necessary. If the hyperplasia is nodular, the risk of developing gland cancer is significantly higher. For this form of the disease, in addition to iodine preparations, hormonal medications are always prescribed (L-thyroxine, Propicil, Tyrosol, etc.).
If the gland does not continue to enlarge, the drug Iodomarin is prescribed.
Alternative medicine
Drug treatment, in consultation with a doctor, can be supplemented with folk remedies. Popular recipes:
- take 1 tbsp. l. flaxseed oil in the morning on an empty stomach;
- 1 d.l. Boil chopped white cinquefoil herb in 0.4 liters of water for 5 minutes, leave for half an hour. Drink 1 glass in the morning and evening;
- mix 1 part dead bees with 2 parts vodka, leave for 20 days, strain. Take 1 tbsp tincture for hyperplasia. l. three times a day before meals for 2 months.
Herbal infusions
Multicomponent mixtures are more effective:
- Collection No. 1: mix 100 g of dry herbs gorse, cocklebur, walnut leaves and 200 g of Icelandic lichen. 2 tbsp. l. collection, pour 1 liter of boiling water in a thermos, leave for 30 minutes. Drink a little throughout the day.
- Collection No. 2: take 50 g of norichnik herb, 100 g each of mint leaves, St. John's wort and linden blossom, 200 g each of agrimony herb, blackhead and black cumin seeds. 1.5 tbsp. l. pour the mixture with 2 glasses of water, cook for 15 minutes, leave for half an hour. Drink half a glass four times a day until hyperplasia is cured.
Multicomponent mixtures of medicinal herbs are more effective for thyroid hyperplasia. For example, the collection may include cocklebur, gorse grass, walnut leaves and Icelandic lichen.
Exercises
Oriental medicine practices are popular. Their goal is not the treatment of a particular disease, but the restoration of energetic harmony in the body. Therefore, for any pathology of the thyroid gland, including hyperplasia, one, but “golden” exercise “Frog” is used:
- stand straight, legs together, arms along the body;
- squat down slightly, stretch your neck and arms forward;
- imitate swimming, making circles with your hands 6-8 times;
- return to the starting position;
- imitate a swim, only circles - not away from you, but towards you, also 6-8 times;
- return to the starting position;
- imitate swimming towards yourself 6-8 times.
Other methods
If gland hyperplasia does not respond to conservative treatment, surgical intervention is resorted to. Most often, nodes or the entire pathological area are removed. After this, hormone replacement therapy is carried out under the close supervision of a doctor.
If surgery is contraindicated, a technique is used to destroy the affected tissue with radioactive iodine. After 2-3 months, a therapeutic effect occurs, similar to the result of a surgical operation.
If gland hyperplasia does not respond to conservative treatment, surgical intervention is resorted to.
Prevention
The main measures to prevent pathology include the constant use of iodized salt. In addition, replenishing the diet with seafood and iodine-containing products also plays an important role. The iodine supply in the body can be replenished by eggs (it is also advisable to give preference to iodized ones), milk, beef, etc.
Excess weight plays an important role in the development of many thyroid pathologies. In addition to the fact that it provokes the body to produce excess hormones, excess weight is the same risk factor for cancer as smoking and living in areas of environmental disaster.
Diet
Nutrition for hyperplasia of the thyroid gland should be fractional: you need to eat little, but often. The following should be excluded from the diet:
- fatty foods, dishes, sauces;
- spicy seasonings;
- canned food, smoked meats, sausages;
- products with goitrogens: all types of cabbage, radishes, soybeans, peanuts, corn;
- alcoholic drinks;
- food with synthetic additives, which are designated by codes E;
- sweet sodas, coffee.
For thyroid hyperplasia, foods rich in iodine are useful:
- sea fish, seafood;
- buckwheat, oatmeal, rice, pearl barley;
- lean poultry;
- low-fat fermented milk products;
- linseed oil;
- walnuts;
- spinach;
- feijoa.
For thyroid hyperplasia, foods rich in iodine are useful. This could be sea fish, seafood, spinach.
Treatment
If there is no suspicion of the formation of a malignant process, and the tissue does not compress the trachea, which is dangerous to human life, surgical intervention is not required.
The basis of treatment is taking hormonal medications and vitamins
Treatment is based on taking hormonal medications and vitamins to strengthen the immune system. Drugs are also prescribed to restore the required amount of iodine in the body.
It is worth noting that drug treatment alone will not bring the desired result if you do not follow a proper diet. Therefore, while taking hormonal medications, you should follow the following diet:
- Avoid eating fatty and spicy foods;
- complete absence of alcohol;
- You can’t eat food with dyes;
- limit sweets.
Instead, you should include foods high in iodine in your daily diet:
- fruits and vegetables;
- spinach;
- fish.
Treatment along with proper nutrition will undoubtedly give positive results.
Traditional methods
Many often turn to traditional medicine and, thus, consciously avoid traditional medicine, without realizing the full severity of their disease. It is worth emphasizing that in relation to this disease, the effectiveness of traditional methods does not receive scientific approval. Treatment of this pathology with some folk methods can even be dangerous.
For example, in no case is it recommended to self-prescribe large dosages of iodine, regardless of whether the medicine is of organic or inorganic origin. Since with this type of hyperplasia, focal formations have already formed in the tissues, against the background of which unjustified consumption of iodine can lead to thyrotoxicosis.
Surgical intervention
Surgical treatment is also required for patients suffering from compression of such important organs as the esophagus and trachea by the gland. Surgery is also required for those patients in whom atypical cells were found in the altered gland tissue during histological examination.
The second degree of the disease is characterized by a significant increase in nodal changes that can grow from three centimeters or more. In these cases, surgery to remove the nodes will not be the only step towards recovery, since they can grow again. In this regard, the further fight against relapse of the disease will consist in eliminating the pathogenic factors that provoke thyroid disease.
Often surgery is the only option to save the patient's life. This is explained by the fact that the advanced course of the disease can lead to the fact that a growing tumor in the gland can degenerate into a malignant manifestation.
Degrees of hyperplasia: 0 degree
The pathological process developing in the endocrine system and the body as a whole is just beginning to gain momentum. Neither during palpation nor externally does the thyroid gland reveal itself.
Laboratory studies may show persistent hormonal imbalance, which may cause the following symptoms:
- weight fluctuations up or down,
- sleep disorders,
- irritability,
- increased fatigue.
As a rule, grade 0 hyperplasia is diagnosed completely by accident if the patient consults a doctor with concomitant complaints regarding other organs, or during a routine examination.
Forecast
Hyperplasia is initially a benign process. The disease in its initial stages can be treated quickly and effectively and rarely leads to complications.
If hyperplasia is not detected promptly and its treatment is not started, the nature of the tumor can become malignant. This phenomenon occurs in 5% of cases. This means the risk of metastasis, that is, germination into other organs. The heart, mammary glands and other nearby organs are at risk.
Signs of the disease in the nodular form of goiter disappear in every third patient with replacement therapy. Surgical intervention during which the nodes are removed is effective.
Progressive hyperplasia leads to a deficiency of the hormone thyroxine. This is fraught with cardiac dysfunction and can even result in cardiac arrest.
Successful treatment does not mean that the disease will not return. Even if therapy is effective, relapses are possible, so preventive measures in the form of diet and sufficient iodine intake (foods, medications) should become an integral part of life.
If hyperplasia is detected in a timely manner, the prognosis is positive, but subject to treatment and nutritional adjustments. If the pathology was detected at stage 4 or 5, treatment will be complex and lengthy. At an advanced stage of hyperplasia, the possibility of death cannot be excluded.
Conservative therapy
At an early stage of the disease, with zero degree of hyperplasia, patients are prescribed conservative therapy aimed at normalizing the functioning of the thyroid gland. As part of its implementation, it is important to systematically adjust the prescribed dosages of drugs, based on changes in the general condition of the endocrine organ, and its activity should also be taken into account.
If drug treatment for diffuse nodular hyperplasia of the thyroid gland does not give the desired result, and the patient feels much worse, and the pathology continues to worsen, then there is a need for surgical intervention.
What are follicles in the thyroid gland - look through a microscope
The structure of the glandular tissue of the thyroid gland is represented by follicles. These are microscopic vesicles filled with a colloidal mass - thyroglobulin, in which hormones accumulate.
The follicles in the unchanged gland are evenly distributed.
The shell is a 1-layer epithelium of cells of type A, B. Single cells of type C are located in the contents of the follicles.
The biosynthesis of iodides into hormones containing iodine atoms occurs in A cells (thyrocytes). Their shape changes, from flat to cubic and then cylindrical, which is caused by the high activity of the gland.
The surface of thyrocytes of three types. The apical part (with villi) faces the inside of the follicle, the lateral parts merge with each other into a dense continuous layer.
The basal surface of the cells separates the follicles from the parenchyma, penetrated by capillaries, and is connected with them.
B cells (another name is Ashkenazi-Hurthle cells) begin to appear at the age of 14, reaching their maximum number by the age of 50-60.
They are larger than thyrocytes with a rounded nucleus in the center; they contain serotonin, a biogenic neurotransmitter. The pathological role of type B cells is being studied.
It has been proven that they form Hurthle cell thyroid cancer.
Type C cells are larger than thyrocytes, their cytoplasm is lighter, they are located singly in follicles, and do not have an apical surface.
They do not absorb iodides and produce the hormone calcitonin, which is necessary for calcium-phosphorus metabolism.
A pathological feature of C-cells is that aggressive medullary gland cancer develops from them.
Parafollicular islands are located between the follicles. They are made up of all types of cells.
If organ regeneration is necessary, the islets develop into full-fledged follicles.
With age, a gradual natural decrease in the volume of the gland occurs: the number of follicles decreases, interfollicular islands disappear, and the function of the organ decreases.
Blood supplying iodides to the gland enters through the lower and upper arteries; the outflow of blood containing thyroid hormones occurs through the veins of the gland, connected to the internal jugular and facial veins.
Lymph with hormones enters the cervical lymph nodes through lymphatic vessels.