Pancreatitis is a serious pathology in which the pancreas becomes inflamed. The immediate cause of inflammation is the premature activation of enzymes that begin to digest organ tissue.
Active enzymes damage not only the cells of the pancreas parenchyma, but also corrode the vascular walls. Having penetrated the blood in this way, they spread throughout the body and affect vital organs - the heart, kidneys, stomach and brain.
Pancreatitis can occur in acute and chronic forms. In case of a sudden attack or exacerbation of chronic pancreatitis, treatment is carried out in a hospital. The main objectives are relief of acute symptoms, restoration of the digestive process and compensation of exocrine insufficiency. To normalize pancreatic function, medications of several groups are used.
Symptoms of pancreatic inflammation
The main symptom of pancreatitis in an adult is pain. It encircles the entire body, including the stomach and back. Nausea, weakness, drowsiness are combined with painful vomiting, which does not bring relief.
50% of patients experience weight loss. 15% have diarrhea. During palpation, signs of paresis and intestinal bloating are detected. As the pathology progresses, symptoms of irritation of the abdominal cavity, as well as nearby organs, appear.
The skin turns pale and signs of cyanosis are observed. This is typical for the acute form of the disease. Blueness appears in the navel area, and the patient's face turns red.
Enzymatic preparations
The choice of enzymatic preparations should take into account the characteristics of the course of the disease. The main components of this group of medications are protease and lipase. The active components are extracted from the pancreas of pigs, since this animal is closest to humans in terms of biological characteristics.
In chronic pancreatitis, the necessary enzymes are destroyed by hydrochloric acid, which is part of the gastric juice, so all enzyme preparations are placed in a special capsule with an acid-resistant shell. All manufactured medications are divided into two categories: with one shell and two.
Drugs of the second group are more effective due to the special release of active components. The active ingredients are placed in special microspheres, which in turn are located in a capsule. The drug gradually dissolves in the intestines and, due to microspheres, is evenly distributed over the walls of the organ. This group includes Pancitrate, Creon.
Pancreatin and Mezim are produced with one shell. They are often prescribed for acute pancreatitis. The drugs can reduce the activity of the digestive organ and reduce inflammation of its tissues.
Some types of enzyme preparations are contraindicated for the disease in question, for example, Festal, Digestal. Medicines contain elements of bile, which accelerate the secretion of the pancreas and thereby intensify attacks of pain.
Enzyme preparations are the main basis for the treatment of pancreatitis, because thanks to their action:
- the load on the pancreas is reduced;
- the process of breakdown of fats, proteins and carbohydrates in the body improves;
- attacks of nausea and heartburn are eliminated;
- stool is normalized;
- the risk of pain and discomfort in the abdomen is reduced;
- the process of absorption of nutrients by the body improves.
As a rule, enzyme preparations are taken for a very long time. Their dosage is determined strictly on an individual basis, depending on the general condition of the patient and the course of the disease.
In order for these remedies to really give a good result, their use must be combined with a diet, and always either while eating or after eating. It is not recommended to take them before meals, as they can cause serious harm to the stomach. All enzyme preparations contain bovine pancreas extract – pancreatin.
Pancreatin is the cheapest enzyme preparation, but despite its low cost, it is highly effective
Pancreatin contains the following components:
- lipase, which ensures the digestion of fats;
- amylase, which promotes the breakdown and absorption of carbohydrates;
- protease that improves protein digestion.
It is thanks to these components that pancreatin is able to compensate for pancreatic dysfunction and normalize digestion processes in the body. Among the drugs that contain this substance, the most popular are:
- Creon;
- Pancreatin,
- Festal,
- Digestal,
- Pankurmen,
- Mezim.
It should be noted that these drugs also contain other substances that have their own effects. Therefore, only a doctor should prescribe them, taking into account the patient’s concomitant gastrointestinal disorders.
As for antienzyme agents, they are used in acute cases of the disease to reduce the production of digestive enzymes. You cannot drink them during chronic pancreatitis in remission, as they can only aggravate the course of the disease.
Among the antienzyme drugs, the most effective are:
- Kontrikal,
- Trasylol,
- Pantripin,
- Antagozan.
Contrical is an antienzyme drug for intramuscular administration.
Treatment of pancreatitis is impossible without enzymes. Such drugs are prescribed not only for the treatment of chronic pancreatitis. They are the main way to combat cholecystitis. The action is to reduce the secretion of the pancreas, the person feels less pain.
Many people note the positive aspects of the drug. Patients say that only Wobenzym is able to keep the pancreas normal. Due to the positive effect of the drug, patients do not want to replace it with other drugs for the treatment of pancreatitis. Remember, take the medication for chronic forms of the disease for a course of three to six months. The drug is prohibited for children under 5 years of age.
Wobenzym is easily tolerated by patients. Long-term use of the drug did not cause side effects or addiction. Wobenzym consists of enzymes similar to human ones. The decision to prescribe the drug is solely within the competence of the attending physician. The dose does not exceed tablets three times a day. Wobenzym must be taken while following a diet. The drug is taken for a month.
https://www.youtube.com/watch?v=75tumoQL9l4
A time-tested drug used in conjunction with others is Festal. The medicine breaks down fats, carbohydrates and proteins thanks to lipolytic, amylolytic and proteolytic actions. The drug is used for a long time.
We suggest you read: How is beer measured?
Remember that only a doctor can advise which enzymes are best to choose in each case.
Treatment of pancreatitis in adults
If you find one or more signs of inflammation of the pancreas, you should immediately consult a physician. He will send you for tests. After this, the patient should visit the gastroenterologist's office. The doctor prescribes the necessary medications to the patient. Then you need to contact a nutritionist. The specialist will determine the diet. The patient is also prescribed a diet.
How is pancreatitis treated in adults? Therapy involves:
- Pain relief.
- Elimination of inflammation in the affected organ.
- Elimination of symptoms of glandular deficiency.
- Relief of inflammation in nearby organs.
- Preventing complications.
To treat this disease, anti-enzyme medications, analgesics, antispasmodics, H2 blockers, and antacids are prescribed. The best effect is achieved during the first time of using medications. Medicines containing the polypeptide aprotinin have the most powerful effects. At the same time, procedures are carried out to cleanse the body of pancreatic enzymes.
Drugs for the treatment of chronic pathologies of the pancreas
Chronic pancreatitis is no less dangerous than acute pancreatitis, as it can lead to functional failure. And it is for this reason that doctors prescribe enzyme preparations that support the functioning of the pancreas. Among these medications, the most popular are:
- Mezim,
- Creon 1000,
- Almagel A,
- Maalox.
Maalox is one of the most effective drugs for normalizing pancreatic functions
Treatment with such drugs should be carried out over a long period of time (at least 6 months). They contain enzymes that help improve digestive functions. They begin to act immediately after they penetrate the stomach. And to avoid exacerbation of the disease, it is recommended to take them during or after meals.
As an additional therapy to restore digestive functions and normalize intestinal microflora, the following is also prescribed:
- Lactone,
- Linux,
- Lacidophilus.
Important! Please remember that all drug names are presented for informational purposes only. Only a doctor can select truly effective drugs for the pancreas after assessing the general condition of the organ and studying the patient’s medical history.
Treatment with enzymes and antienzyme agents
For swelling of the pancreas in adults, anti-enzyme medications for pancreatitis are prescribed. Intravenous drip administration is practiced. Patients are recommended to take Aprotinin, Contrikal. These medications are used twice a day. The duration of the therapeutic course for adults varies from 1 to 1.5 weeks. These medications are not prescribed only if individual intolerance is identified.
The patient is also recommended to take enzymes containing trypsin, amylase, and lipase.
The following medications are prescribed to treat pancreatitis in adults:
- Ferestal;
- Enzyme forte;
- Festal;
- Creon 25000;
- Pancreatin;
- Mezim;
- Creon 8000.
The active ingredients and composition of these tablets are the same. Enzymes for pancreatitis should be taken immediately after meals. The dosage is determined by the doctor depending on the level of lipase deficiency. If signs of steatorrhea are present, the patient is recommended to take vitamins B, A, E, D, K.
Medicines used in the treatment of pancreas
To relieve pain, analgesics and antispasmodics are prescribed. The first group of drugs relieves pain by suppressing the production of prostaglandins, the second eliminates spasm, due to which the sphincter of Oddi relaxes and the passage of pancreatic enzymes into the duodenum becomes possible.
Of the analgesics, preference is given to salicylates (Aspirin) or acetaminophen (Paracetamol), which should be taken before meals.
Antispasmodics may be prescribed:
- Drotaverine. Available in 40 mg tablets and 2 ml ampoules. When administered intramuscularly, the dosage for adults is 40–240 mg. When taken orally, 1-2 tablets are prescribed. The patient should receive the medicine 1-3 times a day;
- Papaverine. Produced in suppositories, solution, tablets (40 mg). You need to take 1 tablet three times a day. Suppositories are administered rectally, 1–2 suppositories (20–40 mg), 2–3 times a day. The solution is administered subcutaneously, intravenously or intramuscularly, 1–2 ml 2–4 times a day, and the interval between injections should be at least 4 hours;
- Mebeverine. You need to drink 400 mg of the drug, dividing the dose into 2-4 doses. One capsule 200 mg;
- Platyfillin. Available in ampoules. Prescribed 1–2 mg during periods of intense pain. You can drink no more than 10 mg at one time, and no more than 30 mg per day.
Ganglion blockers relax smooth muscles, dilate blood vessels, reduce the production of hydrochloric acid and gastrointestinal motility. This group belongs to:
Who treats the pancreas?
- Gangleron. Take 1 capsule 3-4 times a day before meals. The solution is administered subcutaneously or intramuscularly, 1 ml every 6–8 hours.
- Pyrylene. Available in tablets of 0.005 g. You need to take one tablet or half. The maximum single dose is 2 tablets, and the daily dose is 6 tablets.
- Benzohexonium. Prescribed intramuscularly, intravenously or subcutaneously. The dose is set individually and can be from 0.25 to 0.5 ml. The solution is administered an hour before meals 2-4 times a day.
The following drugs can reduce pain and weaken pancreatic secretion:
- Ranitidine. Histamine H2 receptor blocker. The dosage is prescribed depending on the patient’s condition (usually one tablet 1–2 times a day or parenterally 2 ml every 6–8 hours);
- Famotidine. This H2 receptor antagonist is available in 20 and 40 mg tablets. A single dose (10 or 20 mg) suppresses gastric acid secretion for 10–12 hours. The medicine begins to act within an hour after administration;
- Cimetidine. First generation histamine H2 receptor blocker. After taking 300 mg, the effect appears after an hour and lasts for 4-5 hours. For oral administration, a single dose is 100–800 mg, for intravenous or intramuscular infusion, 200 mg. The maximum dose for children over one year of age is 25–30 mg/kg/day, for infants – 20 mg/kg/day.
- Omeprazole. Refers to proton pump inhibitors. One capsule contains 20 mg of active substance, in bottles for preparing a solution for intravenous administration and infusion therapy 40 mg. Capsules should be taken in the morning before meals without crushing or chewing. Duration of action of the drug is 24 hours. Omeprazole is administered intravenously for 3–5 days, 20–40 mg, and then the patient is transferred to oral medication (Omez, Ultop) for 4–6 weeks;
- Atropine sulfate. It has an antispasmodic effect and also blocks M-cholinergic receptors. After taking atropine, the secretion of glands decreases, the heart rate increases, and the tone of smooth muscle organs decreases. The drug can be administered parenterally or orally. The dosage is selected individually;
- Pirenzepine. It has an M-anticholinergic and antiulcer effect, reduces the production of hydrochloric acid. Available in tablets of 0.025 and 0.05 g and in powder of 0.01 g (ampoules with solvent). Prescribed 1-2 tablets three times a day before meals, and after 2-3 days the frequency of administration is reduced to two times. Parenterally administered only in case of severe pain or hemorrhage.
Treatment of pancreatitis with antispasmodics
For acute pancreatitis in adults, cholinergic and antispasmodic medications are prescribed
The patient is recommended to take pills such as:
- Buskopan.
- Analgin.
- Paracetamol.
- Baralgin.
- No-Shpa.
These medications relieve spasms well. If a person suffers from very severe pain, then he is prescribed injections rather than tablets.
All medications for the treatment of pancreatitis in adults should be taken only as recommended by a doctor.
When are antibacterial agents needed?
Antibiotics are used if serious complications develop. For the treatment of acute pancreatitis, characteristic manifestations are swelling and stagnation of the gland, after which the fluid that the human body produces in the event of an inflammatory process begins to accumulate. This can lead to a dangerous complication such as peritonitis. And this condition can lead to the death of the patient. In order to avoid consequences in time, it is necessary to take antibiotics and injections into the abdominal cavity in a timely manner. In this case, the patient requires close attention from the doctor.
Unpleasant effects from treatment
To carry out proper treatment, a comprehensive treatment regimen is necessary to avoid side effects.
These include:
- Excessive fatigue;
- Constipation;
- Malfunction of the liver or bile;
- Fever.
Use of additional medications
Treatment of this disease involves the use of H2 blockers. The patient is recommended to take Ranitidine, Famotidine. In case of exocrine insufficiency, the patient is prescribed the use of antacids. They help normalize the functioning of the duodenum. Treatment for acute pancreatitis in adults involves taking Phosphalugel, Almagel.
The use of enveloping, choleretic, and sedative medications brings great health benefits. It is also recommended to drink hormones and calcium.
In order to prevent pancreatitis in adults, Asentra, Galstena, Gordox, Digestal, Duspatalin, Yogulakt, Creon 10000, Pangrol 10000, Pankreoflat, Reopoliglyukin, Hofitol are prescribed.
Antibiotics
Antibacterial drugs are prescribed in extreme cases. An indication for antibiotic therapy may be infection of the gallbladder or peripancreatitis against the background of the underlying pathology. For this purpose, patients are prescribed:
- Amoxicillin;
- Augmentin;
- Levomycetin;
- Cefoperazone;
- Cefixime.
If inflammation of the bile ducts is diagnosed during the disease, then patients are recommended to take Amoxicillin. Before using this drug, you must undergo a number of diagnostic measures:
- bacterial examination of bile, gastric and intestinal juice;
- bacterial seeding of biological material for flora;
- determination of the sensitivity of the pathogen to various groups of antibacterial agents.
Thanks to the tests, the doctor is able to select the most effective drug that will not provoke an imbalance in microbiocenotic processes and will have a minimal list of side effects. For non-infectious chronic pancreatitis, antibiotic therapy is not prescribed. In this situation, taking medications will do more harm than good.
Antibiotics are rarely used in the treatment of pancreatitis. The use in some cases is dictated by the complexity of the disease, when antimicrobial drugs cannot be avoided. Metronidazole often comes to the rescue. The doctor decides to prescribe medication for complex forms of the disease, when there is a threat of infection of the pancreas tissue.
The main thing is to be on time. Start taking metronidazole in a timely manner. With timely treatment, you can get rid of the disease. After passing the diagnosis, the doctor will prescribe a list of medications needed at the developing stage.
Antibiotics are used extremely rarely to treat pancreatitis. This is due to the fact that they do not help either relieve inflammation, or reduce the secretion of digestive enzymes, or eliminate pain. Their use is indicated only if the patient has:
- addition of a bacterial infection;
- pancreatic necrosis or cholangitis;
- rupture of the pancreatic duct;
- bile stasis.
In this case, antibiotics are used only to prevent the development of complications. And in the case of acute pancreatitis, the following are used:
- Ampioks,
- Amoxiclav,
- Vancomycin,
- Ceftriaxone,
- Ampicillin.
The dosage and duration of taking antibiotics is determined by the attending physician and can be adjusted depending on the patient’s condition and the course of the disease.
Remember that treatment of pancreatitis is a very complex and time-consuming process that requires a lot of strength and patience from the patient. Undoubtedly, drug therapy is necessary in this case. But we should not forget that diet plays an important role in this matter. And if you want to avoid constant exacerbations of pancreatitis, you will need to not only periodically take various medications, but also strictly monitor your diet.
Therapy for chronic pancreatitis
The main therapeutic goal for pancreatitis is to relieve pain, as well as avoid further exacerbation in the gland. The ability to take and digest food is normalized.
If the patient does not have serious complications, he is discharged from the hospital. For severe pain, analgesics are prescribed. In case of chronic pancreatitis, a person undertakes to follow a diet. You can only eat foods that contain virtually no fat. You can't drink alcohol. Sometimes additional medications are prescribed for chronic pancreatitis in adults. The patient is recommended to take pancreatic enzymes.
If the organ does not produce the normal amount of insulin, the doctor prescribes appropriate injections.
Diseases of the pancreas and their symptoms
It is errors in eating that often lead to damage to pancreatic tissue.
Over time, stones begin to form, leading to the development of diseases:
- Pancreatitis with inflammation in the pancreas. Reasons: unbalanced diet, abuse of medications, alcohol. Symptoms: swelling, death and disintegration of glandular tissue, self-digestion of trypsin, scarring, formation of replacement connective tissue, impaired outflow of secretions, narrowing of the glandular ducts. Obvious signs of pancreatitis are acute, cutting pain in the navel area against the background of pancreatic destruction, dyspepsia, bloating, rumbling in the intestines, nausea, aversion to fatty foods, profuse bowel movements in the form of diarrhea with an unnatural odor, leaving greasy marks on the toilet after flushing. Lack of treatment can cause complications: cyst, pustular abscess, type 2 diabetes.
- Lipomatosis with the formation of capsules (wen), damage to the subcutaneous fat. The disease is provoked by metabolism, hormonal imbalance, hereditary factors, the pituitary gland of the thyroid gland, changes in the body during adolescence, physical inactivity, smoking, alcohol, kidney and liver pathology, intoxication and dehydration of the body. Symptoms: discomfort, painful lump in the wen area, vomiting, poor digestion, flatulence, bloating, nausea. Possible complications: arthrosis of the knee joint, accumulation of fat in the blood. Lipoma can be treated well with painkillers and antiemetics (Mebeverine, Loperamide).
- Cyst , a self-developing pathology due to the deposition of salts in the tissues of the pancreas. It is possible that stones may form against the background of other past pathologies. Most often, pebbles clog the bile ducts, which can be easily felt by palpation in the anterior part of the peritoneum. Symptoms: fever, cutting pain in the abdomen, yellowness of the skin as stones pass through the bile ducts, indigestion, dyspepsia, nausea, vomiting. Treatment is surgery to excise the cystic tumor. If not removed, it may develop into pancreatic cancer.
- Gland cancer is an inflammatory course with the transition of the tumor to a malignant form. Signs: diarrhea followed by constipation, passage of greasy stool, weight loss, severe pain in the epigastric region. Treatment with medications helps only at the initial stage - choleretic drugs (Enzistal, Festal, Digestal), antispasmodics (Papaverine, Baralgin), antisecretory drugs (Pancreatin, Creatine).
Treatment of pancreatitis
Pancreatitis is the most common disease of the pancreas among all known ones. The treatment process will depend entirely on the identified form (acute, chronic). The patient must adhere to a strict diet.
In case of exacerbation, urgent hospitalization is required. The drug treatment regimen is selected by the doctor on an individual basis. In acute cases, fasting for several days and intravenous administration of drugs (Glucose, Albumin) are indicated.
In severe cases, artificial administration of pancreatic juice is possible in order to slow down damage to the body’s own cells. Treatment with medications is carried out during the period of exacerbation and in acute cases.
Main groups of drugs:
- antisecretory (Famotidine, Ranitidine);
- proton pump inhibitors (Rabeprazole, Omeprazole);
- antacids (Maalox);
- enzymes (Gordox);
- anticholinergics (Platifillin, Atropine);
- antispasmodics (Papaverine, no-shpa, Drotaverine);
- non-narcotic drugs (Ketorolac, Paracetamol, Analgin);
- prokinetics (Motilium, Cisapride);
- choleretic (Festal, Enzistal, Digestal);
- opioid drugs (Promedol, Meperidine, Tramadol).
In the first days, in case of exacerbation, a gentle diet with the inclusion of lactic acid products in the diet is indicated.
For chronic pancreatitis, treatment is carried out according to the following scheme: hunger + cold + rest. Next, a strict diet is prescribed. Patients should avoid fried and fatty foods, alcohol, and smoking.
Reference! The main symptom of pancreatitis is debilitating pain in the epigastric region, usually in a lying position, after eating. To alleviate the condition, you need to take a sitting position and apply cold (ice) to your stomach. In acute cases, you can take a painkiller. In severe cases, surgical removal of the destroyed parts of the organ cannot be avoided.
Treatment of diabetes
The main medicine for insulin-dependent type 1 diabetes is insulin. A distinctive feature of type 2 diabetes is high levels of glucose in the blood, leading to metabolic disorders and sudden weight gain in patients.
During treatment, an anti-carbohydrate diet is indicated. For insulin-dependent diabetes mellitus, medications are not used. It is simply necessary to carry out maintenance therapy, since medications become powerless.
If the sugar level rises to critical levels, the production of insulin in the pancreas is disrupted, then insulin is prescribed - the main hormones in tablets or a solution for intravenous administration using a syringe directly into the blood. Doctors use a special pump for this purpose.
The following drugs are prescribed:
- sulfonylurea derivatives (Maninil, Oltar);
- new generation drugs (Glidiab, Starlix, Diabeton);
- biguanides (Bagomet, Metformin, Glucophage);
- thiazolidinediones (Pioglar, Amalia, Aetos, Diaglyside, Ozone, Januvia, Trajenta, Insulat, Glucovance) to normalize metabolism and lower blood sugar levels;
- glucocorticosteroid drugs for persistently high blood sugar levels.
In case of complications, increased doses of insulin are prescribed.
Treatment of tumors
The main drugs used in oncology are chemotherapy drugs and cytostatics, which are more sensitive to tumor cells.
Prescribed for leukemia and other types of malignant neoplasms, they contribute to:
- suppression of cell proliferation in the bone marrow;
- reducing the number of aggressive lymphocytes;
- inhibition of the excretory function of pancreatic cells;
- rapid distribution of elements throughout the body;
- blocking the division of pathogenic cells when they enter the blood.
Cytostatic drugs are aggressive drugs that quickly destroy not only malignant cells, but also the body’s own cells, mistaking them for foreign ones. Prescription of drugs and dosages is carried out exclusively by a specialist.
Medicines have many side effects:
- hair loss;
- diarrhea, up to dehydration;
- severe bleeding.
Attention! As the tumor grows and reaches a large size, it becomes less sensitive and no longer responds to cytostatics. After their use, it is possible to prescribe other drugs in tablets that the patient swallows to achieve the effect. Dosages are selected exclusively by the attending physician.
Comment on the forecast
If the patient seeks medical help on time, then recovery soon occurs, and the gland returns to normal functioning. Life-threatening manifestations occur in approximately 5-10% of patients. The most serious complication is diabetes. Some patients show signs of kidney failure and brain damage.
Chronic pancreatitis is not completely cured. Organ damage is a continuous process. This often causes bleeding, pseudocysts or cancer.
Treatment and first aid for acute pancreatitis
Treatment in the presence of acute inflammation of the pancreas should be carried out in a surgical hospital or ICU, since this disease, even despite drug treatment, can sometimes be accompanied by life-threatening complications.
Patients with acute pancreatitis at the prehospital stage and in the first days of hospital treatment are given a strict gentle regimen - cold, hunger and rest. Medications prescribed by specialists during illness are designed to relieve pain, eliminate intoxication, reduce the functional activity of the pancreas, and also prevent possible infectious complications.
First aid that can be provided to a patient before the arrival of a medical team is based on the same principles:
- Cold . During pancreatitis, a massive release of pancreatic enzymes into the blood occurs, as well as its self-digestion, which can lead to necrosis. In order to reduce the functional activity of the organ, a cold compress is applied to the stomach and back. For this purpose, you can use an ice pack, a heating pad with cold water, even frozen foods.
- Hunger . The patient is strictly forbidden to eat food in the first days of illness. Also, until the permission of the attending physician, fluid intake is limited. You can drink no more than 50 ml every 30-60 minutes.
- Peace . The patient must be provided with complete rest, excluding physical activity and sudden movements.
- Antispasmodics . In order to relieve intense pain, you can give the patient No-Shpu or inject papaverine. These drugs have an antispasmodic effect on the smooth muscles of the common bile duct and lead to relaxation of the sphincter of Oddi, which prevents bile from entering the pancreatic ducts.
- Painkillers . To eliminate painful sensations, you can give the patient the drug Nimesulide, which has a pronounced analgesic and anti-inflammatory effect.
It is important not to self-medicate and not to take excessive amounts of painkillers. Eliminating pain will only bring temporary relief and give the appearance of well-being. Without specialized treatment, the inflammatory process in the pancreas will continue, leading to irreversible changes and complications.
The attending physician must be informed about all medications taken by a patient with acute pancreatitis at the pre-hospital stage.
Treatment for chronic illness
Chronic pancreatitis indicates inflammation of the bile duct with disruption of the anatomical structure and secretion of enzymes in the pancreas. The disease is accompanied by acute pain, so antibiotics cannot be avoided. Drug treatment of chronic pancreatitis includes taking drugs that have a complex therapeutic effect.
Important information: Can I take Omeprazole for pancreatitis?
Intramuscular administration of No-Shpa, Platiphylline or Papaverine in combination with analgesics will help eliminate pain. If there is no vomiting, you can take it in tablets.
To inhibit the secretion of digestive enzymes, Contrikal and Gordox are administered intravenously.
When remission occurs, Pentoxyl and Methyluracil are prescribed.
To block the formation of juices in the stomach and duodenum, take Rabeprazole, Ranitidine, Losek, Omez, Pariet. Other drugs are also used to treat chronic pancreatitis: antibacterial, to eliminate intoxication, and relieve swelling. For example, Trasylol, which is administered intravenously, helps against swelling of the gland (not intended for children under 18 years of age). The range of medicines is wide, you just need to choose them correctly after consultation with your doctor.
Symptoms of acute pancreatitis will disappear no earlier than after 5 weeks.
If chronic pancreatitis is diagnosed, then medications need to be taken for a long time, possibly years. Patients will need fermentation therapy throughout their lives. In this case, the tablet treatment regimen must be strictly followed.
As a result of alcohol dependence and long-term drinking, chronic alcoholic pancreatitis can develop. After a single dose of an alcohol-containing drink (or surrogate) in combination with fatty foods, manifestations of acute alcoholic pancreatitis are possible.
Classification of drugs
N-2 blockers
The activity of this group of drugs is aimed at counteracting gastric secretion. Such agents block H-2 receptors, suppress the formation of hydrochloric acid, relieve irritation of gastritis and acetylcholine.
Anticholinergics
A group of drugs helps eliminate pancreatitis. They facilitate the action of acetylcholine. If the disease is already chronic, then it needs to be treated with m-anticholinergic drugs. Drugs in this group block pathological impulses in the nerves and cerebral cortex.
Antacids
Antacids are medications whose action is aimed at removing hydrochloric acid. They are prescribed to patients who have high stomach acidity. When the formation of hydrochloric acid is high, the products produce a pancreatic enzyme. These drugs reduce the secretory function of the stomach.
Antispasmodics
Medicines that eliminate spasms are used in cases of impaired motor function of the gastrointestinal tract. Such failures appear due to a decrease in the tone of the sphincter of the pancreatic duct.
Enzymes
Enzymes include protease, amylase, and lipase, which are needed to break down food. They support the proper functioning of the pancreas, normalize digestion and stimulate the digestion of proteins and carbohydrates.
Causes
The pancreas is a delicate organ, the dysfunction of which can be caused by any negative impact of an external or internal nature. Treatment of the pancreas with any medications should be tailored to the individual characteristics of the person, the presence of concomitant pathologies, the nature of the disease itself and the circumstances under which the rapid development of the disease began.
Inflammatory processes in the glandular structure of the organ most often begin due to the negative impact of the following factors:
- Alcohol abuse;
- Gallstone disease, as a concomitant disease that aggravates the patient’s well-being;
- Infections;
- Chemotherapy;
- Hormonal effects that cause harm to the body (this can be either a hormonal imbalance or abuse of pharmacological drugs);
- Organ injuries;
- Idiopathic origin of the disease.
Antacids
Antacids introduced into the therapeutic regimen at the earliest stages demonstrate a good therapeutic effect. Due to the blockade of the secretory ducts, an increase in the secretion of juices occurs. Because of this, the acid-base balance is disrupted, provoking the development of unnatural processes in the stomach.
To remove the patient from such an unfavorable condition, a number of antacid drugs are prescribed. The following medications help relieve acute pain:
- Omez;
- Hectrocalm;
- Zantac;
- Acylok;
- Ocid;
- Contralock;
- Gastrozol;
- Pepsidil;
- Zoran;
- Famotodin;
- Gastrogen.
Important nuance
In addition to “classical” antacids, therapists and gastroenterologists resort to the use of proton pump blockers. A typical representative is Lanzoprazole. To reduce the production of pancreatic substances and relieve the inflamed organ, Aprotinin is used.
We also recommend viewing: The mechanism of formation of fibrolipomatosis and methods for its relief
Features of drug treatment
The effectiveness of treatment of all pathologies of the pancreas depends on its timeliness. You should consult a doctor as soon as possible if symptoms of dysfunction of this organ appear. And this can happen to anyone. Often, such diseases develop after prolonged use of alcohol, overeating, or excess fatty, fried or spicy foods in the diet. Moreover, inflammation of the pancreas can quickly lead to disruption of its functions and other complications. This is why timely therapy is so important.
For all patients with acute or chronic pancreatitis, the use of medications is the main method of treatment. This therapy helps relieve pain and inflammation, eliminate nausea, improve intestinal function and the production of enzymes. But with some other pathologies, for example, in the presence of a cyst, treatment with medications only helps to alleviate the patient’s condition and prevent complications.
Drug therapy should primarily be aimed at eliminating the cause of pancreatic dysfunction. These can be choleretic drugs, drugs for the treatment of gastritis, antisecretory and antacid drugs. They help improve the flow of bile and reduce the harmful effects of pancreatic juice on the mucous membrane.
The patient cannot independently determine which medications to take. Drug therapy is prescribed individually. Comprehensive treatment is required, which can be adjusted depending on its effectiveness or the development of complications. The dosage and regimen of medications is also prescribed by the doctor. Sometimes you even need to take pills at different times - some before meals, others after.
It is necessary to understand that in 90% of cases, the development of pancreatitis and other diseases of the pancreas is provoked by an unhealthy lifestyle, namely the abuse of tobacco and alcohol products, as well as the presence of a high content of fatty and fried foods in the diet. All this negatively affects the functioning of the gland and provokes the development of inflammatory processes in it.
And for treatment with pancreatic drugs to give a positive result, therapy must include a diet and giving up bad habits. If negative factors continue to influence the pancreas, it will not be possible to prevent further progression of the disease and the occurrence of complications against it. Your doctor will tell you how to eat if you have pancreatitis.
Proton pump inhibitors
Recently, H2-histamine receptor blockers have begun to replace more effective and safe drugs - proton pump inhibitors (PPIs). Their action is aimed at blocking the work of enzymes known as the “proton pump”, which are directly involved in the synthesis of hydrochloric acid. The advantage of PPIs is that they are not addictive after withdrawal, they are unable to provoke the development of pancreatitis, and cause a small number of adverse reactions.
All proton pump inhibitors are benzimidazole derivatives and therefore have the same mechanism of action. The active substance of the drugs selectively accumulates in the secretory tubules, where, under the influence of high acidity, it is converted and activated, blocking the work of the enzyme. PPIs are able to control the synthesis of hydrochloric acid throughout the day, regardless of what stimulates its release.
The most studied drug in this group is Omeprozole, a single dose of which provides rapid inhibition of hydrochloric acid synthesis. For acute inflammation of the pancreas, the drug is prescribed in a dosage of 20 mg once a day, for recurrent inflammation - 40 mg/day, chronic - 60 mg/day. After consuming Omeprozole, the production of hydrochloric acid is reduced by 50%. The decrease in acidity begins after 2 hours, the maximum effect is observed on the fourth day.
An effective medicine for pancreatitis is Pantoprazole, which is sold under the names Nolpaza, Sanpraz, Ulsepan. Pantap. The drug is effective regardless of food intake, but it is better to take it 10 minutes before a meal. The maximum concentration of the drug in the blood is observed after 2.5 hours, the effect lasts for a day. The duration of the course of treatment is determined by the doctor.
For the treatment of pancreatitis, Rabeprazole (analogs - Pariet, Razo, Khairabezol) is used as a complex therapy. PPIs begin to suppress acid production within an hour of taking the medication. The maximum decrease in the level of acidity in the stomach is recorded two to four hours after the first dose, a stable effect after 3 days of treatment. On the first day, the acidity level decreases by 61%, on the eighth day of treatment - by 88% of the original numbers.
Symptoms of pancreatitis
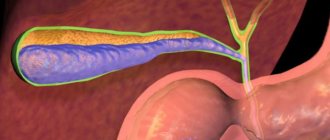
The pancreas synthesizes digestive enzymes and hormones that regulate protein, fat, and carbohydrate metabolism - insulin, glucagon, somatostatin. The organ has an oblong shape and is located in the upper abdomen, behind the stomach, in close contact with the duodenum. Iron weighs about 70 g, length ranges from 14 to 22 cm, width - from 3 to 9 cm, thickness - 2-3 cm.
Inflammation of the pancreas can occur in acute and chronic forms, the clinical manifestations of which are different. Acute pancreatitis is deadly, since toxins can provoke necrosis of pancreatic tissue and other organs, infection, and purulent processes. Even with timely treatment with modern means, the mortality rate is 15%.
There is no clearly defined clinical picture for acute pancreatitis, so additional examinations are necessary for an accurate diagnosis. In the acute form of the disease, false cysts often form in the pancreas, which cause pain in other organs and disrupt the movement of food through the stomach and intestines. In addition, the pathology manifests itself with the following symptoms:
- acute pain in the upper abdomen, radiating to the left side, back;
- nausea;
- vomiting with bile, which does not bring relief;
- bloating;
- dehydration;
- Jaundice may develop, accompanied by yellowing of the skin, dark urine, and light-colored feces;
- in some cases, bluish spots appear near the navel or on the left side of the abdomen, sometimes with a yellow tint.
With chronic inflammation, irreversible changes occur in the pancreas. It shrinks, the ducts narrow, the cells are replaced by connective tissue, which is why the organ ceases to perform its functions, and the synthesis of digestive enzymes and hormones decreases. Chronic pancreatitis is characterized by a vague clinical picture; its symptoms can easily be confused with other diseases of the digestive system.
The disease develops gradually and does not make itself felt for a long time. The pathology manifests itself as constant or periodic pain in the abdomen, near the left hypochondrium, and can radiate to the lower back. The disease is accompanied by nausea, vomiting, belching, heartburn, and an unpleasant sour taste in the mouth. Diarrhea may alternate with constipation; particles of undigested food are released along with feces. Sudden weight loss and the appearance of vascular spots are possible. Since the pancreas synthesizes insulin, chronic pancreatitis is often accompanied by diabetes mellitus.
Anti-enzyme medications
Pancreatitis is widespread and completely curable, so modern medicine has an extensive arsenal of tools to combat this disease. Treating an inflamed pancreas with medications at home takes a lot of time, but with proper selection of medications, healing is possible.
The listed medications will help relieve the attack, but after this the patient must immediately go to the hospital, where qualified specialists will prescribe conservative therapy. In case you or someone in your household experiences an attack of pancreatitis with an increase in temperature, make sure that you always have the following medications in your first aid kit:
- No-shpa;
- Drotaverine;
- Papaverine;
- Gentamicin;
- Omeprazole;
- Rennie;
- Ranitidine.
An exacerbation of pancreatitis cannot be without cause, so temporary relief after an attack cannot be regarded as a return to a normal healthy state. Refusal of professional medical care can lead to the development of fibrosis. This dangerous concomitant disease does not manifest itself in any way. It can only be detected by ultrasound.
The chronic form of inflammation can lead to functional failure. To avoid an increase in the size of the head of the pancreas, doctors prescribe long-term treatment with medications from the list:
- Almagel A;
- Maalox;
- Creon;
- Pancreatin;
- Mezim.
Such tablets for the pancreas are necessary, since organ dysfunction can develop under the influence of the inflammatory process. Restoring the functionality of the digestive tract without support will occur more slowly. During this period, complications may develop or the disease may become chronic.
Drugs in this group are divided into types according to composition:
- bile-containing (in addition to bile, they also contain enzymes);
- enzyme-containing (without bile in the composition).
In the first case, the products have a number of restrictions on use: ulcers, urolithiasis, gastritis. If you take bile-containing tablets, the condition of the affected organ may worsen. This group includes Festal and Enzym Forte. However, enzyme-containing drugs should be used with caution, since long-term therapy with their use may well lead to pancreatic dysfunction. If enzymes are used correctly, the pathological condition of this organ can be cured.
Review of drugs
When choosing a drug, the composition, indications and restrictions on use are taken into account. In addition, you must always remember that any drug can cause side effects. If the pancreas is being treated, medications containing enzymes are selected from a number of effective ones:
- Creon. Available in capsule form. The active ingredient is pancreatin. Creon helps normalize the digestion process; it does not contain bile. It is used to treat various pathological conditions that require enzyme replacement therapy: chronic pancreatitis, cystic fibrosis, surgical intervention for diseases of the pancreas and oncology of this organ, partial resection of the stomach, pathologies of the pancreatic ducts. It is important to remember that these tablets may well aggravate the patient’s condition in acute pancreatitis and in cases where an exacerbation of this disease in a chronic form has developed.
- Festal. Contains pancreatin and bile. With the help of the drug you can compensate for enzymatic deficiency. This medicine provokes many side effects: bowel dysfunction and abdominal pain, dizziness, vomiting and nausea, allergies. Festal helps increase uric acid levels. Indications for use: surgical intervention in which partial resection of the pancreas is performed, as well as inflammatory processes of various types. The drug is not prescribed for acute pancreatitis or during the development of exacerbation of chronic pancreatitis, as well as for intestinal obstruction, jaundice and urolithiasis.
- Enzistal. This is another combination medicine that contains ox bile and pancreatin. This remedy not only normalizes the process of enzyme production, but also helps improve the general condition of the digestive organs. Indications for use are pathologies of the pancreas that develop in various gastrointestinal diseases. There are few restrictions on the use of the medicine: bile duct obstruction, jaundice.
- Enzyme Forte. Represents a group of dietary supplements. The drug contains enzymes - pancreatin, as well as fennel extract. The solution to the question of how to treat enzymatic deficiency in pancreatitis should be sought together with a doctor, and not independently.
- Mezim. The active ingredient is pancreatin. The drug helps normalize the process of enzyme production and alleviates the condition of diseases of the digestive system. Restrictions on use: acute form of pancreatitis and exacerbation of chronic pancreatitis, lactose intolerance. The drug is not prescribed for children under 3 years of age.
Complications
Chronic pancreatitis, which occurs over a long period of time, affects all systems and organs. Its complications often include liver damage, morphohistological changes and complications of a purulent-inflammatory nature.
In the acute course of the disease, intoxication and pain are combated. In addition, specialists prescribe a course of antibiotics.
The patient during and after treatment must adhere to a diet, quit smoking and alcohol and follow all doctor’s recommendations, as well as treat concomitant gastrointestinal diseases in a timely manner. Periodic spa treatment can also be a good help in avoiding exacerbations.
What medications are prescribed
What pills can help with pancreatitis and properly restore functions in the gastrointestinal tract? This is the main question that is constantly asked by victims during a consultation at a medical institution.
With pancreatitis, periodic acute attacks and pain symptoms occur, so tablets are prescribed to eliminate these issues:
- Antispasmodics. The drugs are used for acute and cutting pain in the abdomen, so they are well suited: No-spa, analgin, baralgin and other painkillers. In case of severe pain, it is recommended to use it by injection.
- H2 blockers. To reduce the production of pancreatic juice and pancreatic enzymes, use Ranitidine and Famotidine.
- Antacids. If the clinical picture of the gland disease shows insufficient ability to secrete secretions and enzymes, the doctor will prescribe treatment for the pancreas, such tablets or drugs: Almagel, Phosphalugel.
- Enzyme agents. These preparations contain lipase, amylase, and trypsin. Among the most common medications, the main ones in demand are: Creon 8000, Mezim, Festal, Pancreatin.
Drug treatments and some medications for inflammation of the pancreas have to be used for more than one year, and the effect of taking the drugs is visible only after 3-4 months of constant and systematic use.
Antispasmodics
The main symptomatic effect on the body during inflammation of the pancreas is pain. Therefore, first of all, therapeutic fasting and medications - antispasmodics - are prescribed. They will help relieve pain and not spoil the clinical picture of the disease, which will not create problems or interfere with establishing the correct diagnosis.
There are a huge number of causes of pain symptoms during the inflammatory process of the pancreas. Among them, the main and most painful:
- swelling of the gland organ;
- severe stretching of the pancreas due to swelling;
- Oddi valve condition and spasmodic attack;
- spasms of the gallbladder and ducts;
- spasms of the small intestine.
All these negative actions are a vegetative reaction to the strong production of adrenaline and cortisol (the hormone of fear and stress). By acting on smooth muscles, these hormones provoke pain and side effects on the human body.
Therefore, when it appears, antispasmodics are used, which have a relaxing effect on this muscle group, which relieves pain completely or partially. How does the drug work for a developed chronic disease and what remedy should be used to relieve pancreatic pain?
It has been generally proven that the cause of pancreatitis is a spasm of the valve of Oddi, through which digestive juice and bile substance penetrate into the duodenum. Therefore, we treat the pancreas using the drug Duspatalin. It helps well with the chronic pathology of pancreatitis, but since the drug is in the form of tablets or powder, use in the acute phase of pancreatitis is undesirable.
In the acute form of pancreatitis, the pain syndrome has a severe attack, which in some cases provokes shock and death. Therefore, to relieve this painful condition, special drugs and injections are used:
The drug No-shpa is of plant origin, which allows it to be used in tablets, but only in the absence of vomiting. Therefore, you should not delay use, since the pain threshold of a person with acute pancreatitis will cause severe harm to the mental state and cause pain shock.
As for papaverine, the drug is similar to its actions on No-shpu, and relieves tension from the smooth muscles of the abdominal region. The disadvantage is the short duration of action, which requires repeating the dose after 3-4 hours.
A long-acting drug is Platiphylline. Consumption relieves pain symptoms for 12-14 hours and is administered intramuscularly. Having a strong effect on the source of pathological pain, its use is carried out under the supervision of doctors.
Antispasmodics cope well with painful symptoms of the pancreas; drugs are used to maintain muscle tone in a relaxed state, which improves the course of the disease.
Antibacterial drugs
Prescribed drugs in the treatment of acute inflammation of the pancreas stop the negative state of the sick person and bring this pathology into a stable direction of remission. A dangerous manifestation of pancreatitis in the acute phase contributes to damage not only to the organ itself, but also to the corrosion of the walls of the gland and its ducts by pancreatic juice. In turn, this will lead to the appearance of dead areas of the pancreas - tissue necrosis or peritonitis.
The goal of treating the pancreas with antibiotics is:
- relieving the inflammatory process;
- preventing the development of infectious diseases of neighboring organs exposed to enzymes and pancreatic juice;
- relieving inflammation from the gland itself.
When tests confirm a rupture of the bile ducts or stagnation in the bladder, broad-spectrum antibiotics are also the main drugs. The doctor, using the available tests, prescribes, depending on the developmental pathology, the necessary course of drug treatment with antibacterial drugs.
What helps and what antibacterial tablets help treat the pancreas and gland:
- at the time of home therapy and a mild stage of the disease, Oletetrin, Tetracycline group of drugs, Sigmamycin are prescribed;
- development of acute pancreatitis, Tienam, Cefotaxime, Abaktal, Vankrmitsin are used in hospital hospitals;
- improvement of microflora, give Linex, Bifiform, Lactiale.
The attending physician will tell you in more detail which medications to take and which ones should be avoided when treating the pancreas, after a full course of diagnostic measures.
Anti-inflammatory
Anti-inflammatory drugs are used to treat various pathologies of inflammatory diseases. Non-steroidal drugs NSAIDs are considered one of the most powerful drugs. They do not easily relieve pathogenic processes, but also lower body temperature and relieve pain in the body. These drugs are prescribed by a gastroenterologist. Therefore, independent decisions and uncoordinated use are categorically unacceptable, as they will lead to health consequences if used incorrectly. What drugs are used to treat pancreatic pathology?
Basically, in the treatment of inflammation of the pancreas, anti-inflammatory medications are used in hospital hospitals, which are mostly introduced into the body, bypassing the gastrointestinal tract, intravenously, intramuscularly. Thanks to the method, the medicine quickly enters the human bloodstream, which speeds up recovery and relief from the symptoms of the disease.
A good anti-inflammatory drug for the treatment of the pancreas is a combined composition of Analgin and Baralgin, depending on the symptoms of pancreatitis, the size and quantity of each drug is prescribed by the attending physician.
And also in the treatment of the gland, Atropine with the addition of Papaverine and Phenicaberane is used in treatment. Having strong capabilities to relieve inflammation and pathogenic properties of pancreatitis, this composition relieves symptoms and accelerates recovery.
Diagnostics
Diagnosis of pancreatitis is a complex and multi-stage process, which includes collecting complaints and conducting laboratory tests. Such a variety of diagnostic methods is necessary in order to make an accurate diagnosis. After all, pancreatitis can occur under the guise of diseases of other organs. Therefore, a comprehensive examination of the patient is required.
This examination is prescribed to all patients with pancreatitis of the pancreas. Ultrasound is a high-quality and highly informative study. All other research methods are not highly effective.
This study is often prescribed when complications occur. X-rays allow you to examine the organ in detail, assess the extent of its damage and determine the amount of healthy and fatty tissue.
An endoscopic examination is carried out using a special probe, which is inserted into the main duct and an x-ray is taken. With the help of such an examination, the patency of the ducts is assessed. During the examination, small stones that are excreted naturally can be removed. This method is minimally invasive, which is why many people prefer it.
Enzyme preparations
After the patient’s condition has been alleviated, when he has already begun to eat, enzyme therapy is used to maintain the pancreas and improve the digestion process. These drugs should be taken immediately after meals, the dose is prescribed individually. Typically, such tablets for the pancreas are taken for quite a long time, in cases of chronic disease or severe insufficiency of the functions of this organ - constantly.
The most common enzyme preparation is Pancreatin. The tablets Mezim, Festal, Creon, Panzinorm and others have a similar effect. But they are made from pork, so they can cause allergic reactions in some people. In this case, you need to take enzymes based on plant components - rice fungus or papain. The most famous drugs are Unienzyme, Somilaza and Pepfiz.
Features of taking medications for pancreatitis
The doctor must prescribe a treatment regimen and explain which medications for the pancreas should be taken after and which ones during meals. For example, enzyme medications for pancreatitis are taken simultaneously with meals, while antibiotics are taken after, proton pump inhibitors are taken once a day. Painkillers can be taken if necessary at any time, strictly following the dosage indicated in the instructions.
All tablets for pancreatitis should be taken with plenty of clean drinking water. During illness, alcohol is strictly prohibited, the toxins of which have a destructive effect on all cells of the body, including the pancreas. The combination of drugs with ethanol will increase the load on the liver, kidneys, and other organs of the digestive tract, leading to serious complications.
Any medicine can cause side effects and has contraindications, so before use you must read the instructions and tell your doctor about any chronic diseases. If a medicine for pancreatitis provokes complications and serious side effects, it should be discontinued immediately, replacing it with another active ingredient.
The duration of treatment with each specific drug is prescribed by the doctor. For example, antibiotics should not be taken for more than two weeks, as bacteria become addicted and the medications become ineffective. It is impossible to interrupt the prescribed therapy, since this can not only reduce the effectiveness of treatment, but also provoke a relapse of the disease.
For treatment to be effective, you must adhere to a diet. In the acute form of the disease, a hunger strike is indicated in the first two days, after which you can begin to eat low-calorie foods. Fatty, spicy, salty, peppered, smoked foods and other dishes that stimulate the secretion of gastric juice and gas formation in the intestines are prohibited.
Treatment with folk remedies
Traditional medicine in combination with drug therapy will speed up recovery and alleviate the patient’s condition. The following recipes will help:
- You need to drink 100 ml of infusion from the leaves of strawberries, lingonberries, blueberries, and corn silk. The components are taken in equal parts, crushed, and poured with a glass of hot water. Leave overnight.
- Various herbs are very effective. You need to drink 50 g of iris and wormwood decoction for a week.
- Stir a tablespoon of flour in a glass of kefir, eat the mixture in the morning, replacing breakfast with it.
- Take 30 drops of Rhodiola rosea tincture before meals.
- The parsley is washed, placed on the bottom of the pan, milk is added, which should cover the greens completely. The dishes are placed in the oven. The milk should melt, but not boil away. Strain. Take two tablespoons every hour. The product must be drunk completely the day before. It is an effective diuretic. It has a beneficial effect on the pancreas and can refresh and improve complexion.
Reasons for appearance
The development of acute and chronic pancreatitis can be caused by general and pathological factors. The latter are consequences or complications of existing diseases of the internal organs, the course of which has disrupted the functioning of the pancreas.
The following causes of the disease are identified:
- poisoning with low-quality food products or daily contact with chemicals of toxic etiology;
- chronic alcoholism (recent scientific studies have shown that about 70% of all patients with pancreatitis abuse alcohol);
- the presence of a concomitant disease in the form of cholelithiasis, the development of which disrupts the stable supply of bile, reduces the function of the entire digestive system (about 20% of all patients have a history of this pathology);
- infectious diseases of the stomach and intestines (most patients suffering from pancreatitis are carriers of the bacterial microorganism Helicobacter pylori);
- anomalies in the intrauterine development of pancreatic tissue, when the first signs of pancreatitis are observed in an infant from the first days of his independent life;
- mechanical injuries to the abdominal cavity, which led to contusion of pancreatic tissue and the formation of internal hematomas;
- parasitic diseases of the endocrine system organ in the form of opisthorchiasis or trematodiasis;
- damage to pancreatic tissue by fungal infections that cause premature death of its cells;
- acquired or congenital dysfunction of the sphincter of Oddi;
- negative consequences of a previous surgical intervention or endoscopic examination (this reason for the development of pancreatitis occurs in 5% of cases when the disease is diagnosed).
Treatment of pancreatitis with medications (drugs are prescribed based on the results of a diagnostic examination) brings a much greater therapeutic effect if the cause that triggered the development of the disease is initially established.
This approach allows you to eliminate harmful factors, create the right diet and lifestyle that minimize the risk of relapse of the disease.