Among all primary vasculitis, the most common is hemorrhagic vasculitis or Henoch-Schönlein disease. This pathology is also known as rheumatic purpura. Against the background of this disorder, a shift occurs in the hemostatic system with the subsequent development of microthrombovasculitis. It can occur either instantly or chronically, so treatment is individualized.
Hemorrhagic vasculitis (HDV or Henoch-Schönlein disease) is an inflammatory disease from the group of vasculitis, which affects small blood vessels (capillaries). It is usually a self-limiting pathological condition. Synonyms - allergic purpura, allergic vasculitis, anaphylactoid purpura, hemorrhagic capillary toxicosis, leukocytoclastic vasculitis, non-thrombocytopenic idiopathic purpura, rheumatic purpura, vascular purpura.
This is the most common form of vascular inflammation in children (among vasculitis), which leads to inflammatory changes in small blood vessels.
The development of hemorrhagic vasculitis is based on a disruption of the immune system, which causes inflammation of the vascular wall. The disease is most often diagnosed in children under 5 years of age, and in such cases the fulminant form of GDV most often develops. With timely treatment, it is possible to improve the patient’s quality of life.
Video: Henoch-Schönlein purpura - Hemorrhagic vasculitis
Reasons for development
The exact causes of the disease are not reliably known. The disease can suddenly appear even in a healthy person. Official medicine puts forward several basic theories regarding the causes of the development of vasculitis.
In 90% of cases, the disease occurs against the background of another infectious or viral disease. Viruses and bacteria give a powerful impetus to the development of inflammation in the vascular system of the body.
The most dangerous from the point of view of the possibility of developing vasculitis is viral hepatitis. It is after this disease that inflammatory processes in blood vessels occur most often.
Predisposing factors
They are not the main “culprits” for the development of vasculitis, but can contribute to the development and progression of the pathology.
The most common predisposing factors:
- frequent and prolonged hypothermia;
- negative effects on the body of various toxic substances;
- genetic predisposition;
- weakening of the body's protective functions (reduced immune status);
- hyperactivity of the immune system (as a reaction to infection);
- overheat;
- poisoning;
- skin damage (mechanical, thermal, etc.);
- allergies to certain types of medications;
- diseases and inflammatory processes of the thyroid gland;
- autoimmune diseases;
- complications of diseases such as systemic lupus erythematosus, reactive arthritis.
Development mechanism
The development of vasculitis occurs as a result of the formation of so-called immune complexes. Getting into the blood and circulating, these elements are deposited on the walls of blood vessels and provoke their damage with the subsequent development of inflammation. The inflammatory process, in turn, increases vascular permeability and causes the appearance of the main pathological signs of vasculitis.
Causes of hemorrhagic vasculitis
The exact cause of GDV is not fully understood, although research suggests that it is associated with an abnormal immune system response. In some cases, the causative factor is an extreme allergic reaction developing to some offending substance (such as food or drugs).
Research suggests that hemorrhagic vasculitis may be caused by dysfunction of the immune system (ie, increased levels of IgA immune complexes). Autoimmune disorders occur when the body's natural defenses against “foreign” or invading agents (such as antibodies) begin to attack healthy tissue for unknown reasons.
It has been suggested that this disorder may result from:
- An extreme allergic reaction to certain foods, such as chocolate, milk, eggs, or beans.
- Various drugs (eg, nifedipine, diltiazem, cefuroxime, diclofenac, etc.), bacteria (eg, Streptococcus) and insect bites have also been reported as possible causes of GDV.
- Rubella precedes the first symptoms of GDV in approximately 30% of cases.
- In about 66% of cases, upper respiratory tract infection precedes the onset of symptoms by about 1-3 weeks.
The connection between GDV and viral infections has not been proven.
Video: Causes of vasculitis
Prevalence
GDV is a rare disorder that affects more men than women. The disease can occur in all age groups, but is more common among children.
In children, initial symptoms usually begin after 2 years of age and last for about 4 weeks. The disease in such cases is characterized by a mild course. About 50% of affected children experience one or more relapses within two to three months. The relapse rate appears to be higher in those children with a more severe onset of illness.
The affected children are mostly between 2 and 11 years old. In the United States, there are about 14 cases for every 100,000 school-age children. As a rule, a benign (non-threatening) disorder appears in most cases for self-medication (self-restraint).
Types, forms, classification
Vasculitis has a huge number of types, forms, subtypes and classifications.
Some forms and types of the disease affect exclusively the skin. Others affect vital organs and cause significant harm to the entire body, in extreme cases leading to death.
According to the causes of occurrence, vasculitis is divided into:
- Primary. They are a consequence of inflammation of the walls of the blood vessels themselves. They arise independently and are in no way associated with other pathologies.
- Secondary . They represent the reaction of the vessels themselves to other diseases occurring in the body. Secondary vasculitis is inflammation that occurs against the background of viral or infectious diseases, oncology, or taking certain medications.
Let us consider below the classification of vasculitis (CHCC nomenclature) depending on the location of the disease.
Vasculitis of large vessels . We are talking about the following diseases:
- Takayasu arteritis. A pathology of an autoimmune nature, in which the walls of the aorta and its branches are affected by a pronounced inflammatory process. Women suffer from Takayasu's arteritis much more often than men - in a ratio of 8:1.
- Giant cell arteritis. Another pathology of an autoimmune nature, which also affects the aorta and its branches and often occurs against the background of rheumatism. The most common reason for the development of this type of vasculitis is infection of the patient with herpes or hepatitis viruses.
Vasculitis of medium vessels:
- Kawasaki disease. A disease that occurs in an acute febrile form and most often affects children. The inflammatory process in this type of pathology involves not only large, but also medium-sized vessels - veins and arteries.
- Periarteritis nodosa. An ailment during which inflammation of the walls of small and medium-sized vessels occurs, which provokes more serious diseases and pathologies - myocardial infarction, thrombosis, etc. The most common “culprits” of the pathology are the hepatitis virus, as well as individual intolerance to certain medications.
Small vessel vasculitis . ANCA-associated vasculitis is in turn divided into:
- Granulomatosis with polyangiitis. A severe autoimmune disease that tends to progress rapidly. Affects capillaries, venules, arterioles. Quite often the lungs, organs of vision, and kidneys are involved in the pathological process.
- Microscopic polyangiitis. A pathology poorly studied by modern medicine. With inflammation of small vessels of this nature, several vital organs are affected at once - most often the kidneys and lungs.
- Eosinophilic granulomatosis with polyangiitis. A disease that occurs when there is an excess amount of eosinophils in the blood, an excess of which leads to the development of severe inflammation in small and medium-sized vessels. In most cases, this disease affects the respiratory organs and kidneys, and the patient suffers from severe shortness of breath, severe runny nose or bronchial asthma.
- Immune complex small vessel vasculitides: immunoglobulin A associated vasculitis, cryoglobulinemic vasculitis, anti-GBM disease.
In addition, official medicine identifies vasculitis, which can simultaneously affect large, medium and small vessels. We are talking about diseases such as:
- Behçet's disease. The pathology manifests itself by the frequent appearance of ulcers on the surface of the mucous membranes (in the mouth, in the genital area, on the gastric mucosa, etc.).
- Cogan's syndrome.
In some situations, the disease affects specific organs (vasculitis of individual organs). When 2 or 3 organs are affected simultaneously, doctors diagnose “systemic vasculitis.”
Forecast
There are many types of vasculitis, but overall the condition is rare. If you have angiitis, the prognosis depends on:
- Vasculitis type;
- What parts of the body are affected;
- How quickly the condition worsens;
- The seriousness and severity of your condition.
The disease responds well to treatment if it is started in a timely manner. In some cases, vasculitis may go into remission. “Remission” means “reduction, weakening” of the ongoing disease process, but it can also return at any time.
Sometimes vasculitis is chronic (long-lasting) and does not go into remission. Long-term medication treatment can often control the signs and symptoms of chronic vasculitis.
It is rare, but it happens that angiitis does not respond well to treatment, which can lead to disability and even death.
Much is still unknown about vasculitis. However, scientists continue to study what this disease is and its different types, causes and treatments.
Symptoms
Regardless of the form and type, most vasculitis occurs with similar symptoms. The most characteristic symptoms of the pathology:
- loss of appetite followed by weight loss;
- decrease in body temperature;
- the appearance of unsightly rashes on the skin;
- constant persistent pain in the joints;
- pale skin;
- fatigue, weakness, malaise;
- frequent sinusitis;
- regular exacerbations of heart and vascular diseases;
- nausea and vomiting;
- sensitivity disorders - from minimal to pronounced;
- myalgia and arthralgia.
Clinical manifestations of the disease may vary depending on the type of vasculitis and its location. In this case, the main symptom of the pathology, in any case, remains a violation of normal blood circulation in the organs and systems of the body.
Signs of hemorrhagic vasculitis
Symptoms of GDV usually begin suddenly and may include:
- Headache.
- Fever.
- Loss of appetite.
- Spasms.
- Abdominal pain.
- Painful menstruation.
- Hives.
- Bloody diarrhea.
- Joint pain.
Red or purple spots usually appear on the skin and are called petechiae. Classically, the rash appears on the buttocks, back and legs .
(A and B) Classic skin lesions of GDV with palpable purpura on the extremities. (C) Arthritis and purpura on the lower extremity. (D) Bullous and necrotic lesions of the lower extremities in a patient with complex purpura.
Inflammatory changes associated with GDV can also develop in the joints, kidneys, digestive system and, in rare cases, the brain and spinal cord (central nervous system).
Features of manifestations of different forms of hemorrhagic vasculitis:
- With Schonlein purpura, the skin and joints are affected, but there is no inflammation of the gastrointestinal tract.
- With Henoch's purpura, patients are characterized by purple spots on the skin and acute processes in the abdominal cavity, such as glomerulonephritis (a type of kidney disease). In this form of GDV, the joints are not affected.
In addition to the characteristic red spots on the skin, headache, loss of appetite and/or fever may be detected.
- The skin usually becomes red (diffuse erythema).
- Abdominal pain becomes most severe at night.
- Blood may be present in the stool, and abnormal bleeding (hemorrhage) from the gastrointestinal tract is diagnosed as bloody diarrhea.
- Joint pain (arthralgia) can occur in any joint, but most often the knees and ankles are affected.
- Some people with GDV experience vomiting and diarrhea, while others have severe constipation and unusually dark stools (melena).
Patches of purpura are caused by small hemorrhages under the skin and are not associated with abnormally low platelet counts (nonthrombocytopenic disorder) that occur in some other forms of purpura. Other skin lesions associated with GDV include large blisters (hives) or sores (tissue necrosis), especially on the buttocks and legs.
Swelling may occur in the face and neck due to abnormal accumulation of fluid in the soft tissue of the affected areas (angioedema). In rare cases, swelling develops in the larynx, which can cause difficulty breathing, which can lead to life-threatening respiratory complications.
A quarter to a half of people with GDV develop problems with kidney function, such as glomerulonephritis , which damages the kidney tissue. As a result, the process of purifying the blood from various metabolites is disrupted. The pathological process is expressed in the determination of blood in the urine (hematuria) and inflammatory changes in the kidneys. Some people may develop severe kidney disease, including nephropathy, chronic kidney inflammation (nephritis), and/or nephrotic syndrome, leading to kidney failure.
In rare cases, part of the victim's intestine may fold in on itself ( intussusception ). This results in significant pain and, if conservative measures do not resolve the problem, surgery may be required.
When the central nervous system is involved, people with this disorder may experience severe headaches, perceptual changes, visual difficulties (optic atrophy), and/or seizures.
In children
Children suffer from pathology many times more often than adults. The incidence of the disease is 25 cases per 100 thousand children. Young patients are overwhelmingly faced with Kawasaki disease, as well as various types of systemic vasculitis. Children aged 4 to 12 years are most susceptible to the disease. Children under 3 years of age suffer from vasculitis extremely rarely.
In minor patients, the disease affects the joints, gastrointestinal tract, small vessels of the epidermis, and kidneys.
As the disease develops, inflammation of the walls of blood vessels occurs, followed by their blockage with blood clots. As a result, there is a disruption in tissue nutrition processes. Adequate and timely prescribed therapy makes it possible to cope with the disease within 4-6 weeks in 70% of children. In 30%, the pathology becomes chronic and periodically manifests itself with relapses.
Symptoms
Figure A shows a normal artery with normal blood flow.
The small image next to the right side shows a cross-section of a normal artery. Figure B shows an inflamed, narrowed artery with reduced blood flow. The image on the right shows a cross-section of an inflamed artery. Figure C shows an inflamed, blocked artery and scarring on the artery wall. The small adjacent image on the right shows a cross-section of a blocked artery. Figure D shows an artery with an aneurysm. The adjacent image shows a cross-section of an artery containing an aneurysm. Poor circulation caused by inflammation can damage the body's organs. Signs and symptoms depend on which organs are damaged and the extent of the damage.
Typical symptoms of inflammation and damage to the walls of blood vessels:
- fever;
- swelling;
- general malaise and pain.
Photos of people with angiitis:
Photos of vasculitis on people's legs
Diagnostics
To ensure timely detection of a dangerous disease, a comprehensive examination is carried out. Tests and specific studies that are indicated for patients with suspected vasculitis:
- a general blood and urine test (allows you to confirm or refute the presence of an inflammatory process in the body);
- biochemical blood test (with the development of vasculitis, it determines a decrease in hemoglobin, moderate thrombocytosis, leukocytosis and hematocrit);
- angiography;
- ECHO-cardiography;
- Ultrasound of the heart, kidneys, abdominal organs.
X-ray examination of the lungs allows you to assess the condition of the affected vessels and the location of the inflammatory process.
Vasculitis is most difficult to diagnose in the early stages, when the disease does not have pronounced symptoms. With the intensive development of the disease, it is much easier to determine it. More obvious signs appear only when several organs are affected at once.
In the most severe cases, to diagnose the disease, a biopsy of the affected tissue is performed, followed by a detailed examination.
Complications
With the help of modern therapy aimed at suppressing the immune system, it is possible to achieve stable remission and delay the consequences of vasculitis. If the treatment is chosen incorrectly, or the patient does not follow the rules for taking medications, the disease continues to progress and lead to various complications.
The most common complications are:
- arterial hypertension;
- infectious complications;
- thrombosis and bleeding;
- nephrotic syndrome;
- pulmonary hypertension.
Systemic vasculitis has a very high risk of complications, but timely treatment helps to slow down their occurrence. If treatment aimed at suppressing the immune system is not carried out, the prognosis becomes unfavorable. Only 10% of the total number of patients survive for 5 years. If active therapy is carried out using cytostatics and glucocorticosteroids, then 60-90% of patients survive for 5 years.
Since the disease is autoimmune, there is no specific prevention of vasculitis. You need to harden your body, eat right, treat inflammatory and infectious diseases, and strengthen your immune system. If signs of inflammation appear, such as a sharp decrease in body weight, constant weakness, fever, accompanied by skin rashes, you should consult a doctor. In this case, after diagnosis, adequate therapy will be prescribed, and the disease can be kept under control.
Treatment
Accurate and timely diagnosis determines 50% of the effectiveness of treatment for vasculitis of any form or type. Of no small importance is the elimination of initial organ damage and associated diseases.
When treating pathologies with severe symptoms, an integrated approach is required. Only complex therapy will quickly relieve the unpleasant symptoms of the disease, improve the patient’s condition and avoid serious complications.
Any type of treatment for vasculitis should be agreed with the attending physician and carried out only after a comprehensive diagnosis and diagnosis.
Drug treatment
Conducted for the purpose of:
- eliminating pathological reactions from the immune system that underlie the disease;
- prolongation of periods of stable remission;
- therapy for relapses of pathology;
- preventing the occurrence of secondary ailments and complications.
Treatment with medications involves prescribing and taking the following medications:
- Glucocorticoids . A special group of hormonal drugs that have a pronounced effect: antiallergic, anti-inflammatory, anti-stress, immunoregulatory and some others. Taking the drugs has high rates of therapeutic effectiveness and provides longer and more stable periods of remission. The most popular and frequently used glucocorticoids for vasculitis are Hydrocortisone and Prednisolone.
- Cytostatics . Medicines that slow down the growth and division of all cells in the body, including tumor cells. Taking medications in this series is especially effective for vasculitis accompanied by kidney damage. For systemic vasculitis, simultaneous administration of glucocorticoids and cytostatics ensures the fastest possible relief of pathological symptoms and improvement of the condition. The average course of taking cytostatics for vasculitis is from 3 to 12 months. Common cytostatics recommended for use for vasculitis are Doxorubicin, Methotrexate, Cyclophosphamide, etc.
- Monoclonal antibodies . A special type of antibody produced by the body's immune system. Drugs from this category are indicated for patients who, for one reason or another, cannot undergo cytostatic therapy. Medicines in this series have their own contraindications for use. The main one is viral hepatitis B. The most popular monoclonal antibodies among doctors to prescribe are Rituximab.
- Immunosuppressants . Drugs that are used as part of complex therapy together with glucocorticoids and provide an inhibitory effect on the immune system. Azathioprine and Leflunomide are the most popular drugs in this series.
- Human immunoglobulins . Medicines that are most effective for severe infectious lesions of the kidneys and other organs, hemorrhagic alveolitis.
- Anti-infectives . Used in case of development of vasculitis against the background of diseases and pathologies of an infectious nature of bacterial origin. Viral lesions are treated with antiviral medications - Interferon, Lamivudine. Viral hepatitis is treated with drugs based on the type of hepatitis virus.
- Anti-intoxication therapy . The main purpose of its implementation is to remove toxins from the body. For binding, popular absorbent preparations are used - Atoxil, Enterosgel.
- NSAIDs . They are used in the case of thrombophlebitis with nodular forms of vasculitis, persistent inflammatory processes, and extensive necrotic foci. Ibuprofen, Indomethacin, Acetylsalicylic acid are the most popular and frequently prescribed non-steroidal anti-inflammatory drugs with high rates of effectiveness.
- Anticoagulants . Indicated for use by patients with a tendency to thrombosis. Drugs in this category prevent the formation of blood clots in blood vessels, improve circulatory processes, normalizing blood flow in the bloodstream. Coagulants effective for vasculitis are Heparin and Warfarin.
- Antihistamines . Antiallergic drugs are prescribed when allergic reactions occur - food or drug allergies. Tavegil, Claritin, Diazolin are relatively inexpensive, but quite effective antihistamines.
For certain indications, ACE inhibitors and vasodilators can be used for vasculitis.
Quite often, for vasculitis with damage to the skin, local agents are used - creams, ointments, gels with anti-inflammatory and analgesic effects. They are applied directly to the affected areas of the skin. The main purpose of their use is to reduce the severity of the inflammatory process, as well as relieve intense pain.
In patients with areas of necrosis on the skin, as well as ulcers, regular dressings with the use of local antiseptic drugs, as well as ointments that accelerate epithelialization processes are indicated.
Non-drug therapy
It includes modern methods of extracorporeal hemocorrection - special procedures for purifying the blood of substances that cause the occurrence and development of vasculitis.
Main types of non-drug treatment:
- Hemocorrection . Provides for purification of the patient's blood using a special sorbent. Blood is drawn using a venous catheter. Afterwards, the blood is passed through a special apparatus, which introduces an absorbent component into it. The blood then returns to the bloodstream. At the same time, the sorbent does its job - cleanses the blood and its components, improves blood circulation and tissue nutrition.
- Immunosorption . A procedure during which the patient’s blood is passed through a device filled with immunosorbent. It is this substance that binds antibodies produced by the immune system, which provoke vascular damage.
- Plasmapheresis . A special method of purifying blood plasma using a special centrifuge. The procedure has a beneficial effect on the condition of blood vessels, reduces the severity of inflammation, and also prevents the risk of developing renal failure, and generally improves kidney function.
Diet
The main principle of the diet for vasculitis is to exclude from the diet foods that can cause or intensify allergies. For this purpose, the following products are excluded from the patient’s diet:
- milk and eggs;
- seafood;
- strawberries and wild strawberries;
- mango, bananas, citrus fruits;
- some vegetables - bell peppers, carrots, tomatoes;
- canned food;
- chocolate;
- baked goods;
- products to which the patient has an individual intolerance.
If vasculitis is accompanied by kidney damage, the doctor may recommend diet No. 7. For patients with severe disorders of the gastrointestinal tract, table No. 4 is recommended.
Preventive actions
They are necessary not only to prevent the occurrence of pathology, but also to speed up the recovery process, reduce the risk of complications, and also prolong periods of stable remission.
Basic preventive measures:
- minimizing stress;
- rational and proper nutrition with the exclusion of harmful foods from the diet;
- maintaining body weight within normal limits;
- refusal of any self-medication - taking medications without a doctor’s prescription;
- timely treatment of emerging diseases to avoid the transition of ailments to a chronic form;
- maintaining an active lifestyle;
- giving up bad habits - alcohol, smoking, etc.;
- eating a large amount of foods rich in vitamins, minerals, micro- and macroelements.
In children, treatment of vasculitis is carried out according to the same scheme and with the same drugs as in adults. After recovery or achieving stable remission, the child is registered with a rheumatologist and subsequently undergoes routine examinations by a specialist at least 3-6 times a year.
Diet
Diet for hemorrhagic vasculitis in children is an important part of therapy. In case of severe abdominal syndrome (abdominal pain, diarrhea), a gentle diet is prescribed excluding foods that cause allergic reactions:
- cocoa, chocolate;
- all types of citrus fruits;
- berries;
- eggs;
- spices;
- canned food, smoked meats;
- mushrooms and nuts
Important information: How to treat hemorrhagic vasculitis (purpura) in adults and what are the symptoms of Henoch-Schönlein disease
The consumption of animal protein, meat and fish broths rich in extractive substances is limited, and the daily amount of salt is reduced. The following products are allowed:
- vegetables - cabbage, including cauliflower, potatoes, zucchini;
- meat - chicken, rabbit, turkey, lean beef and lamb;
- fermented milk drinks, low-fat cottage cheese;
- fruits - green apples (at first - only baked ones), pears, bananas;
- crackers, bagels, bread, waffles without filling;
- tea (not strong), compote of dried apples and pears, still mineral water.
Children should eat frequently, in small portions 5-6 times a day. The recipe for preparing the recommended products is boiled, stewed or baked; the dishes should initially be liquid or pureed. After recovery, a hypoallergenic diet must be followed for a year, then, with the doctor’s permission, foods that were banned should be gradually, one at a time, introduced. A gap of several days (5-7) should be maintained between the introduction of new foods to the child’s diet.
Classification [edit | edit code ]
According to forms [edit | edit code]
- cutaneous and skin-articular:
- simple
- necrotic
- with cold urticaria and swelling
- abdominal and cutaneous-abdominal
- renal and cutaneous-renal
- mixed
Downstream [edit | edit code]
- fulminant course (often develops in children under 5 years of age)
- acute course (resolved within 1 month)
- subacute (allowed up to three months)
- prolonged (allowed up to six months)
- chronic.
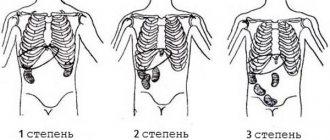
By degree of activity [edit | edit code]
- I degree of activity - the condition is satisfactory, body temperature is normal or subfebrile, skin rashes are not abundant, all other manifestations are absent, ESR is increased to 20 millimeters per hour.
- II degree of activity - a state of moderate severity, severe skin syndrome, body temperature rises above 38 degrees (fever), severe intoxication syndrome (headache, weakness, myalgia), severe articular syndrome, moderate abdominal and urinary syndrome. In the blood, the number of leukocytes, neutrophils, eosinophils is increased, ESR will be increased to 20-40 millimeters per hour, albumin content decreases, dysproteinemia.
- III degree of activity - the condition will be severe, symptoms of intoxication are pronounced (high fever, headache, weakness, myalgia). Skin syndrome, articular, abdominal (paroxysmal abdominal pain, vomiting, mixed with blood), severe nephritic syndrome will be expressed, and there may be damage to the central nervous system and peripheral nervous system. In the blood there is a pronounced increase in leukocytes, an increase in neutrophils, an increase in ESR above 40 millimeters per hour, there may be anemia, a decrease in platelets.
What complications may occur in pediatric patients?
In children, hemorrhagic vasculitis usually resolves safely and without any consequences. But if the disease is severe, then complications are possible.
The latter include:
- Intestinal rupture and development of peritonitis;
- Violation (intussusception) of intestinal loops;
- Bleeding in the gastrointestinal tract;
- Acute anemia, as a result of blood loss.
The diagram shows intussusception with one loop bending inside the other, while the inner loop is compressed, which leads to its gangrene
Complications of systemic vasculitis
https://www.youtube.com/watch?v=Hi1z7T-BZFc
If treatment of hemorrhagic vasculitis is not carried out in a timely manner, then negative consequences are possible. Everyone should know about them. The following complications are possible with Henoch-Schönlein disease:
- renal failure;
- bleeding in the brain (hemorrhagic stroke);
- epileptiform seizures;
- pneumonia;
- pulmonary hemorrhage;
- hemorrhage into the endocardium;
- inflammation of the pericardial sac;
- myocarditis;
- meningitis;
- peritonitis;
- persistent joint deformation;
- massive bleeding;
- collapse;
- necrosis and perforation of the intestinal wall;
- intussusception;
- intestinal obstruction.
An experienced attending physician knows what this pathology can lead to. The greatest danger to children and adults is damage to the kidneys and blood vessels of the brain. This can cause uremia and stroke. The prognosis is relatively unfavorable.
Causes
Doctors cannot say for sure why hemorrhagic vasculitis appears in children, since the causes of the disease have not been established. It is assumed that there is some connection between various bacterial agents, for example, streptococci and staphylococci, and the development of pathology. In addition, it has been noted that children suffering from allergies are more susceptible to developing this pathology. And such a disease can become a reaction of the body to preventive vaccinations.
The cause of the development of the disease in a child can also be helminthiasis, due to which the body is sensitized to toxins, proteins and metabolites.
In addition, very often sick children have foci of chronic infection, such as untreated caries, tonsillitis, and sinusitis. But experts cannot claim that these lesions provoked the body’s immune reaction.
One of the main factors in the development of pathology is considered to be a hereditary factor. It has been established that in families where one of the relatives has this disease, the likelihood of it developing in a child increases significantly.
Recovery after treatment
Children who have had hemorrhagic vasculitis require a long recovery period. Parents of children need to completely change their lifestyle: daily routine, nutrition, habits and behavior. It is very important to be able to prevent the development of infectious diseases. Avoid taking antibacterial and other medications that can cause allergic reactions during treatment. Every day you need to work on strengthening your immune system. To do this, take daily walks in the fresh air, take vitamin complexes, and use products with immunomodulatory properties. It is necessary that the child is protected from contact with infected people. The apartment should be constantly wet cleaned and systematically aired. The child must know about his condition in order to behave correctly. It is very important to find a suitable activity for him that would limit active actions, but at the same time be exciting and interesting.
Forms of the disease
This or that form of the disease (previously we described the forms of the disease) will depend on where exactly the pathology is localized.
Highlight:
- Skin form;
- Articular shape;
- Abdominal form;
- Kidney form;
- Mixed form.
For convenience, we have combined all forms of hemorrhagic vasculitis and their manifestations into a small table.
| Form of hemorrhagic vasculitis | Clinical manifestations and features |
| Skin | 1. Rashes on the surface of the skin, which begin with a dense small nodule (the nodule becomes pale after pressure). |
| 2.The color of the rash becomes purple (stops changing color after pressing). | |
| 3. The rash is localized in the lower and upper extremities, on the buttocks, on the stomach, palms (may be absent on the torso itself). | |
| 4.Darkening and disappearance of the rash after a few days. | |
| 5. Some patients experience itching and swelling of the lips, eyelids, feet and perineum. | |
| Articular | 1. The appearance of symmetrical swelling in large joint groups. |
| 2.Change in the formation of joints. | |
| 3. Deterioration in health, increase in temperature. | |
| 4. Reversible nature of the lesions and restoration of motor functionality. | |
| Abdominal | 1. Contractions and pain in the abdomen. |
| 2. The appearance of a rash (simultaneously with pain or a day later). | |
| 3. Moderate pain. | |
| 4. Imitation of acute appendicitis | |
| 5. Pain accompanied by nausea. | |
| 6. Gastrointestinal bleeding is possible. | |
| 7. Disappearance of pain after three to four days. | |
| Renal | 1. Clinical picture – acute glomerulonephritis. |
| 2.Weakness. | |
| 3. Fever. | |
| 4.Red blood cells and protein appear in the urine. | |
| 5.Increased blood cholesterol levels (not in all cases). | |
| 6.Risk of developing kidney failure. | |
| Mixed | Depending on the combination of one form or another, a different clinical picture may be observed. |
Hemovasculitis in children can develop with certain characteristics. Skin symptoms are observed only in half of the cases.
Other features include:
- The first signs of vasculitis are joint lesions and gastrointestinal lesions;
- Renal dysfunction is quite rare;
- The most favorable prognosis for most cases.
In addition to the renal form, cerebral and pulmonary forms are extremely rare in children. They are detected only by analyzing the volume of red blood cells and proteins in urine and other body fluids.
The pulmonary form is also diagnosed if the child has a cough with sputum and shortness of breath. The cerebral form of vasculitis is characterized by pain and cramps. The appearance of the latter strongly resembles the symptoms of viral meningitis.
Treatment [edit | edit code ]
First, you need a diet (allergenic foods are excluded). Secondly, strict bed rest. Thirdly, drug therapy (antiplatelet agents, anticoagulants, corticosteroids, immunosuppressants - azathioprine, as well as antithrombotic therapy). The following drugs are used:
- disaggregants - chimes 2-4 milligrams/kilogram per day, trental intravenous drip.
- heparin in a dosage of 200-700 units per kilogram of body weight per day subcutaneously or intravenously 4 times a day, gradually withdrawn with a decrease in the single dose.
- activators of fibrinolysis - nicotinic acid.
- In severe cases, plasmapheresis or glucocorticosteroid therapy is prescribed.
- In exceptional cases, cytostatics such as Azathioprine or Cyclophosphamide are used.
In general, the course of the disease is favorable, and immunosuppressive or cytostatic therapy is rarely used (for example, in the development of autoimmune nephritis).
Children must be registered at a dispensary. Conducted over 2 years. For the first 6 months, the patient visits the doctor monthly, then once every 3 months, then once every 6 months. Prevention is carried out by sanitation of foci of chronic infection. Regularly examine stool for helminth eggs. Such children are contraindicated in sports, various physical procedures and exposure to the sun.
Acute and chronic vascular diseases are encountered in the practice of specialists somewhat less frequently than cardiac problems. Within the framework of the international classifier (ICD-10), both groups of disorders are in a single complex within one section, therefore in many cases there is a clear connection between the diagnoses.
Hemorrhagic vasculitis is an acute autoimmune disease with the formation of severe skin rash, damage to the joints, digestive tract and kidneys. The essence is inflammation of blood vessels. More precisely, capillaries and small structures that provide nutrition to these tissues.
Prevention methods
In order to prevent the development of relapse of hemorrhagic vasculitis, you should limit active sports, heavy physical activity, you should not get carried away with vaccinations and physiotherapy, it is recommended to reduce the time spent in the sun (tanning is not recommended). You should also completely eliminate allergenic foods from your diet.
Prevention of hemorrhagic vasculitis is based on reducing the level of blood clotting. For this, heparin, aspirin, trental, nicotinic acid injections, and chimes are prescribed. But preventive measures using pharmaceuticals should be prescribed by the attending physician and carried out under medical supervision. Sometimes a blood transfusion of its components, as well as plasmapheresis, is prescribed.
Development mechanism
Doctors cannot yet say exactly why and how the deviation is formed. This is due to the complex and multifaceted complex underlying the genesis of the disorder.
However, the theory of hypersensitization of the body remains prevalent.
As a result of exposure to unfavorable external factors, the body is mobilized, the intensity of the defenses and the immune system increases sharply. Biological existence depends on it.
Man inherited such activity from his distant ancestors. Typically, such unfavorable external factors are pathogenic microorganisms, viruses or allergens.
In the first case, it is possible to transfer the infectious process. The second refers, among other things, to weak immune responses. Up to simple urticaria.
At the end of the course of the disorder, the body maintains a state of “increased combat readiness.”
At a certain point a failure occurs. A false immune response begins. The body's own tissues suffer: small vessels. In particular, venules and capillaries.
In this regard, hemorrhagic vasculitis is no different from other autoimmune pathologies such as Crohn's disease or rheumatoid arthritis. Only the localization is different.
The defense system produces special antibodies to its own cells. They are observed to form complexes that settle on tissues and cause destruction.
The result is inflammation of varying severity. The clinical picture varies and depends on the strength of the response and the characteristics of the patient’s body.
The inflammatory process is of aseptic origin and is not accompanied by bacterial or viral damage, but this does not make it any less dangerous.
In the absence of therapy, the next stage is the development of complications that crown the general mechanism (see below).
Disease prevention
After treatment, the child must be regularly monitored by a doctor for 5 years. If the kidneys are damaged by hemorrhagic vasculitis, the doctor may increase the observation period. A urine test should be taken regularly so as not to miss signs of a new manifestation of the disease. To prevent the disease, the following conditions must be met:
- Foci of infection must be detected in time.
- All infectious pathologies must be treated completely.
- Hypothermia should absolutely not be allowed.
- Limit prescribing and taking unnecessary medications.
- Do not allow foci of chronic infection to worsen.
After treatment of hemorrhagic vasculitis, children should not be vaccinated for 2 years. This condition is mandatory and cannot be neglected.
Etiology [edit | edit code ]
In the majority of patients (66-80%), the development of the disease is preceded by an upper respiratory tract infection [6], vaccinations (no source, no evidence)
The manifestation of the disease after typhus, paratyphoid A and B, measles, and yellow fever has been described [7].
Other potential starting agents of the disease may be [8]:
- medications (penicillin, ampicillin, erythromycin, quinidine, enalapril, lisinopril, chlorpromazine)
- food allergy
- insect bites
- hypothermia
Sometimes hemorrhagic vasculitis complicates the development of pregnancy, periodic illness, diabetic nephropathy, liver cirrhosis, and malignant neoplasms [8].
What are the causes of the disease?
Diagram of the affected vessel
Pathology represents inflammatory processes in the walls of small vessels. At the same time, the destruction of the latter occurs.
Microscopic blood clots form inside the vessels. Because of this, circulatory problems occur, and blood partially stops flowing to some organs.
The inflamed wall ceases to prevent the release of plasma and red blood cells. Skin rashes appear. Bleeding is observed in these rashes. The causes of hemorrhagic vasculitis in childhood are not fully understood.
This is because they are not explicit. In recent years, experts have established a direct connection with viral and bacterial infections.
Among the latest:
- Influenza and other acute respiratory viral diseases;
- Chickenpox;
- Scarlet fever;
- Measles;
- Angina.
IMPORTANT: The disease affects children's skin, joints, and kidney tissue. The functioning of the immune system is disrupted, and the disturbances are expressed in the fact that the body begins to produce antibodies to its own cells
Another significant factor that can become a catalyst for hemorrhagic vasculitis is helminths of various types. They can cause the main symptoms simultaneously with an allergic reaction.
If a sick child has tuberculosis intoxication, then one of the consequences may be the formation of capillary-toxic protein complexes.
There are several established provoking factors:
- Sudden changes in ambient temperature;
- Hypothermia of the body;
- Side effects from taking certain medications;
- Intolerance to the components of medications taken;
- Food or household allergic reaction;
- Vaccinations.
Causes and provoking factors
The main cause of vasculitis is the presence of immune complexes in the blood. They are a “lump” of antigens and antibodies. In a healthy body, their number is controlled by the phagocytic system. But with an excess of foreign substances (antigens), there are too many of them and it does not have time to remove them. This leads to their settling on the inner wall of the vessels, followed by inflammation of this place.
The main provoking factor of allergic purpura is diseases of the throat and lungs: acute respiratory infections, ARVI, sore throat and others.
Another group of provoking factors is an allergic reaction to foods, medications, vaccinations, insect bites, and household chemicals.
Manifestations of hemorrhagic vasculitis can be divided into 2 groups: general and specific. The first includes an increase in temperature to 38-40°C, intoxication, lack of appetite, and weakness.
The second group includes:
- rash;
- articular, abdominal, renal syndromes;
- damage to the lungs and nervous system.
Characteristic rashes are the main sign that the vessels are affected by vasculitis. The rash consists of many rust-colored dots. Each of them has the shape of a circle with a diameter of 2 millimeters and rises above the surface of the skin. They can unite with each other and form large spots, up to the absence of healthy areas between them. It appears mainly on the skin of the lower leg (the part of the leg below the knee). If untreated, it gradually rises upward, covering the thighs, buttocks and lower back.
Joint syndrome in 70-90% of cases appears simultaneously with rashes and causes pain in the knee, ankle and other joints, as well as in the muscles adjacent to them.
With abdominal syndrome, the digestive organs are affected and symptoms characteristic of gastrointestinal diseases appear: nausea, vomiting, diarrhea, gastrointestinal bleeding. It is also possible for holes to appear in the intestinal walls or peritonitis.
With renal syndrome, the functioning of the kidneys is impaired. It appears in the third week of disease development, i.e. after other manifestations of vasculitis. Kidney damage manifests itself in the appearance of various proteins in the urine.
In very rare cases, the disease affects the blood vessels of the lungs and brain. In the first case, it is expressed by bleeding and hemorrhages into the walls of the organ.
In the second - severe headaches and can cause encephalopathy, polyneuropathy, seizures, changes in behavior and heart attack.
Vasculitis is treated by 2 specialists: a therapist and a rheumatologist. If abdominal and renal syndromes appear, additional consultation with a gastroenterologist and nephrologist may be required.
In order to cure the disease, the doctor uses 2 methods: a hypoallergenic diet and medications. In the first case, the goal is to reduce the number of allergens entering the body. Ideally, it is recommended to switch to a diet for patients with stomach ulcers - table No. 1. But a temporary refusal of oranges, chocolate, tea, coffee, salty and spicy foods is also effective.
In the second case, drugs reduce symptoms and slow down pathological processes. These include:
- Ticlopidine, Dipyridamole - prevent the formation of blood clots.
- Nicotinic acid stimulates the process of dissolution of fibrin formations and blood clots.
- Heparin - reduces blood clotting.
- Dexamethasone, Prednisolone - regulate the functioning of the immune system.
- Antibiotics – to treat secondary bacterial infections.
The duration of treatment ranges from 2 months to a year, depending on the severity. If it was started on time, then the likelihood of complications is very low.
Hemorrhagic vasculitis is a disease that affects the walls of capillaries and small vessels. The ICD-10 code assigned to it is D69.0. It occurs due to overworking of the immune system. The main symptom is a specific rust-colored rash caused by subcutaneous hemorrhages. It also manifests itself as a violation of the integrity of the digestive organs and kidney function.
Read also: Hemorrhagic vasculitis urolithiasis
In order not to provoke hemorrhagic vasculitis, the main condition is adherence to a balanced diet, timely medical examination and testing.
What diseases should be excluded when diagnosing hemovasculitis?
The differential diagnosis of hemorrhagic vasculitis in a child is carried out with other diseases that occur with hemorrhagic, renal or articular symptoms.
It is extremely important to exclude:
- Meningitis;
- Septic endocarditis.
- Systemic lupus erythematosus.
The first two diseases are infectious diseases, during which hemorrhagic puncture is observed. Lupus is a systemic rheumatic disease that is accompanied by skin manifestations similar to vasculitis.
The diagnosis should exclude the presence of tumors, thrombocytopenia with purpura, hepatitis A, B, C and D. It is very important to pay attention to blood diseases. Of particular importance are diseases during which an increase in lymphatic growth is possible
Forms of vasculitis and symptoms
In children, systemic vasculitis is observed much less frequently, but manifests itself more actively than in adults. Each of the above types of vascular inflammation has its own clinical picture and specific signs inherent only to it.
Common symptoms of childhood vasculitis include:
- deformation of vascular walls;
- pain in muscles and joints;
- temperature increase;
- dysproteinemia (violation of the normal ratio between protein fractions in the blood);
- increase in ESR.
With timely and competent treatment, in 80% of children the signs of vasculitis disappear after 1–1.5 months, and in only 20% the disease becomes chronic.
Cutaneous purpura
The most common type of vasculitis in young patients. It has several subtypes and occurs in approximately every third child aged from six months to 18 years. The highest incidence in children occurs between 2 and 8 years of age. Skin purpura affects boys twice as often as girls.
This type of vasculitis, as a rule, occurs after severe ENT diseases of a staphylococcal nature and is manifested by multiple hemorrhagic rashes in the thighs and buttocks. In young children, erythema spots are accompanied by itching and skin irritation.
Other signs of hemorrhagic vasculitis in a child:
- lethargy, whims, crying without reason;
- refusal of food;
- headache;
- persistent increase in temperature to 37.2–38.0 °C.
In severe cases, blisters with traces of blood form on the surface of the erythema, and tissue necrosis is possible.
With a benign course of vasculitis, hemorrhages change color and shape after 3–4 days and gradually disappear.
Cutaneous rheumatoid form of vasculitis in children
This type of vasculitis is often accompanied by damage to vital organs and tissues. In the rheumatoid form of inflammation, skin symptoms are combined with damage to large joints - knees, elbows, ankles. Hemorrhagic hemorrhages are localized around these joints.
Cutaneous rheumatoid vasculitis in a child can be recognized by the following signs:
- pronounced pain in one or more joints;
- swelling and redness of the skin in the area of the inflamed joints;
- mild paresis of the lower extremities is possible;
- numbness and tingling in the toes.
The rheumatoid type is considered one of the most complex vasculitis in young children and requires urgent and competent treatment.
Cutaneous-abdominal form of vasculitis in children
It manifests itself as a hemorrhagic rash in the lower extremities and damage to the abdominal aorta. This form of vasculitis in a child can be recognized by the accompanying symptoms:
- intestinal colic;
- sharp pain in the navel area, aggravated by palpation;
- flatulence and bloating;
- nausea, vomiting with blood;
- diarrhea;
- functional intestinal obstruction is possible.
Cramping abdominal pain is very similar to an attack of cholecystitis or appendicitis, which often leads to confusion in diagnoses and incorrect treatment.
Renal form of vasculitis in children
This type of childhood vasculitis is much less common than previous forms. The pathology, better known as Henoch-Schönlein syndrome, develops 30–45 days after the onset of vascular inflammation.
Characteristic signs of the disease:
- changes in the amount, composition and structure of urine;
- pallor and swelling of the skin;
- short-term increase in blood pressure;
- presence of blood in urine.
Unlike other forms of vasculitis, in children the renal variety rarely produces accompanying symptoms on the skin, which significantly complicates the process of diagnosis and subsequent therapy.
Pulmonary form of vasculitis in children
Lung damage is characterized by the appearance of necrotizing granulomas, which, when disintegrating, form large cavities. In 20% of young children, the disease occurs without visible symptoms - with no cough, shortness of breath, or hemoptysis.
However, upon examination, half of the patients are found to have a violation of the pulmonary vascular pattern, the presence of nodules and infiltrates.
Allergic form of vasculitis in children
Allergic vasculitis in children affects small arteries located in the outer layer of the skin. Accompanied by various forms of skin rashes, often resembling urticaria, eczema or dermatosis. This creates certain difficulties during diagnosis and requires a differentiated approach.
The culprits of allergic vasculitis at an early age can be a variety of factors: infectious diseases, medications, food, dust, pollen, chemicals, frequent colds.
Signs of an allergic form of vasculitis:
- itchy and painful rash;
- general malaise;
- low temperature;
- lack of appetite.
Skin rashes in children can be localized anywhere - on the legs, arms, face and body. With severe vasculitis, blisters with hemorrhagic contents and the formation of ulcers with a necrotic rim may appear.