Retrocerebellar cyst of the brain is a benign tumor. A pathological neoplasm in the head is a bubble filled with fluid. It can form in any part of the brain where necrosis of the gray matter develops against the background of exposure to provoking factors.
Delayed diagnosis and therapy can cause the destruction of neurons and the development of dangerous neurological disorders. Therefore, you need to know what a retrocerebellar cyst in the brain is and what size is dangerous for humans.
Types of cysts
The nature of brain cysts does not skimp on variety, but most often medicine encounters the following types:
- A retrocerebellar cyst of the brain is a cavity filled with brain fluid. The breeding ground for the development of such a cyst is the diseased part of the brain. Its destroyed cells provoke the growth of the disease.
- An arachnoid cyst of the brain usually occupies a position in the outer meninges. The fluid filling the arachnoid cyst is spinal fluid. The patient may be a carrier of this atheroma from birth, or may acquire it over time.
Arachnoid cysts are usually asymptomatic, and many of these cysts are discovered incidentally on CT and MRI scans of the brain.
- A choroid plexus cyst is a pathology of the fetus in the seventh month of pregnancy. The nature of this atheroma is benign, and after some time it simply disappears.
- Pineal cyst. Its birthplace is the pineal gland, but this pathology is rare. It causes problems with coordination of movements and vision of the patient.
Main symptoms of retrocerebellar arachnoid cyst
There are often cases of asymptomatic disease, when the patient is diagnosed by chance, during examinations for the presence of other diseases. This type of tumor grows slowly, imperceptibly, sometimes over a long period of life. In some cases, an arachnoid cyst may freeze, without changing its size, and without manifesting itself in any way. The manifestation of cyst symptoms is associated with disturbances in the functioning of the nervous system.
The first symptom of an arachnoid cyst is a headache (migraine), often with a pronounced localization (in a certain place on the head). Nausea may be added to it, as a result of which vomiting usually does not occur. You definitely need to pay attention: a person can feel sick almost constantly, regardless of food intake.
The patient's coordination of movements is impaired, his gait changes, and it becomes more difficult to maintain balance. A cyst in the brain can affect the parts responsible for the functioning of the sensory organs. As a result, vision clarity (blurred picture), hearing acuity, and skin sensitivity may decrease. There are known cases of deterioration in visual acuity or loss of vision in only one eye, twitching of the eyeballs (nystagmus).
The disease may also affect the function of the limbs. You should pay attention to the appearance of paresis, paralysis of the arms or legs, and decreased muscle tone.
Arachnoid retrocerebellar cyst affects the nervous system. This affects the performance, well-being, and mental state of the patient. He sleeps poorly, feels constantly tired, weak, and has difficulty thinking quickly and concentrating. His mood often changes, irritability or, conversely, an apathetic state appears. Attacks of severe dizziness may begin, including loss of consciousness. Hallucinations are possible. An inferior retrocerebellar cyst often manifests itself as a disturbance in orientation in space and time.
Retrocerebellar cyst: types
The retrocerebellar cyst has its own divisions.
Retrocerebellar arachnoid cyst of the brain
This atheroma is located between the membranes of the brain, its cavity is filled with cerebrospinal fluid. Appears for various reasons:
- mechanical damage to the head;
- inflammation of the brain;
- high pressure in arachnoid atheroma;
Retrocerebellar cerebrospinal fluid cyst
This tumor is also filled with fluid. Causes of the disease:
- mechanical damage to the head;
- the patient suffered a stroke;
- the process of inflammation in the brain;
- undergone surgery.
In addition, the cerebrospinal fluid cyst is divided by origin:
- illness from birth resulting from abnormalities in the development of the child in the prenatal period;
- an acquired disease resulting from a head injury or some kind of inflammation.
Main consequences and complications
Why is an intracerebral cyst dangerous? In childhood, a pathological formation can provoke hypermobility or delayed physical and mental development of the child. In adult patients, a retrocerebellar cyst provokes an increase in pressure on the gray matter, causing the following consequences:
- focal disorders. Enlarged brain cysts lead to the development of speech, vision, motor function disorders, and hearing loss. Specific symptoms develop according to the affected area in which the tumor is localized;
- cerebral syndrome. Patients complain of increased blood pressure and headaches of varying intensity. The cause of the development of the syndrome is operations performed in the brain area;
- development of convulsive syndrome. Characterized by the development of seizures and epilepsy. Convulsive readiness is a characteristic sign of a congenital cyst;
- neurotic manifestations. Patients note the development of weakness, unbearable headaches that cannot be relieved by conventional analgesics, and decreased immunity.
The most dangerous complication of a retrocerebellar cyst in the head is rupture, which leads to complicated sepsis, extensive hemorrhage, and death of the patient.
Specifics
Despite the fact that a retrocerebellar arachnoid cyst of the brain is known as a benign tumor, it is dangerous because it can provoke a more serious illness.
The specificity of this type of cyst is its ability to grow. In case of advanced disease, atheroma can have a destructive effect on brain tissue.
Retrocerebellar cysts also occur from birth, but they can also be of a hidden nature, not manifesting themselves for some time. However, under the influence of any factors, the cyst begins to grow in size, impairing blood circulation in the brain and its functions.
Possible complications
After treatment of a brain cyst, the patient needs a long recovery period. If treatment is carried out incorrectly or not, the disease is dangerous due to the possible development of the following complications:
- Very severe headaches;
- convulsive syndrome;
- a decrease in visual and hearing acuity, up to blindness and deafness, associated with the growth of a neoplasm;
- sepsis;
- cerebral hemorrhage;
- rupture of a tumor with damage to brain tissue.
All this suggests that it is necessary to carry out preventive measures in a timely manner, and if you suspect a pathology and feel unwell, immediately seek medical help. If the disease is detected early, a person has a chance to be completely cured. Otherwise, the consequences may become irreversible and lead to death.
Causes of pathology
The most common reasons include the following:
- mechanical effects on the brain (concussion, bruise);
- genetic deviations from the norm when the brain is devoid of partitions;
- hemorrhage as a consequence of surgery;
- infectious diseases affecting the central nervous system (encephalitis, meningitis, etc.);
- poor ecological state of the environment as a negative factor affecting the development of the embryo.
- use by the mother during pregnancy of drugs dangerous to the fetus;
- ischemic cerebral disease.
Causes
This type of cyst can appear without any obvious reason. This makes it much more difficult to identify. There are quite a few factors that can trigger its development. These include:
- Circulatory disorders;
- Head injuries, concussions;
- Inflammatory diseases caused by infectious exposure;
- Serious negative brain changes;
- Performed brain surgeries;
- Previous stroke;
- Heredity;
- Birth injuries, negative effects on the fetus of medications taken by the mother during pregnancy.
All people affected by the problems listed above are at risk. The increased likelihood of cyst formation requires observation by a doctor. You need to visit him at least once a year to exclude unexpected development of the disease.
Symptoms
The symptoms of a retrocerebellar cyst of the brain are similar to those of other diseases. Sometimes the disease is asymptomatic, and then it is very difficult to diagnose it.
Symptoms are determined by the size and position of the tumor. The larger it is, the more active the manifestation of its presence.
The growth of atheroma is stimulated by poor blood supply, multiple sclerosis, and infectious diseases.
The main symptoms of a retrocerebellar cyst of the brain:
- A depressed mental state, expressed in feelings of indifference to everything and hopelessness. This condition is accompanied by insomnia, as well as problems with concentration and mental activity.
- Headache, often migraine-like with aura. While the atheroma is small, headache is often the only sign of the disease. As the cyst enlarges, the pain intensifies.
- Balance imbalance caused by a malfunction of the vestibular apparatus, the appearance of dizziness.
- Deterioration in the functioning of the organs of hearing and vision.
- Paralysis is temporary, turning into permanent, affecting some part of the body or the entire body.
- A symptom of hydrocephalus (dropsy), in which the brain experiences severe pressure.
Symptoms of the disease in children
The presence of this pathology in a child can lead to serious consequences. The larger the brain tumor, the more severely the baby suffers the pathological symptoms. It is especially worth noting small and infant children, whose brain functions are in their infancy and active development.
The clinical picture includes the following signs of pathology:
- Hearing disorders.
- Numbness of arms and legs.
- Paresis and paralysis of the upper and lower extremities may occur; they can be complete or partial.
- Coordination of movements may be severely impaired.
If the cyst grows rapidly, then intracranial pressure increases. This condition, in turn, is accompanied by characteristic symptoms:
- Severe persistent headaches that are difficult to relieve.
- Nausea.
- Vomit.
- An infant has bulging and pulsation of the large fontanel. He becomes moody.
- The baby is sleepy.
- General weakness, fatigue.
In severe cases of the disease in infants, there is a divergence of the sutures of the skull, and the large fontanelle heals poorly or does not heal at all. All this leaves its mark. The child's development is disrupted. There is a lag in both physical, mental and mental development.
Diagnostics
To detect a cyst, there is a special diagnosis:
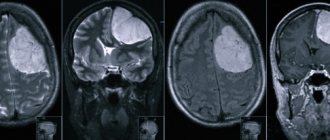
- Magnetic resonance imaging is the most commonly used. It provides fairly accurate data and a complete description of the current state of the disease.
- Doppler ultrasound scanning is used as an additional diagnostic method . It allows you to identify more detailed information about the tumor.
- Diagnosis through blood pressure monitoring. To determine the nature of the formation (tumor or cyst), a contrast agent is injected, to which the brain tissue reacts.
In addition to the above diagnostic methods, ECG and computed tomography are used.
Diagnostic measures
Making a diagnosis is one of the most important components of tumor therapy. If done incorrectly, there is a high probability of death. Thus, in the case when an oncological tumor is confused with a similar cyst, a surgical operation may be prescribed, which in no case should be done in the event of dangerous tumors.
First, the specialist interviews the patient, drawing up a complete picture of the patient’s clinical symptoms. After this, MRI, CT and ultrasound are mandatory, and ultrasound must be carried out with intravenous administration of contrast agents, which helps determine whether the patient has a benign or malignant tumor. The specialist also prescribes other examinations to reliably determine the cause of the formation of the pathological neoplasm. It is important to do this right away in order to begin treatment and eliminate the negative impact of the root cause of the disease.
Treatment methods
If there are no changes in the volume of the retrocerebellar cyst and manifestations of the disease, no course of treatment is required; you just need to be systematically checked by a neurologist.
Sometimes, when the size of this cyst increases, treatment with medications that can extinguish the infectious and inflammatory processes that cause the formation of the cyst can help.
If symptoms listed above appear, surgery is required immediately. However, before this, the patient undergoes a thorough examination.
It is necessary to determine the causes of the appearance of the tumor and the degree of risk of surgical intervention.
The examination result shows what type of operation is needed in this case.
- Neurosurgical is the most dangerous, since it is carried out through craniotomy. Neurosurgical surgery involves removing the entire tumor and the tissue adjacent to it.
- Brain shunting is used when there is a continuous flow of fluid into the tumor. The bypass method involves using shunts to connect diseased vessels to arteries. This allows fluid to flow normally from the affected areas.
- Endoscopic puncture is the safest method. Through a puncture of the skull, the cyst is removed and the fluid flows out. This method cannot always be used, because the cyst is most often located deep inside the brain.
A patient who has undergone one of these operations must undergo rehabilitation, which normalizes brain function.
About the consequences of the operation
- In the postoperative period, the patient may experience increased blood pressure and frequent headaches.
- If one of the functional parts of the brain has been affected by the disease, then speech, visual, motor and other functions can significantly deteriorate.
- In some cases, the immune system is seriously affected, resulting in malaise and weakness. The reason for this condition is asthenic syndrome.
- One of the complications may be convulsive syndrome, which manifests itself in the patient’s epileptic seizures.
- Problems in behavior and communication may arise.
In the postoperative period, it is necessary to take special vitamins and medications that strengthen blood vessels. You should not neglect your doctor's recommendations . In addition, your lifestyle should be healthy; it is better to give up bad habits. Vigorous sports activities are recommended.
Features of therapy
If a retrocerebellar benign brain tumor does not provoke the development of unpleasant symptoms and does not increase in size, then treatment is not required. It is enough for patients to be observed by a neurologist.
Drug therapy
How to treat a retrocerebellar cyst of the brain? If the tumor grows slowly, conservative therapy may be required, which involves the use of antibiotics and antiviral drugs. Additionally, immunomodulators are prescribed, which increase the body's resistance and help cope with autoimmune pathologies.
For bleeding disorders and elevated cholesterol levels, Aspirin and Pentoxifylline are indicated. Enalapril and Capoten can normalize blood pressure. Anticoagulants will help eliminate adhesions. Nootropics are widely used to restore the supply of glucose and oxygen to the brain.
Surgery
In what cases is it necessary to remove a retrocerebellar cyst of the brain? If the tumor rapidly increases in size, causing severe symptoms, then surgical treatment is required. Before surgical manipulations, it is necessary to carefully examine the patient and eliminate the factors that provoke the appearance of such neoplasms. The tactics and type of operation are determined based on the size and location of the tumor:
- craniotomy. The most traumatic type of surgery, which allows you to completely remove the cyst and surrounding tissue;
- shunting. The method is used when there is a constant flow of fluid into the cyst. Shunting allows you to connect damaged vessels, which helps normalize the outflow of fluid from the cyst;
- endoscopy. This is a modern and least traumatic technique that involves piercing the skull and then removing the formation or suctioning out the fluid. This treatment is rarely used, since the retrocerebellar neoplasm is located deep in the gray matter (unlike an arachnoid cyst of the brain).
After surgery, patients need long-term rehabilitation, which is aimed at restoring normal brain function.
Recommendations
A retrocerebellar arachnoid cyst is a benign tumor; it does not have such a destructive effect on the human body as a cancerous tumor. Nevertheless, the appearance of this atheroma must be responded to immediately.
The symptoms of this disease have a very negative impact on a person’s quality of life, because the growing tumor puts pressure on the adjacent brain tissue.
A frivolous attitude towards the symptoms of this disease can have serious consequences, including death. That is why, if you feel like there is a hint of the presence of a retrocerebellar cyst in the brain, you should immediately consult a doctor and undergo an examination.
If the suspicion is confirmed, then a set of measures is needed, including removal of the cyst and a rehabilitation period. Only in this way can one defeat the disease and return to a full life as a healthy person.
Classification of neoplasms
Tumors, which are usually benign, are classified based on location:
- Liquor retrocerebellar cyst - located deep in the brain, containing liquid exudate. It often appears as a result of damage to the skull and intracranial formations, operations, and cerebral hemorrhage.
- Arachnoid retrocerebellar cerebrospinal fluid cyst - forms more often, in contrast to cerebrospinal fluid cyst. It is formed on the surface of the hemispheres of the main organ of the central nervous system and is filled with cerebrospinal fluid. Most often diagnosed in childhood due to intracranial pressure, inflammation, brain and cranial injuries.
What do arachnoid and retrocerebellar cysts look like?
Treatment options depend on the location of the retrocerebellar cysts. Moreover, the following subtypes of cystic formations are distinguished:
- Congenital (primary) - appears in the fetus during embryogenesis.
- Acquired (secondary) - occurs as a result of damage to brain structures, traumatic brain injury.
Preventive actions
There are no special measures to prevent retrocerebellar cysts. To prevent the intrauterine formation of a neoplasm, the expectant mother should refrain from bad habits and take medications with caution.
To prevent acquired tumors, it is recommended to take the following measures:
- avoid damage to the skull, face and intracranial formations;
- treat infections promptly;
- maintain cholesterol levels;
- diagnose cerebral blood flow disorders in a timely manner.
Despite the fact that a retrocerebellar tumor is a benign formation, when the pathology develops, complications for the health and life of the patient are possible. The appearance of painful symptoms requires a visit to a specialist. The doctor will carry out diagnostic measures and prescribe effective treatment, thanks to which it will be possible to prevent negative consequences and completely recover.
Candidate of Medical Sciences, mammologist-oncologist, surgeon
More articles
Congenital arachnoid cysts can be prevented by correct management of pregnancy and the exclusion of harmful factors to the fetus.
In case of acquired tumors, it is important to promptly treat injuries, vascular inflammation and cerebral disorders.
Treatment
The method of treatment, medicinal or surgical, depends on the severity of the clinical course and localization of the pathological process. Surgery is performed in the following cases:
- Optical-chiasmal type of arachnoiditis.
- Arachnoiditis of the posterior cranial fossa.
- For hydrocephalus, a shunt is performed to create pathways for the outflow of cerebrospinal fluid.
With the help of surgery, it is possible to restore the passage of the cerebrospinal fluid pathways; cysts can be removed and adhesions can be separated. If visual acuity is significantly reduced, electrodes are implanted to stimulate the optic nerves.
Drug therapy:
- Antibacterial therapy directed against a specific infection. Antibiotics of the penicillin group, cephalosporins, etc. are prescribed. They are administered intramuscularly, intravenously, and also into the posterior cervical lymph nodes (endolymphatic route of administration). Chronic foci of infection are sanitized with antibiotics.
- Anti-inflammatory therapy. It consists of prescribing corticosteroids: prednisone, dexamethasone, etc. They are effective in cases of infectious and allergic nature of brain damage.
- Dehydration therapy is carried out to reduce the level of intracranial pressure. Diuretics are prescribed: Diacarb, Mannitol, Furosemide, etc.
- Antiepileptic drugs are prescribed for convulsive syndromes: Finlepsin, Carbamazepine, etc.
- Neuroprotectors and drugs to improve metabolic processes: Actovegin, Piracetam, Mildronate, Iodine preparations, Lidaza, etc.
- Psychiatric drugs: antidepressants, tranquilizers.
- Vasodilator drugs are prescribed to improve cerebral circulation: Cavinton, Vinpocetine, Cerebrolysin, etc.
- Antihistamine therapy: Diazolin, Tavegil, etc.
- Lumbar puncture is performed to reduce intracranial pressure.
- Vitamin therapy is prescribed to increase the internal strength of the body.
- Antioxidant therapy is allowed.
The disease is quite serious. Treatment is carried out in a hospital setting. Treatment with folk remedies in this case is ineffective.
Clinical manifestations of arachnoiditis and its types
Arachnoiditis is classified into several categories.
I. Based on the localization of the pathological process, the following types of disease are distinguished:
- Cerebral arachnoiditis. It has its own subtypes: convexital arachnoiditis, basal arachnoiditis, opto-chiasmal type, arachnoiditis of the posterior cranial fossa.
- Spinal view.
II. According to morphological changes and pathogenesis:
- Adhesive arachnoiditis.
- Adhesive-cystic type.
- Cystic arachnoiditis.
III. With the flow:
- Acute course of the disease.
- Subacute course.
- Chronic course.
The clinical picture of arachnoiditis does not develop immediately. Several months or even a year may pass from the moment of the infectious disease. Post-traumatic cerebral arachnoiditis can appear even after 2 years. The inflammatory process that has begun continuously progresses with alternating periods of exacerbation and remission.
Due to the fact that the disease develops gradually, the manifestation of clinical symptoms is subacute and can become chronic. After the infection enters the arachnoid membrane, after a certain time, symptoms of asthenia and neurasthenia gradually begin to appear: increasing weakness, sleep disturbances, fatigue, increased irritability, emotional instability: outbursts of anger, followed by tearfulness or unexpected joy, fearfulness is noted.
Against the background of such symptoms, epileptic seizures may appear. With subsequent progression of the disease, general cerebral and focal symptoms appear, characteristic of types of cerebral arachnoiditis.
Causes of the disease
Most often, a retrocerebellar tumor is formed due to disturbances in intrauterine development or appears as a result of difficult childbirth. With a congenital anomaly (as well as with an acquired one), instead of healthy tissue, a cavity is formed, filled with cerebrospinal fluid or protein fluid from the serous membranes.
Most often, a retrocerebellar tumor is formed due to disturbances in intrauterine development or appears as a result of difficult childbirth.
Secondary retrocerebellar neoplasm is diagnosed as a result of the following pathologies:
- hemodynamic disturbance;
- damage to the skull and brain structures;
- brain surgery;
- infections, inflammations.
Types of arachnoid cysts of the brain and stages of disease development
Depending on the structural features (morphological feature), the formations in question are:
- Simple . The cyst is lined with cells that can actively produce cerebrospinal fluid.
- Complex . A cystic neoplasm consists of various types of tissue: neuroglia, ependyma, etc.
According to the nature of origin (etiological sign), as mentioned above, arachnoid cysts are divided into:
- Primary . They are inherently defects in the structure of the brain.
- Secondary . They occur against the background of certain phenomena: trauma (including during surgery), bleeding, inflammation. In addition, the cause of such a cyst can be birth trauma, as well as difficult childbirth, as a result of which the baby subsequently develops oxygen starvation of the brain.
Based on the clinical picture, the cysts in question are divided into:
- Progressive. Over time, they increase in parameters, provoking neurological complaints from the patient.
- Frozen . Such formations do not grow and do not manifest themselves in any way.
Risk factors
Often, an arachnoid cerebrospinal fluid cyst is present completely asymptomatically. Its symptoms are pronounced only in every fifth case. The main factors influencing the growth of education are:
- Inflammatory process (such as a virus, cystic arachnoiditis, or infectious lesion);
- An increase in the size of the formation can occur due to an increase in the pressure of the fluid inside it;
- Trauma or any other condition of the brain that results in arachnoid changes. In this case, the formation of optochiasmal arachnoiditis occurs.
Important! What is arachnoiditis can be defined as an inflammatory formation that precedes the formation of a cyst in the arachnoid region of the brain.
About prevention
In most cases of detection of a cerebrospinal fluid cyst in a person, the prognosis of doctors is positive. Of course, to fulfill this prognosis, a benign course of the disease and its treatment are necessary. With a successful operation and a good recovery period, the patient recovers completely.
Modern medicine has not invented any special prevention for these types of cysts. We are talking about following the general rules of maintaining your health at the proper level, basic attentiveness to your own body. In order to avoid congenital pathologies, you must carefully monitor your health during pregnancy and consult a doctor if you feel unwell.
It is advisable to eliminate bad habits forever. You also need to get rid of other bad habits: eating unhealthy food, leading a sedentary lifestyle. In the modern world, fast food is actively imposed, but at the same time there is a choice and a lot of alternatives. Choose as healthy habits as possible for yourself and your loved ones.
There are no preventive measures to prevent the formation of a retrocerebellar cyst. In this case, the medical history is important: from birth or acquired during life.
If atheroma is acquired from birth and there is no growth trend in its volume, then no special measures are needed.
For prevention in this situation, a neck massage may be indicated or medications may be prescribed for good vascular tone.
When the formation of a cyst is due to some external reasons, then preventive measures are taken taking into account these reasons.
Treatment of arachnoiditis
Inflammation of the meninges is treated comprehensively. It is necessary to first establish the cause of the disease to clarify the use of appropriate remedies. In addition, medications are used that enhance the immune system and ensure the absorption of fluid.
Traditional
Treatment of brain arachnoiditis is carried out with antibacterial agents: for purulent tonsillitis, sinusitis or otitis. For allergies - drugs that reduce sensitivity and remove the consequences. Absorbable drugs and diuretics are used to reduce hypertension. Medicines are used against seizures, as well as substances that improve metabolism.
Folk
It is impossible to cure cerebral arachnoiditis using traditional methods of therapy. Tinctures and decoctions can be used as an additional remedy for conservative treatment. However, it is practically impossible to recover using only traditional methods.
Prevention
In order to prevent it, it is necessary to promptly treat foci of infectious processes in the body (caries, sinusitis), treat acute inflammatory diseases, and monitor the condition of brain structures after injuries.
Possible pathologies ↑
Common pathologies of the spinal cord membranes include:
- infectious inflammatory diseases - meningitis, arachnoiditis, neurosyphilis;
- developmental defects;
- damage;
- tumors;
- parasitic diseases.
Developmental defects
Among anomalies in the development of the integument, a special place is occupied by spina bifida and spina bifida, which can cause serious complications.
As a result, the spinal cord with its covering, nerves, and cerebrospinal fluid can be located directly under the skin.
More often, hernias are localized in the lumbosacral region. Sizes can reach gigantic sizes.
Photo: congenital pathology of the spinal cord - spina bifida
The most typical symptoms are dysfunction of the pelvic organs, combined with weakness in the legs and impaired sensitivity.
Inflammation
Meningitis is accompanied by dilation of blood vessels, edema, compression of elements in the spinal canal and impaired fluid dynamics.
Compression of the posterior roots is accompanied by sensitivity disorders, compression of the anterior ones is accompanied by muscle cramps or paralysis.
The lesions are segmental in nature and depend on the location of the pathological process.
Damage
Spinal cord injury is the most dangerous type of spinal injury and is observed in 10–15% of injured people.
Most of the survivors become disabled with serious disorders of movement, bladder function, and pain that persist for many years or for life.
During trauma, like brain injuries, the underlying substance and membranes can be damaged.
Due to significant crushing of brain tissue and rupture of its blood vessels. blood may enter the subarachnoid space and subarachnoid hemorrhage occurs.
The same mechanism underlies the more rare intracerebral hemorrhages.
Fig.: damage to the spinal cord and its consequences
Meningeal hematomas are of particular importance in case of brain injury:
- epidural - between the bone and the hard shell;
- subdural - between the brain and the above integuments.
Tumors
Tumors of the meninges:
- from meningothelial cells;
- mesenchymal non-meningothelial neoplasms;
- melanocytic neoplasms of the membranes.
Tumors formed outside the spinal cord include:
- arachnoidendothelioma formed from the meninges;
- neuromas formed predominantly from Schwann cells occur with approximately the same frequency as meningiomas;
- hemangioblastoma is a highly vascularized tumor;
- lipomas are usually combined with spina bifida or other developmental anomalies.
Photo: hemangioblastoma
The last two types of tumors are relatively rare.
Neoplasms dramatically disrupt the function of the spinal cord:
- compress or destroy, growing into its substance;
- reduce the space in the spinal canal, which disrupts blood and cerebrospinal fluid flow;
- there is an increase in the block of the subarachnoid space - the progression of the tumor, at its location, the flow of cerebrospinal fluid completely stops.
Transverse brain lesion syndrome is the result of its compression and irreversible degenerative changes.
During the clinical course of tumors, certain stages can be distinguished:
- radicular stage - the appearance of pain and paresthesia, first unilateral, then bilateral or encircling;
- compression of half the brain (Brown-Séquard) - on the sore side below the tumor, deep sensitivity is impaired and paresis develops, and on the healthy side, superficial sensitivity is impaired;
- complete compression - lower para- or tetraplegia (paralysis in the legs or all extremities, depending on the level of damage), bilateral sensory impairment, dysfunction of the bladder.
Diagnostic methods
Due to the fact that arachnoid changes are usually asymptomatic, diagnosis is carried out only when one or more alarming signs appear.
Usually the doctor prescribes several procedures:
- MRI or CT. They allow you to prove the presence of a cyst, determine its size and location.
- Angiography using a contrast agent. Proves or disproves the presence of cancer cells.
- Blood test for infectious diseases.
- Cholesterol level analysis.
- Dopplerography. This is the study of the patency of blood vessels. Shows whether there are any disturbances in the blood circulation process.
- Electrocardiogram and ultrasound of the heart. Irregularities in the functioning of the heart can provoke deterioration of blood circulation in the brain.
Structure and functions ↑
Hard (outer) shell
The outer shell envelops the spinal cord from the outside in the form of a wide, elongated cylindrical sac from top to bottom.
It has the appearance of dense, shiny, whitish fibrous tissue with a huge number of elastic cords.
The outer surface is rough, facing the walls of the spinal canal.
From above, the border between the membranes of the spinal cord and the brain coincides with the foramen magnum.
Between the shell and the bony walls of the spinal canal is the periosteum.
Some authors call it the outer layer of the dura mater.
The inner surface is covered with endothelium (a single layer of covering cells), resulting in a shiny, smooth appearance.
Approaching the head, the hard shell fuses with the occipital bone, forming the edges of the foramen magnum, and approaching the lower parts of the spinal canal, it narrows in the form of a thread that is attached to the periosteum of the coccyx.
At the top it is tightly connected with the atlanto-occipital membrane, where the vertebral artery passes through it.
Small connective tissue bridges attach the membrane to the posterior longitudinal ligament of the spine.
The hard shell envelops the nodes and nerves in the form of peculiar containers that expand towards the intervertebral foramina.
This property is one of the fixing factors.
The membrane receives blood supply from the spinal arteries, which arise from the thoracic and abdominal aorta.
Venous blood flows into the internal vertebral venous plexus. Innervated from the meningeal branches of the spinal nerves.
Arachnoid
This is the middle shell, in the form of a thin transparent sheet that does not have blood vessels.
It is connective tissue covered with endothelium.
Adjacent from the inside to the hard tissue in the area of the nerve roots. The space between them is called subdural.
Soft shell
The soft membrane directly envelops the spinal cord.
It is represented by delicate loose connective tissue, covered on the outside with endothelium and consists of two sheets, between which there are numerous vessels.
The outer plate forms serrated ligaments that originate between the anterior and posterior roots and stretch from soft to hard, and fix all the integuments of the spinal cord.
Fig.: membranes of the spinal cord: 1 - soft membrane; 2 - subarachnoid space; 3 - arachnoid membrane; 4 - dura mater of the spinal cord; 5 - epidural space; 6 - dentate ligament; 7 - intermediate cervical septum.
The inner lamina fuses with the spinal cord with the help of a glial membrane.
Together with the arteries, it not only envelops the brain, but also enters the grooves and directly into its very substance.
Accompanying the artery into the substance of the brain, it forms around the vessel something like a vagina - a vascular base.
The vessels originate from the anterior and posterior vertebral arteries, which, as they descend, unite and form numerous branches.
The veins are located similarly to the arteries and ultimately flow into the internal vertebral venous plexus.
Lymphatic vessels are represented by perivascular (near-vascular) spaces, which have the appearance of narrow slits communicating with the subarachnoid space.
Its distinctive feature from that of the brain is its greater thickness and strength.
Intershell spaces
The space located between the periosteum and the dura mater is called the epidural.
It contains fatty tissue, connective tissue and extensive plexuses of veins into which venous blood from the vertebrae and spinal cord enters.
Between the arachnoid and soft membranes there is a subarachnoid space in which the nerve roots and brain, surrounded by a large amount of cerebrospinal fluid, lie freely.
Photo: cells producing cerebrospinal fluid
The connection between these layers is carried out using numerous arachnoid trabeculae.
There are especially many strands in the posterior sections (in the cervical region), where they form the posterior subarachnoid septum.
The subarachnoid space is especially wide in the lower sections, where it surrounds the cauda equina of the spinal cord (a collection of nerve roots starting from the lumbar part).
The cerebrospinal fluid filling the subarachnoid space continuously communicates with the fluid of the ventricles of the brain.
Along the lateral sections there is a dentate ligament, which consists of 19-23 teeth and connects with the outer and inner integuments.
These teeth pass between the anterior and posterior nerve roots.
The dentate ligaments are designed to strengthen the brain in the required place, and do not allow it to stretch in length.
Thanks to both ligaments, the subarachnoid space is divided into anterior and posterior sections.
How dangerous is scoliosis for a child’s development? On our website you will find a lot of useful information about the consequences, causes and treatment of scoliosis in children.
Why do subluxations of the cervical vertebrae occur? Find out here.
Do you often suffer from pain in your right side under your ribs? Read about possible reasons in this article.