Thanks to improved diagnostics, the number of autoimmune diseases is growing. Cutaneous vasculitis is a dermatological diagnosis. But the disease belongs to the field of rheumatology, since the etiological factor of its occurrence is autoimmune processes. Inflammation of the vascular wall of allergic origin affects large arteries and veins, small arterioles, venules and capillaries, and can manifest itself in all vessels of the body at once. The disease is polyetiological, that is, it has many causes. Diagnosis is available, but treatment is difficult. Therefore, the importance of prevention and early detection of this pathology is great.
Types and causes of vasculitis
Depending on the root cause of the disease, all vascular pathologies are divided into two types:
- Primary vasculitis. It develops independently, without push from organs and systems. The reasons for the development of the primary disease have not been identified to this day.
- Secondary pathology. It is a consequence of past or existing chronic diseases.
Possible causes of vascular disease are:
- Prolonged or systematic contact with aggressive (biological/chemical) substances.
- The body's reaction to the introduction of any serum (vaccine).
- Long-term chronic or acute infectious processes (including hepatitis).
- Constant or prolonged hypothermia/overheating (including severe skin burns).
- Genetic predisposition.
- Complex injuries.
- Autoimmune processes in the body (reactive rheumatoid arthritis, glomerulonephritis, systemic lupus erythematosus, inflammation of the thyroid gland, Schwartz-Jampel disease, etc.).
Important : with existing pathologies, the immune system of the human body begins to treat certain organs and systems as foreign. As a result, it tries to destroy them by disrupting the functioning of blood vessels. The necrotic process in target organs cannot be reversed. You can only achieve long-term remission.
Etiology
In 50% of cases, the cause cannot be determined. There are some etiological factors of urticarial vasculitis and its relationship with other pathological conditions:
- autoimmune connective tissue diseases (systemic lupus erythematosus, rheumatoid arthritis, Sjogren's syndrome, etc.);
- viral infection (hepatitis C, etc.);
- hemoblastoses (leukemia, Hodgkin's lymphoma, myeloma, b-cell lymphoma, idiopathic thrombocytopenic purpura);
- reactions to medications (such as ACE inhibitors, some types of diuretics, penicillin, and nonsteroidal anti-inflammatory drugs);
- some types of malignant neoplasms;
- amyloidosis;
- physical impact (cold, sun and others);
- endocrinological problems (Graves disease);
- Cogan's syndrome.
Classification of vasculitis
All vasculitis is subject to classification depending on the type (size) of the affected vessels. So, the disease is divided into three groups:
- Damage to large blood vessels. In this case, Takayasu’s and Horton’s diseases, giant cell arteritis, etc. are formed.
- Damage to the middle vessels. It is characterized by Kawasaki disease, periarteritis nodosa, etc.
- Inflammation in small vessels. Granulomatous and cryoglobulinemic vasculitis, microscopic arteritis, etc. are formed.
Classification
There is no single classification as such. Types of the disease are distinguished according to many characteristics. Based on the etiology of the disease, two forms are distinguished:
- Primary vasculitis is an independent disease.
- Secondary vasculitis is a complication or syndrome of another disease.
Many experts subdivide vasculitis according to the depth of location of pathologically altered blood vessels:
- Superficial – vessels located in the dermis are involved in the pathological process.
- Deep – the vessels located between the skin and subcutaneous tissue are affected.
Superficial vasculitis:
- Hemorrhagic.
- Allergic.
- Leukoclastic.
- Chronic capillaritis.
Deep vasculitis:
- Periarteritis nodosa.
- Acute erythema nodosum.
- Chronic erythema nodosum.
Signs and symptoms of the disease
Symptoms of the disease vary depending on the root cause of its occurrence. That is, the symptoms are more likely to be characteristic of damage to a specific organ. In addition, the severity of signs of vasculitis is influenced by the localization of the inflammatory process and the duration of the disease. General signs of vascular inflammation and the onset of necrotic processes in the body are:
- decreased appetite and weakness;
- increased body temperature;
- weight loss;
- numbness of the limbs and cramps;
- joint pain;
- allergic-type skin rashes.
Otherwise, the symptoms of vascular lesions look like this, depending on the affected organ:
- Kawasaki disease. Children under the age of 5–6 years are most often affected. The child develops inflammation of the cornea of the eyes, vision is impaired, the retina of the eyes suffers, body temperature rises, and skin lupus rashes are detected.
- Leukocytoclastic vasculitis. It manifests itself mainly as allergic reactions to foods, serums, etc.
- Thrombangiitis (Buerger's disease). The veins and arteries of the extremities suffer. Due to impaired blood circulation, the patient experiences pain in the legs/legs/arms, and an ulcerative-necrotic process of the skin develops.
- Polyarteritis nodosa. In this case, the circulatory system of various organs (heart, kidneys, muscles, skin, intestines) suffers. The patient has a bright purple rash against the background of pale skin of the face and body.
- Takayasu's disease. With this pathology, the aorta and large blood vessels are affected. Women under 35 years of age are most susceptible to pathology. As Takayasu's disease develops, the patient experiences a weak pulse, weakness in the limbs, decreased vision, and headaches.
- Polyangiitis is microscopic. Small vessels of the lungs, skin and kidneys suffer. There are signs of glomerulonephritis or pulmonary vasculitis in the form of hemoptysis.
- Horton's disease (giant cell arteritis). The circulatory system of the head (arteries) is mainly affected. Due to this, the patient experiences hypersensitivity of the skin of the head and face, blurred vision, soreness in the maxillofacial muscles, and headache.
- Cerebral vasculitis. The vessels of the brain of the head are affected. The patient has hemorrhagic hemorrhages.
- Cryoglobulinemic vasculitis. Develops under the influence of hepatitis C. A patient with cryoglobulinemic essential vasculitis develops persistent weakness, the appearance of red spots on the legs, and arthritis. The essential form of pathology is most treatable.
- Scheleyn-Henoch vasculitis. It is also more common in young patients after a sore throat, acute respiratory viral infection, or scarlet fever. Although in rare cases it affects adults. In the first 2–4 weeks after the infection, the patient develops pain in the joints and abdomen, there may be blood in the urine, and purple spots appear on the feet and buttocks.
- Wegener's granulomatosis. It is also called granulomatous vasculitis. In this case, the patient develops granulomas (growths) in the area of the nasal passages and sinuses, in the kidneys, and lungs. As a result, the patient has a stuffy nose, blood is detected in the kidneys, pulmonary hemoptysis of the tuberculosis type and difficulty breathing are noted.
- Eosinophilic vasculitis. Or otherwise Churg-Strauss syndrome. The lungs, joints, heart, kidneys suffer. The disease is forced extremely rarely, but is of great interest to doctors.
Important: patients with vasculitis receive lifelong disability in case of tissue necrosis. People with this diagnosis are not accepted into the army.
Causes
To date, vasculitis has not been fully studied, and even the list of possible causes of the pathology is incomplete. The most common predisposing factor in the development of pathology is susceptibility to infectious diseases, which can occur hidden. They negatively affect the immune system, resulting in the development of an autoimmune form of pathology.
In addition, the following factors may influence the occurrence of vasculitis:
- individual intolerance to certain medicinal groups or individual negative reaction to them;
- frequent or isolated severe hypothermia;
- negative effects of natural and artificial ultraviolet rays;
- long-term intoxication of various origins;
- exposure to bacteria and viruses;
- serious liver diseases;
- excessive physical activity;
- frequent strong emotional experiences, stress, mental trauma;
- hypertonic disease;
- diabetes;
- mechanical damage to blood vessels during trauma or surgery.
Knowing the true cause of the disease, you can not only choose the right treatment, but also prevent the occurrence of pathology in the future.
Vasculitis is prone to relapse if the patient does not adhere to the doctor’s recommendations, so it is necessary to eliminate all risk factors from your life.
Diagnosis of the disease
To accurately determine the patient’s health status and find out the type of organ affected by vasculitis, the patient is prescribed a set of diagnostic measures. The examination includes:
- General blood and urine tests. They help to identify an increased amount of protein and leukocytes in the body, which confirms the inflammatory process. The presence of red blood cells in the urine and the level of ESR are also detected. A lack of hemoglobin and hematocrit is detected in the blood.
- Blood test for antinuclear antibodies. Detects autoimmune disorders in the body.
- Blood test for cryoglobulin and eosinophils.
- Ultrasound of internal organs. Depending on the results of urine and blood tests (suspicion of a focus of inflammation), the doctor refers the patient to an ultrasound scan of a specific organ. They examine the liver, heart and its aortic valve, kidneys, lungs, etc.
- MRI of the affected organ and blood vessels. Allows you to assess the stage of the disease.
- Angiography of blood vessels. Here the general condition of the vessels is assessed, their topography is monitored and the source of inflammation is identified.
- Histology. A tissue sample of the affected necrotic organ is taken from the patient to confirm or refute the process of necrosis.
Diagnostics
The examination of patients with suspected HF includes anamnesis, examination by a doctor, some laboratory tests, and sometimes requires consultation with specialists such as a rheumatologist, ophthalmologist, pulmonologist, nephrologist, neurologist, cardiologist and others. Blood tests quite often show increased levels of “C-reactive protein” and “ESR” (erythrocyte sedimentation rate), which indicates inflammation in the body. Testing for C1q, anti-C1q, determination of the levels of C3 and C4 complements in the blood is important for determining the type of HC.
Sometimes a test is performed for antinuclear antibodies (ANA), which are positive in 30 - 50% of cases, and antibodies to dsDNA (double-stranded DNA) are also determined.
Many cutaneous vasculitis, in particular urticarial, require a skin biopsy for final diagnosis, which is the “gold standard” for diagnosis for this pathology.
Treatment of vasculitis
The main goal of treatment of vascular inflammation is to achieve stable remission. The pathology can be completely cured in the initial stages. Unfortunately, an advanced disease cannot be overcome. Vasculitis is incurable. Pathology is treated comprehensively using the following methods:
- Drug therapy with antibacterial, anti-inflammatory and hormonal drugs.
- Homeopathy.
- Physiotherapeutic effects on the body.
- Dieting.
- Prevention of relapse.
Important: any medications should be prescribed only by a doctor after making an accurate diagnosis.
Drug therapy
When using drug therapy, the patient is prescribed the following drugs:
- Cytostatics. Particularly indicated in the formation of oncological processes in necrotic organs. These drugs stop the growth and division of malignant cells. In addition, cytostatics work well against nephritis. Medicines such as fluorouracil or cyclophosphamide, doxorubicin, and methotrexate are prescribed.
Important: if cytostatics are contraindicated for the patient, he is prescribed monoclonal antibodies. They have a similar effect. But monoclonal antibodies are not used for neutropenia, hepatitis B and low concentrations of IgG in the patient’s blood.
- Glucocorticoids. These drugs belong to the group of hormonal drugs. They neutralize allergic reactions, regulate immunity, relieve stress and shock in the body. As a result, ulcerative manifestations, rashes, and spots are reduced. The most effective are prednisolone and hydrocortisone. The drugs are prescribed in the form of tablets, ointments and creams. Skin healing occurs quite quickly.
Important: simultaneous use of cytostatics and glucocorticoids works well. In this case, the course of therapy is 4–12 months.
- Immunosuppressants. Drugs that suppress the immune system.
- Human immunoglobulin. Relevant for severe lesions of the urinary system (kidneys), complicated infections, etc.
- Antibiotics. Indicated in case of bacterial infection.
- Anti-infective drugs in the presence of a viral infection.
- Anti-inflammatory non-steroidal drugs. Prescribed in rheumatology for joint damage and thrombophlebitis.
- Detox medications. Helps remove allergens and drug breakdown products.
- Antihistamines. Prevents allergies to medications.
- Anticoagulants. Protects against the development of thrombosis. Heparin and heparin ointment, Detralex, warfarin, etc. are prescribed.
Important: plasmapheresis and hemosorption (mechanical hardware blood purification) can enhance the effect of therapy.
Diet therapy
Dietary food for vasculitis has a hypoallergenic effect. Therefore, all recipes that include allergenic foods are excluded from the diet:
- chicken egg and milk;
- all red berries, fruits, vegetables;
- coffee and black tea;
- chocolate;
- citrus;
- baked goods and confectionery;
- preservation and marinades;
- carbonated drinks and all foods with dyes.
A patient with vasculitis and kidney damage is shown table No. 7. Often patients with vasculitis practice a raw food diet. But this is optional. Especially during pregnancy.
Important: before starting a diet, it is advisable to conduct a hemotest to determine intolerance to specific foods.
Treatment with folk remedies
With the consent of the attending physician, treatment with folk remedies can also be used. The most effective are:
- Green tea. Strengthens the walls of blood vessels and reduces their permeability.
- Sea buckthorn. Oil from the berries heals ulcers well. It can be applied to wounds twice a day.
- Herbal lotions. The following herbal mixture works well: mint, black elderberry flowers, calendula, poplar buds, yarrow, horsetail and string. All herbs are taken in the proportion 2:3:3:2:2:3:3. The collection is boiled and left for about 20 minutes. The strained infusion is used as a compress.
- Tinctures from herbs such as calendula, ginseng, arnica, Rhodiola rosea, Eleutherococcus. Tinctures are taken before meals, 35–40 drops diluted in 100 ml of clean water.
Causes
Doctors say that there are many reasons for the development of vasculitis. A mild infectious disease makes the human immune system weak and practically defenseless. Chronic otitis, tonsillitis, adnexitis can provoke the development of cutaneous vasculitis.
Vasculitis on the legs
Additional reasons for the development of pathology can be considered:
- Long-term intoxication of the body with alcohol, medications or poor quality food.
- Individual sensitivity to drugs (allergy is most often caused by antibiotics).
- Streptococcal or staphylococcal infection.
- Infection of the body with viruses, microbacteria, pathogenic fungi.
Only a physician can accurately determine the cause of vasculitis. He must conduct an initial examination of the patient, study the diagnostic results, and only after that make the correct diagnosis.
Forecast
The most favorable prognosis is vasculitis, which affects the joints and skin. Here, stable remission can be achieved within 1–2 months from the start of treatment. If internal organs are affected, the patient may develop the following complications:
- complete loss of vision;
- myocardial infarction or ischemic heart disease;
- complete kidney failure;
- glomerulonephritis;
- intestinal bleeding;
- death.
Important: the accuracy and effectiveness of treatment depends on a correct diagnosis.
Basic principles of treatment
Treatment of vasculitis is prescribed depending on the activity of progression of the pathological process, the degree of damage to the skin, and an assessment of the systemic manifestation of the disease. If doctors have been able to establish the root cause of the pathology, therapy to eliminate the provoking factors must be prescribed.
Measures must be taken to stop inflammatory processes and speedy healing of damaged areas of the skin. In the photo you can see the different forms of manifestation of pathology. And the earlier treatment measures were taken, the greater the chance of completely clearing the skin, quickly curing inflammation, and eliminating associated symptoms. The rash, which manifests itself as hemorrhagic vasculitis, is periodically treated with Dimexide applications and lubricated with special ointments (Actovegin, Maxidex, Iruksol).
Read also: Urticarial vasculitis photo
To treat pathology that has spread to internal organs, drugs from the NSAID group (Diclofenac, Aspirin), anticoagulants and nicotinic acid are used. If therapy with these drugs is ineffective, doctors recommend undergoing plasmapheresis. Treatment of the disease is a comprehensive approach that eliminates the skin manifestations of the disease, cause and symptoms.
Prevention
To prevent persistent remission from turning into a relapse or primary vasculitis from overtaking a person, it is advisable to adhere to certain preventive measures:
- Healthy emotional state and lack of stress.
- Take medications only as prescribed by a doctor and avoid uncontrolled treatment.
- Maintaining a healthy lifestyle.
- Body weight control.
- Treatment of all chronic diseases and control of health status.
- Maintaining physical activity.
- Maintain a healthy diet that includes plant fiber.
Remember, vasculitis is an extremely dangerous disease, but with persistence it can be treated. Once remission is achieved, it is extremely important to prevent relapse.
Reasons for the development of pathology
The disease develops under the influence of various factors. The main cause of skin vasculitis is considered to be latent and sluggishly developing infections in the body - otitis media, tonsillitis, chronic infectious lesions of the epidermis. Among the accompanying factors that stimulate the appearance of pathology are:
Vasculitis is a term that combines a group of skin diseases caused by damage of various origins to the subcutaneous tissue, as well as small vessels of the skin.
- long-term intoxication of the body of various origins;
- viruses, infections, certain types of pathogenic fungal bacteria;
- increased individual sensitivity to the active components of medications. Most often, broad-spectrum antibiotics and sulfonamide-based products provoke skin vasculitis.
Autoimmune diseases are also the cause of the cutaneous form of this disease. To prescribe treatment, it is important to determine the type of pathology and clarify the cause of the disease.
Elimination of manifestations of atherosclerosis
How to treat cerebral atherosclerosis? In this case, medications are determined after consultation with a neurologist, therapist, and other doctors who specialize in eliminating signs of disease development.
Usually, after appropriate diagnosis, patients are prescribed products designed to cleanse blood vessels and restore healthy blood circulation in the brain area. We are talking about medications containing anion exchange resins, fibrates, antioxidants, cerebrolysin, iodine and lecithin.
Prognosis and prevention
Despite complex treatment, complete and final elimination of skin lesions does not occur; the patient may develop a relapse at any time. Skin vasculitis is not dangerous for the patient’s life. They are also not dangerous to others, are not contagious, and are not directly inherited. A child can only inherit disturbances in the functioning of the immune system, which can manifest themselves in a variety of diseases in the future.
To prevent relapse of the disease it is necessary:
- elimination of foci of chronic infection;
- refusal of prolonged stress on the legs;
- avoiding bruises and hypothermia;
- rational employment with the exclusion of harmful factors.
Practicing dermatologist V.V. tells everything about skin vasculitis. Makarchuk:
What types of vascular inflammations are there?
Inflammation of the blood vessels of the brain is a rather dangerous pathology, since it is very difficult to diagnose vasculitis. This is due to the fact that the problem lies not in the condition of the arteries themselves, but in the organ that is being served. Thus, the symptoms indicate inflammation of one organ, but in reality the pathology is located in another place.
Description of the disease
Vasculitis is an inflammatory process of the entire circulatory system, but the disease is especially dangerous when such a vital organ as the brain is affected. As a rule, the disease is immunopathological in nature, that is, the functionality of the immune system is impaired. At the same time, cells on the walls of blood vessels can be identified as foreign, and therefore are actively attacked.
When antibodies are released into the blood, immune complexes are formed in large quantities. A short period of time is enough for growths of leukocytes and macrophages to form on the walls of the arteries, which increases the number of platelets, and this leads to destruction of the venous system. Initially, the walls lose elasticity and become permeable. And then necrotic irreversible changes occur.
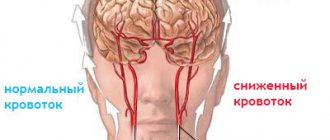
Due to inflammation of the blood vessels in the brain, the symptoms of which do not manifest themselves in any way, blood flow decreases. Consequently, the organ being served does not receive enough oxygen and nutrients. For example, if vasculitis is located in the temporal part of the brain vessels, then the occipital part remains without oxygen, and the disorder is observed in the visual organ.
Classification
Inflammation of the blood vessels of the head can be primary or secondary. In the first case, the disease originates precisely because of pathologies of the walls of blood vessels, and in the second it is a consequence of infection, injury or allergy. Vasculitis is classified according to its location. So, it could be:
- Inflammation of the inner wall of the vessel (endovasculitis).
- Pathology of the middle layers (mesovasculitis).
- Damage to the outer layer of the vessel (perivasculitis).
- Anomaly of all layers simultaneously (panvasculitis).
Elena Malysheva: Heart diseases go away instantly! Read more
Symptoms of inflammation
With inflammation of the blood vessels in the brain, symptoms can be general:
- Feeling weak for no specific reason.
- Fast fatiguability.
- Drowsiness.
- There is no reason for the temperature to rise.
- Pain syndromes in the brain area.
- Decreased appetite.
- Redness of the eyeball.
- Constant itching in the eyes.
- Noticeable deterioration in vision and hearing.
- Speech impairment.
- Memory impairment.
- Depression.
IMPORTANT! As you know, all these signs may well be symptoms of other diseases, so a thorough examination of the circulatory system of the brain is extremely important. You cannot postpone diagnosis until later, as this is fraught with dangerous consequences and complications.
With secondary inflammation, psychosis may increase, manifested by unreasonable aggression. In addition, dementia progresses significantly, and convulsive seizures appear.
What other inflammations could there be?
Of course, inflammation of the blood vessels of the brain includes not only vasculitis, but there are many others. For example, inflammation due to cancerous or benign tumors, pathology of the pia mater, thanks to which the circulatory system functions (it passes through the membrane) and much more, which can mainly be diagnosed by a specialist.
Treatment of inflammation of the vascular system
If you diagnose the inflammatory process in the blood vessels of the brain in a timely manner, you can easily and quickly get rid of it. Thus, in the primary stages of vasculitis, treatment is carried out using drug therapy. These may be antiplatelet agents that restore the normal thickness of blood fluid and prevent the formation of blood clots.
In many cases, the doctor prescribes non-steroidal anti-inflammatory drugs. For example, "Parmidine" or "Stugeron". The doctor may prescribe anticoagulants (Sincumar, Heparin). At later stages of the disease, glucocorticoid medications can be used.
In very difficult cases, surgical intervention is performed. The surgical technique is selected on an individual level. This may be an endarterectomy, that is, removal of an atherosclerotic plaque, or an endovascular method, which involves eliminating an entire section of the inflamed vessel.
GET RID OF varicose veins right at home in just 1 week. Read more
Elena Malysheva: Heart diseases go away instantly! Read more
The health of your head Miscellaneous Inflammation of the cerebral cortex and blood vessels: symptoms and treatment
Brain vasculitis in systemic diseases
Damage to cerebral vessels can occur as a complication of systemic diseases. In Churg-Strauss syndrome and periarteritis nodosa, symptoms include hyperkinesis (involuntary movements) and epileptic seizures. With this form, treatment gives positive results. Wegener's granulomatosis is accompanied by deterioration of vision and hearing, inflammation of the meninges (meningitis).
With Takayasu's disease (nonspecific aortoarteritis), orthostatic syncope occurs. These are fainting spells that occur when the patient moves from a horizontal to a vertical position. Also, while chewing, the headache intensifies. Treatment of cerebral vasculitis in such forms of systemic diseases gives good results.
General signs of cutaneous vasculitis
The rash with cutaneous vasculitis is polymorphic, with elements of inflammation
. Despite the different symptoms, all these angiitis have similar features:
- an allergic rash with elements of inflammation, swelling, subsequently with hemorrhages into the skin and tissue necrosis;
- the elements of the rash are not the same in shape and size, their polymorphism is observed;
- rashes are symmetrical;
- the rash first appears or is most severe on the legs;
- tendency to acute inflammation and frequent relapses;
- combination of angiitis with vascular or allergic diseases.
How to feel quick relief from vasospasm?
To alleviate the patient’s condition in case of spasm, doctors who treat cerebral vessels recommend immersing the legs in a container of cold water for several minutes. Then you should lie down, washing your face with running water before doing so.
Massage procedures also help eliminate negative manifestations. It is necessary to perform stroking movements in the direction from the bridge of the nose to the temporal region, and then massage the head from the forehead to the chin.
The use of aromatic oils has a good effect. How are cerebral vessels treated with their help? To do this, during rest, a small amount of infusion of valerian, mint, lavender or jasmine is dripped onto the upper lip.
What is cerebral vasculitis
Cerebral vasculitis is damage to the walls of blood vessels in the brain due to inflammation.
The result of vasculitis can be transient ischemic attacks and stroke. Diagnosis is an extremely difficult procedure, because in order to 100% confirm the diagnosis it is necessary to perform a biopsy.
The disease is rare - approximately 1 case per 1 million people per year, while systemic vasculitis affects 39 people per 1 million per year.
Causes
To date, the causes of the disease have not been established. The clinical picture and signs are similar to other diseases that are associated with cerebrovascular accidents. A characteristic feature is the presence of rashes on the skin, combined with neurological manifestations.
Frequent symptoms are paresthesia and mood changes - a person becomes irritable, feels apathy, fatigue, and irritability.
Cerebral vasculitis refers to diseases that can potentially lead to disability of the patient. The reasons for its development usually lie in rheumatic lesions, infectious diseases, the formation of malignant tumors, and are caused by taking medications. However, there are cases when vasculitis develops as a primary disease.
Insufficient knowledge of the mechanism of origin and development of pathology, the multiplicity of its clinical manifestations, and the lack of accurate and truthful non-invasive diagnostic criteria greatly complicate diagnosis at the initial stage of the disease.
- Cerebral vasculitis is a severe lesion in which the inflammatory process affects vessels of any diameter. This leads to a deterioration in blood supply, therefore, the brain stops receiving oxygen in the volume it needs.
- The disease appears suddenly and can occur with equal frequency in both men and women. The symptoms are similar to those of a stroke: speech dysfunction, hearing and vision impairment, and motor activity. It should be noted that isolated cerebral vasculitis of the brain is very rare.
- The acute period is replaced by a long remission, followed by a new exacerbation. It is possible to develop mental disorders, which greatly affects a person’s behavior and character.
- Signs of sclerosis and fatigue may appear. Inflammatory processes lead to the development of structural changes in the brain, and subsequently to partial ischemia and death of its areas.
- Gradually the disease progresses. It can be difficult to diagnose, and the clinical picture and symptoms are similar to those of a brain tumor. This form of vasculitis is treated by specialists from the neurological department.
- Often develops against the background of rheumatism and collagenosis. These pathologies are accompanied by impaired renal function and, as a consequence, increased blood pressure. In turn, increased blood pressure provokes the development of neurological symptoms. In rare cases, we can talk about the blood-brain barrier as the cause of vascular damage.
- Cerebral disorders develop in approximately 1/2-1/3 of cases of rheumatic pathologies.
- Secondary vasculitis caused by systemic diseases is accompanied by a blurred clinical picture. Patients do not feel a significant deterioration in their health, but doctors face even greater difficulties in making a diagnosis.
- Laboratory and instrumental research methods can provide some information. Disturbances in the functioning of the central nervous system cause an increase in ESR and SRV. In this case, a slight increase in proteins is detected in the cerebrospinal fluid, and in case of subarachnoid bleeding - red blood cells.
- Angiographic results may be used. Cerebral vasculitis is characterized by differences in the thickness of the vascular wall, stenosis and occlusion of vessels, the occurrence of collaterals, and aneurysms.
- With cerebral vasculitis caused by tuberculosis, disorientation in space, hemiplegia, dysarthria, etc. are observed.
Symptoms of cutaneous vasculitis
Manifestations of the disease depend on how large the skin vessels are affected. Therefore, there are three types of cutaneous angiitis:
- hypodermal - deep, affecting arteries and veins with rather thick muscle walls (this is periarteritis nodosa and angiitis nodosa);
- dermal - superficial, affecting the smallest arteries, veins and capillaries (this is polymorphic dermal angiitis, chronic pigmentary purpura and others).
Cutaneous form of periarteritis nodosa
Usually there are a few formations ranging in size from 1 to 3 cm, periodically appearing along the vessels on the legs. The skin above them acquires a bluish-pinkish tint. Such nodes are painful, can turn into ulcers, and last from several weeks to months.
Angiitis nodosum, or erythema nodosum
Characteristic features are reddish nodules, slightly raised above the surface of the skin and painful. Most often they are located on the front surface of the legs. Such nodes gradually develop and disappear.
The nodes are usually painful and inflamed for several weeks. Then they gradually decrease in size and merge with the skin, leaving bluish spots, which then also disappear without a trace. This condition recurs quite often, so the patient may simultaneously have newly formed nodes on the legs at different stages of development, as well as those that are already disappearing.
Polymorphic dermal angiitis (Gougerot-Ruiter disease)
One of the variants of polymorphic dermal angiitis is hemorrhagic.
This disease has several types:
- urticarial (resembles chronic urticaria);
- hemorrhagic (manifests as a hemorrhagic rash in the form of petechial skin hemorrhages, purpura, bruises - ecchymosis, blisters that open to form erosions and ulcerative defects);
- papulo-necrotic (inflamed nodes in the center undergo tissue disintegration - necrosis, so after their healing, retracted scars remain);
- pustular-ulcerative (reminiscent of gangrenous pyoderma - first, blisters appear on the skin, which then form a continuous inflamed surface, and eventually turn into an ulcer with a diameter of up to several centimeters; after healing, a deep scar remains);
- necrotic-ulcerative (foci of skin necrosis immediately form, turning into ulcers);
- polymorphic (purpura, nodules, blisters and other rashes are present at the same time).
Chronic pigmentary purpura
This disease has synonyms: progressive pigmentary purpura of Chambert or cutaneous hemosiderosis. It manifests itself as constantly recurrent multiple subcutaneous hemorrhages (petechiae), which then transform into brownish spots of iron deposits, that is, hemosiderosis.
Radical treatment methods
How are cerebral vessels treated in a neglected state? With significant progress of the disease, when the use of medications does not produce virtually any positive effect, doctors often resort to surgical interventions.
The primary method here is carotid endarterectomy, a procedure during which cholesterol plaques are removed from dissected vessels. The structure of the damaged walls of the blood ducts is restored over time thanks to the application of sutures.
Angioplasty is also an effective surgical treatment method. During the operation, a very thin catheter is inserted into the artery, which moves to the area of the blocked vessel and pushes out cholesterol plaques.
How to treat cerebral vessels? Folk remedies can provide therapy only if pathology is detected in its early stages of development. Among the most effective recipes are:
- A decoction based on pine shoots. A few tablespoons of raw materials are mixed with a similar amount of ground rose hips. Lemon juice and honey are added here. The resulting composition is poured with a liter of water and boiled. The product is infused throughout the day. Take the resulting decoction 0.5 liters per day. The product saturates the body with a complex of vitamins and acts as an excellent antioxidant.
- Hawthorn decoction. Two tablespoons of the fruits of the plant are poured into a glass of boiled water. As an alternative, you can use a ready-made pharmacy hawthorn tincture. The product must be added a few drops to tea or drinking water. Consumption of the decoction leads to vasodilation, nutrition of the heart muscle, and has an antispasmodic effect on tissues.
- Clover tincture. A liter jar is filled with plant inflorescences and filled with vodka. The composition is infused in a dark place for two weeks. Like hawthorn tincture, clover-based remedy is added 5-10 drops to various drinks. The product eliminates the first signs of the development of atherosclerosis, improves memory, and eliminates the feeling of tinnitus.
Clinical manifestations
Symptoms depend on the form and severity of vasculitis. Common signs include:
- fever;
- the appearance of hematomas on the skin, bleeding;
- joint pain, impaired mobility;
- sudden weight loss.
In severe forms, the nervous system and internal organs are affected. If not treated in a timely manner, it becomes chronic, characterized by frequent relapses.
When small blood vessels are damaged, a small rash resembling hives appears on the body. The affected area turns red and swells. When vessels of medium diameter are affected, small nodular seals are formed.
Drug therapy
How to treat cerebral vasoconstriction? There is a wide range of medications that improve the condition of the bloodstream. Among these it is worth noting:
- Drugs for lowering cholesterol levels - Zocor, Leskol, Lipitor, Crestor.
- Products with a high content of nicotinic acid - Niaspam, Nicolar.
- Medicines that help remove bile acid from the body - “Velhol”, “Cholestide”, “Questran”.
- Medicines that normalize fat metabolism processes - “Atromid”, “Traykor”, “Ezetimibe”, “Clofibrate”.
Before resorting to independent use of the listed remedies, it is strongly recommended to find out which doctor treats cerebral vessels and sign up for a consultation. Only a qualified specialist is able to choose the most effective drug in a particular case, identify side effects, and also determine the incompatibility of individual medications.
How to treat cerebral vasospasm? In addition to medications, it is important to take vitamins. The following substances help improve the elasticity of blood vessels:
- B vitamins;
- vitamin C;
- vitamin A;
- vitamin E;
- zinc, calcium.
The listed substances can be taken without a doctor's prescription. Vitamin complexes help strengthen blood vessels and have a positive effect on the processes of lipid metabolism in the body.
Description of popular diseases
A more detailed description and classification of common and rare vasculitis.
- Hemorrhagic
If a child has been diagnosed with vasculitis, then he needs to be observed by a doctor throughout his life.
It occurs with symptoms of superficial vasculitis, characterized by damage to the capillaries of the skin, joints, gastrointestinal tract and kidneys. It is based on increased production of immune complexes, increased vascular permeability and damage to the capillary wall. The disease can begin at any age, but the maximum number of reported cases occurs between the ages of 4 and 12 years. Hemorrhagic vasculitis, as a rule, manifests itself 1-4 weeks after scarlet fever, ARVI, tonsillitis or other infectious disease. Vasculitis is often a consequence of vaccination, food allergies, hypothermia or drug intolerance. If vasculitis is diagnosed in children, then you need to be observed by a rheumatologist throughout your life.
- Allergic
Allergic vasculitis manifests itself in inflammation of the vascular wall when exposed to infectious and toxic factors. Many of its forms, due to variable polymorphism, are isolated into separate diseases, which are divided into superficial and deep. This form of vasculitis requires a mandatory comprehensive diagnosis, taking into account the history, clinical picture, instrumental and laboratory data and histological results.
In treatment, vascular, desensitizing agents, antihistamines, glucocorticoids and drugs containing Ca are used.
Unlike systemic forms, allergic vasculitis occurs mainly with damage to blood vessels that pass through the skin and subcutaneous tissue (skin vasculitis). There are no preferential age and gender criteria for this disease, but there is one pattern - vasculitis with hemorrhages occurs more often in children under 14 years of age, and Schamberg's dermatosis is the lot of the male population.
- Surface
Characterized by damage to small venules, arteries and capillaries. This group includes:
- hemorrhagic vasculitis;
Hemorrhagic vasculitis belongs to a group of diseases that mainly affect young people
- hemosiderosis
The diseases are characterized by damage to the endothelium, precapillaries and capillaries with the deposition of hemosiderin, an iron-containing pigment formed after the breakdown of hemoglobin. In the clinic they have: petechial rashes, spider veins and small yellow-brown spots. The rash is most often found in the lower extremities (rarely on the arms), which is accompanied by itching of varying intensity. The patient's condition, as a rule, does not change, but sometimes trophic ulcers may appear.
- Ruter's allergic arteriolitis;
- acute smallpox lichenoid parapsoriasis;
- nodular necrotizing vasculitis;
- hemorrhagic leukoclastic microbid.
- Deep
It affects arteries of medium and large caliber, which pass in the subcutaneous fatty tissue at the border with the dermis.
Deep hemorrhagic vasculitis can affect arteries and veins of any caliber and gradually destroy them
Characteristic clinical signs may present differently in the form of acute and chronic erythema nodosum.
Prognosis for recovery
If the disease is in its primary form, then it will be much easier to treat, and the result will come faster. However, everything depends on the patient, the timeliness of seeing a doctor and the correctness of treatment.
Urticarial vasculitis can be easily confused with an allergic reaction, so it is very important to consult a doctor promptly. After a series of studies, he will make a diagnosis and prescribe the correct treatment. In no case should you self-medicate, because the advanced and chronic stage of the disease is very dangerous, and if there are disorders in the brain, it can lead to a stroke.
Hemorrhagic vasculitis in children and adults, causes and treatment, drugs
Disorders based on the processes of aseptic inflammatory reactions in the vascular system of small vessels are hemorrhagic vasculitis (HV). The disease is included in the extensive registry of immune complex pathologies.
It is characterized by damage to the microvessels of the skin and individual organs due to intravascular microthromb formation. In medical terminology it can be called rheumatic, allergic, or anaphylactic purpura.
The genesis of the development of the disease is due to the influence of viral, parasitic, bacterial pathogens and various representatives of toxic infections, provoking the formation of anaphylotoxins (special immune complexes) from their own immune cells, which have the effect of destruction. When the body is healthy, anaphylotoxins break down. In sick people they accumulate, turning into antigens.
Deposition on intravascular walls changes their permeability and disrupts blood circulation processes, causing:
- platelet activation;
- decrease in the level of antithrombin in the blood;
- blocking the fibrinolysis process.
This all becomes a key point in the development of a mass of small blood clots in microvessels against the background of reduced blood coagulation and allergic inflammation processes, causing the development of various forms of hemorrhagic vasculitis in adults and children.
Quick page navigation
Symptoms of urticarial vasculitis
The symptoms of the disease are numerous, but the main one is the appearance of rashes. The rash is quite characteristic - it consists of blisters and nodules that vary in size. The symptoms of the rash are as follows:
- clearly defined contours;
- structure density;
- the formation of a hemorrhagic rash that forms after the blisters break.
In addition to skin rashes, the pathology is accompanied by damage to internal organs. Inflammation may affect:
- joints (in approximately 70% of all cases);
- gastrointestinal organs (approximately 30%);
- inflammation of the conjunctiva and damage to the central nervous system (in 10% of cases);
- lymph nodes (approximately 5%).
Symptoms of joint inflammation (arthritis):
- the appearance of swelling over the inflamed joint;
- pain inside the joint.
Advice! The pain is caused by the appearance of an urticarial rash inside the joint. As a rule, the symptoms of arthritis subside 3-4 days after the onset of the disease.
Symptoms of gastrointestinal tract damage will be as follows:
- there is a disorder of digestive processes;
- nausea ending in vomiting;
- pain syndrome of varying intensity.
In severe cases, inflammation of the gastrointestinal tract with urticarial vasculitis can be complicated by gastric bleeding. Symptoms of central nervous system damage:
- headache;
- paresis;
- surges in intracranial pressure.
Symptoms of hemorrhagic vasculitis by form
Hemorrhagic vasculitis photo in adults
Clinical manifestations of hemorrhagic vasculitis are caused by many forms:
- Skin – in which the pathological process develops only in the skin.
- Skin-articular, caused by the addition of signs of joint inflammation to skin lesions.
- Skin-abdominal, manifested not only by skin changes, but also by functional disorders of the gastrointestinal tract.
- Renal, characterized by vascular damage to the kidneys and impaired filtration and urination.
- Combined – with signs of periodic manifestations of various forms of the disease.
The course of hemorrhagic vasculitis in children and adults can manifest itself in different ways: fulminant, acute, subacute, protracted, recurrent and chronic forms.
Features of general and skin signs
Signs and symptoms of hemorrhagic vasculitis appear unexpectedly without any warning signs - the increase in symptoms occurs quickly. The temperature can be low-grade, but more often it is very high, especially in adult patients. Initial signs of intoxication are noted. This condition is common to many diseases, which makes diagnosis difficult.
hemorrhagic vasculitis photo of a rash on the buttocks
A distinctive feature of hemorrhagic vasculitis is symmetrical skin rashes on the backs of the feet, the skin of the legs and the surface of the buttocks. On the back, stomach and arms, a rash is a rare occurrence, but on the palms, face, soles and cervical area, rashes are not at all typical. They tend to appear in a different color palette:
- bright red small blisters;
- nodular papules that turn pale with light pressure;
- papular purple nodules and blue subcutaneous petechiae;
- hemorrhagic red rash on the mucous membrane of the pharynx and mouth.
The size of the rash elements varies and can reach 1 cm. It stays on the body for up to 4 days, turns pale and disappears. The next wave of skin rashes appears after one and a half weeks.
The initial signs of the cutaneous form of hemorrhagic vasculitis appear in the form of small subcutaneous hemorrhages (petechiae), localized on the upper parts of the feet and legs. Sometimes they appear on the skin of the arms, back and abdomen. In the affected area - under the hair on the head, around the eye sockets, severe itching symptoms and pain are noted.
Lips, eyelids, and perineal area swell. After the rash disappears, pigmentation remains in its place, causing peeling during the period of relapse. Scar formation is possible due to the fusion and necrosis of individual areas of the rash, and the addition of secondary infections.
Hemorrhagic vasculitis is characterized by the manifestation of various syndromes (complex of symptoms) inherent in many pathological processes. Eg:
Articular syndrome of hemorrhagic vasculitis occurs in almost half of adult patients. Large joint groups of the legs are subject to inflammatory processes. Sometimes, inflammatory reactions affect the elbow and wrist joints and can develop within a week and even precede skin lesions.
In this case, the following are noted: swelling and redness of the legs, migratory pain in the extremities and the manifestation of myalgia (muscle pain). Intense pain with severe inflammation and swelling can lead to changes in gait. As a rule, joint deformities and impairment of motor functions do not occur.
Read also: Disability due to vasculitis
Gastrointestinal syndrome (abdominal) is characterized by short-term colic, nausea, and vomiting. It appears simultaneously with the skin lesion or a little later. There are no significant changes in the patient's condition. If the symptoms of hemorrhagic vasculitis are not treated in a timely manner, signs of intestinal and gastric bleeding appear - vomiting with blood and diarrhea with blood.
With severe lesions, manifestations of intussusception (obstruction), perforation (perforation of the intestine) and peritonitis (inflammation of the peritoneum) are possible. Symptoms of this syndrome include: weakness, sensations of noise in the head and flickering before the eyes, dizziness, tachycardia and fainting.
The manifestation of renal syndrome is observed in more than half of patients after a week of skin rashes. It appears very rarely in isolation. Causes the development of an acute form of glomerulonephritis of an autoallergic nature with inflammatory processes throughout the renal apparatus, and a sharp decrease in the tone of the vascular beds.
There are traces of blood in the urine, caused by the weakening of the inflamed walls of the arterioles, through which red blood cells freely leak.
Pulmonary changes appear due to damage to the patient's respiratory tract and pulmonary lobes. Manifested by cough and shortness of breath, blood in the sputum due to increased capillary bleeding.
Cardiovascular changes are characterized by signs of severe tachycardia and a predisposition to arrhythmia.
Nervous system syndrome is considered an unfavorable consequence of hemorrhagic vasculitis. Caused by the spread of the inflammatory process beyond the vascular lesion, involving the lining of the brain in the process. Therefore, the symptoms manifest themselves as signs of encephalitis and meningitis - severe migraines, ataxia (impaired coordination), and convulsions.
Diagnosis of skin vasculitis
Diagnosis of skin vasculitis in typical cases does not present significant difficulties; it is based on clinical and anamnestic data (the presence of a previous general or focal infection, taking allergenic medications, exposure to mechanical, physical and chemical agents, prolonged standing, hypothermia, etc.). In the clinical picture, it is important to determine the degree of activity of the pathological process (Table 2). There are two degrees of activity of the skin process in vasculitis:
— I degree. The skin lesions are limited in nature, there are no general symptoms (fever, headache, general weakness, etc.), there are no signs of involvement of other organs in the pathological process, laboratory parameters are without significant deviations from normal values.
- II degree. The process is disseminated in nature, general symptoms are noted, signs of a systemic process are identified (arthralgia, myalgia, neuropathy, etc.)
To confirm the diagnosis in the case of a persistent course of the disease or its atypical variety, it is necessary to conduct a pathohistological examination of the affected area of the skin.
The most characteristic pathohistological signs of cutaneous vasculitis: swelling and proliferation of the endothelium of blood vessels, infiltration of vascular walls and their circumference with lymphocytes, histiocytes, neutrophils, eosinophils and other cellular elements, the phenomenon of leukocytoclasia (destruction of leukocyte nuclei up to the formation of “nuclear dust”), fibrinoid changes in vascular walls and surrounding tissue up to complete or segmental necrosis, the presence of erythrocyte extravasates. The main pathohistological criterion for vasculitis is always the presence of signs of isolated inflammation of the vascular wall.
Differential diagnosis
Differential diagnosis of skin vasculitis is carried out with skin tuberculosis, eczema and pyoderma.
Stages of the disease
Constriction of cerebral vessels develops in several stages:
- Mild - occurs without significant symptoms. It appears in people who suffer from lack of sleep, moral and physical stress at work. This lifestyle ultimately leads to a deterioration in your general condition. It is extremely rare to diagnose vasoconstriction at a mild stage, since most people are in no hurry to go for examination.
- Intermediate - narrowing of the blood vessels in the brain affects the deterioration of the functioning of a number of organs and systems. First of all, a person begins to suffer from changes in coordination of movements. Limbs may periodically go numb.
- Chronic – is expressed in more serious disorders of the brain. A person periodically loses the ability to control his own body. There is a slowdown in movements. Ultimately, the musculoskeletal system refuses to function normally. In the most advanced cases, visual and speech impairments are noted.
The danger here is that many people independently select drugs that treat cerebral vessels, giving preference to all kinds of analgesics that only relieve pain. Therefore, serious, targeted therapy starts too late, when the patient is on the verge of a stroke or in a pre-infarction state.
The vessels of the brain may narrow gradually, or this phenomenon will be sudden and sharp. In the latter case, cerebral infarction and hemorrhagic stroke are possible. In severe cases, death occurs.
If the disease is chronic, then the first signs of cerebral vasoconstriction do not appear immediately. In the process of studying the main problems arising in the work of the vascular system, three stages (degrees) of vascular damage and circulatory disorders were identified:
- First. There are no signs of the disease, or they are insignificant. The patient occasionally complains of fatigue, insomnia and irritation, but attributes this to hard work and family troubles. At the first stage of the formation of the disease, associated with narrowing of the blood vessels in the brain and neck, headaches (in the afternoon), dizziness, and a slight loss of the ability to concentrate on the task or problem are observed.
- Second. Constricted blood vessels negatively affect the functioning of internal organs. The functioning of the genitourinary and motor systems is disrupted. The patient becomes more irritated, good mood becomes rare, and sometimes his heart hurts. The signs of the disease are clearly visible, but are short-lived, which is why patients attribute them to problems with the heart and kidneys, take appropriate medications and forget about the disease. Most often, patients who seek medical help complain about the appearance of stars and floaters in the eyes, numbness in the muscles of the legs, arms and face, tinnitus, weakness, impaired speech and vision, frequent urination and persistent headaches. Consciousness becomes confused, the skin of the face turns red, and memory deteriorates. The described symptoms last no more than 24 hours, after which they disappear.
- Third. The vessels are narrowed to the limit. The patient is unable to coordinate the movements of his own body, urination and defecation. Due to oxygen starvation, dementia develops, stupor and complete loss of working capacity are possible. Patients' hands, head and chin tremble, their eyes move regardless of their wishes, their face takes on an asymmetrical shape.
Treatment
In cutaneous vasculitis, the definitive cause of the disease is unknown. Therefore, complex therapeutic measures are used, aimed at different stages of the pathogenesis (development) of the disease. Required:
- rehabilitation of infectious foci - treatment of tonsillitis, caries, otitis media, cholecystitis and other inflammatory processes;
- correction of metabolic disorders, normalization of blood sugar levels, weight loss;
- antihistamines;
- preparations of vitamins C, PP, group B;
- calcium preparations;
- non-steroidal anti-inflammatory drugs;
- antibiotics (with a clear connection between the exacerbation of the process and an infectious disease).
In severe cases, methods of extracorporeal detoxification (“blood purification”) are prescribed - hemosorption or plasmapheresis, as well as glucocorticoid hormones with their gradual withdrawal.
In the chronic course of the disease, a rheumatologist may prescribe special medications, for example, delagil.
External treatment:
- for spots, papular rashes, nodules, dressings with hormonal ointments, for example, fluorocort, are indicated;
- for necrosis and ulcers, Vishnevsky ointments, solcoseryl, iruksol, and methyluracil are used.
During an exacerbation of the process, bed rest is necessary. In severe cases, especially those requiring the use of glucocorticosteroids, hospitalization in the rheumatology department is necessary.
Occupational disease
This is a disease that is accompanied by damage to small and medium-sized blood vessels. The degree of manifestation of symptoms depends on the form, stage and action of the provoking factor.
The mechanism of development of cutaneous vasculitis is as follows: neutrophilic leukocytes penetrate into the thinnest walls of blood vessels, thereby causing the process of necrosis (cell death). As a result, vascular permeability increases several times, and the patient notices hemorrhages of various sizes on the skin.
This pathology often develops due to a large accumulation of immune complexes on the walls of blood vessels, which constantly circulate in the blood and react to external irritants (allergic reactions, etc.).