Acute vulvitis in women is pronounced inflammatory processes occurring in the external genitalia. The symptoms of this disease are uncomfortable and can cause serious complications. Women of reproductive age suffer from the disease less often than girls before puberty and women of post-menopausal age. After the first signs of vulvitis appear, you should immediately visit a gynecologist. Timely therapy will help avoid relapses and complications.
Classification
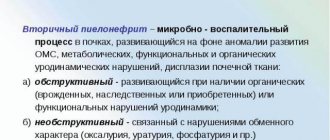
Inflammation of the vulva is classified according to various criteria: mechanism of development, type of course, nature of the inflammatory process, etc. When making a diagnosis, all these points must be taken into account, since this directly affects treatment tactics.
Depending on where the inflammatory process occurred - directly in the vulva or in adjacent organs - primary and secondary vulvitis are distinguished. The disease can have an acute or chronic course. There is also a subacute form, which is quite rare in middle-aged women and teenage girls.
According to the type of pathogen, candidal and bacterial vulvitis are distinguished; by nature - atrophic, allergic, ulcerative, adhesive, etc. These are the most common types of inflammation of the vulva, so we will briefly consider each of them.
- Candidiasis vulvitis occurs when Candida fungi multiply intensively, which are present in small quantities in the body of a healthy woman. The main symptom is the appearance of cottage cheese-like discharge. A plaque forms on the mucous membranes, a sensation of itching and burning occurs, which in acute forms is very strong. The disease has no age limit - women of any age suffer from this disease.
- Bacterial - this type of disease is provoked by pathogenic microorganisms. Chlamydia, gonococci, tuberculosis bacteria and others especially often affect the vulva in diseases of the endocrine system and a general decrease in immunity.
- Atrophic – women in the menopausal and post-menopausal periods most often suffer from the disease. A decrease in estrogen levels is reflected by excessive dryness of the skin and mucous membranes. As a result, this barrier begins to cope with its protective function much worse. Typical for this type of disease is a strong burning sensation and the formation of small but extremely painful erosions.
- Allergic – caused by exposure to an allergen, not necessarily on the skin or mucous membranes in the vulva area. Although the inflammatory process is most often a reaction to underwear (for little girls - diapers), hygiene products, cosmetics, it can also appear as a result of an allergy to a particular food.
- Ulcerative – this form of the disease is characterized by severe burning and tissue damage during scratching. First, plaque forms, and subsequently the injured surfaces become covered with erosion.
- Adhesive - a species found in childhood. With this form, gradual fusion of the labia occurs. One of the main signs is difficulty urinating in a child. The disease usually occurs against the background of hormonal problems.
There are also other types of vulvitis, such as radiation vulvitis, which occurs after the use of radiation therapy, leukoplakic, which is caused by kraurosis of the vulva, plasma cell, the formation mechanism of which has not yet been sufficiently studied. In adolescence, nonspecific vulvitis is often observed against the background of chronic infections and hygienic violations. An advanced inflammatory process leads to the formation of ulcers - in this case, a purulent form of the disease is diagnosed.
Causes
Depending on the reasons that contributed to the development of the pathology, vulvitis can be:
- Primary - the cause of this type of pathology is improper intimate hygiene, disruption of the endocrine system, burns and injuries in the groin area, cystitis, allergic reactions; less often, this form of vulvitis can form while taking antibiotics and hormonal drugs for quite a long time;
- Secondary - external manifestation of disorders of the internal genital organs; vaginitis, herpes and other pathologies are all provocateurs of the occurrence of this form of the disease.
One of the main causes of vulvitis, especially in women under 45 years of age, is the weakening of the body's defenses. Decreased immunity may be a consequence of a systemic bacterial or viral disease, long-term use of certain drugs (glucocorticoids, cytostatics), or a deficiency of essential vitamins in the diet. The risk of inflammation of the external genitalia increases with alcohol abuse and drug use.
Other causes of vulvitis are:
- diaper rash due to the characteristics of a woman’s constitution (for example, the formation of folds of skin on the external genitalia due to excess weight);
- injuries, scratches, scratching;
- dermatological diseases (psoriasis, eczema);
- allergic reaction to pads and intimate hygiene products, latex;
- wearing tight synthetic underwear;
- failure to comply with intimate hygiene rules;
- untimely replacement of tampons and pads during menstruation.
The risk of developing inflammation increases in the presence of concomitant diseases of the reproductive and endocrine systems (colpitis, vaginitis, diabetes mellitus). The occurrence of chronic or acute vulvitis is facilitated by disruption of the vaginal microflora. A similar situation can occur against the background of pregnancy, long-term treatment with antibiotics, taking incorrectly selected oral contraceptives, gynecological diseases accompanied by a decrease in estrogen production. Depending on the cause of the symptoms of vulvitis in women, gynecology distinguishes the following forms of the disease:
- Atopic vulvitis occurs in response to a specific reaction to an allergen that comes into contact with the external genitalia.
- Atrophic vulvitis mainly occurs in old age or in diabetes mellitus due to disruption of the structure of the mucous membrane.
- Candidal vulvitis is a consequence of the pathological proliferation of fungi of the genus Candida.
A bacterial form of inflammation is also isolated, which occurs under the influence of pathogenic microflora. It can also be caused by internal infections of the excretory system (cystitis, urethritis), fistulas between the bladder and vagina.
Causes
Most often, inflammation occurs under the influence of microorganisms. In the secondary type of infection, bacteria penetrate from adjacent organs. The primary form is characterized by external penetration - infection through scratching, injury, tissue damage during hygiene procedures, sexual intercourse, etc.
Among the most common causes of the disease, as well as factors contributing to the development of the inflammatory process:
- acute and chronic diseases of the genitourinary area;
- endocrine diseases;
- disturbances in the functioning of the immune system;
- helminthic infestations;
- hormonal imbalance;
- allergic reactions;
- long-term use of antibiotics, hormones, drugs that suppress the immune system;
- failure to comply with hygiene standards.
Too tight underwear, excessive sweating when overweight, oral sex, physical or chemical exposure, prolonged exposure to a humid environment - all this can trigger the development of inflammation. Cases of the disease are common during pregnancy, and in girls - during the transition period.
Causes of vulvitis in women
Inflammation of the vulva can be caused by the following reasons:
- Oral intimate relations;
- Sexual infections;
- Long-term use of hormonal and antibacterial drugs, which leads to weakened immunity. These drugs have an adverse effect on the vaginal microflora, as a result of which the level of conditionally pathogenic microorganisms increases;
- Malignant tumor neoplasms of the genitals that are in a state of necrosis or decay;
- Severe systemic diseases (thyrotoxicosis, cancer);
- Inflammatory processes of the reproductive organs and urinary tract;
- Worm infestations;
- Urinary incontinence;
- Formation of fistulas in the genitourinary system;
- Temperature (overheating, hypothermia), chemical damage to the genitals;
- Allergic reaction to personal hygiene products or items (gel, cream, soap, lotion, tampons, pads, etc.);
- Mechanical injury to the genitals during childbirth or rough sexual contact;
- Failure to maintain intimate hygiene.
In addition, vulvitis can develop due to a lack of estrogen in the blood.
Symptoms of the disease
Symptoms of the disease vary depending on the etiology. The intensity of symptoms depends on the severity of the processes occurring. Acute inflammation is characterized by pronounced signs. In chronic vulvitis, the symptoms are blurred, and only when the disease worsens is it accompanied by certain symptoms. Most often, patients complain of:
- vaginal discharge;
- itching;
- burning;
- pain in the area of the vaginal opening;
- plaque and plaques on the mucous membranes;
- swelling of the labia;
- redness of the affected area.
Sometimes the temperature rises, the inguinal lymph nodes enlarge, and general health worsens. Painful and other uncomfortable sensations intensify during sexual intercourse and urination. In some cases, erosions and submucosal compactions may form. Hyperemia can spread to the skin. Scratching often results in ulcers. In the acute form, especially in girls, sleep is disturbed and nervous excitability increases.
The nature of vaginal discharge varies depending on the pathogen. If the leucorrhoea has a curd-like consistency, candidiasis vulvitis can be suspected. With staphylococcal infection, yellow purulent discharge is observed. Watery, foul-smelling, yellow-green discharge is characteristic of the species caused by E. coli. In the chronic form, leucorrhoea is not so profuse and is not always accompanied by severe itching or burning.
Often, not just one pathogen, but a group, is involved in a disease. Therefore, without laboratory tests, it is impossible to prescribe adequate treatment based solely on medical history.
Symptoms of vulvitis in women
Inflammation of the vulva can occur in acute and chronic forms. Acute vulvitis develops rapidly, accompanied by pronounced symptoms:
- Swelling, redness of the vulva;
- Painful sensations in intimate places, which intensify during sexual intercourse, physical activity and urination;
- Burning, itching of the genitals;
- Enlargement of the sebaceous glands on the side of the labia majora;
- The appearance of bubbles in intimate places with liquid inside;
- Formation of plaques, plaque on the genitals;
- Enlarged inguinal lymph nodes (not always);
- Temperature increase.
Chronic vulvitis is accompanied by the same symptoms as the acute form, but is less pronounced. A characteristic sign of the chronic course of the pathology is the appearance of purulent vaginal discharge.
Diagnostics
A gynecological examination can reveal a number of changes typical for vulvitis, such as lesions of the mucous membrane, swelling, discharge, etc. In addition to examining the patient, to make a diagnosis, it is necessary to conduct a number of studies that will make it possible to identify the cause of the disease. In addition to blood and urine tests, the following is also prescribed:
- bacterioscopic and bacteriological examination of smears from the vulva, vagina, urethra;
- stool analysis;
- blood sugar test.
In some cases, other studies are also necessary (ultrasound of the pelvic organs, PRC, smear for gonorrhea, serological blood test, hormone tests, etc.). You may also need to consult other doctors (urologist, proctologist, oncologist, endocrinologist). When a pathogen is identified, its sensitivity to antibiotics is determined.
Types of vulvitis
Depending on the reasons for its development, vulvitis is divided into two groups:
- primary. Most often occurs in childhood or adolescence. Mainly the result of non-compliance with hygiene standards, reduced immunity, as well as exposure to chemical or mechanical irritants;
- secondary. Most often it occurs in women of reproductive age in the presence of other diseases, for example, vaginitis or endocervicitis.
Depending on the nature of the course, vulvitis is divided into:
- acute, which is characterized by pronounced clinical symptoms. As a rule, with timely, competent treatment, the clinical picture quickly disappears
- chronic – characterized by sluggish and prolonged signs of the inflammatory process.
We recommend! Fluconazole for thrush: dosage, course of treatment, reviews.
There are also specific and nonspecific vulvitis. The second type most often occurs in girls or elderly women and its causative agents can be protozoa, fungi, streptococci, staphylococci, and viruses. The specific form is caused by Trichomonas, chlamydia, and gonococci after penetration into the genitals.
Candidiasis vulvitis
Candidiasis vulvitis is a disease of the vulva, caused by yeast-like fungi of the genus Candida. Women of reproductive age are most susceptible to this disease. The main provoking factors for the development of candidiasis pathology are:
- use of broad-spectrum antibacterial agents. As a result, not only pathogenic microflora is suppressed, but also beneficial microorganisms. As a result, acidity increases, which is a predisposing factor for the activation of fungal infection;
- pregnancy period. Changes in hormonal levels provoke the spread of yeast-like fungi;
- use of oral contraceptives;
- synthetic underwear, etc.
In general, candidal vulvitis is not classified as a sexually transmitted disease. Fungal infection is classified as an opportunistic microflora. This means that fungi are normally present in our body and do not cause any problems.
Under the influence of certain factors that serve as a trigger, opportunistic microflora can begin to actively multiply, form entire colonies, leading to an inflammatory process.
To confirm the diagnosis, a gynecological smear examination will be required. First, a flora analysis is carried out, from which it will become clear whether a fungal infection is present. And then a bacteriological culture is done to determine the type of pathogenic microorganism.
Treatment of fungal vulvitis is aimed not only at eliminating the etiological factor, but also at combating provoking factors. Mild forms of the disease are treated with local drugs; sometimes it is advisable to combine them with systemic agents.
Allergic vulvitis
Allergic vulvitis is a disease of the external genitalia that occurs as a result of the irritating effects of allergens. As a rule, an increased reaction of the body occurs to such things:
- synthetic underwear. Dyes and synthetic fibers can cause severe irritation and inflammation;
- powders;
- Food;
- contact with condom lubricants;
- medications that come into contact with the mucous membrane of the genital organs: suppositories, ointments, creams, etc.;
- insect bites;
- low-quality diapers;
- the presence of pinworms;
- frequent douching;
- intimate hygiene products.
Often the allergic type of this disease is diagnosed in little girls. This can be explained by two main reasons, namely:
- the immune system is still at the stage of formation, which means it cannot properly resist attacks from allergens;
- The mucous membrane of the genital organs is thin, vulnerable and therefore can easily be damaged.
As for the clinical manifestations of the allergic form, in each individual case the situation can be diametrically opposite, ranging from a rapid course to an almost imperceptible manifestation. Also, the disease sometimes develops slowly, and in some cases - rapidly.
In most cases, allergic vulvitis manifests itself as follows:
- swelling and swelling of the genital organs;
- red spots and rash;
- plaques and plaques;
- discharge of purulent secretion;
- itching and burning;
- enlarged inguinal lymph nodes;
- low-grade fever;
- pain that increases with urination, sexual intercourse, walking;
- weakness, even loss of strength;
- irritability and nervous excitability.
Treatment of allergic inflammation is carried out in two main directions:
- identifying the allergen and protecting the patient from it;
- drug therapy. As a rule, the allergic form is combined with a fungal one, so doctors often prescribe antimycotic drugs. In addition, you cannot do without antihistamines, which effectively remove the manifestations of an increased reaction of the body.
Atrophic type of vulvitis
The atrophic form is characterized by a combination of an inflammatory process with simultaneous thinning of the mucous membrane of the genital organs. This is due to low levels of estrogen in the blood, for which the vulvar mucosa is the main target.
The pathology is most often diagnosed in women during menopause. Also, thinning of the mucous membrane is associated with excess weight. There are other reasons leading to atrophic changes in the vulva:
- microdamage;
- promiscuity;
- helminthic infestations;
- pathologies of the nervous system;
- infectious, viral diseases, etc.
We recommend! Treatment of thrush in men: drugs, prevention.
The mucous membrane begins to thin out long before the onset of the disease. All this is accompanied by severe dryness. The pathological process can be acute or chronic. The acute form is characterized by itching and burning, as well as pain when urinating. At the same time, the clitoris increases in size, and the sebaceous glands also increase.
If the atrophic type is combined with a fungal form, patients may experience abundant white, curd-like discharge from the vagina, irritating the mucous membrane. When combined with bacterial vaginosis, the discharge may become yellow or even green with an unpleasant odor.
The fight against atrophic changes in the mucous membrane involves the use of local or systemic hormonal agents. In addition, antiseptic and anti-inflammatory solutions are used. After conducting a microbiological study and identifying a specific pathogen, the doctor can decide on the advisability of using antifungal or antibacterial agents.
Treatment of vulvitis
The disease does not require hospitalization and can be cured at home. Usually, only in case of complications and concomitant diseases does the doctor decide on the need for inpatient treatment. The best results are achieved by an integrated approach, including:
- therapy aimed at destroying the infectious agent or eliminating another cause;
- local treatment (ointments, suppositories, lotions, compresses, douching, etc.);
- immunostimulating drugs;
- correction of diet, etc.
The selection of a treatment regimen in each case is carried out individually. Bed rest is indicated only for children. In case of complications in adults, semi-bed rest is prescribed. Until recovery, you must abstain from sexual intercourse and masturbation.
Drug treatment
For drug treatment of vaginitis, I use drugs aimed at destroying the causative agent of the disease. Usually antibiotics or antimycotic drugs are used for treatment. The former are prescribed for trichomonas, gonorrhea, and chlamydial infections, the latter for Candida infections. But in some cases specific treatment is required:
- antihistamines in combination with diet, if the cause of the disease is allergic reactions;
- hormonal agents and hydrocortisone ointment for local therapy for vulvitis caused by seborrheic dermatitis;
- estrogens for atrophic forms;
- antiparasitic drugs, if the disease is caused by the presence of worms;
- antiviral drugs if genital herpes is detected.
The most effective are drugs with complex effects (Terzhinan, Polygynax, Macmiror complex and others). They allow for faster subsidence of symptoms and complete cure (the relapse rate is very low). But for children, monocomponent drugs are usually selected.
Positive results are obtained by the use of physiotherapeutic procedures - electrophoresis with novocaine, ultraviolet irradiation. If fistulas form, surgery may be required.
ethnoscience
Among folk remedies, decoctions of medicinal herbs are most often used. They are used for douching, washing, lotions, compresses, and baths. The most effective decoctions are:
- chamomile;
- oak bark;
- nettle;
- St. John's wort;
- oregano;
- calendula.
Also, decoctions of medicinal herbs are used for internal use for chronic vulvitis in long courses (up to three months with a month's break).
In addition, alternative medicine recommends washing with a strong saline solution (dilute a tablespoon of sea salt in a glass of water). The affected mucous membrane is treated with a cotton or gauze swab dipped in the solution. But this recipe should not be used for severe damage. In these cases, a weak concentration of potassium permanganate solution – pale pink in color – or a solution of boric acid is preferable. But treating pathology on your own, without a preliminary examination and medical consultation, is categorically not recommended, and the possibility of using traditional medicine recipes should be agreed upon with your doctor.
Treatment of the disease
Treatment of vulvitis consists of eliminating the cause that causes the symptoms of the disease. If a woman has an acute stage of the disease, the gynecologist will recommend that she abstain from sexual activity and undergo treatment in bed. The disease can be treated with special medications that restore the microflora of the genital organs. In addition, the doctor will prescribe the patient to take baths that contain herbal decoctions, as well as solutions of chlorhexidine, potassium permanganate and other medications.
Treatment is complemented by taking a bath with herbal decoctions
Treatment of vulvitis requires the use of antibacterial drugs (creams, ointments), which are applied to the external genital area and also introduced into the internal organs (vagina). To completely cure a disease means to rid the patient of all unpleasant symptoms. It will be possible to say that a woman is completely healthy only after taking a second smear, in which no pathogens will be detected.
Often, women after menopause develop atrophic vulvitis. This disease is usually diagnosed at an appointment with a gynecologist. In some cases, the woman does not even make any complaints. Treatment of this disease should only be comprehensive - taking vitamins, baths with medicinal herbs, as well as treating the external genitalia with creams and ointments.
Treatment of vulvitis is also carried out with the help of vitamins (group E, C, A). Allergic vulvitis is treated using special antiallergic drugs. Also, in order to properly treat the disease, you need to eliminate allergens. For example, replace intimate hygiene products, soap and other cosmetics. If a woman has been diagnosed with allergic vulvitis, then she needs to choose hypoallergenic hygiene products. It is completely possible to cure this disease both in adolescence and postmenopausal age.
Complications
Vulvitis is not a life-threatening disease. However, you should not self-medicate and use exclusively traditional methods, since the disease often takes chronic forms. The presence of a constant source of infection can provoke the occurrence of other genitourinary diseases. Against the background of acute or chronic vulvitis, the following may occur:
- vulvovaginosis;
- endometritis;
- endocervicitis;
- colpitis;
- salpingitis;
- parametritis;
- urethritis;
- salpingo-oophoritis;
- bartholinitis.
Often the disease in question becomes the cause of adnexitis. In women of childbearing age, prolonged course of the disease without treatment can lead to infertility. During menopause, due to dryness, the mucous membranes are more easily injured, ulcers and blisters with purulent contents form.
In girls, vulvitis is fraught with the formation of synechiae - adhesions in the area of the labia minora. If the inflammatory process affects the hymen, it becomes deformed and thickens. When the opening of the hymen closes during the onset of menstruation, hematocolpos occurs (accumulation of menstrual blood in the vagina).
During pregnancy, pathology often causes urethritis and cystitis. The elasticity of tissues with this disease decreases, so during childbirth the risk of cracks and tears increases. In addition, it is possible for the child to become infected and subsequently develop various diseases in the newborn (pneumonia, conjunctivitis, etc.). Infants may suffer from dysbacteriosis and become sick more often in general due to reduced immunity.
The postpartum period in women with vulvitis is longer, and injuries received during childbirth take longer to heal. Therefore, it is important to treat the disease before childbirth.
Signs of the disease
The acute form of the disease in women is characterized by the following symptoms:
- hyperemia, swelling of the genital organs;
- discharge: purulent, watery, sanguineous;
- enlargement of regional lymph nodes;
- painful sensations that increase when walking, touching, urinating;
- severe itching, burning;
- the appearance of purulent blisters is possible.
Most often, acute vulvitis is characterized by copious discharge. The labia become bright red and become very swollen. This leads to discomfort while walking and pain when urinating. There is unbearable itching and burning in the area of the external genitalia. Patients with vulvitis experience rapid fatigue and possibly increased body temperature. Women feel some weakness. Sometimes small blisters are found on the surface of the genital organs, which are a consequence of the inflammatory process. Pus forms inside them.
Prevention
Among preventive measures, the most important place belongs to hygiene procedures. It is the low level of hygiene that often becomes the “culprit” for the development of the disease. But excessive enthusiasm for hygiene measures, especially with the use of cosmetics, also creates favorable conditions for the development of the disease.
Also for prevention it is necessary:
- carefully choose underwear, avoiding tight and synthetic ones;
- Always use condoms during casual sexual intercourse;
- strengthen immunity;
- restore microflora while taking antibiotics;
- Take care of a healthy diet, limiting fatty and spicy foods.
Since this pathology often occurs against the background of other genitourinary diseases, regular visits to the gynecologist (at least once every six months) are necessary even in the absence of complaints and any symptoms. It is also important to consult a doctor in a timely manner in case of exacerbation of existing chronic diseases. Vulvitis often “accompanies” relapses of genital herpes, so you should respond as quickly as possible when symptoms appear.
Be sure to visit a doctor and get examined after changing your sexual partner and having casual sexual contact without using protective equipment.
The highest risk group is postmenopausal women. It is especially important for them to monitor changes in their health and adjust their diet and lifestyle. This also applies to those with diseases of the endocrine system, in particular diabetes. The risk of developing pathology in girls is also relatively high. It is important to monitor the child’s genitals, change diapers regularly, and do not overuse soap during hygiene procedures to avoid drying out the mucous membranes. Older girls need to be taught daily hygiene and changing their linen. Having discovered any of the symptoms of pathology, the child must be shown to a pediatric gynecologist.
Exacerbation of acute vulvitis
Without timely treatment, acute vulvitis can cause unpleasant complications:
- development of chronic vulvitis, which relapses more often and is more difficult to treat;
- possible development of cervical erosion;
- lack of proper treatment can lead to infertility;
- the infection that caused vulvitis can spread to other parts of the genitourinary system;
- possible inflammation of the inner layer of the uterus, that is, the appearance of endometritis;
- in postmenopausal women, untreated disease leads to hypoxia of the vaginal walls;
- In girls, fusion of the labia - synechia - is possible.
To prevent complications, it is necessary to begin treatment when the first symptoms of the disease appear. Also, you should not treat acute vulvitis in women on your own. This can lead to negative consequences.
Traditional treatment methods
Treatment of vulvitis at home is carried out not only with medications, but also with folk remedies. For treatment, use prescriptions recommended by your doctor.
When carrying out treatment, several rules should be followed:
- avoid injury;
- avoid maceration of the vulva (for this reason, lotions, compresses, and irrigation with clean water are prohibited);
- for washing and douching it is necessary to use astringent antiseptic solutions;
- After water procedures, the vulva should be blotted with a napkin.
Drink
Patients must maintain a drinking regime. To do this, they are advised to drink plenty of warm fruit drinks and compotes made from:
- currants;
- dried fruits;
- cranberries;
- lingonberries.
Children's vulvitis in girls
Among gynecological infections in girls under eight years of age, vulvitis comes first. The primary type of disease is usually a consequence of the peculiarities of the anatomical structure of the genital organs. If little girls are bothered by long-term and recurrent inflammatory processes of the vulva, then in the future this may threaten menstrual irregularities, as well as problems with reproductive function.
The causative agents of the disease in girls can be:
- viruses;
- protozoa;
- fungi;
- gonococci;
- chlamydia.
Let's consider possible routes of transmission of infection:
- infection during passage through the birth canal;
- household way. This can happen in public places or when the rules of intimate hygiene are ignored;
- sexual contact.
As practice shows, vulvitis in girls often appears against the background of helminthic infestations. The problem can develop when foreign objects, such as a grain of sand or an insect, penetrate the genitals.
If we talk about the secondary type of disease, it can be caused as a result of the spread of an infectious process from other foci, for example, with tonsillitis or caries.
Vulvitis in girls is characterized by the appearance of white vaginal discharge. As a rule, they are transparent, but sometimes they can be mixed with pus or blood. If the causative agent is E. coli, the discharge may take on a green tint and have a characteristic fecal odor. And with a staphylococcal infection, they are yellow and viscous.
If the cause of the disease is pinworms, then the anal folds thicken, they become hyperemic, and abdominal pain occurs and appetite worsens. In some cases, the disease can lead to the appearance of general symptoms:
- swollen lymph nodes;
- temperature increase;
- sleep disturbance;
- nervousness and irritability.
Treatment of vulvitis in girls depends on the etiology. It includes a whole range of measures: proper diet, regimen, drug therapy.
Complications of vulvitis
Acute vaginitis, if left untreated, almost always becomes chronic, which often worsens, causing itching, burning, swelling, and an increase in the size of the sebaceous glands. In the acute form, erosions and ulcers may occur on the reproductive organs. In advanced cases, deformation of the vulva sometimes occurs, which is why the patient may experience difficulties in the intimate sphere in the future.
Girls who experience vulvitis in early childhood may experience fusion of the labia. In addition, in the absence of adequate treatment, vulvitis in girls can cause infertility in adulthood. This phenomenon is explained by some features of the body that are characteristic of this period. Therefore, when diagnosed with vulvitis, treatment should only be carried out by a gynecologist. In women, the inflammatory process usually affects only the external reproductive organs.
Methods for detecting the disease
For vulvitis, diagnosis begins with interviewing the patient. The diagnosis can be assumed based on the described clinical signs. This is followed by a mandatory examination in a gynecological chair. The doctor notes reddened and swollen external genitalia, pays attention to the condition of the skin of the perineum, vaginal discharge, its color, consistency and smell.
Further diagnosis of vulvitis is aimed at identifying its cause and possible concomitant diseases. For this purpose, a vaginal smear is taken from women and sent to the laboratory for bacterial culture and determination of the sensitivity of microorganisms to antibiotics. A urine test is also necessary to rule out kidney damage. If the nature of the discharge indicates a sexually transmitted infection, you need to donate blood for testing using the PCR (polymerase chain reaction) method to identify its causative agent.
A vaginal smear is taken from women and sent to the laboratory for bacterial culture and determination of the sensitivity of microorganisms to antibiotics.
In the presence of nonspecific vulvitis, it is necessary to examine the uterus, ovaries and fallopian tubes. For this purpose, an ultrasound of the pelvic organs is prescribed. For greater information content, it is advisable to carry it out using a transvaginal sensor. If cancer or benign formations are suspected, a PET (positron emission tomography) MRI or CT scan should be done.
Also, depending on the severity of the symptoms of vulvitis, the doctor makes a conclusion about the acute or chronic course of inflammation. This is of great importance in determining the tactics of further treatment. If the patient is sexually active, an additional test for hCG (human chorionic gonadotropin) is performed to confirm or exclude a possible pregnancy. The fact is that treatment of vulvitis often requires antibiotics, and many of them are toxic to the fetus.
Causes and prevention of vulvovaginitis in children
The development of vulvovaginitis in children is caused by the activity of nonspecific bacteria (staphylococci, streptococci, Escherichia coli, Klebsiella, Proteus), trichomonas (infection occurs through household contact) or fungi of the genus Candida. Not all children develop the disease. Before puberty, some mechanisms of nonspecific protection of the mucous membrane (acidic environment, the presence of bacteria of normal microflora, which include lactobacilli) are still absent, which makes them more vulnerable to the development of vulvovaginitis. There are several provoking factors, the influence of which significantly increases the risk of the inflammatory process, these include:
- Congenital decrease in immunity, which is determined by changes in the functional state of certain genes.
- Local or general hypothermia of the child.
- Poor nutrition with insufficient intake of vitamins and minerals into the body.
- Improper or insufficient intimate hygiene is the main provoking factor, leading to the fact that the incidence of vulvovaginitis is highest in girls aged 3 to 8 years.
- Infection with Trichomonas, which occurs when using someone else's personal hygiene items (washcloth, towel).
- A metabolic disorder in which glucose levels increase (diabetes mellitus type 1 or 2) and favorable conditions are created for the development of a bacterial or fungal infection. The situation is aggravated by the fact that against the background of metabolic changes, the functional state of the immune system suffers.
Knowledge of provoking factors helps to carry out effective prevention of vulvovaginitis in children. Measures aimed at preventing the development of the disease primarily include instilling in the child the ability to correctly carry out intimate hygiene procedures. It is also important to monitor the child’s nutrition, which should contain a sufficient amount of vitamins, minerals, complete proteins, and limit exposure to adverse factors, in particular general or local hypothermia. Preventive measures in childhood will help avoid the development of many diseases of the reproductive system in the future.
Treatment of vulvovaginitis in women
Despite the apparent frivolity of the disease, treatment cannot be ignored. It is compiled individually after laboratory and instrumental diagnostics and excludes surgical intervention. Treatment of vulvovaginitis consists of many stages and depends on the nature of the pathogen.
Antibiotics for vulvovaginitis
Antibacterial agents play a leading role in the treatment of pathology and are prescribed at any age. Depending on the need, medications can be in the form of tablets, ointments, suppositories, and powders for preparing solutions.
The most common groups of antibiotics are macrolides and penicillins. To reduce the risk of bacteria becoming addicted, different groups of antibiotics are taken alternately.
Treatment of little girls and adult patients who are not sexually active is not carried out with vaginal suppositories. Amoxiclav, cefazolin, ceftriaxone, azithromycin, nifuratel, metronidazole. Of ointments - based on tetracycline and erythromycin.
Antifungal agents
Antifungals are often combined with antibiotics. These can be two different drugs, or one that has the desired properties. Clotrimazole, fluconazole, miconazole, tioconazole, mycosist.
Probiotics
Bifidumbacterin, sporobacterin, acylact.
Hormonal agents
They are prescribed for a lack of the female hormone estrogen. Most often, older women suffer from this form of vulvovaginitis. This group of products normalizes the balance of acidity and microflora of the vaginal environment, restores blood supply and local immunity. Ovestin, estrinorm.
Antiseptics
This group of drugs affects not only the pathogen, but also eliminates itching in the intimate area and accelerates tissue healing. When applied topically, antiseptics are not harmful and are prescribed up to 5-8 times a day. Miramistin, nitrofural.
Antiviral
The causative agent of vulvovaginitis can be either an intestinal virus or a sexually transmitted one. If left untreated, the virus quickly spreads throughout the body and multiplies, reducing immunity.
Antiviral agents quickly activate defenses and suppress the action of the pathogen. Acyclovir, ribavirin, panavir.
Local treatment
These are mainly baths and douches. They have antipruritic, antifungal, anti-inflammatory and antiseptic effects. These are iodine preparations (iodoxide), tantum rose, solutions of boric acid and hydrogen peroxide.
Antihistamines
These drugs are prescribed if the cause of the disease is an allergen - food, cosmetic and hygiene products, composition of linen fabrics. Antihistamines eliminate swelling of the genital organs, their burning and itching. Suprastin, tavegil, clarotadine, loratadine.
Diet for vulvovaginitis
Much attention is paid to proper nutrition during treatment. If you follow a hypoallergenic diet, discomfort (burning, itching, swelling) goes away quite quickly. You need to use:
- Natural fermented milk products;
- Seafood;
- Liver, meat;
- Wild garlic, rose hips, viburnum, lingonberries, dried fruits;
- Oatmeal, wheat, buckwheat, barley;
- Nuts;
- Durum pasta.
- Food should not contain seasonings, pickles, or preserves.
- It is recommended to increase the volume of liquid you drink. It is better to drink homemade non-acidic compotes from rose hips and sea buckthorn.
Treatment of vulvovaginitis with folk remedies
Unconventional methods are quite popular and effective. But if the cause of vulvovaginitis is a sexually transmitted infection, then qualified medical intervention cannot be avoided.
- Garlic or onion tampons. Make a paste from one medium-sized onion (or a pair of garlic cloves), moisten sterile gauze in it and form a tampon. This tampon is placed in the vagina for 3-8 hours.
- Treatment of STIs and fungi in combination with pharmaceutical drugs can also be carried out with propolis. Propolis can be used either as a douche or as a suppository. For douching, you need to prepare 15 ml of a 5% alcohol solution of propolis, heat it to no more than 38 degrees. After the procedure, the vagina should be dried with gauze swabs.
- You can also prepare decoctions for oral administration or take a bath with them. They use chamomile, yarrow, birch and blackberry leaves, dandelion root, thyme, nettle, St. John's wort, peppermint, celandine, barberry shoots and others.
*****
The prognosis for vulvovaginitis is favorable. The disease is easily treatable, but the absence of relapses is possible only if the necessary hygiene is observed, diseases of the reproductive system are treated, and there is no frequent change of sexual partners.
Types of vulvitis, characteristic signs
Depending on what caused the disease, gynecologists distinguish several types:
Atrophic vulvitis - characterized by the appearance of small erosions that are difficult to heal. It is observed in women in menopause and is often associated with insufficient hydration of the vaginal mucosa (see photo above).
Fungal vulvitis - occurs due to an excessive amount of Candida fungi in the flora. It can be acute or take a chronic form. Most often, this type of vulvitis is observed in teenage girls. Treatment of the disease is quite complex and requires the participation of a competent specialist.
Atopic vulvitis is an inflammatory process that begins due to the influence of various allergens on the girl’s body. The reason is an incompletely matured immune system. The atopic form causes severe swelling of the vagina. The treatment plan should be developed together with an immunologist-allergist (see photo 2).
Adhesive vulvitis - affects girls of preschool age and is expressed in the fact that the labia minora gradually grow together due to problems with the endocrine system. In the early stages, the disease can be cured with medication, in more advanced cases - only with surgical intervention.
Treatment
Treatment of atrophic vulvitis always involves the use of hormonal drugs that have systemic or local effects. Regardless of the form of release, these medications are equally effective.
It is desirable that such treatment be carried out no later than 1.5–3 years after the onset of menopause.
Topical hormonal medications often include suppositories and ointments that contain estradiol. These medications are applied to the affected area or inserted into the vagina every day for 2 weeks.
In addition, doctors prescribe hormonal drugs to patients in tablet form. They should be taken without interruption for 5 years. They have a systemic effect and, in addition to treating atrophic vulvitis, relieve unpleasant symptoms of menopause, such as hot flashes and mood swings, stop hair loss, and have a positive effect on the condition of the skin.
In order to cure vulvitis, you need to treat the vagina and vulva with antiseptic and anti-inflammatory solutions. For the same purpose, you can use various suppositories, creams, gels, ointments and sprays.
After the causative agent of the disease has been identified and its sensitivity to drugs has been determined, the doctor prescribes antifungal or antibacterial drugs. These drugs can also be available in different forms.
If vulvitis is caused by an allergic reaction, antihistamines may be prescribed.
When diagnosed with atrophic vulvitis, treatment should also include therapy for any infectious, inflammatory or viral diseases, especially chronic ones with a long course.
In addition, to relieve symptoms of the disease, your doctor may recommend sitz baths with the addition of medicinal solutions or decoctions of anti-inflammatory herbs (such as chamomile or sage).
After treatment is completed, it is recommended to undergo a course of vitamin therapy and, if necessary, a course of immunostimulants. It is also recommended to use vaginal suppositories or tablets containing lactobacilli.
While treatment is being carried out, a woman should exclude sexual intercourse and adhere to a special diet, which involves giving up alcohol, fatty, sweet, spicy foods and, conversely, including a large amount of vegetables, fruits, proteins and lactic acid products in the diet.
After the course of treatment, the doctor examines the woman to determine the maturity of her epithelium. In addition, the Ph of her vaginal discharge is determined.
Atrophic vulvitis is one of the most unpleasant manifestations of the menopause. With a timely visit to a gynecologist, a woman will be able to avoid not only negative changes in the sexual sphere, but also significantly reduce the risk of developing cardiovascular diseases, and prevent increased leaching of minerals from bone tissue, leading over time to osteoporosis.
When adequate therapy is prescribed, the prognosis of the disease is very favorable.
Products for baths, douching, irrigation
- Oak bark extract. Add 2 tablespoons of raw material to 2 liters of water, let it boil, and simmer for 10 minutes. After cooling, the broth is filtered. It is added to baths and used for douching. Take a sitz bath for 20 minutes.
- For candidiasis vulvitis, take soda baths (a tablespoon of soda per 1 liter of water). The duration of the procedure is 20 minutes. Douching is done with a soda solution, and used for washing (1 teaspoon of product per 1 liter of liquid). Treatment lasts 7–10 days.
- Rhizomes of Potentilla erecta. Add a tablespoon of raw material to 250 ml of boiling water and simmer for 10 minutes. The cooled broth is filtered and diluted with boiled water, bringing the volume to a liter. Douche twice a day.
- Chamomile helps fight inflammation of the vulva. Place a tablespoon of herbs in 1 liter of boiled water and allow to cool. The filtered infusion is used for douching or irrigation.
- Infusion of round-leaved wintergreen. Take 2 teaspoons of the plant, pour a glass of boiling water, and filter after two hours. Douche with infusion and wash off.
- Remove the skins from four onions, put them in 0.5 liters of water, let them boil, and simmer for 15 minutes. Cool and filter. Used for irrigation.
- Treatment is carried out using calendula decoction. Dip a tablespoon of marigolds into 1 liter of boiled water and let it sit. The solution is used for douching when it turns golden.
Therapeutic tampons
Vulvitis in women is effectively treated when tampons soaked in antiseptics are used. The procedures are carried out as follows:
- The tampon is dipped in liquid honey, allowed to soak and inserted into the vagina. Removed after half a day. They are treated for two weeks.
- A tampon soaked in sea buckthorn oil is inserted into the vagina before bed. They clean it up in the morning. The oil is also used to treat the labia.
- Peach oil helps with illness. They make tampons with it and lubricate the vulva.
Herbs for internal use
If vulvitis occurs, treatment at home is carried out using decoctions and infusions taken orally. They strengthen the immune system, suppress inflammation, soothe, relieve itching and burning .
- When chewing white acacia flowers, a juice is released that can relieve the symptoms of the disease.
- To eliminate the inflammatory process, use a decoction of viburnum. Place a tablespoon of viburnum leaves in 200 ml of boiling water and simmer for 10 minutes. The cooled and filtered product is consumed in a tablespoon three times a day.
- Strengthens the immune system, relieves symptoms, a collection prepared from coltsfoot, wintergreen, sweet clover (1:1:1). Add a tablespoon of the mixture to 200 ml of boiling water and simmer for 15 minutes. Cool, filter, consume a tablespoon three times a day.
- Mix valerian, lemon balm, mantle and nettle in a ratio of 2:2:3:3. Brew 2 tablespoons of herbal mixture in 1 liter of boiling water. After five hours, filter. The entire infusion is drunk per day, consuming 100 ml at a time. For treatment, a fresh infusion is made daily.
If vulvitis occurs, the symptoms and treatment are determined by the gynecologist. Self-medication is not always effective. Sometimes the result is a deterioration of the condition and the development of complications. Complex therapy helps to quickly cope with the disease: the simultaneous use of medicines and folk remedies.
Clinic and symptoms
The disease is caused by pathogenic bacterial flora, usually penetrating from the vagina. The woman is concerned about swelling, itching, burning, redness of the folds of the perineum and vaginal opening. The course of vulvitis can be acute, subacute and chronic.
Acute inflammation occurs with accompanying symptoms:
- severe pain in the perineum, aggravated by touch, friction of clothing, as well as during intimate contact;
- copious mucous vaginal discharge;
- plaque with an unpleasant odor that accumulates in the folds of the labia minora;
- the skin around the vulva is hyperemic, ulcerative lesions are present;
- the presence of pain during the entire process of urination;
- in severe cases - enlarged lymph nodes in the groin area.
Subacute vulvitis is a precursor to the acute form and has similar, but less aggressive symptoms. It is at this stage that many women turn to the doctor with characteristic complaints.
The chronic form of vulvitis is sluggish: redness, burning and pain subside after treatment, but over time the symptoms return. Such “swings” continue for a long time, sometimes throughout life. A chronic disease often develops against the background of self-medication, when a woman, without consulting a doctor, “prescribes” medications to herself and uses inappropriate methods of traditional therapy.
Typically, inflammation of the external genitalia is not a separate disease, but occurs as a result of another pathology of an infectious nature (see list below). In this case, the inflammation is called “ secondary vulvitis ”.
- Vaginitis is an inflammation of the vaginal mucosa that occurs as a result of external bacterial infection and is manifested in the laboratory by an imbalance of microflora and the presence of pathogenic microbes in the smear. If vulvitis develops against the background of vaginitis (which is not uncommon), then the disease is called vulvovaginitis. Most often, the causative agent is streptococcal, staphylococcal, gonococcal infectious agents, as well as other equally dangerous bacteria - chlamydia, mycoplasma, Treponema pallidum, etc. Typically, pathogenic flora enters the vagina due to unprotected sexual intercourse. Also, the disease is often recorded in women who do not adequately perform cleansing procedures of external organs, wear tight clothes and do not use sanitary pads according to the rules (they need to be changed every 3-4 hours). Sometimes vulvovaginitis develops against the background of long-term antibacterial treatment and even becomes a complication of type 2 diabetes.
The nature of secretory discharge during vaginitis depends on the pathogen that caused the disease. Thus, mucus can be watery, thick or foamy, sometimes with whitish or curd-like inclusions. There is almost always a pronounced unpleasant odor. The color of the discharge is dirty white, yellow-gray, gray, sometimes with a green tint.
- Inflammation of the upper reproductive organs - the cervix and body of the uterus, fallopian tubes, ovaries. Diseases – cervicitis, endocervicitis, endometritis, salpingitis, oophoritis. With these pathologies, a woman experiences nagging pain above the pubis, heavy periods, in addition there is a disturbance in menstrual cyclicity, spotting in the middle of the cycle, and fever. Infection can occur as a result of abortion, childbirth, operations on the pelvic organs (caesarean section, classic resolution of tubal pregnancy, removal of the uterus, ovaries, etc.), as well as hypothermia against the background of reduced immunity.
The above pathologies are serious! Incorrect and untimely treatment can transform the disease into an aggressive form. This is fraught with many negative consequences, such as secondary infertility, a tendency to form benign and malignant tumors.
Photo
Click to see photo (18+)