- Causes
- Symptoms and signs of endometritis
- Diagnostics
- Treatment of endometritis
- Prevention
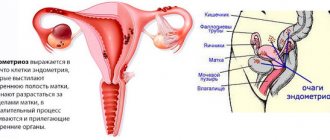
Endometritis is an inflammation of the lining of the uterus. According to the nature of the course, acute and chronic endometritis are distinguished. Treatment tactics will depend on the form of the disease, as well as the presence of one or another concomitant pathology at the time of diagnosis.
Acute endometritis is an acute inflammatory lesion of the endometrium (the inner mucous layer of the uterus). When the pathological process spreads through the blood and lymphatic vessels, metroendometritis develops and then pelvioperitonitis (inflammation of the pelvic peritoneum).
Chronic endometritis is a long-term, sluggish inflammation of the uterine mucosa. Arises as an outcome of inadequate treatment of acute endometritis. It is possible that primary chronic endometritis may develop without previous symptoms of acute inflammation.
Causes
Causes of acute endometritis
Acute endometritis is found in 2% of all gynecologist patients. In every tenth woman, the disease is combined with damage to other pelvic organs (ovaries, fallopian tubes, peritoneum).
Endometritis occurs when the lining of the uterus becomes infected. The causative agents of the disease most often are representatives of opportunistic flora (Escherichia coli, enterobacteria, etc.). Infection with chlamydia, mycoplasma, and ureaplasma is possible. In recent years, mixed infection (simultaneous infection with several microorganisms) has become increasingly common.
Risk factors for developing endometritis:
- any interventions in the uterine cavity (abortion, diagnostic and therapeutic curettage);
- complicated childbirth;
- general infectious diseases;
- infections of the lower genital tract (vagina and cervix).
- installation of an intrauterine device.
Once in the uterine cavity, pathogenic microorganisms provoke the launch of complex reactions leading to the development of inflammation. In such conditions, the uterus cannot fully function. All the symptoms of endometritis occur, forcing the woman to seek help from a doctor. Untreated acute endometritis can progress to the chronic stage and even cause infertility.
Causes of chronic endometritis
Chronic endometritis most often occurs as a natural result of sexually transmitted diseases. The disease develops against the background of reduced immunity and vaginal dysbiosis. The biocenosis is disrupted, the proportion of beneficial lactobacilli on the mucous membrane of the genital tract decreases, and the content of pathogenic and conditionally pathogenic microorganisms increases. Against this background, inflammation develops, which leads to the appearance of all the symptoms of chronic endometritis.
Chronic inflammation of the uterus after childbirth and abortion is a consequence of untreated acute endometritis. The risk of chronicity of the process increases after repeated interventions in the uterine cavity. In rare cases, the cause of chronic endometritis is suture material left after a cesarean section or other operations.
Cervical erosion
Cervical erosion is a kind of violation of the integrity of the epithelium that lines the vaginal part of this organ. This disease is one of the most common gynecological pathologies. Its danger lies in the fact that without the necessary treatment, this defect can lead to the occurrence of polypous growths or malignant degeneration.
Cervical erosion can form both as a result of mechanical damage and under the influence of internal factors. Violation of the integrity of the epithelium often occurs as a result of sexual intercourse, surgical termination of pregnancy, and other medical procedures. In addition, various infectious diseases of gynecological organs, endocrine disorders, difficult childbirth can also cause the development of such pathology.
With cervical erosion, any symptoms rarely occur. In most cases, this pathological process is discovered accidentally during a gynecological examination. However, if the defect is large, women may complain of spotting that is not associated with menstruation. In some cases, there is pain, which intensifies during sexual intercourse.
Symptoms and signs of endometritis
Symptoms of acute endometritis
The first signs of endometritis appear 3-7 days after infection enters the uterus (for example, after childbirth, abortion or other interventions). Typical symptoms of acute endometritis include:
- fever;
- pain in the lower abdomen;
- purulent vaginal discharge;
- bleeding.
The disease begins with a sharp increase in body temperature to 38-40 °C. Chills, severe general weakness, and loss of appetite appear. The inguinal lymph nodes are enlarged. Against the background of high body temperature, nagging pain occurs in the lower abdomen. The pain radiates to the lower back and tailbone, shoots to the groin area. The discomfort disappears after taking analgesics.
Discharge from the genital tract in acute endometritis is profuse, purulent, dirty gray, yellow or greenish in color. Blood may appear. The discharge has an unpleasant, pungent odor. By the nature of vaginal discharge, the causative agent of the disease can be determined.
Acute endometritis after an abortion or miscarriage has its own characteristics. 5-7 days after curettage of the uterine cavity, the woman’s condition deteriorates sharply. The temperature rises, severe pain occurs in the lower abdomen, and bleeding develops. Endometritis in this case is associated with retention of the fertilized egg in the uterine cavity. In severe cases, pyometra (accumulation of pus in the uterus) develops.
Symptoms of chronic endometritis
Chronic endometritis is asymptomatic for a long time. A woman may never find out about her disease until she gets examined by a gynecologist. Over time, the following symptoms appear:
- constant aching pain in the lower abdomen;
- menstrual irregularities.
Cycle disturbances manifest themselves in the form of irregular uterine bleeding. Bleeding can be of varying intensity, from spotting brown discharge in the middle of the cycle to copious discharge. It is very common for minor discharge to appear a few days before the expected menstruation, as well as shortly after it. Menstruation with chronic endometritis becomes profuse and painful.
With hidden chronic endometritis, a woman’s only complaint is the inability to conceive a child. The inflamed mucous membrane of the uterus does not accept the fertilized egg, causing miscarriage in the very early stages. Ectopic pregnancy often develops against the background of endometritis.
Endometrium during menopause
Endometrial hyperplasia often has no symptoms. If you have menstruation, when the body has not yet completely entered the menopause, there may be a cycle disruption. Most often, women during menopause notice bloody discharge. Sudden sharp pains during menopause are also typical.
During the postmenopausal period, the endometrium should be less than 4 millimeters. If the thickness is within 6-7 millimeters, laboratory tests are carried out within 6 months. If the thickness is more than 8 millimeters, the process is pathological.
Diagnostics
Diagnosis of acute endometritis
If you suspect acute endometritis, you should urgently consult a gynecologist. Acute inflammation of the uterus is a condition dangerous to the health and life of a woman. The sooner treatment is started, the greater the chances of a favorable outcome of the disease.
Diagnostic scheme:
Gynecological examination
When examined on a gynecological chair, an enlarged, painful uterus attracts attention. The cervical canal is slightly open. With late miscarriages and endometritis arising as a result, the cervix allows one finger to pass freely.
Laboratory examinations
To diagnose endometritis, the doctor prescribes the following tests:
- general blood analysis;
- general urine analysis;
- smear on vaginal flora;
- bacteriological culture from the cervical canal.
Based on the results of the examination, the doctor can assess the severity of the woman’s condition, as well as identify the causative agent of endometritis. Therapy is selected taking into account the microorganisms found during the examination.
Ultrasound
An ultrasound examination allows you to assess the size of the uterus and the condition of neighboring organs. Ultrasound also reveals retention of parts of the fertilized egg or placenta (after abortion, miscarriage and childbirth).
Diagnosis of chronic endometritis
The diagnostic scheme for chronic endometritis includes:
Gynecological examination
When examined in mirrors, concomitant cervicitis (inflammation of the cervix) is often revealed. With chronic endometritis, the uterus is dense, painful, and slightly enlarged.
Laboratory research
To detect the causative agent of the disease, a smear is taken for flora and bacteriological culture from the cervical canal. This study allows you to identify the causative agent of the disease and determine further tactics.
Instrumental studies
Ultrasound of the pelvic organs is not very informative. To diagnose chronic endometritis, hysteroscopy is performed - an examination of the uterine cavity from the inside under passion. All information is displayed on the screen, and the doctor assesses the condition of the uterine mucosa. During the procedure, a section of the endometrium is taken for analysis. The final diagnosis is made only after receiving the results of histological examination.
Treatment of endometritis
Treatment of acute endometritis
Treatment of acute endometritis is possible only in a hospital. For the entire period of therapy, bed rest, rest and proper sleep are prescribed. It is recommended to take multivitamins and an easily digestible diet. After the symptoms subside, the woman is discharged home under the supervision of a local gynecologist.
Drug treatment of acute endometritis involves taking antibiotics. Antibacterial drugs are prescribed taking into account the identified pathogen. The most commonly used are cephalosporins - broad-spectrum antibiotics that are effective against most known pathogens of endometritis. Cephalosporins can be combined with macrolides and other antibacterial drugs.
The course of antibacterial therapy lasts 7-10 days. According to indications, antispasmodics (drugs that relax the muscles of the uterus) and painkillers are used. After completing the course of antibiotics, agents are prescribed to restore normal vaginal microflora (probiotics).
Surgical treatment of acute endometritis is carried out after an abortion or complicated childbirth. Curettage of the uterine cavity is performed, and the remains of the fertilized egg or placenta are removed. After surgery, broad-spectrum antibiotics and analgesics are prescribed. To restore menstrual function, physiotherapy is indicated after the acute process has subsided.
Treatment of chronic endometritis
Treatment of chronic endometritis is carried out on an outpatient basis. Antibiotics are prescribed taking into account the identified pathogenic microorganisms. Physiotherapy is prescribed to normalize the menstrual cycle. A course of vitamins and agents that stimulate general and local immunity is indicated.
Surgical treatment is carried out in the presence of intrauterine synechiae - special cords that form in the uterine cavity due to chronic inflammation. These cords interfere with the conception of a child and the normal course of pregnancy, and also cause constant pain in the pelvic area. Intrauterine synechiae are divided during surgery. Recently, most operations on the uterus are performed laparoscopically (through small punctures, without an incision).
Hyperplastic processes of the endometrium: causes and remedies
Endometrial hyperplasia is a process in which pathological growth of the mucous layer of the uterus occurs. There are main groups of reasons.
- Hormonal disorders. Increased estrogen levels with decreased progesterone activity. This can be caused by ovulation disorders, hormone-producing ovarian tumors, dysfunction of the pituitary gland, pathology of the adrenal cortex, and uncontrolled use of hormonal drugs.
- Exchange-endocrine disorders. Pathology of fat metabolism, diseases of the gastrointestinal tract, dysfunction of the thyroid gland lead to disturbances in the metabolism of sex hormones. Obesity, arterial hypertension, and diabetes mellitus are often combined with hyperplastic processes in the endometrium.
- Chronic inflammation. Leads to damage to receptors located deep in the mucous layer. Endometrial receptors cease to perceive hormonal impulses and give an adequate response. In 95% of patients with glandular fibrous polyp, the endometrium is infected or there are signs of chronic inflammation.
Depending on the prevalence of the process, focal (endometrial polyp) and diffuse endometrial hyperplasia are distinguished.
How to suspect pathology
The main symptoms of endometrial hyperplasia are uterine bleeding, mostly irregular and not coinciding with the menstrual cycle. Often women of reproductive age come with infertility problems. Endometrial hyperplasia in menopause may not manifest itself in any way and may be an accidental finding during ultrasound examination.
Despite the paucity of clinical symptoms, endometrial thickening cannot be considered a harmless condition. Glandular endometrial hyperplasia without atypia can develop into cancer in 3% of cases, and atypical hyperplasia in 29%. Adenomatous polyps are classified as precancerous conditions. Endometrial hyperplasia and deterioration of general condition due to bleeding are dangerous.
Diagnostic standards
A screening examination that allows mass coverage of the target group is a transvaginal ultrasound examination. In women of reproductive age, it is worth assessing the correspondence between the thickness of the endometrium and the phase of the menstrual cycle. At the menopause stage, the thickness of the mucous layer should normally not be more than 4-5 mm.
However, echographically it is possible to diagnose only thickening of the endometrium, but it is not possible to differentiate glandular hyperplasia from atypical one. Therefore, a reliable diagnosis is possible only after histological analysis of the affected endometrium. To do this, diagnostic curettage or hysteroscopy with biopsy is performed.
Therapeutic techniques
Therapy for endometrial hyperplasia includes the following main tasks:
- stop the bleeding;
- restore menstrual function during childbearing years;
- achieve endometrial atrophy during menopause;
- prevention of relapses of hyperplasia.
Traditionally, after histological examination of the endometrium, hormonal therapy is prescribed. Its purpose is to normalize the regulation of the thickness of the mucous layer of the uterus. It is necessary to take into account the possible infectious component of the disease, so antibacterial therapy is sometimes used.
If the disease recurs, then a woman who has already given birth to a sufficient number of children and is not planning a pregnancy in the future may be offered endometrial resection.
With reliably determined atypical hyperplasia, removal of the uterus is indicated for women in menopause. If surgery is not possible due to severe general somatic pathology, then treatment consists of long-term use of gestagens.
Is it possible to treat endometrial hyperplasia without curettage? Treatment itself is possible, but curettage is often necessary for a correct diagnosis. However, recently hysteroscopy has been increasingly used as a more accurate and informative procedure.
Prevention
Prevention of acute and chronic endometritis includes:
- Refusal of casual sex.
- Using barrier methods of contraception (condom) to protect against infections.
- Careful management of childbirth.
- Rehabilitation after miscarriages, abortions and any interventions in the uterine cavity (antibacterial therapy, physiotherapy, restoration of vaginal microflora).
- Compliance with the rules of intimate hygiene.
- Timely consultation with a doctor when the first signs of the disease appear.
- Strengthening the immune system.
If all recommendations are followed, the risk of developing endometritis is minimized. If the problem cannot be avoided, it is necessary to undergo examination and treatment by a gynecologist as soon as possible. With timely therapy and proper rehabilitation, the prognosis is quite favorable.