What is cervical parakeratosis?
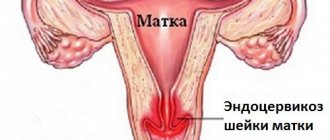
Doctors do not consider parakeratosis to be a separate disease. In their opinion, it is a sign of other various pathologies of the cervix. The disorder appears in conjunction with hyperkeratosis and acanthosis:
- Hyperkeratosis is characterized by epithelial keratinization. When everything is normal with the cervix, its epithelium does not keratinize at all. Hyperkeratosis causes the formation of glycogen-deprived scales.
- As for acanthosis, in addition to the same thickening of the epithelium, it is typically characterized by an increase in the length of the interpapillary processes.
Most often, this trio of pathologies is observed in patients with the dangerous precancerous disease leukoplakia.
Causes
Parakeratosis can be caused by both internal (related to the physiological characteristics of the body) and external factors. The most common causes of the disease are:
- chronic inflammatory processes caused by bacterial and viral pathogens that are transmitted during sexual intercourse. The main ones are chlamydia, mycoplasma, as well as viruses that cause the appearance of papillomas, the development of herpes and ureaplasmosis;
- operations on the uterine cervix, childbirth and intensive medical procedures with elements of surgical intervention;
- acute lack of zinc in the female body;
- serious hormonal problems, especially those caused by high levels of estrogen and lack of progesterone;
- pituitary dysfunction;
- pathological lack of ovulation;
- problems with immunity caused by the immunodeficiency virus (HIV), chronic diseases of the hematopoietic organs (primarily the liver), clinical depression and “unsparing” starvation diets;
- repeated artificial termination of pregnancy (including in the early stages), frequent miscarriages;
- uterine curettage (curettage), which was carried out for diagnostic purposes (to take a sample for analysis);
- violation of the rules of “vaginal” hygiene;
- radical methods of getting rid of uterine erosions (through electropenetration, cauterization);
- incorrectly installed or low-quality contraceptive device;
- various types of displacement of internal organs (ectopia). Especially those with whom relapses often occur;
- extreme sexual practices, such as fisting (stimulation of the vagina with a hand clenched in a fist), the use of overly large dildos for self-satisfaction, rough, very fast sex;
- inflammation of the mucous membrane of the cervix (exo- and endocervicitis), as well as inflammatory processes in the vaginal mucosa (vaginitis).
In addition, parakeratosis can be caused by severe emotional overload, chemotherapy and poor ecology.
Symptoms
In the initial stages, it is not easy to identify parakeratosis, since it does not cause any special symptoms. That is why it is extremely important for preventive purposes to visit a gynecologist at least once a year. Only he will be able to visually determine changes in the epithelium on the cervix and establish through examinations and tests whether this is a separate pathology or a sign of a more serious disease compared to parakeratosis.
Often parakeratosis is poorly visible against the background of pronounced manifestations of the disease that caused it. This happens especially often with infectious diseases, which are usually accompanied by pain or fever. These symptoms “muffle” the signs of parakeratosis. However, the pathology may be more noticeable. In such a case, parakeratosis is characterized by the following symptoms:
- discharge of blood after sexual intercourse during the non-menstrual period. As a rule, it stands out a little;
- unpleasant painful sensations during coitus;
- increased (slightly) amount of vaginal secretion. At the same time, its smell is unpleasant, or at least not the same as always.
Thus, even signs of pronounced parakeratosis are not always noticeable. Only special diagnostics can identify them.
How is the diagnosis carried out?
Due to the insidiousness of the disease, which develops asymptomatically, its diagnosis is associated with certain difficulties in a multi-stage examination, as well as obtaining information about hereditary pathologies. After interviewing the patient, clarifying the number of births and the quality of abortions, the presence of inflammation and previous infectious diseases, and the use of contraceptives, the stages of a traditional examination of the woman begin.
Standard chairside examination
Thanks to the use of a mirror system, the doctor has the opportunity to visualize the condition of the epithelial surface of the cervix.
During a vaginal examination, the gynecologist pays attention to the following aspects:
- damage to the surface of the cervix;
- uniform color of the mucous layer;
- homogeneity of tissue structures.
If, during examination of the surface of the cervix, traces of white spots are detected, colposcopy will be required. The scraping material is necessary for a more detailed study of the epithelium, identifying signs of pathology, and determining its stage.
Taking tests
Laboratory examination of samples for suspected cervical hyperkeratosis is necessary to confirm the preliminary diagnosis.
What tests does the patient undergo:
- the PCR test helps to identify infectious and hereditary pathologies that progress in acute or chronic form;
- cytological testing of PAP, doctors call it a Pap smear, can detect the presence of atypical cellular structures;
- thanks to bacteriological inoculation of the leucorrhoea material, the type of pathogenic microflora of the sample is established;
- to identify the human papillomavirus, called HPV, as well as its type, a smear is taken to conduct a polymerase chain reaction (PCR test);
- During colposcopy, material is taken for a biopsy, which makes it possible to detect traces of dysplasia, as well as the degree of its severity.
A mandatory procedure is donating blood and urine for a general examination and determination of biochemical parameters. Thanks to blood sampling, the patient’s Rh factor and the level of sex hormones are determined.
If, based on the results of colposcopy, the doctor receives information about the localization of changes and the nature of the lesion, then the process of cytological examination of the smear makes it possible to determine whether leukoplakia belongs to a certain type.
Hardware diagnostics
The patient needs to receive the results of an instrumental examination, including radiography to identify associated problems, as well as ultrasound testing using transvaginal access. This type of ultrasound is characterized by maximum accuracy compared to traditional ultrasound through the abdominal wall, and allows you to accurately detect compactions in the cervical tissue.
Diagnostics
To make a correct diagnosis, the gynecologist must know about all the operations the patient has undergone, illnesses, the frequency and nature of her sexual contacts, and her lifestyle.
Full screening includes 4 mandatory procedures:
- Oncocytology.
- Liquid cytology.
- Colposcopy.
- Histological examination.
Parakeratosis is very similar to pseudoparakeratosis - severe cell atrophy, which often ends in the appearance of neoplasms. Therefore, in order to make sure that the cervix is affected by parakeratosis, it is important to undergo all 4 screening procedures.
Liquid cytology
Using a cytological examination, cells taken from the mucous membrane of the cervix are checked for the presence of pathologies. The liquid research method includes the following steps:
- A sample of cells taken from the cervical mucosa is placed on a special membrane.
- Then several special manipulations are performed with them to create a smear for analysis - staining, dispersion, and mixing. In this case, a special stabilizing solution is used.
- Next, a microscopic analysis is carried out for the presence of pathologies.
Liquid-based cytology is considered a fairly accurate way to identify problems at the cellular level.
Oncocytology
Using oncocytology of the uterine cervix, it is determined whether the patient has cancer cells or benign neoplasms. The research technique is in many ways similar to conventional cytology (including liquid cytology).
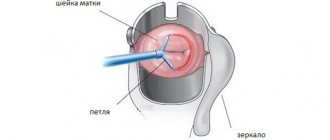
Colposcopy
Using the colposcopic method, a specialist determines the exact location and size of the diseased area. A colposcope allows you to detect even microscopic pathological changes in the cervical mucosa.
Treatment
Treatment of parakeratosis has two goals:
- Getting rid of himself. To cure the disease, you will have to take antimicrobial anti-inflammatory drugs. It is not recommended to treat parakeratosis with various “folk” remedies (baths, tampons, syringes). Such therapy is ineffective and sometimes even harmful.
- Elimination of all foci of the disease. Methods for their elimination may vary. It all depends on whether the patient has signs of an incipient malignant or benign tumor. Standard methods for eliminating areas with parakeratosis are:
- vaporization (evaporation) using a laser;
- diathermocoagulation (cauterization with electric current);
- destruction by cold (cryodestruction using liquid ultra-cold nitrogen);
- argon plasma coagulation (using argon gas plasma);
- invasive intervention. It includes amputation, as well as conization (removal of a cone-shaped area). Invasive intervention is used only if focal parakeratosis begins to develop into precancerous leukoplakia, a neoplasm or cicatricial deformity appears.
It is not necessary to eliminate lesions if there are no traces of an incipient neoplasm, and the areas affected by the disease occupy a small area. In this case, simple treatment of parakeratosis with pharmaceuticals will suffice.
Preventive measures
- Those who have overcome parakeratosis or who do not want to get it should take medications that contain zinc. In this case, she will not have to deal with this unpleasant pathology;
- is at greater risk of developing parakeratosis than others if she has problems with the endocrine system or has had surgery on the uterine cervix. Such a lady should be especially picky about her sexual partners, since any sexually transmitted infection can lead to illness. Also, she should not randomly take the first hormonal drugs she comes across. This should only be done after consulting a doctor.
In order to avoid parakeratosis, you need to follow these simple rules:
- Be sure to get vaccinated against papilloma virus (HPV infection).
- Minimize unprotected sex with an “unverified” partner.
- Do not forget about sexual hygiene - wash your intimate organs daily (best with herbal decoctions).
- Swim in excessively hot water as little as possible.
- Visit your gynecologist regularly.
- Do not smoke and try not to passively inhale smoke.
- Do not drink strong alcohol and do not eat fatty foods.
- Do exercises, get enough sleep, don’t get nervous for no particular reason.
Diseases affecting the female reproductive system often seriously threaten reproductive function. Many of them are dangerous not only to the health, but also to the life of the patient. A woman’s biggest fear is the degeneration of pathology into a malignant formation. To avoid this, a woman simply must be constantly monitored by a specialist and not delay visiting a doctor if the slightest strange symptoms appear.
Cervical parakeratosis is a condition that is manifested by pathological keratinization of the integumentary epithelium of the cervix. This phenomenon is not typical for a healthy organ; a relative exception is pseudoparakeratosis, in which keratinized cells can appear as a result of degenerative processes in endocervical smears in the second half of the cycle, as well as in the postmenopausal period.
Regular visits to the doctor will allow you to identify pathology at an early stage
What is parakeratosis in terms of etiology? This pathology is considered as a consequence of active inflammatory processes, as well as injury to the cervical canal during childbirth, abortion, and surgical interventions. It should be noted that this condition is background, that is, under some circumstances it can provoke dysplastic changes in tissues, which threatens cancer pathologies. Therefore, when parakeratosis is detected, therapeutic measures should be taken immediately.
Risks of developing severe consequences
Lack of treatment can lead to serious complications. Neoplasia is considered the most dangerous; it is a precancerous condition. The risk of developing cancer is very high.
Paraquetarosis negatively affects reproductive function and can cause infertility.
It is also worth paying attention to: what is mastodynia of the mammary glands and how serious the pathology is.
Can a woman diagnosed with monosomy give birth to a child? Information on the link.
Should I take a bath during my period: .
How does parakeratosis manifest?
Essentially, parakeratosis is a failure in the process of keratinization of the mucous membrane of the cervical canal. The condition is not an independent disease; it is a symptom of some pathology of the cervix.
Parakeratosis manifests itself as incomplete keratinization, but in the absence of adequate therapy it can transform into hyperkeratosis, that is, increased keratinization. In this case, the upper layer of the mucous lining of the cervix becomes keratinized, and the foci of the pathological process in structure represent several epithelial layers that have not undergone desquamation.
Both parakeratosis and hyperkeratosis are characterized by the following symptoms:
- there is no granular layer;
- the stratum corneum is thickened;
- rod-shaped nuclei are detected in the cells.
The progression of the pathological process provokes a decrease in tissue elasticity, while the lesions have a rough, wrinkled appearance.
Parakeratosis is a characteristic sign of a disease such as cervical leukoplakia. It is defined as precancer, so detection of this disease requires immediate initiation of treatment.
There are two types of parakeratosis: focal and superficial. The superficial version involves the involvement of a small area of the epithelium in the process, while it is not invasive. This type of pathological condition requires observation, but is rarely dangerous.
Focal parakeratosis is a dangerous phenomenon. In this case, the lesions have clear boundaries, the change in cell structure is clearly expressed. The condition requires treatment. It is focal parakeratosis that is a symptom of leukoplakia.
In addition, the focal variant of the condition is also characteristic of dysplastic lesions. In cervical intraepithelial neoplasia (CIN), areas with parakeratosis are identified in the early and late stages.
Visually, pathological lesions are defined as flat white spots with a matte tint. A common location is the mucous membrane of the vaginal portion of the cervix, a rare location is the depth of the cervical canal. Women of childbearing age are most susceptible to progression of the condition.
Reasons for the development of keratosis
Human papillomavirus
The main etiological factor of parakeratosis is the presence in the body of the human papillomavirus, which is a highly oncogenic type. Activation of infection by this virus provokes cellular changes in the form of pathological and excessive keratinization, disrupted structure of the nuclear apparatus of cells (multiple nuclei, koilocytosis).
Some other factors also contribute to the progression of the condition, namely:
- traumatization of the cervix during childbirth, abortion, curettage, installation of an intrauterine device, and other manipulations;
- therapy for cervical erosion;
- inflammatory diseases, including those caused by sexually transmitted infections;
- hormonal imbalance (insufficient production of progesterone);
- ovarian dysfunction;
- the presence of foci of ectopia.
The specific cause is determined during a complete examination of the patient.
The following are considered as additional provocateurs of pathology:
- weakened immune system;
- exhaustion of the nervous system;
- overwork of the body;
- reduced resistance.
Causes and symptoms of hyperkeratosis
The leading factor in the development of cervical parakeratosis is the circulation of human papillomavirus of high oncogenic risk.
The processes occurring during active papillomavirus infection are accompanied by cellular changes in the form of keratinization (parakeratosis, hyperkeratosis), disturbances in nuclear structures (koilocytosis, multiple nuclei, mitoses).
In addition to HPV, various factors can provoke the development of parakeratosis, including:
- traumatic installation of a spiral;
- curettage of the uterus;
- abortions;
- treatment of erosion;
- rough sexual intercourse;
- STI;
- vaginitis;
- cervical damage;
- lack of progesterone;
- disruption of ovarian function;
- frequent ectopia.
Identifying the cause of the disease is possible after a thorough diagnosis.
Additional provoking factors may include decreased immunity, nervous exhaustion, frequent overwork, and suppression of the body's resistance.
READ MORE: If a layer of cells in cytology what is it
Experts still have not figured out what “triggers” the process of leukoplakia. But it is assumed that the provoking factors are certain conditions of the body or effects on the cervix.
Internal reasons
The formation of various types of cervical dysplasia is influenced by a number of reasons, among which the leading position is occupied by infectious diseases and hormonal imbalances.
With regard to hyperkeratosis of squamous epithelium, the exact causes of development have not yet been fully studied, however, it has been proven that certain circumstances provoke excessive keratinization of cells. These include:
- chronic venereal diseases;
- varied and promiscuous sex life;
- frequent change of sexual partners;
- viral and bacterial lesions, especially HPV;
- sluggish candidiasis and other fungal diseases;
- unsuccessful surgical interventions, including abortions;
- multiple births;
- early onset of sexual activity;
- presence of contraceptive devices;
- taking incorrectly selected hormonal drugs;
- smoking (including passive smoking);
- negligence regarding personal hygiene.
Often the cause of hyperkeratosis is injury due to careless handling of sanitary tampons, medications for vaginal use and intimate objects.
In most cases, the disease is asymptomatic, without causing any discomfort, pain or other causes for concern.
Therefore, signs of hyperkeratosis of the squamous epithelium are detected only during an in-person examination by a gynecologist, who can observe characteristic formations both with the help of special examination instruments and with the naked eye.
They are white spots with clearly defined boundaries, sometimes protruding above the surface of the tissue. It is precisely because of the asymptomatic course of the pathology that it is so important to conduct regular preventive examinations in gynecology.
The diagnosis of “hyperkeratosis of the squamous epithelium of the cervix” is made not only by the results of a visual examination. For confirmation, additional examination methods are required, which include cytological examination, collection of epithelial cells for microbiology and colcoscopy.
If necessary, a biopsy may be performed. And based on laboratory data, when an accumulation of squamous epithelial scales is detected, a conclusion is made about the presence of dysplasia, which, in most cases, is a direct reason for immediate treatment.
Symptoms of keratosis
Parakeratosis and hyperkeratosis are often asymptomatic; as a result, the woman may not be aware of the existence of the problem. Therefore, regular preventive examinations are so important, which help to identify pathologies that occur without symptoms or with a small number of them.
In a number of situations, symptoms can be erased due to the presence of active symptoms of a provoking pathology, most often of an infectious-inflammatory nature.
The following symptoms can help you suspect a problem:
- discomfort during sexual intercourse;
- small amounts of spotting after sex;
- excessive production of vaginal secretions, which may have an unpleasant odor.
The presence of such symptoms should be a reason for mandatory contact with a gynecologist. The doctor will conduct an examination, prescribe additional diagnostic measures, make a diagnosis and determine the direction of the course of therapeutic correction.
Symptoms
Quite often the disease is asymptomatic. Because of this, the disease is detected at later stages of development, which contributes to the development of complications.
The following signs of parakeratosis are cause for concern:
- Discomfort during sexual intercourse.
- Discharge mixed with blood.
- Unpleasant odor from the vagina.
It is important to know! There are cases when paraketarosis manifests itself in the form of symptoms of the disease that provoked its development.
Methods for diagnosing hyperkeratosis
In addition to a gynecological examination, the following diagnostic measures may be needed:
- Schiller's test.
- Colposcopy in extended format.
- Biopsy followed by histological examination of the biomaterial.
- Examination of smears for flora.
- Examination of blood and secretions for sexually transmitted infections, including the human papillomavirus.
- Analysis of hormonal levels.
- Analysis of immune status.
The results of these diagnostic techniques will allow the doctor to make a diagnosis and determine treatment tactics.
Prevention of parakeratosis
Prevention consists of a healthy lifestyle, proper use of contraception, regular monitoring by a doctor and passing diagnostic screening methods. It is also important to strictly follow the rules of personal hygiene, especially in places such as a sauna, swimming pool, etc.
To prevent human papillomavirus, which is one of the most common causes of parakeratosis, vaccination is recommended. It is performed not only for women under 60 years of age, but also for men. However, some fairly reputable doctors have expressed serious doubts about the effectiveness and safety of this vaccine.
Gasanova Sabina Pavlovna
How to treat parakeratosis
If cervical parakeratosis is detected, treatment should be selected on an individual basis, based on the characteristics of a particular clinical case. The degree of the pathological process, the patient’s age and her general health are taken into account. Self-medication is unacceptable and impossible; the condition must be corrected according to prescriptions and under the supervision of a doctor.
Conservative therapy involves eliminating the factor provoking the problem. Treatment of bacterial and viral infectious diseases, vaginal dysbiosis is prescribed. Measures are taken to improve the functioning of the immune system.
Surgical correction involves removing foci of pathology. The specific technique is determined according to the size and location of areas of parakeratosis. The range of possible methods includes the following:
Invasive techniques are advisable in cases where the process is widespread and the presence of neoplastic changes.
To prevent parakeratosis, it is recommended to regularly visit a doctor for preventive purposes. Vaccination against human papillomavirus infection is also recommended.
More details about the pathology in the video:
Cervical pathologies are dangerous because they are often asymptomatic. 30% of cervical cancer cases are diagnosed at advanced stages. Parakeratosis of the cervix is a sign of a violation of the normal structure of the mucous membrane, and may be a harbinger of cancer.
Changes or growths on the cervix should be carefully observed and studied. In case of the slightest suspicion of degeneration into cancer or a precancerous condition, prompt therapy is required.
What it is?
Parakeratosis is a condition of stratified squamous epithelium of the mucous membrane, in which zones of keratinization appear. In this case, cell division occurs at an accelerated rate, and nuclei remain in the stratum corneum of cells, which is not the norm.
Parakeratosis is not an independent disease, but one of the symptoms of the underlying disease. In 70% of cases, cervical parakeratosis indicates the presence of leukoplakia. It is also a sign of chronic inflammation.
Important . Parakeratosis can develop into cancer. In approximately 30% of all cases of leukoplakia with parakeratosis, there is a risk of malignancy.
Parakeratosis is incomplete keratinization of the epithelium. If left untreated, hyperkeratosis occurs - complete keratinization of tissue.
Classification
Leukoplakia of the cervix is divided into several types:
- Hyperkeratosis is complete keratinization of stratified squamous epithelium. Such a change can occur on any mucous membrane, but it is the lining of the cervix that is very prone to the development of this process when there is insufficient content of “female steroids” - estrogen in the body or its low activity.
- Dyskeratosis is keratinization of keratinocytes with a decrease in keratin and the consequences of this process. Epithelial cells simply layer on top of each other. For this pathological condition, surgical treatments are successfully used.
- Parakeratosis is keratinization that occurs for various reasons.
There is also pseudoparakeratosis of the cervix, which can be common and even normal for women during the progesterone phase, or the second phase of the menstrual cycle. In smears, only isolated foci of keratinization can be distinguished, due to the special level of hormones during this period of the cycle.
Reasons for the development of parakeratosis
For the development of epithelial parakeratosis, a combination of certain factors is needed - immediate causes (external factors) and corresponding conditions (internal factors).
The causes of impaired cell division characteristic of parakeratosis include:
- the presence of chronic inflammation;
- hormonal disorders;
- infection with human papillomavirus (HPV);
- infection with STDs (sexually transmitted diseases);
- trauma to the mucous membrane due to surgical interventions;
- improper use of the intrauterine device.
Long-term inflammation leads to disruptions in cell division. One of the manifestations of this disorder is, in fact, parakeratosis.
An imbalance of sex hormones is sufficient for the development of parakeratosis. The mucous membrane of the cervix is sensitive to changes in hormones in the blood, and sometimes reacts to changes in hormonal levels by the appearance of areas of keratinization.
The human papillomavirus is capable of causing cell damage, subsequently disrupting their division. This feature is associated with the high oncogenicity of some types of this virus.
STDs cause inflammation in the mucous membranes and, accordingly, disrupt the structure of the tissue.
Frequent surgical interventions, abortions, and incorrectly installed intrauterine devices lead to trauma to the cervix. Chronic injury is accompanied by chronic inflammatory processes and corresponding cellular disorders (parakeratosis).
There are two types of parakeratosis depending on the direction of spread - deep or plane:
Superficial parakeratosis tends to spread along the plane, over the entire surface of the cervix. Characterized by insignificant depth of damage. It is less likely to become malignant and is easier to cure, even without surgery.
What does cervical cytology show?
Therapy for cervical hyperkeratosis can be divided into general and local methods.
The first category includes taking drugs that have a restorative effect on epithelial cells. These include groups of vitamins A and C, pro- and prebiotics, folic acid and other complexes. This therapy is prescribed for mild dysplasia.
https://youtu.be/VKze6H8LTRM
The second category includes drug (conservative) treatment and surgical intervention. Conservative methods primarily include the method of chemical coagulation, popularly referred to as “cauterization.” However, it is used in mild to moderate conditions.
As well as taking a large number of different drugs based on mineral salts and herbal ingredients, which is also an option for drug treatment.
Surgical intervention is performed according to strict indications and includes the following methods:
- electrical conization;
- cold disruption (cryosurgery);
- laser exposure;
- radio wave therapy;
- Ultrasound irradiation;
- knife conization;
- amputation.
Each of these methods has its own specific indications and prohibitions, and the need for surgical intervention is determined by the nature and extent of the lesion, the results of laboratory tests and the data of a complete, comprehensive examination of the patient.
The PAP test is a fast, inexpensive, informative method for diagnosing diseases of the vagina and cervix.
The main task of cervical smear cytology is: - identification of atypical cells; - diagnosis of precancerous changes (dysplasia) and cervical cancer (CC).
Cervical screening (mass examination of cervical smears) is a method of secondary prevention of cervical cancer.
Primary prevention of cervical cancer is vaccination against the human papillomavirus HPV.
Read more about the symptoms of human papillomavirus infection in women and the treatment of HPV here: Condylomas acuminata.
Atypical cells are morphologically altered cells: precancerous, cancerous.
- In malignant atypical cells, oncogenic mutations affect both the nucleus and the cytoplasm.
Cytological signs of malignant atypia: - increase in nuclear size; - change in the shape and color of the kernel; - abnormalities in the cytoplasm of cells.
The severity of atypia can suggest the level of precancerous changes (degree of dysplasia) of the cervix. But! Cytology does not determine the depth of tissue damage and does not distinguish dysplasia from non-invasive cancer (carcinoma in situ) or invasive microcarcinoma. Histology solves these problems.
How does parakeratosis manifest?
Parakeratosis does not give any signs for quite a long time, so it is detected in the initial stages only through regular examinations by a gynecologist.
What should a woman be wary of:
- the appearance of vaginal discharge with an unpleasant odor;
- scanty bloody smear after sexual intercourse, and soreness;
- pain in the lower abdomen, may radiate to the lower back.
Most symptoms arise as a result of the progression of pathology or the addition of an infectious agent.
Parakeratosis is not only the result of infections, but also an excellent condition for their occurrence. The appearance of discharge indicates infection.
Bloody discharge and pain indicate that blood vessels are involved in the pathological process, which is also characteristic of a malignant process and should alert you.
Predictions and consequences
The detected cervical hyperkeratosis is considered a life-threatening diagnosis for the patient due to the danger of atypical cell degeneration. Therefore, to treat the pathology, one of the surgical techniques is chosen depending on the results of a complete examination. However, you should not give in to panic after identifying leukoplakia of the uterine canal; this is not oncology, but a precancerous condition that can be treated with timely diagnosis. Only after adequate treatment is prescribed, the prognosis is favorable and does not worsen the quality of life.
A complication of untreated focal keratosis is the development of atrophy of cervical tissue, when reduced estrogen production leads to suppression of epithelial renewal and smoothing of tissues. Signs of atrophic vaginitis, accompanied by bloody discharge with vaginal dryness, are more often diagnosed during postmenopause against the background of cancer.
Purulent discharge during the atrophic process provokes infertility; if pregnancy occurs, the child is born with abnormalities.
Confirming the diagnosis of cervical hyperkeratosis not only complicates the woman’s physical health, but also results in psychological trauma due to damage to the reproductive system. Therefore, nulliparous patients, taking into account the severity of the keratinization process, are not prescribed radical surgery.
In order not to expose yourself to the risk of developing a complex and multifaceted pathology for women of any age, and especially those of childbearing age, it is important not to give up regular gynecological examinations. If a doctor prescribes treatment, you should not neglect his recommendations, because the prognosis for severe forms of hyperkeratosis is very sad. In the video about what cervical hyperkeratosis is:
Diagnostics
For correct medical tactics, a number of diagnostic measures are necessary:
- gynecological examination in mirrors;
- colposcopy;
- determination of HPV in a woman;
- microflora smear;
- cytological examination;
- histological analysis.
Important . The conclusion “parakeratosis” is issued to the patient based on cytological or histological examination data and the clinical picture. Visual examination alone is not enough to make a diagnosis.
During a gynecological examination, the doctor assesses the condition of the mucous membrane of the cervix and vaginal walls. If he suspects any abnormality, a colposcopy should be performed.
Colposcopy is an examination of the cervix using a special microscope, a colposcope. Allows you to identify the localization of the pathological process.
An HPV test will determine the likelihood of developing diseases associated with the presence of this virus.
A microflora smear provides information about infection by certain bacteria and the presence of inflammation.
Cytological examination will detect cells characteristic of parakeratosis.
Histological examination is carried out after the biopsy. A biopsy requires taking a piece of tissue from the lesion. Under a microscope, the presence of pathology will be determined, as well as the depth of disturbances in the tissue structure.
Paraquetarosis of the cervix: definition of the disease and its main characteristics
Cervical paraquetarosis is a pathological process that develops in the presence of inflammatory processes. The mucous membrane of the cervix becomes rough and wrinkled.
As a result, the tissues lose their elasticity and become injured. This often happens during sexual intercourse.
Pathology entails a change in the morphological characteristics of the mucosa in the form of:
- Thickening of the stratum corneum.
- Eliminate graininess.
- The appearance of rod-shaped nuclei.
Parakethorosis is divided into two forms of manifestation:
- Superficial - affects a small area and does not pose a serious threat.
- Focal parakeratosis of the cervix - significantly changes the structure of cells and affects large areas of tissue.
Treatment methods
Parakeratosis cannot be left without observation; therapy must be carried out. Treatment of parakeratosis consists of two stages:
- Eliminate the underlying immediate cause.
- Elimination of the focus of parakeratosis.
Since the cause may be hormonal fluctuations, infection, or chronic trauma to the cervix, the underlying disease is treated first. The doctor prescribes a course of antibacterial drugs, depending on the microflora smear and the sensitivity of bacteria to antibiotics. A course of antiviral drugs is prescribed if oncogenic types of HPV are detected.
It may be rational to take hormonal medications, as well as the correct selection of contraceptives.
The resulting focus of parakeratosis in 90% of cases requires surgical intervention, which can be explained by late seeking medical help.
Surgical methods:
- diathermocoagulation - cauterization of pathological lesions using electric current;
- laser removal - destruction of areas of parakeratosis using a laser;
- cryodestruction - the effect of liquid nitrogen on pathological tissues with their subsequent necrosis;
- Conization of the cervix - removal of a section of the cervix with pathological changes with a scalpel.
The method of surgical intervention is chosen in accordance with the woman’s desire to become pregnant in the future, as well as the risk of malignancy.
The most gentle method is laser exposure, and the most traumatic is conization of the cervix, which is used when cancer is suspected.
How to treat cervical hyperkeratosis
The choice of therapy depends on the form of the identified pathology; treatment is also aimed at eliminating concomitant diseases. After determining the factors that caused the pathology, one of the types of therapy is prescribed:
- antiviral;
- antibacterial;
- anti-inflammatory;
- immunostimulating;
- antifungal.
Treatment of leukoplakia is carried out in several ways; they are selected by the gynecologist depending on the degree of damage to the mucous membrane:
- Cryodestruction is targeted freezing of the affected area. This is one of the most common treatment methods. It is popular due to its painlessness, minimal complications, and the absence of scar formations that cause difficulties with conception. Despite all the advantages, the treatment is not without complications for the woman’s body. The procedure may shorten the cervix, making it difficult to conceive. During the healing of the mucous membrane, the discharge becomes excessively abundant, which causes discomfort to the woman.
- Laser vaporization is the essence of treatment in the destruction of pathological cells by cauterization with a laser beam. In this case, healthy tissue does not suffer, relapses are excluded, and a recovery period is not required. The use of laser does not leave scars, the growth of new healthy epithelium is observed a month after the procedure.
- Chemical coagulation is a minimally invasive intervention based on the medicinal effect on leukoplakia lesions. The chemical is harmful to the affected cells, but affects healthy tissue.
- Electrocoagulation is a traditional method of treating cervical hyperkeratosis. This is one of the most traumatic methods; cauterization also affects healthy tissue. The healing process is long and painful, accompanied by bleeding. The procedure is not recommended for girls planning a pregnancy; after electrocoagulation, rough scars remain.
- Radio wave destruction is a non-contact operation in which altered tissues are heated and removed by radio waves. The treatment does not cause pain and minimally damages surrounding cells.
All of the above procedures are performed on an outpatient basis. Patients are advised to abstain from sexual activity, strict hygiene of the genital organs, and taking a hot bath is prohibited.
Recurrences of cervical hyperkeratosis cannot be ruled out, so women who have had this disease should regularly visit a gynecologist for a routine examination.
Complications
Parakeratosis is not an independent disease; it is often a manifestation of leukoplakia or chronic diseases of the cervix. With timely treatment and following the doctor’s recommendations, the pathology may disappear on its own.
Important . Advanced leukoplakia and untreated chronic diseases, together with HPV infection, will continue to affect abnormal cell division processes. The worst outcome may be cervical cancer.
Disease prevention
Parakeratosis cannot be prevented by specific methods. Prevention can be reduced to the following points:
- regular examination by a gynecologist, including cytological examination of smears, microflora analysis;
- using appropriate contraceptive methods. The issue of taking hormonal medications should be discussed with a doctor;
- protection against STDs and HPV;
- timely treatment of inflammatory diseases;
- a healthy lifestyle that minimizes overwork, stress, and poor nutrition.
The presence of parakeratosis is not a reason to panic; treatment measures should be carried out as planned. The most important point of prevention is medical supervision, since only a gynecologist can assess the degree of compliance with subsequent points and correct them.
8 Prevention
To avoid the development of parakeratosis, you need to carefully monitor your health. You need to visit a gynecologist at least once every six months: examinations allow you to promptly identify a number of diseases and disorders that occur in the body without obvious symptoms.
https://youtu.be/5sgNwtgFABw
A method of specific prevention of human papillomavirus infection, which initiates dysplasia, hyper- and parakeratosis, is vaccination. The currently used vaccines are Gardasil and Cervarix.
The reason for an unscheduled visit should be any discomfort in the vaginal area, as well as injuries, menstrual irregularities. In the absence of serious infections and the rapid elimination of unfavorable factors that provoke leukoplakia with hyperkeratosis, the prognosis for cure is favorable.
To prevent hyperkeratosis, a woman needs to eliminate or reduce risk factors:
- Treat existing diseases;
- Observe the rules of personal hygiene;
- Avoid promiscuous sexual intercourse;
- Use barrier methods of contraception instead of hormonal drugs.
It is important to consult a doctor if any new symptoms appear (itching, burning, unusual discharge, soreness, etc.). Leukoplakia develops more often in premenopausal women, and less often in young women.
What do you need to remember?
- Cervical parakeratosis is a process of keratinization of the epithelium.
- The causes are chronic infection, HPV and hormonal imbalance.
- The most unfavorable prognosis is for the focal type of parakeratosis.
- The manifestations of parakeratosis are not specific; sometimes it occurs without giving a single symptom.
- The choice of treatment method depends on the depth of the lesion and pregnancy planning.
- The presence of complications is difficult to predict, but the most serious of them is degeneration into cancer.
Used Books
- Diseases of the cervix. - M.: GEOTAR-Media, 2014. - 160 p.
- Diseases of the cervix. Modern methods of diagnosis and treatment. - M.: Publishing house of the Nizhny Novgorod State Medical Academy, 2006. - 112 p.
- Khachaturyan, A. R. Colposcopy. Fundamentals of diagnostic algorithms and tactics for managing cervical diseases. Methodical recommendations / A.R. Khachaturyan, L.V. Maryutina. - M.: N-L, 2011. - 523 p.
- Prilepskaya V.N., Fokina T.A. Background diseases of the cervix: pathogenesis, diagnosis, treatment // Obstetrics. and gin. - 1990. - No. 6. - P. 12-15.
- Kulakov V.I., Prilepskaya V.N. Prevention of cervical cancer: a guide for doctors. - M.: MEDpress-inform, 2008. - 56 p.