How to get tested
Modern research makes it possible to detect the development of a tumor at an early stage.
This is the latest equipment and innovative technologies, which together make it possible to begin treatment at the first signs of an impending disease. Oncologists use complex diagnostics, which includes several indicators. Tumor markers are specific proteins that are secreted by tumor cells during their life in the host’s body. The formation of these proteins begins from the first days of human cell degeneration and allows for diagnostic testing at an early stage.
https://youtu.be/9nkUa_1NJAU
Oncologists call this type of protein a tumor marker for breast cancer. This approach is due to the fact that its specificity is clearly expressed in relation to this particular type of cancer and its location.
When a breast tumor develops, in 95% of cases the patient experiences an increase in the level of CA 15-3. But we should not forget that CA 15-3 is also characteristic of other malignant neoplasms.
For example, with a benign tumor there is also an increase in blood levels, but only in small quantities. Therefore, a comprehensive diagnosis is necessary to clearly differentiate the pathology.
This tumor marker appears in the patient’s blood during the formation of carcinoma of various organs. According to the classical definition, carcinoma is a malignant neoplasm.
The basis for its origin is epithelial tissue. Clinical studies have shown that this marker is characteristic of cancer of the pancreas, liver, lung, small and large intestine, as well as breast cancer.
The low specificity of the marker led to the abandonment of its use for early diagnosis of tumors. At the same time, doctors evaluate the effectiveness of the chosen treatment method by monitoring the content of CEA in the patient’s blood.
Only in a number of cases do specialists use CEA for early diagnosis of oncology. But not as an independent indicator, but as part of a comprehensive test.
To determine breast cancer, a simultaneous assessment of the content of CA 15-3 and CEA in the patient’s blood is used.
It is necessary to scrupulously evaluate the data obtained from laboratory tests so that the diagnosis is correct.
A tumor marker is used to identify breast carcinoma. Specialists use it as part of a comprehensive diagnosis in combination with other markers (REA, CA 15-3). Their combination makes it possible to monitor the effectiveness of the therapy used, as well as identify tumors at an early stage.
This marker is not highly specific, but clearly indicates the presence of a malignant neoplasm in the patient’s body. That is why it is widely used as part of a comprehensive diagnosis of breast cancer. The combination of CA 15-3 and PC-M2 makes it possible to detect a tumor at an early stage, and additional tumor markers TPA and CA 125 will only confirm the diagnosis.
In the hospital, professional medical staff will ensure that patients are properly prepared for the collection of venous blood necessary to identify tumor markers. But the majority of women do not go to the hospital just to get tested, and therefore you need to know a few absolutely simple conditions, under which the analysis will be much more accurate and of better quality.
In almost every woman with metastases in the mammary glands, an antigen appears in the blood. The breast cancer tumor marker CA 15 3 is elevated and remains within 39 units/ml, and the marker CA27 -29 is over 40 units/ml when carcinoma appears.
If, after a treatment course, the indicators do not return to normal, this indicates that the wrong treatment tactics were chosen and the disease is progressing. The doctor will most likely take measures to change the course of treatment due to the ineffectiveness of the previously chosen methods. Decoding on tumor markers allows you to easily identify the form. The type of cancer, as well as the extent of metastasis.
If the HER 2 marker appears in the blood, this indicates that drugs have been introduced into the patient’s blood: Kadcyla, Trastuzumab, Herceptin in order to block protein synthesis and stop the growth of tumor cells. This biological testing allows you to monitor the body’s reaction to the administration of certain drugs, and, if necessary, change treatment tactics or prescribe a course of chemotherapy.
If cancer markers are elevated in late pregnant women, then most likely there is the development of chronic hepatitis and lupus erythematosus.
Of course, tumor markers may not provide absolute indicators for oncology, so additional mammography is often prescribed.
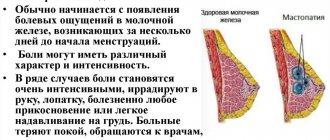
The CA15-3 tumor marker for breast cancer allows one to recognize the nature, shape, type, and location of the tumor. For example, with nodular breast cancer in women, a rocky compaction of dense consistency appears on the chest or a lumpy neoplasm under the nipples on the mammary glands with the release of ichor and deformation of the nipples and the appearance of a tortoise-shell layer with the development of erysipelas.
It happens that an atypical tumor develops, the peculiarity of which is the slow growth of the tumor. Often in women, carcinoma is detected during examination and palpation of the breast area.
It is tumor markers of the mammary glands that allow doctors today to easily establish the correct diagnosis, give a full assessment of the condition of the mammary glands, identify cancer at an early stage of development and stop the malignant process.
The possibility of a positive cancer outcome is directly related to the timing of the start of treatment, so the attitude towards diagnosis should be the most serious.
The following diagnostic methods are required:
- monthly self-check (palpation test);
- check with a doctor once a quarter;
- Ultrasound every six months;
- MRI every year.
Mammograms (x-rays) are not recommended before age 30, as exposure to radiation is best avoided at a young age. If you suspect breast cancer, you will need to undergo the following tests:
- Genetic analysis for cancer. Oncologists recommend that all women undergo this test as early as possible and identify possible changes in the BRCA1 and BRCA genes. In the normal state, they act as regulators of cell repair and proliferation, restraining their excessive proliferation. According to statistics, changes in the BRCA1 and BRCA2 genes are responsible for approximately 7.5% of all cases of the disease. The risk that people with excess proliferation will develop breast carcinoma is 65%.
- A blood test for breast cancer is a mandatory standard. First, a general blood test is done. This test gives an idea of the number and age of leukocytes, their type, erythrocyte sedimentation rate, and hemoglobin level.
Negative test results do not necessarily indicate cancer - there are many reasons for blood counts to deviate from normal. If the results suggest cancer, a biochemical blood test is prescribed. - The biochemical test is aimed at identifying tumor markers in the blood. Biochemistry is more indicative because it can give an understanding of the presence of a tumor, its location and size, degree of prevalence, and the body’s reaction. Biochemistry is carried out in several stages in order to assess the dynamics of changes.
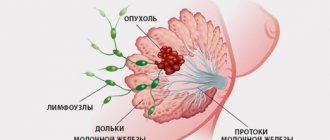
- Histological analysis. Extremely informative is a histological analysis, in which a punctate of the mammary gland or the mammary gland tissue itself is taken. A histological test allows you to find out not only the parameters of the tumor and the extent of its spread, but also the condition of the neighboring lymph nodes. Conducting this type of study well determines the further prognosis of the disease.
Breast biopsy
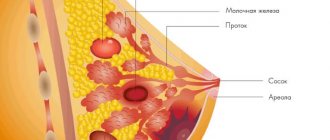
The purpose of a biopsy analysis is to confirm the diagnosis if the presence of a cancerous tumor is suspected. Data are also obtained on the condition of the tissues being studied. The analysis will show whether a benign or malignant tumor has begun to develop in the mammary gland.
A breast biopsy is performed using a needle, which is inserted into the affected area. A needle is used to draw fluid, which will subsequently be studied in the laboratory. A cytologist studies the material. If at least a small number of harmful cells were detected in the liquid, the doctor makes a diagnosis.
Breast biopsy is performed using different methods, using needles of different thicknesses. Before the procedure, you will need to do an additional examination that will help determine the location of the tumor and the extent of its spread. To obtain such data, ultrasound, x-ray or mammography are usually prescribed.
Early detection of pathology increases the chance of recovery.
What is the norm
The blood content of CA 15-3, which does not pose a threat to the patient’s health, does not exceed 25 units/ml.
The blood level of CA 125, which does not pose a threat to human health, does not exceed 25 units/ml.
The norm is considered to be a TPA content in the patient’s blood of no more than 75 units/l.
The normal CA-15 marker in women is 27 units/ml, although today some doctors estimate the threshold at 30 units/ml. CA -15-3 in the initial stages of cancer in percentage will increase in case of severe disease. But at stages 3-4, in most cases in the presence of metastases, it shows, on the contrary, a decrease in marker units in the blood serum.
Normally, CEA should be 5 units/ml. If there are additional gastrointestinal diseases in women, it can reach 9-10 units/ml and this will also be considered normal.
The level of the CA 27-29 marker is normal - 37-41 units / ml, although in women who have previously undergone a treatment course, a different test - mammography can still show the presence of a tumor. The main thing is that the concentration of the CEA marker does not exceed 30 units/ml, and that of the CEA marker – 0-5 units/ml.
Appointments
A referral for blood sampling for this test is given by a practicing oncologist for the following indications:
- primary and prognostic diagnostics - detects the presence of cancer cells in an organ, or their absence. The pathology is often confused with mastopathy, which is characterized by a benign nature and does not threaten the patient’s life;
- choice of therapeutic tactics or assessment of treatment effectiveness — in case of recent detection of an invasive manifestation of the disease, this testing is carried out on the level of hormonal receptors.
Based on its results, it is possible to determine the priority of hormonal or targeted effects on the tumor. The absence of an increase in the concentration of molecules during treatment gives hope for recovery and a return to normal life;
- monitoring of relapse and metastases - in case of aggressive behavior of abnormal cells, activation of metastasis processes, as well as in case of secondary recurrence, the presence of hormonal receptors will help to choose the optimal method of therapy, its dosage and course duration.
Prices
The cost of conducting a laboratory examination in different cities of Russia may differ slightly from each other. This also applies to medical centers and municipal institutions. However, the average cost of determining tumor markers for Russia is:
- CA 15-3: ranging from 750 to 1200 rubles;
- REA: 800-1000r;
- CA 125: 1000-1400 rub.
The cost of conducting the above study for Ukraine ranges from 120 to 250 UAH. for tumor marker CA 15-3 (depending on the selected medical center and the speed of analysis). The average cost of determining the CA 15-3 indicator is 165 UAH.
SA 15-3
It is a carbohydrate gene produced by healthy organ cells. Effective for identifying the disease in patients over 18 years of age. It is characterized by a low degree of sensitivity, as a result of which it does not always reflect it at the initial stages of the pathology.
The antigen is able to diagnose up to 60% of recurrent situations much earlier than the appearance of the most primary signs of their occurrence. Metastases penetrating into bone tissue and liver are especially visible.
It is considered one of the most comprehensive analyzes. Its value is in determining the concentration of embryonic cancer antigen.
Most often, such studies are indicated when tracking the dynamics of oncology. The susceptibility of the antigen is determined by the size, area of dislocation of the formation, stage and nature of the disease.
The main difference of the marker is that its high level is noted in the absence of pathology, and at the stage of the onset of breast cancer, its content can vary within the acceptable norm.
Decoding the analysis makes it possible to predict the degree of effectiveness of conservative therapy when surgery can no longer produce a visible result.
For a fairly complete clinical picture of tumor staging, blood is donated according to the schedule:
- in 1 year - every month;
- in year - once every two months;
- in year 3 – quarterly.
The normal concentration is considered to be no more than 22 IU/l. If the indicator fits into this figure, we can talk about the absence of a malignant formation, or about its primary stage, as well as about the effectiveness of the treatment.
What color should the discharge be after removal of uterine fibroids? This article summarizes the signs of early stage cervical cancer.
How to understand that metastases have appeared in the lungs? Symptoms https://stoprak.info/vidy/metastazy/v-legkix-simptomy-mexanizm-razvitiya-i-terapiya.html and manifestations. Survival prognosis.
In a completely healthy person, this figure should not exceed 13.4 units , with the borderline indicator being considered to be between 20 and 30 units. Exceeding the norm is interpreted as a deviation and indicates breast carcinoma or oncology of other organs.
How the analysis is deciphered
It should be noted that, according to research, breast tumor markers, in particular CA 15-3, are elevated in approximately 20% of patients with breast cancer diagnosed at the first or second stages of the disease. Although at later stages, breast tumor markers are elevated in eight out of every ten patients.
Cancer antigen 15-3 (CA 15-3), cancer antigen 27-29 (CA 27-29), and carcinoembryonic antigen (CEA) are detected in 50-90% of women with metastatic breast cancer when deciphering breast tumor markers.
Despite radiological signs of persistence of the disease, deciphering the breast tumor markers CA 15-3 can show an absolutely normal level (that is, within 30 U/ml), and this means that the treatment was successful, and the residual tumor recorded on the mammogram is no longer viable.
If tumor markers of the breast are elevated - CA 15-3 above 30 U/ml, CA 27-29 above 40 U/ml - then there are good reasons to diagnose oncology. When the indicators do not decrease after treatment, two options follow: either the treatment was incorrect, or the disease is progressing.
If breast tumor markers increase after therapy, this is a clear sign of its ineffectiveness. In this case, the absence or presence of clinical improvements is taken into account.
So, deciphering breast cancer markers helps to identify breast tumor relapses after treatment, as well as metastases at an earlier stage.
Breast tumor markers HER2 indicate whether a drug such as Trastuzumab (Herceptin, Kadcyla), which blocks protein synthesis of transmembrane cell receptors and stops the growth of cancer cells, can be used in treatment.
In some cases, the results of this biological testing help oncologists assess the tumor's tendency to progress, determine how the body responds to treatment, and determine the need for specific chemotherapy.
By the way, breast tumor markers are slightly elevated in the last trimester of pregnancy, with liver cirrhosis, chronic hepatitis, systemic lupus erythematosus, sarcoidosis, and tuberculosis. Therefore, today breast tumor markers are not an absolute indicator of oncology without visualizing tumors using mammography.
Diagnosis of breast cancer by blood test
The most common cancer affecting women is breast cancer. It would be a mistake to believe that women over 50 are affected by this disease. Currently, there are more and more cancer patients who are barely 30 years old. Time plays an important role in the treatment of oncology, so much depends on timely access to a doctor and correct diagnosis at the initial stage of the disease. Thanks to scientific developments by scientists from different countries, it is possible to diagnose breast cancer at the earliest using blood tests. Also, based on the results of blood tests, it is possible to identify not only a progressive disease, but also a predisposition to it. Modern diagnostic methods help many women save their lives.