Sputum is a liquid secretion from the respiratory tract, separated by expectoration. A healthy person does not cough or expectorate phlegm. That is, any sputum is a pathological product formed as a result of certain diseases.
Normally, special goblet cells of the trachea and bronchi constantly produce mucus, which is designed to cleanse the airways. Mucus contains immune cells called macrophages, which capture foreign particles of dirt, dust and microbes and remove them out.
Under the influence of micro-processes of the ciliated epithelium, the mucus formed in the bronchi moves from bottom to top, entering the larynx and nasopharynx. This mechanism is called mucociliary transport. Next, it mixes with saliva and mucus from the nose and paranasal sinuses. Normally, a healthy person produces about 100 ml of such mucous secretion per day, its release occurs gradually and imperceptibly. The resulting secretion is usually swallowed without causing any inconvenience.
In the case of any pathology, the inflamed bronchial mucosa produces mucus in larger quantities; exudate (serous or purulent) containing fibrin is mixed with it (this changes its consistency - it becomes thicker, more viscous). The inflammatory exudate also contains leukocytes, erythrocytes, desquamated epithelium of the respiratory tract, as well as various microorganisms.
Thus, sputum has approximately the following composition:
- Slime.
- Serous exudate.
- Fibrin.
- Pus.
- Red blood cells.
- Epithelial cells.
- Elastic fibers (during the breakdown of lung tissue).
- Bacteria.
- Foreign matter (dust, food particles).
Such sputum irritates the cough receptors and a productive (wet) cough occurs.
The nature of sputum is:
- Mucous membrane – viscous, viscous, transparent.
- Serous - liquid, foamy, transparent, maybe with inclusions of white lumps (admixture of fibrin).
- Purulent - thick, yellow or greenish-yellow.
However, there is practically no purely mucous, purely serous or purely purulent sputum. Most often it is of a mixed nature: fibrin is mixed with the mucous membrane, mucus is mixed with the purulent one, etc.
Color and causes of sputum
The color of sputum can also provide a lot of information about the diagnosis:
- Transparent mucous sputum occurs with viral inflammation and bronchial asthma.
- With purulent bacterial inflammation, it becomes yellow or green. This happens with: purulent bronchitis, staphylococcal pneumonia, exacerbation of COPD, bronchiectasis, lung abscesses, rupture of pleural empyema into the bronchial tree.
- Streaks of blood, as well as clearly bloody sputum, are evidence of destruction of the lung tissue or bronchial walls. This is a rather ominous symptom. It happens most often with malignant processes in the bronchi and lungs, tuberculosis, and pulmonary infarction.
- Rusty or brown sputum (this color is formed by blood breakdown products) occurs with lobar or influenza pneumonia, tuberculosis.
- For heavy smokers and coal industry workers (miners), it can be gray or even black.
The amount of sputum can vary from several spits to 1.5 liters per day (bronchiectasis, destructive pneumonia, cavernous tuberculosis, abscesses, pleurobronchial fistulas).
Mucus may be released and coughed up continuously or coughed up at some time of the day (for example, in the morning). Sometimes it begins to move away only in a certain position of the body - for example, horizontally or when turning on its side. This point is also important for diagnosis, this is especially significant in the presence of cavities in the lungs or bronchiectasis.
Cough with white sputum: symptoms
Any colored clots when coughing are considered abnormal. When white mucus appears in the mouth, you need to pay attention to the accompanying symptoms, which may include:
- Difficulty breathing;
- Shortness of breath and wheezing;
- Feeling of tightness and pain in the chest area;
- Poor appetite;
- Changes in the properties of expectorated clots
When coughing with fever, such symptoms may indicate an inflammatory process in the body.
If the illness occurs without fever, there may be an allergic or occupational cough attack, pathologies of the cardiovascular system, or taking certain medications.
to the content?
Sputum discharge and provoking diseases
Bronchitis
The onset of acute bronchitis is usually manifested by a dry cough. And only after 2-3 days sputum begins to appear. In the vast majority of cases, acute bronchitis is caused by viruses, so the sputum in bronchitis is mucous or serous in nature, transparent, viscous.
The amount of it is usually small, for several days it is difficult to expectorate, then it liquefies, expectoration becomes easier, and within 10-14 days the bronchial tree is gradually cleared of inflammatory secretions, the cough goes away. This is how uncomplicated bronchitis occurs.
In cases of a complicated course (high virulence of infection, chronic somatic diseases, smoking, air pollution), coughing with sputum may drag on and it may become purulent.
In chronic bronchitis and COPD, the cough can continue for a long time after an exacerbation; sometimes sputum can be coughed up constantly, even without an exacerbation of the disease, especially at night and in the morning.
Bronchial asthma
Sputum in bronchial asthma is a variable symptom. It is formed in the bronchi as a component of allergic inflammation and is an additional factor (in addition to bronchospasm and swelling of the mucous membrane) in the narrowing of the lumen of the bronchi during an attack of suffocation.
As a rule, after she clears her throat, the condition improves and the attack of suffocation passes. Sputum in bronchial asthma is thick, viscous, mucous in nature. May be yellow in color due to admixture of eosinophils.
Bronchiectasis
This is a pathology, the main pathological substrate of which is saccular dilatations of the bronchi. In these enlargements, the infection lingers for a long time, evacuation from them is difficult, and the nature of the inflammation is often purulent. Therefore, this disease is characterized by:
- Improving sputum discharge in a certain body position (for example, in the position on the right side with left-sided bronchiectasis and vice versa).
- Copious discharge, sometimes a mouthful.
- Purulent character.
- Unpleasant odor due to the addition of anaerobic flora.
Similar symptoms are also observed with a lung abscess, although here the symptoms of intoxication will be more pronounced.
Tuberculosis
Coughing up sputum during tuberculosis is evidence of an already advanced process. In the initial stages, tuberculosis is asymptomatic.
The nature of sputum in tuberculosis can be different - from mucous to mucopurulent with an admixture of blood. Tuberculosis, along with lung cancer, is the most common cause of hemoptysis.
Its quantity can also be different - from a small amount to 1000-1500 ml in the presence of cavities (destruction cavities).
The causative agent often detected in sputum is Mycobacterium tuberculosis.
Lung or bronchus cancer
Typically, bronchial or lung cancer develops against the background of existing chronic bronchitis or COPD, in which coughing up of sputum is already observed. What should be alarming here is the appearance of blood in it - from veins to obvious blood clots. Lung cancer is also characterized by sputum in the form of “raspberry jelly.”
Postnasal drip syndrome
This is a condition in which discharge enters the nasopharynx not from the bronchi, but flows along the back wall of the pharynx from the nasal cavity and paranasal sinuses. This happens with chronic rhinitis (including allergic ones), characterized by excess mucus production, as well as with chronic exudative sinusitis. Mucus flows into the throat, during the day it is usually swallowed, but at night it accumulates and causes a cough.
Postnasal drip syndrome is thought to be the cause of chronic cough with sputum in more than 50% of cases. In addition to a morning productive cough, this symptom is characterized by a feeling of discomfort in the throat, a feeling of mucus flowing, and the passage of mucous clots, sometimes even without a cough.
Extrapulmonary causes of constant accumulation of sputum in the throat include the hypertrophic form of chronic pharyngitis. The mucous membrane of the pharynx is thickened, hyperproduction of mucus occurs, a bacterial infection is often associated and the patient constantly expectorates mucopurulent sputum.
Gray sputum when coughing
A cough with gray sputum is familiar to smokers and is a harbinger of chronic pulmonary obstruction.
Being a strong irritant, tobacco smoke disrupts the functioning of the ciliated epithelium, which ensures the removal of toxins from the body.
Accumulating in the bronchi, it leads to the production of excess gray mucous exudate. Cleaning products used in everyday life, as well as paints, varnishes, and dust have a similar irritating effect.
The presence of gray discharge during the cough reflex may indicate serious pathologies of the bronchopulmonary system.
The dark gray tint of the expectorated material is a sign of bronchioloalveolar cancer, a condition in which tissue necrosis and decay occurs. Foaming gray phlegm indicates a lung abscess or bronchial asthma.
Similar symptoms:
to the content?
Sputum analysis: conducting research
Sputum analysis is one of the main tests in clinical laboratory diagnostics. To collect it for analysis, use special plastic containers with a lid. It is advisable to collect sputum in the morning before eating, after thoroughly rinsing your mouth and throat with boiled water. The collected portion must be delivered to the laboratory as quickly as possible.
In addition to determining the color and nature of sputum, microscopy is also performed during general clinical analysis. Microscopy can reveal:
- Cells of the bronchial epithelium (cylindrical). Detected in bronchitis, tracheitis, bronchial asthma.
- Squamous epithelial cells. This is the epithelium of the oral cavity and has no diagnostic value.
- Leukocytes. There are small amounts of them in any sputum. During purulent processes, a large number of neutrophils are detected, and during allergic inflammations - eosinophils.
- Red blood cells. Their number matters. Detection of more than two or three in a smear requires further examination.
- Atypical cells in tumors.
- Kurshman spirals – for bronchospastic diseases.
- Pathogens: Mycobacterium tuberculosis, actinomycetes, echinococci.
To detect Mycobacterium tuberculosis, an analysis of at least three portions of sputum is required.
To identify these and other pathogens, bacteriological examination of sputum is also used: sowing it on special media, culturing it, followed by studying the resulting colonies of microorganisms. This analysis takes several days, but has great diagnostic value, and also determines the tactics of further treatment with antibacterial drugs.
Diagnostics: which doctor to go to and what tests to take?
The very first specialist you should contact with a wet cough is your family doctor or primary care physician. He conducts initial diagnostics and treats acute respiratory tract infections, exacerbation of chronic pathology, and also refers to a specialist. With bronchial asthma, bronchiectasis, chronic obstructive pulmonary disease - see a pulmonologist. If you suspect cancer, see an oncologist. If there are signs of tuberculosis, see a phthisiatrician. With cardiac pathology - see a cardiologist. If there is a suspicion of a foreign body, then the patient is treated by general surgeons.
Examinations that help determine the cause of sputum:
- Clinical analysis of blood and urine.
- Blood chemistry.
- X-ray examination of the chest organs in two projections. If there is a suspicion of oncology, then bronchography and computed tomography are performed.
- Microscopic examination of sputum and culture of it on media. If pneumonia is suspected, an antibiotic sensitivity test is needed. If it is an oncological process, then analysis for atypical cells. If there is a suspicion of tuberculosis, then mycobacteria are looked for in the sputum.
- Bronchoscopy for a foreign body. For bronchogenic lung cancer, a tumor biopsy is also taken.
- Spirography for the differential diagnosis of bronchial asthma and chronic obstructive pulmonary disease.
- ECG in 12 standard leads for patients with cardiac pathology and age category of patients.
- Ultrasound of the heart if there is a history of cardiac pulmonary edema. Ultrasound of the pleural cavities, if there are signs of hydrothorax on x-ray.
How to treat phlegm?
Any discharge of sputum is a pathology. It is necessary to clarify the exact cause of this symptom . Purulent and bloody sputum should cause particular concern. This is a situation when you need to see a doctor immediately. It is also necessary to see a doctor if you have been coughing up sputum for a long time - more than a month.
If there is a lingering cough after suffering from an acute respiratory viral infection, this is most likely a manifestation of acute tracheitis or bronchitis. In this case, the doctor will probably prescribe expectorant medications.
It should be noted that coughing with sputum does not always require medication. If uncomplicated bronchitis without signs of bacterial inflammation and bronchospasm is detected, sometimes drinking plenty of warm drink is enough to somewhat facilitate the natural clearing of mucus from the airways.
A comparative study was conducted on the effect of popular cough syrups in children compared to regular drinking. It turned out that these actions are approximately equal in effectiveness.
Drinking plenty of fluids is necessary for any cough. It has been proven that drinking plenty of fluids, especially alkaline drinks, has an effect comparable to the effect of expectorants.
If the sputum is thick, viscous, difficult to cough up and causes significant inconvenience, measures are taken to facilitate its clearance.
There are several types of expectorants:
- Drugs that directly or indirectly stimulate the secretion of bronchial glands.
- Mucolytics - change the structure of the mucus itself.
Reflex-action drugs, when taken orally, irritate the stomach receptors. In large doses they can cause vomiting, and in small doses they indirectly stimulate the secretion of the bronchial glands and the movement of the cilia of the ciliated epithelium through reflex connections. As a result, the proportion of liquid secretion increases, sputum becomes thinner, making it easier to remove and cough up.
The drugs in this group include mainly herbal remedies:
- Thermopsis herb and preparations from it.
- Marshmallow root and products containing it.
- Liquorice root.
- Anise fruit.
Ready-made preparations containing one or more expectorant components include: dry cough medicine, cough tablets (thermopsis herb + soda), breast mixture No. 1, breast mixture No. 3, glycyram, marshmallow syrup, mucaltin, ammonia-anise drops, breast elixir.
Direct expectorants are taken orally, absorbed into the blood and secreted by the bronchial glands, as a result of which the sputum is diluted. These include solutions:
- Iodine salts (2-3% solution of sodium iodide or potassium iodide).
- Sodium bicarbonate.
- Essential oils (used inhalation).
Mucolytics act directly on bronchial secretions , changing the structure of mucus and making it less viscous. These are the drugs:
- Acetylcysteine (ACC, ACC-long, Fluimucil).
- Carbocisteine (Fluifort, Bronchobos).
- Ambroxol (Lazolvan, Ambrobene).
- Bromhexine (Solvin).
- Enzyme preparations. They act directly on sputum proteins, depolymerizing it. These include trypsin, chymotrypsin, ribonuclease.
Mucolytic drugs are taken both orally and, in severe cases, parenterally (there are injectable forms of acetylcysteine and bromhexine for intravenous administration). These products are also available in the form of solutions for inhalation (for use in nebulizers). Enzyme preparations are used only by inhalation.
Inhalation therapy for cough with sputum
Inhalation administration of drugs (inhalation) has a number of advantages compared to taking them orally. To facilitate the discharge of sputum, both conventional steam inhalations and inhalations using a nebulizer can be used.
For steam inhalations, a solution containing herbal decoctions (ledum, coltsfoot, sage, chamomile), saline solution or soda solution (1 teaspoon of soda per glass of water) is heated to a temperature of 50-55 degrees and inhaled through a special inhaler or through a paper cone placed on a cup. A good effect is achieved by adding a few drops of essential oils to the solution; pine, fir, juniper, eucalyptus, and lavender oils are especially good.
Inhalation using a nebulizer is becoming increasingly popular. A nebulizer is a device in which a medicinal solution is converted using ultrasound into tiny aerosol particles; they easily penetrate the respiratory tract and act directly on the surface of the mucous membrane. Using a nebulizer, you can administer various medications, including expectorants. Inhalations using an ultrasonic nebulizer are indispensable for treating a child’s cough.
To relieve phlegm, you can use inhalations:
- With saline solution.
- Alkaline mineral waters.
- Pharmacy solutions of Lazolvan, Ambrobene, Fluimucil.
- For children and pregnant women, inhalations can be done with Pertussin or dry cough syrup dissolved in saline solution.
Traditional methods for coughing with sputum
Among the simplest and most effective means we can recommend:
- Coltsfoot (pour 1 tablespoon over a glass of boiling water, leave for 10 minutes, cool, strain, drink 1 teaspoon 3-4 times a day).
- An infusion of thyme, plantain, wild rosemary, and elecampane root. Pour 2-3 tablespoons of dry raw materials or mixture with a liter of hot water, let it brew for 2 hours. Strain. Drink 1 glass 3 times a day.
- Take one small black radish. Peel, grind it, squeeze out the juice and mix in equal proportions with honey. Take a few (3-4) teaspoons before meals.
Postural drainage and massage
It is possible to facilitate the discharge of sputum not only by taking medications, but also by some physical methods. Postural drainage is the process of placing the body in a position in which mucus can be drained as easily as possible.
This is especially important in patients with chronic bronchitis, in whom the normal mechanism of mucociliary transport is disrupted, as well as in patients with pneumonia, bronchiectasis, and destructive lung diseases.
It is best for sputum to come out of the bronchial tree when the head end is down . The easiest way: the patient hangs over the edge of the bed, rests his hands on the floor, takes a deep breath and tries to make as many coughing impulses as possible. If the pathological process is one-sided, you need to turn on the healthy side. If double-sided - alternately on each side.
It’s even better if someone taps and pats the chest at this time. The duration of this procedure is 10-15 minutes. Be sure to perform it in the morning after sleep and then several times during the day.
Video: how to do massage when treating bronchitis - Doctor Komarovsky
Folk remedies
Despite the fact that there are many drugs for the treatment of cough and respiratory diseases, traditional medicine methods are still used. These products are prepared exclusively from herbal ingredients, therefore they are safe for your well-being:
- coltsfoot leaves;
- plantain;
- sage;
- pine buds;
- Alteyka root.
Often the pharmacy sells ready-made herbal mixtures for its discharge. Before using such drugs, be sure to ask your doctor and also familiarize yourself with the dosage. These herbs can be used for inhalation. To expectorate, you need to prepare the following herbal ingredients:
- take one tablespoon of thyme, chamomile, sage and pour boiling water over it;
- the decoction is infused for about 60 minutes;
- add tsp to the solution. baking soda and eucalyptus oil (a couple of drops);
- The tincture is ready for inhalation.
Another effective method is homemade ointment made from badger fat. To prepare the compress you will need badger fat, which needs to be melted. Then it can be smeared on the chest. For any respiratory disease, the main thing is to maintain a drinking regime. After all, when you cough, you need to drink a lot of liquid as the mucus will thin out. Another important point during treatment is to constantly ventilate the room.
If you follow the advice of doctors, take medications as prescribed, and use traditional medicine when necessary (as prescribed by the doctor), you can improve your well-being and speed up the healing process.
conclusions
So:
- Any expectorated phlegm is a pathology, so you shouldn’t delay seeing a doctor, even if you think you have a common cold.
- Particular concern should be caused by purulent sputum, sputum with blood, as well as mucous sputum expectorated for more than 2 months.
- Coughing with phlegm is a protective reflex and does not need to be suppressed.
- With good expectoration of sputum, the use of medications is not necessary. Sometimes drinking plenty of water is enough.
- You cannot use expectorants and antitussives at the same time, since they have different mechanisms of action (antitussives are prescribed for a debilitating dry cough and only for a few days).
A little about prevention
Such phenomena can always appear if you do not follow the basic norms of a healthy lifestyle. Smoker's bronchitis, accompanied by a large amount of sputum, cannot be removed by any means, because this is a consequence of a bad habit, the body's protective reaction to smoke and nicotine, which an adult deliberately introduces into his own respiratory organs, clogging them by inhaling tar.
Colds, which result in bronchitis and pneumonia, just like viral diseases, are a consequence of poor functioning of the natural immune system. Frequent exposure to such troubles suggests that the body does not have the strength to fight “aliens” in the form of viruses and microbes that attack it from the outside. And where a healthy person sneezes a couple of times, a weak person will lie in bed for weeks and cough painfully for a month, studying on websites how to get rid of phlegm.
Every person can take care of their health simply by doing necessary and healthy little things every day: eating right and often, treating chronic diseases without being excused by lack of time, eating healthy foods rich in vitamins and minerals, fresh fruits and vegetables. And why not get some exercise in the fresh air? Life activity also affects health! It's not as much as it seems when it comes to health.
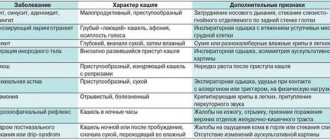
Types of cough
Cough syndrome with sputum is a physiological phenomenon that promotes the removal of accumulated mucus in the respiratory system. The patient is often alarmed that this symptom manifests itself in different ways.
A wet cough may indicate the development of a serious illness, so it is important to know what types of coughing exist in order to make an accurate diagnosis in a timely manner and begin treatment.
Protracted productive cough
If the symptom persists for 4–8 weeks without significant changes, then they speak of a lingering cough with sputum. It is an alarming sign signaling the development of a serious disease.
Long-term productive cough syndrome is observed when infected with tubercle bacilli. The sooner the patient seeks medical help, the more favorable the outcome will be for him.
Quite often, a cough with mucus production occurs in smokers with prolonged bronchitis. The pathology develops into a chronic form, which is difficult to treat.
The appearance of a prolonged wet cough is observed in people whose professional activities are associated with hazardous production. To get rid of this symptom, it is necessary to stop contact with the substance that caused it.
Chest cough
Respiratory diseases of fungal, viral and bacterial nature progress from the common cold to pneumonia or bronchitis. The beginning of pathologies is a dry cough reflex. As phlegm accumulates in the lungs, the cough becomes chesty. This is what often causes bronchitis.
Wet with phlegm
A wet cough is accompanied by sputum production. The mucus discharged has a different nature. In normal health, secretion production is small; in case of illness, its quantity increases as the body tries to flush out the infection that has accumulated in the bronchi. This process ends with recovery.
Carrying out inhalations
Inhalations are carried out using a drug dissolved in water. Prescribed in cases where sputum has not been coughed up for a long time. Compared to tablets, this method has the following advantages:
- the active ingredient of the drug reaches directly the affected areas of the mucous membrane;
- sputum is moistened with steam, becomes liquid and comes off easily;
- Accelerated removal of bacteria from the bronchi occurs.
Doctors recommend inhalation using a nebulizer. The device converts the drug into an aerosol, which is delivered into the respiratory tract through a mask. During the procedure, the nasal canals, throat, tonsils and bronchi are treated. Inhalations with a nebulizer are safer because there is no risk of accidental burns to the respiratory tract.
Steam nebulizer with inhalation mask
Rules for inhalation:
- start the procedure 1 hour after eating or exercising;
- clothing should not restrict the chest;
- you need to be in a clean, ventilated room;
- inhalation cannot be combined with taking mucolytic drugs in the form of tablets or syrup;
- after the procedure, do not leave the room for 1 hour;
- the amount of the drug dissolved in water should not exceed 5 ml.
Time for one procedure:
- children over 2 years old - no more than 1 minute;
- adults - up to 5 minutes 2 times a day.
Preparations for inhalation:
- ACC-100 (10% solution);
- Bromhexine 4 Berlin-Chemie;
- Fluimucil;
- Overslept.
It is prohibited to carry out inhalations in the presence of purulent lesions of the respiratory system. Before the procedure, it is necessary to test for an allergic reaction to avoid complications such as bronchospasm.
Inhalation technique:
- you can use a nebulizer, or any other sterile container;
- add 5 ml of the drug to the water, heat it to steam;
- inhale steam through the nose, slowly and calmly;
- it is forbidden to talk;
- it is necessary to close your eyes to prevent burns;
- After the procedure, you should remain in bed.
If any discomfort occurs, you must stop the procedure.
Diagnostics
Diagnosis is carried out by pulmonologists and phthisiatricians if there is a suspected tuberculosis process. In the case of cancer, you cannot do without consulting an oncologist. At the initial appointment, the specialist interviews the patient about complaints, their nature, duration, and limitation. An anamnesis is collected, that is, the doctor determines what diseases the patient has suffered during his life.
It is important to identify the presence of a focus of chronic infectious lesions in the body, contact with tuberculosis patients and other important factors. To put an end to the issue of the origin of the symptom, a number of instrumental and laboratory studies are carried out aimed at differentiating individual diagnoses.
Accordingly, the following are required:
- Bronchoscopy. An absolutely necessary study aimed at identifying bronchial pathologies. The doctor can evaluate the condition of the anatomical structures with his own eyes.
- X-ray of the lungs. It is carried out first.
- Fluorography. Reveals only the most severe changes in the condition of the chest organs.
- MRI/CT diagnostics. It can replace most studies and allows you to give a comprehensive picture of the disease-causing condition.
- Biopsy followed by histological and morphological examination.
- General blood analysis.
- Biochemistry of blood.
In total, these studies are sufficient to make a diagnosis.
Preventive measures
It’s worth remembering one rule: you can’t treat just a cough. This is a symptom indicating one of the diseases of the pulmonary system. Therefore, there are no preventive measures.
You can protect yourself and your loved ones from infections, bacteria and other provocateurs that affect the appearance of the reflex if you follow the general rules:
- Use environmentally friendly products, always washed;
- do not overload the body physically and mentally. It is a proven fact that most diseases occur due to psychological fatigue;
- carry out a set of measures to strengthen the immune system;
- Conduct annual tuberculosis screenings. In children this is the Mantoux test, and for adults it is an x-ray;
- If you have a runny nose or slight coughing, see a therapist;
- eradicate bad habits.
All these recommendations will help minimize the risk of infection. Doctors also strongly recommend minimizing communication and being in a crowded place during an exacerbation of influenza or acute respiratory infections. At the same time, when an increased epidemiological level is declared, carry out an additional complex of strengthening the immune system.
What to think
- Bacteria or fungi can be found by using special dyes on a sputum sample. This is called a gram spot. Gram spots can help your doctor: Know if a sputum sample is suitable for testing. For example, was the sputum collected correctly? Is there enough sputum in the sample? If the sample is not good enough, another sample may be obtained.
- Make a diagnosis before the culture results come back from the laboratory. In some cases, Gram stain results may be available within 30 minutes. But other test results may not be available for 1 to several days. The information obtained from Gram spots can help your doctor treat the infection earlier rather than waiting for test results.
Causes of brown discharge
Why does the color of sputum change? Brown mucus is a criterion for many diseases. Discharge in the morning appears due to the fact that the muscles of the sternum contract, trying to eliminate everything on their own. Rusty sputum occurs in patients with a disease caused by an infection. Rusty-colored sputum is considered a reason for concern and a visit to the doctor. This tone is often observed with pneumonia. Red sputum indicates the presence of blood, but unlike pinkish mucus there is much more of it. In this case, the mucus radically changes color with the formation of veins.
Brown sputum occurs due to inflammation (usually the lungs). Brown sputum when coughing indicates necrosis (death) of the lung tissue. Thick brown sputum with mucus is characteristic of diseases that are associated with damage to the respiratory system by various infections. This also includes polluted air and tobacco smoking. If we consider cough from this point of view, then it is an absolutely natural phenomenon, because coughing when smoking appears as a cleansing function (removing mucus from the respiratory system). In any case, when mucus is released, it is necessary to consult a pulmonologist. Pharmaceutical substances are prescribed depending on the personal characteristics of the body.
Forecast
The prognosis for wet cough without fever in adults is favorable. There will be no trace of the disease if the cause is identified in a timely manner and treatment is started. After all, a cough is just a symptom of the disease.
Advanced forms of diseases, as a rule, lead to serious changes in the body and transformation into more severe pathologies. If the source of coughing attacks is a tumor, the outcome of treatment will depend not only on the timeliness of therapeutic actions, but also on the type of tumor.
Prevention
A wet cough and runny nose can mean a common cold. But in other situations, such a symptom signals a serious illness in the body. If you have a strong wet cough for 3-5 days, but there is no fever, you should not postpone your visit to the doctor. The same applies to sick children.
Important! In children, diseases develop faster than in adults, since the immune system is not yet fully formed.
In order to prevent diseases, you need to follow a few simple rules:
- lead a healthy lifestyle;
- eliminate bad habits;
- ventilate the living space at least twice a day;
- take vitamins and immunomodulatory drugs;
- try not to come into contact with infectious patients;
- eat healthy foods, fruits, vegetables;
- rest, follow a daily routine.
Preventing a disease and its complications is much easier than treating them for a long time. Paying attention to your health will allow a person to avoid serious health problems in the future.
An adult has trouble coughing up sputum: what to do?
Cough with phlegm can be eliminated only with complex therapy. The mucus will not be able to leave the lungs on its own. You need to visit a doctor who will prescribe the following medications:
- medications that dilute bronchial secretions - in adults, treatment with difficult-to-remove mucus lasts 7-10 days. Before taking, you need to read the instructions and take into account contraindications. The following medications are suitable for the discharge of sputum in adults - ACC, Codelac Broncho, Lazolvan or Fluimucil;
- Medicines that promote the removal of secretions are an excellent means for removing secretions. The medication will not only remove mucus, but also speed up the regeneration process. If the mucus does not come away during a cough, then the doctor’s prescription will contain the following drugs - Marshmallow Root, Mucosol, Licorice Syrup or Carbocisteine.
If secretions are difficult to pass with bronchitis, then you need to consult a therapist. Excessive accumulation of mucus will lead to a chronic course of the disease. Folk remedies are well suited for expectoration. Of course, taking medications should be discussed with your doctor. Sputum in a child deserves special attention, especially at an early age.
Accompanying symptoms
With this disease, accompanying symptoms may appear, which are also characteristic of lobar pneumonia:
- Chills are a serious cause for concern.
- Body temperature rises to approximately 39 degrees.
- Frequent cough, which occurs with pneumonia.
- The appearance of pain in the lateral area or in the abdominal area.
- The respiratory process is disrupted.
- Fever in which the cheek on the side of the affected lung becomes slightly red.
- The heartbeat increases without any reason.
In some cases, this symptomatic picture is mistaken for bronchitis.
In this regard, pulmonologists prescribe an additional blood test, the results of which make an accurate diagnosis.
If a person has an inflamed lung, then a clinical examination shows:
- presence of granularity of neutrophils;
- violation of ESR;
- development of leukocytosis;
- increased blood clotting.
In the case when sputum is produced in small quantities and has a natural transparent color, then a person should not worry.
After all, this is a normal process of functioning of the system of natural cleaning of the bronchi from various foreign substances that can get inside along with the inhaled air.
However, if sputum is produced in increased quantities and also has a certain color, then it is necessary to undergo an examination to check the condition of the lungs and bronchi.
If pus is detected in the discharged bronchial secretion, the doctor makes a diagnosis of chronic inflammation of the respiratory organs.
Where does mucus come from in the respiratory organs?
Sputum is secretion from the tracheobronchial tree. It is produced by goblet cells of the bronchi and trachea. Mucus contains immune cells - macrophages, lymphocytes, so it has bactericidal properties. Performs 2 main functions:
- disinfects mucous membranes;
- removes foreign objects (dust, allergens, bacteria) from the respiratory tract.
In the absence of ENT diseases, the tracheobronchial tree secretes no more than 100 ml of mucus daily.
But when the mucous membranes become inflamed, the goblet cells become activated. Therefore, the content of tracheobronchial secretion increases to 500 ml. The main causes of excessive mucus production:
- bronchitis;
- tracheitis;
- tonsillitis;
- laryngotracheitis;
- pneumonia;
- sinusitis;
- respiratory allergies;
- bronchiectasis;
- adenoiditis;
- reflux disease;
- esophageal diverticula;
- Cardiopathology (unstable angina, heart failure).
Transparent sputum when coughing is a sign of acute inflammation of infectious or allergic origin. If it is thick, like snot, in 8 out of 10 cases this indicates damage to the lower respiratory tract - bronchi, trachea, lungs.
Viscous sputum without cough occurs against the background of pathologies of the nasopharynx - postnasal drip, chronic rhinitis, adenoiditis, sinusitis.
Medications
Each patient needs a different medicine for phlegm in the throat. The doctor decides which remedy to prescribe:
- expectorants and thinners: tablets Mucaltin, Bromhexine, acetylcysteine (Fluimucil), ambroxol drops and syrup (Lazolvan, Fervex, Flavamed, Ambroxol), Pertussin and others; these medications will help remove phlegm from the throat, and along with it the products of inflammation will be removed, which will lead to recovery;
- bronchodilators – syrups Gerbion, Prospan; dilate the bronchi, promote the discharge of sputum;
- lozenges - Lizobakt, Faringosept, Strepsils - have an antiseptic, anti-inflammatory effect, promote the discharge of mucous secretions;
- sprays - Ingalipt, Kameton, Miramistin, Hexoral, Yox - they all have anti-inflammatory, antiseptic, expectorant effects; in case of severe inflammation and swelling of the pharynx, Tantum Verde spray is suitable;
- rinsing solutions - Hexoral, Miramistin.
Stages of lobar pneumonia
The pathological process occurs in 4 stages:
- The first stage lasts 1-3 days. It is characterized by pulmonary edema and hyperemia of blood vessels. The cavities are filled with liquid, which is secreted by the vessels.
- The second stage also lasts 1-3 days. During this time, hemorrhage in the lung is observed. Then a granular structure begins to form in it.
- The third stage lasts 2-6 days. It is characterized by an increase in the concentration of leukocytes in the blood. The lung has a granular consistency.
- Fourth stage. Here, under the influence of leukocytes, a liquefaction of the exudate is observed, it partially resolves, and the rusty sputum during pneumonia disappears during coughing.
Rust-colored sputum is characteristic of the last stage of the disease, which lasts from 2 to 5 days. This pathology is characterized by an acute onset.
You can learn more about the sputum that is released during pneumonia from the video:
https://youtu.be/Ewf5bLk8fjU