Pathogenesis
The prodromal period, a precursor to the development of myocardial infarction, lasts from several minutes to several days, and various symptoms can occur at different periods separately. The absence of trophism, its deterioration due to impaired blood flow due to narrowing ( stenosis ) or blockage of the coronary vessels lead to ischemia and tissue necrosis, ventricular fibrillation. As a result, acute coronary insufficiency , provoked by a violation of oxidative processes in the myocardium, in addition, there is an excessive accumulation of under-oxidized metabolic products, including lactic, pyruvic, carbonic, phosphoric acid, etc.
A heart attack can even begin suddenly, for no apparent reason - exercise or stress. It does not go away even after rest; the patient still experiences compressive pain in the chest. This condition can lead to loss of consciousness and even cardiac arrest.
Features of treatment
Timely, adequate medical care can significantly reduce the risk of developing myocardial infarction. Therefore, when the first signs occur, you need to call a doctor and provide first aid to the person.
It is strictly not recommended to resort to traditional methods of stabilizing the condition. After all, if a heart attack is hidden behind the symptoms of angina, hospitalization should be carried out no later than 6 hours from the onset of pain. Later introduction of some drugs is already useless.
Treatment tactics for pre-infarction conditions depend on the patient’s condition and the likelihood of a heart attack. Most people are advised to take medications (conservative therapy), and if there is a high risk of heart attack, surgery is recommended. After stabilization of the patient’s condition, a diet is prescribed and recommendations are given for lifestyle changes.
First aid
If an angina attack lasts longer than usual, and the pain is more severe, call a doctor immediately. Before the ambulance arrives you need to:
- open the window, balcony;
- sit or lie down so that your head is significantly higher than your body;
- unbutton the collar;
- try not to move;
- take an aspirin tablet;
- put nitroglycerin under your tongue. It is allowed to take up to 3 tablets with an interval of 5-10 minutes;
- no smoking.
Medications
The purpose of drug treatment of unstable angina is:
- decreased oxygen demand of the heart;
- improving the supply of oxygen to the myocardium;
- prevention of possible complications (arrhythmias, myocardial infarction).
To achieve these goals, the patient is prescribed medications that belong to various pharmacological groups.
Antiplatelet drugs
Prevents the formation of new blood clots, helps prevent the development of myocardial infarction, and reduces mortality. The most famous representative of the group is aspirin. It has been proven that taking it reduces the likelihood of a heart attack, the risk of death, by almost 50% (4). Another first choice drug is heparin. Its use also significantly reduces the risk of death.
After relative stabilization of the patient’s condition, the drugs ticlopidine or Plavix are prescribed. They are also used for aspirin intolerance as first choice drugs.
Nitrates
They reduce the tension of the myocardial wall, the oxygen demand of the heart, and dilate large and small coronary vessels. Nitrates are considered the best medicines for eliminating angular pain. The first aid drug is nitroglycerin. It is given to relieve the acute phase of the disease. For long-term treatment, other drugs with a prolonged effect are used - isosorbide, nitrosorbide. There must be a break of at least 8 hours/day between the use of nitrates. Otherwise, the body gets used to them and stops responding to the introduction.
Beta blockers
They reduce the frequency and strength of heart contractions and inhibit cardiac conduction. The nature of the heart's work becomes more gentle, it begins to consume less oxygen. The drugs also reduce the tension of the myocardial wall, which promotes blood redistribution. Beta blockers lower blood pressure and prevent platelet aggregation. In the treatment of unstable angina, selective drugs are used: atenolol, metoprolol, bisoprolol, nebivolol.
Calcium channel blockers
Calcium antagonists prevent the mineral from penetrating into the muscle cell. This ensures a decrease in the frequency and strength of heart contractions, and the opening of spasmodic arteries of the heart. As a result, the oxygen demand of heart cells decreases and blood flow improves. Blood pressure decreases with the use of calcium channel blockers. The main representatives are verapamil, diltiazem.
ACE inhibitors (ACEIs)
Helps lower blood pressure and improve blood supply to the myocardium. If ACE inhibitors are prescribed together with nitro drugs, they enhance their effect. The most commonly used drugs are ramipril and perindopril. Taking them helps reduce the likelihood of death, major myocardial infarction, and cardiac arrest by 20%.
Lipid-lowering drugs
Prescribed to reduce the level of bad cholesterol, triglycerides, and increase the concentration of good cholesterol. Most often, people with a pre-heart attack are prescribed statins. The main representatives of the group are atorvastatin, rosuvastatin, simvastatin. These drugs do not work immediately. A pronounced effect is observed after 30 days. However, their use improves the prognosis, especially long-term.
If lipid levels are poorly normalized during the use of statins, the treatment regimen is supplemented with lipid-lowering drugs of other groups: cholesterol absorption inhibitors, bile acid sequestrants, fibrates.
Surgery
The purpose of surgical intervention in a pre-infarction condition is to restore the patency of the heart vessels. There are two options for the procedure:
Stenting procedure.
- Coronary artery bypass grafting is a complex operation that is performed on an open heart. Using a vessel taken from another part of the patient's body, the surgeon creates a bypass for blood flow, sewing one end above and the other below the narrowing site.
- Stenting is a low-traumatic procedure that does not involve cutting into the chest cavity. The surgeon inserts a catheter with a deflated balloon at the end into a large vessel. Under computer control, he guides the catheter to the area of narrowing. Having reached it, he pumps and deflates the balloon several times. Gradually, the lumen of the vessel expands. To consolidate the result, a stent is delivered to the site of narrowing - a frame that, when expanded, will keep the artery “open”.
Diet, lifestyle changes
Regardless of the treatment method, all patients are prescribed a diet that reduces the likelihood of complications, and a lifestyle review is also recommended.
Proper nutrition involves limiting the intake of salt, cholesterol, and saturated fat. The basis of the diet should be cereals, vegetables, fruits, fish, low-fat dairy products, legumes, nuts, and seeds. Eating fast food, red meat, egg yolks, fatty dairy products, and sweets should be avoided.
Our lifestyle largely determines the likelihood of developing angina attacks and other cardiovascular diseases. To reduce the risk it is recommended:
- quit smoking;
- move more, if your health allows, there are no contraindications - play sports;
- exercise moderation in alcohol consumption;
- control stress levels;
- maintain a healthy weight;
- monitor blood pressure;
- treat diabetes mellitus.
All of the above tips are effective for preventing cardiovascular diseases. Therefore, they are recommended for all people, not just those who have experienced an attack of unstable angina.
Causes
The occurrence of a pre-infarction state is facilitated by:
- general disorders of the circulatory system caused by heart failure , which lead to blood stagnation, accumulation of large amounts of carbon dioxide, tissue hypoxia, acidosis, changes in blood pressure , heart rate;
- atherosclerosis of the arteries and other diseases that cause thickening of the intima of the arteries;
- embolism - blockage of blood vessels by gas bubbles or foreign particles - emboli, which are brought with the bloodstream;
- thrombosis - disruption of normal blood flow formed by blood clots;
- arterial spasms - pathological narrowings caused by excessively intense or prolonged muscle contractions;
- arteritis – inflammation of the artery walls due to infections or autoimmune reactions;
- heart injuries - most often blunt, lead to contusion of the myocardial muscles, rupture of the heart chambers and septa, damage to the valves;
- violation of the rheological properties of blood, for example, increased viscosity and aggregation of red blood cells;
- hyperlipoproteinemia - an increase in the concentration of lipids and lipoproteins in the bloodstream, a common cause of problems with the cardiovascular system;
- hypertension leads to constant tension of the vascular walls, which can cause their thickening, impaired elasticity and trophism;
- hypothermia;
- overdose of medications.
Possible causes of pre-infarction condition
Provoking factors of myocardial infarction
A heart attack in women over 50 years of age can be triggered by many negative factors.
Doctors identify several of the most important:
- Regular stressful situations. Daily nervous tension affects the patient's blood pressure. This leads to poor circulation and increased stress on the heart.
- Poor nutrition with insufficient intake of magnesium, potassium, calcium and B vitamins. The heart muscle must regularly receive the necessary elements. Otherwise, it becomes thinner and loses elasticity.
- Frequent overwork also puts stress on the cardiovascular system. The myocardium wears out, which certainly leads to the appearance of an area of tissue necrosis (necrosis).
- Violation of the work and rest schedule is a common provoking factor. During sleep, the heart works in a gentle mode, which allows it to recover. Lack of sleep leads to disruption of the functioning of the organ.
- Insufficient fluid intake leads to blood thickening, blood clots, and increased stress on the heart.
- Consumption of large amounts of salt, which causes fluid stagnation in the body, increased blood pressure, and increased stress on the organ.
Such factors, repeated over a long period of time, can provoke the development of a dangerous disease.
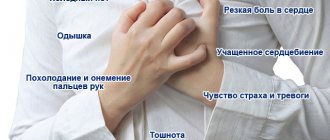
Symptoms of pre-infarction condition
Determining the onset of myocardial infarction is not difficult. It is accompanied by severe and sudden pain in the chest, spreading to the left arm and extending to the back and jaw. In addition, a person may experience:
- a surge of nausea;
- lethargy;
- disturbances in concentration;
- feeling of anxiety;
- increased heart rate;
- dizziness.
A pre-infarction condition can also be determined by the appearance of sticky, cold sweat, shortness of breath, weakness, and anxiety. Signs of dysfunction of the heart muscle appear in the form of heaviness in the chest, strong compression or pressure on the heart area.
Symptoms of pre-infarction in women
In women, signs of a pre-infarction condition are atypical and can only be tingling, difficulty breathing and dizziness.
Unusual symptoms also include abdominal pain, but they can be a symptom of other diseases, so additional examinations are necessary before providing medical assistance.
Symptoms of pre-infarction in men
In men, the signs of a pre-infarction state are usually more pronounced - the patient experiences severe pain in the center of the chest and behind the sternum, severe compression, even burning, and lack of air.
Atypical manifestations may be cyanosis or pallor of the skin, drowsiness or, on the contrary, insomnia , swelling of the lower extremities, and a state of euphoria .
Forecast
The prognosis depends on many factors: the general health of the patient, his age, timeliness of treatment, and test results. Unfavorable prognostic factors include (5):
- angina attacks during rest;
- diabetes;
- hypertension;
- high cholesterol;
- renal failure;
- signs of left ventricular decompensation;
- change in the nature of the ECG (decreased ST wave);
- multiple damage to blood vessels by atherosclerotic plaques.
The following markers increase the likelihood of developing myocardial infarction and death in the short term (5):
- increase in symptoms of cardiac muscle ischemia over the past 2 days;
- the duration of the attack at rest is more than 20 minutes;
- pulmonary edema;
- mitral regurgitation (backflow of blood);
- age over 75 years;
- changes in the nature of the ECG (ST-T interval);
- sustained ventricular tachycardia.
Patients admitted with a pre-infarction state 6 or more hours after the onset of pain have an unfavorable prognosis: 10% of patients develop myocardial infarction by the end of the first week, 15% after 3 months, and the mortality rate is 4%, 10%, respectively ( 4).
Assistance provided in full helps to achieve a significant reduction in mortality. However, unstable angina is still considered a serious disease that is fraught with relapse and fatal or non-fatal complications.
Tests and diagnostics
It is necessary to carry out differential diagnosis with myocardial infarction, as well as monitoring changes in body temperature, ESR, leukocyte formula, ECG (electrocardiogram) and the level of activity of blood enzymes such as creatine phosphokinase, troponin, lactate dehydrogenase, aspartate aminotransferase, alanine aminotransferase .
In addition, pulse oximetry is performed to determine the level of arterial hypoxemia .
Magnetic resonance imaging allows you to determine the characteristics of blood supply and heart function.
Coronography is performed if conservative drug therapy is not effective and the patient is indicated for surgical intervention to solve the problems of narrowing of the arteries that bring blood to the heart.
Why women are less likely to suffer from heart disease
For several decades, experts have been conducting studies involving patients of different genders and ages. As a result of such experiments, it was revealed that women suffer from heart disease several times less often than men.
According to statistics, about 17% of men over the age of 60 suffer from some form of severe heart disease. Researchers attribute this to bad habits, which are more common among male patients. In addition, doctors associate the fact with the inability to throw out negative emotions, as women do.
Men in most cases keep their experiences to themselves, which negatively affects the functioning of the heart.
Additionally, they are less likely to consult a doctor when the first symptoms appear, which leads to a worsening of the disease. An important factor will be lifestyle and nutrition. Men are more often engaged in hard physical labor, take more alcohol, and prefer to eat a lot of fatty, spicy, fried foods.
The latter factor leads to an increase in the level of bad cholesterol in the blood. All this provokes the development of heart disease. This is why female patients are less susceptible to myocardial infarction.
First aid
If a heart attack is suspected, the patient should be seated and calmed down; a tight tie or shirt should be loosened or removed. Next, you should measure the pressure, if it is elevated, then it is advisable to give a nitroglycerin . You can also use aspirin - 300-600 mg in tablets that should be chewed is enough.
In case of loss of consciousness, cardiopulmonary resuscitation measures must be performed. If you are in a public place, perhaps an institution (airport, cafe) has a portable defibrillator, its use greatly increases the chance of survival.
Rehabilitation after a heart attack
Restoring the vascular system and the heart muscle itself is an important step towards getting rid of the consequences of an attack.
Rehabilitation after a heart attack includes the following stages:
- maintenance therapy - after discharge from the inpatient department of the hospital, the woman continues outpatient treatment, taking medications that support and strengthen the heart;
- diet - an individual diet is formed, from which fatty, salty, pickled, smoked and fried foods are excluded, the menu is filled with cereal porridges, boiled meat, fresh vegetables and fruits in order to get the maximum benefit from the dishes eaten;
- spa treatment - it is recommended to go for spa treatment in a specialized boarding house in order to receive therapy in the most comfortable conditions, created specifically for patients with similar pathologies;
- psychotherapy is an important stage in the general course of rehabilitation, which consists of working with a psychologist who will help to realize that myocardial infarction is not a death sentence for a woman, and it is only necessary to learn to live with the consequences of this disease;
- lifestyle correction - to quickly restore stable heart function, it is necessary to gradually introduce moderate physical activity, give preference to walking, swimming in the pool, cycling, and exercising on exercise machines with minimal weights.
The average recovery time after a heart attack ranges from 6 months to 2 years.
It all depends on the individual characteristics of the female body, age, type of activity and the extent of the altered heart tissue.
Prevention
The main way to prevent a heart attack is to give up bad habits and follow a diet. It is important to exclude animal fats, fried, smoked, flour products from the diet and add cereals, fruits, vegetables, and seafood.
Prevention of heart attack
Daily moderate morning exercise will also help prevent heart problems, for example, morning exercises or cycling, walking, adjusting the regime of adequate sleep, work and rest.
Heart attack disease in women: symptoms, prevention
To avoid the development of heart pathology, you should start taking measures at a young age. Prevention of primary and secondary types includes:
- to give up smoking;
- physical activity;
- rare alcohol consumption;
- proper nutrition;
- monitoring cholesterol and blood sugar;
- use of Aspirin or Heparin at increased risk.
Clinical picture of atypical cases
If the signs of this disease are non-standard, diagnosing a progressive heart attack is somewhat more difficult. For example, patients with diabetes mellitus and chronic diseases of the cardiovascular and respiratory systems may encounter this problem. The attack is accompanied by unexpressed symptoms, so help for the person may be delayed. Atypical signs are presented below:
- pain in the left side of the body – sternum, shoulder, lower jaw;
- pain syndrome in the epigastric region, with nausea, bloating, vomiting;
- lack of air, asthmatic attacks;
- signs of acute pancreatitis;
- neurological disorders.
What symptoms, besides pain, does a person experience during a heart attack?
In addition to serious discomfort in the sternum, patients may experience interruptions in heart function, weakness and excessive sweating, and a feeling of lack of air. Upon examination, the doctor discovers pallor of the patient’s skin, bluish coloration of the lips, ears, nose and nail folds. Your breathing rate may increase. The doctor examines the functioning of the cardiovascular system by palpation, identifying changes associated with the nature and extent of the disorder:
- with an extensive transmural infarction, presystolic pulsation is detected during palpation, which is synchronized with the IV sound, which is explained by contraction of the left atrium. This picture tells the doctor that the compliance of the left ventricle of the heart affected by ischemia is reduced;
- if during palpation pulsation is felt in the upper part of the heart in the diastole phase, which corresponds in time to the third sound, this tells the doctor about systolic dysfunction of the heart muscle in the area of the left ventricle;
- when systolic pulsation is determined to the left of the sternum in the region of the III, IV, V intercostal space, this indicates dyskinesia of the lateral or anterior sections in the left ventricle of the heart.
If the heart attack is uncomplicated, then the boundaries of the heart will be normal. Against the background of atherosclerosis of the aorta, expansion of the dullness of the vascular bundle in the region of the second intercostal space is often detected. The boundaries of the heart can sharply expand due to complications; this condition is caused by an aneurysm in the left ventricle, acute mitral regurgitation due to effusion of pericarditis or rupture of the papillary muscles, or rupture of the interventricular septum in the heart. Another reason that causes expansion of the boundaries of the heart may be the death of a large area of the myocardium.
Is it possible to help at home?
You can’t do anything on your own; it’s impossible to distinguish between heart pain and cardiac pathologies without special methods. It is necessary to call an ambulance.
The algorithm before the doctors arrive is as follows:
- Take a Nitroglycerin tablet. If there is no effect, take another one after 10-15 minutes.
- Open the window, window. Provide ventilation in the room.
- Sit down, move less. Do not lie down, your condition may worsen.
- Calm down. Emotional manifestations provoke the release of cortisol and adrenaline. An increase in blood pressure will have an even worse effect on a person’s general condition.
You can't wash your face or eat. Loss of consciousness, vomiting and death from asphyxia are possible. Upon arrival of doctors, tell about your health, briefly and clearly.
You should not refuse offers of hospitalization. This is in the interests of the person himself. It is necessary to prevent the development of a heart attack by all means.
Emergency care for cardiac arrest
But since he will not be able to arrive in a minute, and in such a situation every second counts, the victim needs to undergo chest compressions and artificial respiration.
To do this, the steps should be as follows:
- Carefully place the patient on a hard surface (the floor) and kneel at her side.
- Unfasten all belts, fasteners, ties, and jewelry that may impede breathing.
- Free access to the chest from clothing.
- Place one hand on your chest, palm down, about 2 fingers below the xiphoid process (it can be felt as the end of the chest followed by a depression).
- Place your second hand on top of the first and make 3-4 pushes with sharp, strong movements, without bending your elbows. Frequency – 1 every 2 seconds.
- After this, perform mouth-to-mouth artificial respiration and repeat the entire cycle until cardiac activity resumes (determined by palpating the pulse in the carotid artery located in the neck).
It is necessary to perform indirect cardiac massage and artificial respiration quickly and clearly, for which it is better to learn these skills in a calm environment. In this case, you need to take into account the force of pressing on the chest depending on age - young girls and older ladies should not push as hard as ladies of other age categories.
Acute signs
When an attack occurs, a heart attack in women usually occurs with the following symptoms:
- acute throbbing pain in the heart;
- difficulty breathing, inability to breathe deeply;
- sudden pallor, significant cooling of the extremities;
- panic attack;
- a sharp decrease in pressure;
- loss of ability to speak (or incoherent speech);
- muscle weakness, movement disorders;
- sometimes - complete or partial loss of consciousness.
Symptoms in women are largely similar to those in men. At the same time, there are often cases when they are confused with other diseases and completely different measures of assistance are used.
Heart attack and similar diseases
The signs of a heart attack in a woman are in many ways similar to some other diseases that have completely different causes and treatment methods.
- Bronchial asthma - a sharp shortness of breath occurs due to spasm in the bronchi. In this case, a cough appears, and the attack itself can be relieved by using treatments that will not help with a heart attack.
- Neuralgia - sharp pain in the left side resembles a heart attack. However, during a heart attack, sensations are localized near the heart, while neuralgia is characterized by the spread of pain along the entire left side: in the intercostal part, under the left shoulder blade, right up to the jaw.
- An attack of appendicitis and pancreatitis (inflammation of the pancreas) is similar to the first symptoms of a heart attack in that it is also accompanied by sharp pain in the abdomen. But unlike a heart attack, they are accompanied by nausea and vomiting, and are also relieved by applying a cold object.
Sleep disorders
Sleep disturbances (difficulty falling asleep, insomnia, or restless sleep) may be symptoms of a pre-heart attack. Typically, these conditions appear several weeks before the attack, so precautions should be taken immediately.
If you or someone you love is experiencing all or at least some of these symptoms, don’t hesitate! Timely medical care will help maintain health and even save a person’s life! Do not self-medicate under any circumstances! Doing it yourself can cost you a lot...
Take care of yourself and be healthy!
Maybe,
Signs of the onset of an acute period
More than 100 years ago, the founders of the theory of myocardial infarction, V.P. Obraztsov and N.D. Strazhesko, in addition to the classic anginal symptoms, identified a number of atypical forms in which the disease can manifest itself. Symptoms of a heart attack in women most often have the following forms of manifestation:
- Anginal status - recorded in 60–75% of cases. When this form develops in women, the pain is localized in the left upper part of the body: neck, shoulder, arm, upper chest. There is a feeling of self-limiting toothache. A characteristic feature in women is also acute pain in the back of the head. The remaining manifestations of anginal status are the same as in men: profuse sweating, cyanosis of the skin, numbness of the limbs, panic. The pain is intense and does not go away from taking nitrates.
- Status asthmaticus is registered in 10% of cases, its main characteristic is the presence of signs of bronchospasm. In this case, in the absence of physical activity, the patient experiences shortness of breath and difficulty breathing. These symptoms intensify when turning the body. This form of symptoms occurs in older women, against the background of a previous heart attack or prolonged hypertension.
- Abdominal form - manifests itself in 2–3% of cases. It develops when the posterior wall of the myocardium is damaged. Symptoms of such a heart attack lead to a false suspicion of pathology of the gastrointestinal tract.
Anginal status in asthmatic and abdominal forms may appear later. But the primary symptoms of atypical forms complicate diagnosis, and only an experienced emergency doctor is able to immediately make the correct diagnosis.
How to distinguish atypical forms of heart attack from other diseases:
| Atypical form | What disease does it look like? | Differences |
| Asthmatic status | Bronchial asthma | There is no relief from taking bronchodilators |
| Myocardial infarction is rarely accompanied by cough | ||
| Abdominal status | Acute pancreatitis, appendicitis, perforation of a stomach ulcer | When taking antispasmodics and antacids, the pain does not go away |
| In case of a heart attack, the pain sensations are wave-like, in case of gastrointestinal diseases they are of constant intensity |
The following atypical forms are less commonly recorded in women:
- Arrhythmic status is due to a higher heart rate in women, which predetermines the development of arrhythmia. With this form of heart attack, only a violation of the heart rhythm is recorded, in the complete absence of pain.
- Cerebral form - typical for older people with persistent cerebrovascular accident. At the same time, myocardial ischemia is accompanied by neurological disorders - confused speech, dizziness, loss of coordination, and possibly depression of consciousness.
- The asymptomatic form is more common in patients with diabetes. The attack itself is accompanied by increased irritability and heavy sweating, but the patient does not experience any pain. If such a heart attack did not have a large area of myocardial damage, then it is detected during the next preventive examination on an ECG.
All of the above symptoms indicate the onset of necrosis of a section of the heart muscle and require calling an ambulance. Treatment of the disease is carried out exclusively in inpatient settings.
Useful video
Useful information from doctors about the signs of a heart attack in women can be found in this video:
Content
Among heart and vascular diseases, one of the most dangerous is myocardial infarction. It manifests itself as sharp pain in the heart, often loss of consciousness, and can even lead to death. At the same time, the symptoms of the disease can occur differently in the stronger and weaker sex. In order to correctly recognize the signs of a heart attack in women, you need to have a good understanding of the causes of the disease, its clinical picture, as well as the first aid measures that you need to be able to provide to each person.
The first signs of the disease
Most often, symptoms of a heart attack in women occur some time (at least a month) before the onset of the disease itself.
In general, this is a deterioration in the general condition, which manifests itself in the following:
- Shortness of breath is often the first symptom.
- Constant fatigue, premature onset of fatigue and loss of strength.
- Increased heart rate even after slight physical exertion.
- Aching or tingling pain in the left side.
- Mood swings, unexplained anxiety.
- Snoring during sleep, sudden stops in breathing.
- Swelling in the lower extremities, causing them to become weak and lethargic.
- Increased frequency of headaches.
- Bleeding gums.
- More frequent trips to the toilet at night (increased urination).
Usually, the first signs of myocardial infarction in women are similar to the symptoms of ordinary fatigue, so women often do not pay much attention to them, attributing everything to stress and age-related changes. However, the only right decision in this case would be to consult a doctor, since if this is not done in time, the symptoms will only intensify, and an attack can occur suddenly and quickly.
Typically, the first signs of a heart attack in women occur several months before the possible onset of acute ones, so by quickly contacting a doctor, severe consequences can be avoided.
What to do when the first signs of a heart attack appear
If you suspect that a heart attack is approaching, even at home you need to take a number of measures aimed at avoiding serious consequences:
- Call an ambulance immediately.
- If you feel attacks of panic, fear and cannot force yourself to be at peace, take any sedative.
- Drink 300 mg. “Aspirin”, after chewing it. This drug thins the blood and prevents new blood clots from forming.
Having understood the principles of the occurrence of this disease and learned how to determine myocardial infarction before the doctor arrives, one can hope that by seeking medical help in a timely manner, the most severe consequences will be avoided. Remember: saving your life and avoiding severe disability is possible with careful attention to your health. What consequences will occur after the treatment is the responsibility of not only the doctor, but also his patient.