According to statistics obtained from recent scientific studies, thrombocytopenia (low blood platelet levels) is a fairly common phenomenon. Approximately 2% of the population has encountered this problem at least once. This condition can occur due to a number of reasons, and may also be congenital. If platelets are low in an adult, what does this tell us and how to deal with this disease?
Causes of Low Platelets
If a blood test reveals a small number of platelets, this may indicate the following:
- platelets are formed in the body in small quantities;
- accumulate in the spleen in the depot;
- are destroyed by the body when they are already mature;
- are lost due to chronic bleeding.
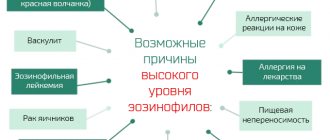
Thrombocytopenia can be due to various reasons. It is often associated with the rapid destruction of these cells. The main reasons for the decrease in this case:
- autoimmune thrombocytopenia, which develops as a result of improper functioning of the immune system (leukocytes destroy healthy cells of the body, mistaking them for foreign or pathological);
- blood transfusion;
- severe injuries;
- vasculitis, diffuse connective tissue diseases (for example, lupus erythematosus).
Platelets may fall due to the fact that their production in the body is reduced. This is typical for such diseases:
- viral infections;
- tumors and metastasis in the bone marrow;
- drug addiction and alcoholism.
Thrombocytopenia develops with an enlarged spleen. This happens:
- for leukemia;
- infectious processes;
- liver cirrhosis.
Thrombocytopenia in children has some features. The reasons for a low level are usually the following:
- In newborns, it may be associated with a conflict between maternal antibodies and child antigens.
- At the age of 4 to 6 months, it can develop against the background of hemolytic-uremic syndrome. The disease is characterized by two more symptoms - hemolytic anemia and renal failure.
- In children, thrombocytopenia is most often associated with congenital pathology and idiopathic.
In adults, thrombocytopenia of autoimmune origin and secondary thrombocytopenia, which is a sign of another disease, are more often observed.
Causes for men and women
Thrombocytopenia is thought to be more common in women than in men. Low platelets occur with congenital pathologies and various somatic diseases. The reasons for low rates in men and women are similar. Congenital thrombocytopenias are usually accompanied by structural changes in cells (thrombocytopathy). Examples of hereditary thrombocytopenias:
- Fanconi anemia;
- May-Hegglin anomaly;
- Bernard-Soulier syndrome;
- Wiskott-Aldrich syndrome.
The causes of low levels of thrombotic cells as a symptomatic manifestation are more varied and include:
- picornavirus infection;
- infectious mononucleosis and other diseases.
Blood cell ratio in thrombocytopenia
In addition, the cause of a decrease in platelets in the blood is often acute hepatitis or thyrotoxicosis, food allergies, or long-term use of certain medications.
Rapid platelet destruction caused by the formation of antithrombotic antibodies is observed in systemic lupus erythematosus and other autoimmune conditions. Frequent reasons why platelets in the blood decrease are tumor metastases, hemoblastosis, hematopoietic aplasia, B-12 deficiency anemia, splenomegaly (enlarged spleen) and others.
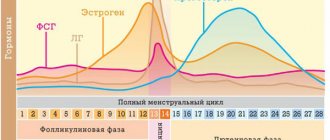
As you can see, there are many reasons for low platelets, which are consequences of pathological conditions in adults, but physiological factors can also provoke thrombocytopenia. For example, a woman’s low platelet count indicates that her period has begun or just ended, or that she is pregnant. The cause of a woman's platelet level falling below normal is blood loss associated with labor. Excessive physical or mental stress, chronic intoxication (alcohol, nicotine), poor diet are also causes.
If there are few platelets in the blood of an adult, this means that he has developed thrombocytopenia, which is a sign of physiological or pathological conditions, congenital or acquired.
During pregnancy
Women often experience low platelet counts during pregnancy, especially in the third trimester. The reasons for the decrease may be the following:
- changes in hormonal balance, leading to a decrease in the lifespan of blood platelets;
- an increase in the amount of circulating blood during pregnancy, while the concentration of all formed elements, including platelets, decreases;
- infectious processes;
- autoimmune diseases;
- lack of folic acid and vitamin B 12;
- obstetric hemorrhage caused by various reasons, including the manipulations of health workers.
Most often, during pregnancy, platelets are not much lower than normal, and this does not manifest itself in any way. But if they have dropped significantly, clinical signs and the risk of bleeding appear, you need to consult a doctor and start treatment. This condition during childbirth can be dangerous for the expectant mother.
Thrombocytopenia in pregnant women and children
The platelet rate for pregnant women decreases
A decrease in platelet levels in pregnant women is considered a physiological norm; in approximately 10% of cases it can reach fairly low numbers. Doctors associate this condition of the body with malfunctions of the immune system, which are especially pronounced in the last trimester.
The most susceptible to thrombocytopenia are those women who have had other pathologies during pregnancy: viral and bacterial infections, preeclampsia and eclampsia, a marked increase in blood pressure. In rare cases, idiopathic thrombocytopenic purpura may occur during pregnancy, a disease associated with the rapid death of platelets that are formed and requiring drug treatment. A mild form of platelet reduction occurs in approximately 20% of newborns born to mothers with thrombocytopenic purpura.
In children, the main cause of thrombocytopenia in the first months of life is prematurity. This is due to the fact that all body systems of such a child are not sufficiently adapted to life outside the mother’s body; platelets can be formed in the red bone marrow in insufficient quantities and in an altered shape, which leads to their rapid death.
Hemolytic disease of the newborn is a cause of thrombocytopenia
The second most common cause is hemolytic disease of the newborn. First of all, it manifests itself as jaundice - a yellow discoloration of the sclera, skin and mucous membranes; in severe cases, this condition requires drug therapy in addition to light therapy.
The reason for a decrease in platelet levels in later childhood may be a lack of protein in the diet, as well as a reduced intake of B vitamins (especially B 12) and folic acid.
Rare causes of thrombocytopenia in children include hereditary diseases and syndromes (Fisher-Evans syndrome, Wiskott-Aldrich syndrome, Fanconi syndrome and others). It is worth noting that the incidence rate of most of them does not exceed 1 case per 10-100 thousand people.
Clinical manifestations of the disease
The following symptoms will help you suspect a decrease in platelets in the blood:
- Prolonged bleeding after minor injuries;
- Formation of large hematomas and bruises with minor bruises;
- Bleeding gums for no apparent reason;
- Small pinpoint hemorrhages on the skin in the form of a rash, which tend to merge into large spots;
- Constant nosebleeds and hemorrhages in the conjunctiva of the eye against the background of normal blood pressure;
In most cases of a slight decrease in platelets, no symptoms occur. This leaves this condition undetected for a long time. Only a critical decrease in platelet cells or a random blood test can suggest an existing problem.
Hemorrhagic rash with thrombocytopenia
What does it mean
Platelets are called red blood cells, the main task of which is to ensure normal blood clotting. When the number of platelets in the blood drops significantly, the cells are unable to perform their function properly. This pathological condition is called thrombocytopenia. Its symptoms: an increase in the time required to stop bleeding, regular releases of blood from the mucous membranes of the nose and mouth, and the appearance of bruises of unknown origin on the body.
Throughout the day, the level of platelets in the blood may fluctuate slightly, deviating from the norm by 5-10 percent. In this case, there is no talk of any violations. In addition, a slight decrease in platelets is considered normal during menstruation and pregnancy. These symptoms are temporary and do not require any treatment.
Analysis to determine
A general blood test is designed to calculate the number of platelets and other indicators (leukocytes, red blood cells, etc.).
But in a clinical analysis, only the number of platelets is determined. Important! To establish the percentage of different cell forms, it is necessary to make a detailed or general coagulogram. This test will evaluate platelet morphology (size, condition, shape and structure)
Preparing for analysis
Blood is drawn in the morning, at 9 – 11 o’clock. Before taking the test, you should not eat, drink sweet or carbonated drinks. Drinking clean water is allowed. Three hours before the pick-up, you are not allowed to smoke. On the eve of the tests, you should avoid alcohol. If the patient is taking any medications or undergoing physical therapy, the doctor must be informed about this.
Treatment
A low platelet count is often a symptom of a serious disease, so cases of its detection require the mandatory elimination of underlying diseases.
Urgent care for the patient is necessary in cases of bleeding due to thrombocytopenia. The main goal of therapy is to prevent extensive blood loss. A person is advised to administer hemostatic drugs, such as:
- Etamsylate;
- Vikasol;
- Aminocaproic acid;
- They also resort to platelet transfusion from a donor.
After the patient’s condition has stabilized, the necessary examination and planned treatment are carried out. When treating low platelet levels in autoimmune diseases, therapy is carried out with glucocorticosteroids, such as Cortinef, Methylprednisolone, Dexamethasone, etc.
If platelets are destroyed by the spleen, then there is a need for organ resection. If platelets are still low after removal of the spleen, chemotherapy is indicated.
To stimulate platelet synthesis, folic acid, vitamin B12, thrombopoietin Revolade, and biostimulants are used.
Sometimes the platelet concentration can be reduced by general therapeutic measures:
- Discontinuation of medications that could cause a decrease in platelet concentrations;
- A balanced diet rich in vitamins and microelements;
- Treatment of infectious diseases;
- Quitting the use of tobacco and alcohol;
- Healing Fitness;
- Taking vitamin preparations.
Prognosis and complications
The prognosis of thrombocytopenia depends on the disease or condition that caused it. So, if it was caused by physiological reasons, then it is favorable, the platelet count will return to normal. In the case of autoimmune diseases, the prognosis is serious and depends on the stage of the pathological process, the adequacy and timeliness of treatment. Blood cancer has a poor prognosis, with a five-year survival rate of no more than 10–12 percent.
The main and serious complication of thrombocytopenia can be internal bleeding, which without emergency treatment can be fatal.
Consequences of long-term retention below normal
Today, the diagnosis of thrombocytopenia is not a death sentence for a person, especially if the cause of the low content of this blood fraction is known and treated. The general prognosis for the disease for such individuals is favorable.
If there are signs of severe chronic thrombocytopenia, there is a risk of death. The risk involves the possibility of severe bleeding or bleeding in the brain. A high risk of severe consequences in adults is indicated by the following symptomatic manifestations, characteristic of men and women:
- frequent subcutaneous bruising, called ecchymoses, petechiae, purpura;
- bleeding gums;
- bleeding from the wound and the inability to stop it in more than 5 minutes;
- profuse nosebleeds;
- tendency of the skin to form long-lasting bruises (ecchymosis).
Heavy and prolonged periods in a woman sometimes mean that the level of platelets in her blood is low. If this condition becomes chronic, it can lead to iron deficiency anemia and other pathologies.
The greatest danger comes from internal bleeding, which often results in hemorrhage in the retina or brain. The first threatens blindness, and in the second case, death is possible.
How it manifests itself
The symptomatic picture, with a moderate course of the disease, does not differ in bright, obvious signs. However, the severe form is characterized by the following negative manifestations:
- numerous, profuse nosebleeds
- When receiving a wound, regardless of size, blood loss is significant
- bruises appear on the body
- possible bleeding from the oral mucosa, bleeding gums
Diagnosis
Here is a list of measures that are necessary to make an accurate diagnosis:
- visit to the hematologist's office
- taking blood tests (general, biochemical)
- identification of factors influencing blood clotting
- detection of autoantibodies to platelets
- trephine biopsy of bone marrow
- aspiration biopsy
How is thrombocytopenia treated?
The administration of glucocorticoid drugs, including prednisolone, helps to increase the level of platelets in the blood. Reasons for use:
- there are signs of increased hemorrhagic syndrome
- rashes on the skin, oral mucosa
- hemorrhages in the conjunctiva were noted
- a critically low platelet count is stated, less than 30,000 in 1 μl
It is worth noting that taking this hormonal drug, which belongs to the steroid class, has negative consequences for the body. List of side effects:
- weight increases rapidly
- the body “leaves” potassium and magnesium - extremely important microelements
- the gastric mucosa experiences a massive negative impact
However, despite the above, therapy for autoimmune thrombocytopenia by taking prednisolone is considered a fundamental method of treating such a blood disease. The effectiveness of the treatment process is evident after the first days of treatment.
Initially, the negative consequences disappear (bleeding of the mucous membranes is minimized), and then an increase in platelet levels is noted.
When the mark of 100 thousand per 1 μl is exceeded, the dose of the drug is gradually reduced.
Sometimes, a one-time course of hormonal therapy is enough to normalize the condition.
Often, an attempt to stop taking hormones, or an inadequate dose reduction, are catalysts for a relapse.
The problem worsens again, “requiring” a return to high doses of the drug. For every tenth patient, treatment with glucocorticosteroids does not bring the desired results.
Although the bleeding can be controlled, thrombocytopenia still remains unconquered.
Long-term remissions, after treatment with hormonal drugs, are recorded in 25% of those suffering from this pathology.
After several months (3-4), in the absence of positive changes after the use of glucocorticoids, or the presence of serious complications caused by taking the drug, the possibility of splenectomy is considered. The procedure for removing the spleen, in the vast majority of patients (more than 70%), radically improves the situation. Persistent improvements are recorded, and a steady increase in platelet levels is noted.
We will definitely mention another method of combating thrombocytopenia. In case of unsatisfactory results after the operation (ineffective removal of the spleen), cytostatic immunosuppressive therapy is resorted to. As immunosuppressants, preference is given to the following drugs: vincristine, cyclophosphamide. The treatment is long-term, the course duration is 3-5 months.
Cytostatic therapy involves an individual approach, choosing the most effective drugs. In this situation, it is not possible to predict the effectiveness of an immunosuppressant in advance. There are no clear evaluation criteria.
This form of treatment is considered as an extreme, exceptional measure to counteract thrombocytopenia. Use is appropriate when the effectiveness of splenectomy is low.
Sometimes, before courses of hormonal therapy, hematologists prescribe a plasmapheresis procedure. From the blood taken from the patient, the liquid part - plasma, which contains toxic components - is isolated and removed.
Prevention of thrombocytopenia
It is strongly recommended to minimize:
- rectal examinations
- intramuscular injections
- enemas
Drugs that reduce platelet function are prohibited. These include:
- nonsteroidal anti-inflammatory drugs
- aspirin, its derivatives
Use soft toothbrushes. Avoid using straight razors and dental floss.
In a nutritious diet, increase the share of foods: pomegranate, apricot, beets - which have a positive effect on the process of hematopoiesis.
If you receive an injury accompanied by loss of blood, even minor, for people suffering from thrombocytopenia, it is advisable to immediately consult a doctor, if possible a hematologist.
How to lift
If your platelet level decreases, you need to evaluate your condition.
In certain cases, platelet levels drop to a critical level, which requires immediate treatment - on an outpatient or inpatient basis. However, most often the violation is so minor that it can be dealt with at home. To raise your platelet levels on your own, use the following recommendations:
- Make a proper diet. Include greens, citrus fruits, kiwi, tomatoes and berries. Avoid undiluted coffee, alcohol, excessively fatty and high-calorie foods, and refined sugar.
- Include foods rich in omega-3 acids in your diet. These products include: fatty fish, eggs, flaxseed oil. A worthy alternative could be fish oil capsules.
- Follow a daily routine. Try to get up and go to bed on time, sleep at least 8 hours a day. Do not forget about vacation, which gives the body the opportunity to “reboot”.
- Drink liquid at room temperature. Drinking cold drinks disrupts the functioning of the gastrointestinal tract and contributes to poorer absorption of nutrients.
- Enrich your diet with minerals and vitamins. You can get them from healthy foods or from special vitamin and mineral complexes.
- Play sports. In physical activity, the emphasis should be placed not on strength training, but on “cardio”. Cardio exercises have the most positive effect on the body: they normalize blood circulation and strengthen the immune system.
Correction of platelet levels
Successful correction is possible if the cause of thrombocytopenia is identified
With a pronounced decrease in the number of blood platelets, the most accessible and quick means of correction is the transfusion of donor platelet mass; this manipulation is carried out in life-threatening conditions. In cases where the decrease is not so significant, plasmapheresis and treatment with hormonal drugs can be performed.
For mild thrombocytopenia, maintenance therapy is used:
- Course intake of multivitamin complexes;
- Treatment with vitamin B12 in high dosage (most often in the form of injections);
- Taking therapeutic doses of iron;
- Herbal medicine using chokeberry fruits and yarrow leaves.
Diagnosis and risk groups
Platelets are important cells in our body. If you notice signs in yourself that indicate a decrease in such cells, then you need to take and interpret a blood test in a regular clinic. If the decoding result shows a low platelet count, then measures must be taken to normalize it.
All people are at risk for low platelet counts. Why? Because no one is immune from contracting an infection, be it a respiratory or any other disease. Is it possible to reduce the likelihood of such a disease? Yes it is possible. To do this, it is necessary to strengthen the immune system as a whole. You can resort to hardening procedures, moderate physical activity, proper balanced nutrition and other methods.
Symptoms of low platelets
A low platelet count cannot always be detected independently. The main way to determine thrombocytopenia is a complete blood count.
However, low platelet counts are characterized by severe blood loss from cuts or injuries, hemorrhages of various origins (nasal, intestinal, eye, mouth, skin, etc.), the formation of bruises even from weak blows, and a reduced level of hemoglobin in the blood.
It is important to remember that you should not draw terrible conclusions based solely on the above symptoms of a low platelet level. Only a doctor can make a correct diagnosis based on laboratory tests.
What determines the platelet count in the blood?
A decrease in platelets can be either an independent disease or a symptom accompanying the disease.
There are three main causes of low platelet count:
- insufficient production of blood cells by the bone marrow (this disorder is associated with the presence of viruses, infections, malignant or benign tumors in the body, and the use of potent blood thinning drugs);
- rapid destruction and inferiority of blood cells (occurs in an autoimmune disease, when antibodies are produced, or when infected with E. coli);
- improper distribution of blood cells in the vessels, resulting in a decrease in the number of blood cells in the bloodstream (the cause may be problems with the functioning of the spleen, for example, with hepatitis).
Common causes of thrombocytopenia
- hereditary predisposition;
- congenital anomaly;
- prematurity of the child, especially with complicated pregnancy;
- incorrect combination of medications and their side effects;
- unbalanced diet;
- viral diseases that become chronic and cannot be treated;
- systemic autoimmune diseases (rheumatoid arthritis, lupus erythematosus), leading to the destruction of platelets by antibodies;
- severe intoxication;
- weakened immunity combined with constant exposure to allergens.
All the reasons causing the problem can be combined into 3 groups:
- decreased production of platelets by the bone marrow;
- increased destruction of platelets;
- disruptions in the distribution of platelets in the circulatory system, which causes their deficiency in the peripheral blood.
How does thrombocytopenia manifest?
Nosebleeds are a possible sign of thrombocytopenia.
The severity of thrombocytopenia depends on how much the platelet concentration in the blood is reduced. At concentrations of more than 100⋅109/L, patients may be practically undisturbed; the first manifestations of a reduced platelet count, as a rule, are mild bruising, as well as prolonged bleeding after minor skin injuries.
With a significant decrease in concentration below 100⋅109/l, the condition begins to deteriorate; as a rule, several of the following symptoms are disturbing:
- Rashes in the form of dots and small threads of dark brown and bluish colors spontaneously appear on the skin and mucous membranes in various places;
- Bleeding may occur in the whites of the eyes and is not associated with any visible damage. In severe cases, the white of the eye may completely “swim” with blood;
- Changes on the tongue and cheeks, similar to small hematomas, a small brown rash;
- Nosebleeds that are difficult to stop. They may often experience vomiting due to ingestion of blood;
- Menstrual irregularities - the appearance of bleeding outside the prescribed period, excessively heavy menstruation;
- Darkening of feces, urine mixed with blood or cloudy.
Treatment with folk remedies
To increase blood density, traditional methods are used along with drug therapy. To increase platelet levels, brew and drink herbal teas:
- from currant leaves,
- rose hips,
- thyme,
- coltsfoot.
It is recommended to include sesame oil in your food and eat more onions and garlic. Sesame oil improves the process of blood clotting; it should be consumed every day, 10 g. Aloe juice and Echinacea purpurea help to improve immunity.
A proven remedy for liquid blood is a decoction of nettles. To prepare it, pour 10 grams of nettle with water (250 ml) and boil for about 10 minutes. Drink the product three times a day.
Another effective medicine is verbena infusion, which should be taken for a month, a glass a day. To prepare, take five grams of verbena and pour boiling water (250 ml), then leave for about 30 minutes.
Formation and functions of thromboplastins
Colorless, nuclear-free blood elements are fragments of megakaryocytes located in the red bone marrow in the form of a mesh frame. When maturing, megakaryocytes “unlace” the cytoplasm - young platelets are formed.
Interesting! The bone marrow is not the only place of platelet production in humans. The lungs form part of the formed elements, as well as a reserve of stem cells in case the bone marrow begins to work intermittently.
The cells can be round or oval, and the size, depending on the stage of maturation, is 2 - 5 microns. They live for 7-12 days, then the platelets are destroyed by macrophages in the red marrow. A small percentage is killed in the liver and spleen.
The main job of these formed elements is blood clotting. This ability is based on three properties that allow the formation of blood clots:
- Adhesion – sticking to surfaces.
- Aggregation is the ability of particles to stick together.
- Adsorption – deposition on blood clotting factors.
In a calm state, thromboplastins are negatively charged. They circulate in the blood, pushing off from the vascular endothelium, allowing the blood flow to easily spread through vessels of different diameters, freely bypassing branches. In this way, blood fluidity improves, and oxygen is delivered in a timely manner by the blood to the cells of organs and tissues.
When a section of a vessel is damaged (the formation of an atherosclerotic plaque), platelets become positively charged due to the rapid formation of protrusions-pedicles and adhere to the adhesive molecules of the inner surface of the vessels. Von Willebrand factor and calcium play a big role in this - they help the platelet quickly grow and change shape to increase the surface area interacting with other cells. Next, thromboplastins activate the release from cells of substances responsible for vasoconstriction: serotonin, thromboxane, adrenaline, as well as growth and coagulation substances.
Platelets not only clog damaged areas of blood vessels. Cells perform a number of other important functions:
- Nutrition and healing - supply growth factors that activate healing processes to the cells of the vascular wall.
- Hemostatics - they trigger the primary coagulation link.
- Transport of hormones and enzymes.
- Capture viruses and antigens.
By participating in the delivery of protein molecules to the organs and systems of the body, platelets ensure an adequate metabolic rate. Binding of foreign agents plays an important role in maintaining immune defense.
Treatment and prevention
If a person notices signs of poor blood clotting, he should immediately consult a doctor. To make a diagnosis and find out the causes of the development of the disease, the following studies are recommended to the patient:
- antibody test;
- magnetic resonance imaging of the abdominal organs;
- Ultrasound examination of the liver and spleen.
If there is a suspicion of a congenital pathology, the patient is examined by a geneticist. All of these studies apply to both adults and children.
Therapy depends on the causes of the disease. If a decrease in platelets is caused by other pathologies, treatment must be started immediately, after which the content of these cells in the blood will return to normal. If pathology occurs against the background of autoimmune diseases or disruption of the hematopoietic process, treatment will consist of drug therapy and the creation of special conditions for the patient. The child is prescribed bed rest and maximum limitation of traumatic situations.
If platelets are destroyed by antibodies produced by the body, the patient is indicated for hormonal therapy, as well as immunoglobulin injections and interferon treatment. If hormonal therapy is unsuccessful, the person may have their spleen removed. The patient may also be indicated for several sessions of plasmapheresis (replacing blood with purified plasma), and in critical cases, platelet transfusion. Internal or local use of Aminocaproic acid is indicated for adults and children with a tendency to hemorrhage. Your doctor may also prescribe vitamin A, C, and B12.
Low platelet levels can be corrected with nutrition. It should be enriched:
- green apples;
- celery;
- lingonberries;
- liver;
- fresh herbs;
- red meat;
- bananas.
Women experiencing menstruation should also consider these products. Alcohol, pickles, marinades, and fast food should be avoided
It is advisable to limit the consumption of blood thinning products (green tea, rose hips, citrus fruits, garlic, vegetable oil).
Both children and adults should lead a healthy lifestyle: move a lot, often be in the fresh air. But it should be remembered that physical activity with a high risk of injury is prohibited if blood clotting is poor.
- A teaspoon of fresh nettle juice is mixed with a quarter glass of water (milk) and drunk three times a day before the main meal.
- 10 grams of dry nettle leaf is poured with a glass of boiling water and the broth is boiled for 3 minutes. Then leave for half an hour in a thermos. Drink half an hour before meals.
If the platelet count is low, it is useful to consume sesame oil: a tablespoon before each meal.
Preventive measures to reduce the number of platelets include proper nutrition, giving up bad habits, and careful use of cleaning, detergents and other chemicals. Do not take medications uncontrollably
A regular biochemical blood test will help determine a decrease in platelets in a timely manner.
Low platelets and nutrition
It is impossible to create a diet to compensate for low platelet levels because it is impossible to take into account all the numerous causes of thrombocytopenia, some of which are in no way related to nutrition.
However, as with almost all unusual blood test results, the patient is interested in what is best to eat and what foods to choose. In this case, we can only give general advice - follow a well-balanced diet, in which preference is given to complex sugars (cereals), legumes, lean meat, fish, vegetable fats, polyunsaturated fatty acids (olive oil). Of course, it is necessary to limit the consumption of alcohol and intoxicants such as coffee or tea.
Main reasons
What are the main reasons for this, sometimes dangerous for humans, condition? As mentioned above, the platelet rate is different in adults and children, and the reasons for a decrease in the number of platelets may be different in children and adult men and women.
Causes of low platelets in children:
- Conflict between the blood type of the child and mother.
- Maternal diseases such as idiopathic thrombocytopenia or systemic lupus erythematosus.
- Prematurity or postmaturity.
- Various immunodeficiency and infectious diseases.
- DIC syndrome.
- Thyrotoxicosis.
- Anemia.
- Hypoxia (oxygen starvation).
- Hemodialysis.
- Taking certain medications (analgesics, antibiotics, corticosteroids).
Blood test for platelets
Causes of low platelets in adults:
- Various immunodeficiency, infectious and hereditary autoimmune diseases (herpes, AIDS, HIV, hepatitis, lupus erythematosus, etc.).
- Anemia.
- The use of medications that thin the blood.
- Drinking large amounts of strong alcoholic drinks.
- Serious injuries accompanied by large blood loss.
- Harmful effects of heavy metal salts.
- Blood leukemia.
- Pregnancy and menorrhagia (heavy menstruation) in women.
Decreased level and its causes
A condition in which the level of platelet concentration is less than 160x109/l of blood (in an adult) is called thrombocytopenia.
What does low platelet count mean?
Pathology is classified according to severity and is distinguished:
- I degree (moderately low content), in which the level of cell content in the blood varies between 50-160x109/l, and hemostasis is characterized as satisfactory;
- II degree (platelets are sharply reduced) - a decrease in platelets to the level of 20-50x109/l, which is characterized by the occurrence of hemorrhages under the skin and prolonged bleeding from wounds;
- Stage III (severe thrombocytopenia) is a condition in which the concentration of platelets in the blood is below 20x109/l. A pronounced decrease in platelets in a patient is accompanied by the development of spontaneous bleeding, both external and internal.
Severe thrombocytopenia is a reason for emergency hospitalization of the patient.
Thrombocytopenia is also classified according to its forms:
- Immune is the most common form of pathology that develops several weeks after an infectious disease or while taking certain groups of medications, including after vaccination;
- Heteroimmune - platelets are reduced due to disruption of the antigenic structure of cells by pathogenic microorganisms, toxins, chemicals;
- Isoimmune - platelets are reduced, mainly in children due to the transfer of cells from the fetus to the mother (identical to Rh factor incompatibility), as well as as a result of donor blood transfusion;
- Autoimmune is a pathology that consists of dysfunction of the immune mechanism, in which the production of antibodies to platelets begins.
Causes of low platelet levels
Only a doctor can determine how low the platelets are and what this means!
There are 3 main causes of low platelets:
- Red bone marrow dysfunction (red bone marrow does not produce the required number of platelets);
- Active production of antibodies that destroy platelets;
- Dysfunction and changes in the spleen.
The causes of moderately low platelets are:
- Abuse of alcoholic beverages, chronic alcoholism . Alcohol inhibits the functioning of the red bone marrow, leading to a lack of folic acid in the body, which is necessary for hematopoiesis. With alcoholism, platelets in the blood are reduced to 80x109/l, as evidenced by the cyanosis of the body;
- Pregnancy. A small number of platelets in pregnant women is observed due to hormonal changes, blood thinning, vitamin deficiency, etc.;
- Liver pathologies. The liver is an organ in which the synthesis of certain substances involved in the process of blood clotting occurs. A decrease in their production due to some liver diseases leads to increased bleeding and consumption of large numbers of platelets;
- Use of certain medications . The development of stage I thrombocytopenia is possible when taking diuretics, antibacterial, antitumor drugs, analgin, heparin, nitroglycerin, reserpine and vitamin K;
- Disseminated intravascular coagulation (DIC syndrome). A condition that develops in various pathologies and is characterized by rapid blood clotting in small vessels with the formation of blood clots in them, which consumes a large number of platelets;
- Heart failure. In heart failure, the blood supply to the organs of the heart is disrupted, which leads to stagnation of blood in the spleen. Also, platelet consumption occurs as a result of thrombus formation in the vessels.
- Radiation therapy. When treating tumor diseases, radiation is used, which, in addition to destroying cancer cells, can damage the red bone marrow, which leads to inevitable disturbances in the production of platelets and other blood cells;
The reason for the decrease in platelets to the stage of moderate thrombocytopenia may lie in autoimmune diseases.
A low platelet level to the point of severe thrombocytopenia can be caused by:
- Acute leukemia. In leukemia, cancer cells form in the bone red marrow, which displace physiological hematopoietic tissue, which affects the formation of platelets and red blood cells;
- Hemolytic disease of the child, the development of which is associated with incompatibility of maternal blood with fetal blood according to the group and Rh factor;
- Systemic lupus erythematosus;
- Severe form of disseminated intravascular coagulation.
Reduced platelets in the blood to critical levels are characteristic of:
- Acute radiation sickness;
- Overdose of antitumor drugs;
- Severe forms of leukemia.
Functions of platelets in the blood
Platelets are blood cells that resemble flat discs of varying diameters (0.002-0.004 mm). They are responsible for several functions in the body:
- Emergency closure of an open wound
Platelets are sometimes called the “first aid” of the blood. This name is due to their ability to quickly stop bleeding.
On the surface of platelets there are special complex compounds, due to which adhesion (sticking) of cells to each other and to the walls of blood vessels occurs. In addition, the composition of the surface of platelets includes biologically active substances that can participate in the process of blood clotting.
So, after receiving a cut in the human body, a mass of platelets is sent to the open wound, rapid division and reproduction of these cells begins, they stick to each other, forming a dense film that prevents blood loss.
- Nutrition and vasoconstriction
Platelets are involved in nourishing the walls of blood vessels, maintaining the functionality and structure of blood vessels.
- Transfer of serotonin, enzymes and other substances in the blood.
- Blood restoration
- Maintaining immunity
- Removal of killed viruses and body antigens.
Why is low platelet count dangerous?
Decreased platelet levels weaken the coagulation system
The main danger of thrombocytopenia is that the human body is defenseless against any, even the most minor, injuries.
Once the blood vessels are damaged, the blood is unable to “coagulate” and close the wall defect, so blood loss can quickly reach life-threatening levels.
In a situation where a healthy person would lose a small amount of blood, a patient with thrombocytopenia can lose tens of times more, and in most cases it can enter the body cavities, causing tissue damage. The most common complication is hemarthrosis, a condition in which the joint space becomes filled with blood, making movement in the joint impossible.
Reasons for the decrease in red plates in the blood
If the level of nuclear-free microorganisms in the analysis is below normal, then there may be several explanations for this factor.
Firstly, a certain pathological condition developing in the body can contribute to a decrease in platelets in the blood.
For this reason, the body of patients with thrombocytopenia is always examined carefully.
Secondly, a blood condition in which fewer nuclear-free red plates are found than necessary can sometimes be an independent disease.
Taking into account the above factors, the causes of thrombocytopenia can be represented by the following three points:
- decreased platelet count due to a deficiency in platelet production by the bone marrow;
- rapid destruction of platelet cells due to autoimmune pathology;
- uneven distribution of red plates in the vascular bed.
Decreased platelet levels may result from the formation of abnormally small platelets in megakaryocytes, which are then rapidly destroyed in the spleen.
It happens in the body, and vice versa, when platelets are lower than normal, because they are produced in small quantities, but at the same time their sizes are called abnormally large.
Video:
Other reasons for the rapid destruction of nuclear-free blood elements come down to autoimmune diseases, when the body perceives platelets as foreign agents and destroys them within 24 hours in the spleen.
The group of autoimmune pathologies in which the body attacks platelets includes viral and infectious diseases and genetic predisposition.
Incorrect distribution of red blood plates between internal organs (spleen, liver) and peripheral blood can be caused by
The meaning and functions of platelets
Platelets are colorless blood cells responsible for the mechanism of coagulation homeostasis or clotting. These cells begin their life cycle in the bone marrow. Since leukocytes and red blood cells also appear there, the level of platelets directly depends on the indicators of other blood cells. Platelets live no more than 11 days, and, moving through the vessels, end their journey in the spleen. It is there that the process of their destruction occurs, after which material appears for the creation of new blood cells.
Why are platelets so important to us? Thanks to their unique plate shape, platelets seem to seal damaged vessels, thereby stopping bleeding, for example, from cuts. Blood viscosity is a kind of buffer that maintains the desired flow rate in the blood vessels.
In addition to their protective function, blood cells act as unique suppliers of microelements, nourishing the endothelium of the circulatory system, which in turn ensures metabolism and protection of the body, immunity.
If the platelet count is below normal, then you may notice changes in the general condition of the body, such as regular nosebleeds, a large number of bruises on the body, and difficulties in stopping bleeding in case of injury. It is important to note that mild forms of the disease do not have significant symptoms.
With a low level of platelets, the body's protective functions are weakened, and a person becomes vulnerable to various infectious and viral diseases. The liver and thyroid gland are mainly affected.
Normal platelet count in blood
Any significant change in the level of platelets in the blood is dangerous. If platelets are below normal , then blood clotting functions are impaired. If it is higher, the likelihood of thrombosis increases.
At different periods of life, the number of blood cells changes. This is not always a symptom of something bad. There are indicators for adult men and women, women during menstruation and pregnancy, as well as for children and newborns.
For an adult male and a child over one year old, the norm is considered to be from 180∙(109) to 320∙(109) units per liter. For women - from 150∙(109) to 380∙(109) units per liter. Deviations from the norm of 10-15% are also allowed, which do not require treatment. For newborns, the figure ranges from 100∙(109) to 420∙(109) units per liter.
A platelet count test is recommended to be performed at least once a year. To get the result, it is enough to take a general blood test.
Signs that platelets are low
Very clear signs and symptoms do not accompany thrombocytopenia. You can suspect a condition in which platelets are low based on a number of manifestations:
- Heavy menstruation. Very heavy monthly bleeding may indicate several abnormalities, one of which is a reduced platelet count in the blood. The gynecologist will find out the causes of this condition and prescribe treatment;
- Hematomas. Bruises appear with very little pressure and sometimes it is impossible to remember what caused them to appear on the body;
- Frequent nosebleeds;
- Severe bleeding when soft tissue is damaged. Sometimes a simple cut can pose a threat to a person's life, in a condition where the platelets in the blood are below normal.
All signs of the disease manifest themselves in the form of violations of bleeding control. Platelets, if there are few of them in the blood, cease to perform their function of “clogging” vascular damage.
How to increase?
When looking for ways to increase platelets in the blood, one should not forget the main thing - self-medication can be life-threatening. Medicines used to urgently increase thrombotic mass have a lot of side effects and should not be used without a doctor's prescription.
If platelets are low due to medications (aspirin, etc.), you should stop using them.
There are no products that can effectively affect platelets if they are low, nor any folk remedies. These drugs can only be used as auxiliary, but not the main methods of increasing platelets.
The main way to eliminate pathological thrombocytopenia is to treat the disease that led to it.
Symptoms of thrombocytopenia
This disease manifests itself in the same way regardless of the cause. All symptoms are caused precisely by a decrease in platelet levels, and not by the mechanics of the development of pathology. Most often in people with thrombocytopenia:
- bruises appear even from minor blows and other damage to the skin;
- causeless nosebleeds occur;
- the amount of discharge during menstruation increases (in women);
- bleeding occurs in the gastrointestinal tract;
- Gums bleed when eating and brushing teeth;
- bleeding of internal organs occurs.
Most of these symptoms cannot be noticed during examinations. However, if bruises or other signs appear, you should immediately consult a doctor. The specialist will prescribe tests. He will also be able to diagnose the cause of low platelet levels. An HIV test is mandatory, because this disease often provokes the destruction of blood cells, reducing blood clotting.
Causes and consequences of thrombocytopenia
A low level of platelets in the blood indicates the development of a pathological process such as thrombocytopenia.
In adults
The disease can develop in adulthood due to the abuse of certain medications, especially those affecting the blood.
The cause of the disease can be various internal diseases:
- liver damage – hepatitis, cirrhosis;
- malfunction of the thyroid gland - hypo- and hyperthyroidism;
- alcohol abuse;
- megaloblastic anemia;
Low blood platelets may indicate megaloblastic anemia.
- bone marrow diseases.
If you do not see a doctor and receive treatment in a timely manner, difficulties may arise in the form of loss of a large amount of blood, which, in turn, can lead to additional disorders and illnesses. In this case, the immune system decreases, the body ceases to cope with various disease-provoking factors.
In pregnant women
In most cases, the first signs of thrombocytopenia during pregnancy occur in the 3rd trimester. This is due to increased stress on the entire body.
Low platelets in the blood, the causes of which can only be determined after special studies, can form in pregnant women with a disease such as lupus erythematosus. The mother’s immune system mistakenly perceives the cells of the developing organism as foreign.
Additional reasons:
- late gestosis;
- low folate levels;
- complications after preeclampsia;
- infectious lesions;
- allergic reactions;
- low quality of food consumed.
Among the external factors affecting the level of blood platelets is the improper use of medications that thin the blood.
The condition is considered dangerous and can lead to complications during childbirth. Open bleeding can cause a cerebral hemorrhage in a child. The pathology requires constant monitoring by a specialist and timely therapy.
In children
The disease in childhood is divided into primary and secondary forms. In the first case, the pathology is caused by autoimmune disorders, in which the child’s body experiences increased production of antibodies to platelets.
The causes of the secondary form are internal diseases and conditions:
- blood diseases;
- allergic reactions;
- poisoning with toxic substances;
- infectious lesion;
- endocrine disorders;
- renal failure.
The development of pathology can be triggered by an enlarged spleen. A similar phenomenon occurs with the development of liver cirrhosis or hepatitis. The condition requires surgical treatment due to the high risks of complications and consequences in the form of hemorrhages.
In teenagers
In adolescence, the provocateurs of a low level of blood cells in the blood are various diseases of the internal organs, blood diseases or toxic poisoning. Untimely treatment in adolescents can lead to bleeding, significant blood loss and cerebral hemorrhages.
Platelets: what are they?
A platelet is an element of blood, shaped like a small colorless plate. It is formed with the help of bone marrow plasma cells. The platelet does not have a nucleus; it consists entirely of tiny granules.
The shape is round, but can take on more oval shapes. When platelets move freely, their size does not exceed 5 microns. When touching the vascular wall or cardiac cavity, the platelet begins active activity.
It develops up to a dozen processes, which are 6-8 times larger than its size. Thanks to this property, bleeding stops in case of abrasions and cuts.
What platelet level is considered low?
The normal level of blood platelets under the age of one year is considered to be above 180 x 10 9 / l, and for children older than one year - 160 x 10 9 / l.
In newborns, the number of platelets per liter of blood can be 100 x 10 9, which is also considered normal.
Gradually, the platelet number increases, reaching at least 150 x 10 9 / l at 10 days of age.
If the blood test form of a child of any age indicates that the platelet count is less than 100 x 10 9 /L, this condition is called thrombocytopenia. As a result of a lower number of platelets, the blood thins and clots poorly, leading to an increased risk of both internal and external bleeding.
How platelets die
Moscow State University scientists: to stop bleeding, the platelet must “die”
Press service of Moscow State University
A team of scientists led by physicists from Moscow University discovered the mechanism of programmed cell death of platelets, as a result of which the blood clotting process is accelerated by 1000 - 10,000 times. The results of the study were published in the Journal of Thrombosis and Haemostasis (Obydennyy et al., Dynamics of calcium spiking, mitochondrial collapse and phosphatidylserine exposure in platelet subpopulations during activation).
Platelets are cells found in the blood that are responsible for stopping bleeding: they recognize when a blood vessel is damaged and clump together, creating strong aggregates and preventing blood loss. This process is called hemostasis (from the Greek haimatos - blood, stasis - stop). The ability to stick together and clog a damaged area of a vessel is obtained by platelets as a result of the activation process. Scientists believe that the platelet is one of the simplest cells in the human body, and the task of its entire life is to decide whether to activate or not. But, despite the fact that it is already well known how platelets are structured, questions still remain about the mechanisms of their functioning. The article, the leading author of which is Professor of the Department of Medical Physics of the Faculty of Physics of Moscow State University, Doctor of Physical and Mathematical Sciences Mikhail Panteleev, is devoted to how the process of platelet activation occurs.
There are two types of activated platelets: simple (aggregating) and overactivated (procoagulant).
On the left is a regular activated platelet (photo from a scanning electron microscope), on the right is a superactivated platelet (photo from a transmission electron microscope). Source: Mikhail Panteleev
When activated, simple aggregating platelets do not enlarge and take on an amoeboid shape with many legs for better adhesion and can spread over the surface. Such platelets form the main body of the thrombus. And overactivated platelets, when activated, become spherical and increase several times (in English terminology they are called “balloons”). They are able to strengthen blood clots and accelerate blood clotting reactions. But the question remained: how do these cells, when activated, divide into two types? A team of scientists has solved the most important mystery of platelet signaling.
It's all about the mitochondria. It is believed that mitochondria - organelles present in all animal (and plant) cells without exception, including platelets - provide them with energy through redox reactions.
“But it seems that platelets need mitochondria not so much for energy, but for quick suicide,” Mikhail Panteleev begins the story.
Scientists were able to show how cellular death of platelets (mitochondrial necrosis) triggers a chain of processes leading to the transition of platelets to a hyperactivated state. In other words, in order for a platelet to become over-activated, it needs to die, because their purpose begins from the moment they “died.” For this reason, platelets are also called “kamikaze cells.”
“Previously, no one understood how a platelet decides which population to go into. We have deciphered the sequence of events: how signaling occurs in a platelet, and how this cell makes a decision about death,” says Mikhail Panteleev.
The process of mitochondrial necrosis in detail. Two platelets are spread out on the substrate. Living mitochondria glow green, and red indicates a marker for cell death. The platelet on the left dies as a result of mitochondrial collapse, while its neighbor on the right lives peacefully. Photographs from a confocal microscope. Source: Mikhail Panteleev
Together with colleagues from the Federal Scientific Center for Children's Orthopedics and Orthopedics named after. Dmitry Rogachev, Center for Theoretical Problems of Physico-Chemical Pharmacology of the Russian Academy of Sciences and the Faculty of Therapeutics of the Russian National Research Medical University named after. N.I. Pirogov scientists have found that the activation process proceeds as follows. The platelet has many activators, but the main ones are: collagen, ADP and thrombyl. The platelet receives different concentrations of the activator, and it responds to them with different pulse frequencies of calcium concentrations in the cytoplasm. This phenomenon is called calcium oscillations. The mitochondria of a platelet take up and accumulate calcium, and when its concentration exceeds a critical level, the process of mitochondrial necrosis (cell death) of platelets starts: calcium and reactive oxygen species splash out from the mitochondria, the cell cytoskeleton is destroyed, and the platelet greatly increases in volume. As a result, the lipid phosphatidylserine appears on the outer membrane of the spherical platelet, which has increased in size, and is responsible for rapid blood clotting. And all this happens at lightning speed.
Last year, the same group of researchers published an article in the journal Molecular BioSystems on the theoretical mechanism of mitochondrial necrosis; in this work, this process was experimentally proven.
Moreover, another article by Mikhail Panteleev and his colleagues (“Systems biology insights into the meaning of the platelet's dual-receptor thrombin singalling”) from the Faculty of Physics and the Faculty of Fundamental Medicine of Moscow State University has been accepted for publication. Scientists explain an interesting mystery about the intracellular signaling of platelets: for the first time, it was shown that the same activator has two receptors in a platelet to achieve maximum sensitivity.
Portal “Eternal Youth” https://vechnayamolodost.ru 08.24.2016
Disease prevention
Prevention is based on preventing the disease or its complications.
Main rules of prevention:
- be careful! It is very important to prevent the appearance of bruises, wounds and hemorrhages, which will contribute to large blood loss;
- reduce physical activity to reduce blood flow;
- do not take aspirin or non-steroidal drugs, as they interfere with the proper functioning of platelets and provoke internal bleeding.
Reference! A person who has experienced a low platelet count in the blood at least once in his life is required to conduct a blood test once every six months.
Author: Content · Published 12/13/2014 · Updated 10/17/2018
Contents of this article:
Normally, the number of cells responsible for blood clotting (platelets) should be in the range of 150,000–400,000 per milliliter. The platelet count is not always within these limits. Depending on various factors, the analysis may show low platelets or, conversely, an excess of them. In medicine, such phenomena are called thrombocytopenia and thrombocytosis, respectively. Conditions of the body in which platelets are low will be discussed later in this article.
How can you determine your platelet count?
To study the state of the platelet link and determine how many cellular elements are contained in the blood, the usual routine methods, which is a general blood test, are sufficient. It can be carried out using standard examination under a microscope or the latest automatic analyzers. In any case, the study requires blood from a finger (capillary).
Usually, when assessing the results of an analysis carried out by microscopic examination, no questions arise, since all indicators, including platelets, are presented in an understandable style. The only difficulty can be in assessing the results of automated analysis. Platelets in it are designated by the abbreviation of the Latin letters PLT. Next to it are numbers that correspond to the result obtained. If there are deviations from the norm, a repeat blood test is mandatory.
Platelets are very important elements of the blood, the study of which is not very difficult. But the assessment of test results and, moreover, their correct interpretation in the event of deviations from the norm should be carried out exclusively by a knowledgeable specialist.
Existing types of thrombocytopenia
This pathology can be either congenital or develop over time. The majority of cases are acquired over time. And directly in a larger number of acquired ones, the factor of low platelets is reactions of an immune nature.
They are divided according to mechanisms into 4 groups:
- Autoimmune. Noticing platelet protein in the blood, the body secretes antibodies against it, considering it harmful; this disease is called autoimmune thrombocytopenia. Cancer, rubella, HIV, as well as autoimmune diseases and the use of certain drugs contribute to their development;
- Alloimmune. Appear as a result of platelet collapse, in the case of incompatible blood group, or during the production of antibodies;
- Transimmune. Antibodies in this scenario penetrate directly from the mother infected with autoimmune platelet disease to the child, transmitted through the placenta;
- Heteroimmune. The body produces antibodies due to the formation of a new antigen in the body, or infection of the red plate protein with viral diseases.
Physiological role for the body
Human blood, in addition to maintaining a liquid state, must have sufficient viscosity. This is necessary in order to create a kind of buffer that is able to retain all its cellular components in the lumen of the vascular bed. And platelets do this. These cells are in a state of high alert and are able to instantly perform their functions in the event of the slightest threat of blood loss.
Due to their small size and large number of platelet blood cells compared to other cellular elements, most of them accumulate near the wall of blood vessels. From the inside it is lined with a specific membrane called intima, formed by endothelial cells. While no pathological changes occur in the body, platelets, which have a negative charge on the cell membrane, are repelled from the endothelium. This allows blood to circulate freely through the branching vessels.
Platelets are the first to respond to damage to the vascular wall
Platelet activation occurs when:
- Minimal changes in the vascular endothelium, which could result from atherosclerosis or an inflammatory process;
- The appearance of collagen in the blood, which is released during injury or intersection of the vascular wall;
- Excessive production of blood clotting factors by the liver;
- Any serious illnesses and critical conditions accompanied by dehydration and severe intoxication.
This triggers a chain of physiological reactions and mechanisms, during which these cells try not only to restore the integrity of the blood vessels, but also to maintain the blood in such a state that it can circulate under conditions of increased viscosity. This is the main function of platelets. The chain of transformation and activation is presented as follows:
More article: Causes of increased platelets in the blood
- Change in platelet membrane charge. This leads to the fact that they begin to adhere (stick) to the site of damage to the vascular wall and to each other;
- Change in platelet shape. Instantly, multiple specific processes appear on the surface of platelets, due to which they acquire a chaotic structure and stellate shape. This feature increases the cell area;
- Accumulation of cells in pathological areas of the vascular bed. In this case, conglomerates are formed, allowing the creation of a mesh frame on which fibrinogen can settle. This coagulation factor is the final link in the coagulation system, interacting with the platelet plug to form a complete thrombus or clot;
- Activation of interconversion of coagulation factors. Aimed at accelerating the formation of fibrinogen and its transformation from a low-active form to an active one;
- Stimulation of the synthesis of platelets by the bone marrow and various substances by the vascular wall, which will speed up the blood clotting process and stop existing blood loss.
Important to remember! Platelets are responsible for the first step in starting blood clotting. If their number exceeds the norm, even in the absence of factors provoking coagulation, there is a threat of spontaneous initiation of blood clot formation in the lumen of blood vessels. In the case of a low platelet count, the risk of blood cell elements leaking through the vascular wall increases sharply, especially in conditions of decreased strength. This is manifested by an increased tendency to bleeding and spontaneous formation of hematomas!
According to recent studies from leading hematology clinics, a significant role of platelets in stimulating wound healing has been documented. This physiological phenomenon is associated with their production of specific growth factors that have a potentiating effect on cell proliferation in the lesion.
Finger prick blood test is a reliable method for determining platelet status
Symptoms
A decrease in platelets in childhood can manifest itself:
- Frequent appearance of bruises (sometimes they can even occur from touching).
- Prolonged bleeding from a cut or abrasion.
- Pinpoint rashes on the skin, as well as the appearance of spider veins or spider veins.
- Periodic occurrence of nosebleeds.
- Headaches.
- Bleeding of the mucous membrane of the gums.
- Acquiring a pink or red tint to the urine.
- The appearance of vomiting blood or blackening of stool.
- Heavy and too long periods in adolescence.
In some children, the spleen becomes enlarged, and in severe cases, hemorrhages occur in different locations, for example, in the retina or brain tissue.
What to do if there is a slight decline
If platelets are slightly reduced, the doctor will recommend:
- Change the child’s diet by adding foods that contain a lot of iron, vitamins C and A. Children with thrombocytopenia are advised to give buckwheat porridge, meat dishes, beets, carrots, cabbage, apples, fish, parsley, olive oil, bananas, nuts and others products. It is advised to avoid eating watermelon, seaweed, lingonberries, cranberries, wild strawberries, strawberries, and tomato juice.
- Monitor physical activity. The child should get enough rest, sleep at least 10-12 hours a day, and play calm games.
As for traditional medicine recipes, with a slight decrease in the number of platelets, the child can be given nettle juice mixed 1:1 with milk (total 100 ml per dose) or sesame oil (a tablespoon per dose). The medications are taken three times a day, half an hour before meals, but before you start using them, you should definitely discuss this issue with your pediatrician.
Platelets are blood cells that do not have their own nuclei and are responsible for the formation of a blood clot and stopping bleeding. Nuclear-free cells are formed, separating from megakaryocytes, in the bone marrow.
It is possible to determine why platelets are low in an adult, what this means, what diseases it indicates, by the degree of deviation of the analysis parameters from the norm.
Diagnostics
The final diagnosis of thrombocytopenia is made based on the patient's medical history, physical examination, and test results. If necessary, the patient is treated by a hematologist. This is a doctor who specializes in diagnosing and treating blood diseases.
Once thrombocytopenia is diagnosed, it is important that the cause of its development be determined. For this, various research methods are used: analysis of medical history, laboratory tests and instrumental diagnostics.
Disease history
During the study of the medical history, the doctor must ask the patient for answers to the following questions:
- What medications are taken, including over-the-counter drugs and herbal remedies. The content of quinine, which is often found in drinking water and food, is also determined.
- Do any close relatives have blood diseases?
- Have you had a recent blood transfusion, change sexual partners frequently, are you taking intravenous medications, or have you been exposed to contaminated blood or hazardous fluids at work?
Physical examination
During a physical examination, symptoms of bleeding, such as bruising or spots on the skin, may be detected. Be sure to check for signs of infection, such as fever. The abdomen is also felt (palpated), which makes it possible to determine an enlarged spleen or liver.
General blood analysis
This test measures the levels of red blood cells, white blood cells, and platelets in the blood. It involves taking a small amount of blood, usually from the patient's finger, and then examining it under a microscope. If thrombocytopenia occurs, the results of this test will show an insufficient platelet count.
Blood smear
A special technique is used to check the appearance of platelets using a microscope. This test also takes a small amount of blood, most often from a finger.
Bone marrow examination
Two tests are performed to study the functionality of the bone marrow: aspiration and biopsy.
A bone marrow aspiration may be done to find out why enough blood cells are not being created. For this test, the doctor takes a sample of bone marrow using a needle, which is then examined under a microscope. In pathology, defective cells are determined.
A bone marrow biopsy is often performed immediately after aspiration. For this test, the doctor takes a sample of bone marrow through a needle. Next, the tissue is examined, which checks the number and types of cells, including platelets.
Other diagnostic methods
Depending on the indications, ultrasound, computed tomography, and magnetic resonance imaging are performed. If there are concomitant diseases, the affected organs are examined.
Classification of thrombocytopenia
Grade 1 (moderate decrease in platelet count). With it, hemostasis is satisfactory, the indicator varies between 50-160X10/9 l.
Causes:
- Dysfunction of cardiac activity, disrupting blood flow to organs, respectively, their nutrition and normal functioning. Heart failure.
- Excessive use of diuretics, antitumor drugs, analgesics, pacemakers can lower the indicators.
- The period of gestation, due to changes in hormonal levels, vitamin deficiency, blood thinning.
- Therapy aimed at destroying cancer cells (radiation) can destroy the red marrow in the bone. Platelet production is disrupted.
- DIC - syndrome. The formation of blockages in small bloodstreams attracts the attention of platelets, which leads to their high consumption. This condition is possible with any pathological changes.
- Liver dysfunction due to illness. The organ synthesizes substances that promote blood clotting. Liver diseases disrupt the process, resulting in bleeding.
- Alcohol-containing drinks negatively affect the activity of the red marrow of the bone. As a result, the amount of folic acid, important for hematopoietic function, decreases. With alcohol dependence, the platelet count decreases significantly.
2nd degree (a sharp decrease in the number of blood plates) - accompanied by subcutaneous hemorrhages and heavy bleeding from injuries. The numbers drop to 20-50X10/9 liters.
Causes:
- Leukemia is characterized by the formation of cancer cells in the bone marrow. They replace hematopoietic tissue, which causes a decrease in platelet production.
- Incompatibility of the Rh factor of the blood of the mother and fetus leads to a hemolytic disease in the baby.
- Systemic lupus erythematosus.
- Intravascular coagulation is widespread throughout the body.
Grade 3 (dangerous, pronounced thrombocytopenia). It is characterized by abundant internal and external hemorrhages that appear spontaneously. Platelets in the blood are critically reduced and can be below 20X10/9 l.
Causes:
- Excessive use of anti-tumor drugs (overdose).
- Advanced form of leukemia.
- Radiation disease in acute form.
By form:
- Immune. The system is weakened due to a previous illness, often infectious or after abdominal surgery. Failures can also occur during intensive drug therapy.
- Heteroimmune. The negative impact of pathogenic microflora and toxic compounds on the structure of the antigen leads to disruption of its function.
- Isoimmune. The transition of cells during intrauterine development from the fetus to the woman, in case of incompatibility (type of Rh factor), leads to reduced levels of platelets in the blood. The cause may also be a blood transfusion from a donor to a recipient.
- Autoimmune. The body perceives platelets as a danger and produces antibodies against them.
Low platelet count: causes
A very low number of platelets in the blood can be caused by various factors.
- Herpes. Symptoms of this disease appear on the lips, the area around the nose, and on the surface of the genitals;
- Hepatitis. All types of the disease affect the liver, increase its size and are accompanied by inflammation of this human organ;
- Cold. All diseases such as ARVI, acute respiratory infections, tonsillitis, laryngitis, influenza and other diseases caused by infection, viruses or bacteria entering the human body;
- Mononucleosis. Can be transmitted through saliva and other human bodily fluids, caused by a virus;
- HIV and AIDS. A disease characterized by viral damage to the human immune system. Treatment of immunodeficiency is ineffective;
- Lupus and other autoimmune diseases. The body begins to fight its cells, mistaking them for pathogens;
- Gaucher's disease. A congenital pathology that affects the normal functioning of various human systems and organs: lungs, spleen, kidneys, liver and brain. Causes a decrease in glucocerebrosidase activity, symptoms may manifest as bone deformation;
- Blood cancer or oncology of another organ;
- Medicines (Heparin, Aspirin) that thin the blood;
- Blood thinning products (ginger, lemon, cherries, garlic, onions and others).
Sometimes platelets are low in a woman’s blood during pregnancy, with vitamin deficiency, enlarged spleen, or intoxication of the human body with alcohol or heavy metals. The causes may be different, so treatment should be prescribed only after identifying the origin of the disease.
Causes
Many factors can cause thrombocytopenia, therefore hereditary and acquired TP are distinguished. “Inherited” is when the affected gene was passed on to the offspring through parents. “Acquired” is when the disease develops throughout life. Sometimes the cause of the disease is unknown, then they talk about idiopathic thrombocytopenia.
Thrombocytopenia can develop for the following reasons:
Bone marrow doesn't make enough platelets
Bone marrow is spongy tissue found inside bones. It contains stem cells that develop into various blood cells: red blood cells, white blood cells and platelets. When stem cells are damaged, the entire process of hematopoiesis is disrupted, leaving platelets unable to form.
- Cancer
A cancerous condition such as leukemia or lymphoma can damage the bone marrow and destroy blood stem cells. Cancer treatment also negatively affects platelet counts, which is why thrombocytopenia is most often diagnosed with radiation and chemotherapy.
- Aplastic anemia
This rare and serious blood disorder prevents the bone marrow from producing enough new blood cells. This ultimately affects your platelet count.
- Toxic chemical compounds
Exposure to many toxic chemicals such as pesticides, arsenic and benzene can slow platelet production.
- Medicines
Some medications, such as diuretics and chloramphenicol, can slow platelet synthesis. Chloramphenicol (an antibiotic) is rarely used in the United States and other countries around the world. Common over-the-counter medications such as aspirin or ibuprofen can also affect platelets.
- Alcohol
Alcoholic drinks can slow platelet production. A temporary decrease in their levels is quite common among alcohol drinkers, especially if they eat foods low in iron, vitamin B12 or folic acid.
- Viral diseases
Chickenpox, mumps, rubella, Epstein-Barr virus, or parvovirus may temporarily reduce your platelet count. People who have AIDS also often suffer from thrombocytopenia.
- Genetic predisposition
Some genetic conditions can cause a low platelet count in the blood. Examples include Wiskott-Aldrich and May-Hegglin syndromes.
The body destroys its own platelets
A low platelet count may be detected even if the bone marrow is making enough platelets. The body can destroy its platelets due to autoimmune diseases, certain medications, infections, surgery, pregnancy, and certain conditions that cause increased coagulation.
- Autoimmune diseases
They occur when the body’s immune system mistakenly destroys platelets and other blood cells. If an autoimmune disease causes platelets to be destroyed, then thrombocytopenia may develop.
One example of this type of autoimmune disease is immune thrombocytopenia (ITP). This disorder involves continuous bleeding, meaning the blood does not clot as it should. An autoimmune response is thought to cause most cases of ITP.
Other autoimmune diseases that destroy platelets include lupus and rheumatoid arthritis.
- Medicines
A reaction to some medications may result in the body destroying its own platelets. Examples of drugs that can cause this disorder include quinine; antibiotics containing sulfate; and some anti-seizure medications such as Dilantin, vancomycin, and rifampicin.
During treatment with heparin, a pathological reaction leading to thrombocytopenia may also develop. This condition is called heparin-induced thrombocytopenia (HITP). Its development is most often associated with hospital treatment.
In HITP, the body's immune system attacks a substance made by heparin and a protein located on the surface of platelets. This attack activates platelets and they begin to form blood clots. Blood clots may form deep in the legs (deep vein thrombosis) or they may break and travel to the lungs (pulmonary embolism).
- Infection
A low platelet count may be the result of a bacterial infection in the blood. Viruses such as mononucleosis or cytomegalovirus can also cause insufficient platelet counts.
- Surgery
Platelets can be destroyed when they pass through artificial heart valves, blood vessel grafts, or machines and tubes used for blood transfusions or bypass surgery.
- Pregnancy
About 5% of pregnant women develop mild thrombocytopenia, especially during the prenatal period. The exact reason for this violation is unknown.
Additionally, some rare and serious diseases can cause low platelet counts. Examples of this are thrombocytopenic purpura and disseminated intravascular coagulation.
Video: Why platelet levels drop
Platelets are low in an adult, what does this mean?
- congenital hemophilia;
- increased production of antibodies caused by infection entering the body; anemia - people with pale skin need to be wary, especially if the slightest blows cause bruises;
- leukemia;
- asphyxia – very often thrombocytopenia develops in people suffering from bronchial asthma;
- disseminated intravascular coagulation syndrome (DIC syndrome);
- viral and autoimmune diseases of various origins;
- severe injuries leading to significant blood loss;
- surgical intervention;
- hemodialysis - blood purification using a special device;
- professional activity in hazardous conditions;
- uncontrolled use of antibiotics, corticosteroids, cytostatics, diuretics, painkillers;
- thyrotoxicosis;
- abuse of alcoholic beverages, which dilate blood vessels, resulting in increased blood pressure.
In women, the cause of a situation where platelets are low can be menstruation and pregnancy.
For reference. If the platelet count has not decreased very much, then you can return it to normal at home.
If platelets are low in an adult, it is recommended to follow these rules:
- If possible, get an office position;
- reduce working hours (up to a maximum of 8 hours);
- sleep at least 8 hours;
- give up dangerous sports;
- do aerobics and other types of cardio exercises;
- increase the consumption of vegetables, herbs, berries, fruits, eggs, flaxseed oil, salmon and tuna meat, vitamin C and glucose;
- give up refined sugar;
- exclude cold drinks;
- Drink coffee and mulled wine periodically (but don’t get too carried away).
If platelets are significantly lower than normal (to a level of 20-50 g/l of blood), then outpatient treatment will be required. If the level drops below 20 g/l, then hospitalization is necessary.
Before prescribing treatment, the doctor finds out why the concentration of blood platelets has dropped below normal. Only by eliminating the cause of the pathology can you get rid of the problem.
Usually, if a decrease in platelets is detected, the doctor prescribes:
- intravenous administration of immunoglobulin;
- taking glucocorticosteroids;
- use of anti-Rhesus serum;
- platelet transfusion.
What foods to exclude to increase clotting?
Certain foods can affect blood thinning or thickening. If coagulation rates are low, it is necessary to remove or reduce the consumption of foods that are not allowed for thrombocytopenia.
Article on the topic: Why pain occurs under the right shoulder blade
They are as follows:
- Green tea;
- Blueberry;
- Fresh tomatoes;
- Pepper;
- Garlic;
- Ginger;
- Celery juice, raspberry juice;
- Sea fish;
- Yogurts and kefir;
- Low-fat meat (turkey and chicken);
- Nuts;
- Sunflower seeds
- Olive oil;
- and others.
The following herbs also lead to low platelets:
- Fresh nettle;
- Yarrow;
- Burdock;
- Needles;
- Burnet;
- and others.
A certain list of medications also affects greater blood thinning, so you should stop using the following medications:
- Aspirin;
- Phenilin;
- Chime;
- ThromboAss;
- Cardiomagnyl;
- Ginko Biloba;
- Aspecard.
Development cycle
All platelets are formed in the bone marrow.
It all starts with a colony-forming megakaryocytic unit, also called a “CFU-Meg”. It divides by mitosis. From it, a promegakaryoblast is first formed, which turns into a megakaryoblast. Over the course of 4-5 days, special cells mature in the bone marrow - megakaryocytes, the diameter of which is about 60-120 microns. They are preceded by a special form with granular basophilic cytoplasm and a tendency towards nuclear polymorphism. It is called a "promegakaryocyte". A mature megakaryocyte is distinguished by the large size of its cytoplasm and the presence of purple-pink grains in it. The core in it is rough, it can be of various bizarre shapes.
It is from the cytoplasm of the megakaryocyte that small blood cells resembling discs are separated. From this moment we can already talk about the life expectancy of platelets. As a rule, only mature forms are assessed. There should be about 90% of them in the body of a healthy person.
Number of cells
To understand why there is such a concentration of nuclear-free bodies in the blood, you need to know not only the life expectancy of platelets, but also the speed and quantity of them that appear. For every kilogram of human weight there are about 15x106. About 3,000 platelets are released from each megakaryocyte during division. Another 7-17% of the total is formed in the lungs. This happens because proplatelets also enter the bloodstream. They independently reach the microcircular bed of the lungs. And already in it the process of releasing platelets occurs.
Every day the human body produces about 66 ± 14.6 thousand platelets per microliter of blood. In the blood of an adult there should be from 180 to 320x109 of these blood cells, in children they can be from 150 to 450x109. But when calculating their number, it is necessary to take into account age. For example, in newborns who are not yet 10 days old, they can be from 99 to 420x109.
Norm and deviations
The level of thromboplastins is measured in thousands of units per 1 microliter of blood. In laboratory test results, the indicator appears as "PLT" or "Platelets".
Table: Permissible limits for platelet levels in people of different ages
| Age | PLT units/µl |
| Adult men | 200 – 400 |
| Adult women | 180 – 320 |
| Children 5 – 7 years old | 180 – 450 |
| Children 1 – 5 years old | 180 – 380 |
| Children from 1 – 12 months | 150 – 350 |
| Newborns up to 1 month | 100 – 420 |
Interesting! In women during pregnancy, the normal threshold decreases to 100 units, and during menstrual bleeding - to 75. This way, the body reduces the likelihood of thrombosis in pregnant women and prevents blood clots from forming during menstruation.
A decrease in the number of platelets is called thrombocytopenia, an excess of the norm is called thrombocytosis. Both deviations signal pathology, so they cannot be ignored.
Thrombocytosis
An increased number of thromboplastins can signal tuberculosis, leukemia, and cancer of internal organs. Deviation is also observed in patients with erythrocytosis, arthritis, myeloid leukemia, as well as in acute infectious diseases.
Thrombocytosis left untreated leads to essential thrombocythemia, a chronic myeloproliferative disease when a tumor arises from a stem (maternal) blood cell from its descendants. A large number of thromboplastins, which are produced in response to tumor growth, function normally, but increase the risk of thrombosis in small vessels.
In case of injury, surgery, or alcoholism, thrombocytosis is secondary. The body is forced to actively produce thrombopoietin, which regulates the processes of cell division and maturation in the red brain. Regardless of the reason for exceeding the norm, it is necessary to consult a doctor and prescribe suitable treatment.
Before making a diagnosis, a number of studies are required:
- determination of the amount of C-reactive protein;
- Ultrasound of internal organs;
- complete urine analysis;
- determination of hemoglobin level;
- triple analysis for thrombomass with a frequency of 3–5 days.
To reduce the indicator, the doctor may prescribe medications based on blood thinning acetylsalicylic acid. You will also need to rationalize your diet - add foods that increase blood volume and contain magnesium (lemon, ginger, beets, tomatoes, fish oil), and also drink at least 2.5 liters of water per day.
What is spontaneous thrombocytopenia?
A decrease in blood clotting occurs with hepatitis, chronic connective tissue damage, leukemia of the lymph nodes, and other pathologies.
At the moment when there is an absence of primary symptoms during the disease, or when they cannot be established, a diagnosis of thrombocytopenic purpura, also called independent thrombocytopenia, is made. In old age, these pathologies in most cases occur in a chronic form, and in 5-7% of cases the disease ends in death, with open bleeding or hemorrhage in the brain.
FACT! Spontaneous thrombocytopenia in children in most cases occurs in an acute form, but in 80% of cases its outcome is recovery. If you notice symptoms, do not hesitate to contact a qualified physician.